Abstract
Objective
We investigated user requirements for a smartphone application to coordinate layperson administration of naloxone during an opioid overdose.
Materials and Methods
We conducted interviews and focus groups with 19 nonmedical opioid users and other community members in the Kensington neighborhood of Philadelphia, Pennsylvania, which has one of the highest overdose rates in the country. Data were analyzed using thematic analysis.
Results
We found high levels of trust and reliance within one’s own social group, especially nonmedical opioid users and members of the neighborhood. Participants distrusted outsiders, including professional responders, whom they perceived as uncaring and prejudiced. Participants expressed some concern over malicious use of a location-based application, such as theft when a victim is unconscious, but overall felt the benefits could outweigh the risks. Participants also trusted community-based organizations providing services such as bystander training and naloxone distribution, and felt that a smartphone application should be integrated into these services.
Discussion
Individuals affected by opioid use and overdose reacted positively to the concept for a smartphone application, which they perceived as a useful tool that could help combat the high rate of opioid overdose fatalities in their neighborhood. A sense of unity with others who have shared their experiences could be leveraged to connect willing bystanders with victims of overdose, but risk must be mitigated for layperson responders.
Conclusion
Based on participant experiences with overdoses, trust-based considerations for the design of smartphone applications to facilitate layperson response will be critical for their adoption and use in real overdose situations.
Keywords: smartphone, user-computer interface, opioid-related disorders, drug overdose, social psychology
INTRODUCTION
The opioid epidemic in the United States continues to claim an increasing number of lives every year. Between 2015 and 2017, the total number of opioid-involved deaths increased by 43.8%, from 33 091 to 47 600.1 Of the largest and most populous cities, Philadelphia, Pennsylvania has the highest annual rate of overdose deaths by far, at 46.8 per 100 000 individuals compared to Chicago's 15.4 and New York City's 11.2.2 In addition, thousands of nonfatal drug overdoses each year test Philadelphia's available resources such as hospitals and emergency medical services.2 Allocating resources is further challenged by incomplete mortality data with unclassified overdoses that indicate significant disparities.3
Naloxone, also known by the brand name Narcan, is administered intranasally to reverse an overdose and prevent death.4 Laypersons can administer naloxone as a nasal spray with few medical risks, making it a feasible intervention for wide use by the public.4 Distribution of naloxone has become a significant effort in combating the opioid epidemic. In Philadelphia, considerable resources have been channeled into increasing access to naloxone among those who use drugs and members of their social networks.2
As such efforts are increasing naloxone saturation, coordinating response during overdose events could also improve response times and further reduce deaths. Policy efforts are encouraging the development of smartphone applications to connect laypersons carrying naloxone with nearby overdose events,5 and nascent research is testing such applications. However, little is known about the acceptability or feasibility of these applications from the perspective of potential users.
We elicited user requirements from those with first-hand experience of substance use and overdose toward smartphone applications in this context. We describe their design preferences regarding smartphone-based support for responding to an overdose, which involves the negotiation of trust in one’s peers, community-based organizations, and professional responders.
BACKGROUND AND SIGNIFICANCE
During an opioid-involved overdose, the victim will lose consciousness rapidly, rendering them incapable of sending out a signal for help or self-administering naloxone.6 Bystander intervention is therefore critical, and studies have found that those who witness opioid overdoses are willing to help, whether or not the victim is a stranger.7–9 Similar to other peer-based interventions,10 bystander response to an overdose is effective due to the availability of peers who have a similar lived experience and are therefore motivated to help.11 The majority of individuals receiving and administering naloxone are persons who use drugs,11,12 reflecting a “buddy ethic” among opioid users who “watch out for each other” when using.13 Family members of those who use opioids are also motivated to participate in naloxone training.14 One study found that 74.6% of naloxone administrations were performed on companions or acquaintances.11
One of the primary barriers to assisting an overdose victim is fear of being prosecuted due to association with illicit drug use. Calling 911 is likely to result in the arrival of police along with emergency medical services. In the face of growing evidence that these fears are both common and well-founded,8,9,15,16 naloxone distribution programs struggle to address the fact that community members often do not call 911 to ensure the victim receives proper medical attention and support services.17 Smartphone applications provide a novel mechanism for facilitating effective response, which may make it be possible to avoid interaction with authorities, but perceptions of their risks (eg, arrest, victimization, loss of anonymity) among potential users are unknown. The only smartphone applications that have been tested with this population are those supporting recovery from drug and alcohol dependence.18,19
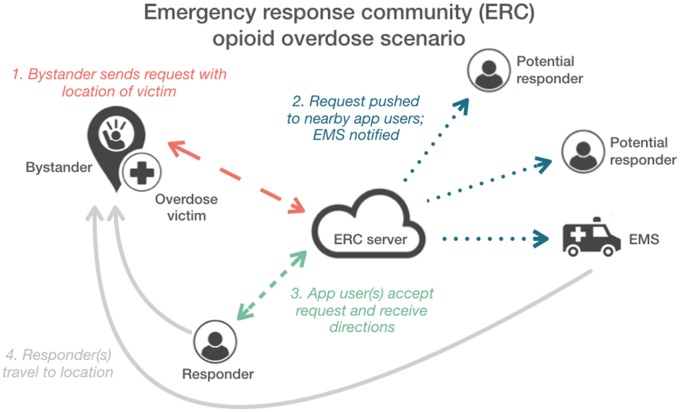
A review of smartphone-based applications showed that response to medical emergencies can include multiple “types of responders with various levels of obligation to help”: caregivers, rescue workers, bystanders, and patient peers.20 Smartphone applications that facilitate layperson response have been tested most extensively for cardiac arrest.21–23 Emergency response communities (ERCs) are a concept based on the ability for laypersons to share life-saving medication, such as epinephrine for anaphylaxis.24 As illustrated in Figure 1, the ERC concept relies on a smartphone application to connect a network of laypersons who carry a particular medication, and coordinate response by mobilizing those within a certain distance to respond to the location during an emergency.24 Modeling with real data from emergency medical services has indicated that a proportion of the time, an ERC would enable bystanders to respond faster than emergency medical services.25
Figure 1.
An illustrated scenario showing how an emergency response community (ERC) can be used to facilitate response to an opioid overdose event. A bystander uses the smartphone application to send a request for help with the location of the victim, and based on that location the server coordinates response by nearby application users.
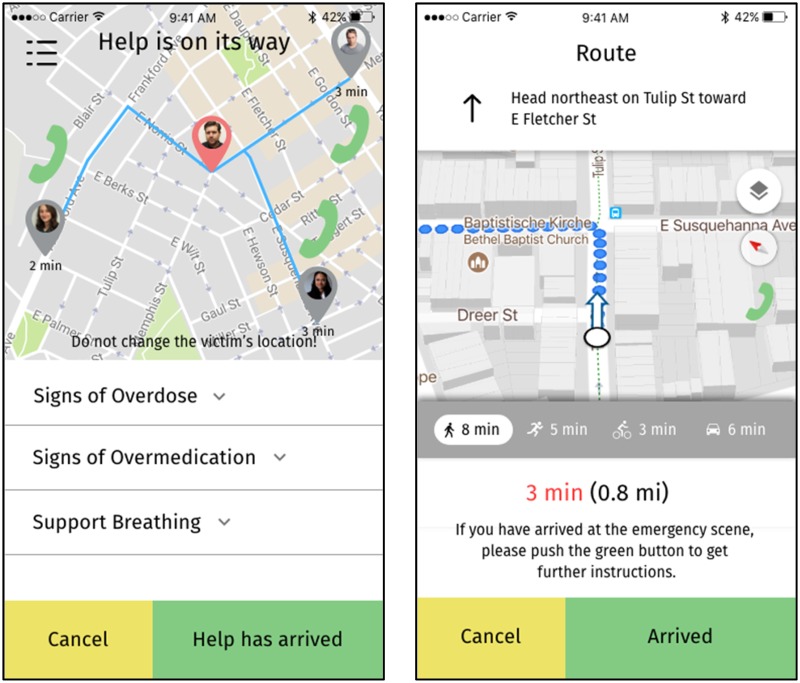
Figure 2.
Sample mockups for a bystander requesting help for an overdose victim (left), and a responder bringing naloxone to the scene of the overdose (right).
This study contributes to literature on user engagement with technology-based interventions. For instance, attrition is high with web-based interventions,26 and those with chronic illnesses may have lower adherence with mobile health devices than healthy individuals.27 In the context of ERCs, engagement involves willingness of users to download the application28 and then use the application to coordinate response to emergencies.29 User engagement with technology involves a complex set of factors including novelty, motivation, control, interactivity, feedback, interruptions, and affect.30 The aim of the present study was to elicit user requirements from those affected by opioid use and overdose, with a focus on acceptability based on the quality metrics of perceived value, information needs, functionality, and security and privacy.31
MATERIALS AND METHODS
Setting
This study was based in the Kensington neighborhood of Philadelphia. This neighborhood (ZIP code 19134) has been among the hardest hit by the opioid crises in the city experiencing 209 reported overdose deaths. This is more than double the proportion reported in the next highest ZIP code.32
Recruitment
Participants were recruited from Prevention Point Philadelphia (n = 11), a harm reduction agency in Kensington that operates the local city-sanctioned syringe exchange program, Angels in Motion (n = 3), a community-based organization that conducts street outreach in Kensington, or through street intercepts (n = 5) in Kensington. Inclusion criteria were owning a smartphone with a data plan, and reporting either (1) misuse of heroin and/or prescription opioids at least 10 times in the past 30 days or (2) knowing active, in recovery, or deceased opioid users.
Procedures
Qualitative interviews (n = 8) and focus groups (n = 3), comprised of 2–3 participants each, lasted between 40 min and 60 min and were conducted by a sociologist (S.L.) with over 2 decades of experience studying substance use. At their conclusion, participants received a $20 cash incentive. These activities took place in a private office within Prevention Point Philadelphia, except for some interviews which were conducted in nearby coffee shops by participant preference.
Questions probed topics on smartphone access and usage trends, experiences with opioids and overdoses, barriers to responding to an overdose, and attitudes toward the use of a smartphone application in the context of response to an opioid overdose. Additionally, participants were asked questions about demographics, for example, age, race/ethnicity, gender, history of drug use, and history of witnessing/experiencing overdose events. To elicit user requirements, we described the concept of a smartphone-mediated ERC and showed participants representative mockups of an ERC for opioid overdoses (see Figure 1). We also described sample scenarios and asked participants what information they would want the application to provide as they are deciding whether to respond (see Table 1).
Table 1.
Sample interview and focus group questions
| Response scenarios | |
| Receiving an alert about an overdose event | You receive an alert on the app at 9 Pm, when you’re home with family or friends. How would you respond? |
| If you were the one responding to an overdose using the app, what kind of information would you want to see about an overdosing victim? Would you want to see a picture of the person? | |
| Responding to the overdose location | You arrive at the location and it appears to be an abandoned building, such as a shooting gallery. What would you do? |
| Would you find it uncomfortable if more than one person showed up to the scene because they were alerted through the app? How about if 911 also showed up to the scene? | |
| General functionality | |
| Sharing personal information | What kind of information about yourself would you be comfortable sharing with others in the app? |
| Do you have any concerns about your geographic location being tracked at all times by the app? | |
| Barriers and facilitators to engagement with app | Do you have any concerns about 911 automatically being called—either if you were the responder or the person signaling the call? |
| Do you think you’d be more or less interested in using the app if it involved some kind of incentives, for example, receive points for responding to an overdose? | |
The research study was approved by the Drexel University IRB and by Prevention Point Philadelphia. In addition, a Certificate of Confidentiality was issued by the NIH to protect the identities of research participants.
Analysis
Qualitative interviews and focus groups were audio recorded, transcribed, and analyzed through inductive thematic analysis.33,34 Five researchers developed initial sets of codes individually. Through discussion, a common set of codes was agreed upon by removing or combining duplicative codes, and preliminary themes were developed. Two researchers (G.M., R.A.) reviewed and revised these themes through a process of data reduction and data complication. The relationship of the themes to trust theory was identified in this process. Final themes were refined and defined by applying Veinot et al’s35 trust-based design framework.
RESULTS
Demographics and experiences
Table 2 shows demographic information for all 19 participants: 11 from focus groups, 8 from interviews. A majority had personal experiences using opioids and overdosing: 13 reported using opioids, for example, heroin, fentanyl, oxycodone, nonmedically, or without a doctor’s prescription within the past 30 days, while 12 reported having overdosed at least once in their lifetime.
Table 2.
Participant demographics
| Total participants | 19 |
| Qualitative interviews | 8 |
| Focus groups | 11 |
| Age | |
| 18–24 | 1 |
| 25–35 | 5 |
| 36+ | 8 |
| Missing | 5 |
| Gender | |
| Female | 9 |
| Male | 10 |
| Race/ethnicity | |
| Black/African-American | 1 |
| Hispanic | 4 |
| White | 14 |
Trust-based design considerations
We found that trust and distrust were issues commonly discussed by all of our participants. Our findings aligned with Veinot et al’s35 research on how distrust in institutions and authority among underserved populations should inform the design of informatics-based public health interventions. Therefore, we use Veinot et al’s trust-centered design framework to interpret and report our findings with regard to: personal and group trust, technological trust, and institutional trust (see Table 3).
Table 3.
Trust-based considerations related to opioid overdose response
| Personal and group trust | |
| Shared experiences | “I may run into, every day, about two people that overdose. It's just every day.” |
| Peers | “They're out there, they're using. They can save each other, and they do… I’ve seen it happen more than once. And I talk to them, and they tell me, they're ready to help each other.” |
| Sharing naloxone | “I have one gentleman in particular… who has over 40 [saves]… he never looks at it like this is my dose. He looks at it like that's a life. And a lot of people on the street, that's how they look at it.” |
| “Euphoria, you know, [saving someone] makes you feel good. Just knowing that something that I prepared for came through, you know what I mean? Like, just to take that precaution.” | |
| Shared responsibility | “I wish somebody would do it for me if the roles were reversed.” |
| “Yeah [multiple responders] would actually be way more comfortable, because all the responsibility is not on you … and maybe one of those people knows CPR.” | |
| Responder safety | “You don't know who's in there or what is going to happen. I don't know if somebody will try to stab you when you're walking in, because you got money on you.” |
| “They get pissed off. They really get pissed off, because you’re blowing their high … and some of them don’t really want to come out of there.” | |
| Technological trust | |
| Naloxone efficacy | “I wish that everybody in the community had [naloxone]… Like how they have fire extinguishers. That it was available for them all.” |
| “I’ve brought back people that I’m very close to. I look at them now and I’m like, wow, look at you now. Look at what naloxone gave you. Look at you.” | |
| Application misuse | “People knowing exactly where you are, and predators who rob people and stuff would know exactly where you are. That would be bad. Because say you’re at your family’s house or something, and then somebody knows exactly where your family lives, and can roll up on you.” |
| “That's one of the concerns I would have. I wouldn't want to be set up to being robbed or anything like that.” | |
| Social stigma | “If you put your picture on there, then that's pretty much openly saying that you use heroin… which could be detrimental.” |
| Social influence | “If people see that… look you weren't called this month, but this many calls came in, this many people went out, and this many people were helped. That could really be an incentive to say, ‘Oh, I'm part of something that’s working’.” |
| Trauma exposure | “I think it could affect some people. Especially if now they have the app, maybe people down here don’t see overdoses, but … they’re going to see a lot of them, if they have the app.” |
| Institutional trust | |
| Community-based programs | “Well, I been coming… [to] Prevention Point for, like, 20 years I guess… I use as many of their services as I can.” |
| “The app should have … a system that would teach you about the [naloxone] training. Better yet, somewhere they can go to a one-course class of how the [naloxone] can be administrated, and that would help them out a whole lot.” | |
| Risk of prosecution | “If somebody has warrants, they're probably going to get taken away even though there is a Good Samaritan law.” |
| “When I overdosed, my friend that was with me, even though there’s a Good Samaritan law, my friend had warrants out for his arrest. And they asked him his name, looked him up in the system, and actually took him to get processed.” | |
| Perceived neglect | “The cops don't even [care] down here. They'll let you die.” |
| Professional response | “I would definitely like emergency medical services to be there. Police, not so much.” |
| “I think it’s always better that emergency medical services comes because I would like them to go to the hospital, and I’d like them to get treatment. So if they’re not there, there’s not even that opportunity for them to go. So I would definitely like emergency medical services to be there. Police, not so much. But emergency medical services definitely.” | |
Personal and group trust
The highest level of trust expressed by participants was interpersonal trust within their own social group, especially nonmedical opioid users and members of their neighborhood community. They perceived outsiders as uncaring and prejudiced, and therefore felt the need to rely on those within the group to protect one another. Participants trusted word of mouth within the group to learn about harm reduction strategies, overdose risks, and how to respond to an overdose. They also trusted those within the group during their most vulnerable moments, asking one another to watch over them while they used, in case they overdosed. Despite carrying a limited supply of naloxone, participants were not selective about choosing on whom they would use it, because they trusted others within the group to do the same for them or a loved one.
Some distrust within group stemmed from the risks common in an environment so deeply affected by opioid use. Participants reported that theft is not uncommon while an overdose victim is unconscious, and bartering with naloxone had also been witnessed. One participant admitted that she would find it difficult to restrain herself from checking an unattended overdose victim's pockets. Victims who are revived can also be aggressive due to the effects of naloxone.
Technological trust
Participants trusted naloxone as the most effective method of responding to an overdose. They generally supported the concept of a smartphone application that facilitates bystander administration of naloxone because they perceived an application as a useful tool that could help combat the high rate of opioid overdose fatalities in their neighborhood.
Participants compared the concept to Uber's ride-sharing model, which indicated how a smartphone application as a mediator could affect trust within the group. Based on this comparison, for example, one participant felt that responders should also be paid for their service, in accordance with the sharing economy. Many participants felt strongly that they would be most motivated by saving someone's life, and that responders should not seek or be provided any other incentives to respond to an overdose.
Location-based applications were a concern to participants because they posed a risk for surveillance of illicit drug activity. However, in the context of responding to overdoses many participants felt the benefits could outweigh the risks. In addition, concerns about theft were amplified because location-based applications could be misused to seek out vulnerable overdose victims.
Institutional trust
Participants characterized the most prevalent barrier to responding to an overdose as the risk of coming into contact with police or other professional responders, whom they did not trust to be concerned with the well-being of nonmedical opioid users. Some participants felt comfortable with the presence of professional responders, trusting their ability to control the situation and provide necessary medical assistance. Emergency medical services were generally preferred over police, due to a perception that they were more compassionate responders.
In contrast, Prevention Point and other community-based organizations were trusted sources of support for coping with daily exposure to the amount of opioid use, overdoses, and deaths concentrated in the neighborhood of Kensington. Participants trusted services such as needle exchange, bystander training, naloxone distribution, social support, and housing support. During focus group discussions, for example, some participants recommended services to each other.
Design preferences for smartphone applications
Integration into community
Participants reacted positively to the idea of integrating a smartphone application for bystander intervention with existing services provided by a community-based organization such as Prevention Point. Overdose reversal training could serve as an entry point to installing an application, helping to establish trust among users of the application including potentially vetting them as potential responders. Community-based organizations also provide important social and emotional support. Participants expressed concerns that smartphone-based notifications could increase exposure to or even awareness of overdoses, which risks further traumatization of community members: “I think it could affect some people. Especially if now they have the app … they're going to see a lot of [overdoses]” (Jennifer). However, participants felt that an application could support emotional resilience and mental health of community members by facilitating online social support, as well as in-person connection within their neighborhood.
Functionality
Participants considered the potential advantages and disadvantages of a smartphone application mobilizing multiple bystanders to respond to a single overdose. They noted that multiple doses of naloxone are sometimes required to revive a victim, and a responder may only carry one dose. Some participants suggested that the safety concerns associated with responding to an unsafe area could be alleviated if they were not alone when responding to an incident. Participants such as Allen felt that multiple responders would be more effective: “yeah multiple responders would actually be way more comfortable, because all the responsibility is not on you… and then there is other people trying to help at the same time.” However, other participants such as Paul thought that adding responders may not be more helpful for the victim: “you don't want to have too many people because everybody thinks they know everything, and now we're all arguing—listen, we're here to do one thing—to save this person's life.” Overall, about half of all participants expressed a preference for mobilizing multiple responders for a given incident.
Some participants expressed concerns that a smartphone application could be misused, for example, helping to identify overdose victims or responders who are vulnerable to theft or violence. Ensuring that users of an application are not exposed to increased risk of theft or violence, and that trust can be promoted among community members, were key prerequisites to implementation of a smartphone application in this context. For example, privacy and accountability mechanisms would be needed to discourage misuse while providing peace of mind to earnest responders. Participants preferred that a smartphone application be able to infer the motives of its users, and only notify potential responders who have been vetted for good intentions.
There are also opportunities to provide support for a responder while they attend to an overdose victim, and after an overdose event. Participants had the expectation that any responders a smartphone application would reach are trained and prepared to intervene. The application should therefore confirm that a potential responder has a dose of naloxone with them before they confirm that they are en route. In addition, participants supported providing reminders of what to do (eg, how to administer naloxone, how to perform CPR) and what not to do (eg, try to slap the victim awake, leave the victim unattended). Participants reported that slapping a victim in an effort to revive them is a misguided but sometimes still employed method during response to an overdose. After an overdose, a smartphone application could also remind the responder to refill their supply of naloxone, including identifying nearby suppliers using their location (eg, by plotting them on a map, listing them by proximity, or providing directions).
Interaction design
If participants were to be notified of an overdose event and needed to make a decision about responding, they wanted clear information about the location and context of the overdose. Making an informed decision about responding primarily involved understanding to what extent they were putting their safety at risk: “That’s one of the concerns I would have, I wouldn’t want to be set up to being robbed or anything like that” (Paul). Understanding the type of area they were responding to was therefore an important consideration in order to know who else they may be likely to encounter. As mentioned, some participants felt that safety concerns could be alleviated by mobilizing multiple responders to the same incident, so a smartphone application could indicate when other trusted responders were on their way or on-site. The ability to share information and communicate directly with the bystander was also recommended by participants, as this could alleviate difficulties stemming from poor location accuracy and enhance situational awareness.
Participants were largely opposed to a smartphone application incentivizing response to overdoses, which indicates that the approach of gamification would not be appropriate in this context. They described their personal motivation to respond to an overdose as solely related to the potential for saving a life, and preferred that an application only reinforce this type of motivation. To this end, interaction design could focus behavioral reinforcement on the ideas of helping others and one’s community. For example, Samuel suggested that sharing application-wide progress may be encouraging to application users even if they are personally not able to respond: “If people see that… look you weren't called this month, but this many calls came in, this many people went out, and this many people were helped. That could really be an incentive to say, ‘Oh, I’m part of something that’s working’.” Using social influence could therefore provide an appropriate incentive to participation, while also potentially providing a more optimistic outlook on the opioid epidemic in one’s community.
DISCUSSION
Our findings show the importance of trust among members of a community deeply affected by opioid use. Community members in our study represent a range of lived experiences—including active opioid users, individuals in recovery from opioid use, those with loved ones who use opioids, and those who have reversed a stranger’s overdose. By including a range of perspectives from the Kensington neighborhood of Philadelphia, we contribute community-based considerations for the complex public health problem of the opioid epidemic. In contrast to a trust-based study with a different underserved population,35 which found that institutional benevolence was questioned, we found that some of the highest and lowest levels of trust were directed toward institutions. Since high levels of institutional mistrust have been shown to have a negative effect on well-being,36 it is important to mediate these effects, for example by applying community-based participatory research approaches37 to developing smartphone applications.
Efforts to prevent opioid overdose fatalities occur within sociotechnical systems of emergency response and community-based support. We found that trust concerns significantly influence how community members navigate sociotechnical systems in responding to an overdose, and smartphone applications have the potential to exacerbate or mediate these issues. For example, bystanders avoid calling 911 due to a distrust of police, and a fear that they or others will be arrested despite the existence of Good Samaritan laws. We found that the idea of a smartphone application facilitating peer-based response to an overdose is therefore appealing to community members. However, community-based organizations have already raised concerns that overdoses are going unreported and victims may not receive adequate medical attention and services.17 Integrating a smartphone application with highly trusted community-based programs, such as naloxone training and distribution, may help to address this aversion to interacting with police, and a mediated reporting mechanism could be explored. We found that community members were supportive of a smartphone application encouraging use of these community-based services.
Community members’ distrust of institutions such as professional emergency responders, and the perception that outsiders’ prejudice renders them less helpful to overdose victims, also enhanced their reliance on one another. Trust was high in one’s peer groups, such as fellow opioid users or members of their neighborhood community, and we found a deep camaraderie similar to that of other studies focused on the design of smartphone applications for a marginalized population.38 In light of the strong motivators for intervening among one’s ingroup, a collaborative smartphone application could be empowering for marginalized communities. Strategies from social computing could be used to promote a shared identity, social support, or social capital. For example, willingness to respond to a peer’s medical emergency has been shown to be highly correlated with shared identity.20 In a two-center (Germany-Israel) study of factors influencing the willingness to respond to peers’ anaphylaxis emergency event by allergy patients carrying epinephrine auto-injectors, results of scenario-based simulations showed the importance of social cohesion amongst participants, concluding that “being coincidentally in proximity is not as effective as feeling you belong to a community group.”20 These findings, in addition to our own, suggest that interaction design could be used to promote ingroup shared identity as a way to facilitate bystander intervention.
At the same time, participants’ concerns about a smartphone application tracking their location stemmed from some distrust of fellow community members. In a community deeply affected by opioid use, theft is commonplace, and bartering with naloxone was even reported. Privacy and protection from surveillance were concerns related to one’s own community members misusing a smartphone application, with the risk of theft or assault. Interestingly, despite a distrust of police, participants made no mention of their location data possibly being obtained by law enforcement. Bailey reports 10 918 requests by law enforcement for information about users from Google and YouTube, and over 1.3 million requests for wireless carriers' subscribers' information.39 This represents an important ethical consideration during design and development, which remains the responsibility of developers. Techniques for preserving privacy while using location-based services should be explored,40,41 and future work should elicit community member preferences for how their privacy will be protected.
Some of our findings can be explained by what Vollhardt describes as “altruism born of suffering,” or prosocial behavior that originates from traumatic experiences and oppression.42 In contrast to the belief that prosocial behavior is caused by positive life experiences, this view of altruism explains how individuals can be motivated to help others as a result of their own pain and suffering. The altruism exhibited by community members affected by the opioid epidemic suggests that supportive smartphone applications could amplify prosocial behavior to facilitate effective bystander intervention. However, participants described several types of risks that responders would be exposing themselves to, so smartphone applications should be transparent about these during decision-making, and protect privacy and safety of responders.
Limitations
Our study was focused on understanding past experiences with overdoses, and scenario-based elicitation with regard to the likelihood of response in the future. This attitudinal focus therefore cannot predict future behavior. During this process, we found it particularly difficult to ascertain all barriers to responding to an overdose, because a discussion around saving a person's life is laden with social, moral, and emotional associations. At times participants were likely responding in a socially desirable manner. Therefore, experimental and deployment studies should be used to understand actual behavior during an overdose event.
Our inclusion criteria limited our participants to individuals who owned smartphones with data plans, so that they could reflect on how those could be applied to opioid overdose response. Exploring acceptability of this type of intervention with a broader range of individuals could help us understand additional barriers to participation, and investigate feasibility of wider user engagement. Our inclusion criteria also aimed to combine the perspectives of those individuals who would be most likely to encounter opioid overdoses in their daily lives: those who reported misuse of heroin and/or prescription opioids in the past 30 days, and those who did not, but knew someone who had a history of opioid use. However, our study design did not explore similarities or differences in attitudes across these 2 groups.
Our analysis was limited to the Kensington neighborhood of Philadelphia. Many of our participants were involved with Prevention Point Philadelphia in some capacity, whether as a client or volunteer. Future work will utilize other recruitment approaches to include additional perspectives. In addition, many other communities around the United States are also struggling with the opioid epidemic. Some of our findings related to social and emotional factors may apply to other neighborhoods, but future studies should examine geographic and cultural factors.
CONCLUSION
Combating the opioid epidemic, a complex public health issue, requires a range of complementary approaches. Distributing naloxone in communities and training bystanders to respond to overdoses is a promising short-term strategy for curbing unprecedented rates of overdose fatalities. Smartphone applications are a novel medium for facilitating naloxone distribution and administration, and policy efforts are encouraging their development. To inform the design of these smartphone applications, we contribute trust-based considerations of community members such as nonmedical opioid users and individuals who have experience administering naloxone. We have also extended prior research on smartphone-based facilitation of layperson response to medical emergencies, by examining a new application domain, alerting and locating individuals carrying naloxone to respond to an overdose. Our findings indicate that future work on these applications could help communities that have experienced trauma. In addition, we expand the potential for smartphone applications to support treatment and recovery from substance abuse, by reaching active opioid users who may not have access to treatment, or may not be motivationally ready to enter treatment.
FUNDING
The research presented in this manuscript is that of the authors and does not reflect the official policy of the National Institutes of Health. Development of this manuscript was supported by a grant from the National Institute on Drug Abuse (NIDA): R34DA044758-01.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to this work.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Centers for Disease Control and Prevention. Multiple Cause of Death 1999-2017 on CDC WONDER Online Database, 2018. http://wonder.cdc.gov. Accessed April 3, 2019.
- 2.Mayor’s Task Force. The Mayor’s Task Force to Combat the Opioid Epidemic in Philadelphia: Final Report & Recommendation, 2017. http://dbhids.org/wp-content/uploads/2017/05/OTF_Report.pdf Accessed July 20, 2019.
- 3. Boslett AJ, Denham A, Hill EL, et al. Unclassified drug overdose deaths in the opioid crisis: emerging patterns of inequity. JAMIA 2019; 26 (8–9): 767–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Doe-Simkins M, Walley AY, Epstein A, et al. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health 2009; 99 (5): 788–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Food and Drug Administration. FDA Launches Competition to Spur Innovative Technologies to Help Reduce Opioid Overdose Deaths. 12 September 2016. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm520945.htm.
- 6. Neale J, Bradford J, Strang J.. Development of a proto‐typology of opiate overdose onset. Addiction 2017; 112 (1): 168–75. [DOI] [PubMed] [Google Scholar]
- 7. Strang J, Best D, Man LH, et al. Peer-initiated overdose resuscitation: fellow drug users could be mobilised to implement resuscitation. Int J Drug Policy 2000; 11 (6): 437–45. [DOI] [PubMed] [Google Scholar]
- 8. Richert T. Wasted, overdosed, or beyond saving—to act or not to act? Heroin users’ views, assessments, and responses to witnessed overdoses in Malmö, Sweden. Int J Drug Policy 2015; 26 (1): 92–9. [DOI] [PubMed] [Google Scholar]
- 9. Lankenau SE, Wagner KD, Silva K, et al. Injection drug users trained by overdose prevention programs: responses to witnessed overdoses. J Community Health 2013; 38 (1): 133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bagnall AM, South J, Hulme C, et al. A systematic review of the effectiveness and cost-effectiveness of peer education and peer support in prisons. BMC Public Health 2015; 15 (1): 290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rowe C, Santos GM, Vittinghoff E, et al. Predictors of participant engagement and naloxone utilization in a community‐based naloxone distribution program. Addiction 2015; 110 (8): 1301–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wheeler E, Jones TS, Gilbert MK, et al. Opioid overdose prevention programs providing naloxone to laypersons—United States, 2014. MMWR Morb Mortal Wkly Rep 2015; 64 (23): 631.. [PMC free article] [PubMed] [Google Scholar]
- 13. Lagu T, Anderson BJ, Stein M.. Overdoses among friends: drug users are willing to administer naloxone to others. J Subst Abuse Treat 2006; 30 (2): 129–33. [DOI] [PubMed] [Google Scholar]
- 14. Bagley SM, Peterson J, Cheng DM, et al. Overdose education and naloxone rescue kits for family members of individuals who use opioids: characteristics, motivations, and naloxone use. Subst Abus 2015; 36 (2): 149–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Clark AK, Wilder CM, Winstanley EL.. A systematic review of community opioid overdose prevention and naloxone distribution programs. J Addict Med 2014; 8 (3): 153–63. [DOI] [PubMed] [Google Scholar]
- 16. Tobin KE, Sherman SG, Beilenson P, et al. Evaluation of the Staying Alive programme: training injection drug users to properly administer naloxone and save lives. Int J Drug Policy 2009; 20 (2): 131–6. [DOI] [PubMed] [Google Scholar]
- 17. Faulkner-Gurstein R. The social logic of naloxone: peer administration, harm reduction, and the transformation of social policy. Soc Sci Med 2017; 180: 20–7. [DOI] [PubMed] [Google Scholar]
- 18. McTavish FM, Chih MY, Shah D, Gustafson DH.. How patients recovering from alcoholism use a smartphone intervention. J Dual Diagn 2012; 8 (4): 294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gustafson DH, McTavish FM, Chih MY, et al. A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry 2014; 71 (5): 566–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gaziel-Yablowitz M, Schwartz DG.. A review and assessment framework for mobile-based emergency intervention apps. ACM Comput Surv 2018; 51 (1): 1. [Google Scholar]
- 21. Brooks SC, Simmons G, Worthington H, et al. The PulsePoint Respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: challenges for optimal implementation. Resuscitation 2016; 98: 20–6. [DOI] [PubMed] [Google Scholar]
- 22. Elsner J, Meisen P, Thelen S, et al. EMuRgency—a basic concept for an AI driven volunteer notification system for integrating laypersons into emergency medical services. Int J Adv Life Sci 2013; 5 (3): 223–36. [Google Scholar]
- 23. Sakai T, Iwami T, Kitamura T, et al. Effectiveness of the new ‘Mobile AED Map’to find and retrieve an AED: a randomised controlled trial. Resuscitation 2011; 82 (1): 69–73. [DOI] [PubMed] [Google Scholar]
- 24. Schwartz D, Bellou A, Garcia-Castrillo L, et al. Exploring mHealth participation for emergency response communities. Australas J Inform Syst 2017; 21. [Google Scholar]
- 25. Khalemsky M, Schwartz DG.. Emergency response community effectiveness: a simulation modeler for comparing emergency medical services with smartphone-based Samaritan response. Decis Support Syst 2017; 102: 57–68. [Google Scholar]
- 26. Christensen H, Mackinnon A.. The law of attrition revisited. J Med Internet Res 2006; 8 (3): e20.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shaw RJ, Steinberg DM, Bonnet J, et al. Mobile health devices: will patients actually use them? J Am Med Inform Assoc 2016; 23 (3): 462–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Khalemsky M, Schwartz DG, Silberg T, et al. Willingness to join a smartphone-based emergency response community: evidence from a field study. JMIR Mhealth Uhealth 2019; 7 (8): e13892.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gaziel-Yablowitz M, Dolle S, Schwartz DG, et al. Proximity-based emergency response communities for allergy patients at risk of anaphylaxis: behavioral decision factors and design considerations for patients’ participation, JMIR Mhealth Uhealth 2019; 7 (8): e13414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. O'Brien HL, Toms EG.. What is user engagement? A conceptual framework for defining user engagement with technology. J Am Soc Inf Sci 2008; 59 (6): 938–55. [Google Scholar]
- 31. Nouri R, R Niakan Kalhori S, Ghazisaeedi M, et al. Criteria for assessing the quality of mHealth apps: a systematic review. J Am Med Inform Assoc 2018; 25 (8): 1089–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Philadelphia Department of Public Health Opioid Program. Incidence of Overdose Deaths in Philadelphia by Zip Code, 2017. https://public.tableau.com/profile/pdph#!/vizhome/UnintentionalDrugRelatedDeaths/UnintentionalDrugRelatedDeaths Accessed April 3, 2019.
- 33. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol 2006; 3 (2): 77–101. [Google Scholar]
- 34. Braun V, Clarke V.. What can “thematic analysis” offer health and wellbeing researchers? Int J Qual Stud Health Well-Being 2014; 9: 26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Veinot TC, Campbell TR, Kruger DJ, et al. A question of trust: user-centered design requirements for an informatics intervention to promote the sexual health of African-American youth. J Am Med Inform Assoc 2013; 20 (4): 758–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hudson J. Institutional trust and subjective well‐being across the EU. Kyklos 2006; 59 (1): 43–62. [Google Scholar]
- 37. Unertl KM, Schaefbauer CL, Campbell TR, et al. Integrating community-based participatory research and informatics approaches to improve the engagement and health of underserved populations. J Am Med Inform Assoc 2015; 23 (1): 60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Marcu G, Dowshen N, Saha S, et al. TreatYoSelf: empathy-driven behavioral intervention for marginalized youth living with HIV. In: Proceedings of the International Conference on Pervasive Computing Technologies for Healthcare; Cancun, Mexico: 63190: IEEE; 2016: 69–76.
- 39. Bailey KD. Watching me: the war on crime, privacy, and the state. UC Davis Law Rev 2013; 47: 1539–89. [Google Scholar]
- 40. Goldenholz DM, Goldenholz SR, Krishnamurthy KB, et al. Using mobile location data in biomedical research while preserving privacy. J Am Med Inform Assoc 2018; 25 (10): 1402–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gupta R, Rao UP.. An exploration to location based service and its privacy preserving techniques: a survey. Wireless Pers Commun 2017; 96 (2): 1973–2007. [Google Scholar]
- 42. Vollhardt JR. Altruism born of suffering and prosocial behavior following adverse life events: a review and conceptualization. Soc Just Res 2009; 22 (1): 53–97. [Google Scholar]