Abstract
Background: Radiation therapy for head-and-neck cancer can cause side-effects, including pain, nausea, vomiting, sensory disorders such as anosmia and dysgeusia, dysphagia, xerostomia, hot flashes, fatigue, sleep disorders, and even anxiety and depression disorders. Therapies using acupuncture are now being adopted at cancer therapy centers. Acupuncture has been clinically proven to reduce the side-effects of cancer therapies, thus, resulting in better quality of life.
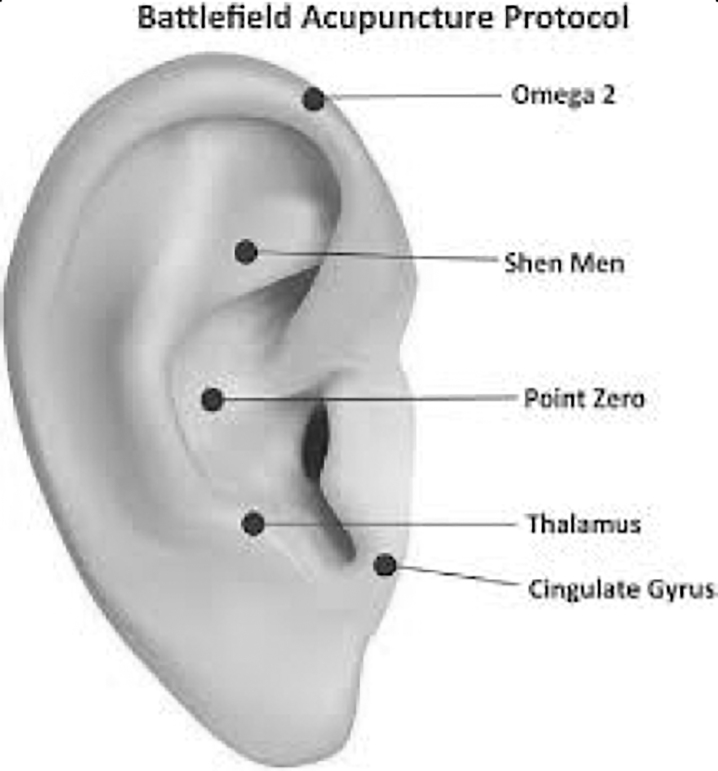
Case: A 65-year-old man was diagnosed with stage I laryngeal squamous-cell carcinoma (SCC), and had missing taste and pain on swallowing (visual analogue scale [VAS]: 4) after undergoing 30 sessions of radiation therapy for head-and-neck cancer with a total radiation dose of 60 Gy. He received acupuncture at: body points (LI 4 Hegu, LR 3 Taichong, ST 36 Zusanli, SP 6 Sanyinjiao, and ST 40 Fenglong); the Battlefield Acupuncture points of the ear (Cingulate Gyrus, Thalamus, Zero Point, Shen Men, and Omega 2); and on the wrist area (according to a balance method). Acupuncture therapy was given 2 times a week, for 45-minute sessions.
Results: After 12 acupuncture sessions, he had improvement in taste function and pain reduction from VAS 4 to VAS 1. This improvement likely occurred due to acupuncture's anti-inflammatory effects through anti-inflammatory mediator secretion, an antipain effect through ß-endorphin secretion, and nerve-cell regeneration through neurotropic factors' secretion.
Conclusions: Routine acupuncture therapy can reduce dysgeusia and pain in postradiated patients with head-and-neck cancer. Acupuncture can be a therapeutic choice for patients with post-radiation head-and-neck cancer toxicity.
Keywords: acupuncture, dysgeusia, radiation therapy, head-and-neck cancer
Introduction
Worldwide, more than 500,000 new cases of head-and-neck squamous cell carcinoma (SCC) are reported annually, with 40,000 new cases and 7890 deaths reported in the United States each year. Head-and-neck SCC can arise from various tissue sites in the oral cavity, oropharynx, hypopharynx, larynx, and nasopharynx. It is well-known that continued exposure to products, such as tobacco and alcohol, increases the risk of head-and-neck SCC. Over the past decade, there has been a shift in the distribution of primary SCC sites, where there has been an increase in the incidence of oropharyngeal SCC and a decrease in laryngeal and hypopharyngeal SCC. This change is said to be associated with a reduction in smoking risk factors and oncogenic human papillomavirus (HPV) exposure.1 The larynx is the second most common site for SCC in the head-and-neck region, and malignant laryngeal tumors comprise 1%–2% of all malignant tumor events all over the world.2
Clinical presentation in a patient with head-and-neck SCC varies depending on the site where the tumor started. At initial presentation, in ∼40% of patients there is regional lymph-node involvement and 10% of patients have metastasis. Prognosis depends on the tumor site, tumor tissue HPV status, and tumor staging. The diagnosis of head-and-neck SCC is based on several tests, namely: (1) HPV examination; (2) examination of molecular phenotypes of SCC and genome sequences; and (3) investigations such as nasopharyngo–laryngoscopy, computed tomography and magnetic resonance imaging (MRI). Management of SCC can involve surgery, radiation, or chemotherapy, or a combination of these, depending on the tumor staging and the primary site of the tumor. In early stage disease, SCC is usually treated with surgery or radiation therapy alone.1 Radiation therapy can cure patients with head-and-neck cancer but there are acute and chronic toxicities; thus, supportive therapy is often needed.3
Radiation therapy in patients with head-and-neck cancer can cause various changes in soft tissue, and also transient—and even permanent—sensory disturbances. The acute effects of radiation therapy on the head-and-neck region include mucositis, mucosal hypersecretion, mucosal infections, and pain and sensory disturbances in taste and smell. The long-term effects include tissue fibrosis, salivary-gland dysfunction, mucosal infections, neuropathic pain, sensory disorders, and oral mucosal diseases.4 Sensory disturbances in the sense of taste (dysgeusia) and sense of smell (anosmia) are quite common disorders in patients undergoing radiation therapy for head-and-neck cancer.
Dysgeusia affects 46%–77% of patients with cancer, including ∼53% of patients treated with chemotherapy agents, 66% of patients treated with radiation therapy, and 76% of patients treated with both modalities. Dysgeusia is considered as one of the most-worrying and disturbing side-effects due to chemotherapy, besides nausea, vomiting, fatigue, and hair loss. This dysgeusia can cause stress in patients and have a big impact on their quality of life because dysgeusia is associated with fatigue and loss of appetite. Thus, there can be a reduction in food intake, and nutritional deficits could develop. These factors can, in turn, affect tissue healing, energy levels, and moods in the patient.5 Management of dysgeusia includes dietary counseling with guidance on food selection, preparation and seasoning, zinc-sulfate supplementation, and medications such as clonazepam, gabapentin, cannabinoid, and megestrol.4
Acupuncture is one of the nonpharmacologic therapeutic modalities, using fine needles at acupuncture points. Acupuncture at the acupoints can activate nerve fibers and peripheral afferent receptors, produce sensory interactions at various levels of the central nervous system (CNS), and release various transmitters, thus producing anti-inflammatory, neuroendocrine, and neuroimmune signals.6 Acupuncture has been clinically proven to reduce the side-effects of cancer therapy, including such effects as pain, nausea, vomiting, dysphagia, xerostomia, hot flashes, fatigue, anxiety and depression disorders, and sleep disorders.7,8 However, the results of studies on the effects of acupuncture in cancer therapy still vary. This can be caused by the variety of acupuncture methods used and the selection of points for acupuncture therapy. There are several acupuncture methods that are currently often used, including the balancing method and Battlefield Acupuncture (BFA).
This case report concerns a patient with head-and-neck cancer, stage I laryngeal SCC, who was missing taste after radiation therapy. Acupuncture was expected to play a role in correcting such abnormalities that occur due to side-effects of cancer therapy.
Case
A 65-year-old male patient, with complaints of missing taste after undergoing radiation therapy for laryngeal SCC at stage I. This patient initially presented in January 2019 with a chief complaint of hoarseness. The hoarseness had first begun ∼1 year earlier, but became progressively worse over the 5 months prior to presentation. He had a history of smoking 1 pack of cigarettes for the past 10 years and also reported a weight loss of 3 kg over the past 6 months, without a decrease in appetite. On examination, a mass was found on the left vocal cord. After a tumor-mass biopsy and histopathologic examination, this patient was diagnosed with laryngeal SCC stage I. He underwent partial laryngectomy and radiation therapy for head-and-neck cancer. The radiation therapy was carried out for 30 sessions with a total dose of 60 Gy.
Following the completion of radiation therapy, this patient presented with complaints of pain in his neck and especially when swallowing drinks or food; this pain was worsening (visual analogue scale [VAS] 4 at presentation) and complaints of loss of taste so that his appetite became greatly reduced. A physical examination revealed swelling of the anterior neck, with a midline tracheostomy. A neck computed tomography scan showed emphysema of the right side of the supraclavicular region, without any tumors or residual disease.
This patient received acupuncture at the body points of LI 4 Hegu (Fig. 1), LR 3 Taichong (Fig. 2), ST 36 Zusanli (Fig. 3), SP 6 Sanyinjiao (Fig 4), and ST 40 Fenglong (Fig. 5); at the BFA points of the right ear (Cingulate Gyrus, Thalamus, Zero Point, Shen Men, and Omega 2; Fig. 6); and on the wrist area according to a balance method. The acupuncture body points were punctured until the patient felt a De Qi sensation. Stainless steel needles were used (Huanqiu, 0.14 × 13mm for BFA points; Huanqiu, 0.25 × 25 mm for body points), and the needles were retained for 45 minutes. Acupuncture therapy was performed 2 times per week, for 45 minutes each time.
FIG. 1.
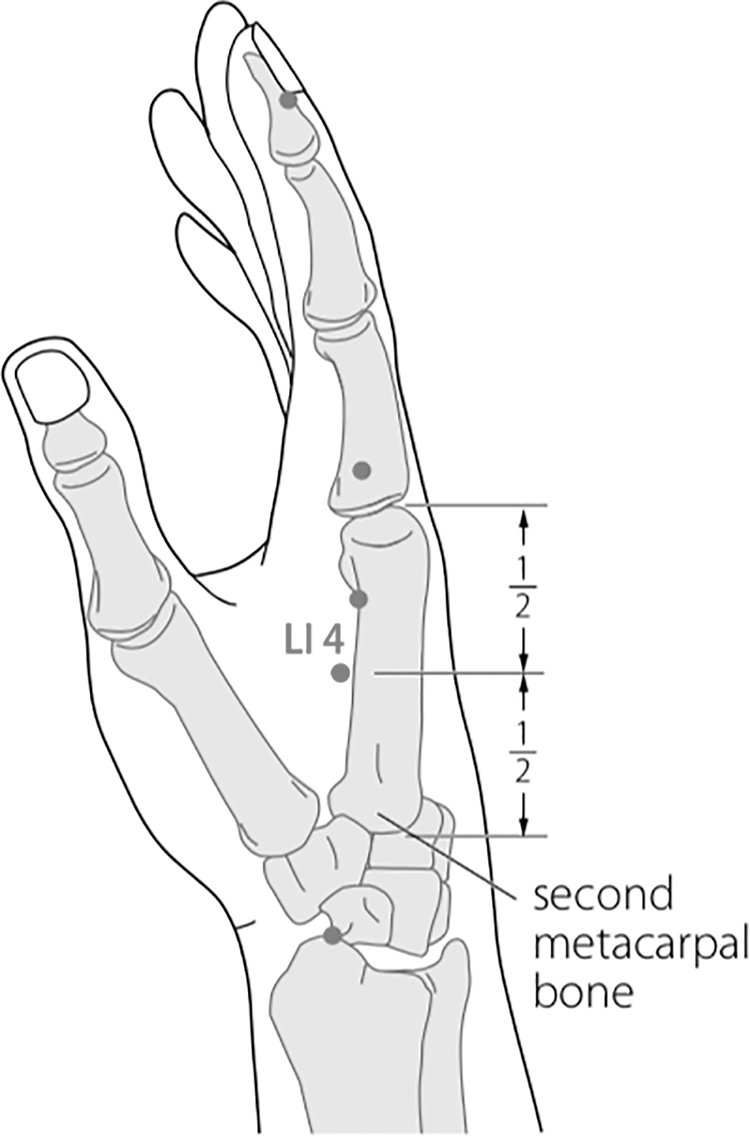
LI 4 Hegu.
FIG. 2.
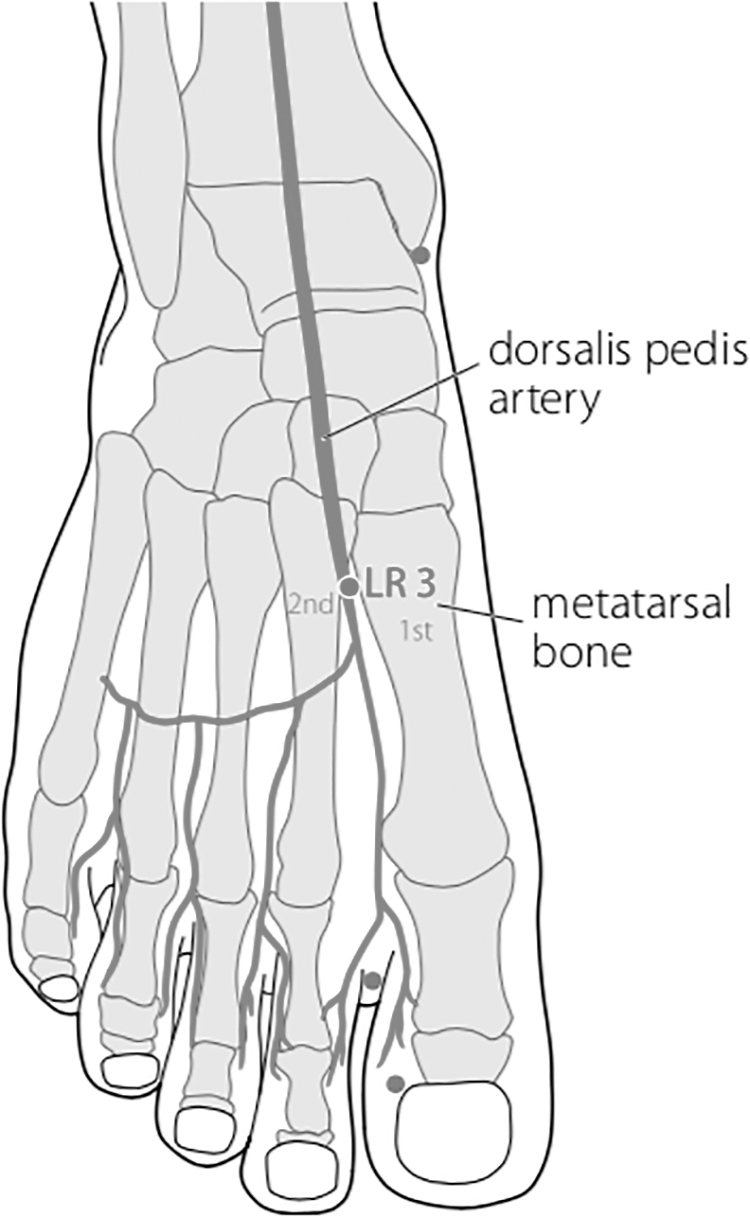
LR 3 Taichong.
FIG. 3.
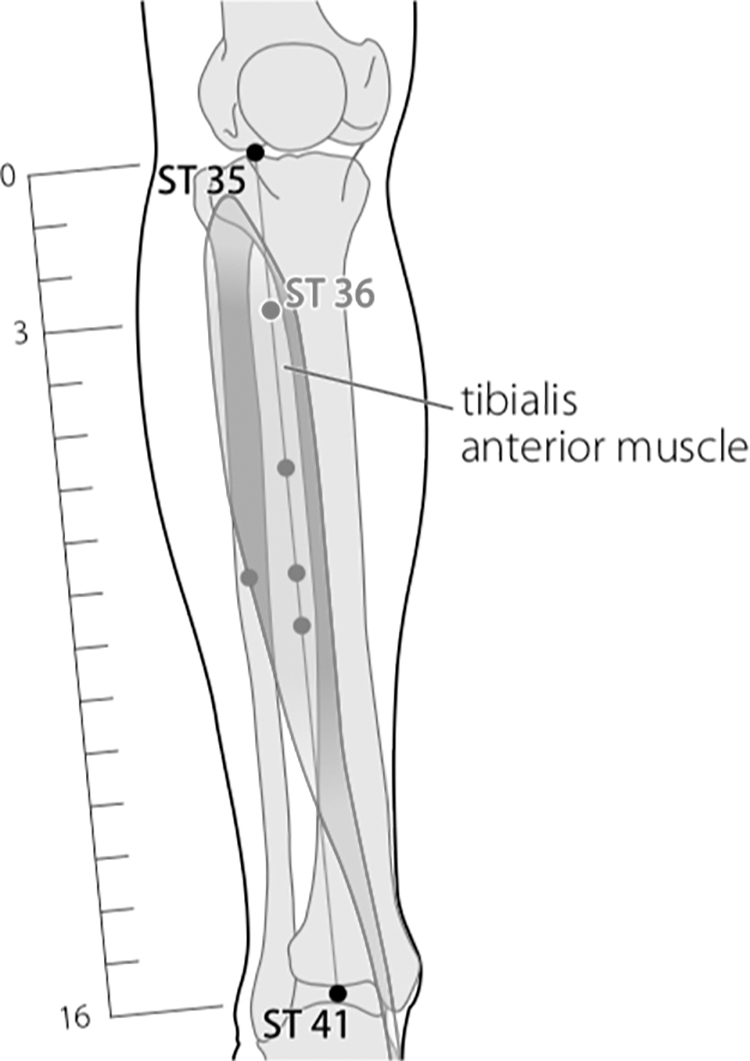
ST 36 Zusanli.
FIG. 4.
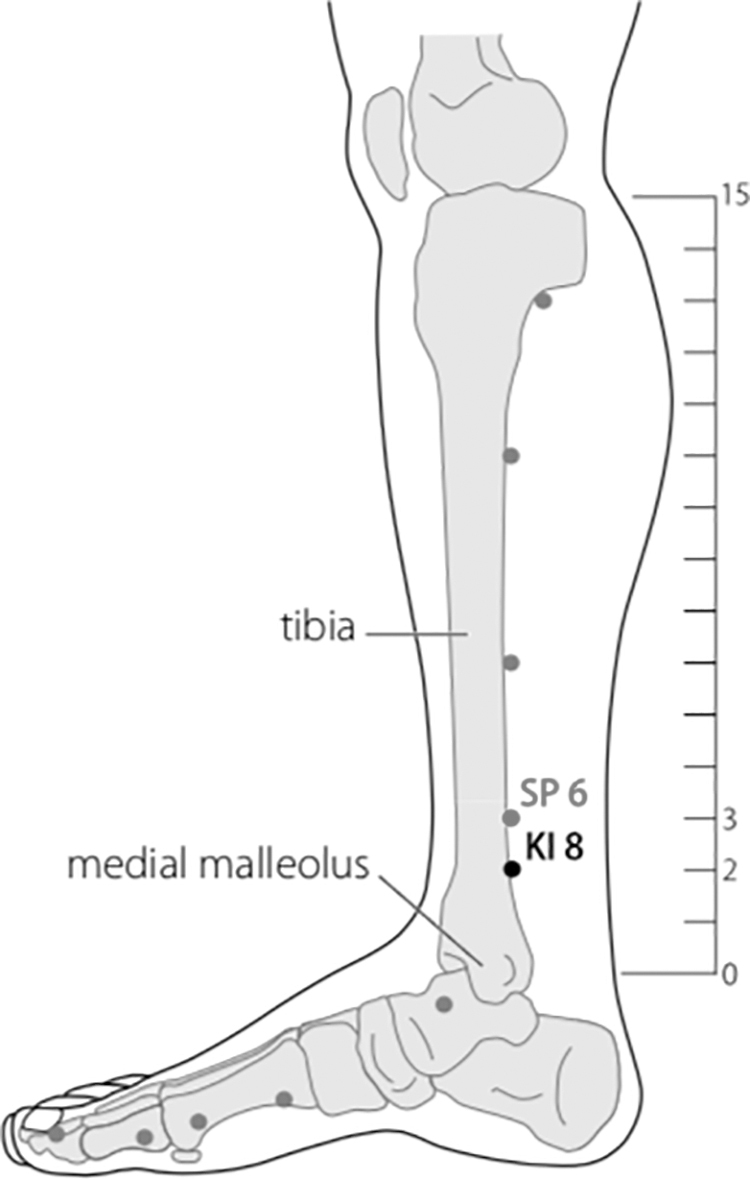
SP 6 Sanyinjiao.
FIG. 5.
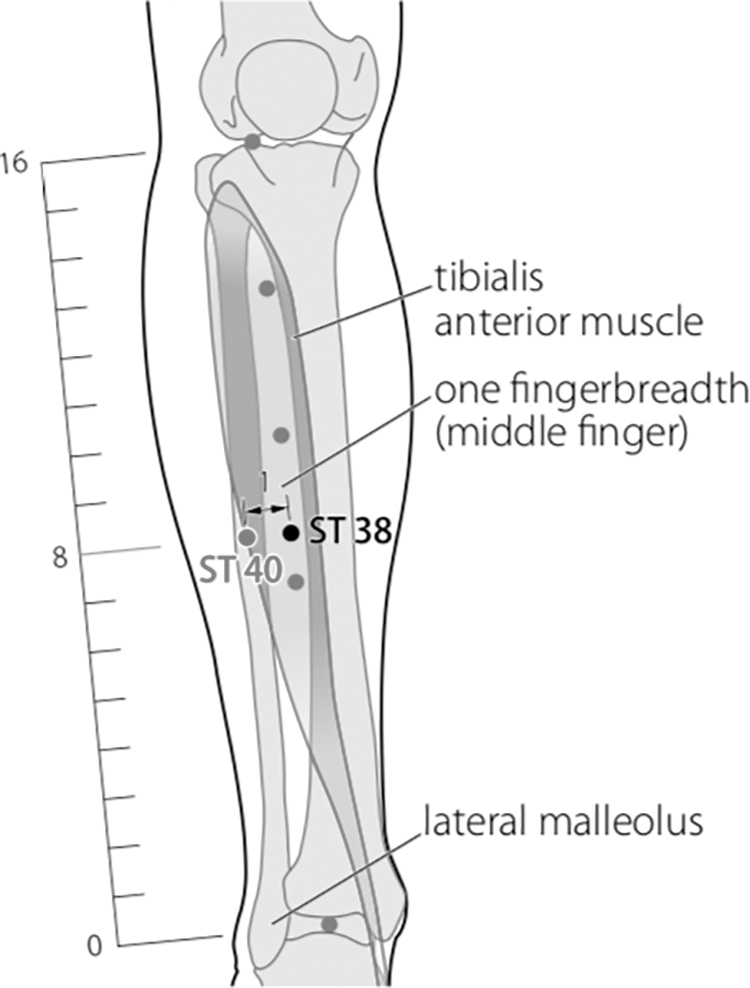
ST 40 Fenglong.
FIG. 6.
Acupoints in Battlefield Acupuncture.
Results
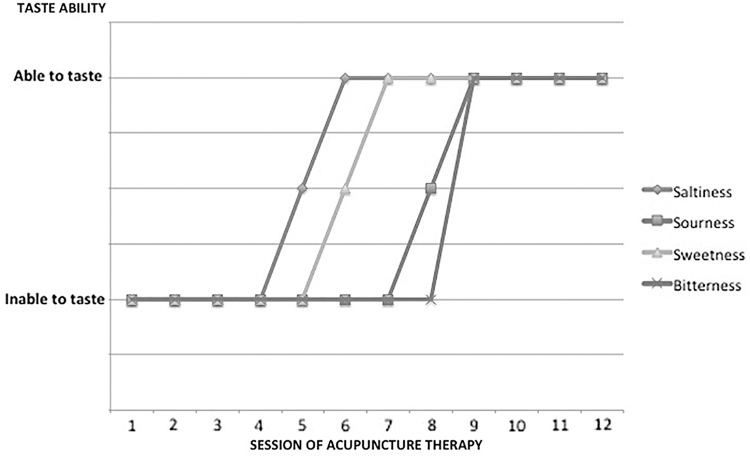
After undergoing 12 sessions of the same treatment in each session, this patient had an improvement in his taste function (Fig. 7) and pain reduction from VAS 4 to VAS 1.
FIG. 7.
Tasting ability chart in 12 acupuncture sessions.
Discussion
This case report described the role of acupuncture in helping to correct abnormalities or dysfunctions that occurred due to side-effects of head-and-neck cancer radiation therapy, in a 65-year-old male patient with laryngeal SCC at stage I. Radiation therapy that exceeds a 30-Gy dose can result in side-effects that can include dermatitis on the skin, xerostomia in the salivary glands, dysgeusia in the papillary gustatorius, mucositis in the oral mucosa, and nausea and vomiting.3 Three acupuncture methods were used to address the complaints; the methods were traditional Chinese body points, BFA ear points, and a balancing method.
In the selection of body-acupuncture points, the chosen points were LI 4 Hegu, LR 3 Taichong, ST 36 Zusanli, ST 40 Fenglong, and SP 6 Sanyinjiao. It has been known that acupuncture in LI 4 can activate the hypothalamus and pituitary gland to secrete endogenous opioid peptides (ß-endorphins, encephalins, and dinorphins) that play a role in analgesia, and can reduce levels of substance P, calcitonin gene-related peptide, natural killer–1 mRNA, cyclo-oxygenase–1 mRNA, and prostaglandin E2 in the spinal cord.
In addition, in a study using functional MRI by Zhang et al.,9 acupuncture in LI 4 activated several areas in the brain, such as the secondary somatosensoric cortex, insula, and primary motor cortex, which are said to be related to reduction of pain. The ST 36 point was chosen because it could reduce the activity of the transient receptor potential vanilloid–1 (TRPV1) in the dorsal root ganglion to reduce pain. In addition, ST 36 has an anti-inflammatory effect and, along with other points, decreases tumor necrosis factor–α, interleukin (IL) IL-6 and increases IL-10.10,11 Acupuncture at the SP 6 point is expected to have antinociceptive and anti-inflammatory effects by decreasing M1 (proinflammatory) macrophages and increasing M2 (anti-inflammatory) and IL10.12 Research in mice showed that the combination of LI 4, LR 3, ST 36 and SP 9 points was effective in suppressing the sensation of pain caused by inflammation.13 Acupuncture also has a general mechanism for reducing pain through the “gate control” system and ß-endorphin secretion in the CNS, which causes analgesia effects.
BFA acupuncture is an ear acupuncture technique that aims primarily to relieve pain. In BFA, the ear acupuncture points are Cingulate Gyrus, Thalamus, Omega, Shen Men, and Zero Point. This acupuncture technique has been proven to relieve pain quickly and pain-free periods can last for minutes, hours, and even up to months. The mechanism of BFA acupuncture is associated with the process of pain modulation in the CNS, involving the hypothalamus, thalamus, cingulate gyrus, and cerebral cortex.14 In ear acupuncture, stimulation is transmitted to the nucleus of the solitarius tract, which will cause various reflexes to stimulate improvement in the general condition of the patient. Stimulation will be sent to the reticular formation, visceral parasympathetic preganglionic neurons, hypothalamus, thalamus, and amygdala to stimulate central activity. Ear acupuncture stimulation can induce the CNS to release endogenous opiate peptides, which help reduce pain and also act as a sedative.15,16
In addition to needling the body points and the BFA points of the ear in this case, a balancing acupuncture method was also applied. Acupuncture with this balancing method is based on the I Ching (Yi Jing). This method is adapted to the meridian theory of Traditional Chinese Medicine (TCM), which has historically been used as a diagnostic tool for effective acupuncture therapy. This method also depends on the relationships among the body's meridians. From the point of view of the balancing I Ching method, health is a state of equilibrium that arises from the reciprocal interactions of a system, whereas pain or disturbance is the opposite. With the balancing I Ching method, balancing the functions of the body systems is expected to cause a return to normal functions.17
The diagnostic and therapeutic steps of the balancing method are: (1) determine the diseased meridian(s); (2) determine the meridians to be treated based on the five systems of the balancing method; and (3) determine the points on the meridians chosen, based on the second step, either by a mirroring format or an imaging format. The selected point can be along the meridian, can be between the meridians, and/or can be a TCM acupuncture point.18 The duration of therapy in the balancing method is 45–60 minutes per session, with a minimum frequency of therapy 2 times per week, while the optimal frequency is 3 times per week.
According to the principle of the balance method, after determining the diseased meridian, which was located in the neck area in this case, acupuncture was performed on the meridian located on the wrist of the anterior side (LU 9 Taiyuan, PC 7 Daling, HT 7 Shenmen) according to the theory of the balancing method. In this theory, the wrist represents the neck.18 The goal is to treat abnormalities that occur in the neck and mouth area; in this case, there were complaints of dysgeusia, pain in the neck, pain on and swallowing.
Acupuncture has several mechanisms that can heal dysgeusia completely, namely, through protective effects on nerve tissue. These mechanisms occurred in this case through increasing expression of neurotrophic factors (NTF), which are brain-derived neurotrophic factors (BDNFs).19 NTF is involved in various processes of development, proliferation, and maturation of nerve cells. NTFs—such as BDNF, nerve-growth factor (NGF), and neurotropin (NT)–3 and NT-4/5—carry out their functions by binding to the tropomyosin-related tyrosine kinase (Trk) receptor, where the specificity of the Trk receptor includes TrkA as an NGF receptor, TrkB as a BDNF receptor, and NT-4/5, and TrkC as an NT-3 receptor. The role of acupuncture is that acupuncture enhances the regulation of Trk receptors to enable an increase in the function of various NTFs. Acupuncture also increases BDNF levels directly.20 NTF will then stimulate neurogenesis and correct nerve synapses to produce a therapeutic effect on dysgeusia disorders that occur in patients.
Conclusions
Routine acupuncture therapy in this case induced a cumulative response that was shown by a perfect improvement in the patient's sense of taste and fairly good pain reduction. By looking at the reduction of his symptoms, it can be concluded that acupuncture played a role in reducing his complaints of dysgeusia, odynophagia, and neck pain after radiation therapy of his head-and-neck cancer.
Author Disclosure Statement
No financial conflicts of interest exist.
Funding Information
The funding of this present work was wholly provided by the first author.
References
- 1. Marur S, Forastiere AA. Head and neck squamous cell carcinoma: Update on epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2016;91(3)386–396 [DOI] [PubMed] [Google Scholar]
- 2. Irfandy D, Rahman S. Diagnosis and Management of Malignant Laryngeal Tumors [in Indonesian]. Jurnal Kesehatan Andalsa. 2015;4(2):618–625 [Google Scholar]
- 3. Galloway TJ, Yom SS. Radiation therapy effects in head and neck cancer. In: Koontz BF, ed. Radiation Therapy Treatment Effects: An Evidence-Based Guide to Managing Toxicity. United States of America: Springer Publishing Company; 2018:19–47 [Google Scholar]
- 4. Sroussi HY, Epstein JB, Bensadoun RJ, et al. Common oral complications of head and neck cancer radiation therapy: Mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6(12):2918–2931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ponticelli E, Clari M, Frigerio S, et al. Dysgeusia and health-related quality of life of cancer patients receiving chemotherapy: A cross-sectional study. Eur J Cancer Care (Engl). 2017;26(2):e12633. [DOI] [PubMed] [Google Scholar]
- 6. Cho Z, Hwang S, Wong E, et al. Neural substrates, experimental evidences [sic] and functional hypothesis of acupuncture mechanisms. Acta Neurol Scand. 2006;113(6):370–377 [DOI] [PubMed] [Google Scholar]
- 7. Garcia MK, McQuade J, Haddad R, et al. Systematic review of acupuncture in cancer care: A synthesis of the evidence. J Clin Oncol. 2013;31(7):952–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Asadpour R, Meng Z, Kessel KA, Combs SE. Use of acupuncture to alleviate side effects in radiation oncology: Current evidence and future directions. Adv Radiation Oncol. 2016;1(4):344–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang W-T, Jin Z, Cui G-H, et al. Relations between brain network activation and analgesic effect induced by low vs. high frequency electrical acupoint stimulation in different subjects: A functional magnetic resonance imaging study. Brain Res. 2003;982(2):168–178 [DOI] [PubMed] [Google Scholar]
- 10. Xu Y, Hong S, Zhao X, et al. Acupuncture alleviates rheumatoid arthritis by immune-network modulation. Am J Chin Med. 2018;46(05):997–1019 [DOI] [PubMed] [Google Scholar]
- 11. Dong ZQ, Zhu J, Lu DZ, Chen Q, Xu YL. Effect of electroacupuncture in. “Zusanli” and “Kunlun” acupoints on TLR4 signaling pathway of adjuvant arthritis rats. Am J Ther. 2018;25:e314–e319 [DOI] [PubMed] [Google Scholar]
- 12. Da Silva MD, Bobinski F, Sato KL, Kolker SJ, Sluka KA, Santos AR. IL-10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol Neurobiol. 2015;51(1):19–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oh JH, Bai SJ, Cho Z-H, et al. Pain-relieving effects of acupuncture and electroacupuncture in an animal model of arthritic pain. Int J Neurosci. 2006;116(10):1139–1156 [DOI] [PubMed] [Google Scholar]
- 14. Niemtzow RC. Battlefield Acupuncture. Med Acupunct. 2007;19(4):225–228 [Google Scholar]
- 15. He W, Jing X, Wang X, et al. Transcutaneous auricular vagus nerve stimulation as a complementary therapy for pediatric epilepsy: A pilot trial. Epilepsy Behav. 2013;28(3):343–346 [DOI] [PubMed] [Google Scholar]
- 16. Ze-tao W, Yi-qin Y, Jun W, Jie-kun L. Observations on the efficacy of auricular-plaster therapy plus medicine in treating heroin addiction. J Acupunct Tuina Sci. 2006;4(2):94–96 [Google Scholar]
- 17. Kotlyar A. Straightforwardness, universality, and effectiveness of the balance method of I Ching acupuncture. Med Acupunct. 2017;29(2):94–104 [Google Scholar]
- 18. Tan RT-F. Acupuncture 1, 2, 3. San Diego: R. Tan; 2007 [Google Scholar]
- 19. Shin HK, Lee S-W, Choi BT. Modulation of neurogenesis via neurotrophic factors in acupuncture treatments for neurological diseases. Biochem Pharmacol. 2017;141:132–142 [DOI] [PubMed] [Google Scholar]
- 20. Zhu W, Ye Y, Liu Y, et al. Mechanisms of acupuncture therapy for cerebral ischemia: An evidence-based review of clinical and animal studies on cerebral ischemia. J Neuroimmune Pharmacol. 2017;12(4):575–592 [DOI] [PubMed] [Google Scholar]