Abstract
Objectives:
To model the relationship between loneliness and sleep disturbance over time.
Method:
Data came from the Health and Retirement Study (2006, 2010, 2014 waves; age ≥ 65 years; n = 5,067). Loneliness was measured via the Hughes Loneliness Scale and sleep disturbance via a four-item scale assessing sleep and restedness. Cross-lagged panel modeling (path analysis) was used to jointly examine reciprocal effects between loneliness and sleep disturbance.
Results:
Higher loneliness correlated with higher sleep disturbance at baseline. There was evidence of reciprocal effects between loneliness and sleep across timepoints. These associations overall remained when accounting for demographics, objective isolation, and depression.
Discussion:
Although causality cannot be established, the findings indicate that the relationship between loneliness and sleep disturbance is bidirectional. This requires revision to the current theory on sleep disturbance as a mechanism for the relationship between loneliness and health and indicates that effective treatment of sleep disturbance may reduce loneliness.
Keywords: loneliness, sleep, insomnia, health, older adults
There is a growing body of evidence documenting the health sequelae of loneliness, yet how loneliness affects health remains unclear. Cacioppo and Hawkley (2003, 2009) proposed a model of the relationship between loneliness and health that identified sleep disturbance as a mechanism underlying the connection between loneliness and health, based on a study showing that lonely participants showed lower sleep efficiency and higher levels of wake time after sleep onset than non-lonely participants (Cacioppo et al., 2002). Cacioppo and Hawkley (2003) argued that this sleep disturbance marks the loss of a fundamentally restorative behavior, thus affecting metabolic, neural, and hormonal processes. The study did not control for measures of objective isolation, nor did it assess for the effects of sleep quality on loneliness.
Although numerous studies have shown that loneliness is associated with sleep disturbance across a wide range of samples and measures (Aanes et al., 2011; Cacioppo et al., 2002; Cheng et al., 2015; Chu et al., 2016; Hom et al., 2017; McHugh et al., 2011; Segrin & Burke, 2015; Stickley et al., 2015), the majority of these studies have not controlled for potential confounds. Moreover, studies differ in terms of which factors they controlled for, which have included a range of demographics, health behaviors, health factors, mental health factors, and social factors. One of the most commonly included potential confounds is depression, which attenuated the relationship between loneliness and sleep disturbance across all relevant studies (Cheng et al., 2015; Hayley et al., 2017; Hom et al., 2017; Kurina et al., 2011; Matthews et al., 2017; McHugh et al., 2011; Yu et al., 2017).
The longitudinal research on loneliness as a risk factor for sleep disturbance is smaller and less conclusive than the cross-sectional literature. Only a handful of empirical, longitudinal studies have evaluated loneliness as a risk factor for sleep disturbance in adults, with differing conclusions: some studies found that loneliness predicted sleep disturbance (Hom et al., 2017; Jacobs et al., 2006; Jaremka et al., 2014; McHugh & Lawlor 2013; Zawadzki et al., 2013), whereas others did not (Hom et al., 2017; Jaremka et al., 2014; Yu et al., 2017). These studies differed in terms of their outcome of interest (to include insomnia symptoms, sleep quality, sleep satisfaction, and sleep adequacy), in addition to other key methodological factors, such as length of follow-up (3 months to 7 years), measures, samples, analyses, attrition rates (5.5%–56.1%), and potential confounds, making it difficult to draw conclusions across studies.
Two papers report on sleep problems as a risk factor for loneliness in adults (Hom et al., 2017; Simon & Walker, 2018). These papers provide preliminary support for sleep disturbance as a risk factor for loneliness: across all studies, sleep disturbance predicted subsequent loneliness. However, the duration of follow-up across studies was limited (follow-up ranged from 2 days to 6 months across studies). Examination of the day-to-day relationship between fluctuations of loneliness and sleep is critical, but it is also important to look at their long-term relationship to understand how effects may accumulate to produce enduring changes in health. Moreover, none of the samples are representative of—or even resemble—the U.S. population.
Sleep disturbance is a correlate of loneliness across multiple studies using a range of measures and samples, but there is insufficient evidence to determine whether loneliness precedes sleep disturbance or vice versa, and therefore, the direction of causal dominance between loneliness and sleep disturbance remains obscure. It is possible that the correlation between sleep disturbance and loneliness is due, at least in part, to the effect of sleep disturbance on loneliness (Simon & Walker, 2018). Moreover, it is unclear how other factors—such as objective isolation and depression—are contributing to the relationship between loneliness and sleep disturbance.
The present study aimed to examine causal dominance in the relationship between loneliness and sleep disturbance in older Americans over an 8-year span using a cross-lagged panel model. The model allowed for the joint examination of the baseline association between loneliness and sleep disturbance and their longitudinal prediction of one another. A second cross-lagged panel model was run to control for potential confounds, including demographics, objective isolation (limited contact with social network), and depression. We hypothesized that (a) higher levels of loneliness would be associated with greater sleep disturbance and (b) loneliness would be a stronger predictor of subsequent sleep disturbance than the reverse, based on the model developed by Cacioppo and Hawkley (2003).
Method
Data
Data for this study came from the Health and Retirement Study (HRS), a panel study of Americans over the age of 50 years and their spouses (Sonnega et al., 2014). Data collection occurs every 2 years and covers a wide array of domains, including income, employment, assets, pension plans, health care expenditures, health insurance, physical health, mental health, physical functioning, and cognitive functioning.
This study used data from the 2006, 2010, and 2014 waves of the HRS. The HRS initiated a mixed-mode follow-up in 2006, whereby 50% of the sample was randomly assigned to in-person follow-up and the remaining 50% of the sample was randomly assigned to telephone follow-up; the method of follow-up then alternated across the following waves. The half of the sample assigned to in-person follow-up were left with a questionnaire (the Participant Lifestyle Questionnaire, also known as the Leave-Behind Questionnaire) to complete and return by mail. The loneliness measure was collected via this questionnaire. Data from the half of the sample that completed Psychosocial and Lifestyle Questionnaire in the 2006, 2010, and 2014 waves were used for the current study.
Sample
Sample characteristics are summarized in Table 1. Only participants aged 65 years and above were included in this study; 5,067 participants returned the Participant Lifestyle Questionnaire in 2006, 2010, or 2014. All of these participants completed the sleep disturbance scale, though only 4,624 of these participants completed the Hughes Loneliness Scale in 2006. In 2010, these numbers dropped to 4,111 completing the sleep disturbance scale and 3,424 completing the Hughes Loneliness Scale. In 2014, 3,121 participants completed the sleep disturbance scale and 2,608 participants completed the Hughes Loneliness Scale. Table 1 provides the characteristics of participants who completed the measure of sleep disturbance in 2014 (n = 3,121) versus those who did not (n = 1,946) to address the possibility of attrition bias. Participants who were lost to follow-up were on average lonelier, older, lower socioeconomic status (SES), and less educated and were more likely to be male and widowed or separated/divorced.
Table 1.
Characteristics of the Sample in 2006, Overall and Stratified by Follow-up Status.
| Full sample | Respondeda | No responsea | Died | |
|---|---|---|---|---|
| n = 5,067 | n = 3,125 | n = 342 | n = 1,600 | |
| n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||
| Male | 2,188 (43.18) | 1,270 (40.64) | 139 (40.64) | 779 (48.69) |
| Female | 2,879 (56.82) | 1,855 (59.36) | 203 (59.36) | 821 (51.31) |
| Education | ||||
| Less than high school | 1,214 (23.96) | 656 (20.99) | 70 (20.47) | 488 (30.50) |
| GED | 234 (4.62) | 138 (4.42) | 17 (4.97) | 79 (4.94) |
| High-school graduate | 1,702 (33.59) | 1,068 (34.18) | 118 (34.50) | 516 (32.25) |
| Some college | 978 (19.30) | 620 (19.84) | 63 (18.42) | 295 (18.44) |
| College and above | 939 (18.53) | 643 (20.58) | 74 (21.64) | 222 (13.88) |
| Race | ||||
| White/Caucasian | 4,281 (84.49) | 2,628 (84.10) | 295 (86.26) | 1,358 (84.88) |
| Black/African American | 628 (12.39) | 391 (12.51) | 33 (9.65) | 204 (12.75) |
| Other | 158 (3.12) | 106 (3.39) | 14 (4.09) | 38 (2.38) |
| Ethnicity | ||||
| Not Hispanic | 4,688 (95.52) | 2,881 (92.19) | 307 (89.77) | 1,500 (93.75) |
| Hispanic | 379 (7.48) | 244 (7.81) | 35 (10.23) | 100 (6.25) |
| Socioeconomic status | ||||
| Lower | 855 (16.87) | 455 (14.56) | 51 (14.91) | 349 (21.81) |
| Lower middle | 967 (19.08) | 537 (17.18) | 61 (17.84) | 369 (23.06) |
| Middle | 1,058 (20.88) | 665 (21.28) | 71 (20.76) | 322 (20.13) |
| Upper middle | 1,122 (22.14) | 734 (23.49) | 83 (24.27) | 305 (19.06) |
| Upper | 1,065 (21.02) | 734 (23.49) | 76 (22.22) | 255 (15.94) |
| Marital status | ||||
| Married | 3,081 (60.81) | 2,003 (64.10) | 220 (64.33) | 858 (53.63) |
| Partnered | 90 (1.78) | 58 (1.86) | 11 (3.22) | 21 (1.31) |
| Separated/divorced | 415 (8.19) | 273 (8.74) | 30 (8.77) | 112 (7.00) |
| Widowed | 1,363 (26.90) | 719 (23.01) | 69 (20.18) | 575 (35.94) |
| Never married | 118 (2.33) | 72 (2.30) | 12 (3.51) | 34 (2.13) |
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Baseline age | 74.31 (7.12) | 72.48 (5.88) | 72.91 (6.57) | 78.19 (7.87) |
| Range | 65 to 104 | 65 to 96 | 65 to 95 | 65 to 104 |
| Baseline loneliness | −0.53 (.53) | −.57 (.51) | −.55 (.51) | −.45 (.56) |
| Range | −1 to 1 | −1 to 1 | −1 to 1 | −1 to 1 |
| M sleep disturbance | 1.64 (.51) | 1.62 (.51) | 1.60 (.50) | 1.68 (.52) |
| Range | 1 to 3 | 1 to 3 | 1 to 3 | 1 to 3 |
Note. n = number of participants. M = mean; SD = standard deviation.
in 2014.
Measures
Loneliness.
Loneliness was measured via the Hughes Loneliness Scale, which consists of the questions: “How often do you feel that you lack companionship?,” “How often do you feel left out?” and “How often do you feel isolated from others?” (Clarke et al., 2008). Responses included “Often,” “Some of the time,” and “Hardly ever or never.” If more than one item was missing, the scale score was set to missing (Clarke et al., 2008). Hughes et al. (2004) have demonstrated that the Hughes Loneliness Scale has satisfactory concurrent validity, discriminant validity, and reliability in older adult samples.
Sleep disturbance.
Sleep disturbance was measured as a modified version of the Jenkins sleep scale (Jenkins et al., 1988) that included the following four items: “How often do you have trouble falling asleep?,” “How often do you have trouble with waking up during the night?,” “How often do you have trouble with waking up too early and not being able to fall asleep again?” and “How often do you feel really rested when you wake up in the morning?.” Responses included “Rarely or never,” “Sometimes,” and “Most of the time.” The sleep items were reverse coded, and then, all four items were averaged to create the total score; this approach is consistent with past uses of this scale in the literature (Lee et al., 2017).
Demographics.
Demographics included age, sex (male, female), education (less than high school, GED, high-school graduate, some college, college and above), race (White/ Caucasian, Black/African American, and other), ethnicity (Hispanic, not Hispanic), marital status (married, single, separated/divorced, widowed), and SES. SES was gauged using the net worth variable (Chien et al., 2013) or the sum of all wealth components (e.g., salary, house, automobile) minus total debt. This variable was converted into an ordinal scale whereby participants were divided into quintiles according to net worth representing lower, lower middle, middle, upper middle, and upper SES. Categorical variables were dummy coded, with the following reference categories: White/Caucasian for race, married for marital status, middle net worth quintile for SES, high school graduate for education, not Hispanic for ethnicity, and male for sex.
Isolation.
Objective isolation was defined as the frequency of contact with social network. Participants reported how often they “Meet up (includes both arranged and chance meetings),” “Speak on the phone,” and “Write or email” their children, other family members, and friends. Responses consisted of “Three or more times a week,” “Once or twice a week,” “Once or twice a month,” “Every few months,” “Once or twice a year,” and “Less than once a year or never.” Values were reverse coded and averaged across all items to create an overall measure of objective isolation; if more than one item was missing, the total score was set to missing (Smith et al., 2013).
Depression.
Depression was measured using the Center for Epidemiologic Studies Depression Scale—Revised (CESD-R). Participants were asked if (yes/no) they had experienced the following over the past week: “I felt depressed,” “I felt that everything I did was an effort,” “My sleep was restless,” “I was happy,” “I felt lonely,” “I enjoyed life,” “I felt sad,” and “I could not get going.” The items “My sleep was restless” and “I felt lonely” were excluded from the total scale score for this study, as they tap into sleep and loneliness, respectively. A composite score of the remaining items was created by summing all items (with the items “I was happy” and “I enjoyed life” reverse coded).
Analyses
A cross-lagged panel model was run to examine the relationship between loneliness and sleep disturbance in 2006, 2010, and 2014. A second cross-lagged panel model was then run, controlling for demographics, depression, and objective isolation. To create the first cross-lagged panel model, the model began with all of the direct paths drawn (i.e., fully saturated), then paths with p < .01 were trimmed successively following a procedure by Meyers, Gamst, and Guarino (2013). The final model was then used as the foundation for the second cross-lagged panel model, which additionally controlled for demographics, depression, and objective isolation.
Expectation maximization (EM) was used to account for missing data, as data were not missing completely at random (MCAR), per examination of the data and significant findings on Little’s MCAR test (p < .001). EM is an algorithm that computes maximum likelihood estimates based on the existing data through the iteration of the expectation step and the maximization step (Dempster et al., 1977). Data preparation (including descriptive statistics) was conducted in SAS 9.4, EM was conducted in IBM SPSS Statistics 25, and path analysis was conducted in IBM SPSS AMOS 25. Raw materials (code and output files) for this study are available on the Open Science Framework (https://osf.io/tv2dg/?view_only=bcd61924a7604c8ab642f4d31ac3576e).
Results
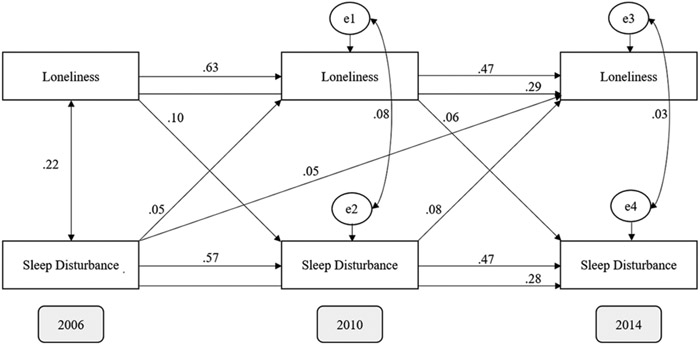
See Figure 1 for the cross-lagged panel model fit using time points 2006, 2010, and 2014 with standardized estimates. The path between loneliness in 2006 and sleep disturbance in 2014 was trimmed (p = .036) to generate the model presented in Figure 1. The chi-square (χ2) goodness-of-fit test was significant, which typically indicates poor model fit, χ2(1) = 4.380, p = .036. However, χ2 statistics are sensitive to large sample size (Bowen & Guo, 2011), rendering this test uninformative in the present study. The root mean square of approximation (RMSEA) was .03 (wherein .08 or lower is reflective of adequate fit and .05 or lower of good fit), comparative fit index (CFI) was 1.00, goodness-of-fit index (GFI) was 1.00, all of which met criteria for adequate fit (≥.90).
Figure 1.
Bivariate (unadjusted) cross-lagged panel model (2006, 2010, 2014), with standardized regression weights. All paths are significant (p < .001).
All paths in this model were significant (ps < .001). The effect sizes of the paths from loneliness to sleep disturbance (2006 to 2010: β = .10, B = .09, standard error (SE) =.01; 2010 to 2014: β = .06, B = .05, SE = .01) and sleep disturbance to loneliness (2006 to 2010: β = .05, B = .05, SE = .01; 2010 to 2014: β = .08, B = .08, SE= .01) were small. There was an additional path between sleep disturbance in 2006 and loneliness in 2014 (β = .05, B = .04, SE = .01). This pattern of cross-lag path estimates suggested that initially loneliness was more causally dominant in its relationship with sleep disturbance, but the reverse was true in the second part of the model. This is reflective of likely reciprocal causality between loneliness and sleep disturbance.
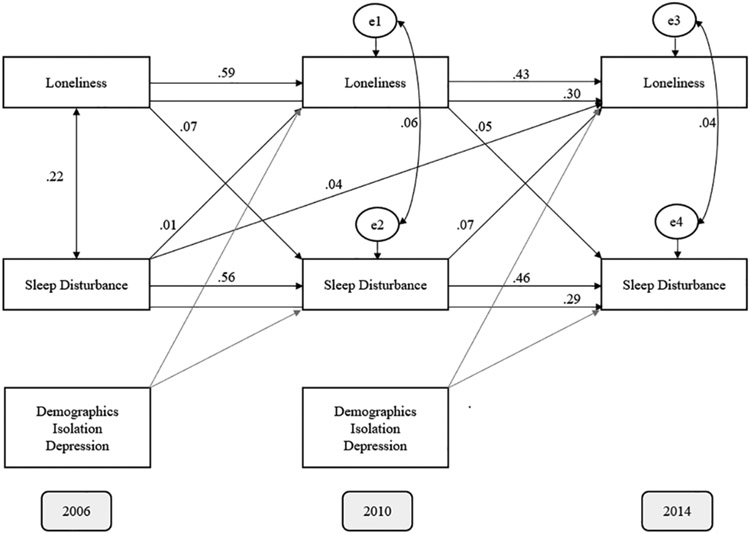
See Figure 2 for the cross-lagged panel model (2006, 2010, 2014; standardized regression weights) with adjustments for age, gender, education, race, ethnicity, objective isolation, depression, marital status, and SES. The χ2 goodness-of-fit test was significant, χ2(506) = 64,327.72, p < .001. The RMSEA was .16, CFI was .17, and GFI was .61. None of these indices reflected adequate fit, which would be expected with a model that includes potential confounds.
Figure 2.
Adjusted cross-lagged panel model (2006, 2010, 2014), with standardized regression weights for paths of interest. All paths are significant (p < .001) with the exception of the path from 2006 sleep disturbance to 2010 loneliness.
The paths from loneliness to sleep disturbance (2006 to 2010: β = .07, B = .06, SE = .01, p < .001; 2010 to 2014: β = .05, B = .06, SE = .01, p < .001) and sleep disturbance to loneliness (2006 to 2010: β = .01, B = .01, SE = .01, p = 61; 2010 to 2014: β = .07, B = .06, SE = .01, p < .001; 2006 to 2014: β = .04, B = .04, SE = .01, p < .001) were attenuated by the inclusion of adjustments in the model, though the majority of paths remained significant.
Discussion
Loneliness was positively associated with sleep disturbance at baseline; this association remained significant but was attenuated in subsequent waves after taking into account previous loneliness and sleep disturbance. Loneliness and sleep disturbance predicted one another over time, suggesting reciprocal causality between loneliness and sleep disturbance, but effect sizes were small (ranging from β = .05 to .09). Controlling for potential confounds—namely demographics, objective isolation (limited contact with social network), and depression—weakened the size of effects, yet findings remained with the exception of 2006 sleep disturbance no longer predicting 2010 loneliness.
The detection of a bivariate association between loneliness and sleep disturbance is consistent with the prior literature, which has demonstrated a correlation between loneliness and sleep problems across a wide array of measures and samples (Aanes et al., 2011; Cacioppo et al., 2002; Cheng et al., 2015; Chu et al., 2016; Hom et al., 2017; McHugh et al., 2011; Segrin & Burke, 2015; Stickley et al., 2015). This study built upon this literature by replicating this finding in a sample that is better equipped to speak to the experience of older Americans. Furthermore, this study extends the previous literature by finding evidence to suggest that these variables likely operate in a reciprocal feedback loop.
This is the first study to examine the reciprocal effects of loneliness and sleep disturbance using a cross-lagged panel model, which allows for the joint examination of effects to speak to causal dominance. Through mapping how change in each variable predicts the subsequent change in the other variable across multiple time points, cross-lagged models provide unique insight onto the directionality of effect. These findings are consistent with previous findings in the literature identifying loneliness as a risk factor for sleep disturbance and vice versa (Hom et al., 2017; Jacobs et al., 2006; Jaremka et al., 2014; McHugh & Lawlor, 2013; Simon & Walker, 2018; Zawadzki et al., 2013), but is one of the first studies to examine these effects jointly to identify reciprocal effects.
The present study found that loneliness and sleep were bidirectionally related. The reciprocal nature of this relationship requires revision to the Cacioppo and Hawkley (2003, 2009) model, which posited that loneliness disrupts sleep but not the reverse. Importantly, cross-lagged panel modeling cannot establish causality, but it can infer causality via the comparative size of effects—that is to say, if one variable predicts another more strongly than the reverse across multiple intervals, it indicates that this variable is causally dominant. Therefore, although the current study indicates that the direction of effects is reciprocal, it remains unclear whether these reciprocal effects are causal, as third variables not controlled for in the current study could still be accounting for this relationship. Future research should evaluate whether outside factors are driving the fluctuations in both loneliness and sleep disturbance. However, the present study provides evidence of reciprocal causality between loneliness and sleep disturbance, requiring that the Cacioppo and Hawkley (2003, 2009) model be revised to include joint effects between loneliness and sleep disturbance and suggesting that treatment efforts aimed at sleep disturbance may indirectly improve loneliness.
It remains unclear how loneliness may exacerbate sleep disturbance and vice-versa. The seminal work on sleep disturbance as a mechanism for the relationship between loneliness and health did not speculate as to how loneliness would disrupt sleep (Cacioppo et al., 2002; Cacioppo, Hawkley, Crawford, et al., 2002). One way in which loneliness could affect sleep is through increased physiological arousal, whereby a person who feels lonely constantly feels more vulnerable than others. Cacioppo and Hawkley (2003, 2009) identified hypothalamic-pituitary-adrenal (HPA) axis activation as a separate mechanism underlying loneliness and health. However, it is likely that increased arousal is entangled with the relationship between loneliness and sleep. The HPA axis controls the output of glucocorticoids, which are integral to the sleep-wake cycle in humans (Oster et al., 2016). Moreover, experimental research indicates that sleep deprivation and restriction impair HPA functioning. Collectively, these findings suggest HPA axis involvement in the reciprocal effects between loneliness and sleep disturbance, but research is necessary to more closely examine this possibility. Furthermore, it is important to elucidate how sleep disturbance may elicit loneliness. Two possibilities are that (a) the time spent awake while trying to sleep fosters distress about perceived isolation and that (b) sleep deprivation hinders a person’s ability to connect with others. Further research is necessary to test these hypotheses as well as other potential ways in which sleep disturbance may worsen loneliness.
The effects detected in these models, though statistically significant, are small. However, the small effect sizes may be attributable to evaluating these variables over the course of years. It would be surprising to detect large effects, given that loneliness and sleep disturbance both fluctuate over time. As a result, it is possible that a person who is lonely at baseline may no longer be lonely 4 years later. The detection of very small reciprocal effects across the span of years may reflect larger reciprocal effects that are occurring day to day between loneliness and sleep disturbance.
Strengths, Limitations, and Future Directions
The present study must be interpreted in the context of its strengths and limitations. A strength of the present study is its sample. The HRS sample draws from a wide range of Americans across the country and is thus better able to speak to older Americans than the previous literature which was limited by the use of convenience samples (e.g., residents of a Chicago condominium) in the studies conducted in the United States. Moreover, there was sufficient statistical power to assess effects that may have otherwise been undetected due to the 4-year lag between measurements. A second strength of the study is that it controlled for potential confounds, to include demographics, objective isolation, and depression, and was thus able to rule out the possibility that findings were entirely attributable to any of the factors included in the model. A third strength of the study is its longitudinal design, which allowed for the determination of the direction of relationships. Furthermore, the use of a cross-lagged panel model allowed for the joint examination of loneliness and sleep disturbance.
However, the study also has several limitations which underline the need for future research to better understand the connection between loneliness and sleep. First, though this study used scales rather than single measurement—a strength relative to much of the literature in the area thus far—these scales were not the best measurement of loneliness and sleep disturbance available. The Hughes Loneliness Scale is an abbreviated version of the University of California, Los Angeles (UCLA) loneliness scale and has been assessed for psychometric properties, but the sleep scale has not been validated. It is critical that future studies replicate the present findings using a sleep scale that has been shown to have adequate validity and reliability.
Second, there was a high rate of attrition in the present study. By 2014, there were data on the Hughes Loneliness Scale for only 51% of the original sample. Moreover, this attrition did not appear to be MCAR, but rather selective whereby certain participants were more likely to be lost to follow-up than others. Participants who were lost to follow-up were on average lonelier, older, lower SES, and less educated and were more likely to be male and widowed or separated/divorced. It is possible that selective attrition obscured effects: if participants suffering from loneliness were less likely to remain in the study, then the connection between loneliness and sleep disturbance over time would be more difficult to detect. However, the current study sought to mitigate the potential of attrition bias through the use of EM to account for missing data.
Third, the present study did not examine the interplay between potential confounds and the variables of interest. Controlling for other factors, though critical, does not shed light on how these factors are involved. Loneliness, sleep disturbance, and health do not occur in a vacuum, but rather are facets of a broader human experience. Further research is necessary to understand how other factors—such as age, demographics, and depressive symptoms—shape the relationship between loneliness and sleep. Moreover, additional research is necessary to examine other components of the Cacioppo and Hawkley (2003, 2009) model—for example, the role of hypervigilance for social threats, attentional and memory biases, negative affect, and HPA activation—and assess other models seeking to explain how loneliness could damage health.
Fourth, it is important to disentangle the effects of different social factors on health (Beller & Wagner, 2018). For example, loneliness and social isolation are comparable risk factors for mortality (Holt-Lunstad et al., 2015), yet only modestly correlated, suggesting that different mechanisms are involved. Further research is necessary to identify overlapping and discrete mechanisms across specific social factors, for example, loneliness versus isolation. Furthermore, future research is necessary to examine how health factors (e.g., chronic pain, functional limitations, medical conditions) tie into the relationship between sleep disturbance and health. Specifically, it is critical that future studies assess whether sleep disturbance mediates the relationship between loneliness and health, as hypothesized by Cacioppo and Hawkley (2003, 2009). This line of research is also necessary to establish that health factors are not driving the connection between loneliness and sleep disturbance.
Conclusion
The present study represents an important step in uncovering the mechanisms underlying the association between loneliness and health in older Americans. Understanding the biopsychosocial interactions shaping the health and well-being of older Americans enables the development of prevention and intervention strategies, which in turn promise to improve quality of life, health outcomes, and longevity for this rapidly growing population. Older adults possess both strengths and vulnerabilities for weathering loneliness (Charles, 2010). On one hand, older adults generally enjoy improved emotion regulation, present awareness, and positivity bias, in conjunction with a preference for emotionally fulfilling relationships (Carstensen et al., 1999), all of which could protect against loneliness. On the other hand, older adults are at greater risk for certain events that may trigger loneliness (Charles, 2010). In addition, older adults are at greater risk for health conditions that may hinder their ability to spend time with others and are also at increased risk of sustaining major changes to their social network, as friends, siblings, and partners die. These changes in social network may be particularly destructive in older adults, who per the Socioemotional Selectivity Theory have trimmed their social networks to prioritize meaningful relationships (Carstensen et al., 1999). As members of this smaller inner circle die, the potential for subsequent loneliness thus may be higher. Moreover, if chronic loneliness occurs, ensuing arousal is likely to precipitate greater health consequences due to age-related changes in cardiovascular functioning, neuroendocrine functioning, and sleep architecture (Charles, 2010; Miner & Kryger, 2017; Ohayon et al., 2004).
This heightened vulnerability makes research examining interactions across biological, psychological, and social factors particularly vital for prevention and intervention. The present study identified sleep as a risk factor for loneliness, suggesting that improving sleep could have cascading benefits on loneliness. This finding is promising in light of the success of behavioral sleep medicine interventions for insomnia (Dzierzewski et al., 2018; Qaseem et al., 2016). Furthermore, this study illustrates how the heightened level of influence between biological, psychological, and social factors in older adults (Garroway & Rybarczyk, 2015) is not unidirectional but rather reciprocal. Further research to understanding these interactions is critical to improve the health and quality of life for the rising number of older Americans.
Acknowledgments
Thanks to Drs Lageman and Dautovich for their valuable feedback on this project.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number K23AG049955 (PI: Dzierzewski).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aanes MM, Hetland J, Pallesen S, & Mittelmark MB (2011). Does loneliness mediate the stress-sleep quality relation? the Hordaland Health Study. International Psychogeriatrics, 23(6), 994–1002. 10.1017/S1041610211000111 [DOI] [PubMed] [Google Scholar]
- Beller J, & Wagner A (2018). Disentangling loneliness: Differential effects of subjective loneliness, network quality, network size, and living alone on physical, mental, and cognitive health. Journal of Aging and Health, 30(4), 521–539. [DOI] [PubMed] [Google Scholar]
- Bowen NK, & Guo S (2011). Structural equation modeling. Oxford University Press. [Google Scholar]
- Cacioppo JT, & Hawkley LC (2003). Social Isolation and Health, with an Emphasis on Underlying Mechanisms. Perspectives in Biology and Medicine, 46(3), S39–S52. 10.1353/pbm.2003.0049 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Bernston GC, Ernst JM, Gibbs AC, Stickgold R, & Hobson JA (2002). Do lonely days invade the nights? Potential social modualation of sleep efficiency. Psychological Science, 13(4), 384–387. 10.1111/j.0956-7976.2002.00469.x [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, & Hawkley LC (2009). Perceived social isolation and cognition. Trends in Cognitive Science, 13(10), 447–454. 10.1016/j.tics.2009.06.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford E, Ernst JM, Burleson MH, Kowalewski RB, … Berntson GG (2002). Loneliness and health: Potential mechanisms. Psychosomatic Medicine, 64(3), 407–417. DOI: 0033-3174/02000/6403-0407 [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, & Charles ST (1999). Taking time seriously: A theory of socioemotional selectivity. American Psychologist, 54(3), 165–181. [DOI] [PubMed] [Google Scholar]
- Charles ST (2010). Strength and vulnerability integration (SAVI): A model of emotional well-being across adulthood. Psychological Bulletin, 136(6), 1068–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng P, Jin Y, Sun H, Tang Z, Zhang C, Chen Y, … Huang F (2015). Disparities in prevalence and risk indicators of loneliness between rural empty nest and non-empty nest older adults in Chizhou, China. Geriatrics and Gerontology International, 15(3), 356–364. 10.1111/ggi.12277 [DOI] [PubMed] [Google Scholar]
- Chien S, Campbell N, Hayden O, Hurd M, Main R, Mallett J, … St Clair P (2013, September). RAND HRS data documentation, version M. RAND Center for the Study of Aging. [Google Scholar]
- Chu C, Hom MA, Rogers ML, Ringer FB, Hames JL, Suh S, & Joiner TE (2016). Is Insomnia Lonely ? Exploring Thwarted Belongingness as an Explanatory Link between Insomnia and Suicidal Ideation in a Sample of South Korean University Students. Journal of Clinical Sleep Medicine, 12(5), 647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, Fisher G, House J, Smith J, & Weir D (2008). Guide to content of the HRS psychosocial leave-behind participant lifestyle questionnaires : 2004 & 2006. HRS Psychosocial Working Group: Survey Research Center, Institute for Social Research, University of Michigan, pp. 1–48. [Google Scholar]
- Dempster AP, Laird NM, & Rubin DB (1977). Maximum likelihood from incomplete data via the EM algorithm. Journal of the Royal Statistical Society: Series B (Methodological), 39(1), 1–22. [Google Scholar]
- Dzierzewski JM, Griffin SC, Ravyts S, & Rybarczyk B (2018). Psychological interventions for late-life insomnia: Current and emerging science. Current Sleep Medicine Reports, 4(4), 268–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garroway AM, & Rybarczyk B (2015). Aging, chronic disease, and the biopsychosocial model In Lictenberg PA & Mast BT (Eds.), APA handbook of clinical geropsychology, Volume 1: History and status of the field and perspectives on aging (pp. 563–586). APA Books. [Google Scholar]
- Hayley AC, Downey LA, Stough C, Sivertsen B, Knapstad M, Øverland S, … Ober C (2017). Social and emotional loneliness and self-reported difficulty initiating and maintaining sleep (DIMS) in a sample of Norwegian university students. Scandinavian Journal of Psychology, 58(1), 91–99. 10.1111/sjop.12343 [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hom MA, Hames JL, Bodell LP, Buchman-Schmitt JM, Chu C, Rogers ML, … Joiner TE (2017). Investigating insomnia as a cross-sectional and longitudinal predictor of loneliness: Findings from six samples. Psychiatry Research, 253, 116–128. 10.1016/j.psychres.2017.03.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs JM, Cohen A, Hammerman-Rozenberg R, & Stessman J (2006). Global sleep satisfaction of older people: The Jerusalem Cohort Study. Journal of the American Geriatrics Society, 54(2), 325–329. 10.1111/j.1532-5415.2005.00579.x [DOI] [PubMed] [Google Scholar]
- Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, … Kiecolt-Glaser JK (2014). Pain, depression, and fatigue: Loneliness as a longitudinal risk factor. Health Psychology, 33(9), 948–957. 10.1037/a0034012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins CD, Stanton B-A, Niemcryk SJ, & Rose RM (1988). A scale for the estimation of sleep problems in clinical research. Journal of Clinical Epidemiology, 41(4), 313–321. [DOI] [PubMed] [Google Scholar]
- Kurina LM, Knutson KL, Hawkley LC, Cacioppo JT, Lauderdale DS, & Ober C (2011). Loneliness is associated with sleep fragmentation in a communal society. Sleep, 34(11), 1519–1526. 10.5665/sleep.1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Chopik WJ, & Schiamberg LB (2017). Longitudinal associations between marital quality and sleep quality in older adulthood. Journal of Behavioral Medicine, 40(5), 821–831. [DOI] [PubMed] [Google Scholar]
- Matthews T, Danese A, Gregory AM, Caspi A, Moffitt TE, & Arseneault L (2017). Sleeping with one eye open: Loneliness and sleep quality in young adults. Psychological Medicine, 47(12), 2177–2186. 10.1017/S0033291717000629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh JE, Casey AM, & Lawlor BA (2011). Psychosocial correlates of aspects of sleep quality in community-dwelling Irish older adults. Aging & Mental Health, 15(6), 749–755. 10.1080/13607863.2011.562180 [DOI] [PubMed] [Google Scholar]
- McHugh JE, & Lawlor BA (2013). Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. British Journal of Health Psychology, 18(3), 546–555. 10.1111/j.2044-8287.2012.02101.x [DOI] [PubMed] [Google Scholar]
- Meyers LS, Gamst GC, & Guarino AJ (2013). Performing data analysis using IBM SPSS. John Wiley & Sons. [Google Scholar]
- Miner B, & Kryger MH (2017). Sleep in the aging population. Sleep Medicine Clinics, 12(1), 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon MM, Carskadon MA, Guilleminault C, & Vitiello MV (2004). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep, 27(7), 1255–1273. [DOI] [PubMed] [Google Scholar]
- Oster H, Challet E, Ott V, Arvat E, de Kloet ER, Dijk D-J, … Van Cauter E (2016). The functional and clinical significance of the 24-hour rhythm of circulating glucocorticoids. Endocrine Reviews, 38(1), 3–45. https://dx.doi.org/10.1210%2Fer.2015-1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qaseem A, Kansagara D, Forciea MA, Cooke M, & Denberg T (2016). Management of chronic insomnia disorder in adults : A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 165, 125–133. 10.7326/M15-2175 [DOI] [PubMed] [Google Scholar]
- Segrin C, & Burke TJ (2015). Loneliness and sleep quality: Dyadic effects and stress effects. Behavioral Sleep Medicine, 13(3), 241–254. 10.1080/15402002.2013.860897 [DOI] [PubMed] [Google Scholar]
- Simon B, & Walker MP (2018). Sleep loss causes social withdrawal and loneliness. Nature Communications, 9(1), 3146 10.1038/s41467-018-05377-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, Fisher G, Ryan L, Clarke P, House J, & Weir D (2013). Psychosocial and lifestyle questionnaire. Survey Research Center, Institute for Social Research. [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, & Weir DR (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stickley A, Koyanagi A, Leinsalu M, Ferlander S, Sabawoon W, & McKee M (2015). Loneliness and health in Eastern Europe: Findings from Moscow, Russia. Public Health, 129(4), 403–410. 10.1016/j.puhe.2014.12.021 [DOI] [PubMed] [Google Scholar]
- Yu B, Steptoe A, Niu K, Ku P-W, & Chen L-J (2017). Prospective associations of social isolation and loneliness with poor sleep quality in older adults. Quality of Life Research, 27(3), 683–691. 10.1007/s11136-017-1752-9 [DOI] [PubMed] [Google Scholar]
- Zawadzki MJ, Graham JE, & Gerin W (2013). Rumination and anxiety mediate the effect of loneliness on depressed mood and sleep quality in college students. Health Psychology, 32(2), 212–222. 10.1037/a0029007 [DOI] [PubMed] [Google Scholar]