During the rapidly evolving novel coronavirus disease 2019 (COVID-19) outbreak, more than a million cases have been diagnosed worldwide; however, there have been limited reports of HIV and COVID-19 coinfection at the time of writing. We report a case highlighting the challenge of diagnosing COVID-19 and Pneumocystis jirovecii pneumonia (PJP) in an individual with HIV.
A 55-year-old male presented with a 7-day history of fevers, cough, and hypoxia. Comorbidities include well controlled HIV infection (diagnosed 2006, current CD4+ cell count 422 cells/μl (35.6%), HIV-1 viral load <20 copies/ml), on emtricitabine/tenofovir disoproxil 200/245 mg and raltegravir 1200 mg once daily; and mild asthma. He had no prior history of PJP, was an ex-smoker, lived with his partner, and neither had recent travel histories nor contact with confirmed COVID-19 cases.
Chest computed tomography (CT) (Fig. 1) showed extensive subpleural and para-mediastinal cystic changes, subpleural ground-glass changes bilaterally, most prominent in the upper lobes with relative sparing of the lung bases; consistent with PJP. Incidental interstitial lung fibrosis and paraseptal emphysema was also reported.
Fig. 1.
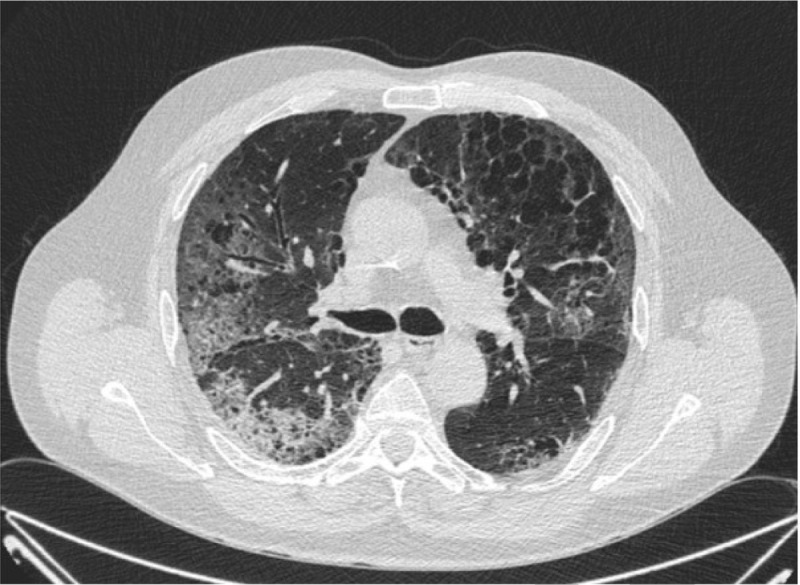
Chest computer tomography image slice showing extensive subpleural and para-mediastinal cystic changes, subpleural ground-glass changes bilaterally.
A lower respiratory tract-induced sputum was tested for respiratory pathogens using multiplex PCR and P. jirovecii DNA was detected. SARS-CoV-2 RNA was not detected by real-time PCR (RT-PCR) of an initial combined nose and throat swab (day 2). Investigations for other respiratory pathogens were negative.
PJP treatment was commenced with intravenous cotrimoxazole (120 mg/kg/24 h) and oral prednisolone 40 mg twice daily. He deteriorated 3 days into treatment and required critical care. A repeat throat swab (day 7) detected SARS-CoV-2 by RT-PCR.
He improved with high-flow oxygen not requiring intubation or ventilation. He was discharged (day 14) to complete 21 days oral treatment followed by long-term PJP prophylaxis.
We report the first case of P. jirovecii and SARS-CoV-2 detection in an individual with well controlled HIV. At the time of writing, only one other HIV/COVID-19 coinfection case has been published, with limited details of the individual's HIV status [1], and an European regional database of HIV/COVID-19 cases is currently under way [2]. We recommend further epidemiological data from HIV/COVID-19 cases to be collected and reported to understand the relationship between COVID-19, HIV, and antiretroviral therapy.
Sensitivity of RT-PCR from throat swabs to detect SARS-CoV-2 RNA has been reported as 95% [3]. However, retrospective studies comparing RT-PCR against combined clinical and radiographic criteria to diagnose COVID-19 in an epidemic setting reported lower sensitivities of RT-PCR at 70–80% [4]. Lower detection rates are associated with time from symptom onset, dropping from 100% to 40% if taken after day 5 of symptoms [5]. Retrospective testing of this patient's-induced sputum, taken within 26 h of the negative throat swab, confirmed the presence of SARS-CoV-2. Lower respiratory samples by induced sputum may aid diagnosis in the presence of negative upper respiratory samples [6].
The detection of P. jirovecii DNA in the induced sputum and an initial negative SARS-CoV-2 result in the presence of characteristic features of PJP formed the basis of the PJP diagnosis. The significance of detected P. jirovecii DNA using PCR alone remains uncertain and may represent colonization of the respiratory tract. Immunofluorescence microscopy was not available in this case. The prevalence of detectable P. jirovecii DNA in healthy immunocompetent adults has been reported between 0% and 20% [7,8]. However, in 100% of lung autopsy samples from immunocompetent individuals with detectable P. jirovecii DNA, detailed immunofluorescence microscopy revealed both cyst and trofozoite forms suggestive of actively replicating P. jirovecii[9], suggesting mild PJP infection may be present even in immunocompetent adults with detectable P. jirovecii.
Clinically COVID-19 and PJP may present with similar features of dry cough, exercise desaturation, and relatively normal chest auscultation. Common chest CT findings for both conditions include ground-glass pattern with interlobular septal thickening [10,11]. Implications of missed COVID-19 diagnoses include missed opportunities for contact tracing and prevention of onward transmission in an epidemic setting. Clinical management of PJP and COVID-19 also differs, particularly high-dose corticosteroid therapy is recommended in severe PJP [12]; however, there is no evidence for corticosteroid therapy in COVID-19, and observational data suggest increased mortality and secondary infection rates in influenza, and impaired clearance of the closely related SARS-CoV and MERS-CoV viral infections [13].
In conclusion, we report the first case of an individual living with HIV diagnosed and treated for both COVID-19 and PJP. Diagnosis of either conditions in the presence of both pathogens is challenging due to overlapping clinical and radiological features and limitations of current diagnostic assays, with clinical and public health implications in the current COVID-19 pandemic.
Acknowledgements
We would like to acknowledge the person described in the case report for their consent and contributions to this article.
Ethics and consent: Ethics committee approval was not required, nor funding requested. Patient consent was granted for this article and images to be used.
Author contributions: H.C., L.B.S., M.J.L.: cowritten. R.S., S.T.D.: review.
Conflicts of interest
M.J.L. has received grants and honoraria by Gilead Sciences not related to this work. H.C., L.B.S., R.S., S.T.D. have no disclosures to make.
References
- 1.Zhu F, Cao Y, Xu S, Zhou M. Co-infection of SARS-CoV2 and HIV in a patient in Wuhan City China. J Med Virol 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NEAT ID Foundation 2020. COVID-19 HIV co-infection data dash-board. NEAT ID Foundation. [online]. Available from https://www.neat-id.org/. [Accessed 6 April 2020].
- 3.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DKW, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill 2020; 25:2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-19. Nature 2020; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 6.Han H, Luo Q, Mo F, Long L, Zheng W. SARS-CoV-2 RNA more readily detected in induced sputum than in throat swabs of convalescent COVID-19 patients. Lancet Infect Dis 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leigh TR, Kangro HO, Gazzard BG, Jeffries DJ, Collins JV. DNA amplification by the polymerase chain reaction to detect sub-clinical Pneumocystis carinii colonization in HIV-positive and HIV-negative male homosexuals with and without respiratory symptoms. Respir Med 1993; 87:525–529. [DOI] [PubMed] [Google Scholar]
- 8.Medrano FJ, Montes-Cano M, Conde M, de la Horra C, Respaldiza N, Gasch A, et al. Pneumocystis jirovecii in general population. Emerg Infect Dis 2005; 11:245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ponce CA, Gallo M, Bustamante R, Vargas SL. Pneumocystis colonization is highly prevalent in the autopsied lungs of the general population. Clin Infect Dis 2010; 50:347–353. [DOI] [PubMed] [Google Scholar]
- 10.Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hidalgo A, Falcó V, Mauleón S, Andreu J, Crespo M, Ribera E, et al. Accuracy of high-resolution CT in distinguishing between Pneumocystis carinii pneumonia and nonpneumocystitis carinii pneumonia in AIDS patients. Eur Radiol 2003; 13:1179–1984. [DOI] [PubMed] [Google Scholar]
- 12.BHIVA British HIV Association and British Infection Association Guidelines for the treatment of opportunistic infection in HIV-seropositive individuals 2011. HIV Med 2011; 12: Suppl. 2: 1–140. [DOI] [PubMed] [Google Scholar]
- 13.Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet 2020; 395:473–475. [DOI] [PMC free article] [PubMed] [Google Scholar]


