Abstract
Background
Future projections for both TKA and THA in the United States and other countries forecast a further increase of already high numbers of joint replacements. The consensus is that in industrialized countries, this increase is driven by demographic changes with more elderly people being less willing to accept activity limitations. Unlike the United States, Germany and many other countries face a population decline driven by low fertility rates, longer life expectancy, and immigration rates that cannot compensate for population aging. Many developing countries are likely to follow that example in the short or medium term amid global aging. Due to growing healthcare expenditures in a declining and aging population with a smaller available work force, reliable predictions of procedure volume by age groups are requisite for health and fiscal policy makers to maintain high standards in arthroplasty for the future population.
Questions/purposes (1) By how much is the usage of primary TKA and THA in Germany expected to increase from 2016 through 2040? (2) How is arthroplasty usage in Germany expected to vary as a function of patient age during this time span?
Methods
The annual number of primary TKAs and THAs were calculated based on population projections and estimates of future healthcare expenditures as a percent of the gross domestic product (GDP) in Germany. For this purpose, a Poisson regression analysis using age, gender, state, healthcare expenditure, and calendar year as covariates was performed. The dependent variable was the historical number of primary TKAs and THAs performed as compiled by the German federal office of statistics for the years 2005 through 2016.
Results
Through 2040, the incidence rate for both TKA and THA will continue to increase annually. For TKA, the incidence rate is expected to increase from 245 TKAs per 100,000 inhabitants to 379 (297-484) (55%, 95% CI 21 to 98). The incidence rate of THAs is anticipated to increase from 338 to 437 (357-535) per 100,000 inhabitants (29% [95% CI 6 to 58]) between 2016 and 2040. The total number of TKAs is expected to increase by 45% (95% CI 14 to 8), from 168,772 procedures in 2016 to 244,714 (95% CI 191,920 to 312,551) in 2040. During the same period, the number of primary THAs is expected to increase by 23% (95% CI 0 to 50), from 229,726 to 282,034 (95% CI 230,473 to 345,228). Through 2040, the greatest increase in TKAs is predicted to occur in patients aged 40 to 69 years (40- to 49-year-old patients: 269% (95% CI 179 to 390); 50- to 59-year-old patients: 94% (95% CI 48 to 141); 60- to 69-year-old patients: 43% (95% CI 13 to 82). The largest increase in THAs is expected in the elderly (80- to 89-year-old patients (71% [95% CI 40 to 110]).
Conclusions
Although the total number of TKAs and THAs is projected to increase in Germany between now and 2040, the increase will be smaller than that previously forecast for the United States, due in large part to the German population decreasing over that time, while the American population increases. Much of the projected increase in Germany will be from the use of TKA in younger patients and from the use of THA in elderly patients. Knowledge of these trends may help planning by surgeons, hospitals, stakeholders, and policy makers in countries similar to Germany, where high incidence rates of arthroplasty, aging populations, and overall decreasing populations are present.
Level of Evidence
Level III, economic and decision analysis.
Introduction
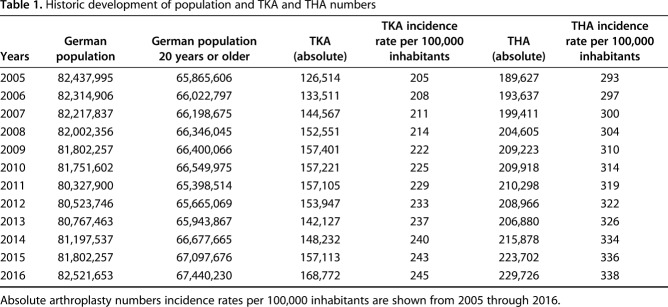
In Germany, primary TKAs and THAs are among the most commonly performed surgical procedures. The German federal office of statistics, Destatis, reported that there were 168,772 primary TKAs in 2016. At the same time, 229,726 primary THAs were performed in the country with a population of 82.5 million people (Table 1) [20]. According to the Organization for Economic Cooperation and Development, the incidence rate was 206 for TKA and 299 for THA per 100,000 inhabitants in Germany in 2015. Thus, Germany had the highest incidence rate for THA after Switzerland within the Organization for Economic Cooperation and Development (OECD). Only the United States, Switzerland, and Austria had higher incidence rates for TKAs [14]. The reasons for this observed trend are manifold. The aging of patients with associated osteoarthritis has been considered a cause [11]. The World Health Organization estimates that osteoarthritis will be the fourth leading cause of physical restriction by 2020 [22]. In addition to medical necessity, other reasons such as economic performance and healthcare expenditures have been demonstrated to play a vital role in the number of joint arthroplasty procedures [5, 8, 15].
Table 1.
Historic development of population and TKA and THA numbers
When dealing with future numbers of joint replacement, projections for the United States are usually referenced in other orthopaedic studies. These projections are based on either demographic or economic data such as healthcare expenditures [8]. However, the demographic and economic characteristics of the United States cannot easily be transferred to other industrialized countries, although the overall demographic trend around the world is similar. In most countries, the overall population is getting older and individuals are less willing to accept activity limitations. In France, the United Kingdom, Australia, Scandinavia, and the United States, the population is still growing due to immigration and comparatively high fertility. However, other developed countries with lower fertility rates and less immigration, such as Japan, Eastern European countries, Russia, Italy, and Germany, face population declines in the near future. This is a trend that many developing countries are likely to follow within a few decades (Fig. 1) [1]. Demographic changes such as population decline and aging have economic and social consequences especially on the healthcare system. As the workforce is aging and shrinking, healthcare systems are challenged by higher demand and costs. The German social healthcare system, which is the oldest in the world, still provides a wide range of benefits, free choice of providers, and unrestricted access to all levels of care [16]. Total joint arthroplasty is a covered treatment, which is generally performed as an inpatient procedure that is remunerated according to diagnosis related groups (DRG) set by a national DRG institute [19]. Due to growing healthcare expenditures in a declining and aging population with a smaller available work force, reliable predictions of future demands for TKA and THA procedures by age groups is information that is necessary for health and fiscal policy makers to sustain high standards in arthroplasty in the next 10, 20, and 30 years.
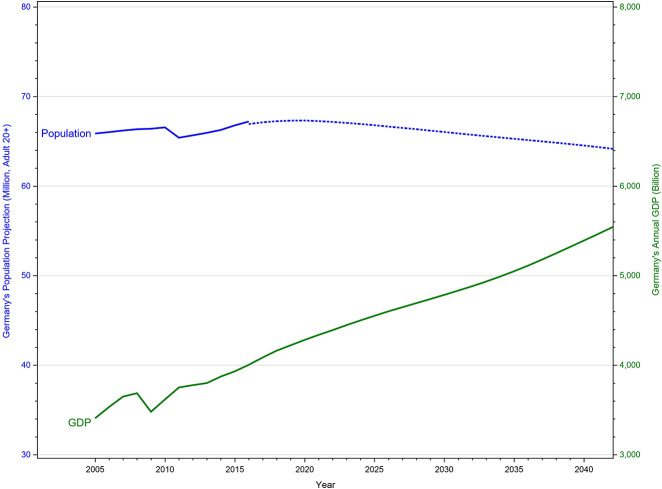
Fig. 1.
Germany's population since 2005 (solid blue line) and projected population through 2040 (dotted blue line), and Germany's historic and projected GDP (green line) are shown.
We therefore asked: (1) By how much is the usage of primary TKA and THA in Germany expected to increase from 2016 through 2040? (2) How is arthroplasty usage in Germany expected to vary as a function of patient age during this time span?
Patients and Methods
Our projections are based on historical arthroplasty data from 2005 to 2016 provided by Destatis. Within this period, an increase in TKA numbers of 33% was observed from 126,514 TKAs in 2005 to 168,772 in 2016. The number of THAs increased 21% between 2005 (189,627) and 2016 (229,726) (Table 1) [20]. For each year of this period, the number of inhabitants in each of the 16 German federal states was considered by gender and year of birth. The deadline of each year was December 31. TKA and THA are generally performed as inpatient procedures, and TKA and THA numbers set by Destatis according to the diagnosis-related group system of 2005 to 2016 were recorded for all patients aged 20 years or older. Surgery and procedure keys (Operation and Procedure Classification System codes) were used to identify all TKAs and THAs, regardless of the underlying disease or injury. For the primary implantation of a hip joint prosthesis, the Operation and Procedure Classification System code "5-820, hip endoprosthesis implantation" was used, and for the implantation of a primary knee prosthesis, the Operation and Procedure Classification System code "5-822, implantation of an endoprosthesis of the knee joint" was used. A detailed breakdown of these data by age group, sex, and place of residence by state was also made.
For the future projection of primary arthroplasties, we used a population projection model. For this purpose, we used the detailed individual results of the 13th coordinated population projection for the German federal states. Destatis used two different variants to estimate population development, namely “continuity of weaker immigration” and “continuity of higher immigration” [17]. These data were broken down by gender, age group, and single age years. The number of live births, deaths, and migration balance were also considered in the calculation.
To calculate future healthcare expenditures, we used estimates of the gross domestic product (GDP) and percentages of healthcare expenditures. We obtained forecasts of the GDP by 2040 from the Frederick S. Pardee Center for International Futures at the University of Denver, Denver, CO, USA (pardee.du.edu). Future healthcare expenditures were calculated as the percentage projections of various scenarios of the “2018 Ageing Report: Economic and Budgetary Projections for the EU Member States (2016-2070)” published on May 25, 2018 (Fig. 1).
Projection Methodology and Statistical Analysis
We estimated the annual number of primary TKA and THA in the next 20 years based on population projections and estimates of future healthcare expenditure as a percent of the GDP in Germany. For this purpose, we performed a Poisson regression analysis using, age, gender, state, healthcare expenditure, and calendar year as covariates. The dependent variable is the historical number of primary TKA and THA performed as compiled by Destatis, which published Germany’s historical population and projection of future population [17]. This data is organized by age groups, sex, and states. The healthcare related GDP is obtained from the Pardee Center of University of Denver, as described in the previous paragraph. The Poisson model basically calculated the historical rates of TKA and THA by age, sex, and state. More importantly, the “time” (year) variable provides a way to calculate the trend or slope parameter of the TKA and THA rates. As indicated, we also included the healthcare expenditure factor as a concurrent covariate. We included this factor to help reflect the overall economics in Germany and its effect on use of hip and knee arthroplasty. For example, an economic downturn and cut back in healthcare expenditures may decrease the number of TKAs and THAs performed, independent of any change in the population. Thus, the slope or trend in the rate of TKAs and THAs reflect the historical trajectory in population and the overall influence of Germany’s healthcare expenditure on TKA or THA use. The model also includes interaction terms between age, sex, states, and year, so the rate of TKA or THA at a given year in the future is governed by the overall trend by age, sex, and states, and adjustments to the trend by the combinations of these factors. The results from the Poisson model is an estimated rate of TKA or THA through 2040 for every combination of age, sex, and state. The estimated number of TKAs and THAs are simply the product of these estimated rates and the projected population for that combination of age, sex, and state. The overall number of TKA and THA is obtained by summation of these estimated numbers across age, sex, and state categories. Our methodology is consistent with that used in previously published studies [7, 8].
The estimated rate from the Poisson model also comes with 95% CIs. Thus, the upper and lower bound of these rates estimates also converted into upper and lower bounds 95% confidence of the potential number of TKAs and THAs.
Results
Anticipated Increase in Arthroplasty Usage in Germany from 2016 Through 2040
When we compared the incidence rates for both TKA and THA, we predict there will be a continuous increase from 2016 through 2040 (Table 2). In total numbers, we project a 45% (95% CI 14 to 8%) increase in TKA usage in Germany from 2016 to 2040. TKAs will increase from 168,722 in 2016 to 244,714 (95% CI 191,920 to 312,551) in 2040 (Table 3). The incidence rate of TKAs will increase from 245 in 2016 to 379 in 2040 (95% CI 297 to 484). Until 2040, the number of women patients who undergo TKA will increase by approximately 44% (95% CI 35 to 56). This corresponds to 151,706 TKAs (95% CI 119,019 to 193,607) in 2040. For men, an increase of 46% (95% CI 36 to 59) to 93,008 TKAs (95% CI 72,901 to 118,944) in 2040 is expected (Fig. 2).
Table 2.
Total numbers of TKAs and THAs
Table 3.
Estimated numbers and incidence rates of TKA compared with estimated population numbers from 2016 through 2040

Fig. 2.
The numbers of TKAs in Germany are shown. For both genders (blue = women [W]; red = men [M]), numbers from 2005 to 2016 and projected numbers (dashed lines) until 2040 are shown. The spread resulting from the statistical calculation increased with time for both genders.
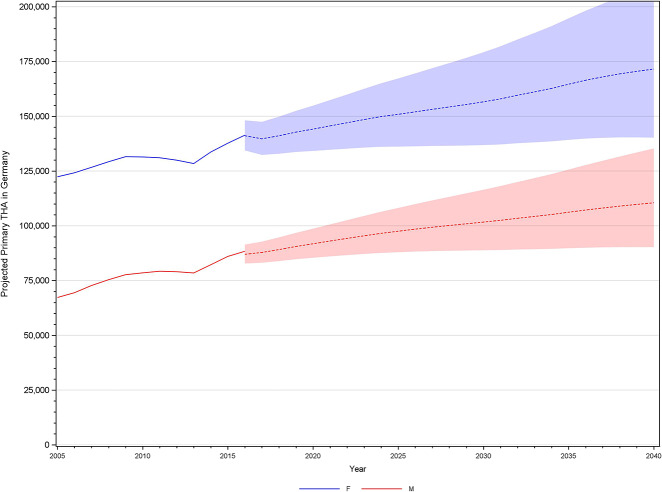
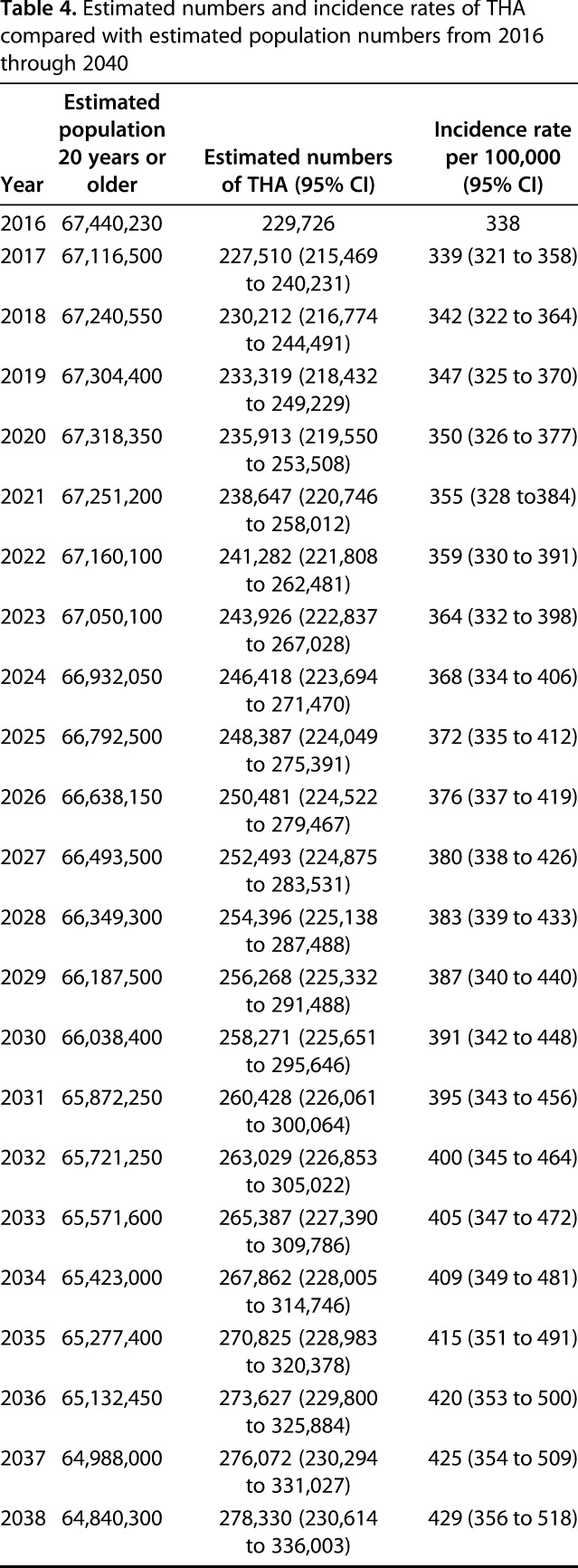
For THA, we project a 23% increase in usage (95% CI 0 to 50) (Fig. 3), which corresponds to an increase from 229,726 THA procedures in 2016 to 284,034 primary THAs (95% CI 230,473 to 345,228) in 2040. Despite a decline in population, a 29% increase in incidence rate (95% CI 11 to 58) in 2040 will lead to an overall increase in the absolute THA numbers (Table 4). The incidence rate for THA will increase from 338 in 2016 to 437 (95% CI 357 to 535) in 2040. In women, the THA incidence rate will increase 21% (95% CI 1 to 49) from 407 in 2016 to 523 (95% CI 427 to 640) in 2040. This correlates with 141,364 THA procedures in 2016 and 171,541 procedures (95% CI 140,215 to 209,917) in 2040. For men, the incidence rate will rise from 265 in 2016 to 349 (95% CI 285 to 427) in 2040, which mirrors an increase in absolute numbers of about 25% (95% CI 2 to 53) (2016: 88,362 THA procedures; 2040: 110,493 (95% CI 90,258 to 135,311).
Fig. 3.
This figure shows the annual number of THAs in Germany. In addition to the current trend from 2005 to 2016, the projection of prosthetic implants until 2040 is shown for both genders (blue = women [W]; red = men [M]) (dashed line). The spread resulting from the statistical calculation increased with time for both genders.
Table 4.
Estimated numbers and incidence rates of THA compared with estimated population numbers from 2016 through 2040

Arthroplasty Usage as a Function of Age in Germany Through 2040
We predict that the rising incidence of arthroplasty in patients younger than 70 will have the largest effect on the total number of TKAs performed, while total numbers of THAs are driven by rising incidence in patients older than 70 years. Breaking down the numbers by age groups (Fig. 4), there will be a 269% increase in TKA procedures in patients aged 40 to 49 years (95% CI 179 to 390), which correlates with an increase from 4990 TKA procedures in 2016 to 18,429 TKAs (95% CI 13,932 to 24,395) in 2040. In patients aged 50 to 59 years, we anticipate an increase of 89% (95% CI 48 to 141) TKA procedures, which reflects an increase from 28,438 to 53,790 TKA procedures (95% CI 42,160 to 68,644) between 2016 and 2040. In patients aged 60 to 69 years, the TKA numbers are expected to increase in a similar way, reaching 81,746 in 2031 (95% CI 69,321 to 96,406). This number is half the TKAs performed in 2015 (157,113).
Fig. 4.
This figure shows the past and future numbers of TKAs by age group in 10-year increments. Especially in patients aged 40 to 60 years, an exponential increase in primary TKAs is expected by 2040. For people aged 60 to 69 years, we expect an initially steep increase in the number of procedures through 2034 followed by an annual decline.
For patients aged 70 to 79 years, we expect an increase of approximately 6% (95% CI -16 to 26); this corresponds to an increase from 63,122 TKA procedures in 2016 to 66,928 (95% CI 52,943 to 84,624) TKA procedures in 2040 (Fig. 4). In patients who are 80 to 89 years old, TKA procedures will increase 63% (95 CI 28 to 109) between 2016 and 2040. In total numbers, TKA procedures will increase from 19,615 TKAs in 2016 to 32,008 (95% CI 25,046 to 40,917) in 2040.
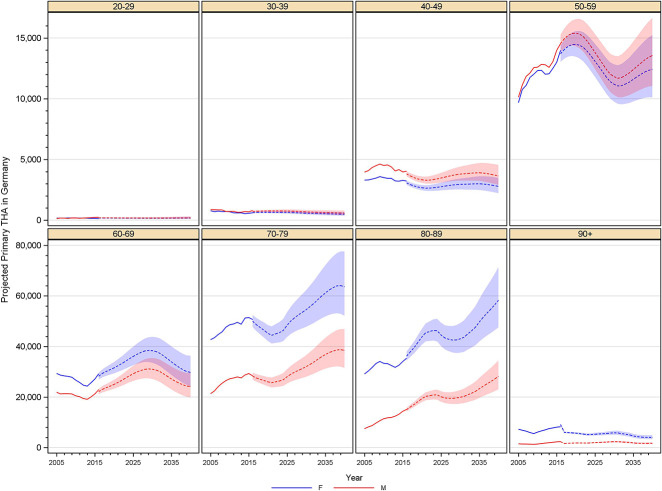
Similar to TKA procedures in patients younger than 40 years (Fig. 4), the number of primary THAs among patients younger than 40 years is negligible (Fig. 5). For primary THA, a -7% decrease (95% CI -26 to 17) is anticipated in patients aged 40 to 49 years (2016: 6881 procedures; 2040: 6416 procedures; (95% CI 5120 to 8041). In patients aged 50 to 59 years, THAs will peak in 2022. According to analysis, the number of primary THAs in this age group will decline until 2031 and rise again afterwards. Overall, the number of procedures will decrease by -8% (95% CI -19 to 13) until 2040. This corresponds to 28,246 THA procedures in 2016 and: 25,972 procedures (95% CI 21,155 to 31,888) in 2040.
Fig. 5.
This figure shows the past and future numbers of primary THAs by age group in 10-year increments, beginning at the age of 20 years. Particularly in patients aged 70 to 90 years, an increase in the number of procedures can be expected in the next two decades.
In patients 60 to 69 years of age, THAs will peak in 2029, up 34% (95% CI 17.5 to 51.6) from 2016 (2029: 69,549 procedures; 95% CI 61,245 to 78,982). For patients aged 70 to 79 years, an increase in THA is expected during the next few years. Beginning in 2021, there will be an increase of 46% from 70,109 procedures (95% CI 64,950 to 75,678) to 102,091 procedures (95% CI 83,724 to 124,500). Patients aged 80 to 89 years will also have a large increase of 71% (95% CI 40 to 110), in primary THAs by 2040 (2016: 50,425 procedures; 2040: 86,422 procedures; 95% CI 70,579 to 105,831). with a low decline in procedure numbers between 2023 and 2028 (Fig. 4).
Discussion
In recent years both TKA and THA have been one of the most often performed surgical procedures in Germany [21]. Aging and concomitant shrinking of the population challenge the healthcare system not only in Germany but also in most other Western industrial nations. Other high-income countries have already confronted the same issue. Developing countries will follow in light of global aging [9, 18]. To be able to continue unrestricted access to arthroplasty, which can be deemed one of the most successful surgical procedures in terms of restoring quality of life, detailed and reliable forecasts of procedure numbers are extremely useful. The projections estimated in this study demonstrate an increase in both incidence rate and total arthroplasty numbers for TKA (Table 3) and THA (Table 4) through 2040. The predicted incidence rate increase is higher than the increase in total numbers, which can be explained by population decline. Although the increase in TKA numbers will mainly be driven by an increase of TKAs in patients who are 40 to 70 years old (Fig. 4), THAs will mainly increase in patients who are 70 to 90 years old (Fig. 5).
Limitations
Our study has several limitations. As for any projection study, initial underlying historical data and the model parameters derived from it have to be correct. Although TKA and THA superordinate Operation and Procedure Classification System codes were available, it was not possible to differentiate between prosthesis types and diagnoses leading to joint arthroplasties. We thought it appropriate to rely on those superordinate codes because technical surgical trends (cementless, cemented, short-stem, etc) should not influence the overall implantation rates. Further, we based our projection on population data and healthcare expenditures as a share of the GDP. Future estimates for both population numbers and the health-related GDP are based on current trends. In 20 years, however, different unforeseeable events such as new arthritis treatments, war, changes in migration, health financing or structure of health care might occur. Especially in challenged healthcare systems, financing shortfalls may lead to changes in funding mechanisms as well as higher risk and pain tolerance of the patients. This uncertainty cannot be captured or completely avoided in our or in any other predictive study [3, 17]. In addition, the decision to undergo TKA and THA is not just driven by the population size or overall economic well-being in the country. For example, changes in osteoarthritis prevalence would have an effect on TKA and THA need [10]. Availability and acceptance of another treatment modality would also play a role; however, no prediction model can account for these possibilities. Not including any potential risk factors that could increase future arthroplasty numbers in the projection model may result in underestimation of future arthroplasty numbers. If shortcomings in financing result in restricted access to health care, future estimates would overestimate the real future arthroplasty numbers. Thus, one is limited by the availability of future population data and health-related GDP as the main drivers of future TKA or THA growth.
We recognized that over the period of this study, the population trend is not strictly linear. Some periods may experience a more rapid growth, and there may be periods of slower growth. We have tried to include nonlinear terms in the year trend to capture these nonlinear patterns. However, the projections, when quadratic or other higher-order terms were included, produced unreliable numbers; in some cases, these were dramatically higher and unrealistic. Thus, we chose a more conservative approach and adopted only linear estimates for the trends, knowing that it was not able to capture some of the nonlinearity in the historical data but was able to avoid the ill effect of excessively high or low projections. Incorporating nonlinear trends into the Poisson model could be accomplished by a spline function, for example. However, such an attempt would require further research.
Anticipated Increase in Arthroplasty Usage in Germany from 2016 to 2040
If current trends continue, we project a substantial increase in the number of patients undergoing primary TKA (Fig. 2) and THA (Fig. 3) in Germany between now and 2040. However, this increase in absolute numbers by 45% for TKA and 23% for THA is moderate compared with projections previously published for the United States [7, 8]. Kurtz et al. [7] predicted increases of 673% for TKAs and 174% for THAs from 2007 through 2030 in the United States; this is by far higher than the anticipated increase in Germany, the country in the OECD with the second most TKA and THA procedures. Demographic changes such as population aging and decline seem to be the key driver for the lower increase of total numbers compared with a stronger increase of TKA and THA incidence rates in Germany. However, in other European countries like Sweden (49% TKA increase and 25% increase in THA between 2013 and 2030 [12, 13]) and the United Kingdom (40% TKA increase, 32% THA increase between 2015 and 2035 [2]) a similar increase in numbers is to be expected. Unlike Germany (Fig. 6), the Swedish and UK populations are expected to increase over the time of our projections. Although different methodologies may be responsible for observed differences, other nondemographic factors must be discussed as potential reasons. As for any kind of service, access and costs are of paramount importance when talking about use. In Germany, unrestricted access to orthopaedic specialists is guaranteed. In addition, government health insurance as well as private health insurance cover costs for primary arthroplasty which is reimbursed at set rates under the terms of law passed in 2004 (for example, TKA about USD 6500, ICD-10-GM 2020: M17.1, Operation and Procedure Classification System code 5-822.01, DRG I44D; THA about USD 7500 (ICD-10-GM 2020: M16.1, Operation and Procedure Classification System code 5-820.00, DRG I47B) [4]. In Germany, this reimbursement is generally deemed profitable for healthcare providers. Nevertheless, compensation by a single lump-sum payment, which reduces financial incentives inherent in fee-for-service reimbursement models, might be an important nondemographic factor, which accounts for differences between predicted implantation rates in different countries.
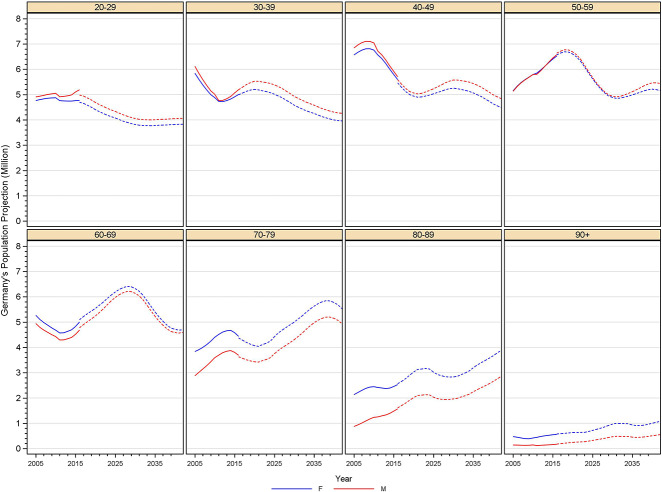
Fig. 6.
Germany's population projection broken down by age group in 10-year increments is shown.
Arthroplasty Usage as a Function of Age in Germany Through 2040
If current trends continue, we project a marked change in the age distribution of patients undergoing primary TKA and THA in Germany between now and 2040, with the greatest increases in TKA coming in patients between the ages of 40 and 69 years (Fig. 4) and in THA between the ages of 70 and 89 years (Fig. 5). Mean prosthesis survival rates of 97%, 89%, and 78% at 5, 10, and 15 years, respectively, and greater complication rates in younger patients versus older patients may mean we will face more revision surgeries after TKA because of aseptic loosening, periprosthetic joint infection, and prosthesis instability [6]. Although a rise in revision TKA seems inevitable, key strategies such as prevention programs and using nonoperative treatment options to delay primary TKA should be further highlighted by healthcare providers. In addition to the economic obligation for healthcare systems that accompanies higher revision rates, the high burden of disease for affected patients should considered when arguing for financing for nonoperative treatment strategies with policy makers.
Conclusions
We found that numbers of TKAs are expected to increase by 45% and THAs by 23%, respectively, in Germany through 2040. The strongest increase in TKA numbers can be anticipated in patients aged 40 to 70 years. For THA, the strongest increase in numbers is expected in patients aged 70 to 90 years. In the same period, the adult German population is expected to age and decrease in number, a fate currently faced by several other developed countries, with developing countries such as China close behind in the near future. Although the predicted increase in numbers is not as strong as formerly predicted for the United States for both TKA and THA, the German health care system is challenged by growing economic pressure from higher costs and a smaller working force to pay for it. In light of limited resources and finite healthcare budgets, the predicted increase in total joint arthroplasty procedures will require less costly and resource-intensive alternatives for perioperative care and rehabilitation. Fast-track surgery and outpatient total joint arthroplasty have been established as possible options but are unlikely to be feasible in the elderly. The expected higher demand in primary THA in a more vulnerable patient cohort should encourage stakeholders in the healthcare systems to reflect additional demands for geriatric treatment and care.
Acknowledgments
We thank Sabine Nemitz and Melanie Scheller from the Federal Statistical Office of Germany (Destatis) for their support of this work.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each remaining author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution waived approval for the protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Exponent Inc, Menlo Park, CA, USA.
References
- 1.Coleman D, Rowthorn R. Who's afraid of population decline? A critical examination of its consequences. Popul Dev Rev. 2011;37:217-248. [DOI] [PubMed] [Google Scholar]
- 2.Culliford D, Maskell J, Judge A, Cooper C, Prieto-Alhambra D, Arden N, Group CS. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage. 2015;23:594-600. [DOI] [PubMed] [Google Scholar]
- 3.European Commission. Publications Office of the European Union Luxembourg. The 2018 ageing report economic and budgetary projections for the EU member states (2016–2070). https://ec.europa.eu/info/publications/economy-finance/2018-ageing-report-economic-and-budgetary-projections-eu-member-states-2016-2070_en. Accessed May 20, 2019.
- 4.DRG Katalog. [In German]. Reimbursement institute; https://app.reimbursement.info/drgs. Accessed January 30, 2020. [Google Scholar]
- 5.Iorio R, Davis CM, III, Healy WL, Fehring TK, O'Connor MI, York S. Impact of the economic downturn on adult reconstruction surgery: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2010;25:1005-1014. [DOI] [PubMed] [Google Scholar]
- 6.Khan M, Osman K, Green G, Haddad F. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J. 2016;98:105-112. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz S, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624-630. [DOI] [PubMed] [Google Scholar]
- 9.Li X, Fan L, Leng SX. The aging tsunami and senior healthcare development in China. J Am Geriatr Soc. 2018;66:1462-1468. [DOI] [PubMed] [Google Scholar]
- 10.Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michael JW, Schlüter-Brust KU, Eysel P. [Epidemiology, etiology, diagnosis und treatment of osteoarthritis of the knee] [In German]. Dtsch Arztebl Int. 2010;162:152-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nemes S, Gordon M, Rogmark C, Rolfson O. Projections of total hip replacement in Sweden from 2013 to 2030. Acta Orthop. 2014;85:238-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nemes S, Rolfson O, W-Dahl A, Garellick G, Sundberg M, Kärrholm J, Robertsson O. Historical view and future demand for knee arthroplasty in Sweden. Acta Orthop. 2015;86:426-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.OECD. Hip and knee replacement. In: Health at a Glance 2017: OECD Indicators, OECD Publishing, Paris, 10.1787/health_glance-2017-65-en. Accessed September 16, 2019. [DOI] [Google Scholar]
- 15.Pabinger C, Geissler A. Utilization rates of hip arthroplasty in OECD countries. Osteoarthritis Cartilage. 2014;22:734-741. [DOI] [PubMed] [Google Scholar]
- 16.Polin K, Quentin W, Stephani V, Geissler A. Country report: Germany. The Law and Policy of Healthcare Financing: Edward Elgar Publishing; 2019:305-331. [Google Scholar]
- 17.Pötzsch O, Rößger F. [Population projection in Germany through 2060. 13th coordinated population projection] [In German]. Statistisches Bundesamt, Wiesbaden: 2015:45-56. [Google Scholar]
- 18.Shetty P. Grey matter: ageing in developing countries. Lancet. 2012;379:1285-1287. [DOI] [PubMed] [Google Scholar]
- 19.Stargardt T. Health service costs in Europe: cost and reimbursement of primary hip replacement in nine countries. Health economics. 2008;17:S9-S20. [DOI] [PubMed] [Google Scholar]
- 20.Statistisches Bundesamt (Destatis). https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/Publikationen/Downloads-Krankenhaeuser/operationen-prozeduren-5231401187014.pdf. Accessed September 20, 2019.
- 21.Wengler A, Nimptsch U, Mansky T. [Hip and Knee Replacement in Germany and the USA. Analysis of Individual Inpatient Data From German and US Hospitals for the Years 2005 to 2011] [In German]. Dtsch Arztebl Int. 2014;111:407-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646-656. [PMC free article] [PubMed] [Google Scholar]