Abstract
Background
When conservative treatments do not work, TKA may be the best option for patients with knee osteoarthritis, although a relatively large proportion of individuals do not have clinically important improvement after TKA. Evidence also suggests that women are less likely to benefit from TKA than men, but the reasons are unclear. Widespread pain disproportionately affects women and has been associated with worse outcomes after joint arthroplasty, yet it is unknown if the effect of widespread pain on TKA outcomes differs by patient gender.
Questions/purposes
(1) Does the association between widespread pain and no clinically important improvement in osteoarthritis-related pain and disability 2 years after TKA differ between men and women? (2) Does the use of pain medications 2 years after TKA differ between those with widespread pain and those without widespread pain before surgery?
Methods
Osteoarthritis Initiative (https://nda.nih.gov/oai/) study participants were followed annually from March 2005 until October 2015. Participants who underwent TKA up to the 7-year follow-up visit with pain/disability assessment at the protocol-planned visit before TKA and at the second planned annual visit after surgery were included in the analysis. Among 4796 study participants, 391 had a confirmed TKA, including 315 with pain/disability assessment at the protocol-planned visit before TKA. Overall, 95% of participants (298) had the required follow-up assessment; 5% (17) did not have follow-up data. Widespread pain was defined based on the modified American College of Rheumatology criteria. Symptoms were assessed using the WOMAC pain (range 0 to 20; higher score, more pain) and disability (range 0 to 68; higher score, more disability) scores, and the Knee Injury and Osteoarthritis Outcome Score for pain (range 0 to 100; higher score, less pain). Improvements in pain and disability were classified based on improvement from established clinically important differences (decrease in WOMAC pain ≥ 1.5; decrease in WOMAC disability ≥ 6.0; increase in Knee Injury and Osteoarthritis Outcome Score for pain ≥ 9). At baseline, more women presented with widespread pain than men (45% [84 of 184] versus 32% [36 of 114]). Probability and the relative risk (RR) of no clinically important improvement were estimated using a logistic regression analysis in which participants with widespread pain and those without were compared. The analyses were done for men and women separately, then adjusted for depression and baseline outcome scores.
Results
Among women, preoperative widespread pain was associated with an increased risk of no clinically important improvement 2 years after TKA, based on WOMAC pain scores (13.5% versus 4.6%; RR 2.93 [95% CI 1.18 to 7.30]; p = 0.02) and the Knee Injury and Osteoarthritis Outcome Score for pain (16.5% versus 4.9%; RR 3.39 [95% CI 1.34 to 8.59]; p = 0.02). Given the lower and upper limits of the confidence intervals, our data are compatible with a broad range of disparate associations between widespread pain and lack of clinically important improvement in WOMAC pain scores (RR 0.77 [95% CI 0.22 to 2.70]; p = 0.68) and the Knee Injury and Osteoarthritis Outcome Score for pain (RR 1.37 [95% CI 0.47 to 4.00]; p = 0.57) among men, as well as clinically important improvement in WOMAC disability scores among men (RR 0.72 [95% CI 0.20 to 2.55]; p = 0.61) and women (RR 1.98 [95% CI 0.92 to 4.26]; p = 0.08). Participants presenting with widespread pain before TKA were more likely than those without widespread pain to use medication for symptoms of knee osteoarthritis most days for at least 1 month 2 years after TKA (51% [61 of 120] versus 32% [57 of 178]; mean difference, 18.8 [95% CI 7.3 to 30.1]; p < 0.01).
Conclusions
Widespread pain before TKA was associated with an increased risk of no clinically important improvement in knee pain 2 years postoperatively among women. Because of the small number of men with widespread pain in the sample, the results for men were inconclusive. In clinical practice, screening TKA candidates for widespread pain may be useful, and expectations of surgical outcomes may need to be tempered if patients have a concurrent diagnosis of widespread pain. Future studies should include more men with widespread pain and investigate if treatment of widespread pain before or concurrent with TKA surgery may improve surgical outcomes.
Level of Evidence
Level III, therapeutic study.
Introduction
Osteoarthritis is a leading cause of disability among elderly people in the United States [24], and in the Global Burden of Disease study of 291 conditions, hip and knee osteoarthritis was ranked as the 11th highest contributor to global disability [9]. When nonoperative management of knee osteoarthritis does not work, TKA is recommended [42]. Although TKA is performed frequently, has been shown to be cost effective, and is associated with improvement in osteoarthritis-related pain and function, a relatively large proportion of patients do not have major improvement in pain and function after surgery [13, 20, 21, 37]. In a recent US study, approximately 70% of participants had clinical improvement, based on improvement in the WOMAC score 1 year after TKA [37]. In a Canadian study using the same criterion, only 52% of patients who underwent TKA had improvement [20]. Evidence also suggests that women may be less likely to benefit from TKA than men [10, 14, 27]. This potential gender-associated disparity in the effectiveness of treatment for end-stage osteoarthritis is particularly troubling given the higher prevalence of symptomatic and radiographic knee osteoarthritis in women [12, 35].
The reasons why women are less likely to have improvement in pain and disability after TKA than men are unclear [10, 14, 27]. Large-scale epidemiologic studies have found that women more frequently report chronic musculoskeletal pain than men [16]. Gerdle et al. [18] found that women had a higher prevalence of pain in 10 different anatomic regions and had a much higher prevalence of widespread pain than did men. The prevalence of several common chronic pain conditions (for example, fibromyalgia, migraine, and tension headache) is also greater for women than for men [16]. Although chronic widespread pain and fibromyalgia are often used interchangeably, patients with fibromyalgia represent only a subgroup of those with chronic widespread pain [7]. Regardless, both chronic widespread pain and fibromyalgia disproportionately affect women [3, 7, 8, 18]. Greater widespread pain was also associated with worse post-joint arthroplasty outcomes in a limited number of studies [5, 11, 20, 29, 41]. It is not known whether gender-associated differences in TKA outcomes are related to mechanisms underlying widespread pain.
We therefore asked: (1) Does the association between widespread pain and no clinically important improvement in osteoarthritis-related pain and disability 2 years after TKA differ between men and women? (2) Does the use of pain medications 2 years after TKA differ between those with widespread pain and those without widespread pain before surgery?
Patients and Methods
Study Design, Setting, and Participants
This is a retrospective study that draws data from the Osteoarthritis Initiative, a multicenter, longitudinal observational study with publicly available detailed protocols and data releases (https://nda.nih.gov/oai/). Individuals aged 45 to 79 years at risk of having or with symptomatic knee osteoarthritis were recruited from four clinical centers (University of Maryland School of Medicine and the Johns Hopkins University [Baltimore, MD, USA], The Ohio State University [Columbus, OH, USA], University of Pittsburgh [Pittsburgh, PA, USA] and Memorial Hospital of Rhode Island [Pawtucket, RI, USA]) and examined annually.
The Osteoarthritis Initiative enrolled participants between 2004 and 2006. The aim of the current study was to examine outcomes 2 years after TKA, and the Osteoarthritis Initiative follow-up data are available through the 9-year follow-up visit; thus participants who underwent TKA up to the 7-year follow-up visit were selected for analysis. We did not include partial knee arthroplasties. The Osteoarthritis Initiative coordinating center confirmed receipt of TKA based on medical records and/or radiographs. If a participant underwent more than one TKA during the follow-up period, we selected the first replaced knee for outcome analysis. If both knees were replaced on the same day, we randomly selected one knee.
We included participants in the analysis if they had an assessment of knee pain and disability at the protocol-planned visit before TKA (T0) and at a second planned annual visit after surgery (T + 2) (see Fig. 1, Supplemental Digital Content 3, http://links.lww.com/CORR/A248). Widespread pain assessment (described below) was also required at the visit before surgery (T0) for inclusion in the analysis. However, if the annual visit before TKA was performed via telephone and did not include a complete assessment of body pain, the widespread pain assessment at the clinic visit 1 year before TKA was used (T-1).
Fig. 1.
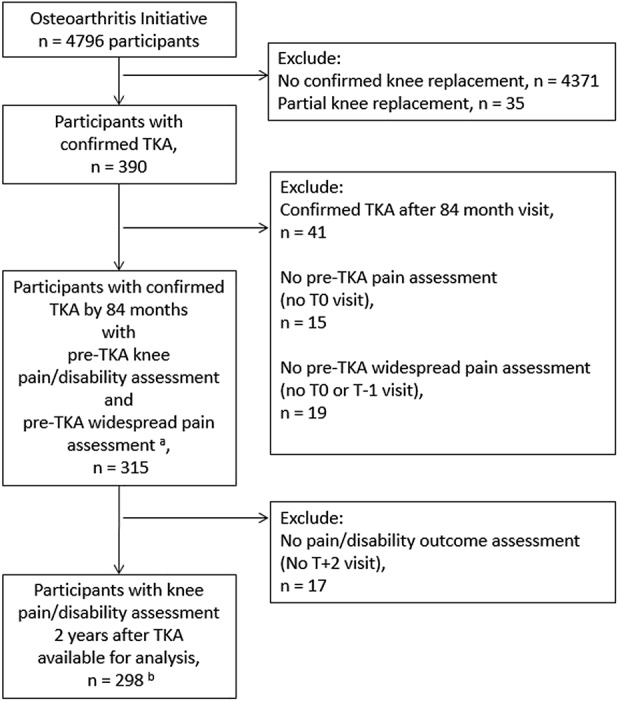
Sample selection flow diagram is shown here. T0 is the clinic visit before TKA; T+2 is the visit 2 years later. aT-1 assessment of widespread pain is used when T0 is a telephone examination, because telephone examinations do not include an assessment of widespread pain. bThe available sample size varies for different outcomes because of both missing values and lack of opportunity to improve (pre-TKA score too low to have potential for clinically important improvement) based on variable-specific definitions of clinically important improvement (sample sizes for each analysis: WOMAC pain: 284 [one missing; 13 cannot improve], WOMAC disability: 271 [seven missing; 20 cannot improve], pain severity in the past 7 days: 281 [four missing; 13 cannot improve], and Knee Injury and Osteoarthritis Outcome Score pain score: 297 [one missing]).
Among 4796 Osteoarthritis Initiative participants, 390 underwent at least one confirmed TKA during the follow-up period (March 2005 to October 2015). We excluded 41 participants with TKA after 84 months (that is, no planned clinic visit 2 years after TKA), 15 participants with no pre-TKA assessment of pain and disability (T0), and 19 participants with no pre-TKA assessment of widespread pain at either T0 or T-1, leaving 315 eligible participants. Among the eligible participants, those without an outcome assessment of knee pain or disability at the second protocol-planned visit after TKA (T + 2) were excluded (5%, 17 of 315 participants), leaving 298 participants available for an analysis of TKA outcomes (Fig. 1).
Primary Outcomes
Pain and disability were assessed at the Osteoarthritis Initiative visit immediately before TKA (T0) as well as at the Osteoarthritis Initiative visit 2 years after TKA (T + 2). The WOMAC index, a 24-item questionnaire, is a reliable and validated measure that consists of three different subscales of osteoarthritis-related disease severity: pain (0 to 20), stiffness (0 to 8), and disability (0 to 68) [2], with higher scores indicating greater disease severity. The Knee Injury and Osteoarthritis Outcome Score, also a reliable and validated measure of osteoarthritis-related disease severity, is a 42-item questionnaire that includes a pain measure ranging from 0 to 100, with 100 indicating no pain [34]. The severity of knee pain at its worst in the past 7 days was reported using a numerical rating scale (range 0 to 10).
Clinically important improvement from T0 to T + 2 was defined as reduction in the WOMAC pain score greater than or equal to the minimum clinically important difference proposed by Angst et al. [1] (1.5 on a 0-20 scale). The following definitions of clinically important improvement were also considered: reduction in the 7-day pain severity numerical rating scale score greater than or equal to the clinically important difference proposed by Farrar et al. [15] (1.7 on a 0 to 10 scale); minimal clinically important increase in Knee Injury and Osteoarthritis Outcome Score for pain proposed by Roos and Lohmander [33] (9 on a 0 to 100 scale); and reduction in the WOMAC disability score greater than or equal to the minimum clinically important difference proposed by Tubach et al. [36] (6.0 on a 0 to 68 scale).
Secondary Outcomes
Any use of medication, including both prescription and over-the-counter, for pain, aching, or stiffness in either knee during the past 12 months and on most days for at least 1 month during the past 12 months was self-reported at annual visits. Specific medications used for joint pain or arthritis on most days during the past 30 days were also reported. Medication use specifically for the left rather than the right knee and vice versa was not determined. To evaluate change in medication use, we compared the strongest class of pain medication reported at the visit before TKA and 2 years postoperatively. We classified continued use of medication as a medication in the same category or stronger, compared with a weaker class, based on the following hierarchy: acetaminophen, over-the-counter NSAIDs, prescription NSAIDs or cyclooxygenase-2 selective inhibitors, and strong prescription pain medications, including opioids (see Table 1; Supplemental Digital Content 1, http://links.lww.com/CORR/A246).
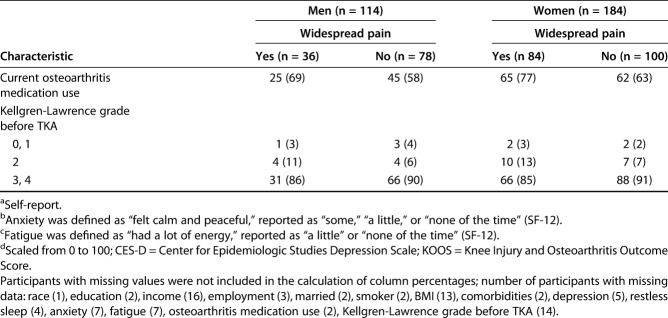
Table 1.
Participant characteristics and widespread pain status before TKA
Widespread Pain
The 1990 American College of Rheumatology Criteria for the Classification of Fibromyalgia defined widespread pain as “pain that affects both sides of the body both above and below the waist, including some part of the axial skeleton” [40]. We adapted this definition of widespread pain based on available Osteoarthritis Initiative data. Widespread pain was defined in a similar manner as in other studies [6, 32]. The Osteoarthritis Initiative questionnaire included a homunculus figure for participants to indicate the presence of pain, aching, or stiffness in various joints of the body on most days during the past 30 days (see Fig. 2, Supplemental Digital Content 4, http://links.lww.com/CORR/A249). The homunculus figure, combined with specific back, hip, and knee questions, facilitated identification of pain symptoms in the joint areas surveyed. To meet the definition of widespread pain used in this study, a study participant had to report pain in a minimum of at least one joint area in each of the following five body regions: right hand, wrist, elbow, or shoulder (the right upper body region); left hand, wrist, elbow, or shoulder (the left upper body region); right hip, knee, ankle, or foot (the right lower body region); left hip, knee, ankle, or foot (the left lower body region); and in the neck, upper back, middle back, or lower back (the axial region). All questions addressed symptoms in the past 30 days, with the exception of hip-specific questions, which asked about symptoms on most days for at least 1 month during the past 12 months. Research technicians recorded the responses electronically based on the marked homunculus figures and responses to hip and knee questions. Widespread pain was then categorized using the American College of Rheumatology Criteria for the Classification of Fibromyalgia definition of widespread pain.
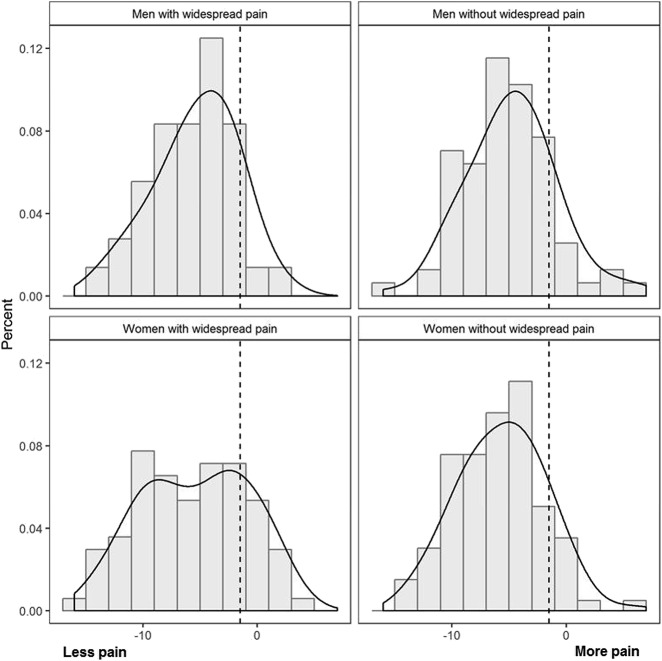
Fig. 2.
Histograms with density estimate for change in WOMAC pain scores from T0 to T+2 are shown here. Levene’s test for homogeneity of variance for absolute deviations from group means, p = 0.0076.
Participant Characteristics
Sociodemographic information collected at baseline included age, gender, race, educational attainment, income, marital status, and smoking status. The Katz-modified Charlson Comorbidity questionnaire [22] was administered at annual or biennial clinic visits, and employment status was self-reported. Body weight was measured by trained examiners at annual or biennial clinic visits, and BMI was categorized based on the World Health Organization’s criteria. Knee radiographs from clinic visits were centrally read and scored using the Kellgren-Lawrence grading system [23].
Mental health was assessed using the SF-12 [39] and the validated Center for Epidemiologic Studies Depression Scale [30] at all clinic visits. Restless sleep was assessed by response to the Center for Epidemiologic Studies Depression Scale item “My sleep was restless”: less than 1 day, 1 to 2 days, 3 to 4 days, and 5 to 7 days. Anxiety was categorized based on the participant’s response to the SF-12 item “How much time during the past 4 weeks have you felt calm and peaceful?”, while fatigue was categorized based on the response to the SF-12 item “How much time during the past 4 weeks did you have a lot of energy?” Response choices for both questions were none, a little, some, most, or all of the time. For all participant characteristics, we reported the measures and radiographic scores collected at the annual study clinic visit before TKA.
Women presented with widespread pain before TKA more often than men (45% [84 of 184 participants] versus 32% [36 of 114 participants]). Among both men and women, participants with widespread pain were more often employed and obese and more likely to report fatigue. Black race and annual income of less than USD 50,000 per year were more common among women with widespread pain than among women without widespread pain. Men without widespread pain had greater comorbidities than men with widespread pain in our sample. WOMAC pain and disability scores before TKA were on average higher among women with widespread pain (42 and 41, respectively) than among women without widespread pain (37 and 34, respectively), while the differences were less remarkable among men (Table 1).
Statistical Analysis
Participant characteristics were summarized using means and SDs for continuous measures and numbers and percentages for categorical variables for those with widespread pain and those without widespread pain before TKA, and separately for men and women, to identify potential sources of confounding in our sample.
To answer our first question, we estimated the probability of no clinically important improvement 2 years after the before-TKA assessment of pain and disability for participants with and without widespread pain. Logistic regression was used to estimate the probability of the outcome conditional on covariates. The conditional probabilities were marginalized over the covariate distributions and used to estimate relative risk (RR) and 95% CIs [28]. For each outcome-specific analysis, we excluded participants with pain and disability scores lower than the established clinically important improvement criteria before TKA because there was no potential for improvement given the definitions of improvement. We obtained RR estimates from an adjusted model, which included only the strongest covariates based on model fit and likelihood ratio statistics, specifically depression and the measure-specific pain and disability scores before TKA [38]. Also, we estimated RRs from a fully-adjusted model that additionally included age, race, education, income, marital status, BMI, comorbidities, and use of medication for knee pain before TKA, to address concerns about other potential sources of confounding (see Table 2, Supplemental Digital Content 2, http://links.lww.com/CORR/A247). In the adjusted models, probabilities were estimated using the mean value of the continuous covariates (Center for Epidemiologic Studies Depression Scale score, baseline score, age, and BMI) and the most common category of the remaining categorical variables. We tested for an interaction between widespread pain and gender by including an interaction term in each logistic regression model.
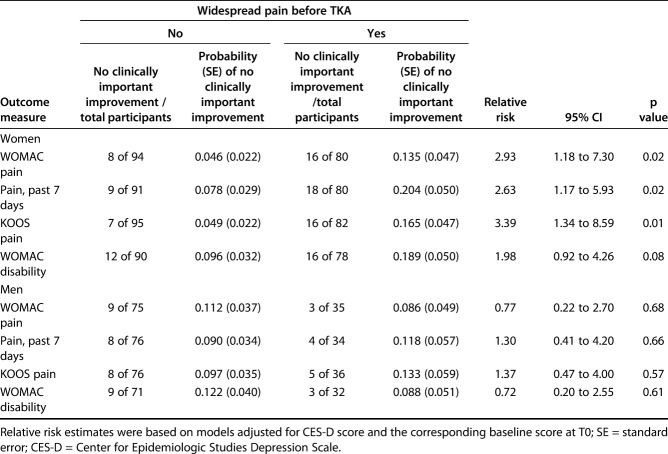
Table 2.
Widespread pain before TKA and estimated probability of no clinical improvement 2 years later
We demonstrated the distribution of change in pain and disability measures from the visit before TKA to 2 years postoperatively using histograms with kernel density estimates to visualize the spectrum of post-TKA pain and disability outcomes. The established clinically important difference was superimposed for reference. We created histograms for gender separately for participants with and without widespread pain. Levene’s test for homogeneity of variance was conducted to test the null hypothesis that the population variances are equal.
The proportions of participants reporting medication use 2 years after TKA (T + 2) for pain, aching, or stiffness in either knee in the past 12 months and medication use on most days for at least 1 month during the past 12 months were reported for participants with and without widespread pain before TKA, and the difference in proportions was provided with exact 95% CIs to answer our second question. Continued use of medication in the same class or stronger compared with a weaker class 2 years after TKA was similarly compared between participants with and without widespread pain before TKA in a restricted sample that excluded those who did not take pain medication before TKA.
A p value less than 0.05 was considered statistically significant. All analyses were performed using SAS® version 9.4 (SAS Institute Inc, Cary, NC, USA) or Stata version 15.0 (StataCorp LP, College Station, TX, USA).
Results
Gender, Widespread Pain, and Clinically Important Improvement After TKA
Among women, widespread pain before TKA was associated with an increased risk of no clinical improvement 2 years after TKA, based on WOMAC pain score (13.5% versus 4.6%; RR 2.93 [95% CI 1.18 to 7.30]; p = 0.02), 7-day numerical rating scale pain severity score (20.4% versus 7.8%; RR 2.63 [95% CI 1.17 to 5.93] ; p = 0.02), and the Knee Injury and Osteoarthritis Outcome Score for pain (16.5% versus 4.9%; RR 3.39 [95% CI 1.34 to 8.59]; p = 0.01) after adjustment for Center for Epidemiologic Studies Depression Scale score and baseline outcome measure score. Only 36 of 114 men presented with widespread pain, precluding precise estimation (Table 2). Among the men in our study, data were compatible with a wide range of effect sizes given the lower and upper limits of the confidence intervals for associations between pre-TKA widespread pain and lack of clinical improvement in WOMAC score, 7-day pain severity score, and the Knee Injury and Osteoarthritis Outcome Score for pain 2 years postoperatively; thus, considerable uncertainty remains regarding any potential associations between widespread pain in men and TKA outcomes.
Further, our data were compatible with a broad range of effect sizes for the association between widespread pain and clinically important improvement in WOMAC disability scores among men (RR 0.72 [95% CI 0.20 to 2.55]; p = 0.61) and women (RR 1.98 [95% CI 0.92 to 4.26]; p = 0.08), given the lower and upper limits of the confidence intervals (Table 2). The test for interaction between widespread pain and gender in adjusted models did not provide evidence that the association between widespread pain and each outcome measure differs between women and men (data not shown).
Two years after TKA, the distribution of change in WOMAC pain score had greater variance among women with widespread pain than among women without widespread pain, with a greater proportion reporting no clinically important improvement (Fig. 2). We did not observe this difference when we compared men with widespread pain and those without. We did not observe differences in the variance for the distribution of change in WOMAC disability scores (see Fig. 3, Supplemental Digital Content 5, http://links.lww.com/CORR/A250) and numerical rating scale scores for pain severity (see Fig. 4, Supplemental Digital Content 6, http://links.lww.com/CORR/A251).
The proportion of participants who reported no clinical improvement in pain 2 years after TKA ranged from 14% to 16% for women and 11% to 13% for men, based on WOMAC pain scores, the Knee Injury and Osteoarthritis Outcome Score for pain, and numerical rating scale scores for pain severity. In all, 17% of women and 12% of men reported no clinically important improvement in WOMAC disability score 2 years after TKA.
Widespread Pain and Pain Medication Use 2 Years after TKA
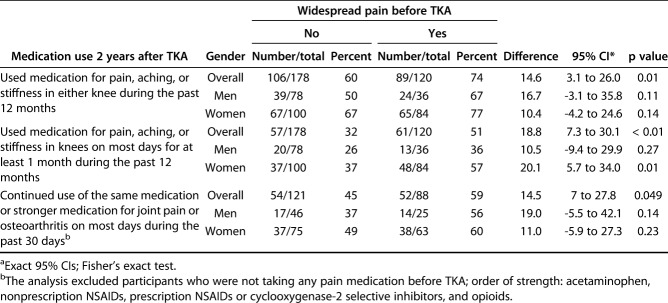
Two years after TKA, any use of medication for pain, aching, or stiffness in either knee during the past 12 months was more frequent among participants presenting with widespread pain than those without widespread pain before TKA (74% versus 60%; mean difference 14.6 [95% CI 3.1 to 26.0]; p = 0.01) (Table 3). Use of medication for pain, aching, or stiffness in the knees on most days for at least 1 month during the past 12 months was also more frequent among participants who initially presented with widespread pain than those without widespread pain (51% versus 32%; mean difference, 18.8 [95% CI 7.3 to 30.1]; p < 0.002). Among participants who reported using pain medication before TKA, continued use of the same medication or a stronger medication for joint pain or arthritis on most days during the past 30 days was also more common among those with widespread pain than those without widespread pain (59% versus 45%; mean difference, 14.5 [95% CI 0.7 to 27.8]; p = 0.049).
Table 3.
Medication use 2 years after TKA
Discussion
Women may be less likely to benefit from joint arthroplasty than men [10, 14, 27]. Chronic widespread pain is also more frequently observed in women than in men [3, 7, 8, 18]. However, from these previous studies it is unknown if the association between widespread pain and TKA outcomes differs by gender. In this observational study of participants with knee osteoarthritis, women who presented with widespread pain before TKA had approximately twice the risk of no clinically important improvement in knee pain at 2 years of follow-up compared with women without widespread pain. Notably, 80% of women with widespread pain reported clinically important improvement. Among men, no evidence of an association between widespread pain and no clinically important improvement was observed. However, few men in our sample had widespread pain, thus limiting our conclusions regarding men. We were not able to demonstrate an association between widespread pain and clinical improvement in osteoarthritis-related disability among women and men. Preoperative widespread pain was associated with a higher rate of analgesic use for arthritis symptoms 2 years after TKA.
Limitations
Our study has a few limitations. First, the relatively small number of men with widespread pain in the sample limits our ability to draw conclusions about men with widespread pain. A sample that includes more men with widespread pain is needed to examine TKA outcomes in this subgroup. Second, the definition of widespread pain we used was based on the 1990 American College of Rheumatology Criteria for the Classification of Fibromyalgia rather than the more recent (2010-2011) definition of widespread pain, although the 1990 American College of Rheumatology Criteria for the Classification of Fibromyalgia has been used in many previous studies [3, 6, 8, 18, 26, 32]. Pain symptoms were identified based on joint areas, rather than whole body areas, also a strategy that was used in other studies on widespread pain [6, 32]. Regardless, our definition of widespread pain may not be comparable to how others may have defined the term in previous investigations. Third, there is variability in the timing of the clinic assessment of widespread pain, knee pain and disability relative to the actual TKA date, given that clinic visits were conducted annually per the Osteoarthritic Initiative protocol, although this has not been shown to be an important determinant of osteoarthritis-related pain and disability after TKA [37]. Fourth, postoperative use of medication for osteoarthritis was not necessarily specific to the knee that underwent TKA and could have been used for osteoarthritis symptoms in other joints. However, participants in this cohort were most likely using analgesic medication before surgery to primarily treat their most symptomatic joint that eventually underwent surgical replacement. Fifth, while self-reported medication use may be susceptible to recall and/or social desirability bias, questionnaires which measure medication use behavior generally exhibit high concordance with non-self-report methods [17].
Gender, Widespread Pain, and Clinically Important Improvement After TKA
Our results confirm previous findings that widespread pain is associated with worse pain outcomes after joint arthroplasty, specifically among women [5, 11, 20, 29, 41]. In a study of 1294 patients who underwent hip or knee replacement surgery, the number of pain problems elsewhere (joint and nonjoint) was an independent determinant of persistent pain after joint arthroplasty [41]. In another study, painful or problematic ankles, feet, or toes were associated with worse postsurgical WOMAC pain and physical function scores [29]. A study that followed the course of knee and hip arthroplasty patients over 6 months demonstrated that a higher fibromyalgia survey score was an important predictor that a patient would not achieve at least 50% improvement in WOMAC pain scores after undergoing joint arthroplasty [5]. Finally, a more recent study found that more body pain was associated with the inability to achieve minimal clinically important improvement after TKA [11]. Of note, our study has important distinctions and builds on these previous findings. Postoperative assessment of clinical outcomes ranged between 6 months and 1 year in most of these studies [5, 11, 20, 29], while we assessed participants roughly 2 years after TKA. This is particularly relevant because improvement from TKA plateaus at approximately 18 months after surgery [31]. In addition, research participants were recruited from four distinct regions across the United States, extending the generalizability of our findings. Most importantly, none of the previous studies that reported an association between widespread pain and TKA outcomes examined potential differences by gender [5, 11, 20, 29, 41].
The clinical implications of our study findings are substantial. A homunculus figure or a fibromyalgia survey to measure preoperative widespread pain can be used/completed readily and easily by patients. Surgeons and clinicians may consider using such tools in practice to identify people at risk of little or no improvement in pain and disability after undergoing TKA [5, 11]. Patients’ and clinicians’ expectations of surgical outcomes may need to be tempered if patients have a concurrent diagnosis of widespread pain or other common chronic pain conditions. The presence of widespread pain should neither be a contraindication for TKA nor be used to screen potential candidates for TKA, however. Even among women with widespread pain in our study, approximately 80% reported clinically important improvement; therefore, widespread pain clearly does not preclude having improvement in osteoarthritis-related pain and disability after TKA. Moreover, TKA candidates with widespread pain may benefit from preprocedural therapies targeting centralized pain [7]. Centrally acting drugs (for example, serotonin and norepinephrine reuptake inhibitors and gabapentin) and exercise therapy can improve the effect of endogenous analgesia, while cognitive behavioral therapy may target cognitive-emotional sensitization in patients with osteoarthritis [25].
Widespread Pain and Pain Medication Use 2 Years after TKA
Widespread pain has been linked to greater analgesic use shortly after joint arthroplasty [4, 19]. A study suggested that patients with higher fibromyalgia survey scores consumed more opioids in the acute postoperative period after joint arthroplasty [4]. Another study showed that greater overall body pain preoperatively was independently associated with persistent opioid use 6 months after TKA and THA [19]. In our study, the difference in medication use for participants with widespread pain compared with those who did not have widespread pain was evident up to 2 years after TKA.
Conclusions
Our study suggests that women presenting with widespread pain may be at an increased risk of having no clinically important improvement in knee pain 2 years after surgery compared with women without widespread pain. Although we did not find similar evidence of an increased risk of no clinically important improvement after TKA among men with widespread pain, few men in our sample presented with widespread pain, thus limiting our ability to draw inferences for men. Screening TKA candidates for widespread pain, especially women, may be helpful in setting expectations for a wide range of outcomes after joint arthroplasty, and identifying candidates for widespread pain treatment, including medications, exercise, and/or cognitive behavioral therapy. Our findings offer a potential explanation for previously reported gender-associated disparities in TKA outcomes [10, 14, 27]. We confirmed previous reports that widespread pain before TKA is associated with more analgesic use after TKA [4, 19] and with a greater follow-up time than previously reported. Treatment of widespread pain preoperatively or concurrently with TKA and recovery may improve the chance of clinically important improvement in pain and disability postoperatively and should be investigated further in future studies.
Supplementary Material
Acknowledgments
We thank all Osteoarthritis Initiative participants, study staff, and investigators.
Footnotes
The institution of one or more of the authors (EV, CK) has received, during the study period, funding from the National Institutes of Health (NIH)/National Institute of Arthritis and Musculoskeletal and Skin Diseases (award numbers K23AR067226 and R01AR066601, respectively). The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
One or more of the authors certifies that he (EV) or a member of his immediate family, has received or may receive payments or benefits, during the study period, in an amount less than USD 10,000 from AstraZeneca (Cambridge, UK). One or more of the authors certifies that she (EA) or a member of her immediate family, has received or may receive payments or benefits, during the study period, in an amount of USD 10,001 to USD 100,000 from EMD Serono (Darmstadt, Germany). One or more of the authors certifies that he (CK) or a member of his immediate family, has received or may receive payments or benefits, during the study period, in an amount less than USD 10,000 from Astellas (Tokyo, Japan); in an amount of USD 10,0001 to USD 100,000 from EMD Serono (Darmstadt, Germany); in an amount less than USD 10,000 from Thuasne (Levallois-Perret, France); in an amount of USD 10,0001 to USD 100,000 from Express Scripts (St. Louis, MO, USA); in an amount less than USD 10,000 from Novartis (Basel, Switzerland); in an amount less than USD 10,000 from AbbVie (North Chicago, IL, USA.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Arizona, Tucson, AZ, USA.
References
- 1.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384-391. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833-1840. [PubMed] [Google Scholar]
- 3.Bergman S, Herrstrom P, Hogstrom K, Petersson IF, Svensson B, Jacobsson LT. Chronic musculoskeletal pain, prevalence rates, and sociodemographic associations in a Swedish population study. J Rheumatol. 2001;28:1369-1377. [PubMed] [Google Scholar]
- 4.Brummett CM, Janda AM, Schueller CM, Tsodikov A, Morris M, Williams DA, Clauw DJ. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lower-extremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology. 2013;119:1434-1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brummett CM, Urquhart AG, Hassett AL, Tsodikov A, Hallstrom BR, Wood NI, Williams DA, Clauw DJ. Characteristics of fibromyalgia independently predict poorer long-term analgesic outcomes following total knee and hip arthroplasty. Arthritis Rheumatol. 2015;67:1386-1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlesso LC, Niu J, Segal NA, Frey-Law LA, Lewis CE, Nevitt MC, Neogi T. The effect of widespread pain on knee pain worsening, incident knee osteoarthritis (OA), and incident knee pain: The Multicenter OA (MOST) Study. J Rheumatol. 2017;44:493-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clauw DJ, Crofford LJ. Chronic widespread pain and fibromyalgia: what we know, and what we need to know. Best Pract Res Clin Rheumatol. 2003;17:685-701. [DOI] [PubMed] [Google Scholar]
- 8.Croft P, Rigby AS, Boswell R, Schollum J, Silman A. The prevalence of chronic widespread pain in the general population. J Rheumatol. 1993;20:710-713. [PubMed] [Google Scholar]
- 9.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323-1330. [DOI] [PubMed] [Google Scholar]
- 10.Cushnaghan J, Bennett J, Reading I, Croft P, Byng P, Cox K, Dieppe P, Coggon D, Cooper C. Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis. 2009;68:642-647. [DOI] [PubMed] [Google Scholar]
- 11.Dave AJ, Selzer F, Losina E, Usiskin I, Collins JE, Lee YC, Band P, Dalury DF, Iorio R, Kindsfater K, Katz JN. The association of pre-operative body pain diagram scores with pain outcomes following total knee arthroplasty. Osteoarthritis Cartilage. 2017;25:667-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deshpande BR, Katz JN, Solomon DH, Yelin EH, Hunter DJ, Messier SP, Suter LG, Losina E. Number of persons with symptomatic knee osteoarthritis in the US: Impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res (Hoboken). 2016;68:1743-1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Escobar A, Gonzalez M, Quintana JM, Vrotsou K, Bilbao A, Herrera-Espineira C, Garcia-Perez L, Aizpuru F, Sarasqueta C. Patient acceptable symptom state and OMERACT-OARSI set of responder criteria in joint replacement. Identification of cut-off values. Osteoarthritis Cartilage. 2012;20:87-92. [DOI] [PubMed] [Google Scholar]
- 14.Escobar A, Quintana JM, Bilbao A, Azkarate J, Guenaga JI, Arenaza JC, Gutierrez LF. Effect of patient characteristics on reported outcomes after total knee replacement. Rheumatology (Oxford). 2007;46:112-119. [DOI] [PubMed] [Google Scholar]
- 15.Farrar JT, Young JP, Jr., LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149-158. [DOI] [PubMed] [Google Scholar]
- 16.Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL., 3rd Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10:447-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42:649-652. [DOI] [PubMed] [Google Scholar]
- 18.Gerdle B, Bjork J, Coster L, Henriksson K, Henriksson C, Bengtsson A. Prevalence of widespread pain and associations with work status: a population study. BMC Musculoskelet Disord. 2008;9:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B, Clauw DJ, Brummett CM. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157:1259-1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawker GA, Badley EM, Borkhoff CM, Croxford R, Davis AM, Dunn S, Gignac MA, Jaglal SB, Kreder HJ, Sale JE. Which patients are most likely to benefit from total joint arthroplasty? Arthritis Rheum. 2013;65:1243-1252. [DOI] [PubMed] [Google Scholar]
- 21.Judge A, Arden NK, Kiran A, Price A, Javaid MK, Beard D, Murray D, Field RE. Interpretation of patient-reported outcomes for hip and knee replacement surgery: identification of thresholds associated with satisfaction with surgery. J Bone Joint Surg Br. 2012;94:412-418. [DOI] [PubMed] [Google Scholar]
- 22.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73-84. [DOI] [PubMed] [Google Scholar]
- 23.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lluch Girbes E, Nijs J, Torres-Cueco R, Lopez Cubas C. Pain treatment for patients with osteoarthritis and central sensitization. Phys Ther. 2013;93:842-851. [DOI] [PubMed] [Google Scholar]
- 26.McBeth J, Macfarlane GJ, Silman AJ. Does chronic pain predict future psychological distress? Pain. 2002;96:239-245. [DOI] [PubMed] [Google Scholar]
- 27.Mehta SP, Perruccio AV, Palaganas M, Davis AM. Do women have poorer outcomes following total knee replacement? Osteoarthritis Cartilage. 2015;23:1476-1482. [DOI] [PubMed] [Google Scholar]
- 28.Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios and risk differences in Stata. Stata Journal. 2013;13:492-509. [Google Scholar]
- 29.Perruccio AV, Power JD, Evans HM, Mahomed SR, Gandhi R, Mahomed NN, Davis AM. Multiple joint involvement in total knee replacement for osteoarthritis: Effects on patient-reported outcomes. Arthritis Care Res (Hoboken). 2012;64:838-846. [DOI] [PubMed] [Google Scholar]
- 30.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385-401. [Google Scholar]
- 31.Riddle DL, Perera RA, Stratford PW, Jiranek WA, Dumenci L. Progressing toward, and recovering from, knee replacement surgery: a five-year cohort study. Arthritis Rheum. 2013;65:3304-3313. [DOI] [PubMed] [Google Scholar]
- 32.Riddle DL, Stratford PW. Knee pain during daily tasks, knee osteoarthritis severity, and widespread pain. Phys Ther. 2014;94:490-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88-96. [DOI] [PubMed] [Google Scholar]
- 35.Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769-781. [DOI] [PubMed] [Google Scholar]
- 36.Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, Bombardier C, Felson D, Hochberg M, van der Heijde D, Dougados M. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005;64:29-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vina ER, Hannon MJ, Kwoh CK. Improvement following total knee replacement surgery: Exploring preoperative symptoms and change in preoperative symptoms. Semin Arthritis Rheum. 2016;45:547-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165:710-718. [DOI] [PubMed] [Google Scholar]
- 39.Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220-233. [DOI] [PubMed] [Google Scholar]
- 40.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160-172. [DOI] [PubMed] [Google Scholar]
- 41.Wylde V, Hewlett S, Learmonth ID, Dieppe P. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566-572. [DOI] [PubMed] [Google Scholar]
- 42.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476-499. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.