Abstract
Cancer undergoes “immune editing” to evade destruction by cells of the host immune system including natural killer (NK) cells and cytotoxic T lymphocytes (CTLs). Current adoptive cellular immune therapies include CAR T cells and dendritic cell vaccines, strategies that have yet to show success for a wide range of tumors. Cancer resistance to immune therapy is driven by extrinsic factors and tumor cell intrinsic factors that contribute to immune evasion. These extrinsic factors include immunosuppressive cell populations such as regulatory T cells (Tregs), tumor-associated macrophages (TAMS), and myeloid-derived suppressor cells (MDSCs). These cells produce and secrete immunosuppressive factors and express inhibitory ligands that interact with receptors on T cells including PD-1 and CTLA-4. Immune checkpoint blockade (ICB) therapies such as anti-PD-1 and anti-CTLA-4 have shown success by increasing immune activation to eradicate cancer, though both primary and acquired resistance remain a problem. Tumor cell intrinsic factors driving primary and acquired resistance to these immune therapies include genetic and epigenetic mechanisms. Epigenetic therapies for cancer including DNA methyltransferase inhibitors (DNMTi), histone deacetylase inhibitors (HDACi), and histone methyltransferase inhibitors (HMTi) can stimulate anti-tumor immunity in both tumor cells and host immune cells. Here we discuss in detail tumor mechanisms of immune evasion and how common epigenetic therapies for cancer may be used to reverse immune evasion. Lastly, we summarize current clinical trials combining epigenetic therapies with immune therapies to reverse cancer immune resistance mechanisms.
Keywords: cancer, immune evasion, epigenetic, DNA methyltransferase inhibitor, histone deacetylase inhibitor
Cancer Immune Evasion
Cancer cells avoid the immune response in a process known as “immune editing” or immune evasion1. Initially, lymphocytes including cytotoxic T cells and natural killer (NK) cells target cancer cell elimination by secreting perforin and granzyme or by the death ligand/death receptor pathway 2. Perforin creates pores in the membrane of the target cell, which allows granzyme to enter, triggering apoptosis. Death ligands like TNFα, FasL or TRAIL secreted by or expressed on the surface of cytotoxic T cells or NK cells interact with death receptors on cancer cells to trigger apoptosis2. Though these cancer elimination mechanisms are the same in cytotoxic T cells and NK cells, the activation of these two cell types differs. NK cells have non-specific cell targets and are activated when activating receptors are stimulated more than inactivating receptors by ligands expressed by the cancer cell3. For instance, MHC class I is an NK cell inhibitory ligand expressed by the cancer cell. On the contrary, cytotoxic T cells are specific to peptides presented by MHC class I molecules, so expression of MHC class I molecules is required for cytotoxic T cell activation. Activation of the cytotoxic function requires TCR-CD3 complex recognition of the specific peptide bound to the MHC class I, as well as two co-stimulatory signals through the CD8 and CD28 molecules2. Activation of NK cells results in immediate cytotoxic function, whereas activation of CD8 T cells requires priming by an antigen-presenting cell and then time to develop cytotoxic function. During cancer initiation, cells including natural killer cells and T effector cells fight and kill the cancer cells, but as tumors progress they exhibit mechanisms of immune suppression. These include expression of PD-L1, a ligand for the PD-1 protein on CD3 T cells, that inhibits killer T cell action against tumor cells. In addition, T regulatory cells that express CTLA-4 and normally suppress autoimmunity secrete cytokines to inhibit the action of T and NK cells against tumors1. In addition, suppressive immune cell populations can infiltrate tumors to promote immune evasion.
Regulatory T cells
Regulatory T cells (Tregs) play a key role in suppressing effector T cell (Teff) immune responses in order to maintain self-tolerance4. Tregs suppress immune responses through the secretion of cytokines that inhibit effector T cells. These cytokines include IL-35, IL-10, and TGF-β5. In the tumor microenvironment, Tregs downregulate antitumor immune responses. In many human tumor types, there is increased infiltration of Tregs into the tumor microenvironment6. In addition, elevated levels of Tregs are associated with increased tumor invasion, and a more favorable balance of T effector cells to T regulatory cells is associated with better patient outcomes7.
Tumor-Associated Macrophages
Macrophages are phagocytic myeloid cells that reside in tissues and act as immune sensors8. Tumor-associated macrophages (TAMs) contribute to resistance to immune therapy through a variety of mechanisms. TAMs include both M1 macrophages (classically activated) and M2 macrophages (alternatively activated), though M2 macrophages are the majority in many tumor types9. These TAMs are recruited to tumors in large numbers by chemokines such as CSF1, CCL2, and CXCL1210. M2 macrophages promote tumor progression and metastasis, and TAM infiltration is associated with poor prognosis in cancers11. TAMs suppress antitumor immunity through the recruitment of MDSCs to the tumor and can suppress the T cell immune response directly through the expression of the immunosuppressive ligand PD-L110.
Myeloid Derived Suppressor Cells
Another class of immune cells with an inhibitory effect on the anti-tumor immune response are myeloid derived suppressor cells (MDSCs). MDSCs are associated with the promotion of angiogenesis and tumor invasion and create an immunosuppressive environment that promotes the growth of malignant cells12. Activated MDSCs recruit Tregs through the secretion of TGF-B and IL-1013. MDSCs also inhibit anti-tumor cells such as CTLs, dendritic cells, and NK cells14, creating a suppressed immune environment that promotes cancer growth13. MDSCs express arginase, which inhibits T cell and NK cell proliferation through the depletion of L-arginine15. Additionally, MDSCs express high levels of inducible NO synthase (iNOS), which leads to the accumulation of NO and causes T cell anergy through inhibition of the IL-2 pathway. MDSCs produce high concentrations of reactive oxygen species (ROS) which are known to impair TCR signaling and induce T cell apoptosis. MDSCs express high levels of indoleamine 2,3-dioxygenase (IDO), which degrades tryptophan, inducing anergy and cell cycle arrest in T cells. MDSCs can also inhibit T cells through the expression of immunosuppressive ligands such as PD-L1 and death receptor CD9513. Increased MDSC frequency is correlated with poor patient prognosis16 and increased levels of MDSCs in the tumor microenvironment are associated with increased resistance to immune therapies17.
Cancer immunotherapy
Adoptive cell therapies
As our understanding of the immune system’s capacity for anti-tumor response grows, researchers have developed new strategies to initiate and strengthen the anti-tumor immune response including adoptive T cell therapy, CAR T cell therapy, and dendritic cell vaccines. The anti-tumor immune response depends most basically upon the ability of T cells to infiltrate the tumor while being able to recognize and react to cancer-specific antigens. One method for achieving this is Chimeric Antigen Receptor (CAR) T cell therapy. CAR T cells are engineered to express synthetic receptors specific to cancer cells, allowing for subsequent tumor elimination18. CAR T cells have demonstrated success in eradicating specific hematological cancers including acute lymphoblastic leukemia19. B cell leukemia patients who were treated with CD19 CAR T cell therapy showed complete eradication of the cancer and significantly improved outcomes. However, clinical results in solid tumors have been less impressive due to difficulty selecting a suitable target antigen and lower T cell infiltration20. In addition, while CAR T cell therapy has displayed encouraging results, significant issues remain with regards to toxicity. CAR T cell therapy may cause Cytokine Release Syndrome (CRS), a spectrum of inflammatory symptoms caused by immune activation of large numbers of lymphocytes that can be very toxic to patients21.
Cytokine-Induced Killer (CIK) cells are a similar type of adoptive cell therapy that have proven to be better tolerated than CAR T cell therapy. CIK cells are a heterogenous preparation of natural killer (NK) cells and CD3+ T lymphocytes that possess enhanced cytotoxic activity, allowing them to recognize and kill tumor cells with minimal residual disease22,23. Thus far, clinical trials with CIK adoptive cell therapy have shown a recurrence-free survival (RFS) benefit and overall survival (OS) benefit in some cases24.
Another class of adoptive cell therapy seeks to harness the power of dendritic cells, the immune system’s most potent antigen-presenting cells. Dendritic cell vaccines load dendritic cells with antigens which, upon administration, activate antigen-specific T cells to trigger an immune response25. In many clinical trials, DC vaccines induce tumor-specific T cell responses, though significant evidence for clinical efficacy of DC vaccines alone is yet to be seen26. The combination of DC vaccines with other therapies has shown promise in several clinical trials and is an area of active research.
CTLA-4 Immune Checkpoint and Drug Target
Immune checkpoints are pathways within the immune system that normally maintain self-tolerance but can be co-opted by tumors to evade destruction. By disrupting these pathways with monoclonal antibodies, immune checkpoint therapies can strengthen the anti-tumor immune response and improve patient outcomes27. One of the best characterized immune checkpoints is CTLA-4, a receptor on the surface of T cells that acts as a negative regulator of T cell activation when bound to a B7 protein on the surface of an antigen-presenting cell28. CTLA-4 also plays a major role in driving the suppressive function of regulatory T cells, ultimately inhibiting effector T cell responses29. Blocking the CTLA-4 pathway with anti-CTLA-4 monoclonal antibodies including ipilimumab and tremilimumab leads to more T cell activation and proliferation and reduced Treg-mediated immunosuppression. The anti-CTLA-4 drug ipilimumab produces significant, durable responses in about 20% of melanoma patients but has not shown similar promise in clinical trials for other solid tumors, exhibiting less than 10% response rates27,30.
PD-1 Immune Checkpoint and Drug Target
Programmed Death 1 (PD-1) checkpoint bears similarities to CTLA-4, ultimately acting as a negative regulator of T cell function. When PD-L1 binds to PD-1, it inhibits T cell proliferation and cytokine production, decreasing the T cell immune response31. Monoclonal antibodies blocking PD-1 produce an anti-tumor response in a variety of cancers. Melanoma patients exhibit the best response to anti-PD-1 (about 30% objective response rate) with renal cell carcinoma (30%) and non-small cell lung cancer (about 20%) close behind27,32. However, many common solid tumors such as breast, colon, ovarian, and pancreatic cancer have less than a 10% overall response rate to anti-PD-127.
In addition to anti-CTLA-4 and anti-PD1 therapies, many other receptors are the subject of ongoing research for cancer therapeutics, including LAG-3, Tim-3, VISTA, ICOS, OX40 and 4–1BB33. LAG-3 inhibits TCR signaling by interacting with MHC II34, and Tim-3 inhibits T cells through the binding of ligands which include Galectin-9, Ceacam1 and HMGB135. VSIG-3 is the ligand for VISTA, which also acts by inhibiting T cells36. OX40, 4–1BB and ICOS are all co-stimulatory molecules, therefore interactions with OX40 (CD134) and 4–1BB (CD137) enhance T cell differentiation and cytotoxic function. Antibodies against LAG-3, Tim-3, or VISTA block T cell inhibition (antagonist) whereas antibodies against OX40, 4–1BB or ICOS act as agonists, augmenting T cell function37. Therapies targeting these receptors are in the preclinical stages of development and have the potential to yield exciting responses either alone or in combination with anti-CTLA-4 or anti-PD-1.
Resistance to immunotherapy in cancers
The above immune therapies demonstrate significant advances for the treatment of many different types of cancer. However, as noted, none is curative for a majority of patients. Cancer resistance to immune therapy results from a variety of factors within the tumor microenvironment that can either prevent cytotoxic anti-tumor cells from infiltrating or make it unfavorable for these cells to survive and function appropriately upon infiltration. The unfavorable microenvironment is largely due to two main immunological factors: immunosuppressive cytokines and inhibitory immune checkpoints. Suppressive immune cells are the main contributors to this unfavorable tumor microenvironment. Cancer resistance to immunotherapy can also result from tumor cell-intrinsic factors, which can be categorized as primary or acquired resistance. Primary resistance is natural resistance to immunotherapy that can occur prior to treatment (non-responders), while acquired resistance can develop in response to immunotherapy treatment (initial responders who relapse). Mechanisms of primary resistance may include a reduction in antigen expression, changes in cell surface receptor expression, and changes in metabolic pathways38.
Cancer resistance to immune therapy is epigenetically controlled
Just as cancers are defined by genetic alterations, the epigenetic landscape of cancers is significantly altered compared to normal cells. Cancers exhibit changes in the silencing DNA methylation modification. DNA methylation is the addition of a methyl group to the cytosines of CpG dinucleotides by DNA methyltransferases (DNMTs). Cancers generally exhibit global loss of methylation at repetitive element regions, which are silenced to preserve genome stability in normal cells39. Conversely, cancers exhibit a gain of methylation and other suppressive epigenetic modifications at the promoter regions of tumor suppressor genes39. Therapies that target DNA methylation have shown promise in many types of cancer. 5-azacytidine (Aza) is a cytidine analog that inhibits DNMTs, triggering their degradation and re-expression of genes silenced by promoter DNA methylation40. Aza and another demethylating agent, 5-aza-2’-deoxycytidine (Decitabine or Dac), are approved by the FDA for the treatment of myelodysplastic syndrome41. Recent evidence from pre-clinical studies and clinical trials suggests that DNMTis may reverse immune evasion in cancers.
Another epigenetic silencer, histone deacetylases (HDACs), are a family of enzymes that remove acetyl groups from histones. There are four zinc dependent classes of HDACs which include Class I (HDAC 1, 2, 3, 8), Class IIa (HDAC 4, 5, 7, 9), Class IIb (HDAC 6, 10) and Class IV (HDAC 11) enzymes. The Class III enzymes or sirtuins are non-zinc dependent42. HDACs remove negatively charged acetyl groups from the positively charged histone proteins that DNA is wrapped around, compacting the chromatin and silencing genes. Histone deacetylases inhibitors (HDACi) function by interfering with HDACs and like DNMTis can reverse transcriptional inhibition of tumor suppressor genes. The HDACi suberoylanilide hydroxamic acid (SAHA) was approved for the treatment of persistent or cutaneous T cell lymphoma in 2006. Like DNMTis, recent work has shown that HDACis can also stimulate anti-tumor immunity42,43.
Histone methyltransferase (HMT) enzymes deposit methylation residues on specific lysines of histones, establishing patterns of gene expression, and thus have essential roles in cell cycle regulation and development. HMTs that are overexpressed in cancer include DOT1L, which catalyzes up to three methyl groups to histone H3, lysine 79; G9a, which induces H3K9me; and EZH2, which adds H3K27 methylation. All three of these are silencing marks and inhibiting the HMTs responsible opens up the chromatin to activate gene expression, similar to the effects of DNMTis and HDACis39.
Tumors undergo immunoediting as an adaptive mechanism to evade the immune system, and a growing body of evidence implicates epigenetic control of this immune resistance. Immunoediting often involves downregulation of MHC I or loss of antigen expression, resulting in an overall loss of antigen presentation. MHC class I genes in human breast cancer are suppressed due to silencing DNA methylation marks at their promoter regions. DNA methylation inhibition reversed MHC I gene promotor methylation and upregulated gene expression in response to interferon44. Additionally, Wylie et al. found that downregulated expression of immunogenic antigens correlated with immune escape from adoptive cell therapy. Treating with DNA demethylating agents restored expression of these immunogenic antigens45.
Epigenetic regulation of MHC-I antigen presentation by the polycomb repressive complex can lead to immunotherapy resistance46. Burr et al. showed that an important function of polycomb repressive complex 2 (PRC2) is its ability to mediate the silencing of the MHC-I antigen processing pathway, which leads to the evasion of T-cell mediated immunity. Siebenkäs et al. showed that both colon and ovarian cancer cells have lower expression of the antigen processing and presentation machinery, preventing tumor detection by CD8 T cells. Treating with DNMT inhibitors increased expression of both the antigen processing and presentation genes and cancer testis antigens (CTAs)47. Specific molecules that were upregulated upon treatment included B2M, CALR, CD58, PSMB8, and PSMB947. Siebenkäs et al. thus demonstrate how treatment with DNMT inhibitors might sensitize patients to immunotherapy by upregulating the expression of antigen processing and presentation molecules. Similarly, Gameiro et al. utilized HDAC inhibitors to upregulate silenced antigen processing and presentation machinery in prostate and breast cancer cells. Gameiro et al. demonstrate that exposure to HDAC inhibitors can reverse the ability of tumors to evade immune attack. After HDACi treatment, the tumor cells exhibited increased sensitivity to T-cell mediated lysis48. Thus, repressive histone modifications and DNA methylation silence antigen processing and presentation in cancers to promote immune evasion.
The high rate of proliferation of tumor cells also contributes to immune evasion through transcriptional mechanisms. The high rate of cell proliferation in tumors leads to an increase in their mutation burden and copy number load, as well as global loss of methylation within late-replicating domains49. Immunomodulatory pathway genes concentrated within these late-replicating methylation domains gain promoter methylation and are transcriptionally suppressed in many solid tumors. Furthermore, methylation loss in these domains corresponds to immune evasion in both lung cancer and melanoma49.
Cancer cells may also evade the immune system through direct epigenetic silencing of Fas. Fas is an apoptotic effector molecule within the TNF receptor family and is also a downstream target of the p53 tumor suppressor50. Maecker et al. demonstrate that epigenetic silencing of Fas promotes growth and prevents apoptosis of tumor cells derived from mouse embryonic fibroblasts. When cells were treated with the HDACi Trichostatin A, tumor growth was suppressed and chemosensitivity was restored50.
Lastly, epigenetic inactivation of follistatin-like 1 (FSTL1) promotes immune evasion. Zhou et al. demonstrate the role that FSTL1 plays in the pathogenesis of nasopharyngeal carcinoma (NPC). In many NPC cell lines, FSTL1 was downregulated via promoter hypermethylation. Furthermore, the expression of FSTL1 suppressed cell proliferation and migration of NPC cells, and treatment with FSTL1 increased secretion of the IL-1β and TNF-α cytokines in macrophage cultures. This suggests that FSTL1 may activate macrophages and reduce immune evasion.
The immune cell response to cancer is also regulated by epigenetic mechanisms. One example is the de novo DNA methylation of the Tcf7 gene promoter by DNMT3a on CD8+ T cells following activation and proliferation. Typically CD8+ T cells differentiate into the early effector cell stage after activation, followed by further differentiation into either memory precursor or terminal effector cells51. Ladle et. al demonstrated that DNMT3a establishes methylation patterns within the Tcf7 promoter which leads to the differentiation of terminal effector CD8 T cells. Ladle et. al also found that DNMT3a KO mice have the ability to clear infections and have improved CD8 T cell memory. Youngblood et al. investigated the effects of DNA methylation patterns on naïve and effector gene expression in CD8 T cells. Following infection, memory precursor CD8 T cells gained de novo DNA methylation to suppress expression of naïve genes52. Deleting DNMT3a during an early stage of differentiation reduced the methylation of naïve genes, resulting in quicker re-expression of these genes to accelerate memory cell development. Overall this work demonstrates that epigenetic repression of naïve genes in CD8 can be reversed in cells that develop into memory CD8 T cells. Ghoneim et al. demonstrated that inhibition of DNA methylation in activated CD8 T cells allows retention of effector function even during chronic stimulation53. During both effector and exhaustion stages of an immune response, de novo methylation patterns restricted CD8 T cell expansion even after anti-PD-1 treatment53. These methylation programs were associated with the exhaustion stage and were an acquired form of resistance in PD-1hi CD8 T cells, which could be reversed by inhibiting DNA methylation.
Due to the intrinsic and extrinsic resistance mechanisms outlined above, most patients do not respond to immune checkpoint therapy alone27. As a result, many current studies focus on combination therapies that seek to enhance the effectiveness of immune therapy for a wider range of patients.
Combination of epigenetic drugs with immunotherapies
Pre-clinical studies combining HMTs with immune therapy have shown effectiveness in several tumor types. Increased expression of EZH2 leads to an increase in H3K27me3, loss of antigen presentation, and reduced immunogenicity in melanoma55. Addition of an EZH2 inhibitor to anti-CTLA-4 or IL-2 treatment reversed many of these immunosuppressive effects and significantly improved immune therapy in preclinical models55. BET (bromo and extra terminal) proteins are a family of proteins that epigenetically regulate the transcription of oncogenes56. EZH2 components silence chemokine expression in mouse models of ovarian cancer and inhibition of EZH2 sensitizes the cancers to immune checkpoint blockade therapy57. In an ovarian cancer model, treatment with the BET inhibitor JQ-1 decreased PD-L1 expression on tumor cells, tumor-associated dendritic cells, and macrophages58. In oral squamous cell carcinoma, JQ-1 downregulated the expression of PD-L1 and combining JQ-1 and with knockdown of PD-L1 was synergistic59. In a Myc-driven lymphoma mouse model, BETi treatment inhibited PD-L1 expression60. Combining JQ-1 and anti-PD-L1 was significantly more effective than treatment with either drug alone60.
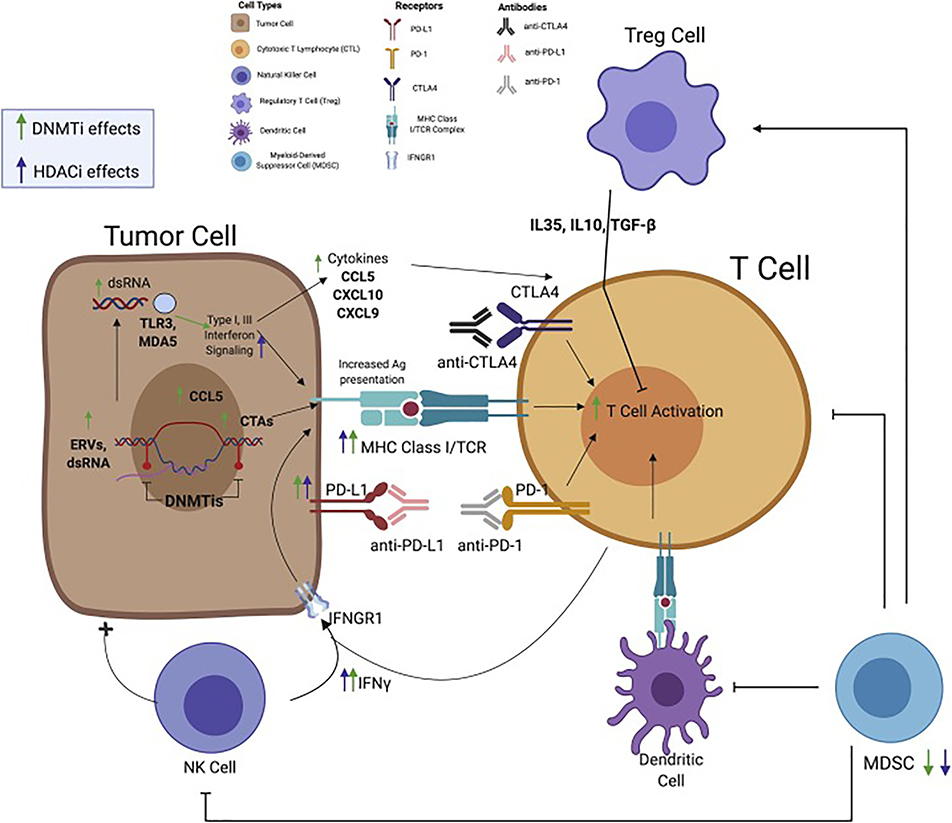
DNMTis upregulate immune signaling in both tumor and host immune cells (Figure 1). Low doses of DNMTis upregulate immune signaling, including the interferon response 61,62,63–66, cancer/testis antigens (CTAs), and antigen processing and presentation in breast, colon, lung, and ovarian cancer cell lines62,67. DNMTis activate a canonical interferon signaling pathway through upregulation of dsRNA, specifically hypermethylated endogenous retroviruses (ERVs) that activate dsRNA sensors TLR3 and MDA561. DNMTis increase expression and reduced methylation of ERVs, which make up 8% of the genome. The interferon response caused by DNMTis is abrogated by inhibiting dsRNA sensors MDA5 and TLR3, proving that transcription of dsRNA species caused the interferon response61,65. The DNMTi upregulation of ERVs and subsequent interferon response can be increased by adding HDACi68, inhibitors of H3K9 methyltransferases69, or Vitamin C, which is a cofactor for the TET DNA demethylases70. DNA methylation silences expression of the CCL5 cytokine in tumor cells, which is required for T cell infiltration in ovarian cancers. Treatment with DNMTi can reverse this silencing and bring in CTLs71. DNMTis also affect host immune cells, specifically effector T cells. Inhibiting de novo methylation in effector T cells prevented their exhaustion51,72 and synergized with immune checkpoint blockade in a mouse model of viral infection72.
Figure 1. DNMTi and HDACi promote anti-tumor immune signaling.
DNMTi treatment removes methylation from endogenous double-stranded RNA species, including ERVs, which activate Type I and III interferon signaling through sensors including TLR3 and MDA5. This signaling in turn leads to increased expression of antigen processing and presentation machinery including MHC I on the cell surface. DNMTis also upregulate cancer testis antigens (CTAs) and the cytokine CCL5 by demethylation of their promoter regions. HDACi increase antigen processing and presentation and PD-L1 expression, along with DNMTi. DNMTi increase T cell activation against tumor cells and both DNMTi and HDACi repress MDSCs, promoting an anti-tumor immune microenvironment.
Epigenetic drugs have also been studied in combination with adoptive T cell therapy. Treatment of mice with the DNMTi decitabine improved the efficacy of adoptive T cell immunotherapy, showing greater inhibition of tumor growth and an increased cure rate73. Similarly, the combination of the HDACi LAQ824 with adoptive T cell therapy resulted in significantly improved antitumor immune activity in recipient mice74.
In preclinical mouse models of cancer, DNMTi and/or HDACi treatment sensitizes tumors to immune therapy (Figure 1). DNMTis plus HDACis increase ERVs in a mouse model of ovarian cancer (ID8)75, activating interferon signaling and recruiting CD8+ T cells to kill the tumors76. DNMTi treatment sensitizes mouse melanoma to subsequent anti-CTLA4 therapy61,77,78 and mouse ovarian cancer to anti-PD-1 therapy76. HDACi improved effectiveness of anti-PD-1 treatment in melanoma and lung adenocarcinoma, causing slower tumor progression and increased survival compared to control and single agent treatments43,79. In another murine model, the DNMTi decitabine in combination with anti-CTLA4 immune blockade decreased tumor burden and improved survival of mice with ovarian cancer73. The combination of DNMTis, HDACis, anti-PD1, and anti-CTLA4 together showed significantly improved treatment outcomes in mice, with over 80% of tumor bearing mice being cured80. HDACi and DNMTis inhibited MDSC function in this study80. These results strongly support the combination of immune checkpoint therapies with DNMTi and/or HDACi in cancer treatment.
Clinical trials combining epigenetic and immune therapy
Many clinical trials are currently testing combinations of epigenetic drugs with immune therapy, most commonly HDACi and DNMTi. While effective for MDS/AML (DNMTi) and cutaneous T cell lymphoma (HDACi), epigenetic drugs have thus far shown limited effectiveness in the treatment of solid tumors as single agents. For example, when non-small cell lung cancer (NSCLC) patients were treated with azacytidine and entinostat, a DNMTi and an HDACi, respectively, only 4% of the patients exhibited an objective response81. Combining epigenetic drugs with conventional chemotherapy improves effectiveness of these therapies. In NSCLC patients, the combination of vorinostat, an HDACi, with carboplatin and paclitaxel enhanced the efficacy of the chemotherapeutic drugs and lead to improved patient survival82. Similarly, the DNMTi azacytidine partially reverses platinum resistance, improving the efficacy of carboplatin in patients with epithelial ovarian cancer83–85. These results point to the potential of epigenetic drugs to improve the efficacy of conventional therapies, though further study is required.
Epigenetic drugs have shown exciting initial results when used in combination with immune checkpoint inhibitor therapies. Following the aforementioned study in patients with NSCLC, several patients who had received DNMTi and HDACi therapy took part in a trial for immune checkpoint therapy with an anti-PD-1 inhibitor. Of the six patients, five survived six months without cancer progression66. Based on the strong preclinical data for DNMTi upregulation of interferon signaling and reversal of immune evasion, many clinical trials combining DNMTi and immune checkpoint blockade cancer are ongoing or completed (see Table 1 for a complete list of trials combining epigenetic therapy with immune therapy in cancer). Trial NCT02664181 combines THU (tetrahydrouridine, a cytidine deaminase inhibitor) with oral decitabine and nivolumab (anti-PD-1) in non-small cell lung cancer. In this trial THU is used to stabilize decitabine as it works by blocking cytidine deaminase, an enzyme that rapidly breaks down decitabine. NCT02900560 combines oral azacytidine and pembrolizumab (anti-PD-1) in epithelial ovarian cancer. Trial #NCT03206047 tests the combination of guadecitabine (SGI-110, a pro-drug form of decitabine), atezolizumab (anti-PD-L1), and a CDX-1401 vaccine (dendritic cell vaccine against the cancer testis antigen NY-ESO-1). NY-ESO-1 antigen is expressed at higher levels on cancer cells than normal cells but can be demethylated and further upregulated by DNMTi treatment. Other clinical trials combining DNMTi and immune checkpoint blockade are being run in a wide range of cancers to determine their safety and efficacy (Table 1). These include diffuse large B cell lymphoma ( NCT02951156), lung cancer ( NCT02546986), ovarian cancer ( NCT02901899), colorectal cancer ( NCT02260440), acute myeloid leukemia ( NCT02845297, NCT02397720), metastatic melanoma ( NCT02816021, NCT02608437), and myelodysplastic syndromes ( NCT02599649, NCT02530463, NCT02890329, NCT02508870, NCT02117219, NCT02775903).
Table 1.
Completed and ongoing clinical trials utilizing epigenetic modifiers in cancer.
| Trial number | Status | Title | Drug and Schedule | Study Type | Notes |
|---|---|---|---|---|---|
| NCT03812796 | Recruiting | Epigenetic Modulation of the immunE response in GastrointEstinal Cancers | Phase IIA: Domatinostat in an oral tablet given at varying doses. Given Avelumab intravenously at 10 mg/kg every two weeks. Phase IIB: Patients treated with domatinostat at safe combination dose found in phase IIA. Given Avelumab intravenously at 10 mg/kg every two weeks. |
Phase 2 GI cancer - microsatellite stable colorectal or gastroesophageal cancer | |
| NCT02664181 | Completed | Rational EpigenetiC Immunotherapy for SEcond Line Therapy in Pateients with NSCLC: Precise Trial | Experimental: Oral THU (10 mg/kg) followed by oral decitabine (0.2 mg/kg) 60 minutes after THU occuring consectuively for two days weekly. Nibolumab adminstered at 3 mg/kg intravenously every two weeks until progression. Active Comparator: Nivolumab 3 mg/kg intravenously every two weeks until progression. |
Phase 2 Lung Cancer, Non-small cell lung cancer |
|
| NCT02900560 | Recruiting | Study of Pembrolizumab With of Without CC-486 in Patients with Platinum-Resistance Ovarian Cancer | Cohort 1: Oral Azacitidine (CC-486) at 100 mg once a day for 21 days and then 7 days off. Given with Pembrolizumab at 200 mg intravenously every 21 days. Cohort 2: Oral Azacitidine (CC-486) at 100 mg twice a day for 21 days and then 7 days off. Given with Pembrolizumab at 200 mg intravenously every 21 days Cohort 3: Oral Azacitidine (CC-486) at 300 mg once a day for 14 days and then 14 days off. Given with Pembrolizumab at 200 mg intravenously every 21 days. Cohort 4: Oral Azacitidine (CC-486) at 300 mg once a day for 21 days and then 7 days off. Given with Pembrolizumab at 200 mg intravenously every 21 days. |
Phase 2 Epithelial Ovarian Cancer |
|
| NCT03206047 | Suspended (Other-Pending Phase 2 Portion of Study) | Atezolizumab, Guadecitabine, and CDX-1401 Vaccine in Treating Patients With Recurrent Ovarian, Fallopian Tube or Primary Peritoneal Cancer | Cohort 1: Atezolizmab administered intravenously over 30–60 minutes on day 1 and 15. Treatment regimen repeats every 28 days for 24 courses. Cohort 2: Guadecitabine administered subcutaneously on days 1–5. Treatment repeats every 28 days for up to 6 courses. Atezolizumab administered intravenously over 30–60 minutes on day 8 and day 22. Treatment regimen repeats every 28 days for up to 24 courses. Cohort 3: Guadecitabine and Aztezolizumab administered in the same manner as cohort 2. Addition of CDX-1401 vaccine intravenously occurs on day 15 and poly ICLC subcutaneously on days 15 and 16. Treatment repeats every 28 days for up to 6 courses. |
Phase 1 Platinum-Resistant: Fallopian Tube Carcinoma, Ovarian Carcinoam, Primary Peritoneal Carcinoma Recurrent: Fallopian Tube Carcinoma, Ovarian Carcinoma, Primary Peritoneal Carcinoma |
|
| NCT02951156 | Active, Not recruiting | Avelumab in Combination Regimens That Include An Immune Agonist, Epigenetic Modulator, CD20 Antagonist and/or Conventional Chemotherapy in Patients with Relapsed or Refractory Diffuse Large B cel Lymphoma | Phase 1b (Arm A): Azelumab, Utomilumab, Rituzimab Phase 1b (Arm B): Avelumab, Utomilumab, Azacitidine Phase 1b (Arm C): Avelumab, Rituxima, Bendamustine Phase 3 (Arm D): Selected regimen from Phase 1b component. Phase 3 (Arm E): Choice of investigator to do either rituximad/bendamustine or rituximab/gemcitabine/oxaliplatin. |
Phase 3 Diffuse Large B-Cell Lymphoma |
|
| NCT03765229 | Recruiting | An Exploratory Study of Pembolizumab Plus Entinostat in Non-inflamed Stage III/IV Melanoma | Entinostat at 5 mg administered orally occuring once weekly of a 21 day cycle starting on day 1 of study treatment; Pembrolizumab at 200 mg administered intravenously every 3 weeks starting at cycle 2 (occurs after research tumor biopsy at the end of cycle 1) | Phase 2 Melanoma | Combination therapy of both entionstat and pembrolizumab will continue if patient has clinical beenfit from therapy for up to 27 weeks. |
| NCT00387465 | Completed | Azacitidine and Entinostat in Treating Patients with Recurrent Advanced Non-Small Cell Lung Cancer | Phase 1: Azacitidine at 30 mg/m2 administered subcutaneously. Entinostat at 7 mg orally on day 3 and 10 of each cycle. Phase 1: Azacitidine at 40 mg/m2 administered subcutaneously. Entiostat at 7 mg orally on days 3 and 10 of each cycle. Phase 2: Azacitidine at 40 mg/m2 administed subcutaneously on days 1–6 and 8–10. Entiostat at 7 mg administered orally on day 3 and 10. Treatment repeats every 28 days. |
Phase 1/ Phase 2 Recurrent Non-small Cell Lung Cancer, Stage IIIA NSCLC, Stage IIIB NSCLC, Stage IV NSCLC |
|
| NCT02437136 | Active, Not recruiting | Ph1b/2 Dose-Escalation Study of Entinostat With Pembrolizumab in NSCLC with Expansion Cohorts in NSCLC, Melanoma, and Colorectal Cancer | Cohort 1: Ph 2 NSCLC (squamous or adeno). Patients not pre-treated with PD-1 or PD-L1 blocking antibody. Given entinostat and pembrolizumab Cohort 2: Ph 2 NSCLC. Patients pre-treated with PD-1/PD-L1 blocking antibody. Given entinostat and pembrolizumab. Cohort 3: Ph 2 Melanoma. Patients pre-treated with PD-1/PD-L1 blocking antibody. Given entinostat and pembrolizumab. Cohort 4: Ph 2 Mismatch Repair-Proficient CRC. Patients not pre-treated with PD-1 or PD-L1 blocking antibody. Given entiostat and pembrolizumab. |
Phase 1/Phase 2 Non-small Cell Lung Cancer, Melanoma, Mismath Repair-Proficient Colorectal Cancer | |
| NCT02936752 | Recruiting | Entinostat and Pembrolizumab in Treating Patients With Myelodysplastic Syndrom After DMNTi Therapy Failure | Patients receive low dose of oral entinostat on days 1 and 8 or a higher dose on days 1, 8, and 15. Pembrolizumab given intravenously over 30 minutes on day 1 of courses 2 and courses after. Treatment repeats every 21 days for up to 4 courses. | Phase 1 Blasts 21–20 Percent of bone Marrow Nucleated Cells, Myelodysplastic Syndrome, Previously treated Myelodysplastic syndrome |
|
| NCT02546986 | Active, Not recruiting | Safety and Efficacy Study of CC-486 with MK-3475 to Treat Locally Advanced or Metastatic Non-Small Cell Lung Cancer | Experimental Arm: Patients receive oral Azacitidine at 300 mg daily on days 1–14 of the 21 day cycles. Pembrolizumab adminstered intravenously for 30 minnutes on day 1 of the 21 day cycles. Control Arm: Patients receive pembrolizumab intravenously for 30 minutes on day 1 of the 21 day cycles. Oral placebo will be adminstered on days 1–14 of the 21 day cycles. |
Phase 2 Non-small Cell Lung Carcinoma |
|
| NCT02909452 | Active, Not recruiting | Continuation Study of Entinostat in Combination with Pembrolizumab in Patients with Advanced Solid tumors | Entinostat at 1 mg given daily with pembrolizumab given every three weeks. Entinostat at 5 mg given once weekly with pembrolizumab given every three weeks. Entinostat at 10 mg given bi-weekly with pembrolizumab given every three weeks. |
Phase 1 Neoplasms (Glandular and Epithelial), Neoplasms by histologic type, brnchial neoplasms, lung neoplasms, respiratory tract neoplams, thoracic neoplasms, digestive system neoplasms, endocrine gland neoplasms, NSCLC, lung diseases, breast disease, renal neoplasm, solid tumors | |
| NCT02697630 | Active, Not recruiting | Efficacy Study of Pembrolizumab with Entinostat to Treat Metastatic Melanoma of the Eye (PEMDAC) | Pembrolizumab at 200 mg adminstered intravenoulsy every third week. Entinostat at 5 mg administered orally once weekly. | Phase 2 Metastatic Uveal Melanoma | |
| NCT02538510 | Active, Not recruiting | Pembrolizumab and Vorinostat in Treating Patients with Recurrent Squamous cell Head and Neck Cancer or Salivary Gland Cancer that is Metastatic and/or Cannot be removed by surgery | Receive vorinostat orally or via PEG on days 1–5 and pembrolizumab intravenously over 30 minutes on day 1. Treatment courses repeat every 21 days for up to 2 years | Phase 1/Phase 2 Head and Neck Squamous Cell Carcinoma, Recurrent Nasal Cavity and Paranasal Sinus Squamous Cell Carcinoma, Recurrent Nasopharynx Carcinoma, Recurrent salivary Gland Carcinoma, Squamous Cell Carcinoma Metastatic in Neck with Occult primary, Stage III Major salivary Gland carcinoma, Stage III nasal cavity and paranasal sinus squamous cell carcinoma, Stage III nasopharynheal carcinoma, Stage IV nasopharyngeal carcinoma, Stage IVA major salivary gland carcinoma, Stage IVA nasal cvity and paranasal sinus squamous cell carcinoma, Stage IVB major salivary gland carcinoma, Stage IVB Nasal cavity and Paranasal sinus squamous cell Carcinoma, Stage IVC major salivary gland carcinoma, Stage IVC nasal cavity and Paranasal sinus Squamous cell carcinoma | |
| NCT02638090 | Recruiting | Pembro and Vorinostat for Patients with Stage IV Non-small Cell Lung Cancer (NSCLC) | Phase 1 (Dose Escalation): Level 1 - Vorinostat at 200 mg given orally daily with pembrolizumab at 200 mg adminstered intravenously every 3 weeks. Level 2 - Vorinostat at 400 mg given orally daily with pembrolizumab at 200 mg adminstered intravenously every 3 weeks. Phase 1b (Expansion): Level 1-Pembrolizumab plus vorinostat given at maximum tolerated dose. Arm A: Pembrolizumab adminstered at 200 mg intravenously every 3 weeks. Arm B: Pembrolizumab plus vorinostat treatment given at maximum tolerated dose. |
Phase 1/Phase 2 Lung cancer, Non-small Cell Lung Cancer |
|
| NCT02619253 | Recruiting | Phase I/Ib study of Pembrolizumab with Vorinostat for Patients with Adavanced Renal or Urothelial Cell Carcinoma | Dose Finding cohort: Patients will be given oral vorinostat daily for 14 days with pembrolizumab at 200 mg intravenously. Two doses of vorinostat will be tested 100 and 200 mg. Each cycle is every 21 days. Expansion Cohort: After determining which dose of vorinostat should be used in the dose finding cohort, patients with prior treatments are enroleed in three different cohorts. 15 anti-PD1 naive renal and urothelial patients, 15 anti-PD1 resistane renal and urothelial pateitns and 15 patients with androgen-sensitive or castration-resistance prostate cancer. Each cohort will then receive the established vorinostat dose along with 200 mg pembrolizumab intravenously. |
Phase 1 Renal Cell Carcinoma, Urinary Bladder Neoplasms |
|
| NCT02901899 | Recruiting | Guadecitabine and Pembrolizumab in Treating Patients with Recurrent Ovarian, Primary Peritoneal, or Fallopian tube Cancer | Patients receive guadecitabine subcutaneously on days 1–4 and pembrolizumab intravenously over 30 minutes on day 5. Treatment courses repeat evry 21 days. | Phase 2 Recurrent - Fallopian Tube Carcinoma, Ovarian Carcinoma, Primary Peritoneal Carcinoma |
|
| NCT02512172 | Active, Not recruiting | A Study of Enhancing Response to MK-3475 in Advanced Colorectal Cancer | Patients given oral azacitidine at 300 mg on days 1–14 or 21 for every 28 days. Given pembrolizumab at 200 mg intravenously on days 1 and 15 every 28 days Patients given Romidepsin at 14 mg/m2 on days 1,8, and 15. Given pembrolizumab at 200 mg intravenously on days 1 and 15 every 28 days. Patients given oral azacitidine at 300 mg on days 1–14 or 21 and romidepsin at 7 mg/m2 on days 1,8 and 15. Given pemrbolizumab at 200 mg intravenously on days 1 and 15 every 28 days. |
Phase 1 Colorectal Cancer |
Romidepsin - Chemotherapy drug approved by FDA for treatment of cutaneous T-cell lymphoma |
| NCT02260440 | Active, Not recruiting | A Phase 2 Study of Pembrolizmab (MK-3475) in Cominaiton with Azacitidine in Subjects With Chemorefractory Metastatic Colorectal Cancer | Pembrolizumab given at 200 mg every 21 days. Azacitidine given at 100 mg daily subcutaneously on days 1–5 every 21 days. 9 cycles of treatment. | Phase 2 Colorectal Cancer |
|
| NCT02845297 | Recruiting | Study of Azacitidine in Combination with Pembrolizumad in Replased/Refractory Acute Myeloid Leukemia (AML) Patients and in Newly Diagnosed Older (>= 65 years) AML Patients | Cohort 1 (Safety Run in Phase) : Treatment of relapsed and refractory AML Patients. Given pembrolizumab intravenously and azacitadine intravvenoulsy or subcutaneously. Cohort 2: Treatment of newly diagnost AML patients (>= 65 years). Given pembrolizumab intravenously and azacitadine intravenously or subcutaneously. |
Phase 2 Acute Myeloid Leukemia |
|
| NCT02816021 | Recruiting | Study of Oral Azacitidine (CC-486) in Combination with Pembrolizumab (MK-3475) in Patients with Metastatic Melanoma | Arm A - Metastatic Melanoma PD-1 Naive: 3 week treatment cycles. Oral azacitidine given for days 1–15 of every cycle. Pemrbolizumab administered intravenously every 3 weeks and after the oral dose of azacitidine on concurrent treatment days. Arm B - Metastatic Melanoma Post PD-1 Progression: 3 week treatment cycles. Oral azacitidine given for days 1–15 of every cycle. Pembrolizumab adminstered intravenously every 3 weeks and after oral dose of azacitidine on concurrent treatment days. |
Phase 2 Melanoma and other malignant neoplasms of skin, metastatic melanoma |
|
| NCT01928576 | Recruiting | Phase II Anti-PD1 Epigentic Therapy Study in NSCLC | Arm C: Nivolumab at 3 mg/kg given every 2 weeks until disease progression. Arm D: Treatment occurs every 28 days for 6 cycles. Azacitidine given at 40 mg.m2 on days 1–5 and days 8–10. Entinostat at 5 mg given on days 3 and 10. Nivolumab given at 3 mg/kg on days 1 and 15. Followed by nivolumab at 3 mg/kg given every 2 weeks until disease progression. |
Phase 2 Non-small Cell Lung Cancer |
|
| NCT02397720 | Recruiting | Nivolumab and Azacitidine with or without Ipilimumab in Treating Patients with Refractory/Relapsed or Newly Diagnosed Acute Myeloid Leukemia | Arm I: Azacitidine adminstered intravenously over 1 hours or subcutaneously on days 1–7 or days 1–4 and days 7–9. Received nivolumab intravenously over 60 minutes on days 1 and 14 (courses 1–4) or on day 1 (course 5 and the courses following). Treatment courses repeat every 28 days. Arm II: Receive azacitidine and nivolumab as in Arm I. Receive ipilimumab intravenously over 90 minutes on day 1 and then every 6 or 12 weeks. |
Phase 2 Acute Bilineal Leukemia, Acute Biphenotypic Leukemia, Acute Myeloid Leukemia arising from previous myelodysplastic syndrome, chronic myelomonocytic leukemia, myelodysplastic syndrome, recurrent acute myeloid leukemia, refractory acute myeloid leukemia, secondary acute myeloid leukemia, therapy-related actue myeloid leukemia | |
| NCT02599649 | Completed | Lirilumab and Nivolumab with 5-Azacitidine in Patients with Myelodysplastic Syndromes (MDS) | Low or Intermediate-1 MDS Group: Lirilumab adminstered at 3 mg/kg intravenously over 60 minutes one time during every 28 day cycle. Low or Intermediate-MDS Group: Nivolumab adminstered at 3 mg/kg intravenously over 60 minutes every 2 weeks during cycles 1–8. Lirilumab adminstered at 3 mg/kg intravenously over 60 minutes one time during every 28 day cycle. High Risk MDS Group: Azacitidine adminstered at 75 mg/m2 intravenously over 60 minutes on days 1–7 of the 28 day cycle. Lirilumab adminstered at 3 mg/kg intravenously over 60 minutes on day 7 of each cycle. High Risk MDS Group: Azacitidine adminstered at 75 mg/m2 intravenously over 60 minutes on days 1–7 of each 28 day cycle. Lirilumab adminstered at 3 mg/kg intravenously over 60 minutes on day 7 of each cycle. On days 7 and 21 of cycles 1–9 nivolumab is adminstered at 3 mg/kg intravenously over 60 minutes. On day 7 of cycle 10 and beyond, nivolumab adminstered intravenously over 60 minutes. |
Phase 2 Leukemia |
|
| NCT02530463 | Recruiting | Nivolumab and Ipilimumab with 5-azacitidine in Patients with Myelodysplastic Syndromes (MDS) | Cohort 1 (Hypomethylating failure MDS cohort): Nivolumab adminstered intravenously at 3 mg/kg every 2 weeks for 6 cycles. After 6 cycles, use of Azacitidine is permitted to test concept of re-sensitization. Cohort 2 (Hypomethylating failure MDS cohort): Ipilimumab adminstered intravenously at 3 mg/kg every 3 weeks for 6 cycles. After 6 cycles, use of Azacitidine is permitted to test concept of re-sensitization. Cohort 3 (Hypomethylating failure MDS cohort): Nivolumab adminstered intravenously at 3 mg/kg on days 1 and 15. Ipilimumab adminstered intravenously at 3 mg/kg on day 1. After 6 cycles, use of Azacitidine is permitted to test concept of re-sensitization. Cohort 4 (Previously untreated MDS cohort): Azacitidine admintered intravenously at 75 mg/m2 for 5 days every 4 weeks. On day 6 nivolumab adminstered intravenously at 3 mg/kg every 2 weeks. Cohort 5 (Previously untreated MDS cohort): Azacitidine adminstered intravenously at 75mg/m2 for 5 days every 4 weeks. On day 6 ipilimumab adminstered intravenously at 3 mg/kg every 4 weeks. Cohort 6 (Previously untreated MDS cohort): Azacitidine adminstered intravenously at 75 mg/m2 for 5 days every 4 weeks. On day 6 and day 20 nivolumab adminstered intravenously at 3 mg/kg and ipilimumab adminstered on day 6 intravenously at 3 mg/kg. |
Phase 2 Leukemia, Myelodysplastic syndrome |
|
| NCT02635061 | Recruiting | Selective HDAC6 Inhibitor ACY 241 in Combination with Nivolumab in Pateitns with Unresectabe Non-smell Cell Lung Cancer | ACY-241 adminstered in combination with nivolumab. | Phase 1 Non-small Cell Lung Cancer |
|
| NCT02890329 | Recruting | Ipilimumab and Decitabine in Treating Patients with Relapsed or Refractory Myelodysplastic Syndrome or Acute Myeloid Leukemia | Arm A (Post allo-HCT): Priming phase - patients are administered decitabine intravenously over 60 mintes on days 1–5 out of 28 days. Induction phase - patients are adminstered decatibine intravenously over 60 minutes on days 1–5 and ipilimumab is adminstered intravenously over 90 minutes on day 1. Treatment repeats every 28 days for up to 4 cycles. Maintenance phase - patients adminstered decitibine intravenously over 60 minutes on days 1–5 and ipilimumab is adminstered intravenously over 90 minutes on day 1. Treatment repeats every 4–8 weeks for up to 4 cycles. Arm B (Transplant naive Patients): Priming phase - patients are adminstered decitabine intravenously over 60 mintes on days 1–5 out of 28 days. Induction phase - patients are adminstered decitabine intravenously over 60 minutes on days 1–5 and ipilimumab is adminstered intravenously over 90 minutes on day 1. Treatment repeats every 28 days for up to 4 cycles. Maintenance phase - patients are adminstered decitabine intravenously ver 60 minutes on days 1–5 and ipilimumab is adminstered intravenously over 90 minutes on day 1. Treatment repeats every 4–8 weeks for up to 4 cycles. |
Phase 1 Blasts 5% of more of bone marro nucleated cells, hemtopoietic cell transplant recipient, myelodysplastic syndrome, previously treated myelodysplastic syndrome, recurrent acute myeloid leukemia, recurrent acute myeloid leukemia with myelodysplasia-related changes, refractory acute myeloid leukemia, secondary acute myeloid leukemia, untreated adult acute myeloid leukemia | |
| NCT02608437 | Unknown | A Study Investigating SGI-110 in Combination with Ipilimumab in Unresectable or Metastatic Melanoma Patients (NIBIT-M4) | SGI-110 administered at 30 mg/m2 subcutaneously on days 1–5 for 2 day cycles. Ipilimmab adminstered at 3 mg/kg intravenously over 90 minutes every 3 weeks for 4 cycles. | Phase 1 Metastatic Melanoma |
|
| NCT02032810 | Active, Not recruiting | Phase I of Histone Deacetylase (HDAC) Inhibitor Panobinostat with Ipilimumab with Unresectable III/IV Melanoma | Patients assigned a dose of panobinostat (5, 10, 15, 20 mg). Dose depends on time point patients enters study. Patients given ipilimumab at 3 mg/kg. | Phase 1 Skin Cancer, Melanoma |
|
| NCT02508870 | Suspended | A study of Atezolizumab Adminstered Alone or in Combination with Azacitidine in Participants with Myelodysplastic Syndromes | Cohort A (HMA R/R MDS): Patients adminstered atezolizumab at 1200 mg intravenously every 3 weeks (21 day cycles) Treatment will continue for up to 17 cycles. Cohort B (HMA R/R MDS): Induction - Patients adminstered atezolizumab at 840 mg intravenously on days 8 and 22 of 28 day cycles. Azacitidine adminstered at 75 mg/m2 subcutaneously on days 1–7 of 28 day cycles for 6 cycles. Maintenance - Patients who completed induction treatment will be adminstered atezolizumab at 1200 mg intravenously Q3W (21 day cycles) for up to 8 additional cycles. Cohort C1 (HMA Naive MDS): Patients adminstered atezolizumab at 840 mg intravenously on days 8 and 22 of 28 day cycles. Azacitidine adminstered at 75 mg/m2 subcutaneously on days 1–7 of 28 day cycles. Cohort C2 (HMA Naive MDS): Patients enrolled in Cohort C1 fulfil dose limiting toxicity, additional patients will be adminstered atezolizumab at 840 mg intravenously on days 8 and 22 of 28 day cycles. Azacitidine admintered at 75 mg/m2 subcutaneously on days 1–7 of 28 day cycles. Cohort A2 (HMA R/R MDS): If atezolizumab alone or in combination with azacitidine is safe and tolerable. Patients will be randomly assigned to be adminstered atezolizumab at 1200 mg intravenously Q3W (21 day cycle) Treatment will continue up to 17 cycles. Cohort B2 (HMA R/R MDS): If atezolizumab alone or in combination with azacitidine is safe and tolerable, patients will be randomly assigned to be administered atezolizumab at 840 mg intravenously on days 8 and 22 of each 28 day cycles and azacitidine admininistered at 75 mg/m2 subcutaneously on days 1–7 of 28 day cycles for 6 cycles during inducation. Patients who complete induction treatment with be adminstered atezolizumab at 1200 mg intravenously Q3W (21 day cycle) for up to 8 cycles. |
Phase 1 Myelodysplastic syndromes |
|
| NCT02708680 | Active, Not recruiting | Randomized Phase 2 study of Atezolizumab and Entinostat in pateitns with aTN Breast Cancer with Phase 1b Lead In | Active Comparator: Entinostat given orally at RP2D in combination with atezolizumab. Placebo Comparator: Placebo given orally in ocmbination with atezolizumab. |
Phase 1 Breast Cancer |
|
| NCT02117219 | Completed | Phase 1 Study to Evaluate MEDI4736 in Subjects with Myelodysplastic Syndrome | Patients adminstered durvalumab intravenously. Azacitidine will be adminstered subcutaneously in combination with durvalumab. Tremelimumab adminstered intravenously. Durvalumab adminstered intravenously in combination with tremelilmumab. Patients adminstered durvalumab intravenously. Tremelimumab adminstered intravenously. Azacitidine will be adminstered subcutaneously in combination with durvalumab and tremelimumab. | Phase 1 Myelodysplastic Syndrome |
|
| NCT02775903 | Active, Not recruiting | An Efficacy and Safety Study of Azacitidine Subcutaneous in Combination with Durvalumab(MEDI4736) in Previously Untreated Subjects with Higher-Risk Myelodysplastic Syndromes (DS) or in Eldery Subjects with Acute Myeloid Leukemia (AML) | Experimental: Azacitidine adminstered at 75 mg/m2 subcutaneously for 7 days every 4 weeks. Durvalmab adminstered intravenously at 1500 mg on day 1 every 4 weeks. Active Comparator: Azacitidine adminstered at 75 mg/m2 subcutaneously every 7 days for 4 weeks. |
Phase 2 Acute Myeloid Leukemia, Myelodysplastic Syndromes |
|
| NCT02805660 | Active, Not recruiting | Phase 1/2 Study of Mocetinostat and Durvalumab in Patients with Advanced Solid Tumors and NSCLC | Mocetinostat adminstered orally three times weekly. Durvalumab adminstered at 1500 mg intravenously in 28 day cycles with mocetinostat. | Phase 1/ Phase 2 Advanced Cancer |
|
| NCT02915523 | Active, Not recruiting | Phase 1b/2 Study of Avelumab with or without Entinostat in Patietns with Advanced Epithelial Ovarian Cancer | Active Comparator: Avelumab adminstered intravenously on day 1 of each 14 day cycle. Entinostat adminstered on day 1 and day 8 of each cycle at maxium tolerated does (MTD)/ RP2D determined in phase 1b part of study. Placebo Comparator: Avelumab adminstered intravenously on day 1 of each 14 day cycle. Placebo adminstered on day 1 and day 8 of each cycle. |
Phase 1/ Phase 2 Epithelial Ovarian Cancer, Peritoneal Cancer, Fallopian Tube Cancer |
Several clinical trials are currently testing HDACi in combination with immunotherapy based on preclinical results showing that HDACi can prime the tumor to respond to immune therapy. NCT03765229 utilizes the HDACi entinostat (MS275) in combination with pembrolizumab (anti-PD-1) in melanoma. This trial will assess whether entinostat can cause the tumor to become less resistant to an immune system attack by making it more visible to the immune system. It will also investigate whether entinostat in combination with pembrolizumab shrinks the tumor in patients who had no immune cells within the tumor environment prior to treatment. The same combination therapy (entinostat and pembrolizumab) is being tested in myelodysplastic syndrome, non-small cell lung cancer, and colorectal cancer ( NCT02936752, NCT02437136, NCT02909452, NCT02697630). In lung cancer, salivary gland cancer, and renal cell carcinoma, the HDACi vorinostat is being tested in combination with pembrolizumab ( NCT02638090, NCT02538510, NCT02619253). The HDAC6i ACY241 is being tested in combination with pembrolizumab in non-small cell lung cancer ( NCT02635061). Other HDACi and immune checkpoint blockade combinations are in trials for melanoma ( NCT02032810), triple negative breast cancer ( NCT02708680), non-small cell lung cancer ( NCT02805660), and epithelial ovarian cancer ( NCT02915523).
Lastly, combination of DNMTi and HDACi with immune therapy has gone to clinical trials based on preclinical success in cell lines and mouse models. Trial #NCT02512172 in colorectal cancer patients combines oral azacytidine with the HDACi romidepsin and anti-PD-1. Other trials combine DNMTi, HDACi, and checkpoint blockade in gastrointestinal cancers ( NCT03812796), non-small cell lung cancer ( NCT00387465, NCT01928576), and advanced colorectal cancer ( NCT02512172).
Conclusions and future directions
Immunotherapy has proven an exciting and productive area of research for the treatment of many cancers. As our understanding of the anti-tumor immune response grows, so will our ability to harness the human immune system for the elimination of cancer. Many of the immune therapies discussed here are effective in a minority of patients. Future research will focus on improving existing immune therapies and critically assessing combination therapy to significantly improve patient outcomes. Because of their effect on the anti-tumor immune response, both HDACi and DNMTi are promising therapeutic agents to reverse tumor immune resistance and to sensitize tumors to immune therapy in a wide variety of solid tumors. We eagerly await results of ongoing clinical trials (Table 1), which will provide information on safety, efficacy, and potential biomarkers for these combinations. Utilizing epigenetic therapies to reverse tumor immune resistance and sensitize to curative immune therapy may prove to be a safe and effective way to treat multiple types of cancer, reaching large numbers of patients.
Acknowledgements
Research reported in this publication was supported by the National Cancer Institute under Award R00CA204592 (to K.B.C.).
Footnotes
Competing Interests
The authors declare no competing interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schreiber RD, Old LJ & Smyth MJ Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331, 1565–1570 (2011). [DOI] [PubMed] [Google Scholar]
- 2.Martínez-Lostao L, Anel A & Pardo J How Do Cytotoxic Lymphocytes Kill Cancer Cells? Clin Cancer Res 21, 5047–5056 (2015). [DOI] [PubMed] [Google Scholar]
- 3.Chan CJ, Smyth MJ & Martinet L Molecular mechanisms of natural killer cell activation in response to cellular stress. Cell Death and Differentiation 21, 5–14 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gershon RK & Kondo K Cell interactions in the induction of tolerance: the role of thymic lymphocytes. Immunology 18, 723–737 (1970). [PMC free article] [PubMed] [Google Scholar]
- 5.Sakaguchi S, Yamaguchi T, Nomura T & Ono M Regulatory T Cells and Immune Tolerance. Cell 133, 775–787 (2008). [DOI] [PubMed] [Google Scholar]
- 6.Sasada T, Kimura M, Yoshida Y, Kanai M & Takabayashi A CD4+CD25+ regulatory T cells in patients with gastrointestinal malignancies: possible involvement of regulatory T cells in disease progression. Cancer 98, 1089–1099 (2003). [DOI] [PubMed] [Google Scholar]
- 7.Gao Q et al. Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J. Clin. Oncol 25, 2586–2593 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Varol C, Mildner A & Jung S Macrophages: Development and Tissue Specialization. Annu. Rev. Immunol. 33, 643–675 (2015). [DOI] [PubMed] [Google Scholar]
- 9.Hu W et al. Tumor-associated macrophages in cancers. Clin Transl Oncol 18, 251–258 (2016). [DOI] [PubMed] [Google Scholar]
- 10.De Palma M & Lewis CE Macrophage Regulation of Tumor Responses to Anticancer Therapies. Cancer Cell 23, 277–286 (2013). [DOI] [PubMed] [Google Scholar]
- 11.Kuang D-M et al. Activated monocytes in peritumoral stroma of hepatocellular carcinoma foster immune privilege and disease progression through PD-L1. J Exp Med 206, 1327–1337 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wesolowski R, Markowitz J & Carson WE Myeloid derived suppressor cells – a new therapeutic target in the treatment of cancer. J Immunother Cancer 1, 10 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fleming V et al. Targeting Myeloid-Derived Suppressor Cells to Bypass Tumor-Induced Immunosuppression. Front. Immunol 9, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gabrilovich DI, Ostrand-Rosenberg S & Bronte V Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol 12, 253–268 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steggerda SM et al. Inhibition of arginase by CB-1158 blocks myeloid cell-mediated immune suppression in the tumor microenvironment. J Immunother Cancer 5, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Solito S et al. A human promyelocytic-like population is responsible for the immune suppression mediated by myeloid-derived suppressor cells. Blood 118, 2254–2265 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meyer C et al. Frequencies of circulating MDSC correlate with clinical outcome of melanoma patients treated with ipilimumab. Cancer Immunol. Immunother 63, 247–257 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newick K, O’Brien S, Moon E & Albelda SM CAR T Cell Therapy for Solid Tumors. Annual Review of Medicine 68, 139–152 (2017). [DOI] [PubMed] [Google Scholar]
- 19.Gill S, Maus MV & Porter DL Chimeric antigen receptor T cell therapy: 25years in the making. Blood Reviews 30, 157–167 (2016). [DOI] [PubMed] [Google Scholar]
- 20.Subklewe M, von Bergwelt-Baildon M & Humpe A Chimeric Antigen Receptor T Cells: A Race to Revolutionize Cancer Therapy. Transfus Med Hemother 46, 15–24 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neelapu SS et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat Rev Clin Oncol 15, 47–62 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao X et al. Cytokine-Induced Killer Cells As Pharmacological Tools for Cancer Immunotherapy. Front Immunol 8, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mohsenzadegan M, Peng R-W & Roudi R Dendritic cell/cytokine-induced killer cell-based immunotherapy in lung cancer: What we know and future landscape. J. Cell. Physiol (2019) doi: 10.1002/jcp.28977. [DOI] [PubMed] [Google Scholar]
- 24.Chen D et al. Cytokine-induced killer cells as a feasible adoptive immunotherapy for the treatment of lung cancer. Cell Death Dis 9, 1–12 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sabado RL, Balan S & Bhardwaj N Dendritic cell-based immunotherapy. Cell Res 27, 74–95 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Draube A et al. Dendritic cell based tumor vaccination in prostate and renal cell cancer: a systematic review and meta-analysis. PLoS ONE 6, e18801 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Topalian SL, Drake CG & Pardoll DM Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell 27, 450–461 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buchbinder EI & Desai A CTLA-4 and PD-1 Pathways. Am J Clin Oncol 39, 98–106 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peggs KS, Quezada SA, Chambers CA, Korman AJ & Allison JP Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumor activity of anti-CTLA-4 antibodies. J Exp Med 206, 1717–1725 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hodi FS et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med 363, 711–723 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keir ME, Butte MJ, Freeman GJ & Sharpe AH PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 26, 677–704 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robert C et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N. Engl. J. Med 372, 2521–2532 (2015). [DOI] [PubMed] [Google Scholar]
- 33.Ni L & Dong C New checkpoints in cancer immunotherapy. Immunol. Rev 276, 52–65 (2017). [DOI] [PubMed] [Google Scholar]
- 34.Long L et al. The promising immune checkpoint LAG-3: from tumor microenvironment to cancer immunotherapy. Genes Cancer 9, 176–189 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Das M, Zhu C & Kuchroo VK Tim-3 and its role in regulating anti-tumor immunity. Immunol Rev 276, 97–111 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J et al. VSIG-3 as a ligand of VISTA inhibits human T-cell function. Immunology 156, 74–85 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Linch SN, McNamara MJ & Redmond WL OX40 Agonists and Combination Immunotherapy: Putting the Pedal to the Metal. Front Oncol 5, (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rieth J & Subramanian S Mechanisms of Intrinsic Tumor Resistance to Immunotherapy. Int J Mol Sci 19, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baylin SB & Jones PA Epigenetic Determinants of Cancer. Cold Spring Harb Perspect Biol 8, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsai H-C et al. Transient Low Doses of DNA Demethylating Agents Exert Durable Anti-tumor Effects on Hematological and Epithelial Tumor Cells. Cancer Cell 21, 430–446 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaminskas E et al. Approval Summary: Azacitidine for Treatment of Myelodysplastic Syndrome Subtypes. Clin Cancer Res 11, 3604–3608 (2005). [DOI] [PubMed] [Google Scholar]
- 42.Villagra A et al. The histone deacetylase HDAC11 regulates the expression of interleukin 10 and immune tolerance. Nat. Immunol 10, 92–100 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Woods DM et al. HDAC Inhibition Upregulates PD-1 Ligands in Melanoma and Augments Immunotherapy with PD-1 Blockade. Cancer Immunol Res 3, 1375–1385 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Luo N et al. DNA methyltransferase inhibition upregulates MHC-I to potentiate cytotoxic T lymphocyte responses in breast cancer. Nat Commun 9, 1–11 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wylie B et al. Acquired resistance during adoptive cell therapy by transcriptional silencing of immunogenic antigens. OncoImmunology 8, 1609874 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Burr ML et al. An Evolutionarily Conserved Function of Polycomb Silences the MHC Class I Antigen Presentation Pathway and Enables Immune Evasion in Cancer. Cancer Cell 36, 385–401.e8 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siebenkäs C et al. Inhibiting DNA methylation activates cancer testis antigens and expression of the antigen processing and presentation machinery in colon and ovarian cancer cells. PLoS ONE 12, e0179501 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gameiro SR, Malamas AS, Tsang KY, Ferrone S & Hodge JW Inhibitors of histone deacetylase 1 reverse the immune evasion phenotype to enhance T-cell mediated lysis of prostate and breast carcinoma cells. Oncotarget 7, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jung H et al. DNA methylation loss promotes immune evasion of tumours with high mutation and copy number load. Nat Commun 10, 4278 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maecker HL, Yun Z, Maecker HT & Giaccia AJ Epigenetic changes in tumor Fas levels determine immune escape and response to therapy. Cancer Cell 2, 139–148 (2002). [DOI] [PubMed] [Google Scholar]
- 51.Ladle BH et al. De novo DNA methylation by DNA methyltransferase 3a controls early effector CD8+ T-cell fate decisions following activation. PNAS 113, 10631–10636 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Youngblood B et al. Effector CD8 T cells dedifferentiate into long-lived memory cells. Nature 552, 404–409 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ghoneim HE et al. De Novo Epigenetic Programs Inhibit PD-1 Blockade-Mediated T Cell Rejuvenation. Cell 170, 142–157.e19 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lal G et al. Epigenetic Regulation of Foxp3 Expression in Regulatory T Cells by DNA Methylation. The Journal of Immunology 182, 259–273 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zingg D et al. The Histone Methyltransferase Ezh2 Controls Mechanisms of Adaptive Resistance to Tumor Immunotherapy. Cell Reports 20, 854–867 (2017). [DOI] [PubMed] [Google Scholar]
- 56.Lai X et al. Modeling combination therapy for breast cancer with BET and immune checkpoint inhibitors. Proc Natl Acad Sci U S A 115, 5534–5539 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peng D et al. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature 527, 249–253 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhu H et al. BET Bromodomain Inhibition Promotes Anti-Tumor Immunity by Suppressing PD-L1 expression. Cell Rep 16, 2829–2837 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang W & Tan J Co-inhibition of BET proteins and PD-L1 as a potential therapy for OSCC through synergistic inhibition of FOXM1 and PD-L1 expressions. Journal of Oral Pathology & Medicine 0, (2019). [DOI] [PubMed] [Google Scholar]
- 60.Hogg SJ et al. BET-Bromodomain Inhibitors Engage the Host Immune System and Regulate Expression of the Immune Checkpoint Ligand PD-L1. Cell Rep 18, 2162–2174 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chiappinelli KB et al. Inhibiting DNA methylation causes an interferon response in cancer via dsRNA including endogenous retroviruses. Cell 162, 974–986 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li H et al. Immune regulation by low doses of the DNA methyltransferase inhibitor 5-azacitidine in common human epithelial cancers. Oncotarget 5, 587 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Karpf AR et al. Inhibition of DNA methyltransferase stimulates the expression of signal transducer and activator of transcription 1, 2, and 3 genes in colon tumor cells. Proc. Natl. Acad. Sci. U.S.A 96, 14007–14012 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Karpf AR et al. Limited gene activation in tumor and normal epithelial cells treated with the DNA methyltransferase inhibitor 5-aza-2’-deoxycytidine. Mol. Pharmacol 65, 18–27 (2004). [DOI] [PubMed] [Google Scholar]
- 65.Roulois D et al. DNA-Demethylating Agents Target Colorectal Cancer Cells by Inducing Viral Mimicry by Endogenous Transcripts. Cell 162, 961–973 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wrangle J et al. Alterations of immune response of non-small cell lung cancer with Azacytidine. Oncotarget 4, 2067–2079 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Siebenkäs C et al. Inhibiting DNA methylation activates cancer testis antigens and expression of the antigen processing and presentation machinery in colon and ovarian cancer cells. PLOS ONE 12, e0179501 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brocks D et al. DNMT and HDAC inhibitors induce cryptic transcription start sites encoded in long terminal repeats. Nat. Genet 49, 1052–1060 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu M et al. Dual Inhibition of DNA and Histone Methyltransferases Increases Viral Mimicry in Ovarian Cancer Cells. Cancer Res. (2018) doi: 10.1158/0008-5472.CAN-17-3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu M et al. Vitamin C increases viral mimicry induced by 5-aza-2′-deoxycytidine. PNAS 113, 10238–10244 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dangaj D et al. Cooperation between Constitutive and Inducible Chemokines Enables T Cell Engraftment and Immune Attack in Solid Tumors. Cancer Cell 35, 885–900.e10 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ghoneim HE et al. De Novo Epigenetic Programs Inhibit PD-1 Blockade-Mediated T Cell Rejuvenation. Cell 170, 142–157.e19 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang L et al. Decitabine Enhances Lymphocyte Migration and Function and Synergizes with CTLA-4 Blockade in a Murine Ovarian Cancer Model. Cancer Immunol Res 3, 1030–1041 (2015). [DOI] [PubMed] [Google Scholar]
- 74.Lisiero DN, Soto H, Everson RG, Liau LM & Prins RM The histone deacetylase inhibitor, LBH589, promotes the systemic cytokine and effector responses of adoptively transferred CD8+ T cells. J Immunother Cancer 2, 8 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Walton J et al. CRISPR/Cas9-Mediated Trp53 and Brca2 Knockout to Generate Improved Murine Models of Ovarian High-Grade Serous Carcinoma. Cancer Res 76, 6118–6129 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stone ML et al. Epigenetic therapy activates type I interferon signaling in murine ovarian cancer to reduce immunosuppression and tumor burden. Proc. Natl. Acad. Sci. U.S.A 114, E10981–E10990 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chiappinelli KB, Zahnow CA, Ahuja N & Baylin SB Combining Epigenetic and Immunotherapy to Combat Cancer. Cancer Res. 76, 1683–1689 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Strick R, Strissel PL, Baylin SB & Chiappinelli KB Unraveling the molecular pathways of DNA-methylation inhibitors: human endogenous retroviruses induce the innate immune response in tumors. OncoImmunology 5, e1122160 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zheng H et al. HDAC Inhibitors Enhance T-Cell Chemokine Expression and Augment Response to PD-1 Immunotherapy in Lung Adenocarcinoma. Clin Cancer Res 22, 4119–4132 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim K et al. Eradication of metastatic mouse cancers resistant to immune checkpoint blockade by suppression of myeloid-derived cells. PNAS 111, 11774–11779 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Juergens RA et al. Combination Epigenetic Therapy Has Efficacy in Patients with Refractory Advanced Non Small Cell Lung Cancer. Cancer Discov 1, 598–607 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ramalingam SS et al. Carboplatin and Paclitaxel in Combination With Either Vorinostat or Placebo for First-Line Therapy of Advanced Non–Small-Cell Lung Cancer. J Clin Oncol 28, 56–62 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fang F et al. The novel, small-molecule DNA methylation inhibitor SGI-110 as an ovarian cancer chemosensitizer. Clin. Cancer Res 20, 6504–6516 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fu S et al. Phase Ib-IIa study to reverse platinum resistance by the use of a hypomethylating agent azacitidine in platinum-resistant or refractory epithelial ovarian cancer. Cancer 117, 1661–1669 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Matei D et al. Epigenetic Resensitization to Platinum in Ovarian Cancer. Cancer Res 72, 2197–2205 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]