Abstract
To assess the current epidemic trend of COVID-19/SARS-CoV-2 in India, the epidemic dynamics of COVID-19 cases in India in terms of Case Fatality Rate (CFR), Case Recovery Rate (CRR) and Mortality rate (MR) COVID-19 have been evaluated during Lockdown-1. The analysis includes (i) epidemic curve of Covid-19 cases (ii) demographic analysis (iii) calculation of the CFR and CRR by different methods (iv) calculation of MR (v) Geo-temporal analysis (vi) epidemiological transmission factor (vii) evaluation of the effects and impact of infection, prevention and control in India. A total of 10,815 COVID-19 confirmed cases have been reported in 31 states/union territories as of April 14, 2020 with 9272 active cases (85.73%), 1190 cured/discharged (11%), and 353 deaths (3.23%). Among confirmed cases, most cases (59%) are aged 20–49 which is working age in India and 76% cases are reported for men. The median age of Indian COVID-19 patients found to be 39. As of April 14, the CFR per total cases in India is 3.32% and per closed cases is 23.27%. The CRR per total cases in India is 11.00% and per closed cases is 76.72%, which indicates that the recovery rate of COVID-19 is more than the fatality rate in India. The prevention and control measures taken by the state and central governments at all levels and measure of maintenance of social distancing by people have resulted in effective curbing in the COVID-19 transmission in India.
Keywords: COVID-19, Corona virus, Epidemics, Fatality Rate
Introduction
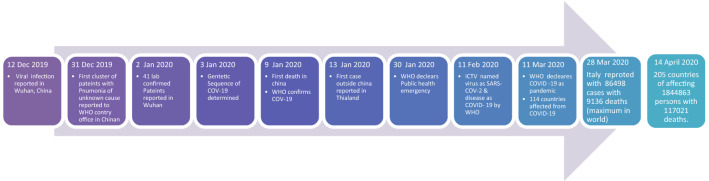
A novel Corona virus is a category of pathogens, which mostly attacks on the respiratory system of human beings. Corona virus outbreaks are emerging earlier also in the form of Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) [1–4]. Now, in the present times, it emerges as a COVID-19, which is caused by the SARS2 Coronavirus and poses a significant risk to the human race. In December 2019, a number of patients with pneumonia symptoms were reported in Wuhan and Hubei Province of China and later identified as symptoms caused due to the spread of corona virus [5]. Epidemiologically, these patients were later on found to be linked to an animal and seafood market of Wuhan [6]. Later on, the Wuhan city of China was recognized as the epicentre of the COVID-19 disease and claimed for spreading the disease across the world. Around 41 lab confirmed COVID-19 patients reported and admitted to hospital up to January 2, 2020 in China. These patients have symptoms of coughing, sneezing, breathing problems, chest pain, indigestion, and respiratory illness. It was also observed that most of these patients are already suffering from varied diseases such as hypertension, diabetes and cardiovascular [7]. According to China National Health Commission, 17 deaths reported in China with COVID-19 up to January 22, 2020 and within four days death rate raised to triple with 5502 confirmed cases [8]. By the end of January 2020, 7734 confirmed cases have been reported in China along with 90 cases in other countries such as Thailand, Japan, Malaysia, Iran, Italy, India, USA, Canada, Taiwan, Vietnam, France, Nepal, Cambodia, Germany, Singapore, Korea, United Arab Emirates, Sri Lanka, The Philippines, Australia and Finland [9]. Furthermore, WHO on 30 Jan declares Public health emergency of international concern due to the severity of the disease [10]. The International Committee on Taxonomy of Viruses named this corona virus as a Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) and the disease caused by the virus designated as Coronavirus Disease-19 (COVID-19) by WHO [11, 12]. The COVID-19 has strewed in more than 114 countries with 118,326 active cases and 4292 deaths on March 11, 2020 and declared as pandemic by WHO [13]. The situation becomes worse within a week after the pandemic declaration and Italy become the second most affected country after china. Presently, about 205 countries are affected by COVID-19 across the globe and shattered the economic growth of developed as well as developing countries. The WHO report documented on 14 April 2020 claimed 5,53,822 cases United States of America, 1,69,496 cases in Spain, 1,59,516 in Italy, 1,25,098 in Germany, 97,050 cases in France, much higher cases in comparison to China from where the disease actually originated (83,696) [14]. The chronology of all these events happened during an outbreak of COVID-19 around the globe depicted in Fig. 1. The certain vulnerable populations such as elderly people, child below 5 or people with multiple chronic disorders are at higher risk of COVID-19. The China was successful in stabilizing the conditions, but it is worst in American, European and South Asian countries in the present situation.
Fig. 1.
Chronology of significant developments occur worldwide during outbreak of COVID-19
India is the most vulnerable country in South Asian region to COVID-19 as India has the second highest population in the world after China. However, COVID-19 expands in India at a very slow pace in comparison to other countries. The India’s March month expansion rate of COVID-19 is much lower than most countries. Even though the transmission rate of COVID-19 increasing day by day within India, but still it remains on the low side due to Lockdown of the country. The Lockdown-1 period started from March 24, 2020 up to April 14, 2020 (the last day of Country Lockdown-1). The objective of this study is to present the current geographical and graphic situation of COVID-2019/SARS-CoV-2 in India during the Lockdown-1 period. This study evaluates Case fatality rate of India and compare with its global scenario along with a discussion on various epidemiological factors responsible for transmission, prevention and control measures taken to control the spread of COVID-19 in India.
Method
Study Design
This research was a descriptive and a preliminary investigation of COVID-19 cases diagnosed on a national scale in India as of the end of April 9, 2020. The Ministry of Health and Family Welfare (MoHFW), India is closely monitoring the outbreak of COVID-19. The Integrated Disease Surveillance Programme (IDSP), National Center of Disease Control has been launched by MoHFW for in country surveillance and outside travellers before the outset of the disease on 25 January, 2020. Each case of COVID-19 was updated and informed to state surveillance control room through hospital, lab and field surveillance teams. A unique state patient number has been provided to each reported case and hence, there is no chance of duplication in data and confirmation of all COVID-19 cases. The data from each state surveillance control room was updated directly to MoHFW. Therefore, the data for analysis of COVID-19 cases nationwide were extracted from the official website of MoHFW [15]. The global data for COVID-19 was extracted from WHO situation reports. The population data was extracted from United Nation Population Report [16].
Analysis
The demographic and epidemiological characteristics of confirmed cases of COVID-19 patients were compiled through descriptive statistics. This descriptive analysis includes the age distribution and sex ratio (male: female ratio) graphs, calculation of Case Fatality Rate (CFR), Case Recovered Rate (CRR) and Mortality Rate (MR) for confirmed cases of COVID-19 diagnosed in India till 14 April, 2020.CFR/ CRR during an epidemic may be represented either as CFR/ CRR per total cases (total confirmed cases) or CFR/ CRR per closed cases (total of recovered and died cases) [17–19]. CFR/ CRR per total cases and per closed cases were calculated by following equations:
| 1 |
| 2 |
| 3 |
| 4 |
Here, we have also calculated the Mortality rate in India for COVID-19 according to The Dictionary of Epidemiology which defined the mortality rate as an estimation of the portion of a population that dies during a specified period per 1,00,000 people [20].
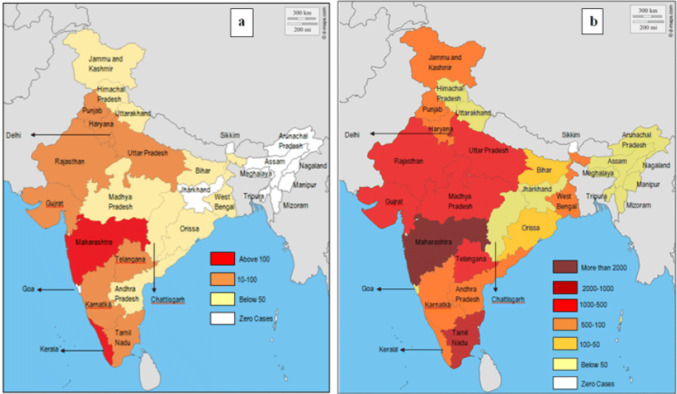
The Geo-temporal analysis for different affected states of the country was also done with colour-coded maps of India which indicate the numbers of cases in different states as of March 24, 2020 (the first day of Country Lockdown-1) and April 14, 2020 (the last day of Country Lockdown-1).
Results and Discussion
According to the MoHFW, a total of 10,815 COVID-19 confirmed cases have been reported in 31 states/union territories as of April 14, 08:00 GMT + 5:30. Among them, 9272 active cases, 1189 cured/discharged, 1 migrated (cured) and 353 deaths were reported.
The first case of COVID-19 reported in India is from Kerala state on 30 January, 2020 and within three day cases increases to 3 up to February 3, 2020. These cases were related to students who had returned from Wuhan, China. After that, no case was reported in the month of February [21]. The transmission reports of COVID-19 have been reported from various states of India during March. The most of cases are imported as infected people with a travel history to affected countries. The first death in the country from Covid-19 was reported of a 76-year-old man in Bangalore who had come back from Saudi Arabia on March 12 [22]. Till March 15, the confirmed cases of COVID-19 reach up to only 100 and up to end of March, approximately 1400 cases were reported and within the span of one week, cases enhances up to 5000. The cases become almost double up to 10,000 till April 14. The timeline of total confirmed patients, recovered and deaths from COVID-19 in India till April 14 (End date of Lockdown 1) has been shown in Fig. 2. Yet the number of COVID-19 cases enhanced day-by-day infection rate of India is still 1.7 in comparison to other affected countries of the world [22]. But, still a high risk of infection is there in India due to high population density, i.e. 464 people/ km2 [23].
Fig. 2.
Timeline of COVID-19 Cases in India from 3 March, 2020 to14 April, 2020
Demographic Studies
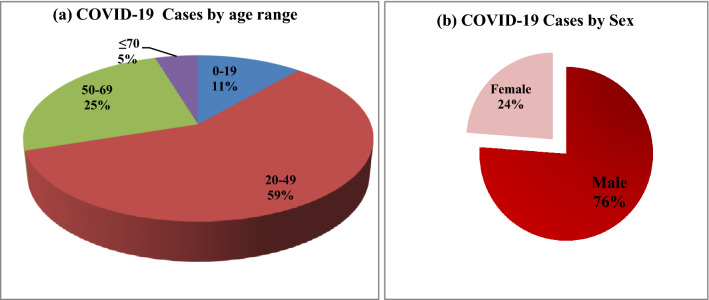
The demographic characteristics of the Infected Indian population vary from other countries. An analysis of the demographic details of 2500 COVID-19 Indian patients shown in Fig. 3a which reveals that 59% are those between the ages of 20 and 49 which are followed by 50–69 age range comprises 25%. It imparts that most of the Indian population infected from COVID-19 is of working age group. The reports of other infected countries like Italy and China, have shown that older people are the most vulnerable to COVID-19 infection [24]. But the older people above the age of 70 are only 5% in India. The 11% young Indian children under the age of 20 are also susceptible to COVID-19 and become severely affected and reported to die also.
Fig. 3.
Age distribution and sex ratio of COVID-19 Cases in India up to 14 April, 2020
The median age of Indian COVID-19 patients found to be 39 which is quite less in comparison to China and Italy, where the median age reported to be 49.5 and 64 [25, 26]. It clearly depicts the demographic differences between India and the other countries. This might be due to the difference between the median age of an Indian which is expected to be 28.4 years and for China and Italy, it is expected to be 38.4 and 41.9 respectively in year 2020 (UN population report) [16].
In India, 76% cases are reported for men of total confirmed case (Fig. 3b). In a contrast with other countries, women are found to be less positive for COVID-19 in India, while for early breakdown reports in China and Italy, the ratio is roughly equal for men and women [25] with an exception of South Korea where 60% women are found to be COVID-19 positive [26]. This difference in India is might be due to the sociological factor of ample discrepancy between male and female. It is possible that this gap may become narrow in coming days when number of testing get increased and more COVID-19 patients get detected. Another possible reason is that women in India, travel less internationally for business purpose as international travelling is the main source of the initial infection in India.
CFR, CRR and MR Studies
In India, a total of 353 deaths has reported among 10,815 confirmed cases with overall fatality rate of 3.2%. India’s fatality rate is quite low in comparison to other affected countries such as France, Spain, China, Italy, USA and overall globally as on Situation Report-85 of WHO of dated April 14, 2020 (Fig. 4) [27]. The total COVID-19 confirmed cases are highest in the USA, followed by Spain and Italy, but France’s CFR was 15.40% on the high side, followed by Italy (12.83%.), United Kingdom (12.78%) and Belgium (12.76%). However, as depicted in Table 1, the population size of China and India is much greater than these countries. Hence, the population size not much contributed in increasing CFR of COVID-19.
Fig. 4.
Comparison of CFR among different nations having cumulative case of COVID-19 above 10,000 till 14 April, 2020. The marked nations with different colored circle showed the severity of spread of COVID-19 in relation to both the number of positive cases and deaths
Table 1.
Comparison on COVID-19 cases among different nations based on Population
| Country | Total population | Total confirmed case | Total death | CFR (%) |
|---|---|---|---|---|
| World | 77,13,468 | 18,44,863 | 1,17,021 | 6.34 |
| China | 14,33,784 | 83,696 | 3351 | 4.00 |
| India | 13,66,418 | 10,363 | 339 | 3.27 |
| USA | 3,29,065 | 5,53,822 | 21,972 | 3.97 |
| Brazil | 2,11,050 | 22,169 | 1223 | 5.52 |
| Japan | 1,26,850 | 7645 | 109 | 1.43 |
| Germany | 83,517 | 1,25,098 | 2969 | 2.37 |
| Turkey | 83,430 | 61,049 | 1296 | 2.12 |
| Iran | 82,914 | 73,303 | 4585 | 6.25 |
| The United Kingdom | 67,530 | 88,625 | 11,329 | 12.78 |
| France | 65,130 | 97,050 | 14,946 | 15.40 |
| Italy | 60,550 | 1,59,516 | 20,465 | 12.83 |
| Spain | 46,737 | 1,69,496 | 17,489 | 10.32 |
| Canada | 37,411 | 24,786 | 734 | 2.96 |
| Republic of Korea | 25,666 | 10,564 | 222 | 2.10 |
| Australia | 25,203 | 6366 | 61 | 0.96 |
| Netherlands | 17,097 | 26,551 | 2823 | 10.63 |
| Belgium | 11,539 | 30,589 | 3903 | 12.76 |
| Switzerland | 8591 | 25,499 | 885 | 3.47 |
| Israel | 8519 | 11,235 | 110 | 0.98 |
| Ireland | 4882 | 10,647 | 365 | 3.43 |
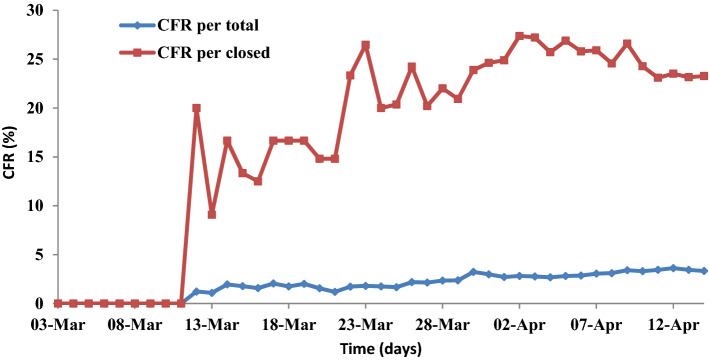
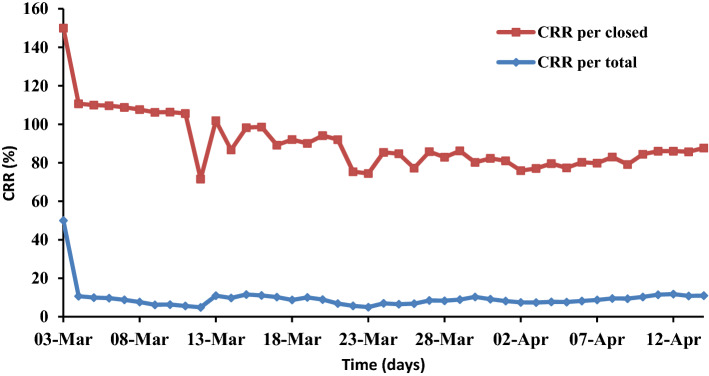
India’s comparison data of CFR/CRR per total and per closed for a period of March 3–April 14 summarized in Figs. 5 and 6 respectively. The initial stage of outbreak in India starts in the second week of March. As the number of confirmed cases of COVID-19 enhanced, the difference between CFR per total and per closed also get increased randomly up to April10. This difference clearly indicates that the outbreak of COVID-19 is still at an infectious stage and has just started to downturn stage. The similar observation was recorded for initial and middle stage of outbreak in China by Spychalski et al. [19]. The peak value of CFR per closed was found to be obtained at 27.38% on April 2 and the value decreases to 23.27% as of April 14, the last day of Lockdown. With these numbers, the Government forced to announce for the Lockdown-2 up to May 3 to control pandemic COVID-19 in India. Therefore, we might expect that CFR per closed reaches to per total when all active cases are closed.
Fig. 5.
CFR comparison of COVID-19 cases in India for a period of March 3–April 14, 2020
Fig. 6.
CRR comparison of COVID-19 cases in India for a period of March 3–April 14, 2020
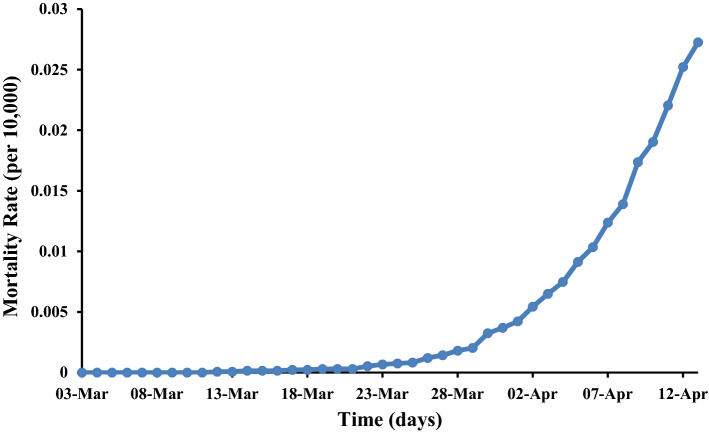
As of April 14, the CFR per total cases in India is 3.32% and per closed cases is 23.27%. In comparison to the CFR, CRR per total cases in India is 11.00% and per closed cases is 76.72%. This observation clearly indicates that the recovery rate of COVID-19 is more than the fatality rate in India. But still, 9272 are active in India and yet to be recovered. The mortality rate per 10,000 people also observed to be increased exponentially as shown in Fig. 7.
Fig. 7.
Mortality rate of COVID-19 in India
Geo-Temporal Studies
The Indian Government issued an advisory for complete lockdown across the country start from March 24 as a preventive measure to combat COVID-19 till April 14 for 21 days. The social distancing during the lockdown seems to be only a way for a decisive battle against COVID-19 for a country like India with such a huge population. The COVID-19 cases crossed the mark of 560 across the country includes 41 foreign nationals on March 24 as reported by MoHFW. From total confirmed cases, only 36 people have been reported to cure along with 11 deaths. As shown in Fig. 8a, Maharashtra was the worst hit, with the total of 107 COVID-19 positive cases with the highest number of confirmed cases nationwide, so far and Kerala is also close behind with 105 cases. The cases from other states such as Karnataka (41), Telangana (39), Uttar Pradesh (35), Gujarat (35), Rajasthan (32), Haryana (30), Delhi (29), Punjab (29), Tamil Nadu (18) also upswing at fast pace.
Fig. 8.
Geo-temporal analysis through India on a 24th March 2020 (the first day of Lockdown-1), b 14th April 2020 (the last day of Lockdown − 1)
The COVID-19 spread apparent in the month of March and by April 14, 2020, 31 states/union territories reported to be affected with a cumulative number of 10,815 cases, 9272 active cases, 1190 cured and 353 deaths. Maharashtra reported 2337 COVID-19 cases, the highest number of infections, followed by Delhi (1510) and Tamil Nadu (1173). The spread of COVID19 in other states has been as shown in Fig. 8b. Only 25 districts, across 15 states in India reported to be free from COVID-19 infection.
According to ICMR study, COVID-19 tally could have reached to 8.2 lakh with 41% cumulative growth rate by April 15 without a lockdown and containment actions taken by government [28].
So the decision of the strict lockdown nationwide seems to be successful in slow down the pace of transmission of the disease. However, the lifting the lockdown with this infection rate could easily activate fresh cases. So, the government has taken the decision to extend the lockdown period up to May 3.
Epidemiological Transmission Factors
There are various Epidemiological and operational factors of the health service which converts this disease from epidemic in China to Pandemic in mostly whole of the world. The Epidemiological triangle depicts the interrelation of host (who carries the disease), agent (virus) and environment of specific place at a given time [29]. Since December 2019, intensity of the spread of COVID-19 from Wuhan (China) to other parts of the world varies at different paces. As COVID-19 are highly infectious, so Indian government immediately followed WHO guidelines on January 25 to check and control the infection at international airports by screening tests before the report of the first case in India. The first case of COVID 19 was reported in India on January 29 when a Kerala student returned from Wuhan, China- epicentre of this disease and later on two more students also detected with same infection, but immediate action of state health department by creating isolation ward and subsequently quarantine for 28 days helped these patients recover fully. Hence, no case of COVID-19 has been reported in India in the month of February. Religious rituals could be one of the factors where people have close contact and greetings in dense population. Though most of the religious places in India get closed after lockdown, but still some worship places remain open and gathering of people at those places become a major concern of its spread. One third, COVID 19 positive cases out of total confirmed cases, are directly associated with Markaj-Musilm religious congregation in which 8000 people gathered, including foreigners from Indonesia, Malaysia etc. responsible for enhancing the cases and spread in twenty seven states of India when Markaj people travelled to other states without informing the concerned authorities [30].
In India, Socio culture practices play both roles, one side it benefits in controlling the disease in joint family structure where homemade eating habits, less use of napkins in toilets, greeting by Namaste on the other side, big gathering at religious places and distribution of Prasadam creating the situation to become more worse. In slum areas, sharing of drugs and cigarettes in the younger generation, sharing same room with many people at unauthorized places in India is also a considerable factor in transmission of the disease. The population density of India (464/km2) is also a major contributing factor to spread the infection as observed earlier in SARS and MERS [31]. People with a systematic disease history as blood pressure, heart problem, diabetes, asthma, etc. will be more chances of aggravation of this virus. In general, outside the cell, the virus does not have a tendency to replicate but on touching the contaminated surface transfer the virus to host [32]. Therefore, diseased surface is becoming significant vectors for spreading the infection at health centres and public places.
President of health care foundation of India, KK Aggarwal predicted that the weather can decrease the growth of corona virus [33]. Further emphasizing epidemiological factor, Arindam Biswas, explained that out of epidemiological triangle- agent (Virus), host and environment, Indian weather condition in severe summer will not be favourable for the virus to replicate [34]. Though still uncertainty is there, but this statement is gaining weight.
In India, health care services are not quality matching as that of other Asian and western countries and this is also a crucial factor to provide efficient services to individual patient during isolation. There is also a concern over the limited numbers of doctors in India, Niti Aayog made a call to retire and military doctors to work as volunteers for handling the situation if COVID-19 enters stage 3 as the pressure on available doctors and medical staff is escalating in the public health system. Moreover, the government is also worried about the quantity of personal protective equipment (PPE) for medical staff as some of the health workers and doctors are becoming the victim to this disease due to shortage of PPE.
Preventive and Control Measures
WHO published its Interim guidance on March 19 for infection, prevention and control (IPC) COVID 19 of suspected patients [35]. Under the IPC guidelines, health care services should have clinical triage to ensure the suspected patients and isolate them. Also to launch triage station to train health workers, screening questionnaire. To ensure the application of the standard precautions on all patients, it should comprise hand hygiene and respiratory hygiene, disinfection of patient care equipment, usage of personal protective equipment, environment cleaning and safe disposable of biomedical waste.
Family members and visitors must follow strictly contact and droplet precautions before visiting to COVID 19 suspected patient. The patient should preferably be kept in a single isolated room of 60 L/s. In the absence of adequate single room, suspected patient could be placed together at different beds. Health care workers should follow specific norms while handling the patients. They should wear goggles for eye protection, medical gloves, and long sleeved gown. Equipment used should be either single used or properly disinfected with 70% Ethyl alcohol. Instead of moving the patient for diagnostic, potable analysis kits should be used for patient examination. To restrict the transmission of virus, family members, visitors and even HCW’s visits are to be limited and recorded. As COVID 19 is highly infectious air transmitted diseases as compared to earlier MERS & SERS so all the airborne precautions for aerosol-generating procedures are to be followed strictly while collecting the samples, handling and transporting to clinical laboratories.
However, the approach for IPC of such pandemic varies nation to nation. IPC of any country depends upon the factors such as its socioeconomic condition, capacity building, competency or alertness against pandemic, geographical location, demographic structure, healthcare networks, etc. India despite being the second largest populous nation with a population in the billions, has reported only a few hundred cases of COVID-19, arises an uncertainty about spread of virus. The preventive measure taken by the Indian Government timely at the public level seems to be appropriate to suppress the COVID-19 infection. The MoHFW declare a well-developed National Programme for the prevention and control of COVID-19. The Government quick actions of suspending visas and quarantining of all travelling from affected countries sustained the virus for community spread. More than one million international as well as national travellers screened at airports which limits the virus entry in the country. However, the Universal health screening is not only adequate for the virus to spread. The asymptomatic infectious people could skip through the screening, but able to spread the infection. The tough decision of nationwide lockdown by Indian Government facilitates effective social distancing as well as identification, and tracing of infected people.
Conclusions
The present research study concludes the current analysis of COVID-19 transmission in India. The disease is still supposed to at the second stage of the infection and not spread at community level. But actually, the data on the transmissibility of the virus is still not reported completely due to low testing rate in India. It has been seen that as the number of testing get increased during the lockdown period, the more and more cases come into the light and reporting of daily infection emerges. The virus is beginning to spread through dense communities in the Dharavi sector of Mumbai (the financial capital of India). However, the immense and strong steps taken by the Indian government have slowed down the pace of the COVID-19 epidemic in India, but still the epidemic not to be appearing in its decline phase, and people of India may have to face many challenges in the coming days.
References
- 1.Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. Journal of Clinical Medicine. 2020 doi: 10.3390/jcm9020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhama K, Sharun K, Tiwari R, et al. Coronavirus disease 2019 – COVID-19. Preprints. 2020 doi: 10.20944/preprints202003.0001.v1. [DOI] [Google Scholar]
- 3.Ramadan N, Shaib H. Middle East respiratory syndrome coronavirus (MERS-CoV): A review. Germs. 2019;9:35–42. doi: 10.18683/germs.2019.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodriguez-Morales A, Tiwari R, Sah R, Dhama K. COVID-19, an emerging coronavirus infection: Current scenario and recent developments-An overview. Journal of Pure and Applied Microbiology. 2020;14:6150. doi: 10.22207/JPAM.14.1.02. [DOI] [Google Scholar]
- 5.Pung R, Chiew CJ, Young BE, et al. Investigation of three clusters of COVID-19 in Singapore: Implications for surveillance and response measures. The Lancet. 2020;395:1039–1046. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malik YS, Sircar S, Bhat S, et al. Emerging coronavirus disease (COVID-19), a pandemic public health emergency with animal linkages: Current status update. Preprints. 2020 doi: 10.20944/preprints202003.0343.v1. [DOI] [Google Scholar]
- 7.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. Journal of Medical Virology. 2020;92:441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19) International Journal of Surgery. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. International Journal of Antimicrobioal Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO Director-General’s Remarks at the Media Briefing on 2019-nCoVon 11 February 2020. (2020). World Health Organization. Retrieved March 31, 2020 from https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11february-2020
- 13.Coronavirus disease 2019 (COVID-19): Situation Report- 51. (2020). World Health Organization. Retrieved April 2, 2020 from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- 14.Coronavirus disease 2019 (COVID-19): Situation Report- 57. (2020). World Health Organization. Retrieved April 2, 2020 from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200317-sitrep-57-covid-19.pdf?sfvrsn=a26922f2_4
- 15.Coronavirus disease (2019) (COVID-19: Daily Reports. Ministry of Family and Health Welfare, Govt. of India. Retrieved April 14, 2020 from https://www.mohfw.gov.in/
- 16.Population Division World Prospects 2019. (2019). United Nations Department of Economics and Social Affairs, Population Division. Retrieved April 16, 2020 from https://population.un.org/wpp/Download/Standard/Population/
- 17.Ghani AC, Donnelly CA, Cox DR, et al. Methods for estimating the case fatality ratio for a novel, emerging infectious disease. American Journal of Epidemiology. 2005;162:479–486. doi: 10.1093/aje/kwi230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim DD, Goel A. Estimating case fatality rates of COVID-19. The Lancet Infectious Disease. 2020 doi: 10.1016/S1473-3099(20)30246-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spychalski P, Błażyńska-Spychalska A, Kobiela J. Estimating case fatality rates of COVID-19. The Lancet Infectious Disease. 2020 doi: 10.1016/S1473-3099(20)30246-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Porta, M. (Ed.). (2014). A dictionary of epidemiology. Oxford: Oxford University Press
- 21.https://www.indiatoday.in/india/story/coronavirus-in-india-tracking-country-s-first-50-covid-19-cases-what-numbers-tell-1654468-2020-03-12
- 22.https://indianexpress.com/article/coronavirus/coronavirus-india-infection-rate-china-6321154/
- 23.Indian Population. (2020). Retrieved April 17, 2020 from https://www.worldometers.info/world-population/india-population/
- 24.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 25.Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 26.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. The Lancet Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30086-4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coronavirus disease 2019 (COVID-19): Situation Report- 85. (2020). World Health Organization. Retrieved April 16, 2020 from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200414-sitrep-85-covid-19.pdf?sfvrsn=7b8629bb_4
- 28.https://timesofindia.indiatimes.com/india/without-lockdown-virus-could-have-affected-8-2-lakh-by-april-15-analysis/articleshow/75102680.cms
- 29.Salama NK, Rabe B. Developing models for investigating the environmental transmission of disease-causing agents within open-cage salmon aquaculture. Aquaculture Environment Interactions. 2013;4(2):91–115. doi: 10.3354/aei00077. [DOI] [Google Scholar]
- 30.https://timesofindia.indiatimes.com/india/coronavirus-about-9000-tablighi-jamaat-members-primarycontacts-quarantined-in-country-mha-says/articleshow/74948832.cms
- 31.Dharamsaktu NS. The lessons learned from current ongoing pandemic public health crisis of COVID 19 and its management in India from various different angles, perspectives and way forward. Epidemiology International. 2020;5(1):1–4. doi: 10.24321/2455.7048.202010. [DOI] [Google Scholar]
- 32.Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.https://economictimes.indiatimes.com/industry/healthcare/biotech/healthcare/india-did-have-an-innate-natural-shield-against-coronavirus-afterall/articleshow/74453719.cms?from=mdr
- 34.https://www.vice.com/en_in/article/wxe4an/could-india-really-be-more-immune-to-coronavirus-
- 35.World Health Organization. (2020). Infection prevention and control during health care for probable or confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: interim guidance. Retrieved April 18, 2020 from https://www.who.int/csr/disease/coronavirus_infections/ipc-mers-cov/en/