Abstract
Introduction
Maternal health services are effective in reducing the morbidity and mortality associated with pregnancy and childbirth. We conducted a systematic review on costs of maternal health services in low-income and middle-income countries from the provider’s perspective.
Methods
We searched multiple peer-reviewed databases (including African Journal Online, CINAHL Plus, EconLit, Popline, PubMed, Scopus and Web of Science) and grey literature for relevant articles published from year 2000. Articles meeting our inclusion criteria were selected with quality assessment done using relevant cost-focused criteria of the Consolidated Health Economic Evaluation Reporting Standards checklist. For comparability, disaggregated costs data were inflated to 2019 US$ equivalents. Costs and cost drivers were systematically compared. Where heterogeneity was observed, narrative synthesis was used to summarise findings.
Results
Twenty-two studies were included, with most studies costing vaginal and/or caesarean delivery (11 studies), antenatal care (ANC) (9) and postabortion care (PAC) (8). Postnatal care (PNC) has been least costed (2). Studies used different methods for data collection and analysis. Quality of peer-reviewed studies was assessed average to high while all grey literature studies were assessed as low quality. Following inflation, estimated provision cost per service varied (ANC (US$7.24–US$31.42); vaginal delivery (US$14.32–US$278.22); caesarean delivery (US$72.11–US$378.940; PAC (US$97.09–US$1299.21); family planning (FP) (US$0.82–US$5.27); PNC (US$5.04)). These ranges could be explained by intercountry variations, variations in provider type (public/private), facility type (primary/secondary) and care complexity (simple/complicated). Personnel cost was mostly reported as the major driver for provision of ANC, skilled birth attendance and FP. Economies of scale in service provision were reported.
Conclusion
There is a cost savings case for task-shifting and encouraging women to use lower level facilities for uncomplicated services. Going forward, consensus regarding cost component definitions and methodologies for costing maternal health services will significantly help to improve the usefulness of cost analyses in supporting policymaking towards achieving Universal Health Coverage.
Keywords: health economics, maternal health, systematic review
Key questions.
What is already known?
Following a systematic search, we found no review in the peer-reviewed literature and the only review we found was published in the grey literature and included only studies published before year 2000.
The available pre-2000 review is outdated as guidance on several service packages and methods of financing healthcare have changed ever since.
What are the new findings?
To the best of our knowledge, this review covering 17 low-income and middle-income countries provides the most up-to-date overview of cost of maternal health service provision in these settings from 2000 until.
Personnel cost was mostly reported as the major cost driver for antenatal care, intrapartum care by skilled health personnel and for family planning.
Economies of scale were also observed, with lower cost per service observed when more women received care.
What do the new findings imply?
The available evidence points to potential cost savings case for task shifting as a policy for delivery of the most critical maternal health services and to the need to encourage women to use lower level facilities for non-complicated services in low-income and middle-income countries.
Findings from this study provide insights for developing future global guidelines for costing maternal health services in low-income and middle-income countries.
Introduction
Reducing the morbidity and mortality associated with pregnancy and childbirth for mothers and newborns remains a key priority for the health and development agenda in the post-2015 era of the Sustainable Development Goals (SDGs).1 Following progress made in reducing global maternal mortality ratio (MMR) by 44% during the preceding Millennium Development Goal (MDG) era, baseline figures at the start of the SDGs era still showed that >300 000 women die annually due to pregnancy and childbirth complications, with the deaths occurring almost entirely in low-income and middle-income countries (LMICs).2 The consensus target for the next decade is to reduce MMR to 70 per 100 000 live births and newborn mortality ratio to below 12 per 1000 live births, globally.1
To achieve these targets, the main strategy has been centred on ensuring access to quality evidence-based maternal health services along the continuum of care.3 Indeed, the effectiveness of these services, which include antenatal care (ANC), skilled birth attendance during spontaneous vaginal delivery, Emergency Obstetric Care, postnatal care (PNC), postabortion care (PAC) and family planning (FP), in reducing these maternal and newborn morbidities and mortalities has been reported in the literature.4–6 However, in addition to considerations on effectiveness in decision-making to provide these services, planners and policy makers need evidence on the cost of their provision. Among experts, the preference for costing health services is to use robust country-specific data collected from representative populations for costing health services,7 more so for maternal health services.8 Such cost data which will typically include component costs for personnel, medicines and supplies, laboratory tests, equipment, capital and overheads will be useful in complementing the already established effectiveness data for cost-effectiveness analyses and will better inform priority setting and resource allocation for maternal health service provision. A systematic literature search revealed only one previous review on this topic. This was published as a book chapter in year 2000 and it included papers published mostly in the 1990s.8 The objective of our review, therefore, was to systematically assess and summarise recent evidence on costs of providing maternal health services in LMICs.
Methods
Study design
In designing methods used for this review, we leveraged best practices for conducting systematic reviews on economic evaluations from the Centre for Reviews and Dissemination,9 the Task Force on Community Preventive Services9 and the Joanna-Brigg’s Institute.10 A protocol-guided systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses approach (online supplementary table S1 in file 1).11
bmjgh-2020-002371supp001.pdf (756.6KB, pdf)
Search strategy
The protocol used in this review is registered on PROSPERO (CRD42018114124) and is published elsewhere.12 The detailed search strategy used for both peer-review and grey literature sources is appended as an online supplementary table S2. In summary, from 30 June 2019 to 30 September 2019, we searched several databases including the African Journal Online, CINAHL Plus, EconLit, Embase, Popline (until 1 September 2019, when the database was retired), PubMed, Scopus and Web of Science. As a general principle, in searching the various databases, search terms were combined using Boolean operators ‘OR’ within categories and ‘AND’ between the three categories of terms (words and phrases) that captured the interventions of interest (ie, maternal health services), their costs and the setting of interest (LMICs). For databases where it was not possible to specify the setting of interest (African Journal Online, Popline and PubMed), we made the call on relevance of retrieved articles during the title and abstract screening. The combination of these search terms guarantees an optimal search strategy for retrieving cost and economic studies relevant to maternal health services,13 and was developed with support from our institutional librarian. Through the entire process of its development, we used the checklist by McGowan et al to assess the adequacy of our electronic search strategy.14
Following guidance for searching and synthesising grey literature in public health,15 we systematically searched websites of organisations who report or have interest in costing of health services. The websites searched were selected based on our experience and that of other experts on the subject matter. Specifically, we searched websites of Averting Maternal Death and Disability, FP2020, Guttmacher Institute, LMIC Ministries of Health, Management Sciences for Health, Maternal Health Task Force, Population Council, United Nations Fund for Population and WHO for relevant reports (including costing analyses, white papers, working papers and internal documentations) focused on cost of providing maternal health services. The grey literature search was conducted during the same period that we searched the peer-reviewed databases.
In addition to the automated search for peer-reviewed and grey literature, we also manually searched for other potentially relevant articles by reviewing the reference lists of retrieved articles. If a study was found in the grey literature, which was later published in the peer-reviewed literature, the peer-reviewed version was selected for the purposes of our review.
For both peer-review and grey literature, we limited the search to studies published between January 2000 and September 2019 (the end date for our search), and written in English and French languages, as these were the languages comprehensible by the review team. The search was conducted independently by three authors (AB-T, FIA and OB-T), with search results compared for completeness. After duplicates were removed, two authors (AB-T and FIA) independently screened titles and abstracts of the retrieved records for relevance and eligibility, with the senior author (CAA) serving as arbitrator in case of discrepancies. If titles or abstracts were deemed relevant, full text were reviewed by AB-T and FIA. Full texts were subsequently stored in shared folders within an automated reference manager, Mendeley Desktop V.1.19.4 (Elsevier, Amsterdam, The Netherlands).
Inclusion and exclusion criteria
To be included, articles had to present cost data specific for any of the maternal health services collected from one or multiple LMIC(s) (as defined by the World Bank),16 from the provider’s perspective. Such cost data are typically reported in full (cost minimisation, cost-effectiveness, cost-utility and cost-benefit analyses) and partial (cost analysis, cost-description studies and cost-outcome studies) economic evaluation studies.17 As such, full or partial economic evaluations on cost of providing maternal health services in LMICs published between January 2000 and September 2019, with retrievable full texts were included for review.
However, articles were excluded if costing was done based on models/projections or if they presented costs that could not be split by individual service (ANC, skilled birth attendance, PNC, PAC, FP). We also excluded commentaries and editorials. In addition, articles that presented cost categories (eg, US$0–US$500), as opposed to actual costs as well as studies published year 2000 onwards using cost data preceding year 2000 were excluded. This decision was made in consideration of the marked difference in health financing approach after year 2000.18 19 Finally, we excluded studies that focused on specialist services such as ANC for HIV-positive mothers as they would typically include additional tests and medicines targeted at prevention of mother-to-child transmission.
Data extraction
Guidance on approach and content for data extraction were sought from previous reviews and expert opinion.8 20 In our review, we used a predeveloped Microsoft Excel (Microsoft, Redmond, Washington, USA) sheet to extract data. We extracted data on country of study, scale of study, site of study, country of organisation conducting study, study participants, perspective of costing, study design, costing of maternal health services costed, costing method used, time frame, facility type, facility ownership, number of facilities, component of cost, year of costs data, currency, stated exchange rate used for analysis and discount rate) as well as findings reported including total service cost per client visit and/or other summary measures of cost such as median and mean.
When specific data were missing from retrieved articles or not publicly available, we made attempts to contact the study authors via portals such as ResearchGate and LinkedIn. Data extraction was conducted independently by two coauthors (AB-T and FIA) and then checked for accuracy by two others (IOA and OB-T).
Quality assessment of included studies
The 24-item Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist has been widely used for assessing the quality of reporting of full economic evaluations.21 However, as partial economic evaluation studies which capture purely cost data were included in this review,17 only the cost-focused criteria in the CHEERS checklist were applied in this review. This choice was based on quality assessments used in similar reviews.22–24
Details of the quality criteria assessed have been published elsewhere.12 In summary, for each item, a score of 1 was awarded if the criterion is fully met; 0.5, if partially met; 0, if not met or if only minimal information was provided and NA if not applicable. The total score achieved across all eight criteria was subsequently summed-up and converted to percentages. As has been done in other similar reviews,22–24 studies with 75% or more criteria fully met were classified as high quality, 50%–74% as average quality and below 50% as poor quality. Each included study was independently assessed by two coauthors (AB-T and FIA).
Data analysis and synthesis
Using a subgroup analysis, the different cost components associated with each service were identified. Articles that included only lump total service costs or those that had total service costs which could not be disaggregated into service cost components were analysed separately.
For those that presented disaggregated cost of service provision (cost per service), where possible, opportunity costs, if included, were excluded before totalling the direct financial cost of each service, which was the focus of our analysis. We also excluded cost that were deemed additional to actual service delivery such as training, scholarship funds for health workers and transport funds for ambulatory services from our analysis. For these, leveraging guidance on adjustments for inflation and currency changes for health economic studies,25 we used a mixed approach to inflate disaggregated component costs, with a general agreement that medicines, supplies and equipment are tradable costs while personnel, capital and overheads are non-tradable. We inflated component costs to 2019 values using the Gross Domestic Product (GDP) implicit price deflator for the year of costing as stated in the study and our selected base year (2019) using estimates derived from the World Economic Outlook database,26 presenting these component costs in US$.25 Based on these adjusted US$ equivalents, total cost per service estimates were recalculated by summing up the component costs. We then compared our derived adjusted costs across studies, across facility type (health centre/clinic/hospital), provider type (public/mission/private) and complexity of care (simple/complicated). In addition, we analysed component costs of service provision, highlighted major cost drivers and attempted to explain any observed patterns, taking cognizance of any methodological differences.
Finally, where we found that it was not possible to disaggregate costs, we captured their stated total cost per service estimates and explored any emerging patterns within services, as part of a broader narrative synthesis.10
Patient and public involvement
Patients and the public were not involved in the design of this systemic review.
Results
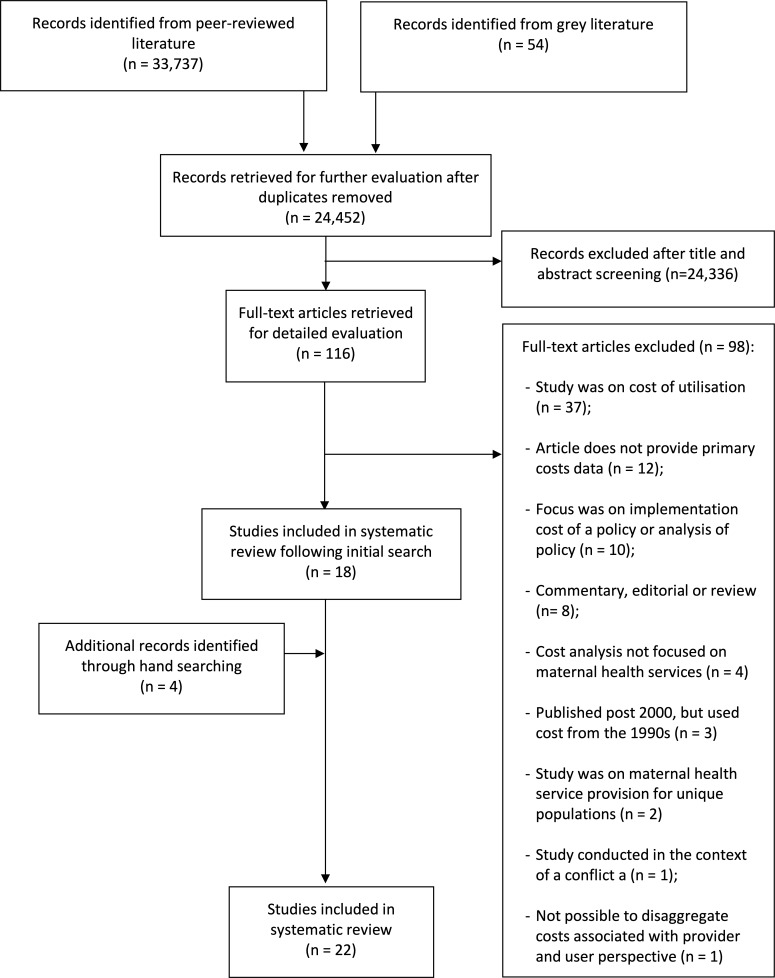
After duplicates were removed, 24 452 articles were screened by title and abstract for inclusion in the full-text review. Subsequently, the full-text of 116 articles were read, of which 18 articles met the inclusion criteria. Four additional articles were identified by snowballing through the bibliography of the selected articles. Thus, 22 studies were included in our narrative review of which 15 provided disaggregated component cost for our analysis (figure 1). Nineteen of the included studies were retrieved from peer-review literature,27–45 while the remaining three were sourced from grey literature.46–48
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart.
Distribution and quality assessment of included studies
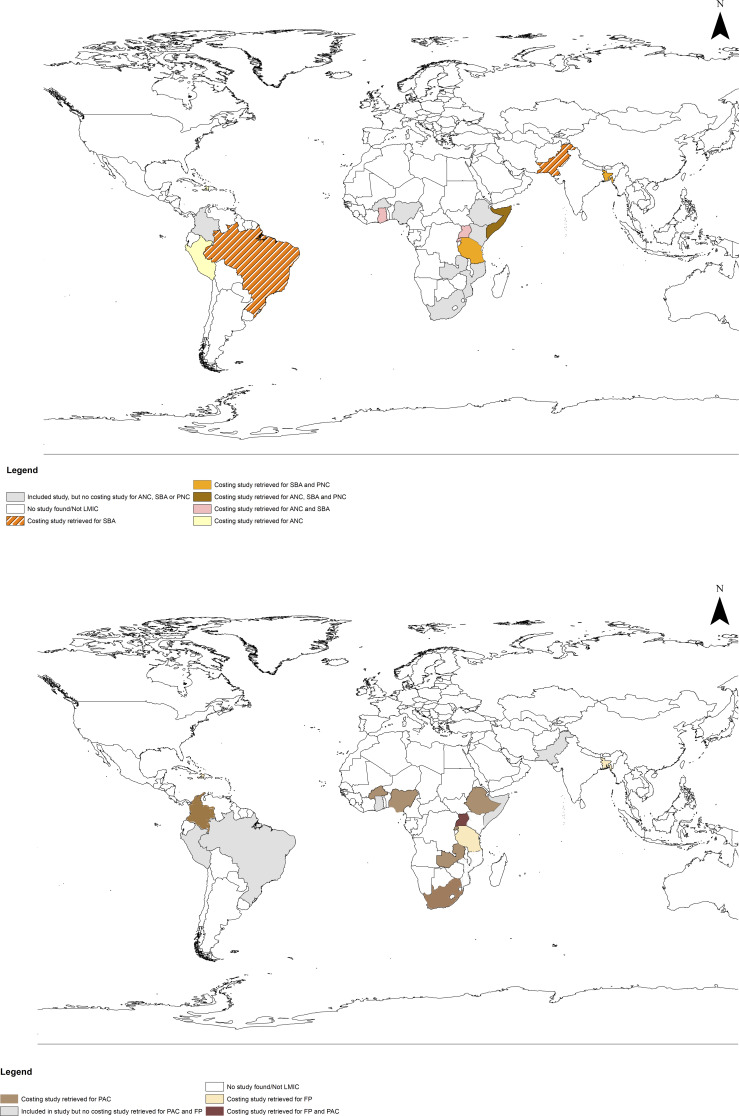
Thirteen studies were conducted in low-income countries (LICs) including four in Rwanda,35 41 45 46 two each in Tanzania32 36 and Uganda29 34 and one each in Burkina Faso,43 Democratic Republic of the Congo,27 Ethiopia,33 Haiti48 and Somalia.47 Five studies were conducted in lower-middle-income countries, with one each conducted in Bangladesh,37 Ghana,39 Nigeria,28 Pakistan42 and Zambia.30 Four studies were done in upper-middle-income countries (UMICs) including Brazil,40 Colombia,31 Peru38 and South Africa (figure 2).44
Figure 2.
Geographical distribution of included studies. ANC, antenatal care; FP, family planning; LMICs, low-income and middle-income countries; PAC, postabortion care; PNC, postnatal care; SBA, skilled birth attendant.
Eleven studies were assessed as high quality,31 34 35 37–39 41–45 eight were average quality27–30 32 33 36 40 and three were low quality.46–48 The criteria warranting the least scores were those related to detailing a breakdown of costs incurred for providing the service and incorporating indirect costs in the analysis (online supplementary table S3 in file 1).
In terms of the maternal health services that have been costed, 11 studies reported costs of vaginal and/or caesarean delivery.27 29 32 36 37 39 40 42 45–47 Nine studies costed provision of ANC.29 32 36–39 41 47 48 Eight studies costed provision of some form of care for abortion and/or its complication.28 30 33–35 43 44 Four studies costed family planning29 36 37 48 and two studies costed PNC provision37 47 (online supplementary table S4 in file 1). Eleven studies were done at a subnational scale.28 29 32 33 37 39–41 46–48 Four studies were each conducted in multiple facilities within one district27 36 38 42 and within several representative facilities at a national scale,31 34 35 while another four studies costed services within a single facility.30 43–45
Methods used in collecting and analysing cost data
Eight studies used a cross-sectional study design using primary data.28 29 37 39–43 Two studies each used a retrospective cross-sectional study32 38 or a mixed methods design,36 45 and one was a cost-effectiveness analysis.44 Four studies reported using the Post-Abortion Care Costing Methodology (PACCM).31 33–35 Five studies did not specifically state the study design used.27 30 46–48 For data collection, cost data were collected either with a questionnaire as part of a survey,37 38 40 41 with a bespoke data collection tool based on the Savings tool in the WHO’s Mother-Baby package28 or using the CORE Plus tool.46 48 Four studies used key informant interviews (KIIs) only,33–35 44 while another study was based on a review of documents only.42 Five studies used a combination of KIIs and document review27 29–31 36 and one study used KIIs and survey.43 Three studies used a combination of KIIs, document reviews and physical inventory of resources to collect cost data (online supplementary table S4 in file 1).32 39 45
Eleven studies used some form of ingredient approach.27 30 31 33–36 41 44 45 48 This included five studies that used methodologies that were variants of the ingredient approach—PACCM31 33–35 and the time-driven activity-based costing (TDABC).45 Six studies used the expenditure approach32 39 42 43 46 47 and three studies used a mixed approach combining both.37 38 40 Two studies did not state the costing methods used.28 29 Nineteen studies reported only mean cost as a summary measure,27–38 40–48 while the other three studies reported mean and median cost of service provision.31 33 39 Fifteen studies provided cost data that could be disaggregated by service.29–31 33–35 37 38 40–45 48 Five studies provided cost breakdown by facility or by district, but not by service32 36 39 46 47 and two studies did not provide any cost breakdown.27 28
Cost of providing maternal health services
Details of the extracted cost of service provision for all included studies and the estimated cost following inflation for studies that presented disaggregated costs are presented in online supplementary table S5 and table S6 of file 1, respectively. In the paragraphs below, a summary of the key cost findings of this review are presented per maternal health service. For each service, the number of studies with disaggregated costs, cost of provision per provider type and per facility type as well as major cost drivers are presented.
For ANC, five studies provided disaggregated cost.29 37 38 41 48 Based on provider type, median cost of ANC provided by non-government organisations (NGOs) was estimated at US$7.24 across Bangladesh and Haiti, US$8.50 for public and missionary provision across Haiti, Peru, Rwanda and Uganda and US$31.42 for private provision in Rwanda. Comparing cost based on facility type, the re-calculated cost of ANC provision ranged from US$5.73 in a public health centre (third ANC visit) to US$81.01 in a private hospital (first visit). In terms of major cost drivers, after excluding capital expenditure, personnel, medicines and equipment were the major cost drivers for ANC provision in Uganda,29 Bangladesh and Rwanda37 41 and Peru,38 respectively (table 1).
Table 1.
Cost of providing antenatal care (ANC)
| Study | Country | Service | Facility type | Facility ownership | Personnel (US$) |
Equipment (US$) |
Medicines (US$) |
Supplies (US$) |
Medicines+supplies (US$) |
Laboratory (US$) |
Housekeeping (US$) |
Capital (US$) |
Overheads (US$) |
Administration (US$) |
Communication (US$) |
Repair and maintenance (US$) |
Utility (US$) |
Indirect (US$) |
Adjusted cost per service provided (US$) |
| Hitimana et al.41 | Rwanda | ANC* | Hospital | Private | 21.21 | 0.43 | – | – | 53.98 | – | – | 0.19 | 5.21 | – | – | – | – | – | 81.01 |
| Hitimana et al.41 | Rwanda | ANC† | Hospital | Private | 15.90 | 0.32 | – | – | 11.20 | – | – | 0.14 | 3.90 | – | – | – | – | – | 31.47 |
| Hitimana et al.41 | Rwanda | ANC‡ | Hospital | Private | 15.90 | 0.32 | – | – | 11.09 | – | – | 0.14 | 3.90 | – | – | – | – | – | 31.36 |
| Cobos Muñoz et al.38 | Peru | ANC | Health centre | Public | 3.25 | 12.43 | 0.44 | 0.08 | – | – | 0.02 | 14.68 | – | 0.05 | 0.01 | 0.18 | 0.09 | – | 31.23 |
| Hitimana et al.41 | Rwanda | ANC† | Hospital | Private | 10.60 | 0.21 | – | – | 16.53 | – | – | 0.09 | 2.60 | – | – | – | – | – | 30.04 |
| Hitimana et al.41 | Rwanda | ANC* | Health centre | Public/Missionary | 2.75 | 0.14 | – | – | 17.56 | – | – | 0.14 | 0.85 | – | – | – | – | – | 21.44 |
| Cros et al.48 | Haiti | ANC | Health centre without bed | Public | 3.37 | – | 0.45 | 0.08 | – | 2.09 | – | – | 7.38 | – | – | – | – | – | 13.37 |
| Hitimana et al.41 | Rwanda | ANC§ | Health centre | Public/Missionary | 1.76 | 0.09 | – | – | 8.43 | – | – | 0.07 | 0.54 | – | – | – | – | – | 10.89 |
| Orach et al.29 | Uganda | ANC | Hospital | Public | 8.19 | – | 0.42 | 1.06 | – | – | – | – | – | – | – | – | – | – | 9.67 |
| Zeng et al.37 | Bangladesh | ANC | Clinic | NGO | 0.60 | – | 4.63 | 0.00 | – | 1.87 | – | – | 0.60 | – | – | – | – | – | 7.70 |
| Orach et al.29 | Uganda | ANC | Health centre IV | Public | 6.53 | – | 0.67 | 0.14 | – | – | – | – | – | – | – | – | – | – | 7.33 |
| Orach et al.29 | Uganda | ANC | Health centre III | Public | 6.10 | – | 0.61 | 0.35 | – | – | – | – | – | – | – | – | – | – | 7.06 |
| Orach et al.29 | Uganda | ANC | Health centre II | Public | 6.16 | – | 0.41 | 0.30 | – | – | – | – | – | – | – | – | – | – | 6.87 |
| Cros et al.48 | Haiti | ANC | Health centre without bed | NGO | 1.71 | – | 0.50 | 0.11 | – | 2.34 | – | – | 2.11 | – | – | – | – | – | 6.77 |
| Hitimana et al.41 | Rwanda | ANC‡ | Health centre | Public/Missionary | 1.22 | 0.06 | – | – | 4.60 | – | – | 0.12 | 0.38 | – | – | – | – | – | 6.38 |
| Hitimana et al.41 | Rwanda | ANC† | Health centre | Public/Missionary | 1.10 | 0.06 | – | – | 4.13 | – | – | 0.11 | 0.34 | – | – | – | – | – | 5.73 |
*First visit.
†Third visit.
‡Second visit.
§Fourth visit.
NGO, non-government organisation.
For skilled birth attendance, including vaginal and caesarean delivery, five studies provided cost data for which disaggregation into cost components was feasible.29 37 40 42 45 Based on provider type, one study in Bangladesh presented cost of NGO provision,37 while the other four presented public provision costs.29 40 42 45 Cost of providing vaginal delivery at clinics managed by NGO (US$35.45) was almost twice the cost of the same service provided by public providers in Uganda (US$18.31). Based on facility type, at a median cost of US$14.32 across all public health facility levels, Uganda reported the lowest cost for providing vaginal delivery supported by a skilled birth attendant (SBA). This was followed by US$33.41 and US$74.19 in Bangladesh and Pakistan, respectively, excluding overheads and capital expenditure. Following similar exclusions, vaginal delivery in Brazil was the most expensive at US$278.22. For caesarean delivery provided in the public sector, the study conducted in Uganda also reported the lowest cost at US$72.11 while it was estimated at US$378.94 in Brazil excluding overheads and capital expenditure. In terms of cost drivers, after excluding capital cost, personnel constituted the major cost driver for vaginal delivery, ranging from 45% in Pakistan at public health centre level to 91% in Brazil at hospital level.29 40 Personnel cost was also the major driver for caesarean delivery, ranging from 68% to 85% in the NGO-managed clinic in Bangladesh and the public hospital in Brazil, respectively (table 2).37 40
Table 2.
Cost of providing skilled birth attendance during delivery
| Study | Country | Service | Facility type | Facility ownership | Personnel (US$) |
Equipment (US$) |
Medicines (US$) |
Supplies (US$) |
Laboratory (US$) |
Blood (US$) |
Housekeeping (US$) |
Lodging (US$) |
Capital (US$) |
Overheads (US$) |
Administration (US$) |
Communication (US$) |
Repair and maintenance (US$) |
Utility (US$) |
Indirect (US$) |
Adjusted cost per service provided (US$) |
| Entringer et al.40 | Brazil | Caesarean delivery | Hospital | Public | 330.78 | – | – | 48.16 | – | – | – | – | 13.20 | – | 8.45 | – | – | – | – | 400.59 |
| Entringer et al.40 | Brazil | Vaginal delivery | Hospital | Public | 262.42 | – | – | 15.80 | – | – | – | – | 32.03 | – | 9.74 | – | – | – | – | 319.98 |
| Odhiambo et al.45 | Rwanda | Caesarean delivery (all phases) | Hospital | Public | 53.86 | – | 116.86 | 130.80 | – | – | – | – | 4.95 | – | – | – | – | – | 29.27 | 335.75 |
| Khan & Zaman42 | Pakistan | Caesarean delivery | Hospital | Public | 133.84 | 15.49 | 15.49 | – | 1.79 | 8.13 | 2.87 | 23.90 | 43.33 | – | 11.95 | 6.21 | 15.30 | 64.53 | – | 342.82 |
| Odhiambo et al.45 | Rwanda | Caesarean delivery (post) | Hospital | Public | 22.25 | – | 58.97 | 64.33 | – | – | – | – | 23.42 | – | – | – | – | – | 24.59 | 193.55 |
| Zeng et al.37 | Bangladesh | Caesarean section | Clinic | NGO | 93.11 | – | 38.79 | – | 2.15 | – | – | – | – | 3.27 | – | – | – | – | – | 137.32 |
| Odhiambo et al.45 | Rwanda | Caesarean delivery (intra) | Hospital | Public | 19.91 | – | 48.24 | 57.89 | – | – | – | – | 1.17 | – | – | – | – | – | 1.17 | 128.39 |
| Orach et al.29 | Uganda | Caesarean section | Hospital | Public | 35.33 | – | 19.64 | 17.15 | – | – | – | – | – | – | – | – | – | – | – | 72.11 |
| Khan & Zaman42 | Pakistan | Vaginal delivery | Hospital | Public | 33.46 | 3.57 | 3.57 | – | 0.36 | 1.43 | 0.72 | 5.98 | – | – | 3.11 | 1.43 | 3.82 | 16.73 | – | 74.19 |
| Odhiambo et al.45 | Rwanda | Caesarean delivery (pre) | Hospital | Public | 12.88 | – | 9.65 | 7.50 | – | – | – | – | 18.74 | – | – | – | – | – | 3.51 | 52.28 |
| Zeng et al.37 | Bangladesh | Vaginal delivery | Clinic | NGO | 24.26 | – | 7.90 | – | 1.25 | – | – | – | 8.60 | 2.04 | – | – | – | – | – | 44.06 |
| Collins et al.46 | Rwanda | Vaginal delivery | Health centre | Public | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 0.00 |
| Orach et al.29 | Uganda | Vaginal delivery | Health centre IV | Public | 15.58 | – | 0.56 | 2.01 | – | – | – | – | – | – | – | – | – | – | – | 18.15 |
| Orach et al.29 | Uganda | Vaginal delivery | Hospital | Public | 16.11 | – | 0.22 | 1.99 | – | – | – | – | – | – | – | – | – | – | – | 18.31 |
| Orach et al.29 | Uganda | Vaginal delivery | Health centre III | Public | 13.06 | – | 0.57 | 1.69 | – | – | – | – | – | – | – | – | – | – | – | 15.32 |
| Orach et al.29 | Uganda | Vaginal delivery | Health centre II | Public | 11.47 | – | 0.37 | 1.62 | – | – | – | – | – | – | – | – | – | – | – | 13.45 |
NGO, non-government organisation.
Only one study provided disaggregated costs for PNC. This study was conducted in an NGO-managed clinic in Bangladesh. The study estimated cost of providing PNC at US$5.04, with medicines noted as the major cost driver (79%).37 For FP, two studies conducted in Bangladesh and Uganda provided total costs disaggregated into component costs.29 37 However, only the study, conducted in Uganda, specified the type of FP commodity being provided.29 In that study, provision of condoms in a health centre was the least expensive FP service (US$2.72) while the most expensive FP service was the provision of the injectable contraceptive, Depo-Provera in a hospital (US$5.27).29 As regards cost drivers of service provision, personnel cost was higher when commodities such as oral pills and Depo-Provera were being provided, while cost of supplies were higher than personnel when condoms were being provided (table 3).
Table 3.
Cost of providing postnatal care and family planning
| Study | Country | Service | Facility type | Facility ownership | Labour (US$) |
Medicines (US$) |
Supplies (US$) |
Laboratory (US$) |
Overheads (US$) |
Adjusted cost per service provided (US$) |
| Orach et al.29 | Uganda | FP—Depo-Provera | Hospital | Public | 4.14 | – | 1.13 | – | – | 5.27 |
| Zeng et al.37 | Bangladesh | PNC | Clinic | NGO | 0.48 | 3.96 | – | 0.08 | 0.53 | 5.04 |
| Orach et al.29 | Uganda | FP—Depo-Provera | Health centre IV | Public | 3.84 | – | 0.76 | – | – | 4.61 |
| Orach et al.29 | Uganda | FP—oral pills | Hospital | Public | 4.28 | – | 0.24 | – | – | 4.52 |
| Orach et al.29 | Uganda | FP—condom | Hospital | Public | 2.05 | – | 2.40 | – | – | 4.45 |
| Orach et al.29 | Uganda | FP—condom | Health centre III | Public | 1.66 | – | 2.79 | – | – | 4.45 |
| Orach et al.29 | Uganda | FP - Depo-Provera | Health centre III | Public | 3.68 | – | 0.76 | – | – | 4.44 |
| Orach et al.29 | Uganda | FP—Depo-Provera | Health centre II | Public | 3.65 | – | 0.75 | – | – | 4.39 |
| Orach et al.29 | Uganda | FP—oral pills | Health centre IV | Public | 3.88 | – | 0.11 | – | – | 3.99 |
| Orach et al.29 | Uganda | FP—oral pills | Health centre III | Public | 3.58 | – | 0.16 | – | – | 3.74 |
| Orach et al.29 | Uganda | FP—condom | Health centre II | Public | 1.46 | – | 2.12 | – | – | 3.58 |
| Orach et al.29 | Uganda | FP—oral pills | Health centre II | Public | 3.15 | – | 0.16 | – | – | 3.31 |
| Orach et al.29 | Uganda | FP—condom | Health centre IV | Public | 1.59 | – | 1.13 | – | – | 2.72 |
| Orach et al.29 | Bangladesh | FP | Clinic | NGO | 0.21 | 0.42 | – | – | 0.19 | 0.82 |
FP, family planning; NGO, non-government organisation.
For PAC, seven studies provided disaggregated cost that could be used in this analysis.30 31 33–35 43 44 Based on facility type, cost of providing PAC without management of complications in a public hospital ranged from US$120.66 in Rwanda35 to US$379.40 in Uganda,34 while cost of providing simple PAC in a health centre was lower with estimates of US$97.09 in Rwanda35 and US$172.09 in Uganda.34 When PAC presented with complications, uterine laceration and shock were the most expensive complications to manage, with costs ranging from US$259.52 in Zambia to US$1299.21 in Colombia.30 31 33 As for cost drivers of PAC, personnel cost for providing PAC with complications constituted the lowest proportion of provision cost in Burkina Faso at US$0.77 for PAC with incomplete abortion or vaginal laceration and US$1.37 for PAC with shock.43 Irrespective of the presenting complication, cost of personnel required for PAC was highest in Colombia (US$464.33–US$1019.80) (table 4).31
Table 4.
Cost of providing postnatal care and family planning
| Study | Country | Service | Facility type | Facility ownership | Personnel (US$) |
Equipment (US$) |
Medicines (US$) |
Medicines on admission (US$) |
Supplies (US$) |
Medicines+supplies (US$) |
Laboratory (US$) |
Blood (US$) |
Lodging (US$) |
Capital (US$) |
Overheads (US$) |
Operating theatre (US$) |
Adjusted cost per service provided (US$) |
| Prada et al.31 | Colombia | PAC+UL | Hospital (3°) | Public | 1019.80 | – | 279.41 | – | – | – | – | – | – | – | – | – | 1299.21 |
| Prada et al.31 | Colombia | PAC+S | Hospital (3°) | Public | 409.29 | – | 455.29 | – | – | – | – | – | – | – | – | – | 864.58 |
| Prada et al.31 | Colombia | PAC+UL | Hospital (2°) | Public | 742.92 | – | 114.76 | – | – | – | – | – | – | – | – | – | 857.68 |
| Prada et al.31 | Colombia | PAC+S | Hospital (2°) | Public | 345.66 | – | 341.78 | – | – | – | – | – | – | – | – | – | 687.44 |
| Prada et al.31 | Colombia | PAC+Sep | Hospital (3°) | Public | 553.75 | – | 109.77 | – | – | – | – | – | – | – | – | – | 663.52 |
| Prada et al.31 | Colombia | PAC+Sep | Hospital (2°) | Public | 464.33 | – | 77.34 | – | – | – | – | – | – | – | – | – | 541.66 |
| Vlassoff et al.33 | Ethiopia | PAC+UL | Mixed | Public/Private | 274.31 | – | – | 99.67 | – | – | – | – | – | – | – | 16.25 | 390.23 |
| Vlassoff et al.34 | Uganda | PAC | Regional hospital | Public | 26.18 | – | – | – | – | 48.49 | – | – | – | 271.07 | 33.66 | – | 379.40 |
| Prada et al.31 | Colombia | PAC+VL | Hospital (3°) | Public | 297.51 | – | 67.36 | – | – | – | – | – | – | – | – | – | 364.87 |
| Prada et al.31 | Colombia | Legal abortion | Hospital (2°) | Public | 328.47 | – | 27.44 | – | – | – | – | – | – | – | – | – | 355.91 |
| Prada et al.31 | Colombia | PAC+VL | Hospital (2°) | Public | 290.63 | – | 29.94 | – | – | – | – | – | – | – | – | – | 320.57 |
| Prada et al.31 | Colombia | Legal abortion | Hospital (3°) | Public | 288.91 | – | 26.19 | – | – | – | – | – | – | – | – | – | 315.11 |
| Vlassoff et al.35 | Rwanda | PAC | Referral hospital | Public | 40.39 | – | – | – | – | 76.42 | – | – | – | 104.63 | 91.06 | – | 312.50 |
| Vlassoff et al.33 | Ethiopia | PAC+VL | Mixed | Public/Private | 205.73 | – | – | 74.76 | – | – | – | – | – | – | – | 12.18 | 292.67 |
| Parmar et al.30 | Zambia | PAC+S | Hospital | Public | 33.41 | – | – | – | – | 23.08 | 5.38 | 148.25 | 49.41 | – | – | – | 259.52 |
| Vlassoff et al.34 | Uganda | PAC | District hospital | Mixed | 25.68 | – | – | – | – | 34.59 | – | – | – | 169.22 | 27.13 | – | 256.62 |
| Vlassoff et al.34 | Uganda | PAC | Health centre | Public | 16.99 | – | – | – | – | 25.62 | – | – | – | 95.41 | 34.06 | – | 172.09 |
| Prada et al.31 | Colombia | PAC+IA | Hospital (2°) | Public | 137.58 | – | 23.70 | – | – | – | – | – | – | – | – | – | 161.28 |
| Vlassoff et al.35 | Rwanda | PAC | Clinic | Private | 77.01 | – | – | – | – | 26.11 | – | – | – | 9.62 | 36.24 | – | 148.98 |
| Parmar et al.30 | Zambia | PAC+Sep | Hospital | Public | 29.34 | – | – | – | – | 5.40 | 33.06 | 24.35 | 53.90 | – | – | – | 146.04 |
| Prada et al.31 | Colombia | PAC+IA | Hospital (3°) | Public | 118.66 | – | 22.45 | – | – | – | – | – | – | – | – | – | 141.11 |
| Vlassoff et al.35 | Rwanda | PAC | District hospital | Public/Private | 33.49 | – | – | – | – | 42.72 | – | – | – | 4.56 | 39.89 | – | 120.66 |
| Vlassoff et al.33 | Ethiopia | PAC+Sep | Mixed | Public/Private | 83.70 | – | 15.62 | 5.03 | – | – | – | – | – | – | – | – | 104.35 |
| Ilboudo et al.43 | Burkina Faso | PAC+Sep | Hospital | Public | 3.05 | – | 50.34 | – | – | – | – | – | – | – | 45.73 | – | 99.13 |
| Vlassoff et al.35 | Rwanda | PAC | Health centre | Public | 7.77 | – | – | – | – | 20.16 | – | – | – | 21.52 | 47.63 | – | 97.09 |
| Vlassoff et al.33 | Ethiopia | PAC+S | Mixed | Public/Private | 71.45 | – | 17.68 | 6.24 | – | – | – | – | – | – | – | – | 95.37 |
| Ilboudo et al.43 | Burkina Faso | PAC+UL | Hospital | Public | 1.93 | – | 26.24 | – | – | – | – | – | – | – | 57.67 | – | 85.84 |
| Lince-Deroche et al.44 | South Africa | MVA | Hospital | Public | 48.27 | 10.09 | 1.83 | – | 20.65 | – | – | – | – | – | – | – | 80.84 |
| Prada et al.31 | Colombia | Legal abortion | Clinic | Private | 65.35 | – | 8.73 | – | – | – | – | – | – | – | – | – | 74.08 |
| Prada et al.31 | Colombia | PAC+IA | Clinic | Private | 65.35 | – | 8.73 | – | – | – | – | – | – | – | – | – | 74.08 |
| Lince-Deroche et al.44 | South Africa | Medication abortion | Hospital | Public | 36.67 | 5.68 | 18.59 | – | 11.29 | – | – | – | 1.17 | – | – | – | 73.40 |
| Parmar et al.30 | Zambia | MVA | Hospital | Public | 14.59 | – | – | – | – | 3.89 | 11.80 | 20.87 | 6.74 | – | – | – | 57.88 |
| Ilboudo et al.43 | Burkina Faso | PAC+VL | Hospital | Public | 0.77 | – | 38.34 | – | – | – | – | – | – | – | 14.80 | – | 53.90 |
| Parmar et al.30 | Zambia | PAC+IA | Hospital | Public | 13.34 | – | – | – | – | 10.75 | 3.35 | 8.70 | 12.57 | – | – | – | 48.71 |
| Vlassoff et al.33 | Ethiopia | PAC+UE | Mixed | Public/Private | 25.13 | – | 19.26 | – | – | – | – | – | – | – | – | – | 44.40 |
| Parmar et al.30 | Zambia | Medication abortion | Hospital | Public | 16.97 | – | – | – | – | 13.99 | 11.68 | – | – | – | – | – | 42.64 |
| Ilboudo et al.43 | Burkina Faso | PAC+S | Hospital | Public | 1.37 | – | 24.31 | – | – | – | – | – | – | – | 14.80 | – | 40.48 |
| Ilboudo et al.43 | Burkina Faso | PAC+H | Hospital | Public | 0.69 | – | 20.62 | – | – | – | – | – | – | – | 9.37 | – | 30.68 |
| Ilboudo et al.43 | Burkina Faso | Incomplete abortion | Hospital | Public | 0.77 | – | 15.43 | – | – | – | – | – | – | – | 11.44 | – | 27.64 |
2°, secondary hospital; 3°, tertiary hospital; MVA, manual vacuum aspiration; PAC+H, postabortion care with haemorrhage; PAC+IA, postabortion care with incomplete abortion; PAC+S, Postabortion care with shock; PAC+Sep, postabortion care with sepsis; PAC+UE, postabortion care with uterine evacuation; PAC+UL, postabortion care with uterine laceration; PAC+VL, postabortion care with vaginal laceration.
One other finding from our review was as it relates to the output (number of services) provided for the available input (total cost). Five studies conducted in Burkina Faso, Ghana, Haiti, Peru and Rwanda reported some economies of scale in cost of service provision.38 39 41 43 48 Three of the studies reported this finding in lower cadre staffed public facilities such as health centres and clinics38 39 41 and one was reported in referral hospital.43 In Ghana, simply increasing the number of deliveries by 10% reduced the unit cost per delivery by 18.75% (from US$63.23 to US$51.37).39 Similarly, in Peru, Mi Peru district had one of the highest total costs of provision but it had the lowest mean cost per visit.38
Discussion
This systematic review based on 22 studies covering 17 individual countries provides the most up-to-date and comprehensive overview of cost of maternal health service provision in LMICs from year 2000 to today. In all, we found that only 16% of all LMICs have at least one costing study published. A previous article associated the dearth of costing studies in LMICs to the lack of technical capacity to conduct such studies, and incomplete or absent records of activity-linked resource data.49 It might also be a case of lack of interest locally on the part of policy makers, providers and researchers.
Of the available studies that we were able to retrieve, diverse methods were used in collecting and analysing cost. Indeed, the impact on final cost estimates that these various methods bring are well recognised.50 For example, cost estimates will vary depending on if a bottom-up or top-down costing approach is taken.50 The real issue though is not the use of different methods, but the need for more application of best practices for costing in order to improve validity and comparability of results. Apart from established best practices including use of bottom-up or combined use of both bottom-up and top-down costing approaches in a mixed approach, the use of US$ or International Dollars in presenting findings and incorporation of indirect costs into analysis,25 49 50 our review showed that there are other methodological issues requiring consensus. These include requirement for triangulation of data sources for cost analyses, specific cost components that should be included, for example, should fringe benefits such as health insurance, scholarship for health workers, etc be included in costing? Other issues include approach to cost disaggregation, time allocation for health workers and use of median cost as a summary measure, as well as approach to amortisation of capital projects in cost analyses.
As regards cost of service provision, median cost of publicly provided ANC provision in health centres across four countries was US$8.50. Cost of ANC was slightly cheaper with NGO-led provision while it was costlier to provide in hospitals and within the private sector. We were able to draw these parallels because all studies used the microcosting approach and costing was principally based on the 2001 WHO recommendation of focused ANC.51 The latest global guidelines however, recommend an increase from four visits during pregnancy to eight contacts with skilled personnel.52 This will ultimately have implications on service cost, as time spent in consultation and human resources required for ANC contacts will have to increase. As such, cost of ANC provision with this new package may be higher than initial estimates.
For delivery with skilled birth attendance in public health facilities, there was a wide variation for both normal vaginal and caesarean delivery with the least cost reported in Uganda and the highest in Brazil. A previous study suggests that there is a relationship between cost per service increments with increasing GDP per capita.37 Yet, it is difficult to accept that the marked difference in cost is because Brazil is an UMIC and others are LMIC/LIC. Looking more closely at the break down of cost in Brazil, it becomes apparent that the major cost drivers in Brazil relates to personnel. While service in Uganda was provided by medical doctors, clinical or nursing officers,29 the Brazil study costed vaginal delivery provided by obstetricians.40 Based on this finding, there may be a financial case for cost savings as it relates to task-shifting and task-sharing of delivery services in LMICs, as has been demonstrated for several other global health priorities.53 This finding adds to the established evidence on efficiency and effectiveness of task-shifting of maternal health interventions as a policy.54
After adjustments, the range of cost for FP service provision estimated in our review was put at US$0.82 to US$2.72. This tallies with findings from an evidence brief by WHO, which estimated the average cost per modern contraceptive as US$1.01.55 In our review, FP service provision by NGOs was the least costly. This is probably because of the significant financial contributions from international donors which help subsidise the cost of FP commodities and the widely lauded efficiency of NGO-managed health services.56 We could not ascertain a pattern with cost of PNC provision because only one study in our review costed the service and provided disaggregated cost, with cost per service estimated at US$5.04.37
As complications require more resources, it was not surprising to find that PAC with management of complications was costlier than PAC alone. The more severe the complication, the higher the cost of service provision with uterine laceration and shock costing the highest. The cost also varied based on type of facility, with the service costing more if care is provided in a hospital as opposed to health centres. Keeping hospitalisation rates to the barest minimum was an approach used to reduce cost of PAC provision in South Africa.44 We noted though that while cost of the actual emergency treatment was reported in all studies, none of the studies costed for FP and community empowerment through awareness and mobilisation, both of which are key components of comprehensive PAC.57
Our review pointed to some economies of scale for service provision as reported in Burkina Faso, Ghana, Haiti and Rwanda.38 39 41 43 48 This phenomenon occurred irrespective of the provider (NGO vs public) and the facility level (health centre vs hospital). Indeed, a major share of cost of service provision are fixed costs, so an increasing output does not necessarily increase the unit healthcare provision costs proportionally.58 A coordinated approach to ensure maximal utilisation of facility-based maternal health services may result in a more efficient use of resources for service provision.
Implications for practice and research
Our review highlights some critical methodological issues that need to be addressed to develop the practice of costing maternal health services. We believe that propagating consensus around already established costing approaches such as the WHO’s Mother-Baby Package Costing tool,59 PACCM developed by the Guttmacher Institute33 and TDABC, promoted as being valuable in LMICs60 will be a good next step in improving the quality of costing studies.
Indeed, there is global recognition of the need for more transparency and monitoring of financial resources required for achieving the SDGs in LMICs.61 However, from this review, it is clear that the number of available costing studies done at high level of methodological rigour that can be used for monitoring investments made in maternal health is low in LMICs. Certainly, more costing studies of PNC need to be conducted to better understand patterns, especially given the need for LMICs to scale up the implementation of postpartum care.62
Strengths and limitations
Strengths of this review are its inclusion of costing studies published in both peer-reviewed and grey literature, inflation of cost to comparable 2019 US Dollar equivalents and disaggregation of cost components for the various services. Doing this allowed us to for the first time be able to compare and contrast costs of providing the different maternal health services across countries, facility and provider types.
However, some limitations of our review need to be acknowledged. It was not possible to make meaningful comparisons in all cases. For example, there was only one study that costed provision of PNC which also had disaggregated cost.37 In addition, we could not fully describe the specific package of care provided to women in every study, as significant detail on care packages were not typically reported in the included studies. However, by including only studies published from year 2000, we ensured that we were comparing like-for-like recommended services, as global guidance regarding care packages were updated around this period. Finally, despite our best efforts, there were some costing studies not publicly available. For example, Blaakman makes reference to costing studies published in Kenya, Malawi and Rwanda.47 However, full texts of these could not be retrieved. Anecdotal evidence also suggests that there are more costing exercises being conducted in LMICs by Ministries of Health, many of which are not published online.
Conclusion
While we have been able to move the discussion in the field from comparing ‘apples and oranges’ to maybe comparing ‘green apples and red apples’, there is still a need to build consensus around definitions and methodology for costing maternal health services in LMICs. Indeed, as evidenced in our review, with rigorous adjustments made to cost data, there are some patterns emerging and a lot of shared learning on what can be done to increase cost savings and improve efficiency and effectiveness of service delivery in LMICs. As the global community moves forward with planning for and implementing service delivery in the SDG era, in addition to increased call for transparency, consensus around costing methodology is important to improve comparability and increase opportunities for learning and evidence-based resource allocation across countries.
Footnotes
Handling editor: Seye Abimbola
Twitter: @abankethomas, @lade_abeji, @ejemaim, @acameh
Contributors: AB-T, I-OOA, OB-T and CA conceptualised the review. AB-T and FIA conducted literature searches, screened them for inclusion and conducted the quality assessment. Discrepancies were resolved through discussions with CA. AB-T, I-OOA and FIA reviewed the included studies and were involved in data extraction. Data synthesis was conducted by AB-T, OB-T and EAE. All authors were involved in writing the manuscript and approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.United Nations Sustainable Development Goals: 17 goals to transform our world [Internet]. Sustainable Development Goals, 2016. Available: http://www.un.org/sustainabledevelopment/sustainable-development-goals/ [Accessed 20 Jun 2020].
- 2.Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the un maternal mortality estimation Inter-Agency group. Lancet 2016;387:462–74. 10.1016/S0140-6736(15)00838-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kerber KJ, de Graft-Johnson JE, Bhutta ZA, et al. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet 2007;370:1358–69. 10.1016/S0140-6736(07)61578-5 [DOI] [PubMed] [Google Scholar]
- 4.Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open 2017;7:e017122. 10.1136/bmjopen-2017-017122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paxton A, Maine D, Freedman L, et al. The evidence for emergency obstetric care. Int J Gynaecol Obstet 2005;88:181–93. 10.1016/j.ijgo.2004.11.026 [DOI] [PubMed] [Google Scholar]
- 6.Ahmed S, Li Q, Liu L, et al. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet 2012;380:111–25. 10.1016/S0140-6736(12)60478-4 [DOI] [PubMed] [Google Scholar]
- 7.Stenberg K, Lauer JA, Gkountouras G, et al. Econometric estimation of WHO-CHOICE country-specific costs for inpatient and outpatient health service delivery. Cost Eff Resour Alloc 2018;16:11. 10.1186/s12962-018-0095-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borghi J. What is the cost of maternal health care and how can it be financed? : Brouwere D, Van Lerberghe W, Safe motherhood strategies: a review of the evidence [Internet. Antwerp, Belgium: ITGPress, 2001. : 243–92. http://hdl.handle.net/10390/2661 [Google Scholar]
- 9.Nixon J, Khan KS, Kleijnen J. Summarising economic evaluations in systematic reviews: a new approach. BMJ 2001;322:1596–8. 10.1136/bmj.322.7302.1596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gomersall JS, Jadotte YT, Xue Y, et al. Conducting systematic reviews of economic evaluations. Int J Evid Based Healthc 2015;13:170–8. 10.1097/XEB.0000000000000063 [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Banke-Thomas A, Abejirinde I-OO, Banke-Thomas O, et al. Cost of maternal health services in low and middle-income countries: protocol for a systematic review. BMJ Open 2019;9:e027822. 10.1136/bmjopen-2018-027822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilczynski NL, Haynes RB, Lavis JN, et al. Optimal search strategies for detecting health services research studies in MEDLINE. CMAJ 2004;171:1179–85. 10.1503/cmaj.1040512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGowan J, Sampson M, Lefebvre C. An evidence based checklist for the peer review of electronic search strategies (press EBC). Evid Based Libr Inf Pract 2010;5:149 10.18438/B8SG8R [DOI] [Google Scholar]
- 15.Adams J, Hillier-Brown FC, Moore HJ, et al. Searching and synthesising 'grey literature' and 'grey information' in public health: critical reflections on three case studies. Syst Rev 2016;5:164. 10.1186/s13643-016-0337-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Bank World Bank Country and Lending Groups [Internet]. Data, 2019. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 [Accessed 20 Jun 2020].
- 17.Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. Oxford University Press: Oxford, 2015. [Google Scholar]
- 18.Dieleman JL, Schneider MT, Haakenstad A, et al. Development assistance for health: past trends, associations, and the future of international financial flows for health. Lancet 2016;387:2536–44. 10.1016/S0140-6736(16)30168-4 [DOI] [PubMed] [Google Scholar]
- 19.Pitt C, Grollman C, Martinez-Alvarez M, et al. Tracking aid for global health goals: a systematic comparison of four approaches applied to reproductive, maternal, newborn, and child health. Lancet Glob Health 2018;6:e859–74. 10.1016/S2214-109X(18)30276-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stone G, Hutchinson A, Corso P, et al. Understanding and Using the Economic Evidence : Zaza S, Briss PA, Harris KW, et al., The guide to community preventive services. New York: Oxford University Press, 2005: 449–63. [Google Scholar]
- 21.Husereau D, Drummond M, Petrou S, et al. Consolidated health economic evaluation reporting standards (cheers) statement. BJOG 2013;120:765–70. 10.1111/1471-0528.12241 [DOI] [PubMed] [Google Scholar]
- 22.Mangham-Jefferies L, Pitt C, Cousens S, et al. Cost-Effectiveness of strategies to improve the utilization and provision of maternal and newborn health care in low-income and lower-middle-income countries: a systematic review. BMC Pregnancy Childbirth 2014;14:243. 10.1186/1471-2393-14-243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banke-Thomas A, Wilson-Jones M, Madaj B, et al. Economic evaluation of emergency obstetric care training: a systematic review. BMC Pregnancy Childbirth 2017;17:403. 10.1186/s12884-017-1586-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeng W, Li G, Ahn H, et al. Cost-Effectiveness of health systems strengthening interventions in improving maternal and child health in low- and middle-income countries: a systematic review. Health Policy Plan 2018;33:283–97. 10.1093/heapol/czx172 [DOI] [PubMed] [Google Scholar]
- 25.Turner HC, Lauer JA, Tran BX, et al. Adjusting for inflation and currency changes within health economic studies. Value Health 2019;22:1026–32. 10.1016/j.jval.2019.03.021 [DOI] [PubMed] [Google Scholar]
- 26.International Monetary Fund World Economic Outlook database [Internet]. Data and statistics, 2019. Available: https://www.imf.org/external/pubs/ft/weo/2019/01/weodata/download.aspx [Accessed 10 Jun 2020].
- 27.Deboutte D, O'Dempsey T, Mann G, et al. Cost-Effectiveness of caesarean sections in a post-conflict environment: a case study of Bunia, Democratic Republic of the Congo. Disasters 2013;37 Suppl 1:S105–20. 10.1111/disa.12015 [DOI] [PubMed] [Google Scholar]
- 28.Benson J, Okoh M, KrennHrubec K, et al. Public hospital costs of treatment of abortion complications in Nigeria. Int J Gynaecol Obstet 2012;118 Suppl 2:S134–40. 10.1016/S0020-7292(12)60012-5 [DOI] [PubMed] [Google Scholar]
- 29.Orach CG, Dubourg D, De Brouwere V. Costs and coverage of reproductive health interventions in three rural refugee-affected districts, Uganda. Trop Med Int Health 2007;12:459–69. 10.1111/j.1365-3156.2006.01788.x [DOI] [PubMed] [Google Scholar]
- 30.Parmar D, Leone T, Coast E, et al. Cost of abortions in Zambia: a comparison of safe abortion and post abortion care. Glob Public Health 2017;12:236–49. 10.1080/17441692.2015.1123747 [DOI] [PubMed] [Google Scholar]
- 31.Prada E, Maddow-Zimet I, Juarez F. The cost of postabortion care and legal abortion in Colombia. Int Perspect Sex Reprod Health 2013;39:114–23. 10.1363/3911413 [DOI] [PubMed] [Google Scholar]
- 32.Saronga HP, Duysburgh E, Massawe S, et al. Efficiency of antenatal care and childbirth services in selected primary health care facilities in rural Tanzania: a cross-sectional study. BMC Health Serv Res 2014;14:96. 10.1186/1472-6963-14-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vlassoff M, Fetters T, Kumbi S, et al. The health system cost of postabortion care in Ethiopia; the health system cost of postabortion care in Ethiopia. Int J Gynecol Obstet 2012;118:127–33. [DOI] [PubMed] [Google Scholar]
- 34.Vlassoff M, Mugisha F, Sundaram A, et al. The health system cost of post-abortion care in Uganda. Health Policy Plan 2014;29:56–66. 10.1093/heapol/czs133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vlassoff M, Musange SF, Kalisa IR, et al. The health system cost of post-abortion care in Rwanda. Health Policy Plan 2015;30:223–33. 10.1093/heapol/czu006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.von Both C, Jahn A, Fleba S. Costing maternal health services in South Tanzania: a case study from Mtwara urban district. Eur J Health Econ 2008;9:103–15. 10.1007/s10198-007-0048-3 [DOI] [PubMed] [Google Scholar]
- 37.Zeng W, Halasa YA, Cros M, et al. Costing essential services package provided by a non-governmental organization network in Bangladesh. Health Policy Plan 2017;32:1375–85. 10.1093/heapol/czx105 [DOI] [PubMed] [Google Scholar]
- 38.Cobos Muñoz D, Hansen KS, Terris-Prestholt F, et al. Matching comprehensive health insurance reimbursements to their real costs: the case of antenatal care visits in a region of Peru. Cost Eff Resour Alloc 2015;13:16. 10.1186/s12962-015-0042-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dalaba MA, Akweongo P, Savadogo G, et al. Cost of maternal health services in selected primary care centres in Ghana: a step down allocation approach. BMC Health Serv Res 2013;13:287. 10.1186/1472-6963-13-287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Entringer AP, Pinto MFT, Gomes MAdeSM. Costs analysis of hospital care for vaginal delivery and elective caesarean section for usual risk pregnant women in the Brazilian unified National health system. Cien Saude Colet 2019;24:1527–36. 10.1590/1413-81232018244.06962017 [DOI] [PubMed] [Google Scholar]
- 41.Hitimana R, Lindholm L, Krantz G, et al. Cost of antenatal care for the health sector and for households in Rwanda. BMC Health Serv Res 2018;18:262 10.1186/s12913-018-3013-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khan A, Zaman S. Costs of vaginal delivery and caesarean section at a tertiary level public hospital in Islamabad, Pakistan. BMC Pregnancy Childbirth 2010;10:2. 10.1186/1471-2393-10-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ilboudo PGC, Greco G, Sundby J, et al. Estimating the costs for the treatment of abortion complications in two public referral hospitals: a cross-sectional study in Ouagadougou, Burkina Faso. BMC Health Serv Res 2016;16:559. 10.1186/s12913-016-1822-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lince-Deroche N, Fetters T, Sinanovic E, et al. The costs and cost effectiveness of providing first-trimester, medical and surgical safe abortion services in KwaZulu-Natal Province, South Africa. PLoS One 2017;12:e0174615. 10.1371/journal.pone.0174615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Odhiambo J, Ruhumuriza J, Nkurunziza T, et al. Health facility cost of cesarean delivery at a rural district hospital in Rwanda using time-driven activity-based costing. Matern Child Health J 2019;23:613–22. 10.1007/s10995-018-2674-z [DOI] [PubMed] [Google Scholar]
- 46.Collins D, Mukunzi JL, Jarrah Z, et al. Rwanda Health Service Costing: Health Centre Analysis. Cambridge, MA, 2011. https://www.msh.org/sites/default/files/rwanda_health_service_costing_-_health_center_analysis.pdf [Google Scholar]
- 47.Blaakman A. Cost Analysis of the Essential Package of Health Services (EPHS) in Somalia. Oxford, 2014. https://assets.publishing.service.gov.uk/media/57a089e8e5274a27b2000305/Somalia-cost-analysis-of-the-essential-package-of-health-services-.pdf [Google Scholar]
- 48.Cros M, Estavien L, Saint Firmi PP, et al. Santé pour le Développement et la Stabilité d Haïti / Pwojè Djanm. Analyse de Coûts du Paquet Minimum des Services de sante (PMS) d’Haïti 2011 [Internet]. Cambridge, MA, 2012. Available: http://docplayer.fr/12478734-Projet-sante-pour-le-developpement-et-la-stabilite-d-haiti-pwoje-djanm-analyse-de-couts-du-paquet-minimum-des-services-de-sante-pms-d-haiti-2011.html#show_full_text
- 49.Conteh L, Walker D. Cost and unit cost calculations using step-down accounting. Health Policy Plan 2004;19:127–35. 10.1093/heapol/czh015 [DOI] [PubMed] [Google Scholar]
- 50.Mogyorosy Z, Smith P. The main methodological issues in costing health care services [Internet]. York; 2005. (CHE Research Paper). Report No.: 7. Available: https://www.york.ac.uk/media/che/documents/papers/researchpapers/rp7_Methodological_issues_in_costing_health_care_services.pdf
- 51.Villar J, Ba'aqeel H, Piaggio G, et al. Who antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet 2001;357:1551–64. 10.1016/S0140-6736(00)04722-X [DOI] [PubMed] [Google Scholar]
- 52.World Health Organization WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization, 2016: 1–172. https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1 [PubMed] [Google Scholar]
- 53.Seidman G, Atun R. Does task shifting yield cost savings and improve efficiency for health systems? A systematic review of evidence from low-income and middle-income countries. Hum Resour Health 2017;15:29. 10.1186/s12960-017-0200-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dawson AJ, Buchan J, Duffield C, et al. Task shifting and sharing in maternal and reproductive health in low-income countries: a narrative synthesis of current evidence. Health Policy Plan 2014;29:396–408. 10.1093/heapol/czt026 [DOI] [PubMed] [Google Scholar]
- 55.World Health Organization Family Planning Evidence Brief – Ensuring adequate financing of family planning commodities and services. Geneva, 2018. https://apps.who.int/iris/bitstream/handle/10665/255863/WHO-RHR-18.26-eng.pdf?ua=1 [Google Scholar]
- 56.Gilson L, Sen PD, Mohammed S, et al. The potential of health sector non-governmental organizations: policy options. Health Policy Plan 1994;9:14–24. 10.1093/heapol/9.1.14 [DOI] [PubMed] [Google Scholar]
- 57.Huber D, Curtis C, Irani L, et al. Postabortion care: 20 years of strong evidence on emergency treatment, family planning, and other programming components. Glob Health Sci Pract 2016;4:481–94. 10.9745/GHSP-D-16-00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Flessa S, Moeller M, Ensor T, et al. Basing care reforms on evidence: the Kenya health sector costing model. BMC Health Serv Res 2011;11:128. 10.1186/1472-6963-11-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Weismann E, Sentumbwe-Mugisa O, Mbonye AK, et al. Uganda Safe Motherhood Programme Costing Study. Geneva, Switzerland, 1999. https://apps.who.int/iris/bitstream/handle/10665/65984/WHO_CHS_RHR_99.9.pdf;jsessionid=3A60E2D9AA61499821332D51DC371546?sequence=1 [Google Scholar]
- 60.McBain RK, Jerome G, Warsh J, et al. Rethinking the cost of healthcare in low-resource settings: the value of time-driven activity-based costing. BMJ Glob Health 2016;1:e000134 10.1136/bmjgh-2016-000134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stenberg K, Hanssen O, Edejer TT-T, et al. Financing transformative health systems towards achievement of the health sustainable development goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health 2017;5:e875–87. 10.1016/S2214-109X(17)30263-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fort AL, Kothari MT, Abderrahim N. Postpartum care: levels and determinants in developing countries. Calverton, Maryland, USA, 2006. https://dhsprogram.com/pubs/pdf/CR15/CR15.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-002371supp001.pdf (756.6KB, pdf)