Abstract
Background.
Stigma can exacerbate negative health outcomes in people living with HIV (PLWH). This longitudinal, cluster randomized controlled trial in rural Mpumalanga, South Africa, examined the interdependence of HIV-related stigma among pregnant couples living with HIV, and the potential impact of a lay health worker delivered intervention, Protect Your Family, on changes in stigma over time across couples, controlling for physical intimate partner violence (IPV), verbal IPV, gender, HIV knowledge, and months since HIV diagnosis. Using a form of the Actor-Partner Interdependence model, changes in stigma over time were also examined within each dyad of seroconcordant participants with HIV.
Method.
Antenatal clinics were randomized to experimental or control conditions, and participants completed baseline antenatal and 12-month postpartum assessments. Both women and male partners participated in intervention sessions in gender concordant groups and couple or individual sessions.
Results.
Multilevel models (N = 1475) revealed stigma was related to condition and verbal intimate partner violence, but not time. Using an Actor-Partner Interdependence cross-lagged path model to examine within dyad changes in stigma for seroconcordant couples (n = 201), intervention condition participants’ stigma levels were not interdependent over time. Women’s 12-month stigma was related to their partners’ stigma at baseline in the control condition, but not in the intervention condition.
Discussion.
Compared to women in the control condition, postpartum stigma among women in the intervention condition was not related to their male partners’ stigma, suggesting that women’s perception of stigma became uncoupled from that of their partners. The intervention may have promoted female empowerment to shape their own beliefs and attitudes towards what it means to be infected with HIV, and express their own agency in responding to how others treat them and they treat themselves.
Keywords: South Africa, HIV, Stigma, Dyadic, Couples, Intervention
Introduction
Stigma has been defined by Goffman (1963) as a quality or characteristic that a person may have that is seen by others as an undesirable stereotype. Stigma related to HIV is a product of attitudes regarding: a) acquisition of HIV and personal accountability for infection, b) the lethality and spread of the virus, c) visibility of being in a diseased state, and d) fear of being associated with the disease or diseased (Alonzo & Reynolds, 1995; Lee, Kochman, & Sikkema, 2002; Novick, 1997). HIV infection can cause individuals to experience feelings of social isolation and internalized stigma (i.e., taking on stigmatizing assumptions and stereotypes, coming to believe them, and applying them to oneself). Stigma can also reduce disclosure of HIV status in the healthcare setting (Alexandra Marshall, Brewington, Kathryn Allison, Haynes, & Zaller, 2017). Demographic factors may contribute to internalized stigma (Hasan et al., 2012), though some studies have found no relationship between levels of experienced internalized stigma and gender or income level (Sekoni, Obidike, & Balogun, 2012). In sub-Saharan Africa, people living with HIV from poorer households were at more than twice the risk of experiencing internalized stigma (Tsai, 2015), and people living with HIV who completed higher levels of education experienced lower rates of internalized stigma.
Stigma has a powerful negative impact on relationships, access to resources, social support, and wellbeing (Bos, Schaalma, & Pryor, 2008). Structural stigma has been associated in marginalized groups with poorer life satisfaction, mental health, and overall health, with this process potentially mediated through social support (Perales & Todd, 2018). The fear of being stigmatized by a partner can directly impact relationships and self-stigmatization, and can also result in fear of HIV status disclosure. Couple dynamics can contribute to engagement with HIV testing, care, and treatment for both partners (Wamoyi et al., 2017). Gender roles are also influential in conversations about HIV within relationships. For example, men may more commonly hide their status so that they may sustain or obtain a sexual/marital partner or assert their masculine role in the family to dismiss a woman’s suggestion to seek testing and/or treatment (Wamoyi et al., 2017). Relationships may be dominated by fear, reducing motivation to obtain treatment (Wamoyi et al., 2017). Among serodiscordant heterosexual couples, HIV-related stigma has been found to repress communication regarding HIV and sex, status disclosure, and seeking treatment (Van Der Straten, Vernon, Knight, Gómez, & Padian, 1998). Stigmatized partners may experience a lack of mutual support, violence, relationship dissolution, or difficulty coping (Rogers et al., 2016) rather than a mutually beneficial approach to treatment. For example, if partners living with HIV disclose their HIV status to each other, they can remind and support each other to actively engage in treatment (Wamoyi et al., 2017). Fear of stigma, coupled with potential discrimination, which is associated with deleterious mental health outcomes (Bauer & Scheim, 2019), may place individuals in a situation where they are cut off from this valuable social support, and this could further reinforce their feelings of alienation.
Stigma negatively impacts treatment uptake and adherence at each step of the prevention of mother to child transmission (PMTCT) protocol (Turan & Nyblade, 2013). HIV-related stigma can cause women to fear the results of an HIV test if they do not know their status, to worry about the reactions of partners, and to anticipate shame and exclusion from society if their status is disclosed, all of which can result in neglecting treatment crucial to their health, partners’ health, and the health of the neonate. A crucial component of the PMTCT program, antenatal HIV clinics (ANCs), may be avoided as a result of HIV-related stigma, fear of testing and unwanted disclosure (Turan & Nyblade, 2013).
Few studies have examined the impact of HIV-related stigma on close relationships in which one or both partners have HIV/AIDS (Huang, Zhang, & Yu, 2018; Talley & Ann Bettencourt, 2010). A longitudinal study of Chinese HIV serodiscordant couples found the ability of two individuals to move away from identifying as “self” to identifying as “a couple” predicted fewer depressive symptoms (Huang et al., 2018). However, the protective effects of being a couple were diminished when HIV stigma was high (Huang et al., 2018). Among seroconcordant couples in South Africa, within traditional gender scripts, the impact of HIV reduced disclosure, care, support, and adherence, yet at the same time, when power was equalized, risky behaviors were reduced (Bhagwanjee et al., 2013). The characteristics of the relationship appear to interact HIV-related stigmatizing situations and negatively influence couple-level and individual level outcomes (Talley & Ann Bettencourt, 2010). These studies recommend interventions that focus on dyadic functioning to prevent and reduce HIV-related stigma in couples affected by HIV/AIDS.
Interventions aimed at reducing HIV-related stigma in couples affected by HIV/AIDS are needed. This team previously found an intervention to enhance PMTCT among pregnant women living with HIV significantly reduced HIV-related stigma (Peltzer et al., 2018). The current study aimed to evaluate the effectiveness of the PMTCT intervention on reducing stigma among one or both members of couples in South Africa. This is an important area of study because of the high rates of HIV reported in South Africa, with approximately 270,000 new infections per year, an incidence rate of 5.46 infections per 1000 individuals, and approximately 100,000 AIDS-related deaths per year (Joint United Nations Programme on HIV and AIDS, 2018). Among this population, approximately 10% of relationships are among seroconcordant individuals (Lurie et al., 2003). HIV management is not only important to consider among serodiscordant couples, but among seroconcordant couples as well. Compared to their serodiscordant counterparts, seroconcordant couples have immunological profiles which could indicate faster virus progression (Jaumdally et al., 2019). Decreasing stigma is an important avenue to consider, because it might help promote increased medication adherence (Dlamini et al., 2009). It was theorized that an intervention to reduce stigma in pregnant couples could have important implications for HIV prevention and management.
Method
This study utilized data from a larger study designed to examine PMTCT among HIV positive women and the effects of male partner intervention involvement on women’s health behaviors (Jones et al., 2014). Participants were recruited from 12 ANCs in rural Mpumalanga Province, South Africa. Participating ANCs were matched by size and randomized to intervention or control conditions; based on clinic condition assignment, participants from each clinic attended intervention or control sessions. Eligible participants were women 18 years of age or older, HIV-positive, eight to 24 weeks pregnant, and having a male partner. Recruitment was carried out from April 10, 2014 to January 30, 2017, and participants were followed for one year post-delivery. After informed consent was obtained, participants completed assessments in their preferred language (e.g., English, isiZulu, seSotho) using an audio computer assisted self-interview system to promote response accuracy, reduce bias, and improve consistency of measurement.
Conditions
As part of the study women who had not disclosed their HIV status were given the option to disclose to their partner during a session, and to attend sessions with or without their partner present. Between both conditions PMTCT standard of care was offered at the clinic visits. During the prenatal period, both conditions offered gender specific group sessions, followed by one individual or couple’s session. Following delivery, two individual or couple’s sessions were provided.
Intervention condition.
The PMTCT intervention, “Protect Your Family” (PYF), is a manualized intervention that targets ART adherence, partner HIV testing, HIV stigma, HIV serostatus disclosure, partner communication, IPV reduction, safe infant feeding, safer conception, family planning, and dual method sexual barrier use. Information presented is in accordance with guidelines from the Department of Health PMTCT information (National Department of Health - Republic of South Africa, 2015). More information about the PYF intervention can be found in Jones and colleagues (2014).
Control condition.
Control condition participants viewed video presentations on adult and child health issues i.e., diarrhea, dehydration and exclusive breastfeeding, nutrition, immunization, sexual abuse, fevers, burns and alcohol use.
Measures
Demographic and psychosocial characteristics.
Demographic information collected included age, education, relationship status, relationship length, monthly income, if participants were diagnosed with HIV during this pregnancy, and participant’s number of children.
HIV related stigma.
The Berger HIV Stigma Scale (HSS) was used to assess individuals’ levels of HIV related stigma (Berger, Ferrans, & Lashley, 2001). Only individuals living with HIV were asked to complete this measure. The HSS is a 40-item four-point Likert-type scale with response options ranging from 1 = Strongly Disagree to 4 = Strongly Agree. A sample item reads, “People have physically backed away from me when they learn I have HIV.” At timepoint 1, the HSS displayed excellent internal reliability for both women and men (α = .954 and α = .949, respectively), and it continued to display excellent internal reliability at timepoint 2 for women and men (α = .956 and α = .952, respectively).
Intimate partner violence.
Physical and verbal intimate partner violence (IPV) among couples in the past four weeks were measured using an adapted version of the Conflict Tactics Scale 18 (CTS-18) (Straus, 1979) with both physical and verbal subscales demonstrating strong internal consistency at timepoint 1 α = 0.92 and α = 0.86 and timepoint 2 α = 0.93 and α = 0.87, respectively. The CTS is scored on a seven-point Likert-type scale, with responses indicating the frequency of different forms of conflict behaviour. At timepoint 1, the average physical IPV was 1.37 (SD = 4.46) and verbal IPV was 3.74 (SD = 6.28). At timepoint 2, the average physical IPV was 1.48 (SD = 4.83) and verbal IPV was 3.61 (SD = 6.19).
HIV and PMTCT knowledge.
HIV and PMTCT knowledge was assessed using 18 items with response options including, “Yes, No, or Don’t Know.” This measure was partially adapted from Fisher, Fisher, Misovich, Kimble, and Malloy (1996). Sample items included, “Sexually transmitted diseases (STDs) put people at greater risk for HIV infection or infection with new forms of the virus.”, “If both partners are HIV+ unprotected sex can put them at risk for infection with new forms of the virus.”, and “Can a HIV positive mother infect her baby with HIV through breastfeeding?” Each correct answer was awarded 1 point. On average at timepoint 1 participants scored 13.98 (SD = 3.36) and 14.17 (SD = 2.98) at timepoint 2.
Time since HIV diagnosis at baseline.
Time since HIV diagnosis was assessed using one question which asked, “When were you diagnosed with HIV? Give your best guess.” At baseline the average time since HIV diagnosis in months was 28.66 (Median = 13.16; SD = 39.6).
Analytic Plan
First, data were screened by examining descriptive statistics. Any observations on stigma at timepoint 1 or timepoint 2 which were greater than four standard deviations from the mean would be considered an outlier and examined for removal. Next qq-plots would be examined to determine the tenability of normality. Finally, Little’s missing complete at random (MCAR) test would be performed on the stigma data to determine if data could reasonably be assumed to be missing completely at random. After data screening, using all couples’ data (Valid N = 1475, Excluded = 1401), a multilevel model using random intercepts examining stigma changes over time was fit with maximum-likelihood estimation in SPSS version 24 and 25. This was a two-level model, with individuals being the first level and couple being the second level. The model included the variables of condition, time, physical IPV, verbal IPV, gender, HIV knowledge, months since HIV diagnosis at baseline, and the interaction between time and condition. Then, in order to analyze stigma relationships over time within male and female living with HIV partner dyads and control for each partners’ baseline stigma levels, a non-exchangeable cross-lagged actor partner interdependence path model (Kenny, Kashy, & Cook, 2006) was fit using a structural equation modeling (SEM) framework using Mplus version 8 (Muthén & Muthén, 1998-2017). No latent variables were used, so the model would reduce to a saturated path model. If the assumption of MCAR was found to be tenable, full-information maximum likelihood (FIML) would be used to estimate the model. Data were kept unstandardized due to using SEM, and not needing to interpret variance components. Due to fitting a just-identified model, model fit indices would not be available. Using condition as a grouping variable, multi-group analysis was used to test differences in paths between the groups to elucidate if the relationships between male and female stigma across time differed depending on whether participants were in the experimental or control condition. These group differences were tested by assessing model fit by freely estimating parameters in both groups, and comparing the parameters to one another using Wald tests in Mplus. This multigroup strategy would allow for a more flexible analytic approach, as any number of parameters could be compared across groups without introducing complex interactions to the model.
Data Screening
For the combined data of both seroconcordant and discordant couples used in the MLM, no outliers greater than 3 z-scores were found in the outcome variable of stigma. Examination of the qq-plot also revealed the distribution of stigma conformed adequately to a normal distribution. Little’s MCAR test found the assumption of missing completely at random was tenable, χ2(14) = 19.66, p =.141, for all continuous variables used in the MLM (e.g. months since diagnosis, stigma, HIV knowledge, verbal IPV, and physical IPV).
In terms of missingness for seroconcordant couples (n = 201), 3% of female timepoint 1 HIV-related stigma was missing, 24.4% of female timepoint 2 HIV-related stigma, 5% of male timepoint 1 stigma, and 55.2% of male timepoint 2 HIV-related stigma. Little’s MCAR test found the assumption of missing completely at random was tenable, χ2(19) = 15.28, p =.705. QQ plots for male and female stigma revealed no large discrepancies from a normal distribution, and there was no standardized score larger than 3.11 (standardized within group by gender and timepoint).
Results
Psychosocial Outcomes
Results of the multilevel model including both serodiscordant and seroconcordant couples revealed that only condition F(1, 919) = 26.45, p < .001 and verbal IPV F(1, 1458) = 14.55, p < .001 were significantly related to stigma. The random effect for intercepts was also significant (Estimate = 0.11, SE = 0.01, p < .001). Using this as an estimate of the variance explained by couples relative to residual variance at the first level of the model (Residual Variance = 0.17), the intraclass correlation coefficient was computed as 0.39. No differences in stigma were found for time F(1, 736) = 0.25, p = .618, physical IPV F(1, 1347) = 0.09, p = .771, gender F(1, 959) = 2.51, p = .114, HIV knowledge F(1, 1470) = 0.01, p = .945, or months since HIV diagnosis F(1, 890) = 0.72, p = .395. Finally, the interaction between time and condition was also found to be non-significant F(1, 741) = 1.34, p = .247.
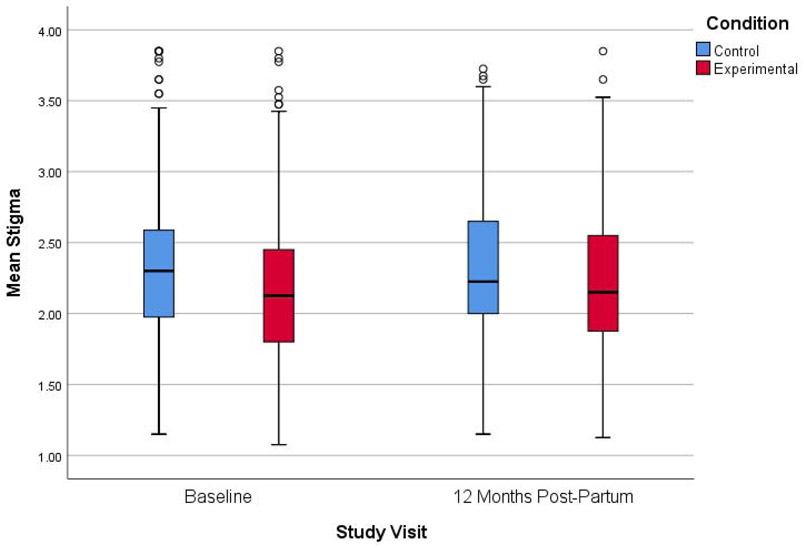
Using the experimental condition as the reference group it was found that the control condition had on average higher levels of stigma (b = 0.14, SE = 0.04, p < .001). Examining the coefficient for verbal IPV (b = 0.01, SE = 0.003, p < .001) revealed that holding all other variables in the model constant, each one-point change in verbal IPV was associated with an average mean change in the stigma scale by 0.01 points. Figure 1 shows differences in stigma over time by condition.
Fig. 1.
Boxplot of Stigma findings from baseline to 12-months post-partum for the experimental and control groups
Cross-lagged Regression
In order to further examine possible associations within each dyad, a cross-lagged path model in SEM was fit on a subset of the overall couples’ data who were both living with HIV (n = 201). Tables 1 and 2 provide key demographic and outcome variables by condition, as well as any significant differences between them at baseline. Figure 2 shows the path model proposed. Using FIML estimation, the total sample size was 201 dyads (seroconcordant couples living with HIV), with 105 in the control condition and 96 in the experimental condition. Table 3 shows model parameter estimates for both groups. To examine whether the actor and partner relationships differed in each group, a Wald test was used to compare the four direct effects. A significant difference in the relationships of HIV-related stigma across time, χ2(4) = 11.2, p =.024, was identified when simultaneously testing all four paths. With an overall significant omnibus test, each parameter was tested separately to determine which specific direct effects differed between groups. A significant difference was found between groups on the male partner effect, χ2(1) = 4.51, p =.034. The female actor effect, χ2(1) = 0.98, p =.321, male actor effect, χ2(1) = 1.15, p =.283, and female partner effect, χ2(1) = 1.75, p =.186 were not significant.
Table 1.
Baseline Differences Between Conditions on Key Female Study Variables (n = 201)
| Variable | Overall | Control | Experimental | p |
|---|---|---|---|---|
| Stigma | 2.18 (0.51) | 2.23 (0.55) | 2.13 (0.46) | .231 |
| Age | 29.64 (5.54) | 30.39 (5.66) | 28.81 (5.3) | .041 |
| Relationship Status | .084 | |||
| Not married, not living together | 75 (37.3%) | 38 (36.2%) | 37 (38.5%) | - |
| Not married, living together | 84 (41.8%) | 39 (37.1%) | 45 (46.9%) | - |
| Married | 40 (19.9%) | 27 (25.7%) | 13 (13.5%) | - |
| Relationship Length | .691 | |||
| Less than 6 months | 8 (4%) | 5 (4.8%) | 3 (3.1%) | - |
| Between 6 and 12 months | 26 (12.9%) | 12 (11.4%) | 14 (14.6%) | - |
| More than a year | 165 (82.1%) | 87 (82.9%) | 78 (81.3%) | - |
| Education | .804 | |||
| Up to 9 | 48 (23.9%) | 25 (23.8%) | 23 (24%) | - |
| 10 to 11 | 103 (51.2%) | 52 (49.5%) | 51 (53.1%) | - |
| 12 years or more | 48 (29.3%) | 27 (25.7%) | 21 (21.9%) | - |
| Monthly Income | 1129.18 (3071.12) | 1409.04 (4131.81) | 822.81 (989.44) | .344 |
| Number of Children | 1.73 (1.26) | 1.79 (1.19) | 1.66 (1.34) | .3 |
| Diagnosed with HIV During Pregnancy | .94 | |||
| Yes | 80 (39.8%) | 42 (40%) | 38 (39.6%) | - |
Note. Continuous variables reported as M(SD), and compared using Mann-Whitney U tests. Categorical variables reported as number (%) falling into group, and compared using chi-square test. For female variables, there were 6 missing cases for baseline stigma and HIV diagnosis during pregnancy, and 2 missing cases for all others.
Table 2.
Baseline Differences Between Conditions on Key Male Study Variables (n = 201).
| Variable | Overall | Control | Experimental | p |
|---|---|---|---|---|
| Stigma | 2.19 (0.53) | 2.2 (0.51) | 2.19 (0.56) | .881 |
| Age | 35.24 (6.76) | 36.14 (6.91) | 34.25 (6.47) | .072 |
| Relationship Status | .128 | |||
| Not married, not living together | 70 (34.8%) | 33 (31.4%) | 37 (38.5%) | - |
| Not married, living together | 85 (42.3%) | 42 (40%) | 43 (44.8%) | - |
| Married | 46 (22.9%) | 30 (28.6%) | 16 (16.7%) | - |
| Relationship Length | < .001 | |||
| Less than 6 months | 5 (2.5%) | 4 (3.8%) | 1 (1%) | - |
| Between 6 and 12 months | 30 (14.9%) | 4 (3.8%) | 26 (27.1%) | - |
| More than a year | 166 (82.6%) | 97 (92.4%) | 69 (71.9%) | - |
| Education | .038 | |||
| Up to 9 | 41 (20.4%) | 18 (17.1%) | 23 (24%) | - |
| 10 to 11 | 83 (41.3%) | 38 (36.2%) | 45 (46.9%) | - |
| 12 years or more | 77 (38.3%) | 49 (46.7%) | 28 (29.2%) | - |
| Monthly Income | 3617.58 (7675.46) | 4513.46 (10210.57) | 2637.71 (2834.96) | .029 |
| Number of Children | 2.16 (1.72) | 2.17 (1.71) | 2.15 (1.75) | .882 |
Note. Continuous variables reported as M(SD), and compared using Mann-Whitney U tests. Categorical variables reported as number (%) falling into group, and compared using chi-square test. For male variables, there were 10 missing cases for baseline stigma.
Fig. 2.
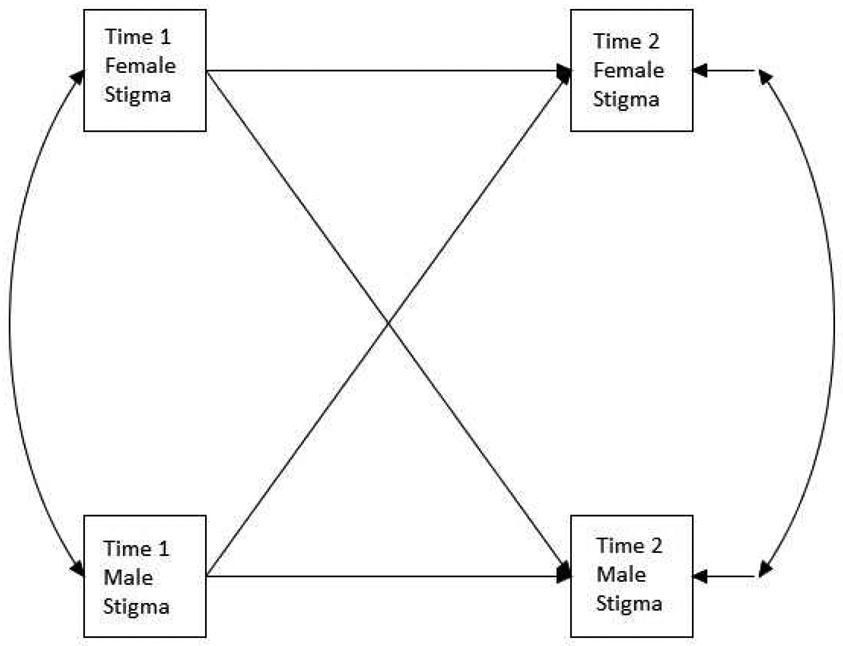
Cross-lagged path model.
Table 3.
FIML Cross-lagged Regression Parameter Estimates.
| Parameter | Estimate | SE | Z | p |
|---|---|---|---|---|
| Control Group | ||||
| Timepoint 2 Female Stigma ON | ||||
| Timepoint 1 Female Stigma | 0.56 | 0.10 | 5.67 | < .001 |
| Timepoint 1 Male Stigma | 0.22 | 0.11 | 2.1 | .036 |
| Timepoint 2 Male Stigma ON | ||||
| Timepoint 1 Male Stigma | 0.40 | 0.14 | 2.84 | .004 |
| Timepoint 1 Female Stigma | 0.29 | 0.12 | 2.43 | .015 |
| Covariance between Time 2 Male and Female Stigma | 0.00 | 0.03 | −0.09 | .929 |
| Covariance between Time 1 Male and Female Stigma | 0.11 | 0.03 | 3.74 | < .001 |
| Means | ||||
| Timepoint 1 Female Stigma | 2.23 | 0.05 | 41.45 | < .001 |
| Timepoint 1 Male Stigma | 2.19 | 0.05 | 43.07 | < .001 |
| Intercepts | ||||
| Timepoint 2 Female Stigma | 0.50 | 0.24 | 2.12 | .034 |
| Timepoint 2 Male Stigma | 0.64 | 0.30 | 2.18 | .029 |
| Variances | ||||
| Timepoint 1 Female Stigma | 0.30 | 0.04 | 7.19 | < .001 |
| Timepoint 1 Male Stigma | 0.25 | 0.04 | 6.96 | < .001 |
| Residual Variances | ||||
| Timepoint 2 Female Stigma | 0.19 | 0.03 | 6.37 | < .001 |
| Timepoint 2 Male Stigma | 0.17 | 0.04 | 4.82 | < .001 |
| Experimental Group | ||||
| Timepoint 2 Female Stigma ON | ||||
| Timepoint 1 Female Stigma | 0.37 | 0.16 | 2.36 | .018 |
| Timepoint 1 Male Stigma | −0.12 | 0.12 | −1.00 | .319 |
| Timepoint 2 Male Stigma ON | ||||
| Timepoint 1 Male Stigma | 0.18 | 0.15 | 1.27 | .205 |
| Timepoint 1 Female Stigma | 0.02 | 0.17 | 0.11 | .911 |
| Covariance between Time 2 Male and Female Stigma | 0.02 | 0.05 | 0.44 | .66 |
| Covariance between Time 1 Male and Female Stigma | 0.03 | 0.03 | 1.14 | .253 |
| Means | ||||
| Timepoint 1 Female Stigma | 2.13 | 0.05 | 44.14 | < .001 |
| Timepoint 1 Male Stigma | 2.19 | 0.06 | 37.98 | < .001 |
| Intercepts | ||||
| Timepoint 2 Female Stigma | 1.61 | 0.39 | 4.09 | < .001 |
| Timepoint 2 Male Stigma | 1.65 | 0.42 | 3.92 | < .001 |
| Variances | ||||
| Timepoint 1 Female Stigma | 0.22 | 0.03 | 6.73 | < .001 |
| Timepoint 1 Male Stigma | 0.31 | 0.05 | 6.85 | < .001 |
| Residual Variances | ||||
| Timepoint 2 Female Stigma | 0.31 | 0.05 | 5.84 | < .001 |
| Timepoint 2 Male Stigma | 0.26 | 0.06 | 4.62 | < .001 |
Control condition results identified that male partner effect was positive and significant (b = 0.22, SE = 0.11, p = .036), indicating that higher levels of male HIV-related stigma at timepoint 1 predicted higher levels of female HIV-related stigma at timepoint 2. Specifically, on average, for each one-point increase in male stigma at timepoint 1, female stigma at timepoint 2 increased by 0.22 points. In contrast, in the experimental condition, this partner effect was not significant (b = −0.12, SE = 0.12, p = .319); partners’ stigma did not influence each other. This finding also held after controlling for baseline male and female income at timepoint 2 within the model.
Discussion
This study examined the impact of an intervention on stigma within couples, and the role of interdependence on both partners. Regarding stigma, the control condition received the standard of care PMTCT and childhood health videos. The experimental condition offered not only the PMTCT standard of care, but components from the PYF program to help directly address HIV stigma. Across all participants, stigma was not seen to significantly change over time (see Figure 1). However, examining stigma changes within HIV-seroconcordant dyads, postpartum levels of stigma among women in the intervention condition were less likely to be associated with that of their male partners (the non-significance of the path from timepoint 1 Male Stigma to timepoint 2 Female Stigma in the intervention condition in Figure 2), suggesting that women’s perception of stigma became uncoupled from that of their partners. Conversely, couples’ perceptions of stigma in the control condition were more likely to be connected, as stigma increased or decreased over time.
Women attending the intervention may have become more empowered to form their own beliefs and attitudes. Feeling empowered in relationships has been linked to experiencing lower levels of IPV and less sexual risk behavior (McMahon, Volpe, Klostermann, Trabold, & Xue, 2015; Muldoon, Deering, Feng, Shoveller, & Shannon, 2015; Teitelman, Ratcliffe, Morales-Aleman, & Sullivan, 2008). Zembe, Townsend, Thorson, Silberschmidt, and Ekstrom (2015) reported finding, “astonishingly high levels of IPV among women who have multiple sexual partners in a peri-urban, Black South African township. Almost 9 out of 10 young women reported being beaten and/or raped, exploited and verbally abused in intimate relationships in the past 12 months” (pg. 13). The authors also note that, “Although young women reported various forms of relationship power inequity in their main partnerships, there were aspects of their main partnerships where many of them perceived equal decision-making power… The men also believed that their female main partners commanded greater respect in their relationships than casual partners” (pg. 14). They recommend the development of strategies that not only serve to reduce violence in intimate relationships, but focus on sexual risk behavior and attempt to foster broader forms of female empowerment (Zembe et al., 2015). Despite finding no evidence that stigma changed over time, intervention effects might have contributed to helping women feel more empowered to express and embody their own beliefs about living with HIV. This experience could potentially lead to them being more inclined to advocate for themselves within the confines of their relationship and more broadly in their larger community. This could help them gain more access to social support to help them avoid negative outcomes associated with stigma (Perales & Todd, 2018), and facilitate in the process to change attitudes in the community and larger social structures (Kontomanolis, Michalopoulos, Gkasdaris, & Fasoulakis, 2017; Rice et al., 2018).
Given previously published results showing decreases in stigma among women (Peltzer et al., 2018), it is important to highlight differences in this study that may be related to these outcomes. The previous study treated stigma as a categorical variable, while this study treated stigma as a continuous variable. Additionally, this study included men in the analysis, which may have affected the results as the program was not as strong in changing their stigma attitudes compared to women. Another key difference was that the previous study examined a phase of the study where male partners did not participate with their female partners, as opposed to this study which focuses on data where both partners participated in the study together. It is possible that having their male partner present weakened the stigma reduction components of the intervention.
Despite not seeing a significant reduction in stigma (see Figure 1), lessening the influence of a male partner’s stigma beliefs may be clinically meaningful. As discussed by Kontomanolis and colleagues (2017), HIV stigma is often perpetuated by societal forces well beyond the purview of individuals. In more patriarchal societies, this can leave women disenfranchised in being able to make use of information that medical providers and public health advocates may be attempting to share in order to reduce stigma and promote better quality of life. These more distal outside forces of stigma can manifest at a number of levels, such as at the structural level of society, within communities, and interpersonally (Rice et al., 2018). In attempting to reduce stigma in women living with HIV, perhaps an intermediate goal of reducing the influence of societies judgements is a first step and more practical goal. Women may not feel less stigma about HIV; it may be that after the PYF program, their attitudes were based on their own conclusions. Once they realize that their opinions are valuable and important, they may be more empowered to change that opinion in the future considering new information they learn.
Limitations
Notable limitations of this study include biases that may have arose due to self-report measures for stigma, and study attrition. Participants may have been hesitant to be completely forthright about how they felt about HIV stigma due to not wanting to speak negatively about themselves or potentially their partner. Also, as noted previously in other publications from this study, attrition could have led to self-selection bias. Rodriguez and colleagues (2017) noted logistics obstacles facing rural communities in PMTCT care. Due to limited resources, certain women may have had to leave the study due to financial or economic considerations. With their vulnerability of living with HIV, and the potential for IPV, this decision might not have been in their control. This differential attrition could have limited the availability of couples with higher levels of IPV and stigma.
Conclusions
HIV does not exist in a vacuum, and during the perinatal period, women are singularly vulnerable to the influence of their partners. In a previous women-only intervention, decreased stigma was associated with participation in the intervention, male involvement, and condom use, while increased stigma was associated with participation in the control condition, unemployment, HIV diagnosis prior to pregnancy, and alcohol use (Peltzer et al., 2018).
This study sought to extend these results to examine the interdependent influence on stigma within the couple. In fact, results suggest that the intervention may reduce the influence exerted by men among women after participating in an intervention. Further research is needed to both identify methods to reduce HIV-related stigma among women during pregnancy and to explore the potential for partners to facilitate that process. It is also recommended that future research examine potential change dyadically both in study design and analytic methodology. Examining change across dyads can obfuscate the nature of complex relationships, and fail to capture the larger scope by which individuals are potentially influenced by a network of others beyond their own agency.
Research Highlights.
Verbal intimate partner violence, but not physical, appeared to predict stigma.
Time since HIV diagnosis and HIV knowledge did not appear to predict stigma.
Intervention group women appeared to have stigma unrelated to their HIV+ partners’.
Acknowledgements:
This study was funded by a grant from NIH (R01HD078187) and with the support of the University of Miami Miller School of Medicine Center for AIDS Research, funded by an NIH grant (P30AI073961).
Footnotes
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alexandra Marshall S, Brewington KM, Kathryn Allison M, Haynes TF, & Zaller ND (2017). Measuring HIV-related stigma among healthcare providers: a systematic review. AIDS Care, 29(11), 1337–1345. doi: 10.1080/09540121.2017.1338654 [DOI] [PubMed] [Google Scholar]
- Alonzo AA, & Reynolds NR (1995). Stigma, HIV and AIDS: An exploration and elaboration of a stigma trajectory. Social Science & Medicine, 41(3), 303–315. doi: 10.1016/0277-9536(94)00384-6 [DOI] [PubMed] [Google Scholar]
- Bauer GR, & Scheim AI (2019). Methods for analytic intercategorical intersectionality in quantitative research: Discrimination as a mediator of health inequalities. Soc Sci Med, 226, 236–245. doi: 10.1016/j.socscimed.2018.12.015 [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, & Lashley FR (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24(6), 518–529. doi: 10.1002/nur.10011 [DOI] [PubMed] [Google Scholar]
- Bhagwanjee A, Govender K, Reardon C, Johnstone L, George G, & Gordon S (2013). Gendered constructions of the impact of HIV and AIDS in the context of the HIV-positive seroconcordant heterosexual relationship. Journal of the International AIDS Society, 16(1), 18021. doi: 10.7448/IAS.16.1.18021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos AR, Schaalma H, & Pryor J (2008). Reducing AIDS-related stigma in developing countries: The importance of theory- and evidence-based interventions. Psychology, Health & Medicine, 13(4), 450–460. doi: 10.1080/13548500701687171 [DOI] [PubMed] [Google Scholar]
- Dlamini PS, Wantland D, Makoae LN, Chirwa M, Kohi TW, Greeff M, . . . Holzemer WL (2009). HIV stigma and missed medications in HIV-positive people in five African countries.(Author abstract). AIDS Patient Care and STDs, 23(5), 377. doi: 10.1089/apc.2008.0164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Misovich SJ, Kimble DL, & Malloy TE (1996). Changing AIDS Risk Behavior: Effects of an Intervention Emphasizing AIDS Risk Reduction Information, Motivation, and Behavioral Skills in a College Student Population. Health Psychology, 15(2), 114–123. doi: 10.1037/0278-6133.15.2.114 [DOI] [PubMed] [Google Scholar]
- Goffman E (1963). Stigma notes on the management of spoiled identity. Englewood Cliffs, N.J.: Prentice-Hall. [Google Scholar]
- Hasan MT, Nath SR, Khan NS, Akram O, Gomes TM, & Rashid SF (2012). Internalized HIV/AIDS-related stigma in a sample of HIV-positive people in Bangladesh.(Report). Journal of Health Population and Nutrition, 30(1), 22. doi: 10.3329/jhpn.v30i1.11272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Zhang J, & Yu NX (2018). Couple identity and well-being in Chinese HIV serodiscordant couples: resilience under the risk of stigma. AIDS Care, 1–9. doi: 10.1080/09540121.2018.1510105 [DOI] [PubMed] [Google Scholar]
- Jaumdally SZ, Liebenberg LJP, Gumbi PP, Little F, Jaspan HB, Gamieldien H, . . . Passmore JS (2019). Partner HIV serostatus impacts viral load, genital HIV shedding and immune activation in HIV-infected individuals. J Acquir Immune Defic Syndr. doi: 10.1097/QAI.0000000000002089 [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV and AIDS. (2018). UNAIDS Data 2018. Retrieved from https://www.unaids.org/sites/default/files/media_asset/unaids-data-2018_en.pdf [Google Scholar]
- Jones D, Peltzer K, Weiss SM, Sifunda S, Dwane N, Ramlagan S, . . . Spence A (2014). Implementing comprehensive prevention of mother-to-child transmission and HIV prevention for South African couples: study protocol for a randomized controlled trial.(Medical condition overview). Trials, 15(1). doi: 10.1186/1745-6215-15-417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, & Cook WL (2006). Dyadic data analysis. New York: New York: : Guilford Press. [Google Scholar]
- Kontomanolis EN, Michalopoulos S, Gkasdaris G, & Fasoulakis Z (2017). The social stigma of HIV-AIDS: society's role. HIV AIDS (Auckl), 9, 111–118. doi: 10.2147/HIV.S129992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R, Kochman A, & Sikkema K (2002). Internalized Stigma Among People Living with HIV-AIDS. AIDS and Behavior, 6(4), 309–319. doi: 10.1023/A:1021144511957 [DOI] [Google Scholar]
- Lurie NM, Williams GB, Zuma PK, Mkaya-Mwamburi DD, Garnett SG, Sweat SM, . . . Karim SS (2003). Who infects whom? HIV-1 concordance and discordance among migrant and non-migrant couples in South Africa. AIDS, 17(15), 2245–2252. doi: 10.1097/01.aids.0000088197.77946.ba [DOI] [PubMed] [Google Scholar]
- McMahon JM, Volpe EM, Klostermann K, Trabold N, & Xue Y (2015). A systematic review of the psychometric properties of the Sexual Relationship Power Scale in HIV/AIDS research. Arch Sex Behav, 44(2), 267–294. doi: 10.1007/s10508-014-0355-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muldoon KA, Deering KN, Feng CX, Shoveller JA, & Shannon K (2015). Sexual relationship power and intimate partner violence among sex workers with non-commercial intimate partners in a Canadian setting. AIDS Care, 27(4), 512–519. doi: 10.1080/09540121.2014.978732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2017). Mplus User’s Guide (Eighth ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Department of Health - Republic of South Africa. (2015). National Consolidated Guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in children, adolescents, and adults. Retrieved from http://www.sahivsoc.org/Files/ART%20Guidelines%2015052015.pdf [Google Scholar]
- Novick A (1997). Stigma and AIDS: Three Layers of Damage. Journal of the Gay and Lesbian Medical Association, 1(1), 53–60. doi: 10.1023/B:JOLA.0000007011.17392.fb [DOI] [Google Scholar]
- Peltzer K, Babayigit S, Rodriguez VJ, Jean J, Sifunda S, & Jones DL (2018). Effect of a multicomponent behavioural PMTCT cluster randomised controlled trial on HIV stigma reduction among perinatal HIV positive women in Mpumalanga province, South Africa. SAHARA-J: Journal of Social Aspects of HIV/AIDS, 15(1), 80–88. doi: 10.1080/17290376.2018.1510787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perales F, & Todd A (2018). Structural stigma and the health and wellbeing of Australian LGB populations: Exploiting geographic variation in the results of the 2017 same-sex marriage plebiscite. Soc Sci Med, 208, 190–199. doi: 10.1016/j.socscimed.2018.05.015 [DOI] [PubMed] [Google Scholar]
- Rice WS, Logie CH, Napoles TM, Walcott M, Batchelder AW, Kempf MC, . . . Turan JM (2018). Perceptions of intersectional stigma among diverse women living with HIV in the United States. Soc Sci Med, 208, 9–17. doi: 10.1016/j.socscimed.2018.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez VJ, Lacabe RP, Privette CK, Douglass KM, Peltzer K, Matseke G, . . . Jones DL (2017). The Achilles' heel of prevention to mother-to-child transmission of HIV: Protocol implementation, uptake, and sustainability. SAHARA-J: Journal of Social Aspects of HIV/AIDS, 14(1), 38–52. doi: 10.1080/17290376.2017.1375425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers AJ, Achiro L, Bukusi EA, Hatcher AM, Kwena Z, Musoke PL, . . . Darbes LA (2016). Couple interdependence impacts HIV-related health behaviours among pregnant couples in southwestern Kenya: a qualitative analysis. Journal of the International AIDS Society, 19(1). doi: 10.7448/IAS.19.1.21224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekoni AO, Obidike OR, & Balogun MR (2012). Stigma, medication adherence and coping mechanism among people living with HIV attending General Hospital, Lagos Island, Nigeria. African Journal of Primary Health Care & Family Medicine, 4(1). doi: 10.4102/phcfm.v4i1.417 [DOI] [Google Scholar]
- Straus M (1979). Measuring intrafamily conflict and violence: The conflict tactics (CT) scales. Journal of Marriage and the Family, 75–88. [Google Scholar]
- Talley A, & Ann Bettencourt B (2010). A Relationship-Oriented Model of HIV-Related Stigma Derived from a Review of the HIV-Affected Couples Literature. AIDS and Behavior, 14(1), 72–86. doi: 10.1007/s10461-008-9493-y [DOI] [PubMed] [Google Scholar]
- Teitelman AM, Ratcliffe SJ, Morales-Aleman MM, & Sullivan CM (2008). Sexual relationship power, intimate partner violence, and condom use among minority urban girls. J Interpers Violence, 23(12), 1694–1712. doi: 10.1177/0886260508314331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A (2015). Socioeconomic Gradients in Internalized Stigma Among 4,314 Persons with HIV in Sub-Saharan Africa. AIDS and Behavior, 19(2), 270–282. doi: 10.1007/s10461-014-0993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan J, & Nyblade L (2013). HIV-related Stigma as a Barrier to Achievement of Global PMTCT and Maternal Health Goals: A Review of the Evidence. AIDS and Behavior, 17(7), 2528–2539. doi: 10.1007/s10461-013-0446-8 [DOI] [PubMed] [Google Scholar]
- Van Der Straten A, Vernon KA, Knight KR, Gómez CA, & Padian NS (1998). Managing HIV among serodiscordant heterosexual couples: Serostatus, stigma and sex. AIDS Care, 10(5), 533–548. doi: 10.1080/09540129848406 [DOI] [PubMed] [Google Scholar]
- Wamoyi J, Renju J, Moshabela M, McLean E, Nyato D, Mbata D, . . . Wringe A (2017). Understanding the relationship between couple dynamics and engagement with HIV care services: insights from a qualitative study in Eastern and Southern Africa. Sexually Transmitted Infections, 93(Suppl 3). doi: 10.1136/sextrans-2016-052976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zembe YZ, Townsend L, Thorson A, Silberschmidt M, & Ekstrom AM (2015). Intimate Partner Violence, Relationship Power Inequity and the Role of Sexual and Social Risk Factors in the Production of Violence among Young Women Who Have Multiple Sexual Partners in a Peri-Urban Setting in South Africa. PLoS One, 10(11), e0139430. doi: 10.1371/journal.pone.0139430 [DOI] [PMC free article] [PubMed] [Google Scholar]