Abstract
Objective
To describe trends in licensed substance use treatment facilities' adoption of telemedicine and how adoption varies across local factors, including county-level drug overdose rates, urbanicity measures, and state policy laws.
Methods
We analyzed data (2016–2019) from the National Directory of Drug and Alcohol Abuse Treatment Facilities. Our main outcome was telemedicine use by a treatment facility. We also captured independent variables from other datasets, including estimated county-level drug poisoning deaths and state-level telemedicine policies. We estimated a multivariable logistic regression model to determine which facility characteristics were associated with offering telemedicine.
Results
From 2016 to 2019, an average of 12,334 treatment facilities were included. During this period, the unadjusted proportion of facilities offering telemedicine grew from 13.5% to 17.4% (p < 0.001). In adjusted models, rural location; offering multiple treatment settings; offering pharmacotherapy; and serving both adult and pediatric patients were associated with greater telemedicine adoption (p < 0.05 for all comparisons).
Discussion
Use of telemedicine is increasing steadily among substance use disorder (SUD) treatment facilities; however, uptake is uneven and relatively low. As such, telemedicine may be an underutilized tool to expand access to care for patients with SUDs.
1. Introduction
Connecting individuals with substance use disorders (SUD) to evidence-based treatment is a key challenge in the U.S. (American Society of Addiction Medicine, 2015) In 2017, only 20% of individuals who needed substance use treatment for alcohol or illicit drug use, received it (Substance Abuse and Mental Health Services Administration, 2018). Barriers to treatment include limits on insurance coverage, stigma, and provider shortages—in particular waivered providers who prescribe medications for opioid use disorder (OUD) (e.g., buprenorphine) (Rapp et al., 2006). Access challenges are particularly problematic in rural and other underserved communities (Haffajee et al., 2018).
Telemedicine, in the form of live videoconferencing with a clinician, is a potential solution (Association for Behavioral Health and Wellness, 2016; Liebelt et al., 2017; National Alliance on Mental Illness, 2018; Substance Abuse and Mental Health Services Administration, 2015; The President's Commission on Combating Drug Addiction and the Opioid Crisis, 2017). Treatment facilities in underserved areas can leverage telemedicine for SUD services to enable access to care that otherwise would not be available. Telemedicine services in this setting can include individual and group treatments, such as medication management, counseling, psychotherapy, and case management. Regulatory barriers have inhibited telemedicine for SUD, most notably from the Ryan Haight Act, which restricts prescribing controlled substances, such as buprenorphine, through telemedicine. Recent policy changes such as the 2018 SUPPORT Act have begun to eliminate many of these regulatory and reimbursement barriers to delivering telemedicine for SUDs. Though use rates remain low, recent work has highlighted the rapid growth of telemedicine for SUD (Huskamp et al., 2018).
Despite this growth, little is known about adoption of telemedicine for SUD. Many factors may influence adoption, including the local provider workforce and local policy environment (e.g., whether visits are reimbursed). To date, there is little evidence on telemedicine adoption by SUD treatment facilities and how it varies across geography and different patient populations. To address this gap in the literature, we studied trends in licensed treatment facilities' adoption of telemedicine and how adoption varies across local factors, including county-level drug overdose rates, urbanicity measures, and state policy laws.
2. Methods
We analyzed data from the National Directory of Drug and Alcohol Abuse Treatment Facilities, which the Substance Abuse and Mental Health Services Administration (SAMHSA) publishes annually. The directory includes all licensed SUD treatment facilities that participated in the previous year's National Survey of Substance Abuse Treatment Services (N-SSATS) and agreed to be listed. In 2018, 14,809 facilities participated in the N-SSATS for a response rate of 92% (Substance Abuse and Mental Health Services Administration, 2019). The directory includes location of the facility, service setting, facility ownership, patient population, and the types of treatment available. We limited our sample to licensed treatment facilities that provided SUD treatment and reported on their adoption of telemedicine each year (83% of participating facilities).
Our main outcome was telemedicine use by a SUD facility. This was defined as facilities that “sometimes” or “always or often” used “computerized substance abuse treatment/telemedicine,” which was asked as part of a checklist of items under the heading “Which of these clinical/therapeutic approaches are offered at this facility?” SAMHSA interprets this question as providing information on whether facilities provide telemedicine, and includes a filter on telemedicine use (yes/no) based on this question in its publicly available Behavioral Health Treatment Services Locator database (Behavioral Health Treatment Services Locator, 2020). We also captured independent variables from other datasets, including estimated county-level drug poisoning death rates from the National Vital Statistics System (Centers for Disease Control and Prevention, 2019); state-level telemedicine policy regarding coverage and reimbursement in 2016 using published American Telemedicine Association (ATA) grades (A,B,C) (Thomas & Capistrant, 2017); and the presence of a telemedicine parity law (yes/no) that required private payers to reimburse for telemedicine (Center for Connected Health Policy, 2017).
We calculated the unadjusted proportion of facilities offering telemedicine from 2016 to 2019. Using chi-squared tests, we compared adoption rates by year. We estimated a multivariable logistic regression model to determine which facility characteristics were associated with offering telemedicine in 2019, the most recent year for which data were available. The unit of analysis was the facility, and the outcome was whether the facility offered telemedicine services in 2019. Variables in the model were U.S. region, urbanicity, treatment setting (inpatient only, residential only, outpatient only, multiple), SUD pharmacotherapy services offered, Medicaid acceptance, drug-related mortality rate in the county, facility ownership, patient populations served, state ATA grade, and state telemedicine parity law. We used robust standard errors, clustered at the state level. Harvard's Institutional Review Board declared this study to be exempt from review.
3. Results
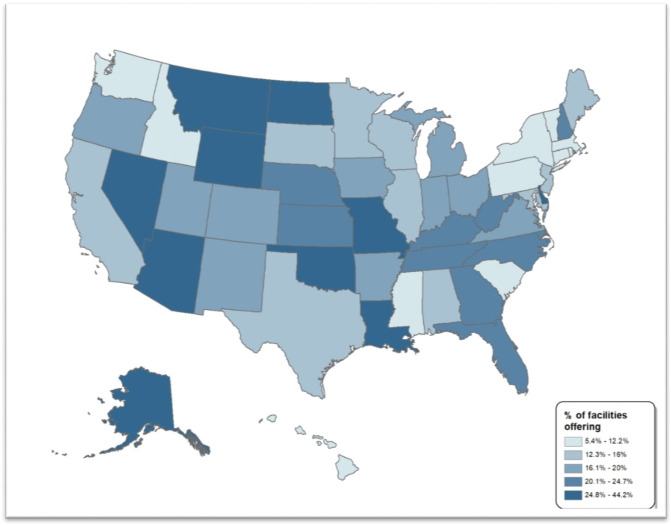
From 2016 to 2019, an average of 12,334 treatment facilities were included in our sample. Over the four-year period, the unadjusted proportion of facilities that reported offering telemedicine grew from 13.5% in 2016 to 17.4% in 2019 (p < 0.001). In 2019, there was wide state-to-state variation in facility adoption of telemedicine; <7% of facilities in Connecticut, Hawaii, Rhode Island, and Vermont offered tele-SUD services compared to >40% in Alaska, Missouri, and Wyoming (Fig. 1 ).
Fig. 1.
Proportion of substance abuse treatment facilities offering telemedicine for SUDs by state.
Facilities offering telemedicine differed from those that did not in several ways. In adjusted models, rural location; offering multiple treatment settings; offering pharmacotherapy; and serving both adult and pediatric patients were associated with greater telemedicine adoption (p < 0.05 for all comparisons) (Table 1 ). Notable differences included rural location, with 22.4% of facilities in rural areas offering telemedicine vs. 15.8% in metropolitan areas (p < 0.001); and pharmacotherapy offered, with 21.0% of facilities that offered naltrexone, methadone, buprenorphine, acamprosate, and/or disulfiram offering telemedicine vs. 14.2% that did not offer any of these pharmacotherapy services (p < 0.001). There were no statistically significant differences in facility telemedicine adoption across state-level telemedicine policy variables, county drug-related mortality rate, Medicaid acceptance, or facility ownership.
Table 1.
Characteristics of substance abuse treatment facilities by telemedicine adoption.
| Tele-SUD offered (n = 2247) |
Tele-SUD not offered (n = 10,660) |
Adjusted odds ratio | 95% confidence interval | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| U.S. region | ||||||
| Midwest | 599 | 18.8 | 2584 | 81.2 | Ref | |
| Northeast | 295 | 11.3 | 2307 | 88.7 | 0.50⁎⁎⁎ | [0.43,0.59] |
| South | 708 | 20.4 | 2765 | 79.6 | 1.07 | [0.94,1.22] |
| West | 645 | 17.7 | 3004 | 82.3 | 0.93 | [0.80,1.07] |
| Metropolitan locationa | ||||||
| Metropolitan | 1531 | 15.8 | 8173 | 84.2 | Ref | |
| Not metropolitan | 716 | 22.4 | 2487 | 77.6 | 1.51⁎⁎⁎ | [1.36,1.68] |
| Type of treatment center | ||||||
| Outpatient only | 1601 | 16.9 | 7883 | 83.1 | Ref | |
| Hospital inpatient only | 17 | 8.3 | 187 | 91.7 | 0.42⁎⁎⁎ | [0.25,0.70] |
| Residential only | 288 | 15.6 | 1559 | 84.4 | 1.12 | [0.97,1.30] |
| Multiple settings | 341 | 24.9 | 1031 | 75.1 | 1.49⁎⁎⁎ | [1.30,1.72] |
| Pharmacotherapy services | ||||||
| Does not offer SUD medicationsb | 981 | 14.2 | 5905 | 85.8 | Ref | |
| Offers one or more SUD medications | 1266 | 21.0 | 4755 | 79.0 | 1.85⁎⁎⁎ | [1.67,2.04] |
| Forms of payment | ||||||
| Does not accept Medicaid | 697 | 16.5 | 3540 | 83.5 | Ref | |
| Accept Medicaid | 1550 | 17.9 | 7120 | 82.1 | 1.09 | [0.97,1.22] |
| Drug-related mortalityc | ||||||
| Location (county) in bottom tertile for drug related mortality rate | 724 | 16.5 | 3657 | 83.5 | Ref | |
| Location (county) in top tertile for drug related mortality rate | 928 | 17.3 | 4426 | 82.7 | 1.13⁎ | [1.01,1.27] |
| Patient population | ||||||
| Serves children (no age limit or 10+) | 1077 | 18.3 | 4821 | 81.7 | Ref | |
| Serves adults only (17+) | 1170 | 16.7 | 5839 | 83.3 | 0.82⁎⁎⁎ | [0.73,0.91] |
| Facility ownership | ||||||
| Government | 234 | 19.6 | 958 | 80.4 | Ref | |
| Private for-profit organization | 893 | 17.9 | 4109 | 82.1 | 1.05 | [0.89,1.25] |
| Private non-profit organization | 1120 | 16.7 | 5593 | 83.3 | 0.97 | [0.83,1.14] |
| American Telemedicine Association Grade for State (2016)d | ||||||
| A | 253 | 18.1 | 1143 | 81.9 | Ref | |
| B | 1634 | 17.6 | 7640 | 82.4 | 1.08 | [0.93,1.27] |
| C | 360 | 16.1 | 1877 | 83.9 | 0.9 | [0.73,1.10] |
| Telemedicine Parity Law (2016) | ||||||
| No | 851 | 17.0 | 4142 | 83.0 | Ref | |
| Yes | 1396 | 17.6 | 6518 | 82.4 | 1 | [0.90,1.12] |
Calculated using National Center for Health Statistics Urban-Rural Classification Scheme for Counties.
Defined as not offering any of the following medications: Naltrexone, Methadone, Buprenorphine, Acamprosate or Disulfiram.
Calculated using National Vital Statistics System multiple cause-of-death mortality files.
ATA grade captures the extent to which state policies governing the Medicaid program and private payers are telemedicine friendly. The ATA grade accounts for various restrictions on the practice and reimbursement of telemedicine services.
p < 0.05.
p < 0.001.
4. Discussion
Although adoption of telemedicine is increasing, <20% of licensed treatment centers offered telemedicine services by 2019. This adoption rate is lower than the adoption rate for telemedicine by other healthcare organizations; in 2016, 26% of all mental health facilities (Zhao et al., 2019) and 58% of all hospitals reported using telemedicine for different health conditions (Zachrison et al., 2018). Several factors may explain SUD facilities' lower adoption of telemedicine, including patient acceptance, patient and provider awareness of telemedicine, regulatory restrictions on prescribing controlled medications via telemedicine (which the SUPPORT Act addresses, but it has not yet been fully implemented), and constrained resources to purchase the telemedicine infrastructure (Zhao et al., 2019).
There was notable state-to-state variation in uptake and treatment facilities located in rural areas, and those that offered pharmacotherapy services had higher rates of adoption. However, despite the opportunity that telemedicine offers for SUD pharmacotherapy, we note the very low rates of pharmacotherapy adoption overall, and among SUD providers who use telemedicine. The fact that facilities treating both adults and children were more likely to adopt telemedicine could reflect the use of telemedicine to bring in pediatric expertise (e.g., pediatric psychiatrists) that may be lacking in the community.
Data for this study were collected prior to the COVID-19 pandemic. The pandemic is likely to have a major impact on telemedicine adoption, as facilities implement social distancing and various regulatory and reimbursement barriers to telemedicine are relaxed. Future research is needed to examine changes in telemedicine adoption beyond 2020, and this study provides important information about the state of telemedicine in substance use treatment facilities pre-COVID-19.
Our study had several limitations. First, our analysis was limited to licensed facilities. Second, we do not know how facilities are using telemedicine, and given how the survey question was worded, respondents may also interpret digital services (e.g., online psychoeducation resources) as telemedicine.
4.1. Public health implications
Telemedicine use is growing steadily among licensed treatment facilities; however, uptake is uneven and relatively low compared to telemedicine adoption among other healthcare organizations. As such, telemedicine may be an underutilized tool to expand access to care for patients with SUDs. Further research is needed on what drives facilities to invest in telemedicine for SUDs and to examine its effectiveness.
Author statement
Lori Uscher-Pines: Conceptualized of the study, helped to secure funding, provided oversight, supported data analysis, drafted manuscript.
Jonathan Cantor: Conceptualized of the study, conducted the data analysis, drafted manuscript.
Haiden A Huskamp: Conceptualized of the study, helped to secure funding, provided oversight, helped with data interpretation, reviewed and edited the manuscript.
Ateev Mehrotra: Conceptualized of the study, helped to secure funding, provided oversight, helped with data interpretation, reviewed and edited the manuscript.
Alisa Busch: Conceptualized of the study, helped with data interpretation, reviewed and edited the manuscript.
Michael Barnett: Conceptualized of the study, provided oversight, supported data analysis, reviewed and edited the manuscript.
Funding statement
This project was supported by NIDA (R01 DA048533).
Declaration of competing interest
The authors have no conflicts of interest to disclose.
References
- American Society of Addiction Medicine The ASAM national practice guideline for the use of medications in the treatment of addiction involving opioid use. 2015. https://www.asam.org/docs/default-source/practice-support/guidelines-and-consensus-docs/asam-national-practice-guideline-supplement.pdf [DOI] [PMC free article] [PubMed]
- Association for Behavioral Health and Wellness Advocacy: Telehealth. 2016. http://www.abhw.org/issues/
- Behavioral Health Treatment Services Locator 2020. https://findtreatment.samhsa.gov/
- Center for Connected Health Policy . 2017. State telehealth laws and reimbursement policies. [Google Scholar]
- Centers for Disease Control and Prevention NCHS - Drug poisoning mortality by county: United States. 2019. https://data.cdc.gov/NCHS/NCHS-Drug-Poisoning-Mortality-by-County-United-Sta/rpvx-m2md
- Haffajee R.L., Bohnert A.S.B., Lagisetty P.A. Policy pathways to address provider workforce barriers to buprenorphine treatment. American Journal of Preventive Medicine. 2018;54(6 Suppl 3):S230–s242. doi: 10.1016/j.amepre.2017.12.022. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huskamp H.A., Busch A., Souza J., et al. How is telemedicine being used in opioid and other substance use disorder treatment? Health Affairs (Millwood) 2018;37(12):1940–1947. doi: 10.1377/hlthaff.2018.05134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebelt E.R.S., Nathan I., Bruland P. Telehealth as means to diagnose and treat opioid abuse. 2017. https://www.himss.org/news/telehealth-means-diagnose-and-treat-opioid-abuse HIMSS.
- National Alliance on Mental Illness NAMI policy brief: Mental illness and the opioid crisis. 2018. https://www.sheriffs.org/sites/default/files/NAMI%20Mental%20Illness%20and%20the%20Opioid%20Crisis.pdf
- Rapp R.C., Xu J., Carr C.A., Lane D.T., Wang J., Carlson R. Treatment barriers identified by substance abusers assessed at a centralized intake unit. Journal of Substance Abuse Treatment. 2006;30(3):227–235. doi: 10.1016/j.jsat.2006.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration CCBHCs using telehealth or telemedicine. 2015. https://www.samhsa.gov/section-223/care-coordination/telehealth-telemedicine
- Substance Abuse and Mental Health Services Administration . 2018. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2019. National survey of substance abuse treatment services (N-SSATS): 2018. [Google Scholar]
- The President's Commission on Combating Drug Addiction and the Opioid Crisis 2017. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Final_Report_Draft_11-1-2017.pdf [DOI] [PubMed]
- Thomas L., Capistrant G. 2017. State telemedicine gaps analysis: Coverage and reimbursement. (American Telemedicine Association) [Google Scholar]
- Zachrison K.S., Boggs K.M., E M.H., Espinola J.A., Camargo C.A. A national survey of telemedicine use by US emergency departments. Journal of Telemedicine and Telecare. 2018 doi: 10.1177/1357633X18816112. [DOI] [PubMed] [Google Scholar]
- Zhao X., Innes K.E., Bhattacharjee S., Dwibedi N., LeMasters T.M., Sambamoorthi U. Facility and state-level factors associated with telemental health (TMH) adoption among mental health facilities in the United States. Journal of Telemedicine and Telecare. 2019 doi: 10.1177/1357633X19868902. [DOI] [PMC free article] [PubMed] [Google Scholar]