The coronavirus disease 2019 (COVID-19) spreads rapidly across the globe in early 2020.1 In Taiwan, there were 429 confirmed COVID-19 cases and 6 deaths as of April 30.2 The outbreak has created unprecedented burden on the society and health care system, particularly the frontline emergency department (ED).
The National Taiwan University Hospital (NTUH) is a 2000-bed tertiary center in Taipei, Taiwan, with approximately 100,000 ED visits annually. We retrospectively collected data regarding ED census and cardiac arrest from the hospital information system from January 2019 to April 2020. Patients with do-not-resuscitate status were excluded. The incidence of in-hospital cardiac arrest (IHCA) in the ED was calculated as the number of IHCA events in the ED divided by the number of ED visits on a monthly basis. The study was exempted from the purview of the hospital’s institutional review board. Linear spline regression was used to test the change in slope before and after the COVID-19 pandemic.
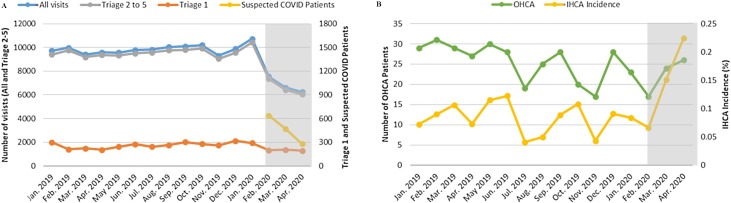
Amid the COVID-19 pandemic, the number of ED visits decreased significantly from approximately 9000–6000 visits per month (change in slope, −1758/month, p = 0.001, Fig. 1 , Panel A). The ED visits with triage levels 2–5 had a similar decreasing trend, while the number of sickest patients with triage level 1 remained unchanged (change in slope, −46/month, p = 0.06). Of note, a new designated outside unit was established in February for suspected COVID-19 patients, where ED staff collected swab samples in full personal protective equipment (PPE). From February to April, we saw 1368 suspected COVID-19 patients, 6 of whom were confirmed. Despite a low prevalence of COVID-19 in the community, ED visits still decreased. This may result from the general public’s fear of getting infection in the hospital,3 as well as government’s advisory to stay at home.4 Nonetheless, the sickest patients cannot avoid a trip to the ED, as shown in our results. The same workload for the high-acuity patients, with additional burden of suspected COVID-19 patients, may overwhelm the ED.
Fig. 1.
Impact of the COVID-19 Pandemic on Emergency Department Services and Cardiac Arrest from January 2019 to April 2020. Shaded region corresponds to the pandemic period in Taiwan. (Panel A) A decreasing trend of ED visits is noted overall, as well as for visits with triage levels 2–5. The number of ED visits with triage level 1 remains unchanged. A separate unit for suspected COVID patients was established in February 2020. (Panel B) The number of OHCA patients remains stable; however, the incidence of IHCA in the ED increases significantly during the pandemic period.
COVID-19 = coronavirus disease 2019; ED = emergency department; OHCA = out-of-hospital cardiac arrest; IHCA = in-hospital cardiac arrest.
As shown in Fig. 1 (Panel B), the number of out-of-hospital cardiac arrest (OHCA) remained largely unchanged during the pandemic (change in slope, +4/month, p = 0.07). By contrast, the incidence of IHCA in the ED increased significantly (change in slope, +0.08% per month, p < 0.001). The stable trend of OHCA in our study differed from the Italian report showing an increasing trend of OHCA during the pandemic.5 It may be that the prevalence of COVID-19 in Taiwanese communities was too low to impact the OHCA number. However, the psychological and physical impact of COVID-19 on healthcare providers are substantial that might lead to lapses in care for non-COVID patients. For example, a team of ED staff was allocated to care for suspected COVID patients, leading to staff shortage in other areas of the ED. Also, more time spent on donning and doffing PPE, more cautious inhalation therapy, and a longer laboratory turnaround, all of which may result in possible delay in care and collateral damages, such as an increase in IHCA incidence.
In summary, we found that COVID-19 pandemic may alter the distribution of emergency services acuity, with sickest patients still presenting to the ED. Additional burden of caring for suspected COVID patients may inadvertently cause collateral damage, such as an increase in IHCA incidence in the ED.
Conflict of interest statement
The authors have no conflicts of interest to disclose.
Funding
None.
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 2020. Coronavirus disease 2019 (COVID-19) situation report—101.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200430-sitrep-101-covid-19.pdf?sfvrsn=697ce98d_4 [Google Scholar]
- 2.Taiwan Centers for Disease Control. Coronavirus disease 2019 (COVID-19). https://www.cdc.gov.tw/en/Disease/SubIndex/.
- 3.Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N Engl J Med. 2020 doi: 10.1056/NEJMp2008017. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 5.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2010418. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]