Living through the coronavirus disease-2019 (COVID-19) pandemic has been the sentinel medical event in most of our professional lives. In the hot spots across America, cardiologists and trainees are deeply immersed working closely with physicians of all specialties as COVID providers. Even in less affected locales, preparations have been made, and the call to duty has been heard. There have been numerous recent perspectives written by clinicians conveying their experience, emotions, and advice on how to cope and care for the victims of this crisis (1,2). As we hear whispers of a “flattening disease prevalence curve” in New York City, and a hint of optimism from the West Coast thanks to early social distancing directives, we are forced to confront the challenging question of what comes next. When we reach the “end” of the COVID era, how will our lives have changed as practicing cardiologists, fellows in training (FITs), and human beings in society at large?
The Practice of Cardiology
Disease burden
It would be foolish to think that at the start of the next academic year everything will return to the way it was. Epidemiologists, economists, and politicians recognize that COVID-19 cases and their indirect effects will linger well into the future. From an inpatient perspective, we are witnessing multiorgan damage from COVID-19, including thrombotic sequelae, marked kidney injury, and cardiac arrhythmias. As cardiologists, we should expect an influx of outpatients who suffered cardiac complications from COVID or for whom hospitalization unmasked conditions of hypertension, diabetes, coronary artery disease, or cardiomyopathy (3). Pent-up demand from patients who avoided cardiac care during the crisis will further contribute to outpatient volume.
Globally, there has been a marked decline in non-COVID medical disease presenting to hospitals, such as myocardial infarctions (MI) (4). Theories abound on whether the decrease in MI represents an actual reduction with at-risk individuals abstaining from triggers or whether patients are avoiding the health care system and infarcting at home. Recent reports of non-COVID mortality statistics from New York of those who never make it to the hospital are alarming (5). In COVID patients, electrocardiographic abnormalities consistent with acute MI do not always represent obstructive coronary disease (6). As true ST-segment elevation MI volumes resurge, discussions favoring fibrinolysis, recently resurrected to reduce personnel exposure and due to delays in door-to-balloon time, should diminish, to re-emphasize primary percutaneous coronary intervention as the standard of care (7).
Processes of re-engagement
At the pandemic’s peak, we limited cardiac testing to emergent indications; however, this will not be tenable moving forward. The American College of Cardiology Interventional Council and Society for Cardiovascular Angiography and Interventions differentiate elective cases from those in which deferment may result in adverse clinical outcomes (8). Postponing cardiac resynchronization therapy in congestive heart failure or delaying a routine echocardiogram in severe valvular disease can have profound repercussions on individual health. The re-engagement of elective procedures will be highly dependent on each hospital system, acknowledging the community’s disease burden and viral projections. However, the basic path to reintegration will include the following: 1) availability of medical staff and the infrastructure to proceed with elective interventions; 2) creation of “COVID-free” areas and implementation of same-day discharge protocols as feasible; 3) categorization of procedures by type; and 4) appraisal of cases by a designated subspecialty review board (9). In this setting, monitoring of iatrogenic COVID-19 cases as a function of total volume will be integral.
Until vaccine development becomes a reality or herd immunity kicks in, we expect ubiquitous use of personal protection equipment during all procedures and outpatient visits. Proponents of “immunology passports” to document severe acute respiratory syndrome coronavirus-2 immunity neglect the limitations of testing, uncertainties of immunology, and associated ethical hazards (10). When an effective COVID vaccination becomes available, we expect there to be tax penalties for refusal and a quality metric for our patient panels. COVID status will additionally become integral to the standard history of present illness. For protection of all parties involved, same-day nasal swab testing and documentation of antibody status should become standard for patients undergoing any invasive cardiac procedure. In our clinical laboratories, deep cleaning protocols must be enforced between cases despite delays in turnaround time and consequences to case volume.
Financial burden
Hospital systems and private practices have suffered considerable financial losses in prioritizing care for patients with COVID-19 coupled with a precipitous decline in elective procedures. The bipartisan CARES (Coronavirus Aid, Relief, and Economic Security) legislation has allocated at least $50 billion to support hospital systems and health care providers (11), and private physician offices and faculty practices are eligible to apply for several loan-based programs, including the Paycheck Protection Program and Emergency Economic Injury Disaster Loans (12). Without the CARES Act and future government intervention, many practices and hospitals will not survive into the future.
Tele-health
One of the silver linings of this human crisis has been cardiology engagement with 21st-century technology. Even though the opportunity to perform video visits has been present for over a decade (13), it has taken a pandemic for telemedicine to be nationally accepted. Centers for Medicare and Medicaid Services has buttressed this effort by the development of toolkits to support states in implementing tele-health for Medicaid and Children’s Health Insurance Program beneficiaries (14). For the duration of the public health emergency, Medicare will pay physicians for services provided during telemedicine visits at equivalent rates to office visits (15). As its use persists post-crisis, expectations of an optimal e-visit will evolve. Patients will obtain their own vitals using home monitors. The transmission of modified electrocardiograms through cell phone apps will be standard. Patient-held telemedicine stethoscopes could preserve auscultation as integral to our cardiology identity. In many ways, telemedicine represents a modern adaption of the home visits performed by our 20th-century predecessors (13).
Fellows-in-Training
In the past months, FITs have learned skills in critical care, virology, and palliative medicine as frontline providers. Yet, we must remain committed to core cardiology education. Despite the Accreditation Council for Graduate Medical Education’s leeway to cancel conferences in pandemic emergency status, we have resisted this, deciding that maintaining education provides stability in disruptive times. Video conferencing has been a success, with widespread participation of fellows and faculty. Whereas live lectures will gradually return, video conferencing will persist in parallel with improved HIPAA (Health Insurance Portability and Accountability Act of 1996)-compliant platforms and interinstitutional sharing. Virtual education is being embraced at international levels. There were over 38,000 attendees representing more than 135 countries at the virtual American College of Cardiology/World Congress of Cardiology Scientific Sessions this year, validating the concept that online learning is far-reaching and inclusive for trainees who may not be able to participate due to financial or logistical reasons.
Loss of rotations and cases has also imperiled fellows in many programs to fall short of procedural requirements. For some, this will mean extension of training pathways, but it will also force educators to reconsider how we teach. Simulation training platforms can provide virtual repetition and pattern recognition for procedures such as transthoracic or transesophageal echocardiography, vascular access, and even structural heart interventions. The distinction between procedural competency and procedure quantity has never been so important to define. FITs themselves have become proponents of creative ways to enhance patient care and education through multidisciplinary care teams, tele-health forums, and social media platforms for international idea exchange (16).
There will certainly be adjustments made for onboarding new fellows this July. It is also likely that the fall 2020 fellowship interview season will be conducted virtually at most institutions. Replicating the in-person interview experience in the digital space will be a formidable challenge. The realities of this era have also reignited the debate of what constitutes the optimal training pathway to be a cardiac intensivist, and who ultimately should be staffing our critical care units. FITs may find new incentives to pursue careers in cardiac critical care. The inherent self-sacrifices by health care providers in this pandemic may inspire a new cadre of clinicians and researchers motivated by the greater good, while dissuading those primarily driven by self-centered ambition.
Community-based impact
With many in self-isolation, the community-based impact of COVID-19 on cardiovascular health will be important to monitor. Exercise programs via online platforms have become pervasive, but will they be enough to counter inactivity while at home? Home quarantine and closing of restaurants have left many to cook for themselves, but will the health benefits of home cooking be mitigated by the potential increased purchasing of “comfort foods” and preservative-laden choices with long shelf lives (17)? FITs who have “grown up” in an era where technology and health care intersect are in an optimal position to innovate and apply technology-based solutions to cardiovascular home health. As an example, the Johns Hopkins Corrie mobile health solution app represents a self-management tool for patients who have suffered an MI to enhance recovery by focusing on lifestyle modification, mindfulness techniques, and constructive data-driven feedback (18).
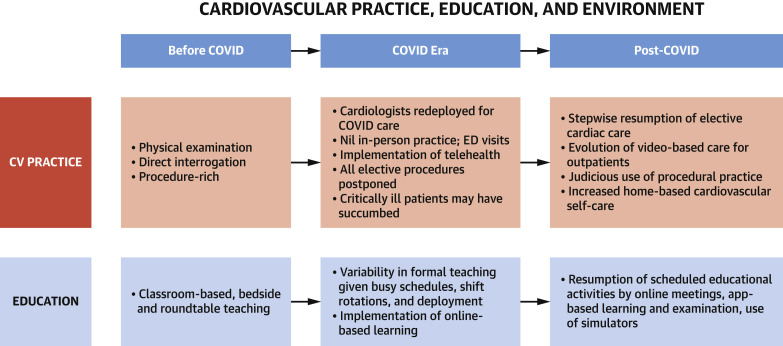
The COVID-19 pandemic will leave a profound imprint on cardiologists, trainees, and society for years to come (Figure 1 ). We will have supported each other to the best of our ability, understanding that the mental health sequelae for health care professionals will be important to address. Although none of us have absolute foresight, we must learn from the harsh lessons faced and plan for medical changes, including the deluge of cardiac care patients that will fill our clinics, flexibility of FITs’ education to support cardiovascular training, and continued integration of clinical science and technology.
Figure 1.
Cardiovascular Practice, Education, and Environment
The coronavirus disease (COVID) 2019 pandemic has resulted in significant changes for cardiology practice and trainee education. CV = cardiovascular; ED = emergency department.
Beyond medicine, some doubts linger. When will we feel comfortable hugging a friend? In New York City, when will Madison Square Garden host its next sporting event? Will our communities survive the economic devastation from prolonged closure? If history has taught us anything, it is that humanity is resilient. At our core, we are social beings, and in time, as we work to get past this and the memories begin to fade, we will re-engage in the social embraces crucial to our soul. But for some time, we must adapt to a “new normal.” Let us use this calamity to improve how we educate our trainees and enhance patient care. From the ashes, our society will emerge more united than ever before, and with a greater consciousness for public good.
Footnotes
Both authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Narula N., Singh H.S. NYC innocence lost: cardiology in the COVID-19 pandemic. Circulation. 2020;141:2039–2041. doi: 10.1161/CIRCULATIONAHA.120.047265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yong C. COVID-19: the isolation that has brought us together. J Am Coll Cardiol. 2020;75:2639–2641. doi: 10.1016/j.jacc.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 Mar 27 doi: 10.1001/jamacardio.2020.1017. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NYC Health . April 14, 2020. Confirmed and Probably COVID-19 Deaths Daily Report.https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-confirmed-probable-daily-04152020.pdf Available at: Accessed April 15, 2020. [Google Scholar]
- 6.Bangalore S., Sharma A., Slotwiner A. ST-segment elevation in patients with COVID-19: a case series. N Engl J Med. 2020 Apr 17 doi: 10.1056/NEJMc2009020. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahmud E., Dauerman H.L., Welt F.G. Management of acute myocardial infarction during the COVID-19 pandemic. J Am Coll Cardiol. 2020 Apr 21 doi: 10.1016/j.jacc.2020.04.039. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Welt F.G.P., Shah P.B., Aronow H.D. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC's Interventional Council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah P.B., Welt F.G.P., Mahmud E. Triage considerations for patients referred for structural heart disease intervention during the coronavirus disease 2019 (COVID-19) pandemic: an ACC /SCAI consensus statement. J Am Coll Cardiol Intv. 2020;13:1484–1488. doi: 10.1016/j.jcin.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . April 24, 2020. “Immunity Passports” in the Context of COVID-19.https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19 Available at: Accessed April 25, 2020. [Google Scholar]
- 11.Health and Human Services . 2020. CARES Act Provider Relief Fund.https://www.hhs.gov/coronavirus/cares-act-provider-relief-fund/index.html Available at: Accessed April 25, 2020. [Google Scholar]
- 12.U.S. Department of the Treasury . 2020. The CARES Act Provides Assistance to Small Businesses.https://home.treasury.gov/policy-issues/cares/assistance-for-small-businesses Available at: Accessed April 25, 2020. [Google Scholar]
- 13.Nesbitt TS. The evolution of telehealth: Where have we been and where are we going? In: Board on Health Care Services; Institute of Medicine, editors. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Washington, DC: National Academies Press; 2012. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207141/. Accessed April 15, 2020. [PubMed]
- 14.Centers for Medicare and Medicaid Services . 2020. State Medicaid and CHIP Telehealth Toolkit: Policy Considerations for States Expanding Use of Telehealth: COVID-19 Version.https://www.medicaid.gov/medicaid/benefits/downloads/medicaid-chip-telehealth-toolkit.pdf Available at: Accessed April 25, 2020. [Google Scholar]
- 15.Centers for Medicare and Medicaid Services . April 7, 2020. Dear Clinician [letter]https://www.cms.gov/files/document/covid-dear-clinician-letter.pdf Available at: Accessed April 25, 2020. [Google Scholar]
- 16.DeFilippis E.M., Stefanescu Schmidt A.C., Reza N. Adapting the educational environment for cardiovascular fellows-in-training during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2630–2634. doi: 10.1016/j.jacc.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muscogiuri G., Barrea L., Savastano S. Nutritional recommendations for COVID-19 quarantine. Eur J Clin Nutr. 2020;74:850–851. doi: 10.1038/s41430-020-0635-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corrie Stay Healthy and Safe With Virtual Healthcare Services. https://corriehealth.com Available at: Accessed April 25, 2020.