1. Background of COVID 19
In December 2019, a local outbreak of pneumonia of initially unknown cause was detected in Wuhan (Hubei, China), and was quickly determined to be caused by a novel coronavirus, namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In early January 2020, a novel type of Coronavirus (CoV) was identified in the bronchoalveolar lavage sample of a subject affected by pneumonia of unknown origin (Li, Q. et al., 2020; WHO-Statement, 2020). The virus was provisionally named novel coronavirus (2019-nCoV) (Zhu et al., 2020b) to differentiate it from the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) (Drosten et al., 2003) and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) (de Groot et al., 2013), responsible for two previous outbreaks, in 2002 and 2012, respectively (Ashour et al., 2020). Successively, the International Committee on Taxonomy of Viruses (2020) defined it as SARS-CoV-2 and the associated disease has been called 2019 Coronavirus Disease (COVID-19). SARSCoV-2 rapidly spread worldwide, forcing the World Health Organization (WHO) to declare the outbreak as a pandemic on March 11, 2020 (Gorbalenya et al., 2020; WHO Director-General's speech, 2020). In response to this ongoing public health emergency, an online interactive dashboard, hosted by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University, Baltimore, MD, USA, was developed to visualize and track reported cases of coronavirus disease 2019 (COVID-19) in real time (Dong et al., 2020a; John Hopkins, 2020).
As of July 1, 2020, almost 11 million cases have been reported in 216 countries, areas, or territories in all continents except for Antarctica, with over half a million deaths [John Hopkins University, 2020]. Children seem to be less affected than adults, but data regarding epidemiologic characteristics and clinical features of COVID-19 in pediatric ages are very poor and essentially based on limited case series (Lu et al., 2020; Liu et al., 2020a). In a report of 72,314 cases from Chinese Center for Disease Control and Prevention (CDC), about 2% of all patients were aged < 19 years, but no specific clinical information was available (Wu and McGoogan, 2020).
COVID-19 is caused by the SARS-CoV-2 virus, which is called a corona virus because under the microscope (Fig. 1 ), it shows spikes, which form a “crown”. The spikes are proteins that protrude from the surface of the virus and that enable the virus to attach to epithelial cells. In particular, the Corona virus uses the spike proteins to attach to angiotensin II receptors on the cells along the airway down to the alveolar cells that line the air sacs in the lungs. After it attaches to these cells, the virus gets incorporated into the cells. It is quite diabolical in how it then takes over the entire cellular apparatus to make RNA copies of itself. Eventually the cell dies, and the many RNA copies of the virus leave to attack other cells.
Fig. 1.
Coronavirus image.
Attacking the lung cells not only causes damage locally, but it also stimulates the immune system. The resulting inflammatory response serves to protect the body by neutralizing the virus, but it can also cause significant damage to bystander tissues, including normal areas of lung. Associated with the inflammatory response is leakage of fluid into the air sacs, which manifests as pneumonia. There is also loss of vaso-regulation of the pulmonary capillary bed, which prevents matching of ventilation and perfusion, disrupting gas exchange, particularly oxygenation. The drop in oxygen levels may increase respiratory drive. The patient breathes more rapidly and deeply inducing stress and strain on the lung and resulting in Patient Self-Inflicted Lung Injury (P-SILI). The lung injury can progress to Acute Respiratory Distress Syndrome (ARDS). Unlike much ARDS, in early stages of COVID-19 the lungs remain very pliable and thus do not require high ventilator pressure or increased work of breathing for carbon dioxide excretion.
The inflammatory response does not restrict itself just to the lungs but also injures other organs in the body. When exaggerated it leads to large increases in blood levels of inflammatory mediators, the cytokines. The consequence of the “cytokine storm” includes dysfunction in the brain (delirium), damage to the heart (inflammation of the heart muscle or myocarditis), and damage to the kidneys (Acute Kidney Injury or AKI). There can also be damage to the liver, which may leak enzymes into the blood early as a marker that identifies the COVID-19 syndrome. Unlike the lungs for which there are ventilators, or the heart for which there are drugs like norepinephrine and vasopressin, and the kidney for which there is dialysis, there is no widely-available life-support technology for the liver. Progression of the liver to failure in a late stage of the syndrome is a poor prognostic sign that portends a terminal state and death.
2. How the Corona virus works
Fig. 2 summarizes the pathophysiological sequence following infection with SARS-CoV-2 virus, starting with damage to the lung that interferes with breathing, and proceeding to an inflammatory response that injures other organs. The pathophysiology helps explain how the patient perceives the syndrome (the symptoms) and how the clinicians can evaluate the patient (the signs).
Fig. 2.
Coronavirus pathway.
Fig. 3 adapted from the CDC website shows a set of common symptoms such as fever; which is the response of the body to inflammation, a dry cough reflecting injury to the lungs, and fatigue, which is a response to generalized inflammation. There are also some less-common symptoms, such as headache, a strange loss of smell and taste; which COVID-19 shares with other viral infections, and then signs such as confusion, blueish face or lips representing the low oxygen levels as the lung starts to fail. Finally, there is the possibility that the virus can attach itself to the GI track in the same way it attaches itself to the lung cells and that could lead to nausea vomiting or diarrhea.
Fig. 3.
Common symptoms of COVID-19 syndrome.
3. Diagnosing COVID-19
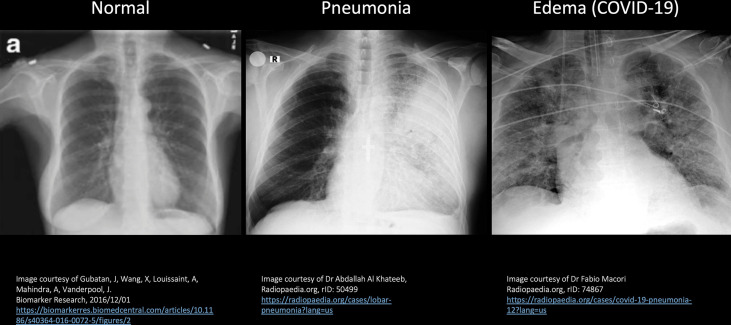
Fig. 4 shows a sequence of Chest X Ray images starting with normal lungs on the left, left lung pneumonia in the middle and COVID-19 pneumonia on the right image, all of which can differentiate disease processes and identify images more likely to be seen with COVID-19 (Gubatan et al., 2016). On the normal patient X-ray (left image), you see that the lungs are filled with air and there are streaks of normal blood vessels which are the white lines going through the lungs. On the middle image, you can see that the right lung is fairly normal, much like what we saw on the left, but the left lung shows this very white area in a highly demarcated area. This so-called consolidation, restricted to one lung, is very typical of a bacterial pneumonia. COVID-19 is a viral pneumonia (right image) which presents with whiteness occurring on both sides. Notice that the lungs are not completely opaque, and you can partially see through the lung, which is termed the ‘Ground-glass’ appearance. Ground-glass opacification/opacity (GGO) is a descriptive term referring to a region of hazy lung radiopacity, often fairly diffuse, in which the edges of the pulmonary vessels may be difficult to appreciate (Hansell et al., 2008). The ground-glass appearance is sort of what you would see with shower glass. This patient is also quite ill as you can see that there is an endotracheal tube placed to support breathing and there is also a visible intravenous line in the superior vena cava (CVP line).
Fig. 4.
Sequence of chest X-Ray images.
SARS-CoV-2 infection can be confirmed based on the patient's history, clinical manifestations, imaging characteristics, and laboratory tests. Chest CT examination plays an important role in the initial diagnosis of the novel coronavirus pneumonia (Liu et al., 2020d). Multiple patchy ground glass opacities in bilateral multiple lobular with periphery distribution are typical chest CT imaging features of the COVID-19 pneumonia (Xu et al., 2020). The sequence of Cat Scan (CT) images shown in Fig. 5 demonstrates the same scenarios, which are similar to the sequence of Chest X-rays. Cat Scans allow us to take a very fine slice through just one section of the body, in this case the lungs. Again, the normal lungs are black with white tubes (or pulmonary blood vessels) going throughout the lung. The CT image on the left shows a normal appearancing right lung; but on the left lung, you see a highly demarcated area of consolidation with a white opaque area typical of a bacterial pneumonia. In the CT image on the right, with the SARS-CoV-2 virus, you not only see abnormality on both the left and right lung with a ground-glass appearance that is partially translucent; but what you also notice is that it is more pronounced posteriorly. The inflammation and fluid that the SARS-CoV-2 virus is producing occurs on both sides, but gravity is pulling that fluid posteriorly. Unfortunately, gravity is also pulling the blood flow towards the back which results in poor matching of air and blood, and it is that matching which is needed in order for oxygen to get in and for carbon dioxide to get out. The posterior lung edema suggests a therapy known as “proning,” which is turning the patient on his or her abdomen, allowing for blood to flow forward where there is greater lung aeration allowing improved matching of ventilation and perfusion for better gas exchange.
Fig. 5.
Sequence of Cat scan images.
Taking critically ill patients to the CT Scanner is not only risky, but is also labor-intensive, costly, and requires potential decontamination of the CT scanner. On the other hand, Ultrasound can be conveniently done at the bedside. Fig. 6 shows a sequence of Ultrasound images starting with normal lungs on the left, left lung pneumonia in the middle and SARS-CoV-2 viral pneumonia on the right image (Macori, 2020). In Fig. 6, the ultrasound transducer is positioned at the top of each image and the sounds from the transducer fan out, sound bounces back and ‘reflected sounds’ are produced, which is then turned into an image by the machine. In the normal lung you have mostly air and it is this interaction of the sound with the air-filled normal lung that produces horizontal lines across the image, called ‘A-lines”. These A-lines are what allows you to recognize a more normal appearing lung. By contrast, in the middle lung image , the sound is coming down and interacts with this wet lung creating what is called a C-line. The C-line is a broad whiteness which corresponds to what was seen on both the CT scan and the chest X-ray as an isolated area of opacity, typical of bacterial pneumonia. In the SARS-CoV-2 virus, there is diffuse fluid throughout both lungs with alternating patterns of light and dark; which are called B-lines. B-lines are defined as hypoechoic subpleural focal images generated by condensed lung tissue, without visceral pleural line gap. You may find ultrasound being used to recognize COVID-19 by looking for B-lines (Wilkinson, 2020).
Fig. 6.
Sequence of ultrasound images.
4. The importance of understanding HOW the SARS-CoV-2 virus spreads
With over 7 million reported COVID-19 cases worldwide, some big outbreaks were to be expected. But SARS-CoV-2, like two of its cousins, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), seems especially prone to attacking groups of tightly connected people while sparing others.
It appears inevitable that severe acute respiratory syndrome coronavirus 2 will continue to spread. Although we still have limited information on the epidemiology of this virus, there have been multiple reports of superspreading events (SSEs), which are associated with both explosive growth early in an outbreak and sustained transmission in later stages. Superspreading events are ill-understood and difficult to study, and the findings can lead to heartbreak and fear of stigma in patients who initiate the spread (Frieden and Lee, 2020).
Scientists tracking the new coronavirus' spread have generally focused on two numbers. The first is called the reproductive number (R), which represents the average number of new infections caused by a single infected person. The second is called the dispersion factor (k), a number indicating the likelihood that a particular disease will spread in clusters.
Most of the discussion around the spread of SARS-CoV-2 has concentrated on the average number of new infections caused by each patient. The R0 (basic reproduction number) of SARS-CoV-2 has been estimated between 2.2 and 3.28 in a non-lockdown population (without social distancing), that is each infected individual, on average, causes between 2-3 new infections (Li et al., 2020; Liu et al., 2020c). But in real life, some people infect many others and others don't spread the disease at all. In fact, the consistent pattern is that the most common number is zero. Most people do not transmit. That's why in addition to R, scientists use the dispersion factor (k) to describe how much a disease clusters. The lower k is, the more transmission comes from a small number or group of people. In a seminal 2005 Nature paper, Lloyd-Smith et al. (2005), estimated that SARS—in which superspreading played a major role—had a k of 0.16. The estimated k for MERS, which emerged in 2012, is about 0.25. In the Spanish flu pandemic of 1918, in contrast, the value was about one, indicating that clusters played less of a role and superspreading was not much of a factor.
These numbers are important because it allows policymakers to target social distancing policies at the types of gatherings where superspreading is likely to occur. If you can predict what circumstances are giving rise to these events, mathematically, it becomes clear very quickly what guidelines are necessary to curtail the ability of the disease to spread. As we learn more about how the new coronavirus spreads, we are also learning why some people are more likely to be superspreaders than others—and the environments most likely to cause superspreading events.
During the 2003 SARS epidemic in Beijing, China, 1 hospitalized index patient was the source of 4 generations of transmission to 76 patients, visitors, and healthcare workers (Shen et al., 2004). During the MERS outbreak in South Korea, 166 (89%) of 186 confirmed primary cases did not further transmit the disease, but 5 patients led to 154 secondary cases (Chun, 2016). The index patient transmitted MERS to 28 other persons, and 3 of these secondary cases infected 84, 23, and 7 persons. During Ebola, SSEs played a key role sustaining the epidemic: 3% of cases were estimated to be responsible for 61% of infections (Lau et al., 2017).
Research to date suggests that the new coronavirus mostly transmits through droplets, though it has also been found to occasionally spread through aerosols that suspend in the air, which can allow one person to infect many more. A 2019 study of healthy people found that some people exhale more droplets than others when they talk, some of which was explained by their speaking volume (Asadi et al., 2019). In addition, a study out of Japan found people are nearly 19 times as likely to become infected with Covid-19 indoors when compared with outdoors (Nishiura et al., 2020).
These findings may explain a recent CDC case study in the US in which a single individual who attended choir practice on March 10, 2020 triggered an outbreak that sickened 53 of the 61 choir members who gathered for practice. According to CDC, three of those individuals were hospitalized and two died. The initial patient had been experiencing cold-like symptoms and was later diagnosed with Covid-19 (Hammer, 2020). The existing data and reports of clusters indicate that enclosed spaces where people are shouting, singing, or breathing heavy from exercise may be riskier than others. There have been reports of outbreaks at places where people typically shout or sing, like choir practices or Zumba classes, while places like Pilates classes have not been associated with outbreaks. Maybe slow, gentle breathing is not a risk factor, but heavy, deep, or rapid breathing and shouting is.
In addition, some people may simply be more likely to spread the new coronavirus than others because of differences in how their body reacts to the virus (Kupferschmidt, 2020).
5. Preventing the spread of COVID-19
More than 10,000 people, including children and those over 70, are set to be involved in the second phase of human trials for developing a vaccine. Researchers at the University of Oxford in the UK and AstraZeneca have begun recruitment for more than 10,000 subjects for advanced human studies of one of the world's fastest-moving experimental coronavirus vaccines. The US government Department of Health and Human Services announced a new investment of $1.2 billion dollars in the coronavirus vaccine, which is a gamble, but believe it is worth the risk. The money comes from the agency's Biomedical Advanced Research and Development Authority (BARDA). Of course, it is yet to be determined if this vaccine will work, but they have good confidence that it should actually be a successful vaccine (Cohen, 2020).
If it is successful, the vaccine supply will be ready by September or October 2020. The only way to meet this short timeframe is to manufacture the vaccine simultaneously while the research study is being conducted. What underpins their confidence is that this is a technology that has been validated for use as a class one vaccine. Work on the vaccine started very early back in January with a great amount of technical testing. The Oxford team launched a phase 1 clinical trial of the vaccine, which contains a harmless chimpanzee adenovirus “vector” carrying the gene for the SARS-CoV-2 surface protein, in 1100 people in the United Kingdom on April 23.
The phase 1 trial has allowed this group to start the phase 2 trial in June 2020, and all of this points to a vaccine that should work. It is possible that some patients will require a second dose, which often happens. This study has an aggressive timeline and should finish wrapping up by the end of August with a delivery of the first of at least 300 million doses arriving in October 2020 (Cohen, 2020).
This is being done without any profit during the pandemic. Three supply chain manufacturing laboratories have been identified to avoid competition; one for the US; one potentially in India and a possible third in China (Cohen, 2020).
The CDC estimates more than a third of coronavirus patients don't have any symptoms at all, and 40% of virus transmission happens before people feel sick. The figures are part of the agency's new guidance for mathematical modelers and public health officials and are not supposed to be predictions of how many people could have or contract Covid-19. The incubation period for COVID-19 was initially calculated to be about five days, which was based on 10 patients only (Li et al., 2020). An American group performed an epidemiological analysis of 181 cases, for which days of exposure and symptom onset could be estimated accurately. They calculated a median incubation period of 5.1 days, that 97.5% became symptomatic within 11.5 days (CI 8.2 to 15.6 days) of being infected, and that extending the cohort to the 99th percentile results in almost all cases developing symptoms in 14 days after exposure to SARS-CoV-2 (Lauer et al., 2020). The CDC has also released mortality figures and scenarios intended to help public health preparedness. Under the most severe of the five scenarios outlined, the CDC lists a symptomatic case fatality ratio of 0.01, meaning that 1% of people overall with Covid-19 and symptoms would die. But some experts say the figures lowball the proportion of people who are succumbing to the disease (CDC, 2020a, CDC, 2020b, CDC, 2020c, CDC, 2020d, CDC, 2020e).
6. COVID-19 in children
Liguoro et al. (2020), completed a systematic review of the main clinical characteristics and outcomes of SARS-CoV-2 infections in the pediatric population (Liguoro et al., 2020). In counts of cases, SARS-CoV-2 appears to affect children less commonly and less severely than adults, with an estimated very low mortality rate. However, there is growing evidence showing that children are as susceptible as adults to becoming infected when exposed. The discrepancy could be due to the fact that children are less frequently exposed to the main sources of transmission. Or it could be that children tend to show milder symptoms and therefore have been tested less frequently.
In a study by Dong et al. (2020b), Nationwide case series of 2135 pediatric patients with COVID-19 reported to the Chinese Center for Disease Control and Prevention from January 16, 2020, to February 8, 2020. Children of all ages appeared susceptible to COVID-19, and there was no significant sex difference. Although clinical manifestations of children's COVID-19 cases were generally less severe than those of adult patients, young children, particularly infants, were vulnerable to infection.
Children with COVID-19 infection may be asymptomatic or have fever, dry cough, and fatigue, with a few upper respiratory symptoms, including nasal congestion and runny nose; some patients have gastrointestinal symptoms, including abdominal discomfort, nausea, vomiting, abdominal pain, and diarrhea. Most infected children have mild clinical manifestations, and the prognosis is good. Most of the pediatric patients have recovered within 1 to 2 weeks after onset (Hong, 2020).
There have been reported cases of the syndrome among children who have tested positive for SARS-CoV-2 and who have displayed respiratory symptoms commonly linked with COVID-19. The condition also has been detected in children who have tested positive for SARS-CoV-2 or who have antibodies to the virus, suggesting they had been infected at some point, but who did not exhibit those respiratory symptoms. However, not every child with the syndrome has tested positive for SARS-CoV-2.
Multisystem inflammatory syndrome in children (MIS-C) is a new health condition associated with COVID-19 that is on the rise globally. The syndrome was previously called pediatric multisystem inflammatory syndrome or PMIS. The condition typically afflicts children, who develop it within days or weeks after they become infected with SARS-CoV-2 (WHO Scientific Brief, 2020).
Multi-System Inflammatory Syndrome causes inflammation of the blood vessels, impairs organ function, and can potentially cause damage to the heart. Other symptoms include fever, skin rashes, gland swelling, abdominal pain, vomiting, and diarrhea. So far, the cause of the condition is unknown, but some physicians believe it stems from the patient's immune system overacting to an infection. The volume of cases of the syndrome in Covid-19 patients implies the conditions are likely linked (WHO Scientific Brief, 2020).
Additionally, an unusual complication in some children with Covid-19 is the rare inflammatory condition called Kawasaki disease. Kawasaki disease, like MIS-C, causes inflammation in the arteries and can limit blood flow in the heart. It is usually treatable, and most children recover without serious problems, but it can be fatal. Cases of these diseases related to SARS-CoV-2 have been observed in the US, UK, Spain and Italy.
Shortly after the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to a region (Bergamo, Italy), a 30-fold increased incidence of Kawasaki disease was found. Children diagnosed after the SARS-CoV-2 epidemic began showing evidence of an immune response to the virus, were older, had a higher rate of cardiac involvement, and features of “macrophage activation syndrome” (MAS). This suggested that SARS-CoV-2 might cause a severe form of Kawasaki-like disease (Verdoni et al., 2020).
Providers now believe there are more than 100 children in New York who also developed the syndrome—including three who died. In addition, medical centers in 14 other states (USA) have reported similar cases. Researchers still say most children who contract the new coronavirus experience mild or asymptomatic of cases COVID-19. Nevertheless, they are concerned about the severity of MIS-C in the relatively few children who develop it, noting that the condition appears in children weeks after a wave of SARS-CoV-2 infection in the community. The presentation of COVID-19 in children is clearly different and the fact that it is happening two months after the initial circulation of the virus gives weight to the idea that it is an “immune-mediated phenomena”(Eunjung & Janes, 2020). Treatment with immunoglobulins, which is the suggested treatment for Kawasaki disease, has been successful in positive COVID-19 children with MIS-C.
7. COVID-19 in pregnant women and delivery
Pregnant women are a population susceptible to COVID-19 and are more likely to have complications and even progress to severe illness (Wang et al., 2020b). There are not enough data to determine the effect of COVID-19 infection on the fetus. Whether COVID-19 has mother-to-child vertical transmission, and its short-term and long-term harm to offspring, is still unclear.
Data on delivery in the setting of COVID-19 are sparse. In a recently published cohort of 64 severely and critically ill pregnant women with COVID-19 from 12 institutions, mean gestational age at onset was about 30 weeks. Half of women were delivered during their hospitalization for COVID-19 (Pierce-Williams et al., 2020), most commonly for maternal/obstetric indications. In the same series 34% of severely ill patients and 85% of critically ill patients were delivered, of which 88% were preterm. The average gestational age at delivery was 32.4 weeks—even for those who were critically ill. Median time between symptom onset and delivery was 10 days, consistent with known disease kinetics in COVID-19. Reassuringly, there were no reports of perinatal or maternal death in this cohort.
Unlike some causes of peripartum critical illness (e.g. preeclampsia), case reports suggest that delivery does not universally improve outcome or avoid complications in COVID-19 (Ferrazzi et al., 2020). Breslin and colleagues reported on two SARS-CoV-2 infected women who were asymptomatic when admitted for routine labor induction but ultimately became critically ill in the postpartum period (Breslin et al., 2020). One was intubated due to respiratory distress during cesarean delivery and another developed respiratory distress and severe hypertension more than a day after delivery. Schnettler and colleagues describe a case in which a 32 week delivery was indicated due to non-reassuring fetal status in an intubated patient; delivery was uncomplicated, but the patient remained intubated at the conclusion of the study, more than a week later (Schnettler et al., 2020). In a case series of 9 critically ill women from Iran, there were 7 fatalities. 5 of the 7 fatalities were among women who delivered 24 or more hours prior to decompensating (Hantoushzadeh et al., 2020). A recent case report describes a patient who presented with mild symptoms but subsequently died within 36 hours of admission, in spite of delivery of a healthy neonate in the interim (Vallejo and Ilagan, 2020).
Taken together, this evidence indicates that timing of delivery should be determined by maternal disease course and trajectory and maternal safety, as well as the usual obstetric indications. If there are obstetric indications for early delivery, delivery should not be delayed, and if preterm labor develops, attempts to delay delivery as would be standard in the absence of infection should be deferred. If infection of COVID-19 is not improved by ‘treatment’ (time, medications, other supportive measures), delivery may be considered even in the absence of obstetric indications. Though there is controversy surrounding the use of corticosteroids in COVID-19 patients, a short course of antenatal corticosteroids for fetal benefit may be considered if preterm delivery prior to 34 weeks is anticipated (SMFM, 2020).
Early reports from China described a very high rate of cesarean section among women with SARS-CoV-2 infection: 92% in a meta-analysis of SARS, MERS and SARS-CoV-2 infections, and 93% in a case series of 118 women (Di Mascio et al., 2020). However, these reports consisted largely of pregnant women presenting with pneumonia (92% and 79% respectively) and do not clearly define the indications for cesarean delivery. Consequently, there is uncertainty about whether these operative deliveries were performed due to fetal, maternal, or institutional indications. Additionally, these reports did not describe mode of delivery among women with mild to moderate disease.
Given the current practice of universal COVID-19 testing for all pregnant women admitted to labor and delivery at many centers around the country, we are recognizing that the large majority of pregnant women with COVID-19 are asymptomatic, pre-symptomatic, or mildly symptomatic (Sutton et al., 2020) and may therefore be expected to have uncomplicated deliveries. In a series of 43 pregnant test-confirmed COVID-19-positive women admitted for labor in two NY hospitals, 86% of women had mild disease (Breslin et al., 2020). In that series 18 of the 43 women delivered, including four symptomatic women and 14 asymptomatic women. In this cohort that is more representative of the US experience, 8 of 18 women (44.4%) were delivered via cesarean section. The indications were distributed between non-reassuring fetal heart rate, arrest of progress in labor, and prior cesarean section. Maternal COVID-19 status was not reported to drive decisions about cesarean delivery. For 10 of 18 women (55.5%) there were uncomplicated normal vaginal deliveries. These data, both more contemporary and generalizable, suggest that vaginal delivery is a viable option for the majority of women. Therefore, no clear COVID-19 specific indication for cesarean delivery exists and decisions on delivery mode should be made based on standard obstetrical indications (Breslin et al., 2020).
7.1. Delivery and potential for transmission
To date, there is no molecular evidence for definitive vertical transmission across the placenta (Liu et al., 2020b). Rigorous attempts to answer this question, however, have yet to be performed. There are several case series and reports of newborns testing positive prior to discharge, but it is unclear if vertical, perinatal, or postnatal transmission occurs in these cases. One study showed that virus can be detected in both the blood and stool of infected women, which infants are often exposed to during the delivery process (Chen et al., 2020a). Another case report identified SARS-CoV-2 virus in the placenta (Baud et al., 2020).
7.2. Separation of mothers and infants
Currently the AAP and CDC recognize that separation of mothers and newborns is the primary way to ensure the infant is protected from infection. However, as mentioned above, case reports exist of infants acquiring the virus despite full separation. Separation is theoretically most important in cases where the mother is experiencing significant symptoms. To date, there is no available data regarding molecular testing on neonates who were not separated from their asymptomatic, SARS-CoV-2-positive mothers.
If a SARS-COV-2 negative, non-exposed adult is not available to care for the baby full time upon discharge, infant separation from the mother while inpatient is discouraged for the following reasons (Korraa, 2020):
-
•
Molecular testing often remains positive for several weeks, making timing of re-unification difficult to determine in the absence of symptoms.
-
•
If the plan is for the newborn to be discharged with the mother, exposure will exist regardless, and she will need instruction in how to provide newborn care while using protective measures (mask wearing/hand hygiene).
-
•
There are a number of practical and logistical challenges in discharging a newborn to a mother who has never cared for her infant.
-
•
Breastfeeding, if the chosen method of feeding, will be exceedingly difficult to establish if a SARS-CoV-2 positive mother is separated from her newborn.
The AAP/CDC provide guidelines on alternative methods of “separation” including distancing within one's room, physical barriers such as drapes and incubators, and mask wearing. Any infant requiring more than level 1 (routine newborn) care is admitted to a single patient room (preferably negative pressure if receiving aerosol generating procedures) on enhanced respiratory precautions until cleared through molecular testing. There is some conflict amongst US and international medical societies regarding the recommendations of location of mother and infant in the immediate post-delivery period (WHO FAQ, 2020; Puopolo (AAP), 2020; ACOG PA, 2020; CDC, 2020a, CDC, 2020b, CDC, 2020c, CDC, 2020d, CDC, 2020e, CPS, 2020). However, if maternal status allows it, it is reasonable to practice what will be done at home to help prepare for the safest practices after discharge.
Data surrounding the care of SARS-CoV-2 infected pregnant women and their newborns are sparse. As such, care for these vulnerable patients is predominantly guided by society recommendations and expert opinion. Currently, there is no clear data to suggest that providers should modify their recommendations for timing or mode of delivery based on the presence of SARS-CoV-2 infection. We await thorough serological analysis of mothers and neonates using validated IgG and IgM antibody tests to clarify the possibility of true vertical transmission of SARS-CoV-2. Decisions regarding separation of the mother-baby dyad, feeding approaches and discharge planning for SARS-CoV-2 positive mothers and their infants must involve a personalized, and shared-decision making approach.
The American Academy of Pediatrics currently recommends routine testing of infants born to SARS-CoV-2 positive mothers at 24hrs and then 48hrs of life, if still inpatient (Puopolo, 2020).
8. COVID-19 in newborns
Neonatal SARS-CoV-2 infections are extremely rare, and to date, there is no evidence of intrauterine infection caused by vertical transmission (Chen et al., 2020b; Baud et al., 2020). As described in a case report and a case series, amniotic fluid, cord blood, neonatal throat swab, and colostrum samples collected from infected mothers were negative for COVID-19 (Elshafeey et al., 2020; Wu, Y. et al., 2020). However, the question remains controversial, as IgM antibodies have been detected in newborns from mothers with COVID-19 (Zeng et al., 2020), even though the probability of a false positivity should be taken in account. There is also growing evidence of cases of neonatal pneumonia which may be explained by SARS-CoV-2 infection (NHC, 2020; Wang et al., 2020a; Zeng et al., 2020).
Perinatal 2019-nCoV infection may have adverse effects on newborns, causing problems such as fetal distress, premature labor, respiratory distress, thrombocytopenia accompanied by abnormal liver function, and even death (Zhu et al., 2020a).
Mortality rates for neonates specific for COVID-19 are minimal, although children aged <1 year accounted for the highest percentage (15%–62%) of hospitalization among pediatric patients with COVID-19. Among 95 children aged <1 year with known hospitalization status, 59 (62%) were hospitalized, including five who were admitted to an ICU (Lucy et al., 2020).
The pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has exposed vulnerable populations to an unprecedented global health crisis. The knowledge gained from previous human coronavirus outbreaks suggests that pregnant women and their fetuses are particularly susceptible to poor outcomes. The objective of this study was to summarize the clinical manifestations and maternal and perinatal outcomes of COVID-19 during pregnancy. Although the majority of mothers were discharged without any major complications, severe maternal morbidity as a result of COVID-19 and perinatal deaths were reported. Vertical transmission of the COVID-19 could not be ruled out. Careful monitoring of pregnancies with COVID-19 and measures to prevent neonatal infection are warranted (Zaigham and Andersson, 2020).
Currently in China, all newborns are separated from their infected mothers for at least 14 days (Adoha, 2020) while the US, the CDC advise to consider a temporary separation between the infected mother and her infant on a case-by-case basis, using shared decision-making between the patient and the clinical team (CDC, 2020e, CDC, 2020d, CDC, 2020c, CDC, 2020b, CDC, 2020a).
8.1. Shared decision-making position statement (NPA/NANN, USA)
The National Perinatal Association (NPA) and National Association of Neonatal Nurses (NANN) offer guidance in creating a culture of shared decision-making when providers must deliver the newborn of a COVID-19+ mother or when the mother's SARS-CoV-2 test is still pending (NANN, 2020; NPA, 2020).
A Joint Position Statement created by the NPA and NANN addresses the need to balance evidence-based practices for both infection control and protection of healthcare providers with the established benefit of newborn bonding and breastfeeding in the 4th trimester.
-
•
NANN and NPA encourage the ideal scenario, which is to keep mother and newborn together while respecting the unique challenges individual institutions may encounter.
-
•
While we recognize the myriad uncertainties in understanding the best evidence-based practice for the mother-newborn dyad during the postpartum period, we encourage families and clinicians to remain diligent in learning up-to-date evidence and ultimately working in partnership for the safest and best practice for all parties involved.
-
•
NANN and NPA acknowledge the potential trauma and exacerbation of postpartum mental health issues that may negatively impact the fourth trimester.
-
•
We encourage healthcare providers to assist the mother to recognize the ideal versus realistic scenarios, acknowledge the uncertainty and grief over changing expectations, and consider higher-touch care in the weeks following delivery.
NANN and NPA have reviewed the recommendations from the American Academy of Pediatrics (AAP) (Puopolo et al., 2020), Centers for Disease Control and Prevention (CDC, 2020a, CDC, 2020b, CDC, 2020c, CDC, 2020d, CDC, 2020e) (US DHHS-CDC), and the World Health Organization (WHO) (WHO, 2020) regarding mother-newborn infant postpartum care in the hospital if a mother is COVID-19+. All statements support and emphasize the importance of a shared-decision model between mother and the healthcare provider team to determine the need for postpartum separation of the mother-newborn dyad while they are in the hospital.
With information changing rapidly as more data is collected, they acknowledge the potential for policy changes based on institutional constraints and regional developments. However, any policy must start with the dignity of the patient at its core and aspire to do no harm as we all navigate these challenging and uncertain times.
As the COVID-19 pandemic continues to shape all our lives, those who provide care to pregnant patients, their families, and newborns face many challenges. As healthcare professionals, we are responsible for developing new policies and procedures related to childbirth and the care of newborns in an ever-changing environment.
We must create and maintain a safe environment for patients and first line healthcare workers, while at the same time, maintain the highest standards of ethical and compassionate care at such a potentially vulnerable time for both parents and newborns.
Contributor Information
Leslie Altimier, Email: laltimier@gmail.com.
Adam Seiver, Email: adam.seiver@philips.com.
References
- Adoha G. Some mothers allowed just 15 minutes with their premature babies due to coronavirus restrictions. The journal.ie Read, Share and Shape the News. 2020 https://www.thejournal.ie/mothers-nicu-covid-19-restrictions-5070051 April. 9. [Google Scholar]
- ACOG Practice Advisory, Riley L.E., Beigi R., Jamieson D.J., Hughes B., American College of Obstetricians and Gynecologists (ACOG) Practice Advisory. Wolters Kluwer Health/Lippincott Williams & Wilkins; The Netherlands: 2020. American College of Obstetricians and Gynecologists (ACOG) Practice Advisory: Novel Coronavirus 2019 (COVID19). American College of Obstetricians And Gynecologists’ Immunization, Infectious Disease, and Public Health Preparedness Expert Work Group.https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus-2019 [Google Scholar]
- Asadi S., Wexler A.S., Cappa C.D., Barreda S., Bouvier N.M., Ristenpart W.D. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 2019;9:2348. doi: 10.1038/s41598-019-38808-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashour H.M., Elkhatib W.F., Rahman M.M., Elshabrawy H.A. Insights into the recent 2019 novel Coronavirus (SARS-CoV-2) in light of past human Coronavirus outbreaks. Pathogens. 2020;9(3):196. doi: 10.3390/pathogens9030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baud D., Greub G., Favre G., Gengler C., Jaton K., Dubruc E., Pomar L. Second-trimester miscarriage in a pregnant woman with SARS-CoV-2 infection [published online ahead of print, 2020 apr 30] J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.7233. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslin N., Baptiste C., Gyamfi-Bannerman C., Miller R., Martinez R., Bernstein K., Ring L., Landau R., Purisch S., Friedman A.M., Goffman D. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am. J. Obstetrics Gynecol. MFM. 2020 May;2(2) doi: 10.1016/j.ajogmf.2020.100118. Supplement; 1–7 Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Paediatric Society (Cps) NICU care for infants born to mothers with suspected or proven COVID-19. 2020. https://www.cps.ca/en/documents/position/nicu-care-for-infants-born-to-mothers-with-suspected-or-proven-covid-19
- Center for Disease Control and Prevention (Cdc) Coronavirus disease 2019 (COVID-19) – inpatient obstetrics. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcareguidance.html
- Center for Disease Control and Prevention (Cdc): Coronavirus 2019 (Covid) Pregnancy and breastfeeding. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancybreastfeeding.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Fpregnant-women-faq.html
- Center for Disease Control and Prevention (Cdc) Coronavirus 2019 (COVID); cases in the US. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- Centers for Disease Control and Prevention (Cdc): U.S. Department of Health and Human Services Considerations for inpatient obstetric healthcare settings. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcare-guidance.html April 4, Retrieved from.
- Centers for Disease Control and Prevention (Cdc) MMWR: coronavirus disease 2019 in children — United States. MMWR Morbid. Mortal. Week. Rep. 2020;69:422–426. doi: 10.15585/mmwr.mm6914e4. February 12–April 2. [DOI] [Google Scholar]
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li J., Zhao D., Xu D., Gong Q., Liao J., Yang H., Hou W., Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Peng H., Wang L., Zhao Y., Zeng L., Gao H., Liu Y. Infants born to mothers with a new coronavirus (COVID19) 2020. Frontiers in Pediatrics; 16 March 2020. [DOI] [PMC free article] [PubMed]
- Chun B.C. Understanding and modeling the super-spreading events of the Middle East respiratory syndrome outbreak in Korea. Infectious Chemother. 2016;48:147–149. doi: 10.3947/ic.2016.48.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Health scientific community: coronavirus. 2020. https://www.sciencemag.org/category/scientific-community Sciencemag.org. [DOI]
- de Groot R.J., Baker S.C., Baric R.S., Brown C.S., Drosten C. Middle East respiratory syndrome Coronavirus (MERS-CoV): announcement of the Coronavirus study group. J. Virol. 2013;87:7790–7792. doi: 10.1128/JVI.01244-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Mascio D., Khalil A., Saccone G., Rizzo G., Buca D., Liberati M., Vecchiet J., Nappi L., Scambia G., Berghella V., D’Antonio F. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. Am. J. Obstetrics Gynecol. MFM. 2020 May;2(2) doi: 10.1016/j.ajogmf.2020.100107. Supplement; 1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. 2020. An interactive web-based dashboard to track COVID-19 in real time.www.thelancet.com/infection (20) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., Tong S. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020;145(6) doi: 10.1542/peds.2020-0702. [DOI] [Google Scholar]
- Drosten C., Günther S., Preiser W., van der Werf S., Brodt H.R. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- Elshafeey F., Magdi R., Hindi N., Elshebiny M., Farrag N., Mahdy S., Sabbour M., Gebril S., Nasser M., Kamel M. A systematic scoping review of COVID-19 during pregnancy and childbirth [published online ahead of print, 2020 Apr 24] Int. J. Gynaecol. Obstet. 2020 April:1–6. doi: 10.1002/ijgo.13182. Wileyonlinelibrary.com/journal/ijgo. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eunjung C., Janes C. The girl who died twice. 2020. https://www.washingtonpost.com/health/2020/05/17/child-coronavirus-kawasaki-inflammation/?arc404=true The Washington Post.
- Ferrazzi E., Frigerio L., Savasi V., Vergani P., Prefumo F., Barresi S., Bianchi S., Ciriello E., Facchinetti F., Gervasi M., Teresa M., Lurlaro E., Kusterman A., Mangili G., Mosca F., Patanè L., Spazzini D., Spinillo A., Trojano G., Vignali M., Villa A., Zuccotti G., Parazzini F., Cetin I. Mode of delivery and clinical findings in COVID-19 infected pregnant women in northern Italy (3/24/2020) 2020. [DOI] [PMC free article] [PubMed]
- Frieden T.R., Lee C.T. Identifying and interrupting superspreading events—implications for control of severe acute respiratory syndrome coronavirus 2. Emerg. Infect. Dis. 2020;26(6):1059–1066. doi: 10.3201/eid2606.200495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbalenya A.E., Baker S.C., Baric R.S. Coronaviridae study group of the international committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubatan J., Wang X., Louissant A., Mahindra A., Vanderpool J. Biomarker Research. 2016 December 01. https://biomarkers.biomedcentral.com/articles/10/1186/s40364-016-0072-5/figures/2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner L., Dubbel P., Capron I., Ross A., Jordan A., Lee J., Lynn J., Ball A., Narwal S., Russell S., Patrick D., Liebrand H. High SARS-CoV-2 attack rate following exposure at a choir practice — skagit county, Washington, March 2020. MMWR Morbid. Mortal. Week. Rep. 2020;69:606–610. doi: 10.15585/mmwr.mm6919e6. May 15. [DOI] [PubMed] [Google Scholar]
- Hansell D.M., Bankier A.A., MacMahon H., McLoud T.C., Müller N.L., Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- Hantoushzadeh S., Shamshirsaz A.A., Aleyasin A., Seferovic M.D., Aski S.K., Arian S.E., Pooransari P., Ghotbizadeh F., Aalipour S., Soleimani Z., Naemi M., Molaei B., Ahangari R., Salehi M., Oskoei A.D., Pirozan P., Darkhaneh R.F., Laki M.G., Farani A.K., Atrak S., Miri M.M., Kouchek M., Shojaei S., Hadavand F., Keikha F., Hosseini M.S., Borna S., Ariana S., Shariat M., Fatemi A., Nouri B., Nekooghadam S.M., Aagaard K. Maternal death due to COVID-19 disease. Am. J. Obstet. Gynecol. 2020:1.e1–1.e16. doi: 10.1016/j.ajog.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong H., Wang Y., Chung H.T., Chen C.J. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr. Neonatol. 2020;61(2):131–132. doi: 10.1016/j.pedneo.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John Hopkins University . 2020. COVID-19 dashboard by the center for systems science and engineering (CSSE) at John Hopkins university (JHU)https://coronavirus.jhu.edu/map.html [Google Scholar]
- Korraa A. Management of neonates born to mothers with COVID-19. Ann. Neonatol. J. 2020;2(2):e1–e14. doi: 10.21608/anj.2020.27830.1009. ISSN: 2636-3596, Article in Press. [DOI] [Google Scholar]
- Kupferschmidt K. Why do some COVID-19 patients infect many others, whereas most don't spread the virus at all? American Association for the Advancement of Science. ScienceMag.org. 2020 doi: 10.1126/science.abc8931. https://www.sciencemag.org/news/2020/05/why-do-some-covid-19-patients-infect-many-others-whereas-most-don-t-spread-virus-all [DOI] [Google Scholar]
- Lau M.S., Dalziel B.D., Funk S., McClelland A., Tiffany A., Riley S. Spatial and temporal dynamics of superspreading events in the 2014-2015 West Africa Ebola epidemic. Proc. Natl. Acad. Sci. U. S. A. 2017;(9):2337–2342. doi: 10.1073/pnas.1614595114. Feb 28; 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguoro I., Pilotto C., Bonanni M., Elena Ferrari M.E., Pusiol A., Nocerino A., Vidal E., Cogo P. SARS-COV-2 infection in children and newborns: a systematic review. Eur. J. Pediatr. 2020 May:e1–e18. doi: 10.1007/s00431-020-03684-7. https://link.springer.com/content/pdf/10.1007/s00431-020-03684-7.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R., Azman A.S., Reich N.G., Lessler J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel Coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Zhang Q., Chen J. Detection of covid-19 in children in early january 2020 in wuhan, China. N. Engl. J. Med. 2020;382:1370–1371. doi: 10.1056/NEJMc2003717. Massachusetts Medical Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Wang Q., Zhang Q., Chen L., Chen J., Zhang B., Lu Y., Wang S., Xia L., Huang L., Wang K., Liang L., Zhang Y., Turtle L., Lissauer D., Lan K., Feng L., Yu H., Liu Y., Sun Z. Coronavirus disease 2019 (COVID-19) during pregnancy: a case series. Preprints. 2020;2020 https://www.preprints.org/manuscript/202002.0373/v1 2020020373; e1–e19. [Google Scholar]
- Liu Y., Gayle A.A., Wilder-Smith A., Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Trav. Med. 2020 March;27(2):1–4. doi: 10.1093/jtm/taaa021. taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Li L., Wu X., Zheng D., Wang J., Yang L., Zheng C. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. Am. J. Roentgenol. 2020 doi: 10.2214/AJR.20.23072. 0 0:0; 1–6. [DOI] [PubMed] [Google Scholar]
- Lloyd-Smith J., Schreiber S., Kopp P., Getz W.M. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X., Zhang L., Du H. SARS-CoV-2 infection in children. N. Engl. J. Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucy A., McNamara L.A. Coronavirus disease 2019 in children — United States, february 12–april 2, 2020. MMWR Morbid. Mortal. Week. Rep. 2020;69:422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macori F. Right Image Courtesy of Dr. Fabio Macori. 2020 March 06. https://radiopaedia.org/cases/covid-19-pneumonia-12?lang=us Radiopaedia.org, rID:74867. [Google Scholar]
- National Association of Neonatal Nurses (Nann), National Perinatal Association (Npa) Mothers with COVID-19 and their newborn infants: Joint position statement. 2020. http://nann.org/uploads/About/PositionPDFS/Position%20Statement%20COVID-19_NPA%20and%20NANN.pdfhttp://www.nationalperinatal.org/resources/Documents/COVID-19/COVID-19_NPA%20and%20NANN.pdf
- Nhc: National Health Commission of the Republic of China New coronavirus pneumonia prevention and control program. 2020. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf (seventh ed.). Accessed May 24, 2020.
- Nishiura H., Oshitani H., Kobayashi T., Saito T., Sunagawa T., Matsui T., Wakita T., Suzuki M. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19) medRxiv. 2020 doi: 10.1101/2020.02.28.2002927. [DOI] [Google Scholar]
- Pierce-Williams R.A.M., Burd J., Felder L., Khoury R., Bernstein P.S., Avila K., Penfield C.A., Roman A.S., DeBolt C.A., Stone J.L., Bianco A., Kern-Goldberger A.R., Hirshberg A., Srinivas S.K., Jayakumaran J.S., Brandt J.S., Anastasio H., Birsner M., O’Brien D.S., Sedev H.M., Dolin C.D., Schnettler W.D., Suhag A., Ahluwalia S., Navathe R.S., Khalifeh A., Anderson K., Berghella V. Clinical course of severe and critical COVID-19 in hospitalized pregnancies: a US cohort study. Am. J. Obstet. Gynecol. 2020 doi: 10.1016/j.ajogmf.2020.100134. MFM 100134, In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puopolo K.M., Hudak M.L., Kimberlin D.W., Cummings J. 2020. Initial Guidance: Management of Infants Born to Mothers with COVID-19. American Academy of Pediatrics Committee on Fetus And Newborn, Section on Neonatal Perinatal Medicine, and Committee on Infectious Diseases.https://downloads.aap.org/AAP/PDF/COVID%2019%20Initial%20Newborn%20Guidance.pdf [Google Scholar]
- Schnettler W.T., Al Ahwel Y., Suhag A. Severe ARDS in COVID-19-infected pregnancy: obstetric and intensive care considerations. [published online ahead of print, 2020 Apr 14] Am. J. Obstet. Gynecol. 2020 April doi: 10.1016/j.ajogmf.2020.100120. MFM 100120, In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Z., Ning F., Zhou W., He X., Lin C., Chin D.P., Zhu Z., Schuchat A. Superspreading SARS events, beijing, 2003. Emerg. Infect. Dis. 2004;10(2):256–260. doi: 10.3201/eid1002.030732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SMFM Society of Maternal Fetal Medicine Management considerations for pregnant patients with COVID-19. 2020. https://s3.amazonaws.com/cdn.smfm.org/media/2336/SMFM_COVID_Management_of_COVID_pos_preg_patients_4-30-20_final.pdf April 30.
- Sutton D., Fuchs K., D’Alton M., Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N. Engl. J. Med. 2020 May;382:2163–2164. doi: 10.1056/NEJMc2009316. [published online ahead of print, 2020 Apr 13]. NEJMc2009316. DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Centers for Disease Control and Prevention Considerations for inpatient obstetric healthcare settings. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/inpatient-obstetric-healthcare-guidance.html April 4.
- Vallejo V., Ilagan J.G. A postpartum death due to coronavirus disease 2019 (COVID-19) in the United States. [published online ahead of print, 2020 may 8] Obstet. Gynecol. 2020 doi: 10.1097/AOG.0000000000003950. 10.1097/AOG.0000000000003950. [DOI] [PubMed] [Google Scholar]
- Verdoni L., Mazza A., Gervasoni A., Martelli L., Ruggeri M., Ciuffreda M., Bonanomi E., D’Antiga L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020 June;395:1771–1778. doi: 10.1016/S0140-6736(20)31103-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Shi Y., Xiao T. Working Committee on Perinatal and Neonatal Management for the Prevention and Control of the 2019 Novel Coronavirus Infection. Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection (first edition) Ann. Transl. Med. 2020;8(3):47. doi: 10.21037/atm.2020.02.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Guo L., Chen L., Liu W., Cao Y., Zhang J., Feng L. A case report of neonatal COVID-19 infection in China. Clin. Infect. Dis.: Off. Pub Infect. Dis. Soc. Am. 2020 doi: 10.1093/cid/ciaa225. Brief Report: CID 2020:XX (XX XXXX); 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson CriticalCareNorthHampton. 2020. https://criticalcarenorthampton.com/thoracic-other-images/ (accessed June 18, 2020)
- World Health Organization (WHO) WHO statement regarding cluster of pneumonia cases in Wuhan, China. 2020. https://www.who.int/china/news/detail/09-01-2020-who-statement-regardingcluster-of-pneumonia-cases-in-wuhan-china Jan 9. (accessed May 11, 2020)
- World Health Organization (WHO) Scientific Brief Multisystem inflammatory syndrome in children and adolescents with COVID-19. 2020. WHO/2019-nCoV/Sci_Brief/Multisystem_Syndrome_Children/2020.1https://www.who.int/publications-detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19
- World Health Organization (WHO) FAQ What matters to women in the postnatal period? 2020. https://www.who.int/news-room/detail/22-04-2020-what-matters-to-women-in-the-postnatal-period April 22, Retrieved from.
- World Health Organization (WHO) Director Speech . March 2020. Director-General’s Opening Remarks at the Media Briefing on COVID-19. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV)https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020;323:1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Wu Y., Liu C., Dong L., Zhang C., Chen Y., Liu J., Zhang C., Duan C., Zhang H., Mol B.W., Dennis C.L., Yin T., Yang J., Huang H. Coronavirus disease 2019 among pregnant Chinese women: case series data on the safety of vaginal birth and breastfeeding. BJOG An Int. J. Obstet. Gynaecol. 2020 doi: 10.1111/1471-0528.16276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Yu C., Qu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imag. 2020;47(5):1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaigham M., Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020 doi: 10.1111/aogs.13867. 00:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng L., Xia S., Yuan W., Yan K., Xiao F., Shao J., Zhou W. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.0878. Published online March 26, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H., Wang L., Fang C., Peng S., Zhang L., Chang G., Xia S., Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020;9(1):51–60. doi: 10.21037/tp.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B. China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]