This cohort study compares injury event rates among Taiwanese children with and without parents with serious mental illness.
Key Points
Question
Are young children whose parents have severe mental illness, including schizophrenia, bipolar disorder, and major depressive disorder, at greater risk of injury compared with children of parents without severe mental illness?
Findings
In this cohort study of the 1 999 322 singleton births in Taiwan from 2004 to 2014, children of parents with severe mental illness had higher rates of injury events, injury hospitalization, and injury death in early childhood compared with children of parents without severe mental illness.
Meaning
In this study, parental severe mental illness was associated with increased risk of several child injury outcomes during early childhood, suggesting that effective treatment, parenting support, and injury prevention strategies for parents with severe mental illness may be needed.
Abstract
Importance
Injury is a leading cause of childhood morbidity and mortality worldwide. Serious mental illness (SMI) is a major contributor to the global burden of disease.
Objective
To compare injury event rates in children from birth to 5 years of age among Taiwanese children with and without parents with SMI, including schizophrenia, bipolar disorder, and major depressive disorder.
Design, Setting, and Participants
This population-based, retrospective cohort study of an 11-year Taiwanese birth cohort used data from the Taiwan National Health Insurance Research Database (covering 99% of Taiwanese citizens), the Maternal and Child Health Database, and birth and death certificate databases. The study included 1 999 322 singletons with Taiwanese citizenship born from January 1, 2004, to December 31, 2014, and followed up from birth to their fifth birthday, December 31, 2014, or the date of death, yielding a total of 7 741 026 person-years. Data analysis was performed from April 20, 2017, to September 24, 2019.
Exposures
Physician-diagnosed parental SMI defined using outpatient and inpatient records from 6 years before the child’s birth to 5 years after delivery.
Main Outcome and Measures
Rates of medically attended injury events, injury hospitalization, and injury death retrieved from outpatient records, inpatient records, and death certificates. Generalized estimating equation for log-linear models estimated injury incidence rate ratios (IRRs) comparing parental SMI-exposed children and unexposed children.
Results
The study cohort included 1 999 322 singletons (52.1% males without parental SMI and 52.2% males with parental SMI). Incidence rates of child injury-related outcomes were higher among children exposed to parental SMI (294.8 injury events per 1000 person-years) compared with children who were unexposed (256.1 injury events per 1000 person-years). After adjustment for sociodemographic factors, children with parental SMI had higher rates of injury events (IRR, 1.14; 95% CI, 1.13-1.15), injury hospitalization (IRR, 1.49; 95% CI, 1.42-1.57), and injury death (IRR, 1.82; 95% CI, 1.38-2.39) compared with unexposed children. The results were confirmed in sensitivity analyses. Appendicitis, a negative control outcome, was not associated with parental SMI (IRR, 1.10; 95% CI, 0.94-1.28). In addition, children with and without parental SMI had similar patterns of preventive health care. The mean (SD) number of prenatal visits was 8.09 (2.50) for children with parental SMI and 8.17 (2.47) among unaffected children. The mean (SD) number of well-child visits was 5.70 (2.24) for children with parental SMI and 5.80 (2.21) among unaffected children.
Conclusions and Relevance
In this study, children with parental SMI had increased risk of injury, particularly serious injury. Excess risk may be reduced by providing effective mental health treatment, parenting support, and home safety education to parents with SMI who are raising young children.
Introduction
Mental illness affects cognition, mood, and behavior and can impair social and occupational functioning. Most mental illnesses are chronic or recurring health conditions first recognized in adolescence or early adulthood and thus have the potential to impair functioning across the life span.1 In 2010, mental illness was the leading cause of years lived with disability worldwide, accounting for 22.9% of all years lived with disability.1 Serious mental illnesses (SMIs), such as schizophrenia, bipolar disorder, and major depressive disorder, are typically associated with greater interference with life activities.2
Given its potential effects on parents and children, parental mental illness is an important public health issue. Related research has focused primarily on maternal depression and its association with child cognitive and language development3 as well as emotional health.4 Parental SMI before childbirth is associated with adverse neonatal outcomes, including premature birth and low birth weight.4,5,6 The effects of parental mental illness on other child physical health conditions are less well known.
Injury is a leading cause of childhood disability worldwide7 and can also have long-term influences on the child and family. Maternal depression has been associated with increased risk of childhood injury.8,9,10 However, most prior studies8,11 used self-reported rating scales administered at a single time point to measure mental health and focused exclusively on maternal perinatal depression (rather than other types of mental illness, other periods, and SMI in both parents). To fill current knowledge gaps, we used national databases in Taiwan to conduct a retrospective cohort study investigating associations between the mother’s and the father’s SMI during an 11-year period surrounding their child’s birth and child injuries before the age of 5 years.
Methods
Data Sources
This cohort study used 4 Taiwanese national databases: the National Health Insurance Research Database (NHIRD), the Maternal and Child Health Database (MCHD), and birth and death certificate databases. In Taiwan, every citizen and foreign resident is assigned a unique national identification number (ID) and a foreign ID, respectively. The Taiwan Health and Welfare Data Science Center used the same encryption algorithm to encrypt these IDs across databases. The Taiwan Health and Welfare Data Science Center and the Cathay General Hospital Institutional Review Board approved this study and exempted informed consent because these databases were anonymized.
The NHIRD contains the insured individual’s sociodemographic and claims data from medical facilities contracted with the Taiwan’s National Health Insurance (NHI) Program. The NHI was established in March 1995, and by 2003, the coverage rate was 99.9% or more of the population.12 In 2015, the NHI contracted with more than 93% of health care institutions in Taiwan.13 The NHI does not use a gatekeeper system; thus, the insured individual can choose any clinic, hospital, or specialist without a referral. The MCHD contains IDs of Taiwanese children (n = 2 171 765) registered from January 1, 2004, to December 31, 2014, and their parents’ IDs, which provide the primary parent-child linkages. The birth certificate database included all live births and reported stillbirths that occurred in Taiwan from January 1, 2004, to December 31, 2014 (n = 2 252 573) and contains only the mother's ID. The death certificate database comprised all deaths that occurred from January 1, 1998, to December 31, 2014, among Taiwanese citizens (n = 2 354 328).
Study Cohort
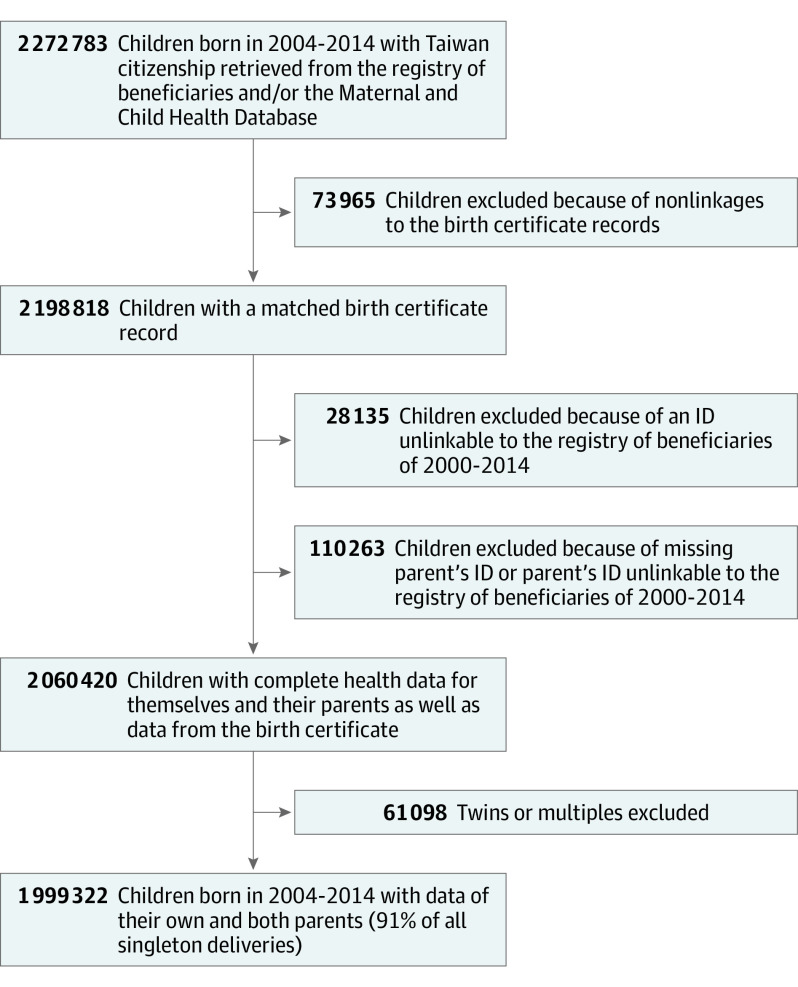
From the registry of beneficiaries of the NHIRD, we retrieved data for 2 225 067 Taiwanese children born from January 1, 2004, to December 31, 2014 (eMethods 1 in the Supplement). We used an exact deterministic linkage to match child-parent pairs and triads in the MCHD and/or the registry of beneficiaries to birth certificates (eMethods 2 in the Supplement). The study cohort was restricted to singletons with complete health data for themselves and 2 parents and birth certificate data. Among the 2 272 783 Taiwanese children born between 2004 and 2014 whose data were retrieved from the MCHD and/or the registry of beneficiaries, 273 461 (12.0%) were excluded (Figure and eMethods 3 in the Supplement).
Figure. Flowchart of Study Cohort Selection.
ID indicates identification number.
Exposure
The exposure variable was SMI in the mother and/or father of a child within our cohort. To initially identify parental SMI exposure, we used parents’ health claims with a visit date from 6 years before childbirth to 5 years after childbirth and relevant diagnostic code(s) for schizophrenia, bipolar disorder, or major depressive disorder (Table 1). A formal SMI disorder was further defined by diagnoses made at least once by a psychiatrist or twice by nonpsychiatric physician(s). If a parent received an SMI diagnosis during the period from 6 years before childbirth until the date of the childbirth, the child was considered exposed from birth to the fifth birthday. If the first SMI diagnosis was given to a parent between the childbirth and the fifth birthday, the child was considered unexposed until the occurrence of first SMI diagnosis and exposed thereafter. Children whose parents did not have an SMI diagnosis anytime within the aforementioned 11-year period were considered unexposed during the follow-up period.
Table 1. ICD-9-CM Codes Used to Define Exposure and Outcomes of Interest.
| Variable | Data sources | Diagnosis codes |
|---|---|---|
| Parental serious mental illness | Inpatient and outpatient records | Serious mental illness includes schizophrenia, bipolar disorder, and major depressive disorder. ICD-9-CM codes: schizophrenia: 295, 297, 298.3, 298.4, 298.9; bipolar disorder: 296.00-296.16, 296.40-296.81, 296.89-296.99, 298.1, 648.4; MDD: 296.20-296.36, 296.82, 298.0a |
| Child injury events | Inpatient and outpatient recordsb | ICD-9-CM codes: injury: 800-999, excluding 905–909.9 (late effects), 958–958.8 (traumatic complications), and 995–999.9 (complications of medical care); injury types14: fracture skull vault/base: 800-801.9; fracture skull (apart from vault/base): 802-804.9; intracranial injury: 850-854.1; nerve and spinal cord: 950-957.9; burns: 940-949.9; fracture neck and trunk: 805-809.9; fracture upper limb: 810-818.9; fracture lower limb: 820-827.9, 829-829.9; multiple fractures of limbs: 819-819.1, 828-828.1; internal trauma: 860-869.1; vascular injury: 900-904.9; crush injury: 925-929.9; open wounds: 870-897.9; superficial injuries and contusion: 910-924.9; dislocations, strains, and sprains: 830-848.9; foreign body: 930-939.9; poisoning: 960-989.9 |
| Child injury hospitalization | Inpatient and outpatient recordsb | Injury events resulting in hospitalization |
| Child injury death | Inpatient records and death certificatesb | Inpatient records: injury-related ICD-9 codes and an expired discharge status; death certificates: D_CODE (ICD-9 E codes) from 2004 to 2007: accident: 800-949, homicide: 960-969, trauma (ICD-9 codes) from 2004 to 2007: 800-994; ICD-10 (ICD-10 codes) after 2008: accident: V01-X59, Y85-Y86; homicide: X85-Y09 |
| Child appendicitis (negative control) | Inpatient and outpatient recordsb | ICD-9-CM codes: 540-542 |
Abbreviations: ICD-9, International Classification of Diseases, Ninth Revision; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; MDD, major depressive disorder; SMI, serious mental illness.
The SMI value was positive after the date of onset for maternal or paternal SMI, whichever came first.
Because infants are typically covered by their parents’ insurance for 60 days, we first retrieved parents’ health claims that belonged to infants (eMethods 4 in the Supplement) as well as all child health claims.
Outcomes
The first outcome was medically attended injury events in children younger than 5 years (measured by International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes) (Table 1). A single injury event comprised all successive visits of the same injury type14 in which an interval between 2 visits was less than 90 days, whereas events recorded 90 days or more after a prior event were considered new injury events. This interval was used rather than the 180-day interval adopted in other studies14,15 because young children typically recover sooner than older children.16,17 In addition, our exploratory analyses found that frequencies of new claims occurring after an injury visit became relatively stable after 12 weeks (eFigure 1 in the Supplement). When creating the outcome injury events to account for multiple injury types that resulted from a single event, a new injury type recorded within 7 days of an initial injury was considered as the same event.14 Injury hospitalization was defined as an injury event that resulted in hospitalization. Injury death was defined on the basis of expired discharge status in inpatient records and/or International Classification of Diseases, Ninth Revision (ICD-9) E codes (2004-2007) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes (2008-2014) on death certificates (Table 1).
First-event appendicitis (Table 1), a condition for which the origin should not be associated with parental SMI, was evaluated as a negative control outcome.18 To evaluate whether injury ascertainment might be biased by differences in health care–seeking behavior, we compared prenatal and well-child visits and median child ages at the third and fifth well-child visits for children with and without parental SMI who were born before 2010 and had complete 5-year follow-up data (eMethods 5 in the Supplement).
Covariates
Relevant covariates measured at a child’s birth (eMethods 6 in the Supplement) included birth year, sex, birth order, low birth weight (<2500 g), preterm birth (<37 weeks), urbanicity of residence, parental ages, mother’s marital status, mother born outside Taiwan, monthly family income, and parental occupations and physical illness (defined by the Elixhauser comorbidity index that excluded psychiatric disorders).
Statistical Analysis
Child and parental characteristics were summarized for children with and without parental SMI. Children were followed up from birth to their fifth birthday, December 31, 2014, or date of death, whichever came first. Observation time was censored when a parent died. Because enrollment gaps were rare, we considered children and parents as having continuous NHI enrollment (eFigure 2 in the Supplement). Incidence rates of child outcomes were calculated by dividing the total number of injury events by follow-up time.
Log-linear models were used to estimate adjusted incidence rate ratios (IRRs) of outcomes in the exposed period compared with the unexposed period. These models were clustered on the child's mother19 to account for recurring outcomes within children and multiple children per mother and included an offset term of log of person-years. We used the generalized estimating equation with an independent working correlation structure instead of mixed-effect models to guard against biased regression estimates that could potentially arise because of time-dependent exposure and endogeneity between parental SMI and the number of future births,20,21 noting that the loss in estimation efficiency is relatively minor because of substantial sample size. Using robust SEs ensured valid inference even with a misspecified correlation structure or overdispersion.22
On the basis of exploratory analyses (eMethods 7 and eMethods 8 in the Supplement) and knowledge of the existing literature, we developed several models that included different covariates (eMethods 9 in the Supplement). Complete-case analyses were used because only 1.6% of children had missing data on covariates (eMethods 10 in the Supplement). We performed several sensitivity analyses, including exclusion of children with complex chronic conditions23 (measured by ICD-9-CM codes) (eMethods 11 in the Supplement), with any parent having multiple IDs or with any parent who died during study follow-up (eMethods 12 in the Supplement). All analyses were performed using SAS software, version 9.4 (SAS Institute Inc). Data analysis was performed from April 20, 2017, to September 24, 2019.
Results
Population Characteristics
The study cohort included 1 999 322 singletons (52.1% males without parental SMI and 52.2% males with parental SMI), 1 396 277 mothers, and 1 401 863 fathers. The children contributed 7 741 026.3 person-years of follow-up. Of the children, 90 917 (4.6%) were ever exposed to parental SMI: 36 389 (1.8%) with paternal SMI and 57 509 (2.9%) with maternal SMI. Of children with parental SMI, 57 074 (62.8%) were diagnosed with parental SMI before birth and 33 843 (37.2%) after birth. Children with parental SMI were more likely to be born prematurely or have low birth weight or complex chronic conditions (Table 2). Parents with SMI were more likely to have the following characteristics: unmarried; age younger than 25 years or older than 39 years; comorbid physical illness; occupation type of union members, farmers, and fishermen; or unemployed and low-income household. Parents and children in the parental SMI group were more likely than the comparison group to die during the study period (2.0% vs 0.8%).
Table 2. Characteristics of Children in the Study Cohort With and Without Parental SMI, 2004-2014 .
| Characteristic | Parental SMI, % | |
|---|---|---|
| Without (n = 1 908 405) | With (n = 90 917)a | |
| Children characteristics | ||
| 2004-2007 | 38.22 | 42.82 |
| 2008-2010 | 25.11 | 28.35 |
| 2011-2014 | 36.67 | 28.84 |
| Male | 52.13 | 52.21 |
| Birth weight <2500 g | 5.79 | 7.29 |
| Gestational age <37 wk | 6.85 | 8.84 |
| Birth order | ||
| 1 | 56.20 | 57.63 |
| 2 | 35.33 | 32.40 |
| ≥3 | 8.46 | 9.98 |
| Complex chronic conditions | 6.60 | 7.78 |
| Parent characteristics | ||
| Father’s age at birth, yb | ||
| <25 | 4.96 | 7.98 |
| 25-29 | 21.87 | 23.00 |
| 30-34 | 38.51 | 33.85 |
| 35-39 | 24.01 | 22.72 |
| 40-44 | 7.95 | 8.72 |
| ≥45 | 2.71 | 3.73 |
| Mother’s age at birth, y | ||
| <20 | 1.73 | 2.97 |
| 20-24 | 12.93 | 17.52 |
| 25-29 | 33.62 | 32.91 |
| 30-34 | 36.70 | 31.72 |
| 35-39 | 13.22 | 12.82 |
| ≥40 | 1.81 | 2.07 |
| Unmarried mother | 3.03 | 6.82 |
| Mother born outside Taiwan | 9.73 | 9.88 |
| Socioeconomic status | ||
| Urbanicity of residenceb | ||
| 1 (Highest urbanicity) | 20.27 | 19.68 |
| 2 | 32.21 | 34.16 |
| 3 | 23.68 | 22.08 |
| 4 | 14.35 | 14.50 |
| 5 | 1.65 | 1.77 |
| 6 | 3.45 | 3.67 |
| 7 | 4.39 | 4.15 |
| Family incomeb | ||
| High | 20.42 | 14.02 |
| Upper-middle | 20.31 | 15.75 |
| Middle | 21.46 | 20.37 |
| Lower-middle | 20.16 | 22.98 |
| Low | 17.65 | 26.88 |
| Father’s occupationb | ||
| Civil servants and teachers | 5.70 | 5.20 |
| Employees, employers, and professionals | 75.83 | 67.74 |
| Union members, farmers, and fishermenc | 5.48 | 6.63 |
| Unemployed and low-income household | 9.75 | 16.12 |
| Dependents | 3.23 | 4.32 |
| Mother’s occupationb | ||
| Civil servants and teachers | 5.51 | 4.31 |
| Employees, employers, and professionals | 63.42 | 53.01 |
| Union members, farmers, and fishermenc | 3.45 | 3.85 |
| Unemployed and low-income household | 6.50 | 13.13 |
| Dependents | 21.11 | 25.69 |
| Parental physical illness | ||
| Father’s Elixhauser index | ||
| 0 | 93.75 | 90.63 |
| 1 | 4.88 | 6.88 |
| >1 | 1.38 | 2.49 |
| Mother’s Elixhauser index | ||
| 0 | 95.70 | 93.93 |
| 1 | 3.85 | 5.19 |
| >1 | 0.45 | 0.88 |
| Death occurred before child’s age of 5 yd | ||
| Father’s death | 0.40 | 1.13 |
| Mother’s death | 0.11 | 0.43 |
| Child's death | 0.29 | 0.48 |
| Censored during the follow-up period | 0.79 | 2.01 |
Abbreviation: SMI, serious mental illness.
At least 1 parent with SMI in the period from 6 years before childbirth to 5 years after childbirth.
Data were complete for all variables except the following: father’s age (n = 1 [1 without parental SMI and 0 with parental SMI]), urbanicity of residence (n = 13 [13 without parental SMI and 0 with parental SMI]), family income (n = 4037 [3716 without parental SMI and 276 with parental SMI]), father’s occupation (n = 28 001 [26 656 without parental SMI and 1345 with parental SMI]), mother’s occupation (n = 8523 [8006 without parental SMI and 517 with parental SMI]), and days to the third well-child visit (n = 303 369 [290 622 without parental SMI and 12 747 with parental SMI]).
Union members refers to workers of the same occupation in the same city or county who organized and participated in an occupational union. Occupational unions are initially developed as insurance agents for (1) self-employed workers or workers who have no definite employer, (2) employees working in small businesses where there are fewer than 10 employees, and (3) small business owners. The occupation types for occupational unions vary, including farming, fishing, mining, transportation, tourism and catering industry, construction and engineering, news advertising industry, and culture and recreational industry.
Children born between 2010 and 2014 did not have 5-year follow-up data.
Injury
Within the study cohort, 1 082 064 children (54.1%) were injured, with 1 993 821 injury events generated from 3 340 554 inpatient or ambulatory visits. A greater proportion of children with (61.0%) than without (53.8%) parental SMI sustained injuries. Incidence rates of child injury–related outcomes were higher among children who were exposed to parental SMI (294.8 injury events per 1000 person-years) compared with children who were unexposed (256.1 injury events per 1000 person-years). Children from birth to 1 year of age and those aged 1 to 2 years had the lowest and highest incidence rates of injury events, respectively (Table 3). The unadjusted IRRs of injury events among children exposed to parental SMI (the exposed period) compared with children who were unexposed (the unexposed period) decreased from 1.21 (95% CI, 1.19-1.23) from birth to 1 year of age to 1.12 (95% CI, 1.10-1.14) at 4 to 5 years of age. When health care visits for injuries were counted instead of injury events, the estimates were similar (eTable 1 in the Supplement).
Table 3. Incidence of Childhood Injury and Appendicitis Among Children in the Study Cohort, Stratified by Child Age and Exposure to Parental SMI.
| Child age, y | Unexposed to SMI | Exposed to SMI | Rate difference (95% CI) | Unadjusted IRR (95% CI) | ||
|---|---|---|---|---|---|---|
| No. of events | IR (95% CI)a | No. of events | IR (95% CI)a | |||
| Injury events | ||||||
| 0 to <1 | 303 917 | 164 (164 to 165) | 11 651 | 198 (195 to 202) | 34 (30 to 38) | 1.21 (1.19 to 1.23) |
| 1 to <2 | 575 065 | 344 (343 to 344) | 23 878 | 393 (388 to 398) | 50 (44 to 55) | 1.14 (1.13 to 1.16) |
| 2 to <3 | 462 823 | 312 (311 to 313) | 21 734 | 356 (352 to 361) | 45 (40 to 49) | 1.14 (1.13 to 1.16) |
| 3 to <4 | 320 376 | 247 (246 to 248) | 16 822 | 281 (277 to 285) | 34 (29 to 38) | 1.14 (1.12 to 1.15) |
| 4 to <5 | 243 671 | 215 (214 to 215) | 13 884 | 239 (235 to 243) | 25 (21 to 29) | 1.12 (1.10 to 1.14) |
| Injury hospitalization | ||||||
| 0 to <1 | 5544 | 3.0 (2.9 to 3.1) | 284 | 4.8 (4.3 to 5.4) | 1.9 (1.3 to 2.4) | 1.62 (1.43 to 1.82) |
| 1 to <2 | 8751 | 5.2 (5.1 to 5.4) | 502 | 8.3 (7.6 to 9.1) | 3.1 (2.3 to 3.8) | 1.59 (1.45 to 1.74) |
| 2 to <3 | 5932 | 4.0 (3.9 to 4.1) | 357 | 5.9 (5.3 to 6.6) | 1.9 (1.3 to 2.5) | 1.47 (1.32 to 1.64) |
| 3 to <4 | 4231 | 3.3 (3.2 to 3.4) | 299 | 5.1 (4.5 to 5.7) | 1.8 (1.2 to 2.4) | 1.54 (1.37 to 1.74) |
| 4 to <5 | 3285 | 2.9 (2.8 to 3.0) | 207 | 3.6 (3.2 to 4.2) | 0.7 (0.2 to 1.2) | 1.25 (1.08 to 1.44) |
| Injury deathb | ||||||
| 0 to <1 | 392 | 21.2 (19.2 to 23.4) | 31 | 52.9 (37.2 to 75.2) | 31.7 (12.9 to 50.4) | 2.50 (1.73 to 3.60) |
| 1 to <2 | 149 | 8.9 (7.6 to 10.5) | 10 | 16.5 (8.9 to 30.8) | 7.6 (−2.7 to 18.0) | 1.86 (0.98 to 3.52) |
| 2 to <3 | 128 | 8.7 (7.3 to 10.3) | 11 | 18.2 (10.1 to 32.9) | 9.6 (−1.3 to 20.4) | 2.10 (1.14 to 3.90) |
| 3 to <4 | 69 | 5.3 (4.2 to 6.8) | 14 | 23.7 (14.0 to 40.0) | 18.3 (5.9 to 30.8) | 4.43 (2.49 to 7.87) |
| 4 to <5 | 57 | 5.0 (3.9 to 6.5) | 7 | 12.3 (5.9 to 25.8) | 7.2 (−2.0 to 16.4) | 2.43 (1.11 to 5.33) |
| Appendicitis (negative control) | ||||||
| 0 to <1 | 605 | 0.33 (0.30 to 0.35) | 19 | 0.32 (0.21 to 0.51) | 0.003 (−0.15 to 0.14) | 0.99 (0.63 to 1.56) |
| 1 to <2 | 876 | 0.52 (0.49 to 0.56) | 41 | 0.68 (0.50 to 0.92) | 0.15 (−0.06 to 0.36) | 1.29 (0.94 to 1.76) |
| 2 to <3 | 745 | 0.50 (0.47 to 0.54) | 22 | 0.36 (0.24 to 0.55) | −0.14 (−0.30 to 0.01) | 0.72 (0.47 to 1.10) |
| 3 to <4 | 681 | 0.53 (0.49 to 0.57) | 42 | 0.70 (0.52 to 0.95) | 0.18 (−0.04 to 0.39) | 1.34 (0.98 to 1.82) |
| 4 to <5 | 787 | 0.69 (0.65 to 0.74) | 44 | 0.76 (0.57 to 1.02) | 0.07 (−0.16 to 0.30) | 1.10 (0.81 to 1.48) |
Abbreviations: IR, incidence rate; IRR, incidence rate ratio; SMI, serious mental illness.
IRs are the number of injury events, injury hospitalization, and appendicitis per 1000 person-years. Injury deaths are per 100 000 person-years. Observation time was censored when the child died; otherwise, a person was assumed to have continuous enrollment.
The study cohort had 878 injury deaths, of which 824 were retrieved from death certificates and 176 from inpatient data. Ten child injury deaths occurred after the death of the child’s parent(s) and are not included in the table.
Exposure to SMI was associated with several specific injury types (eTable 2 in the Supplement), including intracranial injury (unadjusted IRRs, 1.21-1.50); burns (IRRs, 1.17-1.27); crush injury (IRRs, 1.17-1.37); open wounds (IRRs, 1.12-1.28); superficial injuries and contusion (IRRs, 1.11-1.18); poisoning (IRRs, 1.11-1.29); dislocations, strains, and sprains (IRRs, 1.01-1.19); and foreign body–related injuries (IRRs, 1.05-1.23). For other injury types, including skull fracture, nerve and spinal cord injury, fracture of neck and trunk, limb fractures, and vascular injury, the numbers of events were small, resulting in wide 95% CIs containing the null value.
The IRR of injury events before 5 years of age for the exposed period compared with the unexposed period was 1.14 (95% CI, 1.13-1.15) after adjusting for birth year, child sex and age, birth order, parental ages, mother born outside Taiwan, and urbanicity of residence (Table 4). The IRR did not change with adjustment for other covariates. The results of sensitivity analyses were similar to results of primary analyses (eTable 3 in the Supplement).
Table 4. Childhood Injury and Appendicitis Associated With Having a Parent With Serious Mental Illness (Model-Based Estimates)a.
| Child age, y | Adjusted incidence rate ratio (95% CI) | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Injury events | ||||
| 0-5 | 1.15 (1.14-1.16) | 1.14 (1.13-1.15) | 1.14 (1.13-1.14) | 1.14 (1.13-1.15) |
| 0 to <1 | 1.21 (1.18-1.23) | 1.20 (1.18-1.23) | 1.20 (1.17-1.22) | 1.20 (1.17-1.22) |
| 1 to <2 | 1.14 (1.13-1.16) | 1.14 (1.13-1.16) | 1.13 (1.12-1.15) | 1.13 (1.12-1.15) |
| 2 to <3 | 1.14 (1.13-1.16) | 1.14 (1.12-1.16) | 1.13 (1.12-1.15) | 1.13 (1.12-1.15) |
| 3 to <4 | 1.13 (1.12-1.15) | 1.13 (1.11-1.15) | 1.12 (1.11-1.14) | 1.12 (1.11-1.14) |
| 4 to <5 | 1.12 (1.10-1.14) | 1.11 (1.09-1.13) | 1.10 (1.08-1.13) | 1.10 (1.09-1.13) |
| Injury hospitalization | ||||
| 0-5 | 1.51 (1.43-1.59) | 1.49 (1.42-1.57) | 1.40 (1.33-1.48) | 1.40 (1.33-1.47) |
| 0 to <1 | 1.62 (1.44-1.83) | 1.61 (1.43-1.82) | 1.50 (1.33-1.69) | 1.49 (1.32-1.69) |
| 1 to <2 | 1.59 (1.45-1.74) | 1.57 (1.41-1.72) | 1.48 (1.35-1.62) | 1.47 (1.34-1.62) |
| 2 to <3 | 1.48 (1.32-1.64) | 1.45 (1.31-1.62) | 1.37 (1.23-1.53) | 1.37 (1.23-1.53) |
| 3 to <4 | 1.54 (1.37-1.74) | 1.52 (1.35-1.71) | 1.44 (1.28-1.62) | 1.43 (1.27-1.62) |
| 4 to <5 | 1.25 (1.08-1.44) | 1.23 (1.06-1.42) | 1.16 (1.00-1.35) | 1.16 (1.00-1.34) |
| Injury death | ||||
| 0-5 | 1.90 (1.44-2.49) | 1.82 (1.38-2.39) | 1.59 (1.20-2.11) | 1.58 (1.19-2.09) |
| 0 to <1 | 2.02 (1.35-3.03) | 1.96 (1.31-2.93) | 1.66 (1.09-2.53) | 1.64 (1.08-2.50) |
| 1 to <2 | 1.30 (0.61-2.78) | 1.25 (0.58-2.67) | 1.15 (0.54-2.47) | 1.14 (0.53-2.45) |
| 2 to <3 | 1.73 (0.88-3.39) | 1.64 (0.83-3.23) | 1.51 (0.77-2.97) | 1.49 (0.76-2.94) |
| 3 to <4 | 2.85 (1.42-5.72) | 2.70 (1.35-5.40) | 2.28 (1.10-4.75) | 2.26 (1.09-4.71) |
| 4 to <5 | 1.74 (0.70-4.34) | 1.64 (0.65-4.08) | 1.55 (0.62-3.88) | 1.54 (0.62-3.85) |
| Appendicitis (negative control) | ||||
| 0-5 | 1.10 (0.94-1.29) | 1.10 (0.94-1.28) | 1.09 (0.93-1.27) | 1.08 (0.92-1.27) |
Model 1 was adjusted for birth year and child sex. Child age was also adjusted in estimating the incidence rate ratio for ages 0 to 5 years for injury events, injury hospitalization, and injury death. Model 2 was further adjusted for birth order, parental ages, mother born outside Taiwan, and urbanicity of residence. Model 3 was further adjusted for unmarried mother, family income, parental occupations, and Elixhauser indexes. Model 4 was further adjusted for child’s low birth weight and preterm birth.
Approximately 1.5% of injury events resulted in hospitalization. The IRs of injury hospitalization were highest at 1 to 2 years of age and lowest at 4 to 5 years of age (Table 3). The unadjusted IRR for injury hospitalization decreased from 1.62 (95% CI, 1.43-1.82) at birth to 1 year of age to 1.25 (95% CI, 1.08-1.44) at 4 to 5 years of age. The study cohort had 878 injury deaths. The incidence rates of injury death were highest at birth to 1 year of age and lowest at 4 to 5 years of age (Table 3). However, the unadjusted IRR for injury death did not decrease with child age. For the exposed period, the adjusted IRRs were 1.49 (95% CI, 1.42-1.57) for injury hospitalization and 1.82 (95% CI, 1.38-2.39) for injury-related death (Table 4). eTable 4 and eTable 5 in the Supplement list external causes of injury hospitalization and death.
Appendicitis and Health Care–Seeking Behavior
The study cohort included 3862 children with appendicitis (0.19%). The adjusted IRR of appendicitis for the exposed period was 1.10 (95% CI, 0.94-1.28) (Table 4). Among the 1 126 253 children born before 2010, the mean (SD) numbers of prenatal and well-child visits were lower among children with parental SMI (8.09 [2.50] prenatal visits and 5.70 [2.24] well-child visits) compared with unaffected children (8.17 [2.47] prenatal visits and 5.80 [2.21] well-child visits) (eTable 6 in the Supplement). Correlations (Pearson r) between the number of child injury events and health care visits were 0.04 (95% CI, 0.04-0.04) in the children without parental SMI and 0.03 (95% CI, 0.02-0.07) in the children with parental SMI for prenatal visits and 0.08 (95% CI, 0.08-0.08) in the children without parental SMI and 0.08 (95% CI, 0.07-0.09) for the children with parental SMI for well-child visits (eTable 6 in the Supplement).
Discussion
In this cohort study, a greater proportion of children with (61.0%) than without (53.8%) parental SMI sustained injuries before the age of 5 years. Children of parents with SMI had 14% higher rates of injury events, 49% higher rates of hospitalization, and 82% higher rates of death.
Previous studies9,24 have reported associations between maternal depression and specific types of child injury. Using UK health databases, Baker et al24 reported that maternal depressive episodes were associated with increased risk of child poisoning, burns, and fractures before 5 years of age. Using another UK primary care database, Orton et al9 reported maternal perinatal depression to be a risk factor for first occurrences of thermal injury and poisoning. The magnitude of our associations between parental SMI and specific injury types were lower (eTable 2 in the Supplement) than in these studies,9,24 possibly because we excluded children without complete parent data who were more likely to have low socioeconomic status.25 An alternative explanation is that the study sample was more inclusive of the full socioeconomic spectrum within the general population because of nearly universal health insurance coverage. Finally, we used a different study design than Orton et al,9 modeling child injuries as potentially recurring events vs first events. The latter approach would generate different results if children with particular characteristics were more susceptible to recurrent injuries.26 In addition, the odds ratio estimates9 would be high compared with risk ratio estimates given the high rate of occurrence of childhood injuries.27
Several studies28,29 indicate an association between parental psychiatric disorders and child mortality. In Taiwan between 2001 and 2003, children younger than 5 years with parental SMI had a 2.4-times higher risk of mortality.28 In Denmark, children of parents with a psychiatric inpatient admission had a 1.6-times higher risk of mortality between 1 and 4 years of age. 29 Our excess risk estimate for injury death was similar to those in these previous studies.28,29
We observed that IRRs of injury events and injury hospitalization among children with parental SMI decreased as children aged. Providing constant care for a newborn is demanding and stressful, which may exacerbate symptoms of SMI and hinder parents’ capacity to stay vigilant.30 Schwebel and Brezausek10 found that severe maternal depression was associated with child injury risk from birth to 3 years of age but not at older ages. Fathers' depression is more strongly associated with challenges in parenting younger rather than older children.31 As children mature, they require less intensive supervision. However, our IRR estimates of injury death did not decrease with child age. The causes of injury death were less likely to implicate children’s mobility status. Nearly 70% of injury deaths in children younger than 5 years compared with 23.4% of injury hospitalizations were caused by submersion, suffocation, and foreign body and transport incidents.
The risk estimates for child injury varied depending on the injury-related outcome examined. For injury events, parental SMI was associated with a 14% greater risk, whereas the excess risk was 49% for injury hospitalization and 82% for injury-related death. Symptoms and functional impairment, particularly in the parenting role, may influence the ability of parents with SMI to evaluate their child’s injury severity. The children may be exposed to greater risk of severe injury. Several covariates also exhibited differential risk for injury events and hospitalization (eMethods 7 and eMethods 8 in the Supplement). Risk of injury hospitalization was greater among children with markers of disadvantage, including parental physical illness, living in rural areas, lower family income, lower parental occupational class, and unmarried mother. Parents with SMI tend to have lower socioeconomic status, and parents with low socioeconomic status may be constrained by poverty and work demands and thus use less outpatient and more inpatient care for the same injury severity than parents with high socioeconomic status.32 Alternatively, children with parental SMI could be admitted to the hospital for less serious conditions because of the physician’s judgment of the parent’s ability to care for the child. If this is true, the excess incidence of injury hospitalization for exposed children may partially reflect differences in service utilization patterns. However, this would not explain why the excess risk of injury death was higher than that of injury hospitalization.
Given that children with parental SMI had increased injury risk, effective management of parental SMI may have beneficial effects for child health.33 Evidence suggests that home visiting programs are associated with improved maternal depression symptoms33 and reduced child injury.34 Reducing stigma toward mental health treatment, enhancing parenting skills, and enacting home safety interventions for parents with SMI may contribute to a reduction in injury risk for their children.35,36
Strengths and Limitations
This study had several strengths. Selection bias was minimized because study databases had high population coverage, which enabled us to capture parental SMI and child injury across demographic groups and geographic and treatment settings within Taiwan. Use of data recorded in real time decreased the possibility of self-reporting bias.
This study had several limitations. Our study cohort included only singletons; results may not be generalizable to nonsingletons. Approximately half of children born to unmarried mothers, who were more likely to have SMI, were also excluded. Mothers with SMI who are single25 or have multiple births encounter more parenting challenges. Therefore, our IRR estimates could be conservative.
Parental SMI and child injury were based on ICD-9 codes. Studies suggest that the agreement between SMI diagnoses and symptoms or history are high,37,38,39 with a positive predictive value ranging from 81% to 95%.37,38,40 We attempted to improve SMI accuracy by prioritizing diagnoses made by psychiatrists (94.1% of parental SMIs were so determined). As for injury, a Canadian study41 using diagnoses in an injury surveillance system as the criterion standard demonstrated that ICD-9 codes of claims data for child head injuries had high specificity and lower sensitivity.
The Taiwan health care system does not conduct routine mental health screening. Mental illnesses typically manifest years before people seek treatment.42 Accordingly, timing of SMI onset was subject to misclassification, leading to an overestimated risk of childhood injury in the unexposed group. The NHIRD does not include data from private health care practitioners. However, since the implementation of the NHI, most psychiatrists have joined this program. In 2019, a total of 499 of 515 clinics or hospitals (96.9%) providing psychiatric service contracted with the NHI. Citizens who use self-pay psychotherapy often obtain medications from NHI practitioners and are captured within the NHIRD. Nonetheless, in general, using the NHIRD underestimates the occurrence of mental disorders in the general population.43 If the underdiagnosis of parental SMI is not related to child outcomes, it would bias associations toward the null.44 If parents with SMI sought more medical care for themselves and their children, this would artificially inflate risk estimates. However, our results were similar whether counting injuries as events or clinic visits, and children with and without parental SMI had similar preventive health care utilization. Furthermore, child appendicitis, as a negative control, was not associated with parental SMI in our study.
The NHIRD does not reliably capture parent alcohol or drug use in parent medical claims or claims for child injuries. Therefore, we were unable to examine parent substance use disorder as a likely important contributor to the excess risk of injuries among children with parental SMI. We were also unable to measure protective factors, such as social support45,46 or receipt of effective treatment, that might attenuate the associations between parent SMI and child injury. In addition, the databases lacked several key variables, such as symptom severity, parents’ educational level,47 and domestic violence.48
Conclusions
In this study, children younger than 5 years with parental SMI had increased risk of injury, especially serious injury. These findings emphasize the importance of interventions for parents with SMI. Future studies evaluating differences in child injury risk by specific type of parental SMI may help target interventions. Mixed-methods studies that elucidate caregiving challenges and needs among parents with SMI may help inform service planning for affected families.
eMethods 1. Deterministic Linkage Methods for Forming Complete Child-Father-Mother Triads Registry of Beneficiaries and Birth Certificate
eMethods 2. Construction of Study Cohort
eMethods 3. Characteristics of Children of the Study Cohort and Children Excluded From the Study Cohort, 2004-2014
eMethods 4. Retrieving Child’s Health Records Under the Parents’ Coverage
eMethods 5. Retrieval of Prenatal and Well-Child Visits
eMethods 6. Retrieval of Covariates
eMethods 7. Associations Between Childhood Injury Events in the First Five Years of Life and Covariates Among Children in the Study Cohort
eMethods 8. Associations Between Injury Hospitalization in the First Five Years of Life and Covariates Among Children in the Study Cohort
eMethods 9. Variables Used for the Adjustment in All Models
eMethods 10. Missing Data of Child’s Birthweight, Gestational Age and Parental Demographics Among Children in the Study Cohort
eMethods 11. ICD-9-CM Diagnostic Codes of Child Complex Chronic Conditions
eMethods 12. Number of Children and Any Child Injury Event Excluded in Sensitivity Analyses
eFigure 1. Interval Between Two Clinical Visits (in Week) by Injury Type
eFigure 2. Numbers and Days of Enrollment Gaps for Children and Parents in the Study Cohort
eTable 1. Incidence Rates of Injury Healthcare Visits Among Children in the Study Cohort, Stratified by Child Age and by Exposure to Parental Serious Mental Illness
eTable 2. Incidence Rates of Injury Events Among Children in the Study Cohort, Stratified by Child Age and by Exposure to Parental Serious Mental Illness for Each Injury Type
eTable 3. Sensitivity Analyses of Associations Between Parental Serious Mental Illness and Any Childhood Injury Event
eTable 4. ICD-9 E Codes for Individual Hospitalization Associated With Injury ICD-9 Diagnostic Codes
Table 5. ICD-9 external causes of injury deaths
eTable 6. Utilization of Preventive Health Services Among Children in the Study Cohort Born in 2004-2009
eReferences
References
- 1.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575-1586. doi: 10.1016/S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 3.Sohr-Preston SL, Scaramella LV. Implications of timing of maternal depressive symptoms for early cognitive and language development. Clin Child Fam Psychol Rev. 2006;9(1):65-83. doi: 10.1007/s10567-006-0004-2 [DOI] [PubMed] [Google Scholar]
- 4.Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800-1819. doi: 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- 5.Nilsson E, Hultman CM, Cnattingius S, Olausson PO, Björk C, Lichtenstein P. Schizophrenia and offspring’s risk for adverse pregnancy outcomes and infant death. Br J Psychiatry. 2008;193(4):311-315. doi: 10.1192/bjp.bp.107.045146 [DOI] [PubMed] [Google Scholar]
- 6.Lee HC, Lin HC. Maternal bipolar disorder increased low birthweight and preterm births: a nationwide population-based study. J Affect Disord. 2010;121(1-2):100-105. doi: 10.1016/j.jad.2009.05.019 [DOI] [PubMed] [Google Scholar]
- 7.Peden M, Oyegbite K, Ozanne-Smith J, et al. World Report on Child Injury Prevention. World Health Organization; 2008. [PubMed] [Google Scholar]
- 8.Phelan K, Khoury J, Atherton H, Kahn RS. Maternal depression, child behavior, and injury. Inj Prev. 2007;13(6):403-408. doi: 10.1136/ip.2006.014571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orton E, Kendrick D, West J, Tata LJ. Independent risk factors for injury in pre-school children: three population-based nested case-control studies using routine primary care data. PLoS One. 2012;7(4):e35193. doi: 10.1371/journal.pone.0035193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwebel DC, Brezausek CM. Chronic maternal depression and children’s injury risk. J Pediatr Psychol. 2008;33(10):1108-1116. doi: 10.1093/jpepsy/jsn046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myhre MC, Thoresen S, Grøgaard JB, Dyb G. Familial factors and child characteristics as predictors of injuries in toddlers: a prospective cohort study. BMJ Open. 2012;2(2):e000740. doi: 10.1136/bmjopen-2011-000740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng T-M. Reflections on the 20th anniversary of Taiwan’s single-payer National Health Insurance System. Health Aff (Millwood). 2015;34(3):502-510. doi: 10.1377/hlthaff.2014.1332 [DOI] [PubMed] [Google Scholar]
- 13.National Health Insurance Administration, Ministy of Health and Welfare Statistics and surveys. Accessed October 14, 2017. https://www.nhi.gov.tw/english/Content_List.aspx?n=616B97F8DF2C3614&topn=616B97F8DF2C3614
- 14.Spady DW, Saunders DL, Schopflocher DP, Svenson LW. Patterns of injury in children: a population-based approach. Pediatrics. 2004;113(3, pt 1):522-529. doi: 10.1542/peds.113.3.522 [DOI] [PubMed] [Google Scholar]
- 15.Lestina DC, Miller TR, Smith GS. Creating injury episodes using medical claims data. J Trauma. 1998;45(3):565-569. doi: 10.1097/00005373-199809000-00026 [DOI] [PubMed] [Google Scholar]
- 16.Pickett TA. The challenges of accurately estimating time of long bone injury in children. J Forensic Leg Med. 2015;33:105-110. doi: 10.1016/j.jflm.2015.04.012 [DOI] [PubMed] [Google Scholar]
- 17.Prosser I, Lawson Z, Evans A, et al. A timetable for the radiologic features of fracture healing in young children. AJR Am J Roentgenol. 2012;198(5):1014-1020. doi: 10.2214/AJR.11.6734 [DOI] [PubMed] [Google Scholar]
- 18.Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology. 2010;21(3):383-388. doi: 10.1097/EDE.0b013e3181d61eeb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miglioretti DL, Heagerty PJ. Marginal modeling of nonnested multilevel data using standard software. Am J Epidemiol. 2007;165(4):453-463. doi: 10.1093/aje/kwk020 [DOI] [PubMed] [Google Scholar]
- 20.Sullivan Pepe M, Anderson GL. A cautionary note on inference for marginal regression models with longitudinal data and general correlated response data. Commun Stat Simul Comput. 1994;23(4):939-951. doi: 10.1080/03610919408813210 [DOI] [Google Scholar]
- 21.French B, Heagerty PJ. Marginal mark regression analysis of recurrent marked point process data. Biometrics. 2009;65(2):415-422. doi: 10.1111/j.1541-0420.2008.01076.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diggle P, Heagerty P, Liang K-Y, Zeger S. Analysis of Longitudinal Data. 2nd ed. Oxford University Press; 2013. [Google Scholar]
- 23.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington state, 1980-1997. Pediatrics. 2000;106(1, pt 2):205-209. doi: 10.1542/peds.106.1.S1.205 [DOI] [PubMed] [Google Scholar]
- 24.Baker R, Kendrick D, Tata LJ, Orton E. Association between maternal depression and anxiety episodes and rates of childhood injuries: a cohort study from England. Inj Prev. 2017;23(6):396-402. doi: 10.1136/injuryprev-2016-042294 [DOI] [PubMed] [Google Scholar]
- 25.Weitoft GR, Hjern A, Haglund B, Rosén M. Mortality, severe morbidity, and injury in children living with single parents in Sweden: a population-based study. Lancet. 2003;361(9354):289-295. doi: 10.1016/S0140-6736(03)12324-0 [DOI] [PubMed] [Google Scholar]
- 26.Guo Z, Gill TM, Allore HG. Modeling repeated time-to-event health conditions with discontinuous risk intervals: an example of a longitudinal study of functional disability among older persons. Methods Inf Med. 2008;47(2):107-116. doi: 10.3414/ME0478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davies HT, Crombie IK, Tavakoli M. When can odds ratios mislead? BMJ. 1998;316(7136):989-991. doi: 10.1136/bmj.316.7136.989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Y-H, Chiou H-Y, Tang C-H, Lin H-C. Risk of death by unnatural causes during early childhood in offspring of parents with mental illness. Am J Psychiatry. 2010;167(2):198-205. doi: 10.1176/appi.ajp.2009.09070979 [DOI] [PubMed] [Google Scholar]
- 29.Webb RT, Abel KM, Pickles AR, Appleby L, King-Hele SA, Mortensen PB. Mortality risk among offspring of psychiatric inpatients: a population-based follow-up to early adulthood. Am J Psychiatry. 2006;163(12):2170-2177. doi: 10.1176/ajp.2006.163.12.2170 [DOI] [PubMed] [Google Scholar]
- 30.Leach LS, Olesen SC, Butterworth P, Poyser C. New fatherhood and psychological distress: a longitudinal study of Australian men. Am J Epidemiol. 2014;180(6):582-589. doi: 10.1093/aje/kwu177 [DOI] [PubMed] [Google Scholar]
- 31.Wilson S, Durbin CE. Effects of paternal depression on fathers’ parenting behaviors: a meta-analytic review. Clin Psychol Rev. 2010;30(2):167-180. doi: 10.1016/j.cpr.2009.10.007 [DOI] [PubMed] [Google Scholar]
- 32.Kangovi S, Barg FK, Carter T, Long JA, Shannon R, Grande D. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood). 2013;32(7):1196-1203. doi: 10.1377/hlthaff.2012.0825 [DOI] [PubMed] [Google Scholar]
- 33.Leis JA, Mendelson T, Tandon SD, Perry DF. A systematic review of home-based interventions to prevent and treat postpartum depression. Arch Womens Ment Health. 2009;12(1):3-13. doi: 10.1007/s00737-008-0039-0 [DOI] [PubMed] [Google Scholar]
- 34.Kitzman H, Olds DL, Henderson CR Jr, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing: a randomized controlled trial. JAMA. 1997;278(8):644-652. doi: 10.1001/jama.1997.03550080054039 [DOI] [PubMed] [Google Scholar]
- 35.Engle PL. Maternal mental health: program and policy implications. Am J Clin Nutr. 2009;89(3):963S-966S. doi: 10.3945/ajcn.2008.26692G [DOI] [PubMed] [Google Scholar]
- 36.Kendrick D, Young B, Mason-Jones AJ, et al. Home safety education and provision of safety equipment for injury prevention [review]. Evid Based Child Health. 2013;8(3):761-939. doi: 10.1002/ebch.1911 [DOI] [PubMed] [Google Scholar]
- 37.Dalman Ch, Broms J, Cullberg J, Allebeck P. Young cases of schizophrenia identified in a national inpatient register: are the diagnoses valid? Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):527-531. doi: 10.1007/s00127-002-0582-3 [DOI] [PubMed] [Google Scholar]
- 38.Sellgren C, Landén M, Lichtenstein P, Hultman CM, Långström N. Validity of bipolar disorder hospital discharge diagnoses: file review and multiple register linkage in Sweden. Acta Psychiatr Scand. 2011;124(6):447-453. doi: 10.1111/j.1600-0447.2011.01747.x [DOI] [PubMed] [Google Scholar]
- 39.Kessing L. Validity of diagnoses and other clinical register data in patients with affective disorder. Eur Psychiatry. 1998;13(8):392-398. doi: 10.1016/S0924-9338(99)80685-3 [DOI] [PubMed] [Google Scholar]
- 40.Walkup JT, Boyer CA, Kellermann SL. Reliability of Medicaid claims files for use in psychiatric diagnoses and service delivery. Adm Policy Ment Health. 2000;27(3):129-139. doi: 10.1023/A:1021308007343 [DOI] [PubMed] [Google Scholar]
- 41.Kostylova A, Swaine B, Feldman D. Concordance between childhood injury diagnoses from two sources: an injury surveillance system and a physician billing claims database. Inj Prev. 2005;11(3):186-190. doi: 10.1136/ip.2004.006585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang PS, Angermeyer M, Borges G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):177-185. https://www.ncbi.nlm.nih.gov/pubmed/18188443. [PMC free article] [PubMed] [Google Scholar]
- 43.Chien I-C, Chou Y-J, Lin C-H, Bih S-H, Chou P. Prevalence of psychiatric disorders among National Health Insurance enrollees in Taiwan. Psychiatr Serv. 2004;55(6):691-697. doi: 10.1176/appi.ps.55.6.691 [DOI] [PubMed] [Google Scholar]
- 44.Sorensen HT, Sabroe S, Olsen J. A framework for evaluation of secondary data sources for epidemiological research. Int J Epidemiol. 1996;25(2):435-442. doi: 10.1093/ije/25.2.435 [DOI] [PubMed] [Google Scholar]
- 45.Paschetta E, Berrisford G, Coccia F, et al. Perinatal psychiatric disorders: an overview. Am J Obstet Gynecol. 2014;210(6):501-509.e6. doi: 10.1016/j.ajog.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 46.Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA. 2010;303(19):1961-1969. doi: 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- 47.Valdimarsdóttir U, Hultman CM, Harlow B, Cnattingius S, Sparén P. Psychotic illness in first-time mothers with no previous psychiatric hospitalizations: a population-based study. PLoS Med. 2009;6(2):e13. doi: 10.1371/journal.pmed.1000013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805-815. doi: 10.1001/archpsyc.65.7.805 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Deterministic Linkage Methods for Forming Complete Child-Father-Mother Triads Registry of Beneficiaries and Birth Certificate
eMethods 2. Construction of Study Cohort
eMethods 3. Characteristics of Children of the Study Cohort and Children Excluded From the Study Cohort, 2004-2014
eMethods 4. Retrieving Child’s Health Records Under the Parents’ Coverage
eMethods 5. Retrieval of Prenatal and Well-Child Visits
eMethods 6. Retrieval of Covariates
eMethods 7. Associations Between Childhood Injury Events in the First Five Years of Life and Covariates Among Children in the Study Cohort
eMethods 8. Associations Between Injury Hospitalization in the First Five Years of Life and Covariates Among Children in the Study Cohort
eMethods 9. Variables Used for the Adjustment in All Models
eMethods 10. Missing Data of Child’s Birthweight, Gestational Age and Parental Demographics Among Children in the Study Cohort
eMethods 11. ICD-9-CM Diagnostic Codes of Child Complex Chronic Conditions
eMethods 12. Number of Children and Any Child Injury Event Excluded in Sensitivity Analyses
eFigure 1. Interval Between Two Clinical Visits (in Week) by Injury Type
eFigure 2. Numbers and Days of Enrollment Gaps for Children and Parents in the Study Cohort
eTable 1. Incidence Rates of Injury Healthcare Visits Among Children in the Study Cohort, Stratified by Child Age and by Exposure to Parental Serious Mental Illness
eTable 2. Incidence Rates of Injury Events Among Children in the Study Cohort, Stratified by Child Age and by Exposure to Parental Serious Mental Illness for Each Injury Type
eTable 3. Sensitivity Analyses of Associations Between Parental Serious Mental Illness and Any Childhood Injury Event
eTable 4. ICD-9 E Codes for Individual Hospitalization Associated With Injury ICD-9 Diagnostic Codes
Table 5. ICD-9 external causes of injury deaths
eTable 6. Utilization of Preventive Health Services Among Children in the Study Cohort Born in 2004-2009
eReferences