Abstract
Objective
To assess the extent of UK speech and language therapy engagement in assessment and management of primary progressive aphasia, determine the factors contributing to any shortfall and explore a gap in the research literature on current speech and language therapy practices with people with primary progressive aphasia.
Methods
A 37-item, pilot-tested survey was distributed electronically via clinical networks and through the Royal College of Speech and Language Therapists. Survey items included questions on intervention approaches, referral numbers and demographics, referral sources and access to services.
Results
One hundred and five speech and language therapists completed the survey. Over the previous 24 months, respondents reported seeing a total of 353 people with primary progressive aphasia (an average of 3.27 per speech and language therapist). Neurologists were the most commonly reported referrers to speech and language therapy (22.5%). Seventy-eight percent of respondents reported that people with primary progressive aphasia experienced barriers to accessing speech and language therapy. Key barriers were a lack of referrer awareness of a speech and language therapist’s role, and restrictive eligibility criteria for services.
Conclusions
This study highlighted inequities in access to speech and language therapy for people with primary progressive aphasia. The medical and speech and language therapy professions need to develop appropriate care pathways for people with primary progressive aphasia. Speech and language therapists have a duty to develop a relevant evidence base for speech and language interventions for people with primary progressive aphasia.
Keywords: primary progressive aphasia, speech and language therapy, referrals, barriers, service provision, survey
Introduction
The number of people living with dementia worldwide continues to rise, estimated at around 46 million in 2015 and set to increase to around 131.5 million in 2050 (Prince et al., 2015). Fronto-temporal dementia (FTD) is the leading cause of younger onset dementia, often diagnosed in people in their 50s–60s who are still employed, with dependent families; it is therefore liable to have a disproportionate socioeconomic and human impact (Croot, 2009; Dua et al., 2012). The primary progressive aphasias (PPAs) are a heterogeneous group of language-led dementias overlapping the wider spectrum of FTD and Alzheimer’s disease and presenting a number of unique challenges for diagnosis, management and care service provision. All forms of PPA present as insidious deterioration of language skills, initially with relative sparing of other cognitive functions. Language problems in PPA are diverse but commonly include poor naming, reduced comprehension and vocabulary, phonological errors, dysfluency and grammatical errors (Bonner et al., 2010; Dickerson, 2011; Kertesz et al., 2010; Mesulam, 1982). Currently three major PPA syndromes are recognised, each with a different profile of language impairments (Gorno-Tempini et al., 2011). Semantic variant PPA (svPPA) or ‘semantic dementia’ is usually associated with an FTD pathology and presents predominantly as a deficit of single word comprehension and loss of vocabulary. Logopenic PPA (lvPPA) is usually associated with an Alzheimer’s pathology and presents as impaired word retrieval and phonological assembly. Non-fluent agrammatic variant PPA (navPPA) is more commonly associated with an FTD pathology than an Alzheimer’s pathology and presents as dysfluent or apraxic speech (a motor speech disorder) and agrammatism (impaired structuring of more complex messages, such as sentences). The estimated overall United Kingdom population prevalence of FTD is approximately 11/100,000, of which PPA syndromes collectively account for around a third of cases (Coyle-Gilchrist et al., 2016): this means there are, conservatively, likely to be around 2300 people currently living with PPA in the United Kingdom.
Given that language difficulties are at the core of PPA, people with the condition may benefit from a referral to speech and language therapy (SLT) services. However, there are reports of infrequent utilisation of SLT in Australia (Taylor et al., 2009) and Germany (Riedl et al., 2014) by people with PPA. These researchers speculate on the reasons for this, including a lack of awareness of the SLT role amongst referrers (Taylor et al., 2009), the scarcity of speech and language therapists who are experienced in the treatment of PPA, and the geographical dispersion of patients (Riedl et al., 2014).
SLT offers a range of potential benefits for people with PPA including basic communication strategies and aids, education of patients and families, planning care needs and packages and word relearning interventions (Volkmer, 2013; Marshall et al., 2018). At present there is an exclusive emphasis on word relearning interventions in the research literature which overlooks this range of therapeutic options (Bier et al., 2009; Graham et al., 1998; Henry et al., 2011; Heredia et al., 2009; Jokel et al., 2006, 2014). A systematic review of non-pharmacological interventions for PPA (Carthery-Goulart et al., 2013) demonstrates the comparative paucity of speech and language interventions which are not focused on word relearning.
Little is known of current SLT services available for people with PPA. Taylor et al. (2009) surveyed 13 SLT services across the New South Wales state of Australia with the aim of establishing current SLT practice with people with PPA. No single management or care pathway, defined by the European pathway Association (EPA, 2018) as ‘an explicit statement of the goals and key elements of care based on evidence, best practice and patient expectation’, was identified by the survey. Kindell et al.’s (2015) consensus group is the first research to examine SLT practice in the UK. This study was conducted with six expert speech and language therapists who specialised in dementia. It highlighted that in practice, SLTs prioritise working with the people around a person with PPA, i.e. family and other care givers, in order to maximise the communication and life participation of those with the condition.
To assess the extent of SLT engagement in assessment and management of PPA, determine the factors contributing to any shortfall and explore a gap in the research literature on current SLT practices with people with PPA, this study describes a UK-wide survey of speech and language therapists. There is a need for work of this kind to give a picture of current SLT referral patterns in PPA and to identify service shortfalls for framing funding and health policy decisions, and making recommendations for best care of PPA. It was anticipated that respondents would report barriers to SLT services for people with PPA due to a lack of awareness of the SLT role in the wider health community. It was also hypothesised that speech and language therapists would offer a range of interventions beyond those focused on word relearning to people with PPA.
Method
The final survey comprised 37 questions over five sections: (1) Clinical background; (2) Number, type and source of patients; (3) Time spent on management of people with PPA; (4) Specific assessment and intervention approaches; (5) Outcome measures and planning for the future. There were closed questions (for speed of completion) and open questions to elicit additional information (Schaeffer & Dykema, 2011). In order to achieve a representative cohort of UK speech and language therapists, the Royal College of Speech and Language Therapists were contacted to facilitate survey dissemination via links published in the practice magazine and electronic newsletter, emails were sent by the author to all relevant Clinical Excellence Networks and social media networks were utilised. See online supplementary information for a description of the development and dissemination of the online survey. The complete survey is presented in online Appendix 1. The initial page of the survey provided a statement making clear that by continuing, respondents were giving consent to participate in the survey and that their responses would be stored anonymously. Respondents completed initial survey questions on employment, qualification and experience of working with people with PPA. If they were not a UK speech and language therapist with experience of PPA they were instructed not to continue the survey. The Departmental Ethics Chair in Language and Cognition at University College London waived approval as the study met the criteria for service evaluation.
Data analysis
Data were downloaded to IBM’s Statistical Package for Social Science 23 software. Descriptive statistics were used to analyse characteristics of speech and language therapist respondents and referral patterns. In view of the small sample sizes across geographical regions, data were grouped into north England (Yorkshire and the Humber, North East, North West, East Midlands and West-Midlands) and south England (London, South East, South West and East) for further analysis using Mann–Whitney non-parametric statistics to compare referral numbers. Remaining data were examined using frequency counts and contingency tables (Sauerbrei & Blettner, 2009). For open-ended questions or ‘other’ response categories, both descriptive statistics such as coding and counting responses and qualitative analysis was used. The latter included identifying themes and sub-themes using thematic analysis (Braun and Clarke, 2006).
Results
Demographics of speech and language therapist respondents
In total, there were 179 responses to the survey. With no available data on numbers of UK speech and language therapists providing services for PPA, it is not possible to calculate a percentage response rate. However, respondents represented a spread across grade bands and appeared representative in terms of professional location, i.e. primary care, acute health and mental health (see below). (Practising speech and language therapists are employed in the UK National Health Service from a band 5; entry level, to band 8; highly specialist, manager or consultant). Of the 179 respondents, 105 submitted complete surveys, indicating experience of working with PPA.
Table 1 summarises the characteristics of the 105 eligible respondents whose data was analysed. Of these 54.3% (n = 57) had more than 10 years’ SLT experience. About a third were employed at band 6 (31.4%, n = 33) and just over a third at band 7 (37.1%, 39). Respondents based in primary care numbered 48 (45.7%), with 26.7% (n = 28) in acute health and 14.3% (n = 15) in mental health care. Although there is no data on proportions of speech and language therapists employed in primary care, acute health and mental health, this appears representative as services to mental health are known to be less. The highest number of respondents were from Scotland (n = 18; 17.1%) and fewest respondents came from the North West of England (n = 2; 1.9%).
Table 1.
Characteristics of speech and language therapist survey respondents.
| Years post qualification | |
|---|---|
| 1–2 | 12.4% (13) |
| 3–4 | 6.7% (7) |
| 4–10 | 26.7% (28) |
| 10+ | 54.3% (57) |
| Current banding | |
| Newly qualified | 5.7% (6) |
| Band 5 | 6.7% (7) |
| Band 6 | 31.4% (33) |
| Band 7 | 37.1% (39) |
| Band 8 | 11.4% (12) |
| Other | 7.6% (8) |
| Healthcare service | |
| Acute health care | 26.7% (28) |
| Mental health care | 14.3% (15) |
| Primary care | 45.7% (48) |
| Charity/third sector | 3.8% (4) |
| Independent/private | 0 |
| Other | 9.5% (10) |
| Geographical region | |
| East | 7.6% (8) |
| East Midlands | 4.8% (5) |
| Northern Ireland | 9.5% (10) |
| London | 13.3% (14) |
| North East | 3.8% (4) |
| North West | 1.9% (2) |
| Scotland | 17.1% (18) |
| South East | 15.2% (16) |
| South West | 10.5% (11) |
| Wales | 5.7% (6) |
| West Midlands | 4.8% (5) |
| Yorkshire and the Humber | 5.7% (6) |
Referral patterns
Respondents were asked to reflect on the patients with PPA they had seen over the previous 24 months. Collectively, respondents reported seeing a total of 353 patients over this period. On average, 3.27 people with PPA were seen per respondent, with a range of 0–17 (see Figure 1). Geographical variation was observed (see Figure 2) with most patients seen per respondent in the South East (5.6) and least in Northern Ireland (1.6) and Wales (1.5). There was no significant difference in the number of patients across the North (mean = three patients) and the South of England (mean = three patients) (U = 535.5, z = −0.045, ns).
Figure 1.
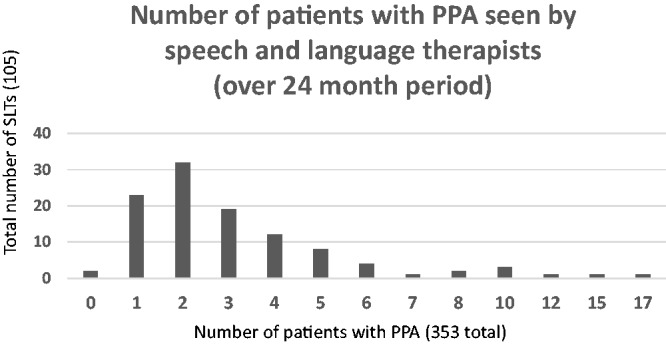
Distribution of people with PPA seen by speech and language therapists over the last 24 months.
Figure 2.
Average number of PPA patients on SLT caseloads across the UK.
Respondents reported seeing patients with PPA across multiple settings within the same service. Most often they were reported to be seen in community (n = 75; 45.5%) or outpatient settings (n = 54; 32.7%), whilst a smaller number were seen in memory clinics (n = 13; 7.9%) or in acute medical settings (n = 12; 7.3%).
There were significant differences between geographical region for people seen in outpatient settings (χ(1) = 23.114, p = 0.017) with more than 75% of respondents in Scotland (n = 14), Wales and the North East reporting that they saw patients in this setting, whilst none of the respondents in the East and West Midlands reported this. No other significant differences in setting were observed across geographical regions.
Characteristics of patients referred to SLT
Almost two thirds (n = 65; 61.9%) of respondents reported seeing patients with PPA aged between 60 and 70 years of age, and just under half (n = 47; 44.8%) reported seeing people aged between 50 and 60 years of age. Most respondents reported patients were from an English-speaking background (n = 92; 87.6%). Of the respondents who reported seeing patients from non-English (n = 13; 12.4%) or multilingual backgrounds (n = 16; 15.2%), these respondents were generally concentrated in London and the South of England. The following languages were listed: Flemish, French, Greek, Irish, Swedish, Turkish and Welsh. Around two thirds (n = 65; 61.9%) of respondents reported seeing patients from high managerial occupations, just over half (n = 53; 50.5%) reported patients with intermediate occupations (Office for National Statistics (ONS) examples include supervisory, clerical & junior managerial, administrative, and professional occupations). A similar number of respondents (n = 56; 53.3%) reported patients with manual occupations.
Access to SLT services
Table 2 summarises the details of how people with PPA access SLT services. Respondents reported that they receive a large number of their referrals from neurologists (n = 52; 22.5%). Almost all respondents reported receiving referrals regarding concerns about word-finding difficulties (n = 101; 96%). Around one third (n = 37; 32.2%) reported patients were ‘always’ or ‘often’ informed they had PPA or FTD. When asked to select a category reflecting when the majority of their patients were referred, almost half of respondents (n = 49; 46.7%) reported that patients were referred within two to three years of symptom onset. A further 40% (n = 42) of respondents reported the majority of their patients were referred within one year of symptom onset.
Table 2.
Access to speech and language therapy (SLT) services.
| Access to SLT services (% response; multiple responses allowed) | |
|---|---|
| Source of referrals | |
| Neurologists | 22.5% (n = 52) |
| General practitioners | 20.8% (n = 48) |
| Psychiatrists | 18.2% (n = 42) |
| Geriatricians | 6.9% (n = 16) |
| Referral reason | |
| Word-finding difficulties | 96% (n = 91) |
| Swallowing difficulties | 17% (n = 18) |
| Slurred speech | 15% (n = 16) |
| Time since symptom onset | |
| Within 2–3 years | 46.7% (n = 49) |
| Within 1 year | 40% (n = 42) |
| Respondents whose patients had always/often been informed of their diagnosis as: | |
| Dementia | 54.3% (n = 57) |
| PPA or FTD | 32.2% (n = 37) |
| svPPA | 3.8% (n = 7) |
| lvPPA | 6.5% (n = 12) |
| navPPA | 6.5% (n=12) |
| Barriers to accessing SLT services | |
| Other | 41.8% |
| Service criteria | 26.23% |
| Geographical location | 13.93% |
| Offered but declined | 13.11% |
| Language barrier | 4.92% |
PPA: primary progressive aphasia; FTD: fronto-temporal dementia; svPPA: semantic variant PPA; lvPPA: logopenic PPA; navPPA: Non-fluent agrammatic variant PPA.
When asked to indicate whether they felt people with PPA may not have accessed SLT services, more than three quarters (n = 82; 78.1%) of respondents agreed with such a statement. The most common barriers to access were identified firstly as ‘other’ (n = 51; 41.8%) and secondly as service criteria (n = 32; 26.2%). An analysis of the text responses under the ‘other’ barrier category revealed two major issues: lack of awareness of the SLT role amongst referrers (69.2%), and difficulties in diagnosis (30.8%). Speech and language therapist respondents working in third sector organisations reported geographical location as a significant barrier for their patients (H(4) = 13.156, p < 0.01). There were no other significant associations found between the type of healthcare service that respondents worked in and barriers reported.
Intervention approaches
The majority of respondents (n = 95; 90.5%) reported there was no care pathway for people with PPA within their service. With regards to specific interventions, many respondents reported providing communication training for families and carers ‘often’ or ‘always’ (n = 89; 84.8%) and just under half (n = 45; 42.9%) reported ‘often’ or ‘always’ working on activity and participation-based communication tasks. In comparison, only one fifth of respondents reported ‘often’ or ‘always’ using impairment based approaches targeting word relearning (n = 21; 20%), for which the evidence base is greatest. (The International Classification of Functioning, Disability and Health (ICF, WHO 2001) describes impairment based interventions as those that seek to remediate, alleviate or improve. Activity and participation based interventions focus on functional communication, engagement in executing an activity and participating in a life situation.)
In terms of other interventions reported to be in use ‘often’ or ‘always’, 20% (n = 21) of respondents provided communication training for staff, 12.4% (n = 13) reported working on reading and writing, 11.4% (n = 12) provided high-tech communication aids, and 8.6% (n = 9) reported using impairment based interventions for speech production deficits (apraxia of speech). Respondents reported having most time available for functional communication interventions (an average of 4.9 sessions), with on average 2.8 sessions available for impairment-based language interventions, 2.4 sessions for educating family, 2.4 sessions for educating the person with PPA, and 0.8 sessions for educating staff. When asked how much time they would ideally like to spend on functional communication interventions, the average response was 7.8 sessions, nearly three sessions more than the average number reported as available.
Discussion
Summary of findings
The findings from this UK-wide survey suggest major inequities in access and referral to SLT for people with PPA. Respondents report seeing a total of 353 patients in the last two years which, given the prevalence numbers for the condition, represents a significant shortfall in terms of overall proportion of PPA cases being seen by SLT. There is poor representation in terms of characteristics of the wider UK adult population; respondents describe their patients as largely from higher socioeconomic backgrounds and of predominantly English-speaking backgrounds. Only European languages are reported for multi-lingual or non-English speaking patients. Clearly only a minority of people with PPA living in the UK have access to SLT. The majority of survey respondents identified a lack of a care pathway for people with PPA in their area. The data reveal socioeconomic status and linguistic background as key barriers to accessing SLT. In addition, respondents identified a lack of awareness of the SLT role amongst referrers, restrictive criteria resulting in people being ineligible for the service, geography and delays in diagnosis as key barriers. The results also highlight a gap between the current research evidence for speech and language interventions and those commonly used by speech and language therapists in clinical practice.
Interpretation of results
Speech and language therapist respondents reported that the majority of their patients with PPA were between 60 and 70 years of age. This is consistent with a recent UK study (Coyle-Gilchrist et al., 2016) and a systematic review (Hogan et al., 2016). Both studies hypothesise that it becomes harder to differentiate PPA from other dementia types in people over 70 years of age. Hall et al. (2013) report that it is not uncommon for younger people with PPA who present with intact cognition to be given a psychiatric diagnosis, such as anxiety or personality disorder, in the early stages of the disease. This may partially explain why many respondents in this survey report their patients are only referred two to three years after diagnosis. The broader difficulties in PPA diagnosis may account for reports from respondents that delays in getting a diagnosis can also be a barrier to people accessing SLT and the concerning report that nearly half of people who are referred do not know their diagnosis.
The finding that many SLTs perceive service criteria to be a barrier to accessing intervention may reflect the division between services for older people (above 65 years) and those who are younger. Many National Health Service SLT services for older people with progressive conditions such as dementia are only commissioned to provide input around management of swallowing disorders. This means people with PPA above 65 years of age, who meet these service criteria but need communication support, may only be able to access input around swallowing. In contrast neuro-rehabilitation services for people under 65 that do provide support around communication, often exclude people with progressive conditions. This means people with PPA below the age of 65 who would benefit from communication therapy are excluded because they have a progressive condition and thus do not meet these service criteria.
The finding that the majority of people with PPA seen by speech and language therapists are predominantly English speaking is not entirely surprising in light of the England and Wales national census data (ONS, 2017), which highlights that 92.3% of people report English as their first language in this study. It is noteworthy that speech and language therapists reported people with PPA with multilingual or non-English backgrounds to speak Western-European languages such as Swedish and Flemish. Even though this survey targeted respondents in greater London, people from Asian and Afro-Caribbean multilingual communities were not reflected in the data. London is the most ethnically diverse area in England and Wales with at least 7% of the London population identifying as African, 6.6% as Indian and 4.2% as Caribbean (ONS, 2017). One explanation for this finding may lie in cultural factors around health and illness. Mukadem et al. (2011) highlight that people from minority ethnic communities are less likely to access health services due to the ‘stigma of mental illness and negative experience of psychiatric services’ (Mukadem et al., 2011, p. 1075).
In this study, the reported socio-economic distribution of people with PPA referred to SLT was predominantly high managerial. This does not reflect that of the general population, close to 50% of whom are employed in manual occupations in comparison to under 30% in high managerial professions (ONS, 2010). Given that research has indicated increased occupational attainment reduces the risk of dementia (Wang et al., 2017) this survey suggests a significant number of people of intermediate and manual occupational backgrounds may be failing to access SLT, or indeed any, services for PPA. Previous research has shown that people with higher levels of education are more likely to seek out support and interventions (Ploeg et al., 2009), and this issue may also offer an explanation for the current findings.
Strengths and limitations
The professional body, the Royal College of Speech and Language Therapists, records that 2000 registered speech and language therapists currently work with adults. There is no available data, however, on how many of those provide a service for people with dementia, so it is not possible to evaluate the representativeness of the sample size in this study. In addition, respondents may have been a self-selecting sample based on clinical interest and confidence. This group is likely to include respondents based in specialist services for people with PPA and this may have skewed the data. However, a sample size of 105 compares favourably with other SLT surveys, with respondent numbers ranging between 13 and 147 (Beckley et al., 2017; Collis & Bloch, 2012; Sirman et al., 2017; Taylor et al., 2009).
One of the major limitations of this study was that no information was collected on the proportion of people with PPA on a respondent’s caseload in relation to those with other conditions. Comparison between services for PPA and other types of dementia is thus not possible, nor is it possible to reflect on whether it is only referral numbers for PPA that are increasing, or whether general referrals to SLT are rising.
It is noteworthy that some respondents reported access to the survey software being blocked by local IT services. This may have prevented some speech and language therapists from responding.
Implications for future research
It is clear that more accurate epidemiological data on PPA in the UK is required; and to understand why particular factors (e.g. under-representation of particular ethnic groups) occurred. Surveys of neurologists and GPs etc. would be useful to determine what proportion of PPA cases they refer to SLT and if not, why not.
Eight out of every 10 speech and language therapists in this study reported using communication training ‘where people around the person with aphasia learn to use strategies and communication resources to aid the individual’ (Simmons-Mackie et al., 2016) always or often in treating PPA, yet significantly fewer (two out of every 10) reported using impairment-based word relearning therapies. The latter have dominated the research literature in this area to date (Carthery-Goulart et al., 2013). The small number of studies that evaluate activity and participation-based intervention for PPA, of which communication training is one example, employ methodological designs that are low in the hierarchy of research evidence. The mismatch between an evidence base that supports word relearning and clinical practice that favours functional approaches to support communication highlights the urgent need for further intervention research. Studies are needed to examine the effectiveness of interventions that speech and language therapists perceive to be clinically relevant for people with PPA, beginning with communication training. Future studies have a duty to consult people living with PPA and their families, through support organisations such as the PPA Support Group (www.raredementiasupport.org).
Implications for practice
In this survey, only a handful of speech and language therapists reported care pathways within their services (less than 10% of respondents). There is currently no national care pathway for people with PPA; in fact, there is no nationally recognised care pathway for people with FTD. Care pathways provide referrers with information on appropriate support services to ensure patients receive the right intervention at the right time (Allen et al., 2009). Without a care pathway, health professionals involved with the care of people with PPA are likely to be unaware of the role of SLT. The results of this survey highlight a need to promote the role of the speech and language therapist to physicians working with people with PPA to ensure they have better access to SLT. A several-pronged approach is required including: education of GPs and other medical practitioners about PPA, education of these professional groups about the role of SLT, improved public awareness of PPA. SLTs could take a leading role in these areas.
Conclusion
This study has highlighted key barriers to accessing SLT services in the UK including a lack of awareness of the SLT role amongst potential referrers, service criteria that exclude people with PPA, geography and delays in diagnosis. There is an urgent need to address these barriers by establishing a care pathway to ensure patients with PPA are routinely referred to SLT. Speech and language therapists have a duty to inform referrers of what their services can offer patients with PPA, and develop evidence based clinical interventions for this client group.
Supplemental Material
Supplemental material, Supplemental material1 for Speech and language therapy for primary progressive aphasia: Referral patterns and barriers to service provision across the UK by Anna Volkmer, Aimee Spector, Suzanne Beeke and Jason D Warren in Dementia
Supplemental material, Supplemental material2 for Speech and language therapy for primary progressive aphasia: Referral patterns and barriers to service provision across the UK by Anna Volkmer, Aimee Spector, Suzanne Beeke and Jason D Warren in Dementia
Acknowledgements
I would like to thank all the speech and language therapists who participated in the survey. I would also like to thank Vanessa Meitanis who assisted in the electronic management of the survey data using the Opinio software.
Biography
Anna Volkmer is a speech and language therapist and NIHR-funded doctoral researcher in the Division of Psychology and Language Sciences at University College London. Anna’s PhD research is focused on developing and trialing a communication training program entitled Better Conversations with Primary Progressive Aphasia. She is also interested in the role of SLT in supporting people who may lack capacity to make decisions. Anna has published three books for speech and language therapists focusing on assessment and management of people with dementia, and on their role in supporting people who may lack capacity to make decisions.
Aimee Spector, professor of old age clinical psychology, is a dementia researcher at University College London and a clinical psychologist specialising in ageing and dementia. She developed Cognitive Stimulation therapy (CST) as her PhD thesis and has been involved in numerous subsequent CST research including the evaluation of maintenance CST and individual CST. She is an author on all the CST manuals, developed the CST training course and has personally trained around 3000 people in CST. She is director of the international CST centre at UCL and involved in CST research in Hong Kong, Brazil, India and Tanzania. Her research programme more broadly focuses on the development and evaluation of psychological therapies for dementia, including Cognitive Behavioural Therapy, Compassion Focused Therapy and Mindfulness. She has published over 80 academic papers, three book chapters and eight books.
Suzanne Beeke is a speech and language therapist and senior lecturer in the Division of Psychology and Language Sciences at University College London. Her research focuses on communication disability in adults with post-stroke aphasia, traumatic brain injury, and dementia, particularly the impact of these conditions on everyday conversations in the home and on healthcare interactions. She is lead author of Better Conversations with Aphasia, a free online resource at https://extendstore.ucl.ac.uk that currently has over 5400 registered users worldwide, with resources translated into Danish and Swedish.
Jason D Warren is professor of neurology in the Dementia Research Centre at University College London Institute of Neurology and a consultant neurologist in the Specialist Cognitive Disorders Clinic at the National Hospital for Neurology and Neurosurgery. His research aims to discover how changes in brain function in different forms of dementia produce complex problems with communication, social and emotional behaviour; how these changes in brain function can best be measured; and how they can be used to diagnose and track the culprit brain degeneration. He has over 240 peer-reviewed papers with over 12,000 citations. His group’s research has featured regularly in lay media including BBC Radio 3 and Radio 4, BBC Breakfast, the front page of The Times and The Wall Street Journal.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This paper presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. This work is supported by a National Institute for Health Research Doctoral Research Fellowship, Anna Volkmer, 2015–08-182.
JDW receives grant support from the Alzheimer’s Society, Alzheimer’s Research UK and the NIHR UCLH Biomedical Research Centre.
Supplemental Material
Supplemental Material for this article is available online.
References
- Allen D., Gillen E., Rixson L. (2009). Systematic review of the effectiveness of integrated care pathways: What works, for whom, in which circumstances? International Journal of Evidence‐Based Healthcare, 7, 61–74. [DOI] [PubMed] [Google Scholar]
- Beckley F., Best W., Beeke S. (2017). Delivering communication strategy training for people with aphasia: What is current clinical practice? International Journal of Language & Communication Disorders, 52, 197–213. [DOI] [PubMed] [Google Scholar]
- Bier N., Macoir J., Gagnon L., Van der Linden M., Louveaux S., Desrosiers J. (2009). Known, lost, and recovered: Efficacy of formal-semantic therapy and spaced retrieval method in a case of semantic dementia. Aphasiology, 23, 210–235. [Google Scholar]
- Bonner M. F., Ash S., Grossman M. (2010). The new classification of primary progressive aphasia into semantic, logopenic, or nonfluent/agrammatic variants. Current Neurology and Neuroscience, 10, 484–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Carthery-Goulart M. T., Silveira A. D. C. D., Machado T. H., Mansur L. L., Parente M. A. D. M. P., Senaha M. L. H., … Nitrini R. (2013). Nonpharmacological interventions for cognitive impairments following primary progressive aphasia: A systematic review of the literature. Dementia & Neuropsychologia, 7(1), 122–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collis J., Bloch S. (2012). Survey of UK speech and language therapists’ assessment and treatment practices for people with progressive dysarthria. International Journal of Language & Communication Disorders, 47, 725–737. [DOI] [PubMed] [Google Scholar]
- Coyle-Gilchrist I. T., Dick K. M., Patterson K., et al. (2016). Prevalence, characteristics, and survival of frontotemporal lobar degeneration syndromes. Neurology, 86, 1736–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croot, K., Nickels, L., Laurence, F., & Manning, M. (2009). Impairment‐and activity/participation‐directed interventions in progressive language impairment: Clinical and theoretical issues. Aphasiology, 23(2), 125–160. [Google Scholar]
- Dickerson B. C. (2011). Quantitating severity and progression in primary progressive aphasia. Journal of Molecular Neuroscience, 45, 618–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dua, T. , Nichols, P. and Setoya, Y. (Eds) (2012), Dementia: A Public Health Priority, World Health Organization, Geneva. [Google Scholar]
- European Pathways Association. (2018). EPA definition of care pathway. Retrieved from http://e-p-a.org/care-pathways/
- Graham K. S., Pratt K. H., Hodges J. R. (1998). A reverse temporal gradient for public events in a single case of semantic dementia. Neurocase: The Neural Basis of Cognition, 4, 461–470. [Google Scholar]
- Gorno-Tempini M. L., Hillis A. E., Weintraub S., Kertesz A., Mendez M., Cappa S. E. E. A., . . . Manes F. (2011). Classification of primary progressive aphasia and its variants. Neurology, 76(11), 1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall G. R., Shapira J., Gallagher M., Denny S. S. (2013). Managing differences: Care of the person with frontotemporal degeneration. Journal of Gerontological Nursing, 39, 10–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry M. L., Meese M. V., Truong S., Babiak M., Miller B. L., Gorno-Tempini M. L. (2011). Treatment for apraxia of speech in nonfluent variant primary progressive aphasia. Behavioural Neurology, 25, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heredia C. G., Sage K., Sage M. A. L., Berthier M. L. (2009). Relearning and retention of verbal labels in a case of semantic dementia. Aphasiology, 23, 192–209. [Google Scholar]
- Hogan D. B., Jetté N., Fiest K. M., Roberts J. I., Pearson D., Smith E. E., Maxwell C. J. (2016). The prevalence and incidence of frontotemporal dementia: A systematic review. Canadian Journal of Neurological Sciences, 43, S96–S109. [DOI] [PubMed] [Google Scholar]
- Jokel R., Graham N., Rochon E., Leonard C. (2014). Word retrieval therapies in primary progressive aphasia. Aphasiology, 28, 1038–1068. [Google Scholar]
- Jokel R., Rochon E. A., Leonard C. (2006). Treatment for anomia in semantic dementia: Improvement, maintenance or both? Neuropsychological Rehabilitation, 16, 241–256. [DOI] [PubMed] [Google Scholar]
- Kertesz A., Jesso S., Harciarek M., Blaire M., McMonagle P. (2010). What is semantic dementia? A cohort study of diagnostic features and clinician boundaries. Archives of Neurology, 67, 483–489. [DOI] [PubMed] [Google Scholar]
- Kindell J., Sage K., Cruice M. (2015). Supporting communication in semantic dementia: Clinical consensus from expert practitioners. Quality in Ageing and Older Adults, 16, 153–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall C. R., Hardy C. J., Volkmer A., Russell L. L., Bond R. L., Fletcher P. D., ….Fox N. C. (2018). Primary progressive aphasia: A clinical approach. Journal of Neurology, 1, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesulam M. (1982). Slowly progressive aphasia without generalized dementia. Annals of Neurology, 11, 592–598. [DOI] [PubMed] [Google Scholar]
- Mukadam N., Cooper C., Basit B., Livingston G. (2011). Why do ethnic elders present later to UK dementia services? A qualitative study. International Psychogeriatrics, 23, 1070–1077. [DOI] [PubMed] [Google Scholar]
- Office for National Statistics SOC. (2010). Volume 3: The National Statistics Socio-economic classification (NS-SEC rebased on SOC2010). Retrieved from http://www.ons.gov.uk/ons/guide-method/classifications/current-standard-classifications/soc2010/soc2010-volume-3-ns-sec–rebased-on-soc2010–user-manual/index.html#11
- Office for National Statistics. (2017). Language in England and Wales: 2011. Retrieved from https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/language/articles/languageinenglandandwales/2013-03-04
- Ploeg J., Denton M., Tindale J., Hutchison B., Brazil K., Akhtar-Danesh N., … Plenderleith J. M. (2009). Older adults’ awareness of community health and support services for dementia care. Canadian Journal on Aging/La Revue Canadienne Du Vieillissement, 28(4), 359–370. [DOI] [PubMed] [Google Scholar]
- Prince M., Wimo A., Guerchet M., Ali G. C., Wu Y. T., Prina M. (2015). World Alzheimer report 2015. The global impact of dementia. An analysis of prevalence, incidence, cost & trends. London: Alzheimer’s Disease International. [Google Scholar]
- Riedl L., Last D., Danak A., Diehl S.J. (2014). Long term follow up in primary progressive aphasia: Clinical course and health care utilisation. Aphasiology, 28, 981–992. [Google Scholar]
- Sauerbrei W., Blettner M. (2009). Interpreting results in 2 × 2 tables: Part 9 of a series on evaluation of scientific publications. Deutsches Ärzteblatt International, 106, 795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeffer N. C., Dykema J. (2011). Questions for surveys: Current trends and future directions. Public Opinion Quarterly, 75, 909–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons-Mackie N., Raymer A., Cherney L. R. (2016). Communication partner training in aphasia: An updated systematic review. Archives of Physical Medicine and Rehabilitation, 97(12), 2202–2221. [DOI] [PubMed] [Google Scholar]
- Sirman N., Beeke S., Cruice M. (2017). Professionals’ perspectives on delivering conversation therapy in clinical practice. Aphasiology, 31, 465–494. [Google Scholar]
- Taylor C., Kingma R. M., Croot K., Nickels L. (2009). Speech pathology services for primary progressive aphasia: Exploring an emerging area of practice. Aphasiology, 23, 161–174. [Google Scholar]
- Volkmer A. (2013). Assessment and therapy for language and cognitive communication difficulties in dementia and other progressive diseases. UK: J&R Press, North Guilford. [Google Scholar]
- Wang H. X., MacDonald S. W., Dekhtyar S., Fratiglioni L. (2017). Association of lifelong exposure to cognitive reserve-enhancing factors with dementia risk: A community-based cohort study. PLoS Medicine, 14, e1002251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental material1 for Speech and language therapy for primary progressive aphasia: Referral patterns and barriers to service provision across the UK by Anna Volkmer, Aimee Spector, Suzanne Beeke and Jason D Warren in Dementia
Supplemental material, Supplemental material2 for Speech and language therapy for primary progressive aphasia: Referral patterns and barriers to service provision across the UK by Anna Volkmer, Aimee Spector, Suzanne Beeke and Jason D Warren in Dementia



