Abstract
Objective
This study was performed to analyze the clinical, radiographic, and pathological features of hand angioleiomyoma causing nerve compression and assess the outcomes of surgical excision.
Methods
This case series included three men and one woman (mean age, 53.3 years; range, 49–56 years). The patients’ chief complaint was numbness of the fingers. The patients’ medical histories were reviewed, and the diagnosis of angioleiomyoma with nerve compression was confirmed by means of imaging examination and pathological analysis.
Results
Three tumors occurred in the palm and one in the finger, and the average maximum tumor diameter was 1.8 cm (range, 0.8–2.6 cm). Preoperative magnetic resonance imaging demonstrated well-defined masses with isointense signals on T1 sequences, hyperintense signals on T2 sequences, and strong heterogeneous enhancement after injection of contrast material. All tumors were located near nerves, leading to nerve compression. The diagnosis of angioleiomyoma was confirmed by postoperative pathology. Finger sensation recovered and no recurrence was found during an average follow-up of 37 months (range, 25–59 months).
Conclusions
Angioleiomyoma should be considered among the differential diagnoses of hand tumors and timely resection should be performed, particularly if the mass is causing numbness and/or pain with positive Tinel’s sign and/or tenderness.
Keywords: Angioleiomyoma, hand, nerve compression, numbness, microsurgery, tumor resection, Tinel’s sign
Introduction
Angioleiomyoma is a benign tumor arising from the tunica media layer of vessels.1–4 It was first described in 1937.5 The understanding of angioleiomyoma has gradually deepened since Morimoto6 classified this tumor according to location in 1973.
Angioleiomyoma rarely occurs in the hand because of the paucity of smooth muscle in this region. Hachisuga et al.7 reported 562 cases of angioleiomyoma in 1984; among these tumors, 89% occurred in the extremities while only 56 cases occurred in the hand. According to another study, angioleiomyoma accounted for less than 1% of all soft tissue tumors within the upper extremity.8 Angioleiomyoma is considered an uncommon benign lesion with a long course and has not received adequate clinical attention, leading to missed diagnosis and misdiagnosis. Most recorded cases are single case presentations. Thus, the etiology and pathogenesis of angioleiomyoma remain unclear. This tumor is often confused with a giant cell tumor of the tendon sheath, ganglion cyst, hemangioma, schwannoma, neurofibroma, and glomus tumor, which are considered the most common types of hand tumors.2,9–11 Only one reported case of hand angioleiomyoma included occasional symptoms of nerve compression.12 No case series of angioleiomyoma have included this symptom. However, we encountered four patients with numbness as their chief complaint. The present case series describes these four patients with hand angioleiomyomas, focusing on their nerve compression symptoms, diagnosis, and treatment outcomes.
Methods
We reviewed four cases of angioleiomyoma involving the palm or finger at the Department of Orthopedics, The First Affiliated Hospital, Zhejiang University from January 2011 to January 2017. Three of the four patients in this series were male and one was female, with a mean age of 53.3 years (range, 49–56 years). No patients had a history of obvious trauma. The tumors had grown slowly from their initial detection to surgical treatment, the duration of which ranged from 6 months to 10 years. The reason that the patients sought treatment was not the mass but numbness of the affected side of the finger. Two patients reported occasional mild pain. The patients’ basic information, symptoms and signs, clinical photographs, and histologic specimens were reviewed. During the surgical excision, the general character of the tumors and their relationship to surrounding vessels and nerves were examined. Hematoxylin- and eosin-stained slides of all four tumors were reviewed.
This study protocol was approved by the Medical Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University. All patients provided written informed consent for publication of their clinical details and clinical images.
Results
All tumors occurred on the hand; three were located in the palm near the metacarpophalangeal joints, and one was located in the middle phalanx of the index finger. Physical examination revealed a subcutaneous oval/round mass with a mean maximum diameter of 1.8 cm (range, 0.8–2.6 cm), positive Tinel’s sign, and impaired finger sensation as verified by a two-point discrimination test. Laboratory studies revealed no abnormalities in routine blood tests, the C-reaction protein level, or tumor marker levels. Magnetic resonance imaging (MRI) is the most helpful imaging modality for determining whether the mass is intrinsic or extrinsic to the nerve, delineating involvement of adjacent structures, and determining the malignant nature of hand tumors.13 Therefore, each of the four patients underwent preoperative MRI with a 3.0-T imager (GE Medical Systems, Milwaukee, WI, USA). Spin-echo T1-weighted images (repetition time/echo time, 600/22) and T2-weighted images (repetition time/echo time, 4000/42) were obtained. MRI was also performed after a rapid bolus injection of 0.1 mmol/kg of gadopentetate dimeglumine (Magnevist; Bayer Schering Pharma, Berlin, Germany) into the cubital vein. The MRI findings of the four tumors were highly consistent. MRI demonstrated well-defined superficial masses that appeared isointense to the surrounding muscular tissue on T1 sequences, appeared hyperintense on T2 sequences, and showed strong heterogeneous enhancement after injection of contrast material. According to the clinical symptoms and imaging manifestations, mainly the MRI features, the patients were initially diagnosed with a hemangioma or giant cell tumor of the tendon sheath; i.e., all of the patients were misdiagnosed before resection. The final diagnosis was achieved by postoperative pathologic examination. During the operation, all of the tumors in this case series were found to be adjacent to the neurovascular bundle, leading to compression of the palmar digital nerve or unilateral digital nerve (Figure 1).
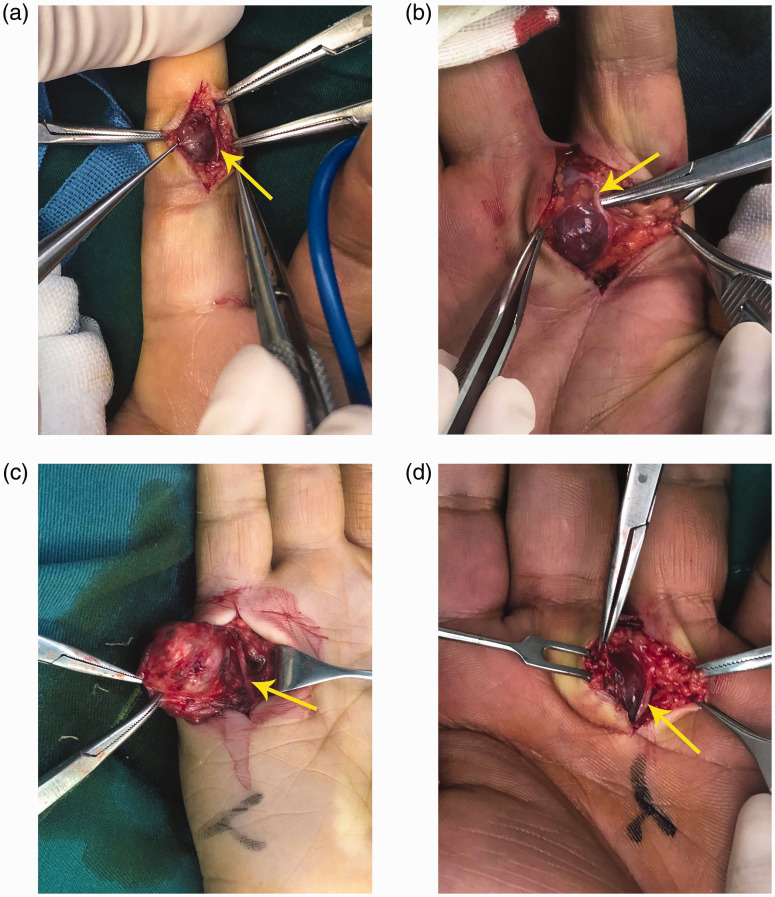
Figure 1.
Intraoperative presentation of the tumors. All tumors appeared well encapsulated and very close to the palmar digital nerve or digital nerve, pushing it to one side (arrow). (a) The angioleiomyoma in Patient 1 compressed digital nerve of the index finger. (b) The angioleiomyoma in Patient 2 compressed the palmar digital nerve to the index finger. (c) The angioleiomyoma in Patient 3 compressed the palmar digital nerve to the little finger. (d) The angioleiomyoma in Patient 4 compressed the palmar digital nerve to the ring finger.
The tumor was exposed through a volar zigzag incision. Mild epineurial scarring was observed under a surgical microscope at ×10 magnification (OPMI Vario; Carl Zeiss Surgical GmbH, Jena, Germany). After the feeding artery was ligated and the tumor was marginally excised, the affected epineurium was released with a microsurgical technique. The whole process was performed under the microscope. Grossly, the excised tumors were smooth, well-demarcated, whitish or reddish, hemorrhagic, elastic masses with a mean diameter of 1.8 cm. Histologically, all were solid tumors. Pathological analysis revealed interlacing and spindle-shaped tumor cell bundles as well as numerous slit-like vascular channels embedded within a smooth muscle component. The pathological diagnosis was angioleiomyoma. All patients underwent simple wound closure after resection. The digits had full range of movement before and after the operation without signs of ischemia. The patients’ clinical features are summarized in Table 1.
Table 1.
Clinical features of four patients with hand angioleiomyoma.
| Patient No. | Sex | Age, years | Duration of symptoms | Symptoms | Tumor location | Size, cm | Compressed nerve | Preoperative diagnosis |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 49 | 0.5 year | Numbness | Finger | 0.8 | Ulnar digital nerve of the index finger | GCTTS |
| 2 | M | 56 | 1 year | Numbness, mild pain | Palm | 2.2 | Ulnar palmar digital nerve to the index finger | Hemangioma |
| 3 | M | 54 | 10 years | Numbness | Palm | 2.6 | Ulnar palmar digital nerve to the little finger | GCTTS |
| 4 | M | 54 | 2 years | Numbness, mild pain | Palm | 1.6 | Radial palmar digital nerve to the ring finer | Hemangioma |
F, female; M, male; GCTTS, giant cell tumor of the tendon sheath.
All patients were instructed to take 500-µg mecobalamin tablets (Eisai, Tokyo, Japan) three times a day for 1 to 3 months postoperatively. Sensation turned to normal throughout the digit in all patients within 6 months as confirmed by a two-point discrimination test. During the average follow-up period of 37 months (range, 25–59 months), no patients developed recurrence or grip strength loss.
Representative case
A 56-year-old man presented with an approximately 1-year history of a well-defined mass on the ulnar side of the metacarpophalangeal joint of his right index finger. He reported having experienced no sensation impairment until 6 months previously, when the mass had grown to bean-size. He had experienced numbness of the index finger during the most recent few months, which was his chief complaint and reason for seeking treatment. The numbness was sometimes accompanied by mild pain. The patient denied any history of trauma in the affected region. Physical examination revealed a subcutaneous, slightly mobile, soft oval-shaped mass of about 2.2 × 1.5 cm in size without skin changes. It was tender to palpation and showed positive Tinel’s sign. Sensory impairment in the ulnar aspect of the index finger was verified by means of two-point discrimination. MRI demonstrated a well-demarcated subcutaneous isointense mass on T1 sequences, hyperintensity on T2 sequences with isointense areas in the mass, and strong heterogeneous enhancement after injection of contrast material (Figure 2).
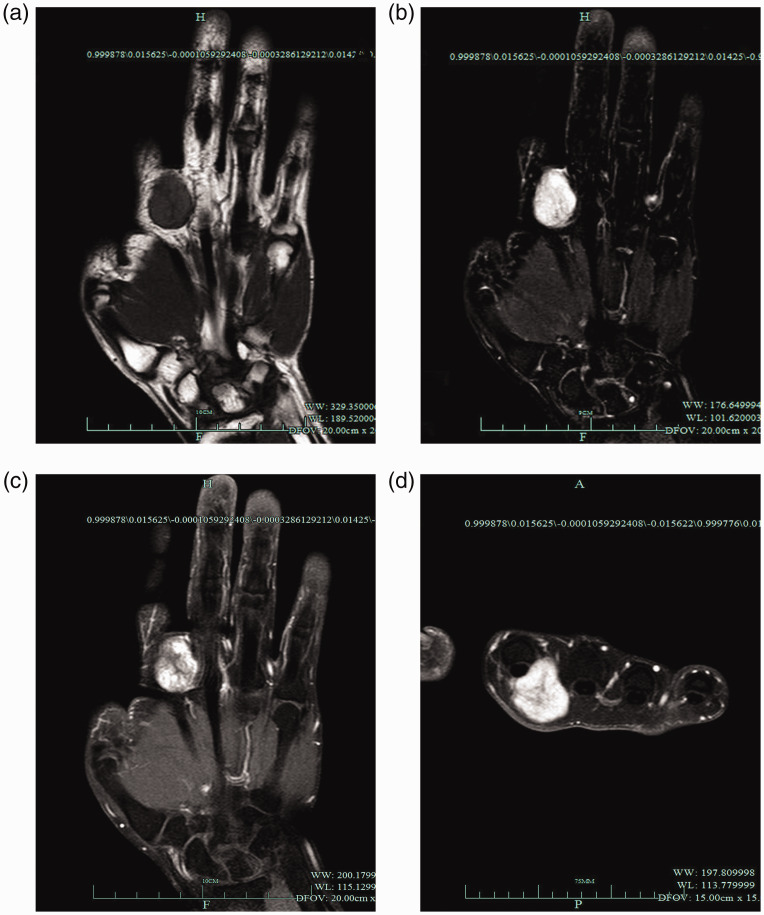
Figure 2.
Magnetic resonance imaging manifestations of a representative case (Patient 2). (a) Magnetic resonance imaging determined a well-demarcated mass isointense to the muscles on T1 sequences. (b) The mass was hyperintense on T2 sequences with isointense areas inside. (c) After injection of contrast material, strong heterogeneous enhancement was observed inside the mass. (d) In transverse section, the tumor showed strong heterogeneous enhancement consistent with the coronal section.
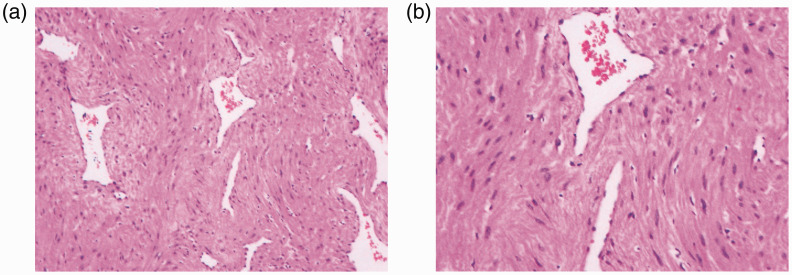
The mass was well encapsulated and close to the palmar digital nerve, pushing it to one side (Figure 1(b)). Careful separation, resection, and neurolysis were performed under microscopy. The final pathologic diagnosis was consistent with an angioleiomyoma (sized 2.2 × 1.5 × 1.0 cm). The tumor was well circumscribed and consisted of short spindle-shaped cells, slit-like vascular channels, and smooth muscle tissue with neither cytological atypia nor mitotic activity (Figure 3). Hemosiderin deposits could be seen in the mesenchyme. Immunohistological markers were positive for smooth muscle (smooth muscle actin and desmin) and vascular tissue (CD31, CD34, and F8-R-Ag).
Figure 3.
Pathological features of a representative case (Patient 2). (a) Microscopic examination revealed a diagnosis of angioleiomyoma, showing short spindle-shaped cells, slit-like vascular channels, and smooth muscle cells in the tumor (hematoxylin and eosin staining; magnification, ×100). (b) The smooth muscle cells and walls of the vessels blended together without cytological atypia and mitotic activity (hematoxylin and eosin staining; magnification, ×200).
During the 2-year follow-up, no recurrence or loss of grip strength occurred, and sensation turned to normal throughout the index digit as confirmed by a two-point discrimination test.
Discussion
Angioleiomyomas may occur throughout the body, including the uterus, esophagus, gastrointestinal stroma, lung pleura, and extremities.7,14–16 They are classified into three subtypes: solid, venous, and cavernous.7 Angioleiomyomas usually present as solitary, painful, and superficial masses that are most common in the lower limbs with a propensity to occur in middle-aged women.2,14,17 Butler et al.18 published the first case of angioleiomyoma of the hand in 1960. All four cases of angioleiomyoma in the present report were located on the hand and characterized not by pain but by symptoms of nerve compression and positive Tinel’s sign, and they occurred in three men and only one woman. As a rare hand tumor, angioleiomyoma has not been systematically found to be characterized by nerve entrapment; it is considered to be a soft, noninvasive mass. However, symptoms of nerve compression were the chief complaint in the present case series. Because the tumor progresses slowly, patients sometimes ignore the mass until numbness develops and gradually worsens.
The etiological factors and mechanism of angioleiomyomas remain unclear. Mechanical factors such as minor trauma, venous stasis, hormonal changes (particularly estrogen), and primary hamartoma or hemangioma changes have been proposed as etiological factors.7,8,19–21 In the present study, local ischemia, nerve compression, and periosteal stimulus caused by the aggravated mass finally resulted in pain1 and numbness.
Angioleiomyomas are benign tumors with slow progression, and they are commonly overlooked. However, some previous reports have described angioleiomyomas that involved arteries,20,22,23 limited the extension of the interphalangeal joints,1 recurred,24 and underwent malignant transformation.7,24,25 Some angioleiomyomas may grow to be huge and develop calcification, hemorrhage, hyalinization, or myxoid degeneration.7,14,26,27
Clinically, it is difficult to differentiate an angioleiomyoma from other subcutaneous lesions of the hand. There are no distinctive symptoms or signs except for pain and/or tenderness, and lesions in the hand are less commonly painful than lesions in the lower limb.19,21,28 Ultrasound and MRI are the main examination methods of hand tumors. The diagnosis of a ganglion cyst can be excluded based on the characteristic MRI features. Glomus tumors usually occur distal to the distal interphalangeal joint and can be discriminated from angioleiomyomas. Radiological findings of angioleiomyomas are compatible with those of a localized form of giant cell tumors of the tendon sheath and hemangiomas. However, these lesions have no specific neurologic presentations. We suggest that an angioleiomyoma should be considered when a mass causes neurologic symptoms. An angioleiomyoma may be misdiagnosed as a neuroma or a benign neoplasm of the peripheral nerves such as a schwannoma, neurofibroma, perineurioma, or ganglioneuroma.29 Moreover, malignant peripheral nerve sheath tumors are uncommon but devastating.30 They may lead to a local mass effect, infiltration of surrounding tissues, or direct nerve invasion.31 Particularly close attention should be paid to the differentiation of intraneural tumors, which are apt to cause nerve compression syndromes as shown in our previous research.32,33 Definitive distinction between angioleiomyomas and peripheral nerve tumors requires pathological examination. The final treatment is directed toward symptomatic control. Notably, micromanipulation of such tumors can be very difficult. We performed the whole process under a surgical microscope to separate the tumor and protect the nerve as much as possible.
To conclude, angioleiomyoma of the hand with nerve compression should not be ignored despite it being a rare condition. It may appear in various locations and can cause disturbing symptoms. We recommend that an angioleiomyoma be considered among the differential diagnoses of hand tumors and that treatment be performed in a timely manner, particularly if the mass has caused numbness and/or pain with positive Tinel’s sign and/or tenderness.
Acknowledgements
We sincerely thank our colleague Dr. HL, who provided support throughout the entire study. We also thank the funding program for sponsoring our research. Finally, we thank Hui Cai for assisting with the figures and ethical principles.
Authors’ contributions
QJJ conceived of the study. HL participated in the design of the study. QJJ drafted the manuscript. Both authors read and approved the final manuscript.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Declaration of conflicting interest
The author(s) declare that there is no conflict of interest.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The data collection and analysis in this study were supported by The National Natural Science Foundation of China (grant number 81702135) and the Zhejiang Provincial Natural Science Foundation (grant number LY20H060007).
ORCID iDs
Qianjun Jin https://orcid.org/0000-0003-3835-910X
References
- 1.Ohtsuka H. Angioleiomyoma of the pulp. J Plast Surg Hand Surg 2014; 48: 285–286. [DOI] [PubMed] [Google Scholar]
- 2.Kulkarni MS, Vijayan S, Naik M, et al. A rare tumour of hand: angioleiomyoma. BMJ Case Rep 2017; 2017: bcr-2017-220005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duhig JT, Ayer JP. Vascular leiomyoma. A study of sixty-one cases. Ama Arch Pathol 1959; 68: 424. [PubMed] [Google Scholar]
- 4.Gassel F, Kraft CN, Wallny T, et al. Soft-tissue angioleiomyoma of the hand as a rare differential diagnosis of haemophilic pseudotumour. Haemophilia 2010; 7: 528–531. [DOI] [PubMed] [Google Scholar]
- 5.Stout AP. Solitary cutaneous and subcutaneous leiomyoma. Amjcancer 1937; 29: 435–469. [Google Scholar]
- 6.Morimoto N. Angiomyoma (vascular leiomyoma): a clinicopathologic study. Med J Kagoshima Univ 1973; 24: 663–683. [Google Scholar]
- 7.Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer 1984; 54: 126–130. [DOI] [PubMed] [Google Scholar]
- 8.Houdek MT, Rose PS, Shon W, et al. Angioleiomyoma of the upper extremity. J Hand Surg Am 2013; 38: 1579–1583. [DOI] [PubMed] [Google Scholar]
- 9.Jiang S, Shen H, Lu H. Multiple schwannomas of the digital nerves and common palmar digital nerves: an unusual case report of multiple schwannomas in one hand. Medicine (Baltimore) 2019; 98: e14605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu H, Chen LF, Chen Q. Rupture of a subungual glomus tumor of the finger. BMC Cancer 2018; 18: 505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu H, Shen H, Chen Q, et al. Artificial finger joint replacement due to a giant cell tumor of the tendon sheath with bone destruction: a case report. Oncol Lett 2015; 10: 3502–3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miyamoto W, Yamamoto S, Kii R, et al. Vascular leiomyoma resulting in ulnar neuropathy: case report. J Hand Surg Am 2008; 33: 1868–1870. [DOI] [PubMed] [Google Scholar]
- 13.Pilavaki M, Chourmouzi D, Kiziridou A, et al. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol 2004; 52: 229–239. [DOI] [PubMed] [Google Scholar]
- 14.Kulkarni AR, Haase SC, Chung KC. Leiomyoma of the hand. Hand (N Y) 2009; 4: 145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hurwitz A. Leiomyoma of the esophagus; report of a case. Surgery 1949; 25: 304–306. [PubMed] [Google Scholar]
- 16.Gupta M, Suryawanshi M, Kumar R, et al. Angioleiomyoma of uterus: a clinicopathologic study of 6 cases. Int J Surg Pathol 2018; 26: 18–23. [DOI] [PubMed] [Google Scholar]
- 17.Huang KC, Lee KF. Angioleiomyoma in the palm of an 11-year-old boy. Skeletal Radiol 2008; 37: 339–341. [DOI] [PubMed] [Google Scholar]
- 18.Butler ED, Hamill JP, Seipel RS, et al. Tumors of the hand: a ten-year survey and report of 437 cases. Am J Surg 1960; 100: 293–302. [DOI] [PubMed] [Google Scholar]
- 19.Callé SC, Eaton RG, Littler JW. Vascular leiomyomas in the hand. J Hand Surg Am 1994; 19: 281–286. [DOI] [PubMed] [Google Scholar]
- 20.Dominguez-Cherit J, Brandariz A. Distal digital angioleiomyoma: a case report and review of the literature. Int J Dermatol 2010; 42: 141–143. [DOI] [PubMed] [Google Scholar]
- 21.Lawson GM, Salter DM, Hooper G. Angioleiomyomas of the hand. A report of 14 cases. J Hand Surg Br 1995; 20: 479–483. [DOI] [PubMed] [Google Scholar]
- 22.Shafi M, Hattori Y, Doi K. Angioleiomyoma of distal ulnar artery of the hand. Hand (N Y) 2010; 5: 82–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yagi K, Hamada Y, Yasui N. A leiomyoma arising from the deep palmar arterial arch. J Hand Surg Br 2006; 31: 680–682. [DOI] [PubMed] [Google Scholar]
- 24.Herren DB, Zimmermann A, Büchler U. Vascular leiomyoma in an index finger undergoing malignant transformation. J Hand Surg Am 1995; 20: 484–487. [DOI] [PubMed] [Google Scholar]
- 25.Neviaser RJ, Newman W. Dermal angiomyoma of the upper extremity. J Hand Surg Am 1977; 2: 271–274. [DOI] [PubMed] [Google Scholar]
- 26.Mok JC, Fan KY, Lui TH. A huge angioleiomyoma of the finger. Hand Surg 2015; 20: 310–312. [DOI] [PubMed] [Google Scholar]
- 27.Dey B, Bharti JN, Gautam P, et al. Angioleiomyoma of the forearm. J Lab Physicians 2014; 6: 53–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hwang JW, Ahn JM, Kang HS, et al. Vascular leiomyoma of an extremity: MR imaging-pathology correlation. AJR Am J Roentgenol 1998; 171: 981. [DOI] [PubMed] [Google Scholar]
- 29.Skovronsky DM, Oberholtzer JC. Pathologic classification of peripheral nerve tumors. Neurosurg Clin N Am 2004; 15: 157–166. [DOI] [PubMed] [Google Scholar]
- 30.Kim DH, Murovic JA, Tiel RL, et al. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg 2005; 102: 246. [DOI] [PubMed] [Google Scholar]
- 31.Mrugala MM, Batchelor TT, Plotkin SR. Peripheral and cranial nerve sheath tumors. Curr Opin Neurol 2005; 18: 604. [DOI] [PubMed] [Google Scholar]
- 32.Li P, Lou D, Lu H. The cubital tunnel syndrome caused by intraneural ganglion cyst of the ulnar nerve at the elbow: a case report. BMC Neurol 2018; 18: 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lu H, Chen LF, Jiang S, et al. A rapidly progressive foot drop caused by the posttraumatic intraneural ganglion cyst of the deep peroneal nerve. BMC Musculoskelet Disord 2018; 19: 298. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.