Abstract
Background
Revision THA represents approximately 5% to 10% of all THAs. Despite the complexity of these procedures, revision arthroplasty service lines are generally absent even at high-volume orthopaedic centers. We wanted to evaluate whether financial compensation is a barrier for the development of revision THA service lines as assessed by RVUs.
Questions/purposes
Therefore, we asked: (1) Are physicians fairly compensated for revision THA on a per-minute basis compared with primary THA? (2) Are physicians fairly compensated for revision THA on a per-day basis compared with primary THA?
Methods
Our deterministic financial model was derived from retrospective data of all patients undergoing primary or revision THA between January 2016 and June 2018 at an academic healthcare organization. Patients were divided into five cohorts based on their surgical procedure: primary THA, head and liner exchange, acetabular component revision THA, femoral component revision THA, and combined femoral and acetabular component revision THA. Mean surgical times were calculated for each cohort, and each cohort was assigned a relative value unit (RVU) derived from the 2018 Center for Medicaid and Medicare assigned RVU fee schedule. Using a combination of mean surgical time and RVUs rewarded for each procedure, three models were developed to assess the financial incentive to perform THA services for each cohort. These models included: (1) RVUs earned per the mean surgical time, (2) RVUs earned for a single operating room for a full day of THAs, and (3) RVUs earned for two operating rooms for a full day of primary THAs versus a single rooms for a full day of revision THAs. A sixth cohort was added in the latter two models to more accurately reflect the variety in a typical surgical day. This consisted of a blend of revision THAs: one acetabular, one femoral, and one full revision. The RVUs generated in each model were compared across the cohorts.
Results
Compared with primary THA by RVU per minute, in revision THA, head and liner exchange demonstrated a 4% per minute deficit, acetabular component revision demonstrated a 29% deficit, femoral component revision demonstrated a 32% deficit, and full revision demonstrated a 27% deficit. Compared with primary service lines with one room, revision surgeons with a variety of revision THA surgeries lost 26% potential relative value units per day. Compared with a two-room primary THA service, revision surgeons lost 55% potential relative value units per day.
Conclusions
In a comparison of relative value units of a typical two-room primary THA service line versus those of a dedicated revision THA service line, we found that revision specialists may lose between 28% and 55% of their RVU earnings. The current Centers for Medicare and Medicaid Services reimbursement model is not viable for the arthroplasty surgeon and limits patient access to revision THA specialists.
Level of Evidence
Level III, economic and decision analysis.
Introduction
Revision THA is a technically demanding procedure that is frequently performed for instability, dislocation, aseptic mechanical failure, and periprosthetic infection [4]. According to contemporary joint arthroplasty registries, the THA revision burden ranges from 10% to 12% of all hip arthroplasties [2, 27] and is projected to increase concomitantly with the rise in primary THA volume [21]. Currently, the mean hospital charge for a single revision THA is estimated to be USD 54,533, with less-involved revision procedures such as head and liner exchanges having a mean cost of USD 42,245 [4]. In 2015 alone, revision THA procedures were estimated to place a USD 3.8 billion annual cost burden on the US healthcare system, up 290% from 2005 [11, 22].
To reduce Centers for Medicare and Medicaid Services (CMS) spending on total joint arthroplasty, several alternative payment models have been implemented with varying success. However, bundling payments for revision procedures has not proven feasible because of the inherent unpredictability of revision THA and its high risk of associated complications [8]. As a result, physicians are generally compensated under the traditional fee-for-service reimbursement model in which services rendered are coded using Current Procedural Terminology (CPT) codes that correspond to a predetermined number of relative value units (RVUs). The number of RVUs associated with a CPT code is calculated based on physician work (time, effort, and skill required), practice expenses, and professional liability insurance expenses [1, 7]. A conversion factor is then applied to convert RVUs to a USD amount.
Prior studies have reported that the increased technical demand of revision THA relative to that of primary THA does not result in a proportional increase in total compensation [3, 31, 33, 36]. One study reported that although surgical time was 1.8 times greater for standard revision THA than for primary procedures, the mean surgeon reimbursement was increased by only 1.3-fold. By their estimates, a surgeon focusing exclusively on revision surgery would face a reimbursement deficit between 32.5% to 50% annually, depending on surgical complexity [36].
To our knowledge, there are currently few, if any, healthcare institutions that have implemented a dedicated revision arthroplasty service line. These service lines would integrate healthcare services commonly used during a revision THA episode of care, potentially allowing for more reproducible patient outcomes, improved healthcare performance monitoring, and maintain the financial sustainability of these complex procedures. In this regard, surgeons who have a higher volume of revision procedures have been shown to produce better outcomes, including lower mortality and fewer re-revisions, than lower-volume revision arthroplasty surgeons [14, 18, 19]. However, under the current RVU-based system a dedicated revision arthroplasty service line may be financially impractical. Specifically, we wanted to model physician RVU reimbursements under hypothetical revision and primary arthroplasty service lines using historical data from a high-volume, dedicated orthopaedic surgery hospital. By doing so, we sought to determine whether a hypothetical dedicated revision THA service line would inadequately reimburse a revision THA service line compared with a primary THA service line, creating a disincentive for skilled arthroplasty surgeons to participate in such a dedicated revision THA program.
In this study, we asked (1) Are physicians fairly compensated for revision THA on a per-minute basis compared with primary THA? (2) Are physicians fairly compensated for revision THA on a per-day basis compared with primary THA?
Patients and Methods
A deterministic financial modeling study was developed to assess if orthopaedic surgeons are fairly incentivized to perform revision THA when compared with primary THA. We sought to answer this question by first evaluating the amount of RVUs earned per surgical time expenditure for primary and revision THA procedures:
 |
To assess a relative percentage gain (positive value) or loss (negative value) when compared with a control procedure, the following formula was derived:
As our study was designed to assess revision THA RVU gain and loss relative to primary THA, the formula was transformed to the following:
This formula was initially applied to assess relative RVU gains and losses for performing a single revision THA. Secondary analyses were performed to assess the effect of a full operative day by accounting for operating room turnover and time constraints of a typical operative day.
Using Microsoft SQL Server Management Studio (Redmond, WA, USA), we queried our institution’s electronic data warehouse, Epic Caboodle (Verona, WI, USA), for all patients undergoing unilateral primary or revision THA between January 2016 and June 2018. Revision THA consisted of all comers, including aseptic loosening, prosthetic hip dislocation, polyethylene wear, and periprosthetic joint infection. Surgical encounters were subsequently separated into five distinct cohorts based on surgical implant logs derived from the electronic data warehouse query: primary THA, THA with liner exchange (polyethylene liner and/or femoral head replacement), acetabular revision (acetabular cup), femoral revision (femoral stem and head), and full revision (all components replaced). Patients who underwent irrigation and débridement without hardware exchange, removal of hardware without reimplantation of hardware, or placement of antibiotic spacers were excluded from the study. In total, 3920 patients underwent primary THA and 399 underwent revision THA. Of the patients undergoing revision THA, 101 had head and liner exchanges, 108 had acetabular component revisions, 96 had femoral revisions, and 94 had full revision THAs (Table 1). Patients who underwent repeat surgery were not excluded from the study as our primary datapoint of interest was mean surgical time for a designated procedure. All retrospective data was derived from prospectively collected, standard of care data at an academic, urban, orthopaedic hospital. Mean surgical time was extracted and used for our deterministic financial model. RVU were assigned to each of the five cohorts based off the 2018 CMS RVU [7].
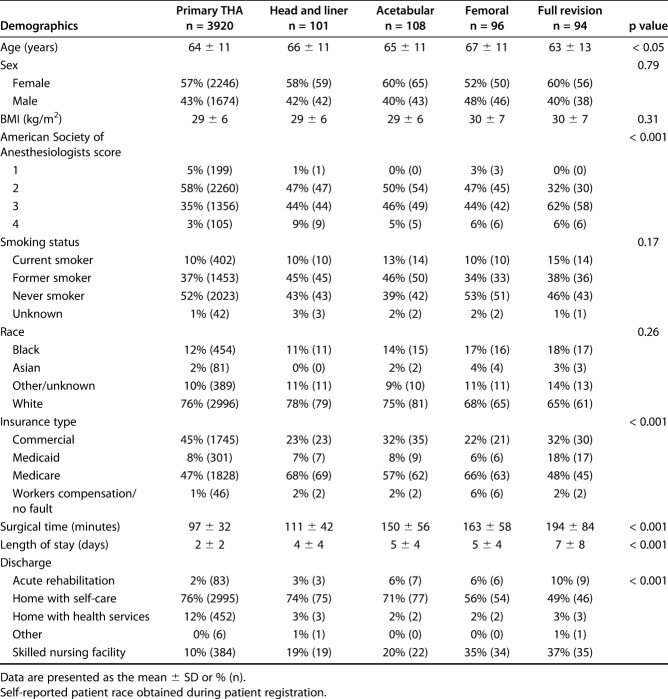
Table 1.
Demographics of patients undergoing primary THA and those undergoing revision THA
Variables, Outcome Measures, Data Sources, and Bias
Variables and Data Sources
We extracted data on patient demographics (age, sex, race, BMI, American Society of Anesthesiology score, smoking status, ZIP code, and insurance type) and inpatient admission data (surgery type, surgical time, length of stay, and discharge information).
Outcome Measures and Derivation
We developed three deterministic financial models based on the Medicare RVU to assess the financial incentives, or lack thereof, for a revision THA service line. These three models included: (1) comparing RVU per mean operative time expenditure for primary versus revision THA; (2) comparing daily RVU earning for primary THAs performed in a single operating room versus revision THAs performed in a single operating room; and (3) comparing daily RVU earnings for primary THAs performed in two operating rooms versus revision THAs performed in a single operating room.
For Model 1, RVUs per minute losses were calculated based on mean surgical time, excluding operating room turnover time, as illustrated by the equation below:
Percentage RVU per minute deficit for revision THA:
 |
In Model 2, the length of the surgical day was 9 hours (8 am - 5 pm). Additionally, the total time for THA was determined to be the mean surgical time for THA plus an additional 30 minute for operating turnover time. While surgeons participating in primary THA services were able to perform 5 surgeries, those partaking in a revision service demonstrated lower operative volumes of four THAs for head and liner exchange, three THAs for acetabular revisions, three THAs for femoral revisions, and two THAs for full revisions. To make a more conservative estimate of revision THA losses, the last revision THA of the day was permitted to exceed the allotted total daily surgical time of 9 hours: head and liner exchange - 7 minutes extra; acetabular - 0.5 minutes; femoral - 8 minutes; full revision - 40 minutes. Conversely, primary THAs were only allotted the surgical day timespan.
To better assess how revision services may affect surgeon reimbursements for a mixed revision operative day and how they would fluctuate with differing levels of participation during a 2-day operative week, revision volumes were blended together. Given the equal distribution of the acetabular, femoral, and full revision cohorts, a daily blend of one acetabular component revision, one femoral component revision, and one full revision was used. Head and liner exchanges were excluded. Daily losses were calculated as follows:
Percentage RVU deficit for revision THA service day:
 |
In Model 3, the volume of primary THA was increased to eight procedures per day to simulate use of a second operating room. Primary THA daily procedural was volume was conservatively set at eight procedures per day to favor revision THA. All subsequent calculations were identical to that of Model 2. Models 2 and 3 were further extrapolated to 1-week and 1-year models for a hypothetical surgeon operating twice per week.
Bias
Our study is a retrospective analysis of all-comers to a single, urban, academic, tertiary healthcare system. Potential areas of bias include selection bias, transfer bias, and assessor bias. Selection bias was minimized in our study by including all-comers of primary and revision total hip arthroplasty. Arguably, as a tertiary, academic healthcare system our patient population may differ from other healthcare systems. Transfer bias was minimal in our study as patient follow-up was limited to the surgical encounter only. Therefore, no patient was lost to follow-up and our data was complete. Assessor bias was minimal in our study because all data was derived from prospectively collected, standard of care data (for example, surgical start/stop time, patient demographics, CMS-defined RVUs, etc.). One potential source of assessor bias, however, was the volume of potential surgical procedures performed by a single surgeon. A conscious attempt by the authors was made to provide financial advantages to the revision THA service line. These included allowing the revision THA service line to exceed the allotted surgical day duration in Models 2 and 3 and not accounting for variability in surgical time for revision THA, which likely decreased the daily surgical volume for the revision THA service line. As such, we believe our estimates are conservative and are biased towards outcomes that favor the current RVU system to be fair in compensation for revision THA.
Demographics, Description of Study Population
The mean age was older for patients undergoing head and liner exchange (66 ± 11 years), acetabular revision (65 ± 11 years), and femoral revision (67 ± 11 years) than for those undergoing primary (64 ± 11 years) or full revision (63 ± 13 years) THA (p < 0.05). The American Society of Anesthesiology score was higher for patients undergoing revision THA (ASA 3 and 4 head and liner, 53%; acetabular, 51%; femoral, 50%; full revision, 68%) than for those undergoing primary THA (ASA 3 and 4 38%; p < 0.001). There was an increased prevalence of commercial insurance among patients undergoing primary THA (primary, 45%; head and liner, 23%; acetabular, 32%; femoral, 22%; full revision, 32%), and increased prevalence of Medicare and Medicaid insurance (primary, 55%; head and liner, 75%; acetabular, 65%; femoral, 72%; full revision, 66%) in patients undergoing revision THA (p < 0.001). Surgical time was longer among patients undergoing revision THA (primary, 97 ± 32 minutes; head and liner, 111 ± 42 minutes; acetabular, 150 ± 56 minutes; femoral, 163 ± 58 minutes; full revision, 194 ± 84 minutes) than among those undergoing primary THA (p < 0.001). In addition, more patients undergoing revision THA were discharged to a skilled nursing facility than those undergoing primary THA (Table 1). Several demographic variables including sex, BMI, smoking status, and race did not vary between the cohorts (Table 1).
All patients undergoing revision THA were used for this point of care study. Data regarding demographics, implant type, and surgical time were derived from our electronic health record. All missing data from our original query were obtained through manual chart review.
Statistical Analysis, Study Size
This study was an economic modeling study of the data available to us in our electronic health records. Subgroups were defined by their surgical treatment modality. ANOVA tests were performed for patient baseline demographics. All other analyses were performed as described above. Initial analyses demonstrated differences in patient demographics between the groups. Although patient morbidity and demographics are likely to affect postoperative patient outcomes, they do not alter the RVUs awarded to each surgical procedure as described by the CMS. The deterministic financial models in this study were developed to evaluate the distribution of RVUs with respect to surgical complexity when assessed by surgical time. Therefore, we did not adjust for differences in patient demographics in the deterministic financial models. Lastly, we did not perform a sensitivity analysis in our study because the only input for uncertainty in our study was surgical time. Statistical calculations and graphical visualizations were performed using MatLab 2018a (The MathWorks Inc, Natick, MA, USA). Significance was taken as p < 0.05.
Results
Are Physicians Fairly Compensated for Revision THA on a Per-minute Basis Compared with Primary THA?
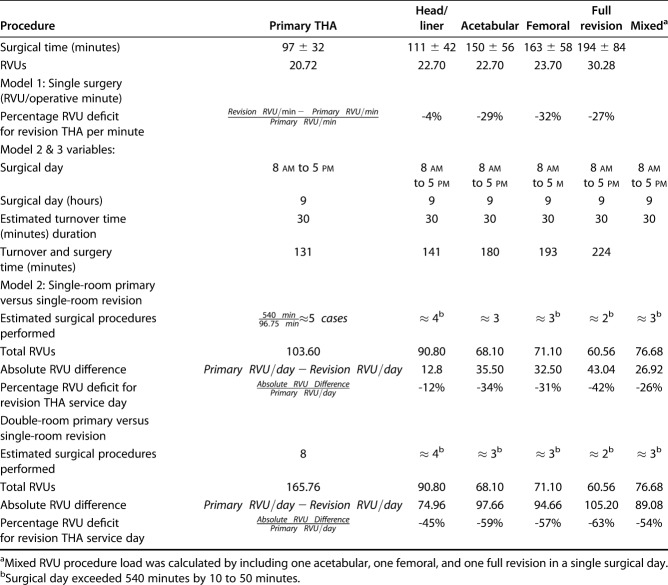
When comparing revision THA with primary THA in a model that evaluated RVU earnings on a per-minute basis, we found that surgeons performing revision THA accrued RVU deficits compared with those performing exclusively primary THA. Head and liner exchange demonstrated a 4% per minute deficit, acetabular component revision demonstrated a 29% deficit, femoral component revision demonstrated a 32% deficit, and full revision THA demonstrated a 27% deficit in revision THA (Table 2).
Table 2.
Single-room primary versus single-room revision THA
Are Physicians Fairly Compensated for Revision THA on Per-day Basis Compared with Primary THA?
Single-room Primary THA versus Single-room Revision THA (Per Day)
Under Model 2, surgeons performing exclusively revision surgery in a single-room setting accrued large RVU deficits compared with surgeons performing primary THA in a single-room setting. This resulted in a 12% RVU deficit for head and liner exchanges, 34% RVU deficit for acetabular revisions, 31% RVU deficit for femoral revisions, and 42% RVU deficit for full revisions in single-room revision THA, compared with single-room primary THA.
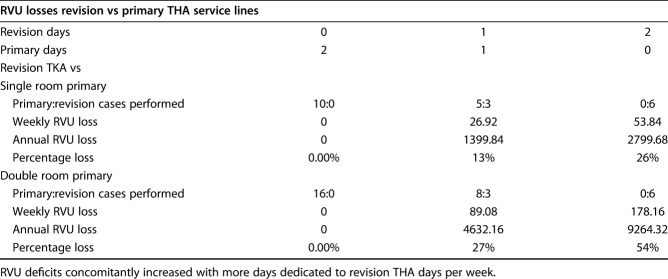
Compared with primary service lines with one room, revision surgeons lost 26% potential RVUs for an operative day with mixed surgical volume (one acetabular revision, one femoral revision and one full revision). When a single room primary THA versus revision THA with mixed surgical volume was extrapolated to a 2-day operative week, surgeons partaking in more operative days on a revision service team had a greater deficit in RVU (1-day revision service: 26.92 RVU deficits per week, or 1399.84 RVU deficits per year [13%]; 2-day revision service: 53.84 RVU deficits per week, or 2799.68 RVU deficits per year [26%] Fig. 1 and Table 3).
Fig. 1.
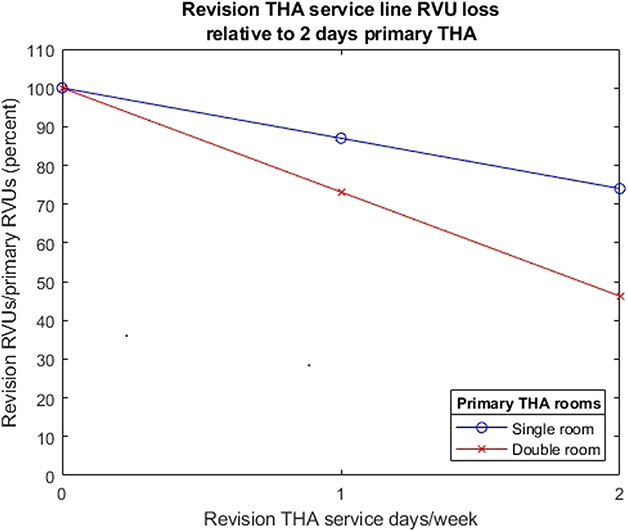
Revision THA service line potential RVU deficit for a simulated operating room week. RVU deficits concomitantly increased with more days dedicated to revision THA days per week.
Table 3.
RVU losses for a simulated calendar of 2 operating room days per week
Double-room Primary THA Versus Single-room Revision THA (Per Day)
Under a model that allowed surgeons to run two rooms for primary THA and a single room for revision THA, primary THA volume increased from five surgical procedures to eight surgical procedures per day. Revision THA volume did not change. This resulted in a 45% RVU deficit for head and liner exchanges, 59% RVU deficit for acetabular revisions, 57% deficit for femoral revisions, and 63% RVU deficit for full revisions compared with double-room primary THA.
Compared with a two-room primary THA service, revision services with a blended load (one acetabular, one femoral, and one full revision THA) experienced a decrease of 55% RVUs per day. When modeled for 2 operative days per week, participation in 1 day of the revision THA service and 1 day of primary THAs resulted in a decrease of 27% in potential RVU earnings (89.08 RVUs per week and 4632.16 RVUs per year) compared with a double-room primary THA service (Fig. 1). Surgeons partaking full-time in a revision service line (2 days per week) saw an even greater decrease in potential RVU earnings of 54% (178.16 RVUs per week; 9264.32 RVUs per year).
Discussion
Revision THA is a challenging surgical procedure, even for the arthroplasty-trained subspecialist. Although prior studies investigating compensation for revision THA compared with primary THA suggest that it may be undervalued, few if any provide precise estimates as to the magnitude that revision THA may be undervalued and how it might be affected by the surgical time or revision type [3, 16, 33, 36]. Therefore, we performed a modeling study to calculate the impact of these practice settings on RVU generation in a hypothetical primary THA service line compared with a hypothetical revision THA service line. Our models corroborated the findings of the prior studies and demonstrated revision surgeries were substantially undervalued as a function of time and complexity, potentially resulting in RVU deficits as high as 54% for surgeons dedicating two full OR days a week for revision surgeries. Even in more conservative models, comparing primary THAs to a mix of revision surgeries performed in one OR for one day, surgeons faced a deficit of 26% of their potential RVUs per day. These deficits disincentivize surgeons from performing revision surgery, potentially limiting patients access to fellowship-trained arthroplasty surgeons.
This study is not without limitations. In this study, the revision THA cohort had a greater percentage of patients who were discharged to a skilled nursing facility with a longer mean length of stay. They were also more likely to have higher American Society of Anesthesiology scores and be insured by Medicare or Medicaid, both of which have been associated with worse postoperative outcomes [5, 10, 15, 20, 23, 25]. This difference may in part be attributed to Medicare eligibility as patients undergoing revision THAs were more likely to be 65 years and older. Without the actual implementation of a revision THA service, true costs savings or losses associated with such a service can only be speculated. However, the goal of the current study was to apply historical data to elucidate why technically competent, high-volume surgeons may not be incentivized to perform a high volume of complex revision THAs.
Additionally, our model did not account for the large variability in surgical time for revision THA (primary THA ± 31.63 minutes versus revision THA ± 84.23 minutes), which can further reduce the surgical volume in an allotted operating room day. As result, it is likely that our estimates of the surgical volume and percentage deficit are conservative estimates of the true deficit of engaging in a revision THA service. Furthermore, a breakdown of surgical complexity (for example, full revision of aseptic components versus well fixed components) was not accounted for in this study because CMS does not adjust RVUs based on surgical complexity. Finally, one factor that plays a role in the operative time required to complete a revision surgery is surgeon skill and experience. In one example for TKA, the expected reduction in operative time for a surgeon after 25 years in practice was 51 minutes [26]. Although surgeon skill would offset some of the possible RVU deficit, even using our conservative model, the operative time for a full revision would need to consistently be one hour faster to be compensated equivalently to that of a primary THA on a RVU/minute basis, without considering the increased variability of revision surgery and more challenging postoperative care many of these patients need.
Are Physicians Fairly Compensated for Revision THA on a Per-minute Basis?
Our model found that surgeons performing exclusively revision THA consistently accrued per-minute RVU deficits compared with those performing exclusively primary THA, with larger deficits arising as more-complex revision procedures were considered. These results support the previous findings that the mean RVUs/minutes for primary THA are greater than those for revision THA, with a 4.2% increase in compensation for the primary group [33]. Our study goes further, breaking down the RVUs/minutes to look at each specific revision surgery type, allowing surgeons to see which specific revision types have the largest deficit and impact on overall RVU deficits. For example, performing head and liner exchanges rewards the same amount of RVUs as longer and more technically challenging acetabular and femoral revisions, resulting in a high RVU deficit for these more complex procedures. The heterogeneity and inverse relationship between surgical complexity and revision THA demonstrates the inadequacy of the current RVU system.
Are Physicians Fairly Compensated for Revision THA on a Per-day Basis Compared With Primary THA?
Surgeons performing exclusively revision surgery accrued large RVU deficits compared with both single-room or double-room primary THA models, largely due to a lower daily operative volume for all categories of revision THAs compared with primary THAs. Most notably, with a conservative estimate of eight primary THAs per day in the two-room model, our results demonstrated that four to six fewer revision THAs could be performed resulting in an RVU deficit of 54% to 63%, depending on the revision type.
Our findings reaffirm those of previous studies that illustrate the differences in reimbursement between primary and revision THA [3, 16, 33, 36]. One model evaluated individual reimbursement differences using a large national database, assuming seven primary THAs or four revision THAs could be performed each surgical day. This resulted in a difference in daily reimbursements of USD 706.58, and an annual reduction of approximately USD 113,052 for a surgeon who performs solely revision THA, similarly due to the reduction in surgical volume [36]. Another study analyzed the operative time, length of stay, and estimated blood loss in 80 patients undergoing primary THA and 76 undergoing revision THAs to determine the “percent effort” associated with the surgical aspect of each procedure. By their analysis, revision THA demonstrated a 1.66-fold greater percent effort, while the surgeon compensation was increased by 1.3-fold compared with that of primary THA [16]. These results were further corroborated in additional studies of reimbursement for revision total joint arthroplasty advocating that current payment methods are inadequate and fail to compensate for the greater time and effort seen with revision arthroplasty [3, 6, 9, 30, 36]. Our current analysis supports these authors’ findings and suggests that the current reimbursement model disincentivizes hospitals and surgeons from performing complex revision THA, especially at the volume necessary to run a dedicated revision service.
In the present analysis, revision THAs were categorized into liner exchange, acetabular revision, femoral revision, and full revision to better assess how the procedure type affects volume and reimbursements. Although Tokarski et al. [36] stratified their results by the complexity of revision, no prior study that we know of has analyzed these categories of revision distinctly. Additionally, our study accounts for fixed variables such as turnover time. However, an additional consideration, which is important for understanding the impact of a revision service line on arthroplasty-trained orthopaedic surgeons, is the use of two sequential operating rooms to decrease turnover time in a primary THA service line. This practice occurs frequently in orthopaedics and can improve operational efficiency and output while enhancing patient access to experienced surgeons without compromising the outcomes of total joint arthroplasty [24, 29, 34, 35]. However, because of the unpredictable nature of revision THA and its complexity, it would be prudent to use a single room.
Other Relevant Findings
Although it is important to reach fair compensation for revision THA, it is also imperative that the unintended consequences of increasing the RVUs associated with revision surgery be considered. Due to the budget neutrality law, any increase in RVU expenditures for physicians’ services (by more than 20 million) must be offset by decreases in payments for other services [28]. Therefore, increasing revision RVUs may result in lower primary RVUs, decreasing overall physician reimbursement and possibly shift surgeon incentive toward revision THA. This may encourage surgeons to be more liberal in their indications for revision THA. Conversely, by failing to appropriately compensate physicians for revision surgery, practices may move away from performing any revisions, instead sending them to tertiary care centers and limiting patient access to care in smaller and more rural communities. In a recent study reviewing the referral trends in revision THA over the past 10 years at a single tertiary referral institution, 83.6% of revision THAs were referred from an outside institution, indicating a large revision burden may already be present at tertiary referral centers [12].
Previous evidence suggests an advantage to surgeons who perform more revision surgeries in terms of decreased risk of re-revision surgery, decreased morbidity and mortality, lowered 90-day readmission rates and shorter operating times compared with low-volume arthroplasty surgeons [18, 19, 32]. In a setting where revision THA is fairly compensated compared with primary THAs, one or a few designated arthroplasty surgeons could perform the majority of complex revision THAs to help facilitate reproducible and improved patient outcomes. Additionally, healthcare systems may be better poised to negotiate implant pricing, which has shown success in primary THA service lines [13, 17], and develop specialized care pathways specific to revision hip arthroplasty.
The current reimbursement model does not adequately compensate surgeons for the increased time and effort required for revision THA. Our results indicate that a dedicated revision THA surgeon may experience a 54% relative reduction in RVUs per day compared with a surgeon exclusively performing primary THA in a two-room setting. Although it is important to evaluate and adjust current compensation for revision THA, an increase in RVU for these surgeries must be offset by decreasing payment for other orthopaedic services. Careful consideration must be given as to how to attribute healthcare value that incentivizes revision specialists to participate in a revision THA service line while not unfairly shifting compensation away from primary THA.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at NYU Langone Health, New York, NY, USA.
References
- 1.Baadh A, Peterkin Y, Wegener M, Flug J, Katz D, Hoffmann JC. The relative value unit: history, current use, and controversies. Curr Probl Diagn Radiol. 2016;45:128-132. [DOI] [PubMed] [Google Scholar]
- 2.Bansal A, Khatib ON, Zuckerman JD. Revision total joint arthroplasty: the epidemiology of 63,140 cases in New York State. J Arthroplasty. 2014;29:23-27. [DOI] [PubMed] [Google Scholar]
- 3.Barrack RL, Hoffman GJ, Tejeiro WV, Carpenter LJ. Surgeon work input and risk in primary versus revision total joint arthroplasty. J Arthroplasty. 1995;10:281-286. [DOI] [PubMed] [Google Scholar]
- 4.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128-133. [DOI] [PubMed] [Google Scholar]
- 5.Browne JA, Novicoff WM, D’Apuzzo MR. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014;96:e180. [DOI] [PubMed] [Google Scholar]
- 6.Bunn KJ, Isaacson MJ, Ismaily SK, Noble PC, Incavo SJ. Quantifying and predicting surgeon work effort for primary and revision total knee arthroplasty. J Arthroplasty. 2016;31:59-62. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services. PFS relative value files. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files. Accessed January 4, 2020.
- 8.Courtney PM, Ashley BS, Hume EL, Kamath AF. Are bundled payments a viable reimbursement model for revision total joint arthroplasty? Clin Orthop Relat Res. 2016;474:2714-2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crowe JF, Sculco TP, Kahn B. Revision total hip arthroplasty: hospital cost and reimbursement analysis. Clin Orthop Relat Res . 2003;413:175-182. [DOI] [PubMed] [Google Scholar]
- 10.Cullen DJ, Apolone G, Greenfield S, Guadagnoli E, Cleary P. ASA physical status and age predict morbidity after three surgical procedures. Ann Surg. 1994;220:3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halpern MT, Kurtz SM, Mowat FS, Ong KL, Chan N, Lau E. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2006;446:22-28. [DOI] [PubMed] [Google Scholar]
- 12.Haynes JA, Stambough JB, Sassoon AA, Johnson SR, Clohisy JC, Nunley RM. Contemporary Surgical Indications and Referral Trends in Revision Total Hip Arthroplasty: A 10-Year Review. J Arthroplasty. 2016;31:622–625. [DOI] [PubMed] [Google Scholar]
- 13.Healy WL, Iorio R, Lemos MJ, Patch DA, Pfeifer BA, Smiley PM, Wilk RM. Single price/case price purchasing in orthopaedic surgery: Experience at the Lahey Clinic. J Bone Joint Surg Am. 2000;82:607–612. [DOI] [PubMed] [Google Scholar]
- 14.Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R. Provider volume of total knee arthroplasties and patient outcomes in the HCUP-Nationwide Inpatient Sample. J Bone Joint Surg Am. 2003;85:1775-1783. [DOI] [PubMed] [Google Scholar]
- 15.Hinman A, Bozic KJ. Impact of payer type on resource utilization, outcomes and access to care in total hip arthroplasty. J Arthroplasty. 2008;23:9-14. [DOI] [PubMed] [Google Scholar]
- 16.Isaacson MJ, Bunn KJ, Noble PC, Ismaily SK, Incavo SJ. Quantifying and predicting surgeon work input in primary vs revision total hip arthroplasty. J Arthroplasty. 2016;31:1188-1193. [DOI] [PubMed] [Google Scholar]
- 17.Iorio R, Clair AJ, Inneh IA, Slover JD, Bosco JA, Zuckerman JD. Early Results of Medicare’s Bundled Payment Initiative for a 90-Day Total Joint Arthroplasty Episode of Care. J Arthroplasty . 2016;31:343–350. [DOI] [PubMed] [Google Scholar]
- 18.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909-1916. [DOI] [PubMed] [Google Scholar]
- 19.Khatod M, Cafri G, Inacio MCS, Schepps AL, Paxton EW, Bini SA. Revision total hip arthoplasty: factors associated with re-revision surgery. J Bone Joint Surg Am . 2015;97:359-366. [DOI] [PubMed] [Google Scholar]
- 20.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995:150-159. [PubMed] [Google Scholar]
- 21.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am . 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 22.Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, Kärrholm J, Garellick G, Havelin LI, Furnes O, Malchau H, Lau E. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89:144-151. [DOI] [PubMed] [Google Scholar]
- 23.LaPar DJ, Bhamidipati CM, Mery CM, Stukenborg GJ, Jones DR, Schirmer BD, Kron IL, Ailawadi G. Primary payer status affects mortality for major surgical operations. Ann Surg. 2010;252:544-550; discussion 550-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levin PE, Moon D, Payne DE. Overlapping and concurrent surgery: a professional and ethical analysis. J Bone Joint Surg Am. 2017;99:2045-2050. [DOI] [PubMed] [Google Scholar]
- 25.Martin CT, Callaghan JJ, Liu SS, Gao Y, Warth LC, Johnston RC. Disparity in total joint arthroplasty patient comorbidities, demographics, and postoperative outcomes based on insurance payer type. J Arthroplasty. 2012;27:1761-1765.e1. [DOI] [PubMed] [Google Scholar]
- 26.Maruthappu M, Duclos A, Zhou CD, Lipsitz SR, Wright J, Orgill D, Carty MJ. The impact of team familiarity and surgical experience on operative efficiency: a retrospective analysis. J R Soc Med . 2016;109:147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGrory BJ, Etkin CD, Lewallen DG. Comparing contemporary revision burden among hip and knee joint replacement registries. Arthroplast Today. 2016;2:83-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medicare Physician Payment Formula Primer. Am. Acad. Orthop. Surg. Available at: https://www.aaos.org/CustomTemplates/Content.aspx?id=22519&ssopc=1. Accessed January 4, 2020. [Google Scholar]
- 29.Padegimas EM, Hendy BA, Lawrence C, Devasagayaraj R, Zmistowski BM, Abboud JA, Lazarus MD, Williams GR, Namdari S. An analysis of surgical and nonsurgical operating room times in high-volume shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:1058-1063. [DOI] [PubMed] [Google Scholar]
- 30.Peterson J, Sodhi N, Khlopas A, Piuzzi NS, Newman JM, Sultan AA, Stearns KL, Mont MA. A comparison of relative value units in primary versus revision total knee arthroplasty. J Arthroplasty. 2018;33:S39-S42. [DOI] [PubMed] [Google Scholar]
- 31.Ritter MA. Simultaneous knee replacement is better for the patient. Orthopedics. 1998;21:415-418. [DOI] [PubMed] [Google Scholar]
- 32.Sharkey PF, Shastri S, Teloken MA, Parvizi J, Hozack WJ, Rothman RH. Relationship between surgical volume and early outcomes of total hip arthroplasty: Do results continue to get better? J Arthroplasty. 2004;19:694–699. [DOI] [PubMed] [Google Scholar]
- 33.Sodhi N, Piuzzi NS, Khlopas A, Newman JM, Kryzak TJ, Stearns KL, Mont MA. Are we appropriately compensated by relative value units for primary vs revision total hip arthroplasty? J Arthroplasty . 2018;33:340-344. [DOI] [PubMed] [Google Scholar]
- 34.Suarez JC, Al-Mansoori AA, Borroto WJ, Villa JM, Patel PD. The practice of overlapping surgery is safe in total knee and hip arthroplasty. JB JS Open Access. 2018;3:e0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sun E, Mello MM, Rishel CA, Vaughn MT, Kheterpal S, Saager L, Fleisher LA, Damrose EJ, Kadry B, Jena AB, Kooij F, Wilczak J, Soto R, Berris J, Price Z, Urman RD, Lins S, Harris JM, Cummings KC, Berman MF, Nanamori M, Adelman BT, Wedeven C, Bittner EA, LaGorio J, McCormick PJ, Tom S, Aziz MF, Coffman T, Ellis TA, Molina S, Peterson W, Mackey SC, Van Klei WA, Mahajan A, Jameson LC, Biggs DA, Neuman MD, Craft RM, Pace NL, Paganelli WC, Durieux ME, Nair BJ, Wanderer JP, Miller SA, Helsten DL, Turnbull ZA, Schonberger RB. Association of overlapping surgery with perioperative outcomes. JAMA. 2019;321:762-772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tokarski AT, Deirmengian CA, Lichstein PM, Austin MS, Deirmengian GK. Medicare fails to compensate additional surgical time and effort associated with revision arthroplasty. J Arthroplasty. 2015;30:535-538. [DOI] [PubMed] [Google Scholar]