Abstract
Introduction
In this proof-of-concept study, we introduce a custom-developed robot-assisted training protocol, named “Assist-As-Asked”, aiming at improving arm function of chronic stroke subjects with moderate-to-severe upper extremity motor impairment. The study goals were to investigate the feasibility and potential adverse effects of this training protocol in both physical and virtual environments.
Methods
A sample of convenience of four chronic stroke subjects participated in 10 half-hour sessions. The task was to practice reaching six targets in both virtual and physical environments. The robotic arm used the Assist-As-Asked paradigm in which it helped subjects to complete movements when asked by them. Changes in the kinematics of the reaching movements and the participants’ perception of the reaching practice in both environments were the outcome measures of interest.
Results
Subjects improved their reaching performance and none of them reported any adverse events. There were no differences between the two environments in terms of kinematic measures even though subjects had different opinions about the environment preference.
Conclusions
Using the Assist-As-Asked protocol in moderate-to-severe chronic stroke survivors is feasible and it can be used with both physical and virtual environments with no evidence of one of them to be superior to the other based on users’ perspectives and movement kinematics.
Keywords: Stroke, rehabilitation robotics, robot-assisted therapy, virtual reality, arm reaching, upper extremity, motor learning, chronic hemiplegia
Background
At six months post-stroke, only 5–20% of hemiplegic stroke survivors show complete recovery of arm function while 30–66% show no sign of function in their paretic arm.1 While the intensity of therapy and increase in number of repetitions have been shown to directly impact stroke recovery,2,3 lack of resources and related costs have prevented conventional therapy to be replaced by intensive therapy. Therefore, in stroke survivors who have reached their chronic stage, we are faced with a subpopulation of individuals with moderate-to-severe4 upper limb (UL) motor impairments who are still suffering from decreased UL function, impairing their ability to perform daily activities independently, and are not receiving any rehabilitation services.
While virtual environment (VE)-based rehabilitation systems are mostly used in mild-to-moderate stroke patients,5 properly designed robot-assisted therapy (RT) systems6–8 that target the requirements of moderate-to-severe stroke patients can be exploited in clinical settings and even in home settings9 to provide an intensive therapy which can be more effective than conventional therapy; studies have shown that RT (which takes much less time and effort of a therapist compared to conventional therapy) is as effective as dose-equivalent intensive conventional therapy10 and sometimes even more effective when designed properly, e.g. RT with three-dimensional (3D) tasks.11
A hybrid system in which a robotic device is coupled with a VE might benefit the moderate-to-severe stroke patients. But a question rises about whether this is necessary in the case of moderate-to-severe stroke or not; robots enable moderate-to-severe stroke patients to complete the unsuccessful movements and also can provide feedback about their performance; these are important motivation factors.12 In addition, there is no need for having a complex VE scene for them as higher repetition of simple tasks seems to be preferable than a task-oriented practice where patients have a hard time or are unable to complete the task.13 Thus, in designing such an RT system, the role of robot may be more prominent than the VE itself. Therefore, there is a question as to whether there is any superiority coupling the robot with a VE than coupling it with a physical environment (PE) and whether movements made in the VE are like those made in the PE, when the task requirements are the same.
In this study, we have developed a robot-assisted protocol aiming at improving arm function of chronic stroke subjects with moderate-to-severe upper extremity motor impairment. The “Assist-As-Asked” paradigm is introduced in this new scheme in which the robot only helps a subject when the subject asks specifically for help. As a prerequisite for a large-scale randomized controlled trial, a feasibility study was required. Therefore, we performed this study on four subjects to evaluate the system’s usability and to determine whether our robot-assisted arm reaching protocol is beneficial in retraining the arm function of chronic stroke individuals with moderate-to-severe UL motor impairment. In addition, we evaluated the users’ perceptions about the system in both environments in terms of motivation and preference. We expected that this novel robot-assisted protocol would improve chronic stroke subject’s motor performance over the course of the training and hypothesized that the choice of environment would not affect the kinematics of the reaching task.
Methods
Subjects
For this proof-of-concept study, we recruited a sample of convenience of four chronic stroke subjects from the Greater Montreal area in Canada (Table 1). None of the subjects had hemispatial neglect or any visual problem which was not corrected by eyewear, any UL surgery, any pain interfering with the arm function, any neurological or neuromuscular conditions other than stroke, or any structural changes secondary to stroke (passive range of motion of the elbow and shoulder restricted more than 20°). The study protocol was presented to Centre for Interdisciplinary Research in Rehabilitation (CRIR) research ethics committee in Montreal and got approved by the committee (approval number: CRIR-1051-0215). All subjects provided their written informed consent.
Table 1.
Characteristics of chronic stroke individuals participated in this study.
| Participant | Gender | Age (years) | Handedness | Time since stroke (years) | C-M | FMA-UE | Type of stroke | Side of hemiparesis |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 53.1 | Right | 1.6 | 3 | 15 | Ischemic | Right |
| 2 | M | 59.8 | Right | 2.7 | 3 | 13 | Hemorrhagic | Right |
| 3 | F | 49.0 | Right | 20.9 | 3 | 18 | Ischemic | Right |
| 4 | M | 53.2 | Right | 6.6 | 3 | 14 | Ischemic | Right |
FMA-UE: Upper Extremity section of Fugl-Meyer Assessment.C-M: Arm section of Chedoke-McMaster Stroke Assessment.
RT protocol
The HapticMaster (MOOG Inc.) robotic arm14 was used as the primary tool for providing anti-gravity and guiding force to the subjects when needed and also for measuring the subjects’ arm movements in 3D space. The HapticMaster is a three degree-of-freedom, programmable endpoint robot which spans a workspace of approximately 1 m3, with low friction and is equipped with force and position sensors (Figure 1). The system can be programmed to create pre-defined and feedback-controlled 3D force fields. A forearm splint, in which the subject’s arm is placed, is linked to the robot arm through a universal joint providing three rotational degrees-of-freedom (passive). The robot arm runs at a fixed update rate of 2500 Hz which guarantees a smooth and realistic experience by users. The force can be measured and applied with a precision of 0.01 N and the position measurements are accurate to 0.012 mm.
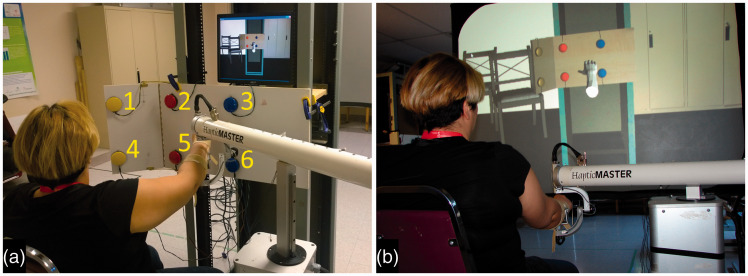
Figure 1.
(a) The physical environment and (b) the virtual environment.
The robot arm assisted the arm movements of subjects in three ways. (A) Virtual Tunnel: before the start of the reaching movement, a virtual tunnel (radius: 4 cm) was created, linking the starting position to the target of interest, thus preventing unwanted deviation of the subjects’ arm movement from the ideal straight-line path. (B) Gravity Support: it always provided gravity support by not letting the subject’s forearm drop. (C) Assist-As-Asked paradigm: when a subject asked for help to complete a movement, the robot arm provided a guiding force to assist the subject in completing the reaching task; when assistance was turned on, the robot produced a virtual spring, with elastic constant of k = 400 N/m. The spring was then moved at a constant velocity of 5 cm/s toward the selected target, thus smoothly helping the subject in reaching that target. The maximum amplitude of the guiding force was set at 150 N. The effect was like having a spring attached between the subject’s forearm and the target, then pulling from the target end of the spring at a constant velocity. During the experiment sessions, the experimenter was near the subject all the time and the robot arm was equipped with software and hardware safety switches, so that the subject or the experimenter could rapidly turn it off.
Experimental setup and procedure
Subjects were required to perform the same reaching task in both PE and VE (Figure 1) in 10 sessions over a course of a month. In each session, subjects were seated on a chair, either in front of a vertical board when performing in PE, or a screen when performing in VE. The affected forearm, i.e. right, was attached to the forearm splint of the robot arm. Based on a pseudo-randomization, subjects either started the experiment in PE followed by VE, or vice versa, in each session.
The experiment in PE consisted of a reaching task to six buttons/targets placed on two rows, each with three buttons with a diameter of 6 cm (Figure 1(a)). The targets were numbered 1, 2, 3 from left to right on the top row and 4, 5, 6 on the bottom row. These six targets were attached to a hinged wooden board. The board was placed so that the middle and right targets (2, 3, 5, and 6) were positioned in front of the subject, parallel to the coronal plane; the two leftmost buttons (1 and 4) were angled at ∼130°. This arrangement of buttons was preferred to account for the shorter range of motions when reaching for the objects placed contralateral to the moving arm. The top and bottom rows of targets were spaced 25 cm apart; the left- and the right-side buttons were placed 15 cm and 30 cm away from the middle buttons, respectively. A light-emitting diode was placed on top of each button. The height of the experiment board was adjusted in a way that the middle bottom target (#5) was at the level of the subject’s xiphoid process of the sternum. Then, based on the subject’s right arm length, the experiment board was moved at a distance from the subject so that 30° of elbow flexion was required to reach the middle bottom target (#5). The starting position was set at 14 cm in front of the xiphoid process of the sternum. This configuration allowed different UL muscle group activations when reaching for the six targets; it covered flexion, extension, and abduction in different directions.
VE mimicked PE as Figure 1(b) illustrates in which the virtual scene shows the wooden board with six call buttons. VE was created by projecting images at 120 Hz to a projection screen, providing a 3D perspective view of the experimental scene. VE was calibrated to have the same metrics as for PE. The position of the robot arm’s end-effector was displayed as a hand in VE. Movements of the robot arm and hand were reproduced onto the 3D VE on a one-to-one scale.
In either environment, subjects were instructed to move at a comfortable speed while doing their best to reach and press the target buttons without using any compensatory trunk movements; the experimenter was monitoring every trial and if an excessive compensatory movement, i.e. leaning forward, was observed, that trial was repeated. If a subject could not reach the target, s/he asked for the robot’s assistance by saying the word “force” and the experimenter turned the guiding force on so that the robot would assist in completing the rest of the reaching movement. To allow subjects to try their best in performing the task before asking for the robot assistance, we did not limit their number of reaching attempts or time in any of the trials. During the robot assistance, the subject was still encouraged to continue his/her effort. In PE, one of the light-emitting diodes above the targets was pseudo-randomly turned on to indicate the reach target. In VE, the target button was visually highlighted. In PE, the movement end was indicated in the recording when the target button of interest was physically touched by the subject. In VE, as there was no physical target button present, the robot arm stopped the subject when the target of interest was reached in the virtual space and a “click” sound was played, like that of a physical button. When the subject completed a trial, either with or without help of the robot arm, the percentage of the movement distance that was completed without the robot’s assistance was displayed as feedback on a monitor placed above the experiment board in PE and displayed on the screen in VE. The robot arm then actively moved the subject’s arm back to the starting position. During each session, there were five reaching trials to each button, for a total of 30 trials in each environment, summing up to 60 trials per session. There was a short break (less than 5 min) when switching between the two environments. If a subject asked for a break between trials, it was given. Any occurrence of adverse events, such as increased pain, motion sickness, dizziness and headaches during engagement with the system, as well as development of new symptoms during the course of experiment, were recorded for reporting.
Outcome measures and analyses
To analyze the movement, the trajectory data were digitally low-pass filtered using a Butterworth filter with cut-off frequency of 6 Hz (dual pass). Then several kinematic metrics from the trajectory data were extracted as the primary outcome measures of interest. The analysis only focused on the portion of movement that was solely performed by the subject, without assistance from the robot. The kinematic metrics were: (1) movement completion ratio, defined as the ratio of the straight-line distance completed by the subject over the distance between the starting point and the target; this measure quantifies the amount of subject’s self-movement without robot’s assistance and is used to track subject’s UL motor performance. (2) Mean speed over the path line (i.e. trajectory); while both peak and mean speed measures are widely used, the mean speed is used for quantifying the movement speed of stroke subjects due to typical presence of multiple peaks in the speed profile of stroke subjects.15 (3) Shakiness, defined as the number of acceleration profile zero crossings over the path line. A lower shakiness value represents a smoother movement in terms of being less jerky. The movement start was defined as the first instance of subject’s speed in target direction exceeding 2% of the peak speed15 and the movement end was defined as the closest point to the target of interest reached by subject himself. However, the last 5% of the trajectory in terms of distance was excluded from the movement analysis due to the following reason. Subjects were only instructed to reach to the targets (the only set goal); thus, when they reached close to their movement limit, they sometimes struggled to go further. This made the last 5% of some reaching movements very different from the other parts of the trajectory. To have an accompanying clinical measure to the kinematics outcome measures, the Upper Extremity section of Fugl-Meyer Assessment (FMA-UE) was used as the secondary outcome measure16; the FMA-UE was measured at the first session prior to the start of the experiment and after the last session following the completion of the experiment for all the subjects.
As the PE and VE were done in the same session, carryover effect analysis was performed on the “movement completion ratio” measure to investigate whether having such an experimental design allows comparison between the two environments. In other words, we investigated whether training in the first environment (e.g. PE) affected the training in the next environment (e.g. VE) within one session (i.e. carryover effect). To this aim, the order of environments in each session was compared with the difference in performance between the two environments over four categories of less, more, equal, and plateau performance. Two “movement completion ratio” measurements were considered equal if were within 5% difference. As subjects reached plateau in some of the trials, we defined the plateau session as the session in which a subject’s self-movement graph reached its highest peak with no apparent decline in improvement (no more than 5% change in average decline of the following sessions).
Along with the kinematic metrics, a custom questionnaire was developed to assess how the stroke subjects perceived and experienced the reaching task in both environments using a modified version of the Intrinsic Motivation Inventory (modified-IMI)17 combined with a modified Short Feedback Questionnaire (modified-SFQ).18 The modified-IMI consisted of 10 questions divided into five items: Interest/Enjoyment, Perceived Competence, Effort/Importance, Pressure/Tension, and Value/Usefulness. The modified-SFQ consisted of two questions about Repeating the experiment and Comfort of the experiment. There were three additional questions about which environment they preferred, which one was easier for them, and whether they felt fatigued.
With a small sample size, no statistical comparison was performed. Instead each subject’s results are illustrated and reported in both environments.
Results
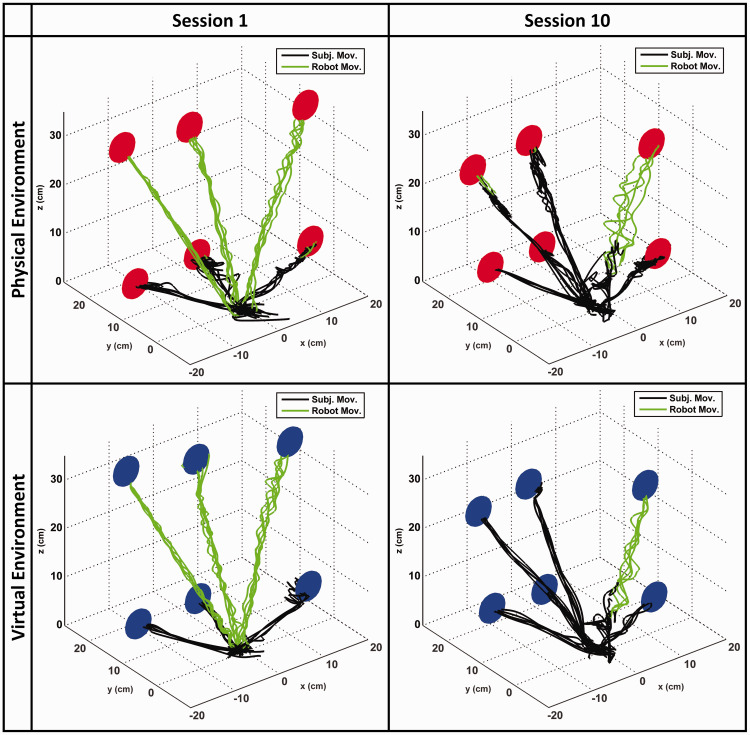
The results are presented for both environments to provide an illustration of their differences. During the course of the experiment, none of the subjects reported any adverse events such as increased pain or development of new symptoms. Training sessions varied between 30 and 40 min. Over the 10 sessions of training, the movement completion ratio of all the subjects increased; i.e. more self-movement and less robot assistance when compared to the first session. In average, the movement completion ratio increased 30%. Breaking down to targets, in average there were 44%, 47%, 28%, 9%, 20%, and 32% increase in movement completion ratio across targets 1–6, respectively. In all the subjects, multiple reaching attempts during a single trial before asking for the robot assistance were observed. Figure 2 shows the forearm trajectories of one of the subjects in both environments during the first and last session; the progression/improvement can be well seen in the figure in which the black lines represent the subject’s self-movement trajectories without any robotic assistance and the green (lighter) lines represent the portion of movement completed with the robot’s assistance. The shaky trajectories of the robot assistance show that the subject continued interaction with the robot during the robot assistance.
Figure 2.
Typical trajectories for sessions 1 and 10 in both environments. Black lines represent the trajectories performed by the subject (no robot assistance). After 10 sessions of practice, the improvements in reaching without robot assistance are quite evident. No noteworthy difference can be seen between the two environments in terms of reaching trajectories.
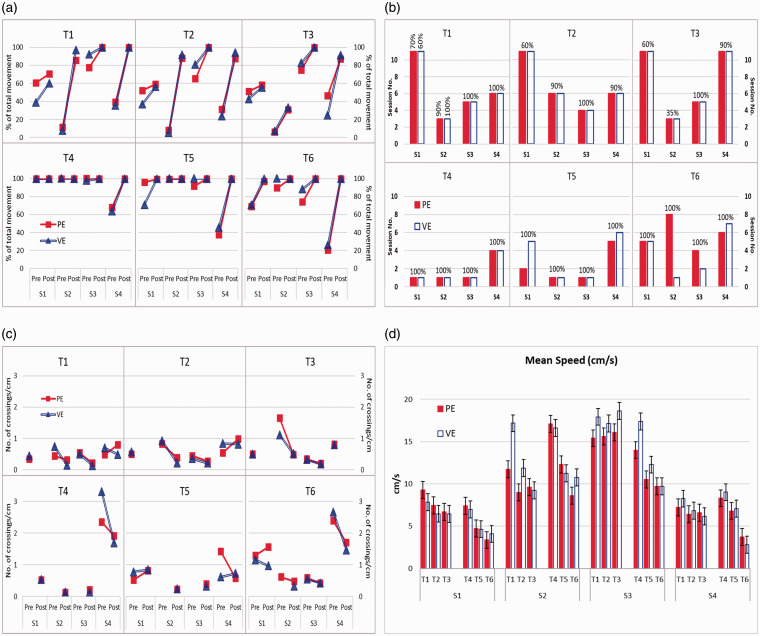
To illustrate each subject’s improvement in reaching performance following the 10 sessions of practice, we showed each subject’s self-movement in the first session versus the last session in reaching to the six targets of interest in both environments in Figure 3(a). Clear improvements in each subject’s reaching in both environments can be observed in this figure. This improvement in reaching was achieved in most cases in less than 10 sessions and reached a plateau; this plateau was dependent on the subject and the target (Figure 3(b)) but not the environment. There were negligible and inconclusive differences between PE and VE in terms of the plateau session number and the amount of final self-movement completion. Subjects 1 and 4 never reached a plateau in some targets (targets 1, 2, 3 for S1 and target 3 for S4), while completing respectively 60% and 90% of the whole movement in those targets. For Subject 2, while the plateau was reached in the third session in target 3, it was stopped at 35% of the whole movement for the rest of sessions and the subject could not improve his independent reaching movement toward that target. Target 4 (bottom left) was the easiest target for the subjects to attain 100% of movement completion ratio. It was followed by target 5 and then 6 (bottom middle and right, respectively). The upper targets were harder for the subjects to improve their reaching performance during the study sessions. Figure 3(c) illustrates reduction in the average shakiness measure after reaching the plateau in all the subjects except for Subject 1 (and Subject 4 at targets 1 and 2 in PE). We did not find any noticeable differences between the two environments (PE and VE) in terms of changes in shakiness measure.
Figure 3.
(a) Changes in subjects’ self-movement in reaching between session 1 (Pre) and session 10 (Post). (b) The session number that each subject reached their self-movement plateau during the 10 sessions of reaching practice; subject’s self-movement following plateau is indicated. Values more than 10 sessions indicate that the plateau was not reached. (c) Changes in the shakiness measure between the plateau session (marked as Pre) and the last session (marked as Post). At those that plateau was not reached only the shakiness measure of the last (10th) session is shown on Pre value. At those that plateau was reached right at the first session, the shakiness measure of the last (10th) session is shown on Post value. (d) Difference in Mean Speed between targets for each subject in both environments. The error bars show standard deviation. S1–S4 indicate subject IDs. T1–T6 indicate target numbers. PE and VE represent Physical and Virtual environments.
In terms of Mean Speed outcome measure, the visual inspection of all the subjects’ data did not reveal any trend across the ten sessions of practice. However, some differences/trends in the mean speed between the targets were noticed. Figure 3(d) shows the average and standard deviation of the mean speed over the 10 sessions of the study in reaching each target for each subject. No noticeable differences between the two environments can be seen in this figure. The common trend among all the subjects was in the lower targets (i.e. targets 4, 5, and 6) in which all the subjects, in either environment, demonstrated the highest speed when reaching for target 4, followed by targets 5 and then 6.
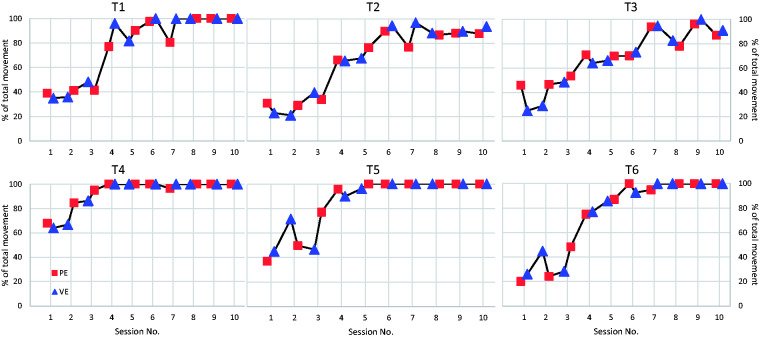
The results of carryover effect analysis are displayed in Table 2. The “PE-VE” represents that PE trials were performed first by the subjects followed by VE, while the “VE-PE” shows the reverse order. The differences between the “movement completion ratio” of PE and VE (VE was subtracted from PE) was categorized into four sections of “PE < VE” (less), “PE > VE” (more), “PE = VE” (equal within 5% difference), and “PLATEAU” (in both PE and VE, the “movement completion ratio” has reached 95–100%). The “No. of Trials” in the “PE-VE” order shows that if there was a carryover effect, we would have seen a higher number of trials in “PE<VE” category; however, this is not the case and all the three categories have similar number of trials. On the other hand, in the “VE-PE” order, presence of carryover effect should have caused higher number of trials in “PE>VE” category which is not the case. In addition, the mean difference and its standard deviation do not show much difference between the categories based on the environment order. Figure 4 shows one of the subject’s “movement completion ratio” (self-movement) over the 10 sessions with the order of the environments being displayed. Similar to the carryover effect analysis, no evident carryover effect can be observed.
Table 2.
Carryover effect analysis on all the trials of all the subjects.
| Environment order |
||||||
|---|---|---|---|---|---|---|
| Movement Completion Ratio Difference Category |
PE-VE |
VE-PE |
PE-VE |
VE-PE |
PE-VE |
VE-PE |
| No. of trials | Mean difference (%) | Standard deviation (%) | ||||
| PE < VE | 23 | 22 | –11.5 | –17.1 | 5.4 | 10.4 |
| PE > VE | 27 | 12 | 15.7 | 12.2 | 11.0 | 7.6 |
| PE = VE | 24 | 15 | 0.4 | –0.4 | 3.1 | 3.0 |
| PLATEAU | 64 | 53 | –0.3 | 0.1 | 1.2 | 1.2 |
PE: physical environment; VE: virtual environment.
Figure 4.
The order of environments across the 10 sessions of training is shown for one of the subjects. No evident carryover effect can be observed.
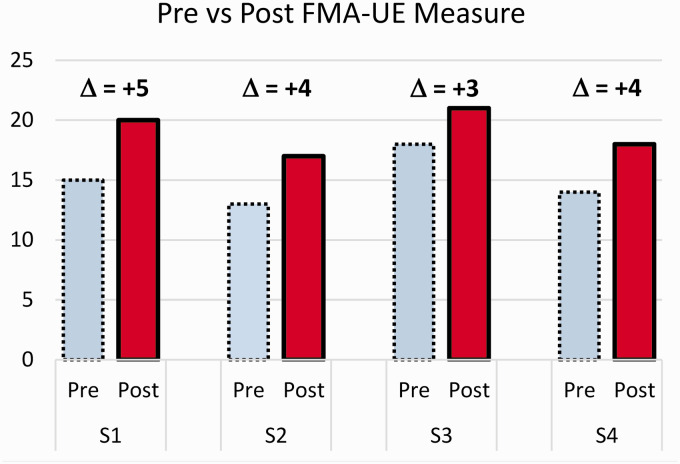
The changes in FMA-UE scores prior to the start and following the end of the study are shown in Figure 5. All subjects showed improvement in their FMA-UE score following the completion of the study. These improvements were between 3 and 5 points. At the sixth session, S3 reported (with a lot of emotion) that while she had not been able to push the elevator button in the last 20 years following her stroke, she has become able to do it; we checked this with her on the last session and she said she has become very comfortable in doing it. She mentioned that this has been the most effective therapy she has taken, and she wanted to know if there was a way she could continue the RT sessions. Another subject, S4, showed a lot of excitement when he became able to reach the targets during the sessions. S4 also reported that prior to this study, he had instances of burning his affected hand when opening the oven door, but now he has more control of using his affected hand when handling the oven door and have not had any burning incidence. These statements were self-reported by these two subjects.
Figure 5.
Changes in the FMA-UE scores of all the subjects before the start (Pre) and after the completion (Post) of the study. S1–S4 are subject IDs.
FMA-UE: Upper Extremity section of Fugl-Meyer Assessment.
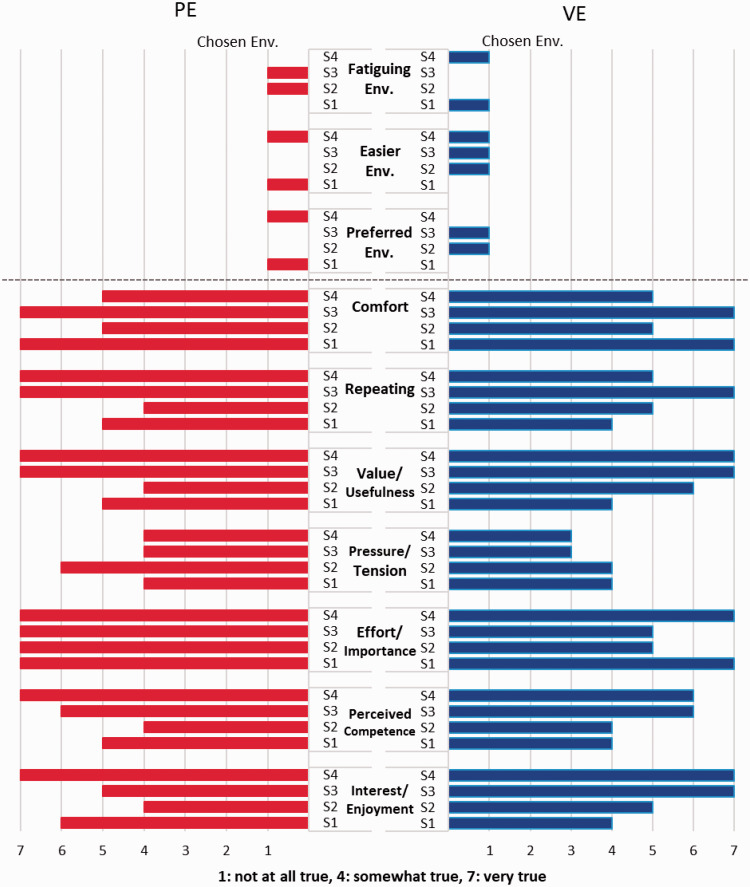
The responses to the custom questionnaire are summarized in Figure 6. We did not find any noticeable difference between the two environments in terms of subjective experience. All the subjects expressed positive feedback in terms of enjoyment and interest, were comfortable in either environment, were positive about repeating the task in either environment, were all satisfied with their perceived performance/competence in both environments, felt some pressure in doing the tasks in both environments, and reported feeling some fatigue. In other items, subjects were divided and sometimes preferred PE and sometimes VE.
Figure 6.
The responses to the custom questionnaire, consisting of modified-IMI, modified-SFQ, and questions about the choice of environment (Env.). The modified-IMI and modified-SFQ used a seven-point Likert scale, while the choice of environment was dichotomous questions. S1–S4 are subject IDs.
PE: physical environment; VE: virtual environment.
Receiving feedback on their movement was very important to the subjects. They were all asking how much of self-movement they achieved the session before for each target and were trying to improve their reaching performance based on that score.
Discussion
In this study, all the subjects increased their shoulder and elbow active range of motion and improved their arm reaching performance between the first and last session. We consider two possible factors in achieving such results. First, in developing this RT protocol specific to moderate-to-severe chronic stroke patients, due to the severity of their UL impairment, we only focused on arm reaching training as opposed to training a functional task involving both arm and hand based on the results obtained by the Krebs group.19 We focused on reducing the arm impairment in this subpopulation before proceeding to any functional task training. However, our protocol was not a pure impairment-oriented training, but a simple goal-directed training which was attainable by the subjects. Such a simple goal-oriented task may have let the subjects become focused on the task, i.e. reaching, and be very attentive and aware of their performance results (i.e. the feedback).
Second, we used the Assist-As-Asked paradigm in the RT protocol, rather than the well-known Assist-As-Needed (AAN) paradigm.20 In an AAN paradigm, the subject’s movement is continuously monitored by the robot and the amount of assistance required to achieve a given task is then provided by the robot.21 It has been suggested that this paradigm might not let subjects perform at their full potential, leading to submaximal or lower efforts by the subjects and therefore a strategy involving reducing the amount of assistance had been suggested and implemented.11 However, our Assist-As-Asked paradigm might help subjects reach their peak performance before asking for robot assistance; we observed that all the subjects had trials in which multiple reaching attempts (during a single trial) were done before asking for any assistance and they were quite responsive to the feedback about their movement. That being said, developing a modified version of the Assist-As-Asked paradigm that ensures subjects reach their peak performance and comparing its effectiveness with other RT paradigms should be pursued in future studies.
The improvements in reaching were achieved in most cases in fewer than 10 sessions of practice and reached their plateau which was subject and target dependent implying that the RT protocol should be individually tailored. In most cases where subjects reached a plateau, the shakiness decreased afterwards. The underlying neurological mechanism responsible for these improvements in the kinematic measures is still not known.22 However, the theory of sub-movements blending states that during post-stroke recovery, the criterion for refinement of movement patterns is not constrained to improving smoothness measures such as shakiness, but more toward gaining back the function; following the regain of the function, the shakiness decreases.15 In other words, shakiness exhibits a non-monotonic behavior during motor recovery. Therefore, the decision to stop the training of a movement should not only be based on the movement completion plateau but also on tunings of other movement parameters such as shakiness. Tracking these changes is possible in RT.23
While improvements in kinematic measures were evident and measurable, the FMA-UE only changed 3–5 units of score, which was below the minimal detectable change24 of 5.2 and minimal clinically important difference (MCID)25 of 7. A recent study, however, has shown that the MCID can be accepted at 4.26 As we only focused on training the arm, not the wrist and hand, we did not expect a major improvement in FMA-UE. Furthermore, the tests in FMA-UE do not differentiate between the two aspects of movement: strength and motor control.27 Therefore, it might not be a clear representative of the improvements by the subjects achieved with the RT. In addition, both FMA-UE score variation and the assessor’s bias giving more score in post-evaluation should be considered as a design limitation of this study. In future works, several clinical measures should be used as the main outcome measures of interest in evaluating the effectiveness of the Assist-As-Asked protocol with multiple baseline, post, and follow-up measures to investigate its long-term effect.
The results of this proof-of-concept study show that it is feasible to use the Assist-As-Asked protocol in both PE and VE. We did not find any noticeable and/or meaningful differences in terms of the kinematic variables between the two environments. A study on healthy subjects comparing reaching tasks in a PE vs VE in presence/absence of visual/haptic feedback showed that the subjects’ performance were similar in both environments when the subjects had visuo-haptic feedback in VE.28 In this study, besides the presence of visual feedback in PE and VE, both PE and VE shared the same haptic feedback in terms of forearm attachment to the robot arm and the robot arm provided haptic feedback at the end-point in VE. Subjective experience of the participants was also similar between the two environments. In other words, the choice of environment was more of a personal preference than having any effect on the outcomes.
The current study has several limitations in the study design. The main one is the small number of subjects and therefore the results presented here must be cautiously interpreted and only used for designing a larger experiment. Another issue was the experimental design in which both PE and VE were performed in the same session (AB design) and whether this would have resulted in carryover effects. Having used an alternating intervention design, such as ABAC design, in which the PE and VE were not used concurrently, would have been more suitable. A between-subject design to compare the effect of environment on RT might not be practical considering the high between-subject variability in stroke survivors.
Conclusion
This proof-of-concept study demonstrated that using the Assist-As-Asked protocol in moderate-to-severe chronic stroke survivors is feasible. It was also shown that the Assist-As-Asked protocol can be used with both PE and VE with no evidence of one to be superior to the other based on users’ perspectives and movement kinematics.
Supplemental Material
Supplemental material, sj-pdf-1-jrt-10.1177_2055668320926054 for Changes in arm kinematics of chronic stroke individuals following “Assist-As-Asked” robot-assisted training in virtual and physical environments: A proof-of-concept study by Nahid Norouzi-Gheidari, Philippe S Archambault and Joyce Fung in Journal of Rehabilitation and Assistive Technologies Engineering
Acknowledgements
We would like to thank Mr. Gordon Tao for his involvement in data collection and analysis.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded in part by the Fonds de recherche du Québec – nature et technologies (FRQNT), through the ingénierie des technologies interactives en réadaptation (INTER) strategic network, and by the Living Lab Mall Project of the Centre for Interdisciplinary Research in Rehabilitation (CRIR).
Guarantor
NN-G.
Contributorship
NN-G was involved in all part of this research work, including study design, patient recruitment, data processing/analysis/interpretation, statistical analysis, and the manuscript writing. Both PSA and JF were involved in study design, data interpretation, and providing critical review as well as providing funding. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iDs
Nahid Norouzi-Gheidari https://orcid.org/0000-0001-9623-7712
Philippe S Archambault https://orcid.org/0000-0002-8656-4477
References
- 1.Kwakkel G, Kollen BJ, Van der Grond J, et al. Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke 2003; 34: 2181–2186. [DOI] [PubMed] [Google Scholar]
- 2.Kwakkel G. Impact of intensity of practice after stroke: issues for consideration. Disabil Rehabil 2006; 28: 823–830. [DOI] [PubMed] [Google Scholar]
- 3.Langhorne P, Wagenaar R, Partridge C. Physiotherapy after stroke: more is better? Physiother Res Int 1996; 1: 75–88. [DOI] [PubMed] [Google Scholar]
- 4.Woytowicz EJ, Rietschel JC, Goodman RN, et al. Determining levels of upper extremity movement impairment by applying a cluster analysis to the Fugl-Meyer Assessment of the upper extremity in chronic stroke. Arch Phys Med Rehabil 2017; 98: 456–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saposnik G, Levin MF. Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke 2011; 42: 1380–1386. [DOI] [PubMed] [Google Scholar]
- 6.Huang X, Naghdy F, Naghdy G, et al. Robot-assisted post-stroke motion rehabilitation in upper extremities: a survey. Int J Disabil Hum Dev 2017; 16: 233–247. [Google Scholar]
- 7.Oña ED, Cano-de la Cuerda R, Sánchez-Herrera P, et al. A review of robotics in neurorehabilitation: towards an automated process for upper limb. J Healthc Eng 2018. DOI: 10.1155/2018/9758939. [DOI] [PMC free article] [PubMed]
- 8.Veerbeek JM, Langbroek-Amersfoort AC, Van Wegen EEH, et al. Effects of robot-assisted therapy for the upper limb after stroke: a systematic review and meta-analysis. Neurorehabil Neural Repair 2017; 31: 107–121. [DOI] [PubMed] [Google Scholar]
- 9.Sivan M, Gallagher J, Makower S, et al. Home-based Computer Assisted Arm Rehabilitation (hCAAR) robotic device for upper limb exercise after stroke: results of a feasibility study in home setting. J Neuroeng Rehabil 2014; 11: 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norouzi-Gheidari N, Archambault PS, Fung J. Effects of robot-assisted therapy on stroke rehabilitation in upper limbs: systematic review and meta-analysis of the literature. J Rehabil Res Dev 2012; 49: 479–496. [DOI] [PubMed] [Google Scholar]
- 11.Reinkensmeyer DJ, Wolbrecht ET, Chan V, et al. Comparison of three-dimensional, assist-as-needed robotic arm/hand movement training provided with Pneu-WREX to conventional tabletop therapy after chronic stroke. Am J Phys Med Rehabil 2012; 91: S232–S241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bejarano NC, Maggioni S, Rijcke LD, et al. Robot-assisted rehabilitation therapy: recovery mechanisms and their implications for machine design In: Pons JL, Raya R, González J. (eds) Emerging therapies in neurorehabilitation II. Cham, Switzerland: Springer International Publishing, 2016, pp.197–223. [Google Scholar]
- 13.Fischer HC, Stubblefield K, Kline T, et al. Hand rehabilitation following stroke: a pilot study of assisted finger extension training in a virtual environment. Top Stroke Rehabil 2007; 14: 1–12. [DOI] [PubMed] [Google Scholar]
- 14.Van der Linde RQ, Lammertse P, Frederiksen E, et al. The HapticMaster, a new high-performance haptic interface. In: Proc Eurohaptics, Edinburgh University Press, Edinburgh, UK, 2002, pp.1–5.
- 15.Rohrer B, Fasoli S, Krebs HI, et al. Movement smoothness changes during stroke recovery. J Neurosci 2002; 22: 8297–8304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fugl-Meyer AR, Jääskö L, Leyman I, et al. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med 1975; 7: 13–31. [PubMed] [Google Scholar]
- 17.McAuley E, Duncan T, Tammen VV. Psychometric properties of the intrinsic motivation inventory in a competitive sport setting: a confirmatory factor analysis. Res Q Exerc Sport 1989; 60: 48–58. [DOI] [PubMed] [Google Scholar]
- 18.Kizony R, Raz L, Katz N, et al. Video-capture virtual reality system for patients with paraplegic spinal cord injury. J Rehabil Res Dev 2005; 42: 595–608. [DOI] [PubMed] [Google Scholar]
- 19.Krebs HI, Mernoff S, Fasoli SE, et al. A comparison of functional and impairment-based robotic training in severe to moderate chronic stroke: a pilot study. NeuroRehabilitation 2008; 23: 81–87. [PMC free article] [PubMed] [Google Scholar]
- 20.Basteris A, Nijenhuis SM, Stienen AH, et al. Training modalities in robot-mediated upper limb rehabilitation in stroke: a framework for classification based on a systematic review. J Neuroeng Rehabil 2014; 11: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Srivastava S, Kao P-C, Kim SH, et al. Assist-as-needed robot-aided gait training improves walking function in individuals following stroke. IEEE Trans Neural Syst Rehabil Eng 2015; 23: 956–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buma FE, Van Kordelaar J, Raemaekers M, et al. Brain activation is related to smoothness of upper limb movements after stroke. Exp Brain Res 2016; 234: 2077–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bosecker C, Dipietro L, Volpe B, et al. Kinematic robot-based evaluation scales and clinical counterparts to measure upper limb motor performance in patients with chronic stroke. Neurorehabil Neural Repair 2010; 24: 62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin J, Hsu M, Sheu C, et al. Psychometric comparisons of 4 measures for assessing upper-extremity function in people with stroke. Phys Ther 2009; 89: 840–850. [DOI] [PubMed] [Google Scholar]
- 25.Sivan M, O’Connor RJ, Makower S, et al. Systematic review of outcome measures used in the evaluation of robot-assisted upper limb exercise in stroke. J Rehabil Med 2011; 43: 181–189. [DOI] [PubMed] [Google Scholar]
- 26.Lundquist CB, Maribo T. The Fugl–Meyer assessment of the upper extremity: reliability, responsiveness and validity of the Danish version. Disabil Rehabil 2016; 39: 934–939. [DOI] [PubMed] [Google Scholar]
- 27.Kitago T, Goldsmith J, Harran M, et al. Robotic therapy for chronic stroke: general recovery of impairment or improved task-specific skill? J Neurophysiol 2015; 114: 1885–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ebrahimi E, Babu SV, Pagano CC, et al. An empirical evaluation of visuo-haptic feedback on physical reaching behaviors during 3D interaction in real and immersive virtual environments. ACM TAP 2016; 13: 19. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jrt-10.1177_2055668320926054 for Changes in arm kinematics of chronic stroke individuals following “Assist-As-Asked” robot-assisted training in virtual and physical environments: A proof-of-concept study by Nahid Norouzi-Gheidari, Philippe S Archambault and Joyce Fung in Journal of Rehabilitation and Assistive Technologies Engineering