Abstract
Objective
Serious health games might have the potential to prevent tobacco smoking and its health consequences, depending on the inclusion of specific game elements. This review aimed to assess the composition of serious games and their effects on smoking initiation prevention and cessation and behavioral determinants.
Materials and Methods
We systematically searched MEDLINE, Embase, PsycINFO, and Web of Science for publications that evaluated serious games aimed at changing smoking behavior or behavioral determinants. A taxonomy by King et al was used to classify game elements.
Results
We identified 15 studies, evaluating 14 unique serious games. All games combined multiple game elements (mean 5.5; range, 3-10). Most frequently used were general and intermittent rewards, theme and genre features, and punishments. Six studies on smoking prevention together assessed 20 determinants and found statistically significant positive effects for 8 determinants (eg, attitude, knowledge, intention). Of 7 studies on smoking cessation, 5 found positive, statistically significant effects on smoking cessation or status. These studies found statistically significant positive effects for 6 of 12 determinants (eg, self-efficacy, attitude, intention). The majority of included studies had poor or fair methodological quality, lacked follow-up measures, and had fixed (as opposed to free, on-demand) play sessions.
Conclusions
Serious games included multiple types of game elements. The evidence from a number of studies suggests that games may have positive effects on smoking-related outcomes, particularly smoking cessation. However, as most studies had important methodological limitations, stronger designs are needed to demonstrate, quantify, and understand the effects of serious games.
Keywords: serious games, game elements, smoking prevention, smoking cessation, smoking initiation, systematic review
INTRODUCTION
Serious games, defined as games with a primary purpose other than pure entertainment,1 evolved rapidly in the last decade.2 Such games can be used to educate, communicate, and improve health.2 The latter can target disease prevention, diagnosis, management, and treatment in a great variety of health behaviors and diseases.3 Previous reviews suggested that serious games had small positive effects on health-related behaviors and their determinants.4 For example, exergaming, which requires rigorous physical exercise, was effective in increasing or substituting physical activity in adults in the short term,5 and to decrease childhood obesity.6 Similarly, serious games were found to be effective in psychotherapy7 and showed positive effects on determinants of sexual health behavior.8
While many studies have assessed the overall effectiveness of serious games, the composition of serious games (ie, inclusion of game elements) is mostly unattended. Serious games commonly combine a series of game elements, which are features that are “found in most (but not necessarily all) games, readily associated with games, and found to play a significant role in gameplay.”9 Many of such elements bear correspondence with behavior change techniques or learning mechanisms,10,11 such as feedback, rewards, and social influences. Specific game elements may strengthen players’ engagement, feelings of progress, and motivation to finish.12
Serious games have been used increasingly to prevent initiation among adolescents or to motivate and support adult smokers to quit smoking. Yet, no review has systematically assessed the cumulated evidence regarding the effects of serious games on smoking-related outcomes, including the strength of such evidence. In addition, there is no systematic overview of which game elements are included in serious games. This review addressed the following 2 specific objectives: (1) assess what game elements are included in serious games aimed at smoking prevention and cessation and (2) assess the effects of those serious games on smoking-related outcomes.
MATERIALS and METHODS
We registered our systematic review protocol a priori in the PROSPERO register (ID CRD42018097430) and we followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for reporting our systematic review.
Inclusion and exclusion criteria
We searched for original research articles that evaluated serious games targeting tobacco smoking prevention, cessation, or behavioral determinants. We structured our inclusion and exclusion criteria according to the PICOS (Population, Interventions, Comparisons, Outcomes, Study designs) model. Regarding population, we included all populations; thus, no specific populations were excluded in this review. Regarding interventions, we included serious games (ie, games with a primary purpose other than pure entertainment)1 and excluded other games, as well as interventions lacking game elements. We included studies with a serious game as intervention targeting tobacco smoking (eg, cigarettes, cigars, pipes), whereas studies on smokeless tobacco (eg, sucking, chewing, and snuffing tobacco) or on substances other than tobacco (eg, cannabis) were excluded. We included both digital and analog games. Regarding comparisons, we included all comparisons; thus, no specific comparisons were excluded in this review. Regarding outcomes, we included studies that evaluated effects of a serious game on smoking-related outcomes and excluded studies only reporting usability evaluations and player experiences. Regarding study designs, we included studies with the following research designs: randomized controlled trials (RCTs), nonrandomized trials, before-after studies without a control group, case-control studies, and cohort studies.
Moreover, we included only 1 study (most comprehensive one) when multiple studies on the same serious game in the same population were found. We included studies in English or Dutch and excluded studies in other languages. We did not apply restrictions on publication year.
Search strategy
Two reviewers (M.E.D., S.v.S.) and a librarian (J.G.D.) systematically searched MEDLINE, Embase, PsycINFO, and Web of Science from inception for relevant published articles. Web of Science includes all ACM Digital Library and IEEE Xplore publications. The World Health Organization International Clinical Trials Registry Platform and Cochrane Library intervention databases were searched to identify (un)published trials, articles, interventions, or reviews. The search was complemented with hand-searching studies in relevant reviews as well as snowballing by means of searching for relevant studies in the reference list of included articles. The search query mainly combined the concept of serious games with the concepts of smoking and health promotion (see Supplementary Appendix A for the full search query). Conceptually, the systematic search strategy can be summarized as follows: (([serious gaming] and ([health promotion] OR [effect measures])) NOT [animal studies]) OR [trials]. In order to enhance precision of search results, we used VOSviewer to visually identify potentially irrelevant terms eligible for NOTing out in our search strategy. This led to disambiguation (eg, excluding irrelevant records on “game” as in “wild game”).13,14 Other than these terms, we have been highly conservative with narrowing our search strategy based on terms that showed up in the VOSviewer word cloud. See Supplementary Appendix B for the corresponding VOS network visualization.
Study selection
After removing duplicates, 2 reviewers (S.v.S., M.E.D.) independently screened studies based on title and abstract and assessed the remaining articles full text for eligibility. Rayyan QCRI (Rayyan, Doha, Qatar) and EndNote (Clarivate Analytics, Philadelphia, PA) were used for screening and data management. Interrater reliability was assessed before a consensus meeting to discuss any disagreements. If no consensus was reached, a third reviewer (M.P.F.) was consulted. Interrater reliability of the screening based on the title and abstract resulted in moderate agreement (Cohen’s kappa = 0.44) and the interrater reliability of the screening based on the full text resulted in moderate agreement (Cohen’s kappa = 0.5).
Quality appraisal
Two reviewers (M.E.D, M.P.F.) independently appraised the quality of each included study by using the most suitable tools of the Study Quality Assessment Tools of the National Institutes of Health.15 Studies were not excluded based on the quality assessment. Quality appraisal yielded a substantial agreement (Cohen’s kappa = 0.67). Interrater reliability was assessed before a consensus meeting in which reviewers discussed, determined, and reported the methodological strength of each study. If no consensus was reached, a third reviewer (S.v.S.) was consulted.
Data extraction and synthesis
A data extraction form was developed based on the Cochrane data collection form for RCTs and non-RCTs.16 The form was pilot-tested on the first 5 studies and adjusted where needed. Two authors (M.E.D., S.v.S.) extracted data in parallel and then checked results against each other. Any disagreements were discussed, and consensus was reached without the need of a third reviewer (M.P.F.). The following items were extracted: full reference, country, study design, setting, participant characteristics, interventions (serious game) characteristics, included game elements, and measures and effects on smoking-related outcomes. We classified the effects as positive (ie, outcomes improved), negative (ie, outcomes worsened), no difference (ie, outcomes did not change or barely changed), or mixed (ie, outcomes both improved and worsened), as well as the statistical significance for each of these effects (if reported).
Game elements were extracted using a taxonomy of game elements by King et al,17 after using 3 different taxonomies11,17,18 for the first 5 studies. This taxonomy was selected as the most relevant taxonomy since all game elements could be categorized in 5 categories: (1) narrative and identity features (eg, interactive storytelling), (2) social features (eg, social aspects of game playing), (3) manipulation and control features (eg, user input influencing in-game outcomes), (4) reward and punishment features (eg, the ways in which players win and lose in video games), and (5) presentation features (eg, the visual and auditory presentation of video games). Every category consists of multiple subfeatures.
Corresponding authors of included studies were contacted twice with a request for additional materials detailing the intervention content when no published materials were available. When not available or no response was received, the intervention description in the published included article was used.
RESULTS
Study inclusion
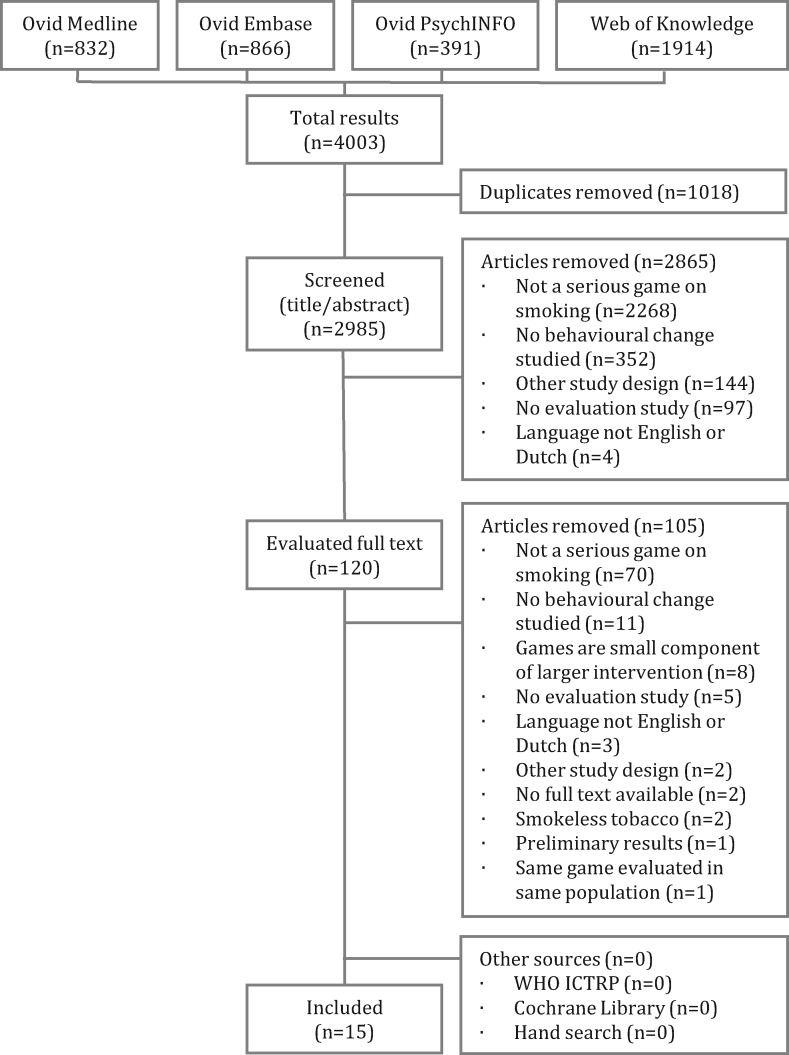
Our PRISMA flow diagram (see Figure 1) shows that the database search yielded 4003 results, including 1018 duplicates. After removal of duplicates, 2985 articles were screened based on title and abstract. We excluded 2865 studies in this screening, mainly because the studies did not report on a serious game as intervention for smoking prevention or cessation. The remaining 120 studies were evaluated as full text. Hereafter, we excluded 105 studies, and once more, the main reason for exclusion was that the studies did not report on a serious game. No studies were added from other sources, resulting in the inclusion of 15 studies in total, evaluating 14 unique serious games.
Figure 1.
PRISMA flow diagram. ICTRP: International Clinical Trials Registry Platform; WHO: World Health Organization.
Study characteristics and quality
Table 1 presents details on study characteristics. All studies were in English and published from 2008 to 2018, except 1 study published in 1999.29 The majority of studies were conducted in North America (n = 11), with the other studies conducted in Europe (n = 4). Seven studies were (randomized) controlled trials, 5 were pre-post studies, 2 studies had a between- or within-subjects factorial design,32,33 and 1 was a cross-sectional study.21 If reported, the clinical and laboratory setting were most common, followed by “not bound to a setting,” and school setting. The target populations were children, adolescents or young adults in 40% of the studies, and the remaining studies covered a broad age range. Sample sizes ranged from 25 to 1698, in which two-thirds of the studies had 25-91 participants. Except for 1 study that only studied women25 all studies included both women and men, with 1 study not reporting on gender.33 Six of 7 studies that reported race and ethnicity included a mixture of races and ethnicities. The 5 studies that reported on educational level included both participants that attended high school or lower education and participants that attended college or university. The mean smoked cigarettes per day was 17.76 among the 7 studies that reported this. Last, study quality scores (good, fair, poor) were evenly distributed over studies (see Supplementary Tables 1-3). Most studies scored fair or poor due to unreported information that is crucial to determine methodological quality, sample sizes that would not detect effects with enough power, high dropout or loss to follow-up, and unblinded stakeholders.
Table 1.
Study characteristics
| Study | Quality scorea | Country | Design | Setting | Participants | Sex | Age (y) | Ethnicity/race | Educational level | Cigarettes smoked/d |
|---|---|---|---|---|---|---|---|---|---|---|
| An 201319 | Good | United States | Randomized controlled trial | Not bound to a setting | Young adult smokers (n = 1698) |
|
24.07 (NR), NR |
|
|
19.82 (NR) |
| Bordnick 201220 | Fair | United States | Randomized controlled trial | Clinic | Nicotine-dependent treatment-seeking cigarette smokers (n = 86) |
|
|
|
NR |
|
| Brinker 201621 | Poor | Germany | Cross sectional study | Secondary schools | Grade 7 students (n = 125) |
|
12.75 (NR), NR | NR | NR | NR |
| DeLaughter 201622 | Fair | United States | Pre-post study | Laboratory | In- or outpatient smokers (n = 30) |
|
NR (NR), 19-65+ | White/Non-Hispanic or Latino 100% |
|
13.8 (10.0) |
| Duncan 201823 | Good | United States | Pre-post study | NR | Adolescents never smokers (n = 25) |
|
11.56 (0.77), NR | African American 72%; American Indian/Native American 12%; Hispanic 12%; other 4% | NR | 0 |
| Girard 200924 | Poor | Canada | Randomized controlled trial | Clinic | Adult smokers (n = 91) |
|
44 (11), NR | NR | NR | >21 (45% of population) |
| Gordon 201725 | Fair | United States | Pre-post study | Not bound to a setting | Female smokers (n = 73) | Female 100% | 39.1 (13.1), NR | African American 16.4%; Asian 1.4%; Caucasian 72.6%; multirace/other 9.6%; other 5.5%; Hispanic/Latino 8.2% |
|
16.0 (13.2) |
| Khazaal 200826 | Good | Switzerland | Pre-post study | Psychiatric hospital | Adult smokers that are inpatients of a psychiatric hospital (n = 51) |
|
43.7 (12.8), NR | NR | NR | 23 (14) |
| Khazaal 201327 | Poor | Switzerland | Randomized controlled trial | NR | Adult smokers in early stages of change (n = 240) |
|
31.5 (12.1), NR | NR |
|
15 (7.9) |
| Metcalf 201828 | Poor | United States | (stratified, wait-list) Controlled Trial | Game setup location (ie, small office) | Adults recently quit smoking (n = 61) |
|
NR (NR), NR | Asian 3.3%; African American 39.3%; white 45.9%; other 3.3%; multiracial 3.3%; prefer not to answer 3.3% | NR | NR |
| Nemire 199929 | Poor | United States | Randomized controlled trial | NR | Grade 7 students (n = 72) | Female ≈ Male | NR (NR), NR | NR | NR | NR |
| Parisod 201830 | Good | Finland | Randomized controlled trial | Schools and not bound to a setting | Early adolescents (n = 151) |
|
11, 10-13 | NR | NR | 0.67% is current smoker |
| Rath 201531 | Good | United States | Randomized controlled trial | Not bound to a setting | Youth and young adults (n = 689) |
|
NR (NR), 13-24 | Non-Hispanic white 59.8%; Non-Hispanic black 14.2%; other non-Hispanic 7.8%; Hispanic 18.2% |
|
58% has never tried cigarettes |
| Song 201332 | Fair | United States | 2 × 2 between-subjects factorial design | Laboratory | Social smokers (n = 62) |
|
22.05 (3.28), NR | NR | NR | Frequency of smoking: once a week (median) |
| Xu 201433 | Fair | United States | 2 × 2 within-subjects factorial design | Laboratory | Couples in long term relationships of which at least 1 is a smoker (n = 40) | NR | 24.10 (6.17), 19-42 | NR | NR | 11.56 (6.01) |
Values are mean (SD), range; mean (SD); or median, range, unless otherwise indicated.
NR: not reported.
See Supplementary Tables 1-3 for detail.
Intervention characteristics
Table 2 presents details on intervention characteristics. Of the 15 included studies, 14 studies evaluated unique serious games. All games were digital games, with the exception of 2 board games.26,27 Khazaal et al26,27 reported on the same game in different populations. Most serious games were aimed at smoking cessation (n = 9), whereas 6 aimed at smoking initiation prevention. About a quarter of studies did not report on the theoretical basis of their serious game. If reported, cognitive behavioral therapy and theory of planned behavior were most often the basis of the game. A third of the serious games were played once, for a range of—if reported—2-90 minutes. In addition, more than half of the serious games were played multiple times in a range of—if reported—2-10 weeks. Two serious games had free usage,25,30 for 1 of these games, it was reported that the serious game was played twice as much as the nongamified website.30 Three serious games were assessed alongside a cointervention.20,24,29
Table 2.
Intervention characteristics
| Study ID | Health objective | Intervention | Availabilitya | Type | Theoretical basis | Intervention group(s) | Game play | Control group(s) |
|---|---|---|---|---|---|---|---|---|
| An 201319 | Smoking cessation | “RealU2” (trial name) aimed at abstinence from cigarette use among young adult smokers. | Digital | Social cognitive theory; theory of reasoned action and planned behavior; self-determination theory |
|
Once per week, for 6 wk | Untailored general interest messages | |
| Bordnick 201220 | Smoking cessation | “Virtual Reality Skills Training” aimed at development and practice of coping skills for smoking cessation. | Digital | Cognitive behavioral therapy |
|
Once per week (1 h), for 10 wk | Nicotine replacement therapy (nicotine patch) only | |
| Brinker 201621 | Smoking prevention | “Smokerface” aimed at smoking prevention. | Google Play; App Store | Digital | Theory of planned behavior | Using photo-aging app | 2 min, once | Not applicable |
| DeLaughter 201622 | Smoking cessation | “Crave-Out” aimed at managing cravings during a quit attempt. | Digital | NR | Playing a distraction/motivation game (Crave-Out) | 10 min, once | Not applicable | |
| Duncan 201823 | Smoking prevention | “smokescreen” aimed at smoking prevention. | App Store | Digital | A logic model of cognitive and motivational variables | Playing a role-playing videogame (smokeSCREEN) | 4 sessions (1 h), in 2 wk | Not applicable |
| Girard 200924 | Smoking cessation | “Virtual arm” (VR therapy) aimed at reducing tobacco addiction. | Digital | Cue exposure therapy |
|
Once per week (30 min), for 4 wk |
|
|
| Gordon 201725 | Smoking cessation | “See Me Smoke-Free” aimed at smoking cessation among women. | Digital | NR | Using “See Me Smoke-Free” application | For 1 mo | Not applicable | |
| Khazaal 200826 | Smoking cessation | “Pick-Klop” aimed at changing the attitude toward tobacco addiction among smokers. | Analogue | Cognitive behavioral therapy | Playing the board game “Pick-Klop,” a group smoking cessation game | Once, 1-1.5 h | Not applicable | |
| Khazaal 201327 | Smoking cessation | “Pick-Klop” aimed at changing the attitude toward tobacco addiction among smokers. | Analogue | Cognitive behavioral therapy | Playing the board game “Pick-Klop,” a group smoking cessation game | Once per week (1 h 30 min), for 2 wk |
|
|
| Metcalf 201828 | Smoking cessation | “Take control” aimed at providing support for those in recovery from tobacco addiction. | Digital | Cue exposure therapy, extinction therapy, virtual reality therapy, cognitive behavioral therapy | Playing the virtual reality cue refusal video game “Take Control” | 3 sessions (15-30 min), in 4 wk | Waiting list | |
| Nemire 199929 | Smoking prevention | “Virtual Environment technology” aimed at smoking prevention among adolescents. | Digital | NR |
|
Once per week (50 min), for 8 wk | Life skills training | |
| Parisod 201830 | Smoking prevention | “Fume” aimed at improving tobacco related health literacy. | Google Play; App Store | Digital | Health literacy determinants |
|
1 session of guided training (20 min), free usage in 2 wk | No intervention |
| Rath 201531 | Smoking prevention | “Flavour Monsters” aimed at improving tobacco related attitudes and beliefs | Digital | Theory of planned behavior | Playing “Flavour Monsters” with tobacco related information | ±4.5 h in several sessions | Not applicable | |
| Song 201332 | Smoking prevention | “Super Smoky” aimed at educating about the risk of social smoking. | Digital | Possible selves |
|
Once | Not applicable | |
| Xu 201433 | Smoking cessation | Cooperative games (not named) aimed at undermining nicotine cravings. | Digital | NR |
|
Once (11 min) | Not applicable |
NR: not reported.
Availability on October 1, 2019.
Game elements
Table 3 presents the results on included game elements. None of the studies explicitly reported any game elements, and consequently, we extracted game elements from the game description in the articles. All serious games included a combination of game elements from multiple categories (mean 5.5 per serious game; range, 3-10). Most game elements were in the category “reward and punishment features” (n = 32), next was “narrative and identity features” (n = 20), followed by “manipulation and control features” (n = 12) and “presentation features” (n = 11), and last was “social features” (n = 8). On game element level, the most frequently included game elements were general rewards types (n = 11). The next most included game elements were theme and genre features (n = 9) (eg, interacting with virtual lungs).29 The next most included game elements (n = 9) were punishments (eg, score reduction).32 Next, graphic and sound features (eg, playing within fictional medieval castle24) (n = 8) and intermittent rewards (n = 7) (eg, varying difficulty of scenarios)20 were the most included game elements. Game elements that were not included were support networks (eg, internet forums to assist playing), negative rewards (eg, repairing items), pay-out intervals (eg, rewarded instantly for playing), franchise (eg, trademarked names), and explicit content (eg, violence).
Table 3.
Game elements categorized according to taxonomy of King et al17
| Categories | Narrative and identity features |
Social features |
Manipulation and control features |
Reward and punishment features |
Presentation features |
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies | Game elements | Avatar creation (eg, animation of 3D selfie21) | Storytelling device (eg, health messages dialog19) | Theme and genre (eg, virtual lungs29) | Social Utility (eg, group comments on questions26) | Social formation (eg, cooperative play33) | Leader board (eg, scores30) | Support network | User input (eg, pick up and crush cigarette24) | Save (eg, checkpoint at each level31) | Player management (eg, use skills to react to cues21) | Noncontrollable (eg, periodic messages25) | General reward type (eg, earning points27) | Punishment (eg, score reduction32) | Meta-game reward (eg, success academically and socially23) | Intermittent reward (eg, difficulty of scenarios20) | Negative reward | Near miss (eg, difficult end boss31) | Event frequency (eg, unlimited replay of game28) | Event duration (eg, no end until button pressed20) | Pay-out interval | Graphics and sound (eg, fictional medieval castle24) | In-game advertising (eg, links to other resources21) | Franchise | Explicit content | Total |
| An 201319 | x | x | x | x | 4 | |||||||||||||||||||||
| Bordnick 201220 | x | x | x | x | x | x | x | x | 8 | |||||||||||||||||
| Brinker 201621 | x | x | x | x | 4 | |||||||||||||||||||||
| DeLaughter 201622 | x | x | x | x | x | x | 6 | |||||||||||||||||||
| Duncan 201823 | x | x | x | x | x | x | x | 7 | ||||||||||||||||||
| Girard 200924 | x | x | x | 3 | ||||||||||||||||||||||
| Gordon 201725 | x | x | x | x | 4 | |||||||||||||||||||||
| Khazaal 200826 | x | x | x | x | x | 5 | ||||||||||||||||||||
| Khazaal 201327 | x | x | x | x | x | x | 6 | |||||||||||||||||||
| Metcalf 201828 | x | x | x | x | x | 5 | ||||||||||||||||||||
| Nemire 199929 | x | x | x | x | x | 5 | ||||||||||||||||||||
| Parisod 201830 | x | x | x | x | x | x | x | x | 8 | |||||||||||||||||
| Rath 201531 | x | x | x | x | x | x | x | x | x | x | 10 | |||||||||||||||
| Song 201332 | x | x | x | x | x | 5 | ||||||||||||||||||||
| Xu 201433 | x | x | x | 3 | ||||||||||||||||||||||
| Total per game element | 6 | 5 | 9 | 4 | 3 | 1 | 0 | 5 | 1 | 2 | 4 | 11 | 9 | 1 | 7 | 0 | 2 | 1 | 1 | 0 | 8 | 3 | 0 | 0 | ||
| Total per category | 20 | 8 | 12 | 32 | 11 | |||||||||||||||||||||
Effects on smoking prevention and behavioral determinants
Table 4 presents the results regarding effects on smoking-related outcomes. Six studies were aimed at smoking initiation prevention. Of these, only 1 study assessed prevention by measuring use of cigarettes, in which no statistically significant difference was found (participants were nonsmokers before and after their study).29 These 6 studies together assessed 20 behavioral determinants of smoking initiation prevention. Statistically significant effects were observed for 8 of 20 of these determinants (ie, attitude, knowledge, intention, perceived risk, perceived susceptibility, and perceptions). Three studies found statistically significant positive effects on attitudes toward smoking,30–32 albeit not statistically significant in all conditions.32 One study found statistically significant positive effects for smoking-related knowledge from pre- to postintervention, but not at follow up.23 One study found a statistically significant positive effect in behavioral intention to not involve in social smoking in 1 of the conditions in 1 study (ie, future face vs current face), and positive but not statistically significant effects in the other condition (ie, self-avatar vs someone else’s avatar).32 Studies that assessed perceived risk,32 perceived susceptibility,32 and perceptions about outcomes of cigarettes smoking30 also reported statistically significant positive effects.
Table 4.
Effects on smoking-related outcomes
| Study ID | Measures | Outcomes | Direction of difference | Statistical significance |
|---|---|---|---|---|
| An 201319 | 1. Self-reported 30-d abstinence of cigarette smoking | 1. Smoking abstinence at 12-wk evaluation was 11% in the control group, 23% in the intervention group with tailored health message, and 31% in the intervention group with tailored health plus peer coaching. |
|
1. Significant |
| Bordnick 201220 |
|
|
|
|
| Brinker 201621 |
|
|
|
|
| DeLaughter 201622 | 1. Cravingsa (Questionnaire of Smoking Urge-Brief; scale 1-7 [low to higher cravings]) | 1. Mean cravings were 3.24 preintervention and 2.99 postintervention. | 1. Decrease | 1. Not significant. |
| Duncan 201823 |
|
|
|
|
| Girard 200924 |
|
|
|
|
| Gordon 201725 |
|
|
|
|
| Khazaal 200826 |
|
|
|
|
| Khazaal 201327 |
|
|
|
|
| Metcalf 201828 |
|
|
|
|
| Nemire 199929 |
|
|
|
|
| Parisod 201830 |
|
|
|
|
| Rath 201531 | 1. Attitudes about tobacco products and the tobacco industry (Anti-Tobacco Industry Index; scale 1 [positive attitude] to 10 [negative attitude]) |
|
|
|
| Song 201332 |
|
|
|
|
| Xu 201433 |
|
|
|
|
Outcome measure valid and reliable.
CI: confidence interval; OR: odds ratio.
Effects on smoking cessation and behavioral determinants
The effects of playing a serious game on smoking status and cessation were assessed in 7 studies. Four studies found statistically significant, positive effects on smoking status,19,25,27,33 and 1 study found positive effects that were significant at one time point but insignificant at another time point.24 Moreover, the 3 studies that assessed the effect on the number of smoked cigarettes all found positive, statistically significant effects.20,25,27 Last, 1 study found statistically significant, positive effects on cravings.20
Six studies assessed the effects of serious games on behavioral determinants of smoking cessation among adult smokers.20,25–28,33 These 6 studies assessed a total of 12 behavioral determinants of smoking cessation. Of these determinants, 6 had statistically significant positive effects (ie, attitude, self-efficacy, intention, self-expansion, and coping skills). One study found statistically significant, positive effects on attitude toward smoking.27 Self-efficacy effects were inconclusive with statistically significant positive effects20,27 and statistically significant negative effects.25 One study found statistically significant, positive effects on behavioral intention to quit smoking.26 Studies that assessed self-expansion33 and coping skills20 also reported statistically significant, positive effects.
Other findings
Three studies evaluated a serious game that was delivered in combination with another intervention. Two studies reported statistically significant, positive effects on smoking cessation.20,24 Although most studies reported on outcomes observed shortly after the intervention,21,22,24,26–30,32,33 5 studies reported on results after a slightly longer follow-up (eg, at 12 weeks).19,20,23,25,31 Of the latter studies, 2 found statistically significant, positive effects on the number of cigarettes smoked and cravings,20 and cessation rates.19 Rath et al31 found statistically significant, positive effects at follow-up on antismoking attitudes. The outcome measures used in the studies were all validated,20,22,24 partly validated,25–27,30,33 or none of the measures were validated.19,21,23,28,29,31,32 Only 2 studies assessed carbon monoxide levels when measuring smoking status.24,33 The majority of the studies with statistically significant effects had a fair or good study quality score. Owing to the heterogeneity of the included studies, it was impossible to perform a pooled meta-analysis.
DISCUSSION
This systematic review aimed to gain insight into the composition and effects of serious games on smoking-related outcomes. We found that serious games included multiple game elements of different categories. The evidence from a number of studies suggests that games may have positive effects on smoking-related outcomes, particularly on smoking cessation. Six studies on smoking prevention together assessed 20 determinants and found statistically significant positive effects for 8 determinants (ie, attitude, knowledge, perceived risk, perceived susceptibility, intention, and perceptions). Nine studies were aimed at smoking cessation, of which 7 assessed smoking status or cessation. Of these studies, 4 found statistically significant, positive effects on smoking status, and 3 studies assessed the effect on the number of smoked cigarettes with all finding positive, statistically significant effects. Six studies assessed the effects of serious games on 12 determinants of smoking cessation, 7 of which found statistically significant positive effects (ie, self-efficacy, self-expansion, attitude, coping skills, and intention).
This review analyzed which game elements are included in serious games aimed at smoking prevention and cessation. Similar to our findings, a review of serious games for sexual health promotion found that “feedback” and “rewards” were most frequently included game elements.8 These game elements are known behavior change techniques or learning mechanisms.10,11 The extracted game elements of the serious games in this review mainly correspond to the “10 ingredients of great games” (eg, avatars, 3-dimensional environments, narrative context).34 Most serious games in this review did not include elements in the category “social features.” The game element “support networks” was not included in any of the studies. Social features, which include support networks, appear thus underrepresented in serious games for smoking initiation prevention and cessation. This underrepresentation suggests that there is a window of opportunity to incorporate these features in these serious games, which could contribute to their effectiveness to prevent or stop smoking. This is because serious games with social features included in this systematic review all reported positive significant effects on smoking cessation and determinants.19,20,33 Moreover, the literature points out that smoking cessation and relapse are strongly associated to smoking behavior in social networks,35 and smoking behavior is impacted by social influence.36 For many people, identification with and social norms of important reference groups play an important role in increasing a smokers’ self-efficacy to quit.37 Social support networks can further offer platforms for increasing motivation or interest in quitting smoking and preventing or sustaining abstinence, and have provided preliminary effectiveness in smoking cessation.38
Our finding that a number of studies suggested that games may have positive effects on smoking-related outcomes is in line with other reviews on serious health games. Sexual health games positively affected behavioral determinants (eg, intention), yet no effect on behavior was found (eg, delayed sexual initiation).8 Exergaming was found to result in positive effects on physical activity–related outcomes, while determinants (eg, self-efficacy) were not assessed.5 Serious games for healthy lifestyle promotion yielded small positive effects on health behaviors (eg, healthy diet) and determinants (eg, knowledge).4 Serious games for chronic disease self-management are effective in improving knowledge and self-management.39 Our review shows that some serious games have the potential to stop smoking and positively influence behavioral determinants of smoking cessation. Considering the effects of serious games on smoking initiation prevention, the results were more ambiguous and will likely require a timespan covering years rather than weeks. Also, some studies may have lacked power to detect statically significant effects.
Our review exposes various limitations in the included studies and raises serious questions. The heterogeneity of studies, intervention characteristics, and outcomes inhibits an unambiguously, conclusive evaluation of the effects of serious games on smoking-related outcomes. Moreover, the reporting of the studies did not allow an analysis of the effects of specific or combinations of game elements on smoking-related outcomes. Further, many studies were classified as poor or fair (methodological) quality, raising questions about the validity of results. One of the main issues was unreported information. This prevents a distinction between studies that reported incompletely but may have in fact good methodological quality and studies that actually had poor methodological quality.40 Lack of information on characteristics of study also creates uncertainty about the generalizability of the results. Moreover, about a quarter of the studies did not report any theoretical basis of their game or intervention; however, this is crucial for effectiveness of serious games on behavioral determinants.4 This is underlined by a review that places theoretical basis in the first stage of a framework for developing serious games.41 Another limitation of the studies in our review is that only 5 studies reported follow-up outcomes up until 12 weeks. As it is known that most smokers have multiple quit attempts before achieving maintained smoking cessation, long-term results are of great importance to assess whether serious games have lasting effects on smoking on smoking-related outcomes. To illustrate, 1 study showed that at follow-up the positive effects on self-efficacy and intention to change health behavior can substantially be reduced.4 In accordance with a Cochrane review, we suggest that for research follow-up of at least 6 months of abstinence should be used as a benchmark for sustained smoking cessation.42 Another limitation is that most studies did not use or partly used validated and reliable measures. In addition, smoking status was only in 2 studies assessed by carbon monoxide; other studies used self-reports. Self-reports tend to underestimate smoking behavior.43 Furthermore, for studies assessing effects of a serious game combined with another intervention, it remains unclear if the effects can be attributed to the serious game, or are a result of the cointervention. Last, the fixed playtime of the serious games is a limitation. The amount of playtime (ie, frequency and duration) of serious games and settings of studies varied greatly among studies in our review, and only 2 studies allowed free usage. Effects assessed based on free usage are likely to reflect effects close to real-life effects in contrast to fixed play sessions. The fixed play of most serious games might thus generate effects that are not (fully) generalizable to real-life settings.
Limitations
Our systematic review might be affected by publication bias, which may have resulted in an overestimation of the potentially positive effects of serious games on smoking-related outcomes. Another limitation of our review is the quality appraisal of included studies. Despite the independent appraisal by 2 reviewers and the use of quality appraisal tools, there was room for subjectivity in the appraisal. Another limitation is that we were dependent on the descriptions of a game in the included articles for the extraction of game elements, which were often not detailed. Therefore, we might have misclassified game elements. Last, the results of this review might be influenced by the taxonomy of King et al,17 which we used for extraction of game elements. Although we used the most relevant taxonomy according to our assessment of 3 taxonomies, game elements might have been missed due to the specific taxonomy used.
CONCLUSION
In this review, we gained insight into the composition and effects of serious games on smoking-related outcomes. As a next step, it would be valuable to assess the contribution of single or combinations of game elements on the effects of these serious games on prevention and cessation of smoking. Based on the results of our review, we suggest to include game elements with reward and social features and subsequently assess their contribution to effects. These features are the most and least included game elements, respectively, and a contribution assessment would show whether this is justified.
This study stresses the need for health informaticians to base serious game design on theories and to apply multiple game elements, among which game elements from the category “social features.” Health informaticians should further consider setting up social networks in relation to game use. They should evaluate these games on their effectiveness, with standardized, valid evaluation measures and measurements. Furthermore, we urge future evaluations to be based on voluntary playtime and to assess long-term results (at least 6 months postintervention). Still, the intended intensity of interaction (ie, intermittent interaction or time-intervals) between the player and the game should be taking into account when determining the length of the follow-up period. Moreover, we highly recommend that future evaluations of serious games be more methodologically homogenous and of high quality. We advocate for detailed descriptions of study populations to shed light on external validity, studies’ methodologies, intervention components, and protocols.
To conclude, serious games included multiple game elements of different categories and seemed to positively affect smoking-related outcomes, particularly smoking cessation. However, owing to the various limitations of the literature, we cannot be conclusive about the effects of serious games on smoking prevention, cessation, or behavioral determinants. At this point, we have insufficient knowledge on the effects and working mechanisms of serious games to make well-founded recommendations to game designers. Once again, future evaluations should be more homogenous, comprehensive, and of high quality.
FUNDING
MED and MPF were supported by FNO-Healthy Future Nearby (102253).
AUTHOR CONTRIBUTIONS
MED and MPF designed the study and JGD, MED, and SvS built the search. MED and SvS carried out the data extraction and drafted the article. All authors (MED, SvS, AEK, JGD, MWMJ, and MPF) were involved in data analysis, contributed to the writing of the final article, and approved the final article.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1. Michael DR, Chen SL.. Serious Games: Games that Educate, Train, and Inform. Florence, KY: Muska & Lipman/Premier-Trade; 2005. [Google Scholar]
- 2. Laamarti F, Eid M, Saddik AE.. An overview of serious games. Int J Comput Games Technol 2014; 2014: 358152. [Google Scholar]
- 3. Ferguson B. The emergence of games for health. Games Health J 2012; 1 (1): 1–2. [DOI] [PubMed] [Google Scholar]
- 4. DeSmet A, Van Ryckeghem D, Compernolle S, et al. A meta-analysis of serious digital games for healthy lifestyle promotion. Prev Med 2014; 69: 95–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Street TD, Lacey SJ, Langdon RR.. Gaming your way to health: A systematic review of exergaming programs to increase health and exercise behaviors in adults. Games Health J 2017; 6 (3): 136–46. [DOI] [PubMed] [Google Scholar]
- 6. Lamboglia CMGF, da Silva VTBL, de Vasconcelos Filho JE, et al. Exergaming as a strategic tool in the fight against childhood obesity: a systematic review. J Obes 2013; 2013:438364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eichenberg C, Schott M.. Serious games for psychotherapy: A systematic review. Games Health J 2017; 6 (3): 127–35. [DOI] [PubMed] [Google Scholar]
- 8. DeSmet A, Shegog R, Van Ryckeghem D, Crombez G, De Bourdeaudhuij I.. A systematic review and meta-analysis of interventions for sexual health promotion involving serious digital games. Games Health J 2015; 4 (2): 78–90. [DOI] [PubMed] [Google Scholar]
- 9. Deterding S, Dixon D, Khaled R, Nacke L. From game design elements to gamefulness: defining “gamification”. In: MindTrek ’11: Proceedings of the 15th International Academic MindTrek Conference: Envisioning Future Media Environments. New York, NY: Association for Computing Machinery; 2011: 9–15. doi: 10.1145/2181037.2181040 [Google Scholar]
- 10. Michie S, Hyder N, Walia A, West R.. Development of a taxonomy of behavior change techniques used in individual behavioral support for smoking cessation. Addict Behav 2011; 36 (4): 315–9. [DOI] [PubMed] [Google Scholar]
- 11. Arnab S, Lim T, Carvalho MB, et al. Mapping learning and game mechanics for serious games analysis. Br J Educ Technol 2015; 46 (2): 391–411. [Google Scholar]
- 12. Brigham TJ. An introduction to gamification: adding game elements for engagement. Med Ref Serv Q 2015; 34 (4): 471–80. [DOI] [PubMed] [Google Scholar]
- 13. Wilczynski NL, McKibbon KA, Haynes RB.. Search filter precision can be improved by NOTing out irrelevant content. AMIA Annu Symp Proc 2011; 2011: 1506–13. [PMC free article] [PubMed] [Google Scholar]
- 14. van Eck N, Waltman L.. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010; 84 (2): 523–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Heart Lung and Blood Institute. Study Quality Assessment Tools. Bethesda, MD: National Institutes of Health. [Google Scholar]
- 16.CochraneAirways. Data collection. https://airways.cochrane.org/data-collection Accessed May 20, 2018.
- 17. King D, Delfabbro P, Griffiths M.. Video game structural characteristics: a new psychological taxonomy. Int J Ment Health Addict 2010; 8 (1): 90–106. DOI 10.1007/s11469-009-9206-4 [Google Scholar]
- 18. Robinson D, Bellotti V. A preliminary taxonomy of gamification elements for varying anticipated commitment. In: proceedings CHI 2013 Workshop on Designing Gamification: Creating Gameful and Playful Experiences; April 27 to May 2, 2013; Paris, France.
- 19. An LC, Demers MR, Kirch MA, et al. A randomized trial of an avatar-hosted multiple behavior change intervention for young adult smokers. J Natl Cancer Inst Monogr 2013; 2013 (47): 209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bordnick PS, Traylor AC, Carter BL, Graap KM.. A feasibility study of virtual reality-based coping skills training for nicotine dependence. Res Soc Work Pract 2012; 22 (3): 293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brinker TJ, Seeger W, Buslaff F.. Photoaging mobile apps in school-based tobacco prevention: the mirroring approach. J Med Internet Res 2016; 18 (6): e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DeLaughter KL, Sadasivam RS, Kamberi A, et al. Crave-out: a distraction/motivation mobile game to assist in smoking cessation. JMIR Serious Games 2016; 4 (1): e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Duncan LR, Hieftje KD, Pendergrass TM, Sawyer BG, Fiellin LE.. Preliminary investigation of a videogame prototype for cigarette and marijuana prevention in adolescents. Subst Abus 2018; 39 (3): 275–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Girard B, Turcotte V, Bouchard S, Girard B.. Crushing virtual cigarettes reduces tobacco addiction and treatment discontinuation. Cyberpsychol Behav 2009; 12 (5): 477–83. [DOI] [PubMed] [Google Scholar]
- 25. Gordon JS, Armin J, Hingle MD, et al. Development and evaluation of the See Me Smoke-Free multi-behavioral mHealth app for women smokers. Transl Behav Med 2017; 7 (2): 172–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khazaal Y, Chatton A, Prezzemolo R, Hoch A, Cornuz J, Zullino D.. A game for smokers: a preliminary naturalistic trial in a psychiatric hospital. Patient Educ Couns 2008; 70 (2): 205–8. [DOI] [PubMed] [Google Scholar]
- 27. Khazaal Y, Chatton A, Prezzemolo R, et al. Impact of a board-game approach on current smokers: a randomized controlled trial. Subst Abuse Treat Prev Policy 2013; 8 (1): 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Metcalf M, Rossie K, Stokes K, Tallman C, Tanner B.. Virtual reality cue refusal video game for alcohol and cigarette recovery support: summative study. JMIR Serious Games 2018; 6 (2): e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nemire K, Beil J, Swan RW.. Preventing teen smoking with virtual reality. Cyberpsychol Behav 1999; 2 (1): 35–47. [DOI] [PubMed] [Google Scholar]
- 30. Parisod H, Pakarinen A, Axelin A, Löyttyniemi E, Smed J, Salanterä S.. Feasibility of mobile health game “Fume” in supporting tobacco-related health literacy among early adolescents: a three-armed cluster randomized design. Int J Med Inform 2018; 113: 26–37. [DOI] [PubMed] [Google Scholar]
- 31. Rath JM, Williams V, Rubenstein R, Smith L, Vallone D.. Assessing the impact of an interactive mobile game on tobacco-related attitudes and beliefs: the truth campaign’s flavor monsters. Games Health J 2015; 4 (6): 480–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Song H, Kim J, Kwon RJ, Jung Y.. Anti-smoking educational game using avatars as visualized possible selves. Comput Hum Behav 2013; 29 (5): 2029–36. [Google Scholar]
- 33. Xu X, Aron A, Westmaas JL, Wang J, Sweet LH.. An fMRI study of nicotine-deprived smokers’ reactivity to smoking cues during novel/exciting activity. PLoS One 2014; 9 (4): e94598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reeves B, Read JL.. Total Engagement: How Games and Virtual Worlds are Changing the Way People Work and Businesses Compete. Brighton, MA: Harvard Business Press; 2009. [Google Scholar]
- 35. Blok DJ, de Vlas SJ, van Empelen P, van Lenthe FJ.. The role of smoking in social networks on smoking cessation and relapse among adults: a longitudinal study. Prev Med 2017; 99: 105–10. [DOI] [PubMed] [Google Scholar]
- 36. Simons-Morton BG, Farhat T.. Recent findings on peer group influences on adolescent smoking. J Prim Prev 2010; 31 (4): 191–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Phua JJ. The reference group perspective for smoking cessation: an examination of the influence of social norms and social identification with reference groups on smoking cessation self-efficacy. Psychol Addict Behav 2013; 27 (1): 102–12. [DOI] [PubMed] [Google Scholar]
- 38. Naslund JA, Kim SJ, Aschbrenner KA, et al. Systematic review of social media interventions for smoking cessation. Addict Behav 2017; 73: 81–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Charlier N, Zupancic N, Fieuws S, Denhaerynck K, Zaman B, Moons P.. Serious games for improving knowledge and self-management in young people with chronic conditions: a systematic review and meta-analysis. J Am Med Inform Assoc 2016; 23 (1): 230–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Reitsma J, Rutjes A, Whiting P, Vlassov V, Leeflang M, Deeks J.. Chapter 9: Assessing methodological quality In: Deeks JJ, Bossuyt PM, Gatsonis C, eds. Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy. London, UK: The Cochrane Collaboration. [Google Scholar]
- 41. Verschueren S, Buffel C, Vander Stichele G.. Developing theory-driven, evidence-based serious games for health: framework based on research community insights. JMIR Serious Games 2019; 7 (2): e11565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Livingstone-Banks J, Norris E, Hartmann-Boyce J, et al. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2019; 2: CD003999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gorber SC, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M.. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res 2009; 11 (1): 12–24. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.