Abstract
Hospital-based care of pediatric trauma patients includes transitions between units that are critical for quality of care and patient safety. Using a macroergonomics approach, we identify work system barriers and facilitators in care transitions. We interviewed eighteen healthcare professionals involved in transitions from emergency department (ED) to operating room (OR), OR to pediatric intensive care unit (PICU) and ED to PICU. We applied the Systems Engineering Initiative for Patient Safety (SEIPS) process modeling method and identified nine dimensions of barriers and facilitators – anticipation, ED decision making, interacting with family, physical environment, role ambiguity, staffing/resources, team cognition, technology and characteristic of trauma care. For example, handoffs involving all healthcare professionals in the OR to PICU transition created a shared understanding of the patient, but sometimes included distractions. Understanding barriers and facilitators can guide future improvements, e.g., designing a team display to support team cognition of healthcare professionals in the care transitions.
Keywords: Macroergonomics, Pediatric trauma care transitions, SEIPS
1. Introduction
In the US, trauma is the leading cause of death in children and young adults (Centers for Disease Control and Prevention, 2015; Stewart et al., 2003), with an estimated economic impact of $70 billion annually (Centers for Disease Control and Prevention, 2010). Prior research on pediatric trauma focuses on the technical, medical aspects of inpatient trauma care (Farach et al., 2015), the role of designated pediatric trauma centers (Beaudin et al., 2012; Chatoorgoon et al., 2010; Cowley & Durge, 2014; Potoka et al., 2001; Potoka et al., 2000; Stroud et al., 2013) and coordination between emergency medical services and hospitals (Bergrath et al., 2013; Moulton et al., 2010; Van Veen & Moll, 2009). Recent research focuses on the work of caring for pediatric trauma patients after they arrive in the emergency department (ED), including understanding the hospital units and health care professionals involved throughout the hospitalization (Durojaiye et al., 2018; Wooldridge et al., 2018). This work highlights that pediatric trauma care involves many care transitions, changing both the physical location of patient care and the clinicians caring for that patient (Wooldridge et al., 2018).
Care transitions involve transfers of information, authority and responsibility for a patient’s care between one or more clinicians (Abraham et al., 2014), and influence patient safety and quality of care. Care transitions provide opportunities to detect and correct errors (Perry, 2004), but risk information loss, delays in care and information flow, and decreased care effectiveness and efficiency (Arora et al., 2009; Hoonakker et al., 2018). Despite much research developing tools to facilitate communication in care transitions (Abraham et al., 2017; Horwitz et al., 2009; Riesenberg et al., 2010; Riesenberg et al., 2009; Zavalkoff et al., 2011), between 2009–2013 there were 7149 instances of patient harm, including 1744 deaths, attributed to communication failures in the U.S. (CRICO Strategies, 2015). This led to a Joint Commission’s sentinel event alert to improve handoff communication (The Joint Commission, 2017).
Transitions between units are transitions from one system to another (Beach et al., 2012), with handoff communication between clinicians and transitions of equipment, support staff, technology and environment (Carayon & Wood, 2009), all required to transfer authority and responsibility for patient care. Some researchers have begun to approach care transitions as processes – i.e., “set[s] of interrelated or interacting activities” (ISO, 2015) – including work outside of transport and communication. Redesigning entire care transition processes, rather than focusing on handoffs, will likely result in more impactful improvement. For example, Catchpole et al. (2007), Craig et al. (2012) and Agarwal et al. (2012) redesigned OR to ICU care transition processes, including preparation in the OR and ICU while the patient was in the OR, patient stabilization upon arrival to the ICU, and an interactive, multidisciplinary handoff. These redesigned processes resulted in significant improvements in information flow (Agarwal et al., 2012; Catchpole et al., 2007; Craig et al., 2012), attentiveness (Catchpole et al., 2007; Craig et al., 2012), errors (Catchpole et al., 2007) and clinical outcomes (Agarwal et al., 2012). In the current study, we will use a human factors and ergonomics (HFE)-based process modeling methodology to analyze current care transition processes in detail, which was not reported in the literature as part of the above process redesign work. We will identify solutions based on work system barriers and facilitators to guide future efforts to improve care transitions.
2. Process Analysis to Guide Improvement Efforts
Process analysis has a rich history in HFE as the foundation for process improvement (Jun et al., 2010; Siemieniuch & Sinclair, 2015). We must clearly understand the current work situation – i.e., the work system (Carayon, 2009; Carayon et al., 2006; Smith & Carayon-Sainfort, 1989) – before we redesign it in an improvement effort (Daniellou, 2005). Further, it is important to understand the work as it is done, not just as prescribed by management (Hollnagel et al., 2015; Leplat, 1989). Process mapping approaches are one way to achieve that understanding and are useful in identifying risks from various sources (Simsekler et al., 2018b). We previously proposed and described the Systems Engineering Initiative for Patient Safety (SEIPS)-based process modeling method (Wooldridge et al., 2017). We developed this process analysis method to clearly understand the care process and the sociotechnical (work) system in which the process is embedded. The SEIPS model (Carayon et al., 2006; Carayon et al., 2014) is the foundation of our method (figure 1). The work system model includes five elements: people, tasks, technologies and tools, organization, physical environment (Carayon, 2009; Smith & Carayon-Sainfort, 1989). The work system elements and their interactions must be addressed together, as they dictate how the process unfolds over time (Carayon, 2009; Carayon et al., 2014) and are key to re-designing processes for improved patient and healthcare professional outcomes (Berg, 1999).
Figure 1.
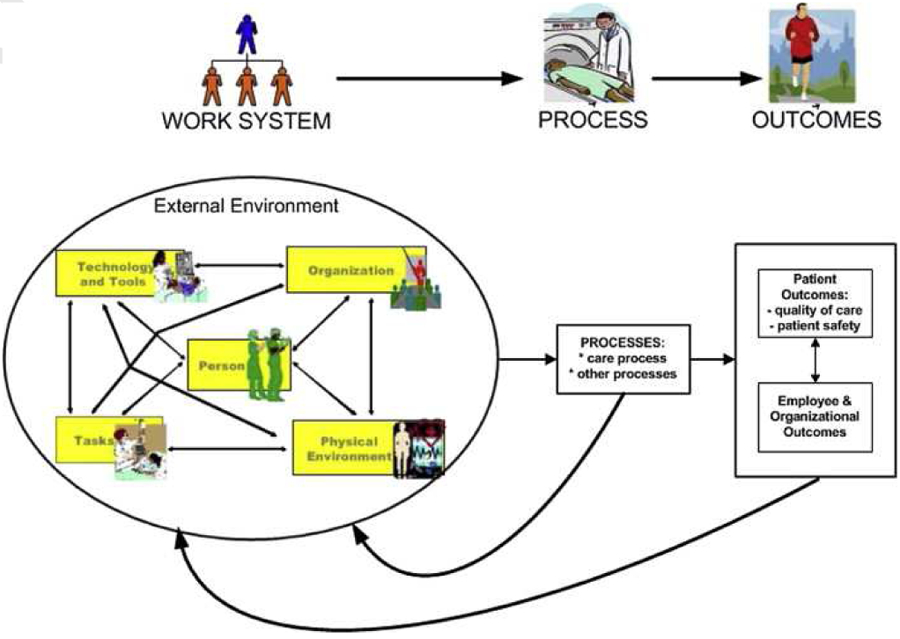
The SEIPS model of work system and patient safety (Carayon et al., 2014)
SEIPS-based process maps are similar to swim-lane diagrams and flowcharts; in the original paper, columns represented roles involved in the process and rows indicated temporality (Wooldridge et al., 2017). The processes previously analyzed involved three to four roles in primary care clinics and spanned a short time period. Pediatric trauma care transitions involve up to 33 individual roles directly participating in patient care in each unit and cross organizational units of a hospital (Wooldridge et al., 2018). We adapted and refined the SEIPS-based process modeling method for application to more complex processes distributed across time (rows) and space (i.e., physical environment; columns). Major steps in the process are shown in boxes in the cells created by rows and columns. Details about which role(s) perform(s) tasks with tools/technologies are in those boxes, which allowed us to eliminate the tables that previously accompanied the process maps. The resulting process maps incorporate all work system elements.
2.1. Work System Barriers and Facilitators
Process analysis can be used to identify opportunities for improvement (Jun et al., 2011; Jun et al., 2010; Jun et al., 2009; Simsekler et al., 2018a, 2018b; Wetterneck et al., 2006; Wooldridge et al., 2017). An important research application of the SEIPS model is the identification of work system obstacles and facilitators (Carayon et al., 2005; Carayon et al., 2014), which are factors that inhibit or facilitate the performance and completion of goal-directed activities (Brown & Mitchell, 1991; Carayon et al., 2005; Hoonakker et al., 2017; Peters & O’Connor, 1980; Peters et al., 1985). Hoonakker and colleagues (2017) described dimensions that could be both barriers and facilitators, rather than defining categories of barriers separately from categories of facilitators. A systems-based approach to evaluating processes can result in a deeper and broader understanding of what hinders and supports system performance, e.g., patient safety and quality in health care. That understanding can inform effective improvement efforts, by identifying what to eliminate or mitigate (i.e., barriers) and what to build upon (i.e., facilitators; Carayon, 2009; Smith & Carayon-Sainfort, 1989).
In research on care transitions, interviews and focus groups are used to understand challenges that negatively influence outcomes. For instance, ambiguous roles and conflicting expectations have been linked with patient harm (McElroy, Collins, et al., 2015; McElroy, Macapagal, et al., 2015; Reine et al., 2019). Using 62 interviews and 3 focus groups, Lane-Fall and colleagues (2018) identified other barriers to safe care transitions, e.g., time pressure and lack of understanding of the information needs of others. They also identified supporting factors (i.e., facilitators), e.g., pre-notification of patient arrival to ICU team, presence of extra nurses upon patient arrival and predictable handoff format. However, these factors – which are, essentially, work system barriers and facilitators – were not identified as part of a systematic analysis of the process.
2.2. Study Objective
The objective of this study is to identify work system barriers and facilitators in transitions of pediatric trauma patients between hospital units. The findings will inform the development of sociotechnical solutions to improve care transitions. We defined work system barriers as characteristics of a work system element(s) that interfere with a person’s ability to efficiently, appropriately and accurately transition a patient (Carayon et al., 2005). We defined work system facilitators as characteristics of a work system element(s) that make it easy or easier to efficiently, appropriately and accurately transition a patient (Carayon et al., 2005).
3. Methods
This study is part of a larger study on health information technology (IT) for teamwork and care transitions in pediatric trauma care (https://cqpi.wisc.edu/research/health-care-and-patient-safety-seips/teamwork-and-care-transitions-in-pediatric-trauma/). This qualitative study uses semi-structured interviews with health care professionals involved in pediatric trauma care transitions. Approval for this study was obtained from the IRB at the University of Wisconsin-Madison.
3.1. Pediatric Trauma Care Transition Processes
Previously, Wooldridge et al. (2018) found that the most critical pediatric trauma patients, i.e., those triaged as level 1, experienced about 4 transitions on average, ranging from 1 to 24. In the current study, we focus on three care transitions commonly experienced by pediatric trauma patients during their hospitalization: transitions from ED to OR, OR to PICU and ED to PICU. The three transitions occur early in the hospitalization under high time pressure (i.e., the patients are more likely to be unstable, requiring life-saving measures quickly) and uncertainty (i.e., much information about the patient and the accident may not yet be known). The inclusion of three care different transitions in the study enhances the external validity of our findings and generalizability of our results across at least three transitions rather than one.
3.2. Setting and Sample
The participating pediatric hospital is a level 1 trauma center with 111 beds, 8 pediatric operating rooms and a 21-bed PICU. An electronic health record (EHR) (Epic Systems) was implemented in this hospital in 2008. We used purposeful sampling of health care professionals based on their role in the care transitions. We recruited potential participants via email; participation was voluntary. We interviewed a total of 18 clinicians in 17 interviews (two OR nurses participated in one interview together), asking each interviewee about two of the three transitions that they are involved in; see table 1. Because we asked about two care transitions in each interview, we have a total of 34 cases.
Table 1.
Sample (17 interviews, 34 cases)
| Profession | ED to OR (N=13 cases) | OR to PICU (N=12 cases) | ED to PICU (N=9 cases) |
|---|---|---|---|
| Physician (attendings, fellows and residents) | ED: 1 Anesthesia: 2 Surgery: 2 |
Anesthesia: 2 Surgery: 2 PICU: 2 |
ED: 1 PICU: 2 |
| Mid-level practitioner | Anesthesia: 1 | Anesthesia: 1 | - |
| Nurse | ED: 2 OR: 4* |
OR: 4* PICU: 2 |
ED: 2 PICU: 2 |
| Ancillary support staff | ED: 2 | - | ED: 2 |
Note:
two OR nurses participated in one interview together, and are counted as one case.
3.3. Data Collection Methods
We conducted in-person semi-structured interviews, which allowed follow-up questions to probe for more detailed answers (Robson & McCartan, 2016), with one or two health care professionals. Each interview was conducted by two HFE engineers, one leading the interview and the other ensuring all questions were addressed, keeping time and managing other logistics. The interview guide (http://cqpi.wisc.edu/teamwork-and-care-transitions-in-pediatric-trauma/) was focused on gaining a detailed understanding of the care transitions. Each interviewee was asked about the two care transitions they participate in (table 1). For each care transition, we asked interviewees to describe the work system and process, including preparation before and follow up after transport, guided by the SEIPS model (Carayon et al., 2006; Carayon et al., 2014). We asked probing questions about each work system element. We then solicited examples of good and bad transitions – i.e., when the patient’s care was not (or might have been) compromised and the transition went (or did not go) well – and what made those go well or poorly, respectively. We asked this set of questions about each care transition for both level 1 and level 2 patients. We concluded the interview by asking the interviewees to compare the two transitions and to identify possible solutions to improve the care transitions.
We conducted 14 hours and 44 minutes of interviews (average duration: 52 minutes). Interviews were recorded and transcribed by a professional transcription service. After the first five interviews were conducted, we iterated between data collection and analysis, monitoring theoretical saturation, i.e., when we saw only repeated or similar instances of interest (Glaser & Strauss, 1967), by tracking the number of new barriers or facilitators from each interview (figure 2).
Figure 2.
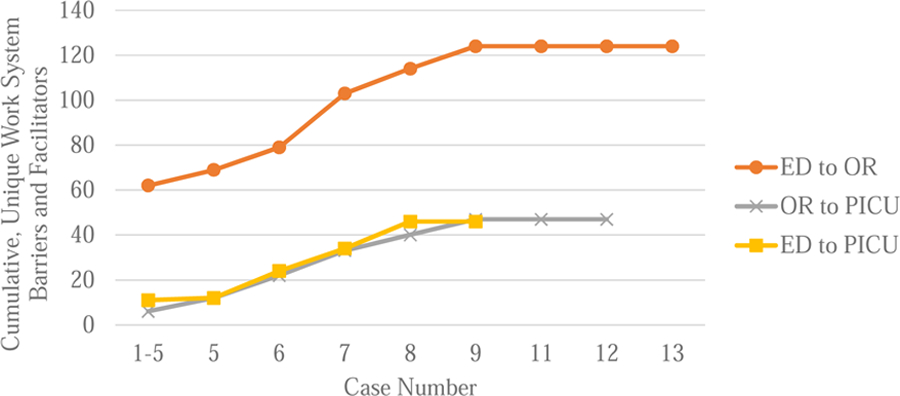
Data Saturation Tracking of Unique Work System Barriers and Facilitators
3.4. Data Analysis Methods
All transcripts were cleaned to remove any identifying information and were uploaded to Dedoose© web-based qualitative data analysis software. We developed SEIPS-based process maps to understand the roles and work involved in the care transition processes. The methodology for the process analysis and the full process maps can be found in Appendix A.
Excerpts of the interview transcript where the interviewee described a barrier or facilitator were identified and coded. The excerpts were also coded to identify the specific transition the interviewee was discussing (i.e., ED to OR, OR to PICU, or ED to PICU). Two researchers independently coded one transcript and met to review and resolve discrepancies. They then independently coded a second transcript, and met to review discrepancies; at this point, there were minimal differences, and each researcher coded half of the remaining interview transcripts.
The barrier/facilitator excerpts were exported to Excel® by transition (i.e. ED to OR, OR to PICU, ED to PICU). Excerpts from two transcripts were each reviewed by four researchers to identify all barriers and facilitators. Some excerpts only mentioned one barrier or facilitator, while some mentioned as many as four. The researchers summarized each barrier and facilitator in each excerpt. The researchers then met to discuss and resolve any differences. The rest of the excerpts were then coded by two HFE researchers independently. The two researchers met to discuss differences, and any differences that could not be resolved were reviewed by all four researchers.
The analysis resulted in identifying 418 barriers and facilitators. We then conducted a thematic analysis of individual barriers and facilitators (Glesne, 2016), grouping similar barriers and facilitators to identify dimensions that could provide guidance about process redesign or technology solutions. One researcher performed the majority of the thematic analysis, with other researchers reviewing the dimensions and discussing questions that arose. The other researchers asked questions and provided suggestions, which were discussed, and final decisions were made by the entire group.
Researchers identified the work system elements most closely involved for each dimension, i.e., the proximal causes of barriers and facilitators (Wooldridge et al., 2017), in a consensus-based process. For example, a barrier related to poor reception of pagers in the hospital is most proximally related to the technology work system element, as it is a technical issue; however, the organization selected the paging system, so the organization work system element is distally involved. In our analysis, this barrier would be associated with the technology work system element but not the organization element. These dimensions were reviewed by clinicians on the research team, who were not involved in the data analysis, some of the participants and other stakeholders (e.g., nursing leadership, trauma program manager) as a form of member checking (Devers, 1999).
Since the goal of our analysis was to identify categories of barriers and facilitators, we report the percentage of interviewees that mentioned barriers and facilitators related to each dimension for each care transition they were asked about (i.e., out of 34 cases). No matter if an interviewee mentioned the dimension as a barrier once or many times in one transition, it was only counted as one occurrence of that dimension as a barrier. We also compared the distribution of barriers and facilitators by dimension across the three care transitions; we report the percentage of interviewees who mentioned the dimension as a barrier or facilitator for each transition.
In order to compare barriers and facilitators in the care transitions, we counted the number of interviewees who mentioned each dimension as a barrier and the number of interviewees who mentioned each dimension as a facilitator for each care transition.
4. Results
4.1. Process Mapping
The ED to OR, OR to PICU and ED to PICU transitions involve similar work:
Preparing the patient for the transition: communication and coordination between the sending and receiving units, gathering necessary personnel, equipment and supplies for transport, and preparation in the receiving unit such as gathering equipment, supplies, personnel and information.
Physical transition: moving the patient and parent(s), family and/or caregiver(s) who may be present between units, although they usually do not move together, and a handoff.
Follow-up after the handoff: the receiving unit assuming and continuing care of the patient and documentation.
The ED to OR care transition involves 25 roles who complete 11 major activities using four technologies – phone, paper notes, fax and EHR. The OR to PICU care transition involves 18 roles who complete 12 major activities using four technologies – phone, pager, paper notes and EHR. The ED to PICU care transition involves 22 roles who complete 13 major activities using three technologies – phone, pager and EHR. The phone and EHR are used in all care transitions.
These transitions also have differences. The OR to PICU transition includes a team handoff in which surgery, anesthesia and PICU physicians and nurses participate; the ED to OR care transition may include phone and/or face-to-face handoffs, separated by profession. The ED to PICU care transition handoff is organized similarly to the ED to OR handoff, but the PICU physicians often participate in patient care in the ED trauma bay; therefore, they often have more shared awareness and thus less information to handoff. Sometimes, the PICU physicians assume care of the patient in the ED and manage the transition themselves.
4.2. Work System Barrier and Facilitator Analysis
We identified nine dimensions of barriers/facilitators: anticipation, ED decision making, interacting with family, physical environment, role ambiguity, staffing/resources, team cognition, technology and characteristic of trauma care. See table 2 for the definitions of the dimensions, the work system elements most proximally involved (indicated by X’s) and examples. Table 3 shows the percentage of cases mentioning each dimension as a barrier and a facilitator, by care transition and total.
Table 2.
Dimensions of Barriers and Facilitators
| Dimension | Definition | Work System Elements | Examples | |||||
|---|---|---|---|---|---|---|---|---|
| Person | Task | T/T1 | O2 | PE3 | EE4 | |||
| Anticipation | How clinicians’ and staff members’ ability to foresee and address in advance the needs related to care of the pediatric trauma patient is impacted (increased or decreased). | X | X | • ED nurse giving situation, background, assessment and recommendation (SBAR) report to PICU nurse lets them anticipate what care will be needed for that patient when they get to PICU from OR. • Time to prepare before patient arrives to ED makes transitions, care smoother. • By policy, PICU nurses cannot look at patient record until patient is in unit which hinders preparation to receive the patient. • Knowing the patient’s condition before surgery and how the patient responded to surgery helps the PICU team care for the patient and ensure nothing is missed (either by going to ED and/or OR or reviewing patient information in advance). |
||||
| ED decision making | Factors that influence how decisions about patient care after the ED are made and how that decision impacts further patient care (beyond simply where the patient goes after the ED) | X | X | X | • Clear, strong leader is needed to provide direction and facilitate agreement about disposition, which improves care and family experience. • Quick decision and agreement between doctors about disposition, i.e. what’s next for the patient, is needed for care to be provided in a timely manner. • PICU clinicians present in ED makes it easier to communicate and have everyone on the same page; if they are not there, there is more communication work when information is given serially. |
|||
| Interacting with family | Factors that impact how clinicians and staff interact with family/caregivers and vice versa. | X | X | • Having a role dedicated to interacting with patient, family face-to-face can ease family concerns during care and facilitate communication. • Parents may be left in OR waiting room or forgotten, and not talked to anyone even though patient is in PICU for two hours. • Someone moving family to PICU waiting room lets PICU nurses settle, begin caring for patient uninterrupted. |
||||
| Physical environment | How the physical environment impacts the care and transitions of pediatric trauma patients | X | • Too many people in the ED can make it difficult to do procedures, provide care. • The team uses the public (e) elevator to move the patient, which can create delays during transport. • Activity during the handoff can create distractions and hinder communication; hard stops during handoff would help avoid those distractions. |
|||||
| Role ambiguity | Factors that cause and/or the impact of clinicians and staff being (un)clear about roles and expectations | X | • Pediatric team going to adult OR can be difficult, even if better for patient care (do not know who to get information from, nurses less comfortable, surgical team does not know charge nurse, etc.). • Surgical attire can make it hard to identify the role of individuals in the OR, and make it difficult to identify who should be given information. • Having defined roles in the care transition makes it smoother because no one is fighting for roles and wondering how to manage fluid/ambiguous roles to provide the best care. |
|||||
| Staffing/resources | How available staff and other resources impact the ability of clinicians and staff to care for the pediatric trauma patient | X | • Having enough nurses in trauma bay lets one nurse prepare to move patient (document, coordinate, gather supplies) without delay or compromising patient care. • A new anesthesiologist who replaced the anesthesiologist mostly involved in the surgery can lead to loss of information because they were not there for more than the last 15–30 minutes or so. • Delays in being able to handoff to the receiving clinician can result in the trauma chief being unable to handoff at all, e.g., if they have to put an emergent chest tube in another patient. • An oversupply of nursing staff when the patient arrives can help with the transition to get things done (e.g. changing the patient, moving them and starting the IV). |
|||||
| Team cognition | Factors that cause and the impact of team cognition (i.e., planning, decision making, problem solving and problem assessment at the team level), which occurs in communication interactions between care team members. | X | X | • Team familiarity (or lack thereof) can make communication and collaboration more difficult; fewer interactions between ED and OR units does not help to build rapport. • Communication between team can ensure everyone knows what to do to care for patient and any special requests to respect (e.g., no female providers). • The transition from surgical team to medical team can require different language, information, more time because they may be less familiar with complex surgical care and are a completely new care team. • Interprofessional handoff at bedside allows all involved clinicians receive the same information, preventing errors and giving better overall picture, if they go to the handoff (e.g., may not know they will be caring for patient or may not want to go). • Incomplete handoff (due to communication mode and/or difference in expectation between sender and receiver), or missing handoff to key groups, results in more time calling to get information and/or delayed feedback; conversely, clear communication with written plans to refer to help the PICU team care for the patient. |
||||
| Technology | Work system barriers and facilitators caused by characteristics, usability and/or usefulness of the technology they use | X | • EHR is not useful because of high time pressure and it may not match verbal information. • Communication tools used by nurses are important for coordination/anticipation/preparation, and some tools (e.g., smart phones) are more useful than others (e.g., pagers, Vocera) because of functionality (reception issues) and features (stored numbers, group text). • Bed assignment system may not be updated, so assigned room number may not work in system (e.g., if room is/is not clean). |
|||||
| Characteristic of trauma care | Inherent properties of caring for trauma patients that impact how clinicians and staff can provide care. | X | • Trauma care transitions (especially for very unstable patients) are high time pressure, which impacts communication and planning; having a concise plan helps. • When people are rushed, the transition can go poorly (inaccurately estimating patient trajectory, delaying calling PICU, etc.). • Having an accurate assessment of the patient and their trajectory is key for a good transition. |
|||||
Notes:
X in a work system element column indicates that element is proximally (i.e., closely) involved in creating a barrier/facilitator of that dimension.
T/T = tools and technology
O = organization
PE = physical environment
EE = external environment
Table 3.
Dimensions of barriers and facilitators in care transitions processes.
| Dimension | ED to OR (N=13) | OR to PICU (N=12) | ED to PICU (N=9*) | Total (N=34) | ||||
|---|---|---|---|---|---|---|---|---|
| Barriers | Facilitators | Barriers | Facilitators | Barriers | Facilitators | Barriers | Facilitators | |
| Anticipation | 62% | 54% | 50% | 75% | 11% | 44% | 44% | 59% |
| ED decision making | 46% | 23% | 0% | 0% | 67% | 78% | 35% | 29% |
| Interacting with family | 46% | 15% | 17% | 0% | 22% | 44% | 29% | 18% |
| Physical environment | 54% | 38% | 25% | 42% | 0% | 0% | 29% | 29% |
| Role ambiguity | 46% | 54% | 25% | 25% | 11% | 11% | 29% | 32% |
| Staffing/resources | 46% | 38% | 42% | 50% | 56% | 44% | 47% | 44% |
| Team cognition | 92% | 85% | 42% | 100% | 89% | 67% | 74% | 85% |
| Technology | 46% | 31% | 33% | 58% | 22% | 44% | 35% | 44% |
| Characteristic of trauma care | 31% | 31% | 0% | 0% | 11% | 11% | 15% | 15% |
Notes:
The percentages shown are the percentage of cases (the number of interviewees asked about that care transition, N in column heading) describing each dimension as a barrier or a facilitator, respectively, by care transition and overall.
One interviewee was not asked about the ED to PICU care transition, but volunteered a barrier for it in her description of another transition based on her previous experience in a role that participated in the ED to PICU transition
Shading in the heat map was defined by increasing the saturation of the red or green shading by 10% for each 10% increase in percentage of cases (e.g., shading for 0% is 0% saturation, shading for greater than 0% and less than 10% is 10% saturation, shading for greater than 10% and less than 20% is 20% saturation, etc.)
4.2.1. Anticipation.
Anticipation refers to the ability of clinicians to foresee and address in advance needs related to the transition of the patient. The anticipation dimension was related to the task and organization work system elements. Anticipation itself is a goal-directed activity and leads to other goal-directed activities, hence the connection with task; organizational rules, procedures and cultures influenced how anticipation occurred in the care transition. Anticipation was mentioned as a barrier (i.e., when clinicians were less or not able to anticipate needs) in 44% of cases. For example, when asked about the use of any technologies other than a phone to gather information about a patient who will be admitted to the PICU from the ED, a PICU nurse responded:
“Well, I can’t [use the EHR] until they arrive. So, and that’s a pretty significant roadblock… if I sought them out before they had a location, then I think I, I’ve never done this, I don’t know, but I’m guessing they would reprimand me.” (PICU nurse).
The hospital has a policy in place to prevent privacy violations, discouraging clinicians from accessing records of patients that they might care for in the near future, which hinders their ability to prepare for the patient’s arrival to the unit.
Anticipation was also mentioned as a facilitator (i.e., when clinicians were able to anticipate needs for smoother transitions) by 59% of cases. For example, when a surgery resident was asked about good care transitions from the ED to the OR, s/he mentioned the importance of the PICU being aware of the patient and expect them after surgery:
“[I]t goes well if a bed is available if everyone is in the loop and is aware of the patient, if there’s a heads up prior to from the ER that a patient might be in the PICU, and that once we finalize a decision, it’s just a simple call.” (Surgery resident).
Anticipating that the patient will need PICU-level care after surgery and sharing information with the PICU so they can prepare and ensure there is a bed, before the patient even leaves the ED, helps the second transition from OR to PICU.
4.2.2. ED decision making.
ED decision making refers to factors that influence decisions about patient care beyond the ED and how that decision-making process influences future patient care; this goes beyond deciding where the patient should go after the ED, i.e., the ED disposition (Cabrera et al., 2015; Calder et al., 2012). ED decision making was related to three work system elements: the person (individual skills related to the leadership involved in ED decision making), the task (determining where the patient should receive care after the ED) and the organization (procedures and policies that influence ED decision making). ED decision making was mentioned as a barrier (e.g., when the decision was not made in a timely manner, what slowed or hindered decision making and how that impacted patient care) by 35% of cases. For example, an ED nurse described how disagreement between physicians on where the patient should go from the ED can hinder care transitions, in particular to the OR: “[A] sticking point, is if the doctors are going, well, are we going to go to the OR, or are we going to go the PICU, or are we going to go somewhere else?…they’re arguing amongst themselves,” (ED nurse).
ED decision making was also mentioned as a facilitator (e.g., what helped the clinicians make the decision in a timely manner and how that impacted future patient care) by 29% of cases. For example, a PICU nurse described a transition from the ED to the PICU that was very smooth and calm: “They had a really great leader. Everything was calm, so it made me feel better about the situation, made me feel better about what we were doing…[it] flowed smoothly from ED to the PICU, it was nice.” (PICU nurse).
4.2.3. Interacting with family.
Interacting with family refers to factors that influenced how clinicians and the family or caregivers interacted, or did not interact. The task and organization work system elements were involved with this dimension. Interacting with family was (or should be) one goal-related activity in the process. Organizational culture, rules and procedures influence how this occurs. Interacting with family was mentioned as a barrier – something prevented clinicians from interacting with the family/caregivers, or made interacting with the family/caregivers challenging – by 29% of cases. For example, an ED support staff – a child life specialist – noted that body language and how clinicians behaved around the patient could hinder and even prevent important interactions with the child’s family – “[W]atch your body language or how you’re supporting the patient, because families feed off of that…feedback that families give often if they feel like they’re an inconvenience, [and] will say, I didn’t want to ask questions,” (ED child life specialist). Another common challenge was simply knowing where the family were. At night, the OR waiting areas are closed, so it could be difficult to know where the family had settled.
Interacting with family was also mentioned as a facilitator, such as factors that made it easier for clinicians to interact with the family/caregivers or things that supported family/caregivers interacting with clinicians, by 18% of cases. One simple, but important, factor was to help the family find nearby waiting areas so they could be close by if needed. An ED nurse described how they, or social workers, help family find the PICU waiting area when a patient is admitted to the PICU from the ED: “we try to direct them to the family waiting room, or as we arrive to the room, somebody from PICU…will say, hey, there’s a waiting room down here,” (ED nurse). The PICU nurses also mentioned this was helpful, in particular if someone let them, or the unit clerk, know where the family were.
4.2.4. Physical Environment.
Physical environment refers to how characteristics of the physical environment (e.g., lighting, noise, layout, distractions) impacted the care and transitions of pediatric trauma patients (Smith & Carayon-Sainfort, 1989). The physical environment work system element is involved in this dimension. Physical environment was mentioned as a barrier (i.e., the physical environment created challenges to clinicians, such as the trauma bay being too small or too noisy) by 29% of cases. For example, the anesthesia resident described a challenge preparing for the ED to OR care transition: “There’s like upwards of 30 people in the trauma bay…it’s absurdly crowded in the room, and that can make it difficult to do jobs that require lots of equipment and quiet,” ED to OR, (Anesthesia resident).
Physical environment was also mentioned as a facilitator (i.e., when the physical environment was appropriate and supported the work of clinicians) by 29% of cases. Some interviewees mentioned the location of where handoffs took place – the physical environment – as being important. A surgery resident said it was very important to conduct handoffs at the bedside, so they could show receiving clinicians rather than just tell them about incisions, drains, etc.
“[O]ftentimes you’re telling them what drains you left in, what incisions you made…And to physically be able to show them, lots of times they’ll, you’ll be like there’s a midline incision, they’ll want to look at it and see what exactly is there…I think that’s really helpful” (Surgery resident)
4.2.5. Role ambiguity.
Role ambiguity (Schmidt et al., 2014; Spear & Schmidhofer, 2005) refers to factors related to clinicians and staff being clear (or unclear) about their specific roles and related expectations. Role ambiguity was related to the organization work system element; the culture and management of the organization, in addition to the procedures, rules and leadership, could create or reduce role ambiguity. Role ambiguity was mentioned as a barrier – e.g., when staff/clinicians were unclear on who to get information from, or what they should or should not do – by 29% of cases. For example, an ED nurse mentioned that they often go to the OR during the transition, but are unsure of what they can or should do to help transition the patient – “ [T]here’s, you know, certain lines that you’re not supposed to cross…this is their territory, and I’m not going to go push any buttons…it’s also a matter of I’ve never worked in an OR, so I don’t know what I can and can’t touch” (ED nurse). Sometimes, particularly in transitions from the ED, personal protective equipment made it difficult to identify personnel and know who to ask questions. Of note, none of the attending physicians reported role ambiguity as a barrier; only physicians-in-training and others reported role ambiguity as a barrier.
Reduced role ambiguity was also mentioned as a facilitator, such as when roles and expectations were clear, by 32% of cases. Despite challenges reported by the surgery nurse, an anesthesia attending noted that the more formalized procedure of the OR to PICU care transition, including knowing who is responsible for doing what, helps prevent conflict and ensure tasks are done.
“The OR to PICU transition is usually pretty smooth, but there’s a, there’s defined roles. Nobody is fighting for those roles… there’s no struggle of roles or power or anything, because everybody has like if there’s an issue, we know exactly whose responsibility that is.” (Anesthesia attending)
4.2.6. Staffing/resources.
Staffing/resources refers to how having (or not having) available staff and resources impacted the ability of clinicians to care for and transition patients. The staffing/resources dimension was related to the organization work system element. The leadership of the organization makes decisions that directly affect staffing and other resource levels. This dimension was mentioned as a barrier when staffing and resources were inadequate, which led to high workload, extra handoffs and delays (e.g., Morrison & Rudolph, 2011), by 47% of cases. For example, an ED nurse described wanting to get a very sick child to the PICU as quickly as possible, where they are more familiar caring for very sick children and have the resources to do so, but experiencing delays because the PICU was full:
“[T]here are also definitely times when I want the patient to go upstairs, and I don’t have anywhere to put them… there are times that I’m like, this kid is really sick, and I would like somebody who is a little bit stronger at taking care of really sick kids to be here…[I have to get] a bed assignment, which usually goes pretty well, but we’ve been really full lately” (ED nurse).
Other barriers related to staff and resources were experienced in the ED, including needing nurses to care for the patient and complete documentation or staff to safely transport the patient.
Staffing/resources was also mentioned as a facilitator when there were enough staff and resources to appropriately care for and quickly transition the patient by 44% of cases. For example, in the ED, having an extra nurse in the trauma bay to complete documentation and coordinate with the OR or PICU while another provided care was very useful. A PICU fellow also noted that extra nurses made transitions go smoother, in particular when a patient first arrived on the unit:
“[T]here’s the nurse that’s assigned to the patient from both the ED and here. But when they get here, there’s like a team of nurses that show up that help… there’s a lot of little things that have to be done, you know, just changing the patient, moving them over, starting this IV here. And so it’s nice when you have an oversupply of staff to do that.” (PICU fellow).
4.2.7. Team cognition.
This dimension refers to factors that influence team cognition – i.e., planning, decision making, problem solving and problem assessment at the team level (Cooke et al., 2013) – as well as how good or poor team cognition impacts the care transition. The team cognition dimension was related to the task and organization work system element. The tasks, or goal-directed activities, of the care transition by definition were in pursuit of exchanging information, responsibility and authority between two or more clinicians. These communication interactions between two or more health care professionals with the goal of a safe transition constitute team cognition. Many organizational characteristics influenced those tasks, such as the rules and procedures about how transitions should occur.
Team cognition was mentioned as a barrier, making communication difficult and impacting the care transition, by 74% of cases. These barriers were primarily related to factors that made it difficult for the whole care team to share and understand information about the patient and plan for future care, in particular during and before handoffs. For example, when asked about what could be improved in the care transitions, an ED nurse described multiple conversations in the ED to OR handoff that forced clinicians to choose which was most important to listen to: “[T]he residents [are] talking over there, and then plus I’m talking. So [anesthetist]’s either going to decide to listen to me or decide to listen to them. And there is a lot of like commotion,” (ED nurse). Other team cognition barriers included factors that impeded team member interactions, such as lack of familiarity between team members (Cooke et al., 2007).
Team cognition was also mentioned as a facilitator, i.e., factors that improved team cognition and how having good team cognition improved the care transition, by 85% of cases. For example, an anesthesia attending described an instance when the entire PICU team, with an emphasis on the nurses, understood the background of the patient they received – “the PICU nurse was already, so when I got called up there, they already knew the background on that patient, and they knew what was going on” (Anesthesia attending). When asked why it was important the whole team was together, s/he responded:
“It’s because, you know, the doctors are only there with the patient for a short period of time. Whereas, the nurse is there for 12-hour shifts at a time, so they know the patient really well and they can voice any concerns they had. And we can also communicate in a team manner… so they’re on the same page.” (Anesthesia attending)
4.2.8. Technology.
This dimension refers to how characteristics, (lack of) usability and/or (lack of) usefulness of technologies, including health information technology, influenced the care transition (Carayon et al., 2006). The technology dimension was related to the tools and technologies work system element (Smith & Carayon-Sainfort, 1989). Technology was mentioned as a barrier, e.g., when technology was not useful, difficult to use or unreliable, by 35% of cases. In particular, paging was described as “archaic” by a surgery resident, with issues related to batteries and the pagers. The devices used by nurses had reception issues. The EHR was not useful in situations with high time pressure, like trauma. A surgery nurse explained issues with the EHR – “[T]he patient probably does not, may not, even have a chart here…CT, MRI, you know, chest X-rays are being read in real time…I don’t have the chance to read the report. I’m gleaning information from people” (Surgery nurse). The patient might not have a chart in the EHR so that the nurse cannot look up background information. While test results are entered as quickly as possible, clinicians may not have time to access the EHR and check the results. Other clinicians described challenges completing documentation in the EHR before the patient transitioned from the unit, which prevented others from viewing patient-related information to anticipate needs.
Technology was also mentioned as a facilitator, e.g., when the technology was easy to use, could be used to accomplish the goal of the user and was reliable, by 44% of cases. A surgical resident described using phones to communicate when they were unable to be present for a handoff because they were treating another emergent patient. The same surgery resident also advocated for using cell phones to text rather than use the paging system: “I can text on my phone and still ride in an elevator, right?… People don’t group text in a page. You can group text with your entire team using a phone…” (Surgery resident).
4.2.9. Characteristic of trauma process.
Characteristic of trauma process refers to inherent properties of caring for trauma patients that impact how clinicians and staff provide care and transition patients, especially including how the unique circumstance and condition of individual patients influence the process. Since this dimension was related to the patient, e.g., nature of injury, severity of illness, etc., it was related to the person work system element. This was mentioned as a barrier, such as when inherent time pressure and instability of patients made transitions stressful or challenging, by 15% of cases. An anesthetist described that, due to the lack of very severe traumas, the OR nurses sometimes feel unprepared to receive trauma patients emergently from the ED: “there’s no way to know [in trauma]. But our nurses aren’t that used to that. They’re used to kind of knowing information and having a plan, and sometimes it just doesn’t happen with trauma,” (Anesthetist).
Characteristic of trauma process was also mentioned as a facilitator, i.e., when individual patient characteristics made care transitions easier, by 15% of cases. A primary example was that transitions were easier with lower acuity or less complex patients because they are less rushed and there is less information to share during the handoff. A surgery resident comparing the ED to OR to the OR to PICU transition said that “less information needs to be transmitted, is essentially why it’s a slightly easier transition and handoff,” (Surgery resident).
4.2.10. Comparison of Care Transitions.
The percentage of total cases mentioning each dimension as a barrier or facilitator are shown in table 3. Anticipation was mentioned more frequently in ED to OR and OR to PICU transitions. ED decision making was not mentioned at all in OR to PICU transition, and was mentioned more frequently in ED to PICU than ED to OR transition. Interacting with family was mentioned more as a barrier in ED to OR care transition, but was also mentioned for the other two transitions. The physical environment and role ambiguity were mentioned most frequently in ED to OR care transition – the trauma bay was especially challenging with unstable, emergent cases. Staffing and other resources were mentioned across all care transitions, as was technology. There were issues related purely to characteristics of caring for a trauma patient, which would not be addressed with sociotechnical system redesign. In general, the ED to OR transition tended to have more barriers than the other transitions. The majority of barriers and facilitators across care transitions were related to team cognition.
5. Discussion
In this study, we identified nine dimensions of work system barriers and facilitators in care transitions of pediatric trauma patients from the ED to OR, OR to PICU and ED to PICU: anticipation, ED decision making, interacting with family, physical environment, role ambiguity, staffing/resources, team cognition, technology and characteristic of trauma care. We determined that all work system elements were involved in at least one dimension. We compared the frequency each dimension was mentioned as a barrier or facilitator in each care transition, looking at case counts to avoid over-emphasizing dimensions mentioned several times by only a few participants.
5.1. Work System Barriers and Facilitators
Many published studies on barriers and facilitators in care transitions include minimal information on the range of barriers and facilitators, and lack justification for the intervention that is implemented and evaluated. Anticipation, in the form of information being available early, gathering people and equipment in advance, was noted as being important in the literature (Agarwal et al., 2012; Craig et al., 2012; Lane-Fall et al., 2018; McElroy, Collins, et al., 2015; McElroy, Macapagal, et al., 2015). Related to this, people and equipment must be available due to staffing/resources (Lane-Fall et al., 2018; McElroy, Collins, et al., 2015; McElroy, Macapagal, et al., 2015). Role ambiguity (or lack thereof) was also very important (Lane-Fall et al., 2018). While we identify barriers and facilitators related to the physical environment and technology, these are less commonly mentioned in the literature (Craig et al., 2012; McElroy, Collins, et al., 2015). Previous studies described problems such as inaccurate or incomplete communication, lack of relationships/familiarity between clinicians (Lane-Fall et al., 2018; McElroy, Collins, et al., 2015; McElroy, Macapagal, et al., 2015); however, those studies did not link those challenges to team cognition theory (Cooke, 2015; Cooke et al., 2007; Cooke et al., 2005; Cooke et al., 2013), which could provide guidance in improvement efforts.
McElroy and colleagues (2015) found that issues varied by profession – that is, work system barriers and facilitators experienced by physicians were different than those experienced by nurses. For example, clinicians from the OR felt that initiating ICU care unnecessarily delayed handoff information, but the ICU clinicians felt it was very important and should be prioritized (McElroy, Macapagal, et al., 2015). In our study, we noted that attending physicians did not report barriers related to role ambiguity, but we did not systematically explore differences by profession as our focus was on the care transition process. This is an area for future work.
Catchpole et al. (2007) used an approach to improving OR to PICU care transitions informed by motor car racing, which involved teamwork under high time pressure and was anchored in HFE; but they did not clearly identify barriers or facilitators in the existing process. The themes they applied in their redesign tie closely to our dimensions. For example, the leadership practices they identified relate to ED decision making; and their task allocation addresses our dimension of role ambiguity. Anticipation in our study is related to their themes of predicting, planning and briefing. The team cognition dimension we identified relates to several themes they incorporated in the process redesign: situation awareness, discipline and composure (related to behaviors during communication), and involvement. To improve situation awareness, the anesthetist and intensivist were given responsibility for situation awareness and stepping back to ensure safety. To improve discipline and composure, the order of roles speaking in the handoff was specified, with a time for discussion set aside to reduce interruptions. The discussion step also included an opportunity for everyone, of all levels to speak up to improve involvement. The approaches used by Catchpole and colleagues (2007) could help address barriers to team cognition.
5.2. Focus on Team Cognition in Improvement Efforts
The prevalence of barriers and facilitators related to team cognition across transitions sets the stage to design an intervention based on team cognition theory (Cooke, 2015; Cooke et al., 2005; Cooke et al., 2013). Research to improve team cognition often utilizes team training (Cooke, 2015). Team training is important and useful in health care (Weaver et al., 2014); but given that clinicians experience high workloads and job demands, additional training may not be feasible nor sustainable. Therefore, changing the design of the sociotechnical (work) system should go beyond requiring additional training and leverage facilitators and mitigate barriers identified in our study. The redesign could include team handoffs when possible or using a checklist in an organized handoff. As our results show, organizational constraints on staff may preclude a team handoff.
Health information technology designed to support team cognition may be another solution. Shared displays have been developed to support team work in resuscitations (Parush et al., 2017; Wu et al., 2017); they may be useful in care transitions. Designing and implementing a technology must be done carefully so as not to unbalance the work system (Carayon et al., 2006; Smith & Carayon-Sainfort, 1989). A new technology could, if not carefully designed, unduly increase the workload of clinicians or create new safety hazards and harm patients. The new technology should support the entire team (Li, 2016). Decisions need to be made about the intended purpose of the technology: should it support the handoff, which has already been a major target for improvement (e.g., Moon et al., 2016; Zavalkoff et al., 2011)? Or should another activity within the care transition be targeted? Future work to design the new technology must focus on the barriers and facilitators related to team cognition that we identified in care transitions.
5.3. Limitations
While we studied multiple transitions to strengthen the validity of our findings, this study was completed at a single health care organization and our results are not necessarily generalizable beyond this setting. The work system barriers and facilitators in care transition may be different in urban or non-teaching hospitals. Future research should expand on our research and examine pediatric trauma care transitions in other settings.
Another limitation of our study is its focus on selected health care professions involved in care transitions. While we included many interviewees of different backgrounds (table 1), we did not include all professionals involved in care transitions (e.g., specific surgical specialties). We did not gather input from patients and their families/caregivers. The perspective of health care professionals is undoubtedly important, but we must also consider the work of patients and their families as we progress towards patient- and family-centered care (Valdez et al., 2015).
Our study uses data collected using semi-structured interviews; hence, our findings are based on the perspective of the health care professionals we interviewed. Interviewees described challenges with crowded and loud physical environments, and issues changing IV pumps, monitors, etc. during handoffs. Direct observations could help to identify additional issues, particularly in the physical ergonomic design of equipment. The combination of multiple methods, e.g., interview and observation, would produce a more complete understanding of the process.
6. Conclusion
Care transitions are important to patient safety and quality of care. When the transition goes well, it is an opportunity for efficient and effective information sharing, error prevention and recovery, enhanced team resilience, and delivery of safe, high-quality patient care. When transitions go poorly, information can be lost, errors can be made, and care can be delayed or inadequate. We investigated three care transitions common early in the hospital care of pediatric trauma patients, which are under high time pressure and uncertainty: transitions from ED to OR, OR to PICU and ED to PICU. Our findings support current evidence that many work system factors hinder and support care transitions. We identified already-known dimensions of barriers and facilitators, like role ambiguity, issues with technology, anticipation in receiving units and characteristics of trauma care, but also highlighted other dimensions, in particular team cognition.
Approaching care transitions from a SEIPS perspective allowed us to identify a wide range of barriers and facilitators while developing a clear understanding of the process involved in care transitions. Understanding barriers and facilitators in different care transitions and incorporating HFE knowledge can help guide improvement efforts to ensure care transitions go well rather than poorly. Future work could investigate solutions to enhance team cognition in care transitions, building on existing theories and research (Cooke, 2015; Cooke et al., 2005; Cooke et al., 2013). The work system could be redesigned to support team cognition through changes in the organization of the process (i.e., a team handoff) and the design of a new team-based health information technology.
Highlights.
Work system barriers and facilitators influence care transitions of pediatric trauma patients.
Team cognition is an important dimension of barriers and facilitators in care transitions.
Future solutions should support all members of the care team during care transitions.
Acknowledgements
Funding for this research was provided by the Agency for Healthcare Research and Quality (AHRQ) [Grant No. R01-HS023837]. The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), [Grant UL1TR002373]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. We thank the study participants, as our research would not be possible without them.
Appendix A. Development of Process Maps.
A1. Methods
A1.1. Data Analysis Methods
A1.1.1. Coding of transcripts.
All transcripts were cleaned to remove any identifying information, and were uploaded to Dedoose© web-based qualitative data analysis software. Relevant excerpts were then coded to a pre-determined coding scheme: (1) the specific transition; (2) the trauma level and at least one of (3) process/role or (4) barrier/facilitator (see table A.1). Two HFE researchers (ARW, BH) independently coded one transcript, and then met to review and resolve discrepancies. The same researchers then independently coded a second transcript, and met to review discrepancies; at this point, there were minimal differences, and each researcher coded nine of the remaining 16 interview transcripts.
Table A.1.
Dedoose Coding Scheme.
| Code | Definition | |
|---|---|---|
| Transition | ED to OR | This excerpt is about the transition from ED to OR. |
| ED to PICU | This excerpt is about the transition from ED to PICU. | |
| OR to PICU | This excerpt is about the transition from OR to PICU. | |
| Level | Level 1 | This excerpt is about level 1 traumas. |
| Level 2 | This excerpt is about level 2 traumas. | |
| Process/role | Who participates in care transitions, what tasks do they do (including preparation and follow-up), where and how are these tasks done, what information is shared during the transition, what tools/technology are used, etc. | |
| Barrier/Facilitator | What about the current organization of care transitions creates barriers or facilitators; what are the barriers and facilitators that makes care transitions more difficult or easier; what are the barriers and facilitators in the care transitions that make the transition go poorly or go well. | |
A1.1.2. Process map creation.
We exported the excerpts from the two transcripts that were coded to as “Process/role” by two researchers to Excel® by groups of each combination of transition and level (i.e. Level 1 ED to OR, Level 2 ED to OR, Level 1 ED to PICU, Level 2 ED to PICU, Level 1 OR to PICU and Level 2 OR to PICU). The process maps were drafted using the SEIPS-based process modeling method described by Wooldridge and colleagues (2017). The columns in these process maps represent the physical location tasks are done (e.g., ED, OR, PICU or patient transport between two units). The rows represent the phase of the care transition, e.g., transition preparation, transition, transition follow-up, similar to pre-turnover, handoff and post-turnover as described by Abraham, et al. (2012). Two researchers constructed two process maps together (ED to OR and OR to PICU) using LucidChart. For each excerpt, the researchers identified which role(s) was described as doing what task(s) with any tool(s)/technology(ies) used. Individual tasks that were mentioned together, as related, were grouped together in higher-level activities, appearing in boxes. The roles that complete each task are listed, with each new line in an activity box indicating a new role(s). Icons representing the tools and technologies used appear to the left of each line. After two process maps were constructed together, each researcher independently reviewed the excerpts for the ED to PICU transition for both levels and drafted a process map. The researchers then met to discuss and resolve any discrepancies.
One researcher then exported all of the excerpts coded to the “process/role” code in groups by care transition: ED to OR, OR to PICU and ED to PICU. Each excerpt was again reviewed to identify what tool(s)/technology(ies) were used by what role to do what task; this was then added to the process map. Any questions were resolved through a consensus-based process. After the process maps were constructed, clinicians on the research team, who were not involved in the data analysis, some of the participants and other stakeholders (e.g., nursing leadership, trauma program manager) reviewed the process maps to validate them as a form of member checking (Devers, 1999).
A.2. Results
Figures A.1, A.2 and A.3 show the process maps of the ED to OR, OR to PICU and ED to PICU care transitions, respectively. In the figures, columns represent the physical location that work occurs in (i.e., the involved hospital units and the physical movement between the two) and rows represent phases of the care transition (i.e., preparation, transition and follow up). The care transition progresses roughly moving right and down through the process map.
Activities that are distributed across time and space are shown in boxes connected by dashed lines, while activities that are related to other care transitions are shown in boxes with grey background. Differences in the care transition processes that vary based on patient acuity are show in different color text.
Figure A.1.
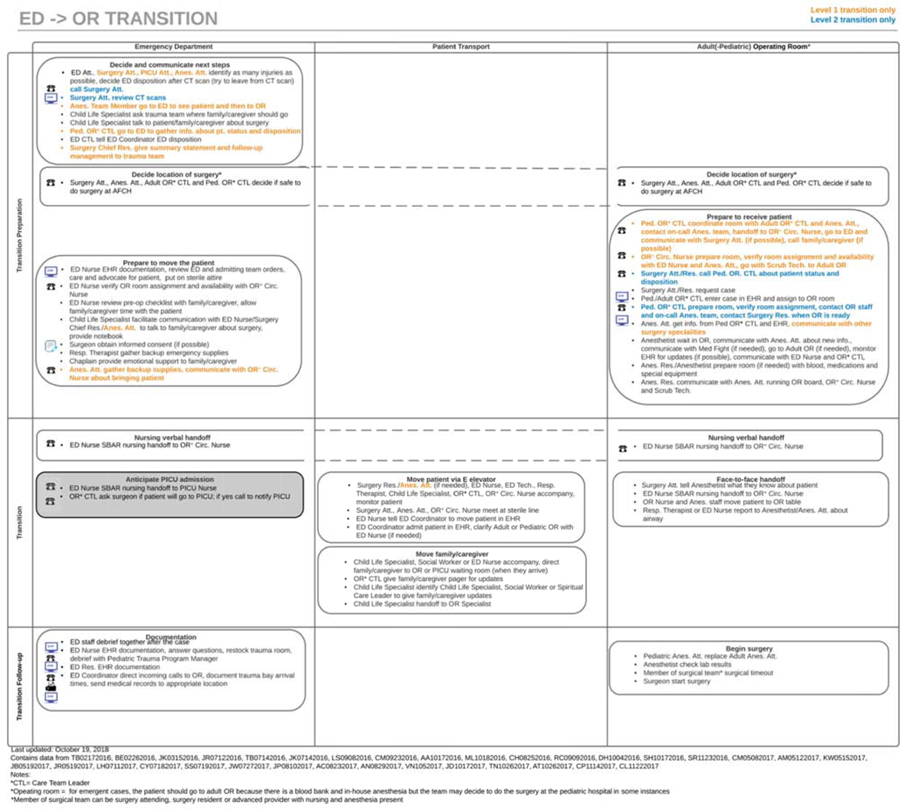
ED to OR care transition process map.
Figure A.2.
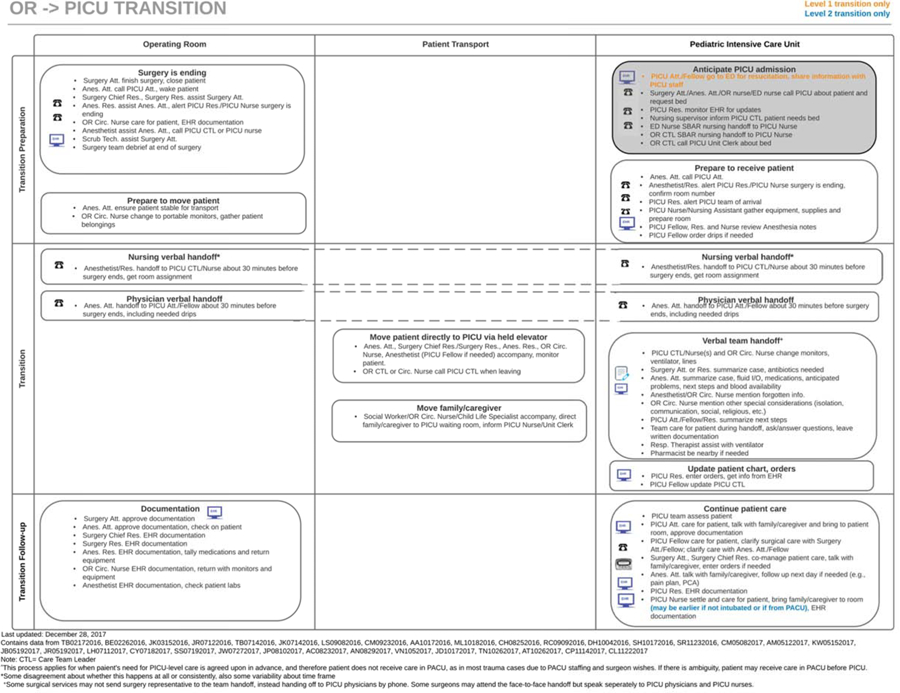
OR to PICU care transition process map.
Figure A.3.
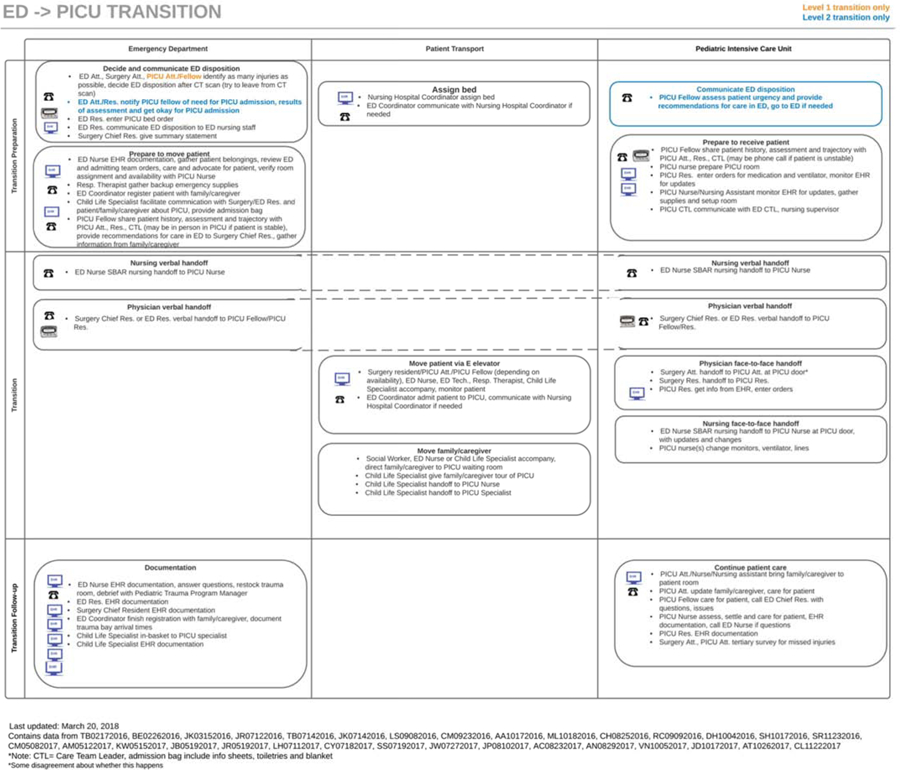
ED to PICU care transition process map.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Abraham J, Ihianle I, & Burton S (2017). Exploring Information Seeking Behaviors in Inter-unit Clinician Handoffs. Paper presented at the International Symposium on Human Factors and Ergonomics in Health Care. [Google Scholar]
- Abraham J, Kannampallil T, & Patel VL (2014). A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc, 21(1), 154–162. doi: 10.1136/amiajnl-2012-001351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham J, Kannampallil TG, & Patel VL (2012). Bridging gaps in handoffs: A continuity of care based approach. Journal of Biomedical Informatics, 45(2), 240–254. doi: 10.1016/j.jbi.2011.10.011 [DOI] [PubMed] [Google Scholar]
- Agarwal HS, Saville BR, Slayton JM, Donahue BS, Daves S, Christian KG, … Harris ZL (2012). Standardized postoperative handover process improves outcomes in the intensive care unit: A model for operational sustainability and improved team performance. Critical Care Medicine, 40(7), 2109–2115. doi: 10.1097/CCM.0b013e3182514bab [DOI] [PubMed] [Google Scholar]
- Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, & Kripalani S (2009). Hospitalist handoffs: A systematic review and task force recommendations. Journal of Hospital Medicine, 4(7), 433–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach C, Cheung DS, Apker J, Horwitz LI, Howell EE, O’Leary KJ, … Williams M (2012). Improving interunit transitions of care between emergency physicians and hospital medicine physicians: a conceptual approach. Academic Emergency Medicine, 19(10), 1188–1195. [DOI] [PubMed] [Google Scholar]
- Beaudin M, Daugherty M, Geis G, Moody S, Brown RL, Garcia VF, & Falcone RA Jr. (2012). Assessment of factors associated with the delayed transfer of pediatric trauma patients: an emergency physician survey. Pediatr Emerg Care, 28(8), 758–763. doi: 10.1097/PEC.0b013e318262414b [DOI] [PubMed] [Google Scholar]
- Berg M (1999). Patient care information systems and health care work: A sociotechnical approach. Int J Med Inform, 55(2), 87–101. [DOI] [PubMed] [Google Scholar]
- Bergrath S, Czaplik M, Rossaint R, Hirsch F, Beckers SK, Valentin B, … Brokmann JC (2013). Implementation phase of a multicentre prehospital telemedicine system to support paramedics: feasibility and possible limitations. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 21(1), 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KQ, & Mitchell TR (1991). A comparison of Just-In-Time and batch manufacturing: The role of performance obstacles. Academy of Management Journal, 34(4), 906–917. [Google Scholar]
- Cabrera D, Thomas JF, Wiswell JL, Walston JM, Anderson JR, Hess EP, & Bellolio MF (2015). Accuracy of ‘My Gut Feeling:’ Comparing System 1 to System 2 Decision-Making for Acuity Prediction, Disposition and Diagnosis in an Academic Emergency Department. The western journal of emergency medicine, 16(5), 653–657. doi: 10.5811/westjem.2015.5.25301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder LA, Forster AJ, Stiell IG, Carr LK, Perry JJ, Vaillancourt C, & Brehaut JC (2012). Mapping Out the Emergency Department Disposition Decision for High-Acuity Patients. Annals of Emergency Medicine, 60(5), 567–576.e564. doi: 10.1016/j.annemergmed.2012.04.013 [DOI] [PubMed] [Google Scholar]
- Carayon P (2009). The balance theory and the work system model…Twenty years later. International Journal of Human-Computer Interaction, 25(5), 313–327. [Google Scholar]
- Carayon P, Gurses AP, Hundt AS, Ayoub P, & Alvarado CJ (2005). Performance obstacles and facilitators of healthcare providers In Korunka C & Hoffmann P (Eds.), Change and Quality in Human Service Work (Vol. Volume 4, pp. 257–276). Munchen, Germany: Hampp Publishers. [Google Scholar]
- Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, & Brennan PF (2006). Work system design for patient safety: The SEIPS model. Qual Saf Health Care, 15(Supplement I), i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, & Gurses AP (2014). Human factors systems approach to healthcare quality and patient safety. Appl Ergon, 45(1), 14–25. doi: 10.1016/j.apergo.2013.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, & Wood KE (2009). Patient safety: The role of human factors and systems engineering In Rouse WB & Cortese DA (Eds.), Engineering the System of Healthcare Delivery: IOS Press. [Google Scholar]
- Catchpole K, De Leval MR, Mcewan A, Pigott N, Elliott MJ, Mcquillan A, … Goldman AJ (2007). Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Pediatric Anesthesia, 17(5), 470–478. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2010). Nonfatal Emergency Department Treated and Released Injuries, Both Sexes, Ages 0 to 24. Retrieved February 28 2019 www.cdc.gov/injury/wisqars
- Centers for Disease Control and Prevention. (2015). Injury Prevention and Control: Data & Statistics (WISQARS). 2015. Retrieved February 28 2019 www.cdc.gov/injury/wisqars
- Chatoorgoon K, Huezo K, Rangel E, Francois N, Schweer L, Daugherty M, … Falcone RA Jr (2010). Unnecessary imaging, not hospital distance, or transportation mode impacts delays in the transfer of injured children. Pediatr Emerg Care, 26(7), 481–486. doi: 10.1097/PEC.0b013e3181e5bef3 [DOI] [PubMed] [Google Scholar]
- Cooke NJ (2015). Team cognition as interaction. Current Directions in Psychological Science, 24(6), 415–419. [Google Scholar]
- Cooke NJ, Gorman JC, Duran JL, & Taylor AR (2007). Team cognition in experienced command-and-control teams. Journal of Experimental Psychology: Applied, 13(3), 146. [DOI] [PubMed] [Google Scholar]
- Cooke NJ, Gorman JC, Kiekel PA, Foltz P, & Martin M (2005). Using team communication to understand team cognition in distributed vs. co-located mission environments. Retrieved from http://www.dtic.mil/docs/citations/ADA441431
- Cooke NJ, Gorman JC, Myers CW, & Duran JL (2013). Interactive team cognition. Cognitive science, 37(2), 255–285. [DOI] [PubMed] [Google Scholar]
- Cowley A, & Durge N (2014). The impact of parental accompaniment in paediatric trauma: a helicopter emergency medical service (HEMS) perspective. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 22(1), 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig R, Moxey L, Young D, Spenceley NS, & Davidson MG (2012). Strengthening handover communication in pediatric cardiac intensive care. Pediatric Anesthesia, 22(4), 393–399. [DOI] [PubMed] [Google Scholar]
- CRICO Strategies. (2015). Malpractice risk in communication failures; 2015 Annual Benchmarking Report. Boston, Massachusetts: The Risk Management Foundation of the Harvard Medical Institutions, Inc. [Google Scholar]
- Daniellou F (2005). The French-speaking ergonomists’ approach to work activity: cross-influences of field intervention and conceptual models. Theoretical Issues in Ergonomics Science, 6(5), 409–427. doi: 10.1080/14639220500078252 [DOI] [Google Scholar]
- Devers KJ (1999). How will we know “good” qualitative research when we see it? Beginning the dialogue in health services research. Health Services Research, 34(5), 1153–1188. [PMC free article] [PubMed] [Google Scholar]
- Durojaiye AB, McGeorge NM, Puett LL, Stewart D, Fackler JC, Hoonakker PLT, … Gurses AP (2018). Mapping the Flow of Pediatric Trauma Patients Using Process Mining. Appl Clin Inform, 09(03), 654–666. doi: 10.1055/s-0038-1668089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farach SM, Danielson PD, Amankwah EK, & Chandler NM (2015). Admission patterns in pediatric trauma patients with isolated injuries. J Surg Res, 198(1), 13–18. doi: 10.1016/j.jss.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Glaser BG, & Strauss AL (1967). The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine. [Google Scholar]
- Glesne C (2016). Becoming qualitative researchers: An introduction (5th ed.). Boston, MA: Pearson Education, Inc. [Google Scholar]
- Hollnagel E, Wears R, & Braithwaite J (2015). Chapter 18: Why is work-as-imagined different from work-as-done? In Resilient Health Care, Volume 2: The Resilience of Everyday Clinical Work. Burlington, Vermont: Ashgate Publishing, Ltd. [Google Scholar]
- Hoonakker PLT, Carayon P, & Cartmill RS (2017). The impact of secure messaging on workflow in primary care: Results of a multiple-case, multiple-method study. Int J Med Inform, 100, 63–76. doi: 10.1016/j.ijmedinf.2017.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoonakker PLT, Wooldridge AR, Hose B-Z, Carayon P, Eithun B, Brazelton T, … Ross J (2018). Things Falling Through the Cracks: Information Loss During Pediatric Trauma Care Transitions. Paper presented at the 20th Congress of the International Ergonomics Association (IEA; 2018). [Google Scholar]
- Horwitz LI, Parwani V, Shah NR, Schuur JD, Meredith T, Jenq GY, & Kulkarni RG (2009). Evaluation of an asynchronous physician voicemail sign-out for emergency department admissions. Annals of Emergency Medicine, 54(3), 368–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISO. (2015). ISO 9000: Quality Management Systems. In. Genève, Switzerland: International Organization for Standardization. [Google Scholar]
- Jun GT, Morris Z, Eldabi T, Harper P, Naseer A, Patel B, & Clarkson JP (2011). Development of modelling method selection tool for health services management: From problem structuring methods to modelling and simulation methods. BMC Health Serv Res, 11(1), 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jun GT, Ward J, & Clarkson P (2010). Systems modelling approaches to the design of safe healthcare delivery: ease of use and usefulness perceived by healthcare workers. Ergonomics, 53(7), 829–847. doi: 10.1080/00140139.2010.489653 [DOI] [PubMed] [Google Scholar]
- Jun GT, Ward J, Morris Z, & Clarkson J (2009). Health care process modelling: which method when? International Journal for Quality in Health Care, 21(3), 214–224. doi: 10.1093/intqhc/mzp016 [DOI] [PubMed] [Google Scholar]
- Lane-Fall MB, Pascual JL, Massa S, Collard ML, Peifer HG, Di Taranti LJ, … Barg FK (2018). Developing a Standard Handoff Process for Operating Room–to-ICU Transitions: Multidisciplinary Clinician Perspectives from the Handoffs and Transitions in Critical Care (HATRICC) Study. The Joint Commission Journal on Quality and Patient Safety. [DOI] [PubMed]
- Leplat J (1989). Error analysis, instrument and object of task analysis. Ergonomics, 32(7), 813–822. [Google Scholar]
- Li Y (2016). Designing Health IT for Teamwork: A Human Factors Study of Hospital Bedside Rounds. (PhD), The University of Wisconsin - Madison, ProQuest database. (Order No. 10125263) [Google Scholar]
- McElroy LM, Collins KM, Koller FL, Khorzad R, Abecassis MM, Holl JL, & Ladner DP (2015). Operating room to intensive care unit handoffs and the risks of patient harm. Surgery, 158(3), 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy LM, Macapagal KR, Collins KM, Abecassis MM, Holl JL, Ladner DP, & Gordon EJ (2015). Clinician perceptions of operating room to intensive care unit handoffs and implications for patient safety: a qualitative study. The American Journal of Surgery, 210(4), 629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon TS, Gonzales MX, Woods AP, & Fox PE (2016). Improving the quality of the operating room to intensive care unit handover at an urban teaching hospital through a bundled intervention. Journal of Clinical Anesthesia, 31, 5–12. [DOI] [PubMed] [Google Scholar]
- Morrison JB, & Rudolph JW (2011). Learning from accident and error: Avoiding the hazards of workload, stress, and routine interruptions in the emergency department. Academic Emergency Medicine, 18(12), 1246–1254. doi: 10.1111/j.1553-2712.2011.01231.x [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulton SL, Haley-Andrews S, & Mulligan J (2010). Emerging technologies for pediatric and adult trauma care. Current opinion in pediatrics, 22(3), 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parush A, Mastoras G, Bhandari A, Momtahan K, Day K, Weitzman B, … Calder L (2017). Can teamwork and situational awareness (SA) in ED resuscitations be improved with a technological cognitive aid? Design and a pilot study of a team situation display. J Biomed Inform, 76, 154–161. doi: 10.1016/j.jbi.2017.10.009 [DOI] [PubMed] [Google Scholar]
- Perry SJ (2004). Transitions in care: Studying safety in emergency department signovers. Focus on Patient Safety, 7(2), 1–3. [Google Scholar]
- Peters LH, & O’Connor EJ (1980). Situational constraints and work outcomes: The influences of a frequently overlooked construct. Academy of Management Review, 5(3), 391–397. [Google Scholar]
- Peters LH, O’Connor EJ, & Eulberg JR (1985). Situational constraints: Sources, consequences, and future considerations. Research in Personnel and Human Resources Management, 3, 79–114. [Google Scholar]
- Potoka DA, Schall LC, & Ford HR (2001). Improved functional outcome for severely injured children treated at pediatric trauma centers. Journal of Trauma and Acute Care Surgery, 51(5), 824–834. [DOI] [PubMed] [Google Scholar]
- Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, & Ford HR (2000). Impact of pediatric trauma centers on mortality in a statewide system. Journal of Trauma and Acute Care Surgery, 49(2), 237–245. [DOI] [PubMed] [Google Scholar]
- Reine E, Rustoen T, Raeder J, & Aase K (2019). Postoperative patient handovers-Variability in perceptions of quality: A qualitative focus group study. J Clin Nurs, 28(3–4), 663–676. doi: 10.1111/jocn.14662 [DOI] [PubMed] [Google Scholar]
- Riesenberg LA, Leisch J, & Cunningham JM (2010). Nursing handoffs: A systematic review of the literature. American Journal of Nursing, 110(4), 24–34. [DOI] [PubMed] [Google Scholar]
- Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C, … Karpovich, K. P. (2009). Residents’ and attending physicians’ handoffs: a systematic review of the literature. Academic Medicine, 84(12), 1775–1787. [DOI] [PubMed] [Google Scholar]
- Robson C, & McCartan K (2016). Real World Research (Fourth ed.). West Sussex, UK: Wiley & Sons Ltd. [Google Scholar]
- Schmidt S, Roesler U, Kusserow T, & Rau R (2014). Uncertainty in the workplace: Examining role ambiguity and role conflict, and their link to depression—a meta-analysis. European Journal of Work and Organizational Psychology, 23(1), 91–106. [Google Scholar]
- Siemieniuch CE, & Sinclair MA (2015). Methods in Systems Ergonomics In Evaluation of Human Work (4th ed., pp. 855–879): CRC Press. [Google Scholar]
- Simsekler MCE, Ward JR, & Clarkson PJ (2018a). Design for patient safety: a systems-based risk identification framework. Ergonomics, 1–19. doi: 10.1080/00140139.2018.1437224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simsekler MCE, Ward JR, & Clarkson PJ (2018b). Evaluation of system mapping approaches in identifying patient safety risks. International Journal for Quality in Health Care, 30(3), 227–233. doi: 10.1093/intqhc/mzx176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MJ, & Carayon-Sainfort P (1989). A balance theory of job design for stress reduction. International Journal of Industrial Ergonomics, 4(1), 67–79. [Google Scholar]
- Spear SJ, & Schmidhofer M (2005). Ambiguity and workarounds as contributors to medical error. Ann Intern Med, 142(8), 627–630. [DOI] [PubMed] [Google Scholar]
- Stewart RM, Myers JG, Dent DL, Ermis P, Gray GA, Villarreal R, … Pruitt BA Jr. (2003). Seven hundred fifty-three consecutive deaths in a level I trauma center: the argument for injury prevention. J Trauma, 54(1), 66–71. doi: 10.1097/01.ta.0000046312.75231.74 [DOI] [PubMed] [Google Scholar]
- Stroud MH, Trautman MS, Meyer K, Moss MM, Schwartz HP, Bigham MT, … Insoft R (2013). Pediatric and neonatal interfacility transport: results from a national consensus conference. Pediatrics, 132(2), 359–366. doi: 10.1542/peds.2013-0529 [DOI] [PubMed] [Google Scholar]
- The Joint Commission. (2017). Inadequate hand-off communication. Sentinel Event Alert(58), 1–6. [PubMed] [Google Scholar]
- Valdez RS, Holden RJ, Novak LL, & Veinot TC (2015). Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc, 22(1), 2–10. doi: 10.1136/amiajnl-2014-002826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Veen M, & Moll HA (2009). Reliability and validity of triage systems in paediatric emergency care. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 17(1), 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver SJ, Dy SM, & Rosen MA (2014). Team-training in healthcare: A narrative synthesis of the literature. BMJ Qual Saf, 23(5), 359–372. doi: 10.1136/bmjqs-2013-001848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetterneck TB, Skibinski KA, Roberts TL, Kleppin SM, Schroeder ME, Enloe M, … Carayon P (2006). Using failure mode and effects analysis to plan implementation of smart i.v. pump technology. American Journal of Health-System Pharmacy, 63(16), 1528–1538. doi: 10.2146/ajhp050515 [DOI] [PubMed] [Google Scholar]
- Wooldridge AR, Carayon P, Hoonakker P, Hose B-Z, Ross J, Kohler JE, … Gurses AP (2018). Complexity of the pediatric trauma care process: implications for multi-level awareness. Cognition, Technology & Work. doi: 10.1007/s10111-018-0520-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge AR, Carayon P, Hundt AS, & Hoonakker PLT (2017). SEIPS-based process modeling in primary care. Appl Ergon, 60, 240–254. doi: 10.1016/j.apergo.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P, Nam MY, Choi J, Kirlik A, Sha L, & Berlin RB Jr. (2017). Supporting Emergency Medical Care Teams with an Integrated Status Display Providing Real-Time Access to Medical Best Practices, Workflow Tracking, and Patient Data. J Med Syst, 41(12), 186. doi: 10.1007/s10916-017-0829-x [DOI] [PubMed] [Google Scholar]
- Zavalkoff SR, Razack SI, Lavoie J, & Dancea AB (2011). Handover after pediatric heart surgery: a simple tool improves information exchange. Pediatric Critical Care Medicine, 12(3), 309–313. [DOI] [PubMed] [Google Scholar]


