Abstract
Objective
The aim of this case series is to describe our experience in diagnosis and management of oncological asymptomatic patients with COVID-19 who underwent 18F-FDG PET/CT.
Methods
From March 9 to March 31, 2020, we identified 5 patients who had PET/CT findings suspicious for COVID-19, but no symptom of infection.
Results
The first three patients were administered an SARS-CoV-2 test in a COVID-dedicated center, while the fourth and fifth were tested in our institution, in accordance with a new internal procedure. The SARS-CoV-2 test yielded positive results in all five patients.
Conclusion
In this COVID-19 emergency, our task as radiologists and nuclear medicine physicians is to be able to identify imaging findings suggestive of the disease and to manage patients without overloading the hospital system.
Keywords: COVID-19, Asymptomatic patients, 18F-FDG PET/CT, Chest CT
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with its epicenter in the Hubei Province of the People’s Republic of China, has spread to many countries and is officially a pandemic. To date, Italy has been one of the most affected countries, in particular the Lombardy region.
The Emergency Medical System (EMS) of the metropolitan area of Milan promptly responded to the rapid outbreak of the disease, creating a procedural algorithm aimed at handling suspected cases, adopting containment measures, and addressing population concerns [1].
As a hospital solely dedicated to cancer treatment and research, we are not at the forefront of this tough battle that is taking place in our country. However, consistent with the high spread of the disease, we diagnosed some unexpected cases during the execution of 18F-FDG PET/CT between March 9 and March 31, 2020.
Common clinical manifestations of COVID-19 include fever, cough, dyspnoea, myalgia, and fatigue. None of our patients had symptoms of infection.
The first two patients were a 54-year-old man who was referred to our division for the staging of a non-Hodgkin lymphoma, and a 61-year-old man who presented lung, lymph nodes, and brain lesions suspected for cancer of unknown primary origin.
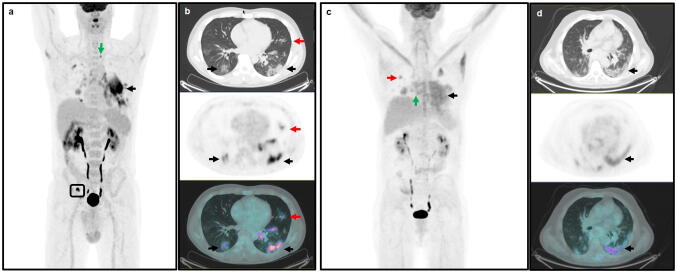
In patient #1, the PET/CT scan revealed pathological uptake in right inguinal lymph nodes (Fig. 1a—box). There was also intense 18F-FDG uptake on multiple bilateral subsegmental peripheral patchy ground-glass opacities (GGOs) with obscure boundaries and mainly subpleural distribution (Fig. 1a, b—black arrows) and areas of focal consolidation in the upper lobes (Fig. 1b—red arrows). Moreover, multiple FDG-avid lymph nodes in the mediastinum and the left subclavian region were detected (Fig. 1a—green arrow).
Fig. 1.
a Left subclavian lymph nodes (green arrow: SUV bw max = 4.6) and right inguinal lymph nodes (box: SUV bw max = 10.9); a, b peripheral and parenchymal GGOs in both lower lobes (black arrows: SUV bw max = 10.7), areas of focal consolidations (red arrows: SUV bw max = 3.9), c, d: multiple peripheral GGOs in the left lower lobe (black arrows: SUV bw max = 4.9); c focal consolidation in the upper lobes (red arrow: SUV bw max = 3.6) and right hilar lymph nodes (green arrow: SUV bw max = 3.9)
Similarly, in patient #2, the PET/CT revealed intense 18F-FDG uptake on multiple peripheral GGOs (Fig. 1c, d—black arrows) in the left lower lobe and areas of focal consolidation in the upper lobes (Fig. 1c—red arrow). Multiple FDG-positive areas were also identified in mediastinal, carinal, subcarinal, and hilar lymph nodes (Fig. 1c—green arrow).
These findings were consistent with interstitial pneumonia and suggested a diagnosis of COVID-19. This diagnosis was confirmed by an experienced radiologist.
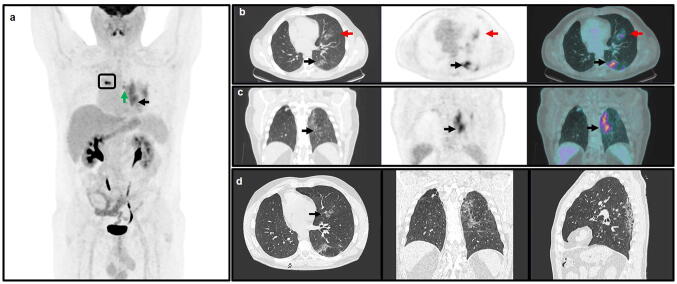
Patient #3 was a 48-year-old man with a stage IV lung cancer already treated with neoadjuvant chemotherapy, radiotherapy, surgery, and adjuvant chemotherapy in 2015, nivolumab for a subsequent lung relapse and radiotherapy on the right retro-bronchial lymph-node metastases in January 2020. He underwent the exam for disease re-staging. The PET/CT scan showed radiotracer uptake in the treated lymph nodes, due to the recent radiotherapy (Fig. 2a—box). There were also intense accumulations on a focal consolidation in the upper left lobe (Fig. 2b—red arrows), multiple peripheral GGOs with interstitial thickening and thin fibrous stripes in the left lower lobe (Fig. 2a–c—black arrows), and multiple FDG uptake in mediastinal and left hilar lymph nodes (Fig. 2a—green arrow).
Fig. 2.
a Left hilar lymph nodes (green arrow: SUV bw max = 5.2) and retro-bronchial lymph nodes (box: SUV bw max = 9.8); b monolateral focal lung consolidation into the left upper lobe (red arrows: SUV bw max = 3.3); a–d multiple peripheral GGOs and septal thickening in the lower lobe (black arrows: SUV bw max = 6.5)
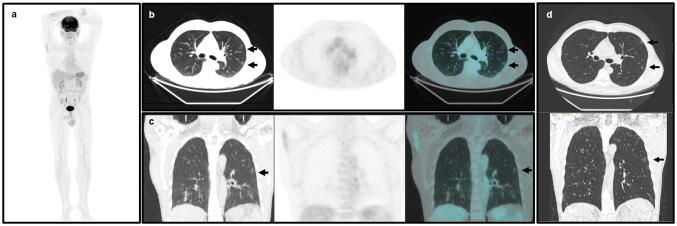
Patient #4 was a 54-year-old man with right cheek melanoma who underwent surgery in 2017 and was treated with pembrolizumab due to the subsequent appearance of lung metastases, with a complete response. The PET/CT was required as a follow-up and, as compared to the previous one, revealed the persistence of intense uptake on subpleural pseudonodular thickenings in the right lower lobe, doubtful for persistence of neoplastic disease. The low-dose CT scan also revealed the presence of multiple small subpleural GGOs and opacities bilaterally without 18F-FDG uptake (Fig. 3a–c—black arrows).
Fig. 3.
a–d Multiple small regions of subpleural GGO in both lungs without 18F-FDG uptake (black arrows)
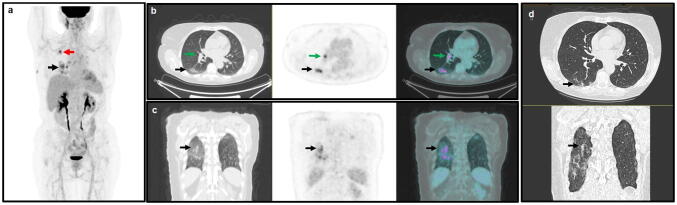
Finally, patient #5 was referred to our division to follow up a tongue carcinoma which had been treated with surgery in 2016–2017 and adjuvant chemo- and radiotherapy. The PET/CT revealed intense 18F-FDG uptake on multiple peripheral GGOs (Fig. 4a–c—black arrows) in both lower lobes and an area of focal consolidation in the right upper lobe (Fig. 4a—red arrow). Focal FDG-positive area was also identified in right hilar lymph node (Fig. 4b—green arrows).
Fig. 4.
a Area of focal consolidation in right upper lobe (red arrows: SUV bw max = 6.8); b right hilar lymph node (green arrow: SUV bw max = 5.9); a–d: peripheral and parenchymal GGOs in both lower lobes lobe (black arrows: SUV bw max = 6.3)
Diagnostic CT scan subsequently performed for patient #3, #4, and #5, and evaluated by an experienced radiologist, confirmed the PET/CT findings of suspected COVID-19 (Figs. 2d, 3d and 4d—black arrows).
For the first three patients, following the operating instructions laid down by the Medical Office of our hospital, we contacted the European emergency number (112), first public safety answering point. Patients #1 and #2 were taken to COVID-dedicated hospital facilities by ambulance, tested for SARS-CoV-2, and then sent home for a 14-day self-isolation period.
In view of the worsening of the emergency situation, the subsequent scarcity of resources, and the need for their adequate allocation, patient #3 was not taken into care by a COVID-dedicated hospital. The nuclear medicine physician who evaluated his PET/CT scan and detected the suspect lung lesions, instead, contacted his lung specialist who made arrangements to send him to a centre where he underwent the test for SARS-CoV-2.
Then, in agreement with our Medical Office, we developed and followed a different procedure for the fourth and fifth patient. The test was performed in our hospital by a dedicated nurse and the patient was sent back home after being instructed on how to avoid spreading the infection (social distancing, hand hygiene, and cough etiquette), by means of a pamphlet and a clinical diary created for this special purpose.
The SARS-CoV-2 test yielded positive results in all five patients. All the patients underwent quarantine for 15 days with daily body temperature measurements and remained asymptomatic during that time. All five patients repeated SARS-CoV-2 test, with a negative result.
Discussion
The proportion of mild or asymptomatic cases, who do not seek health-care and do not receive a diagnosis, is currently unknown, and probably underestimated for SARS-CoV-2, as efforts are directed towards the management and treatment of the most serious and potentially fatal cases. Consequently, the human-to-human transmissibility has not yet been fully assessed, even though recent reports indicate that asymptomatic or paucisymptomatic individuals can transmit the infection, and similar viral loads between asymptomatic and symptomatic patients have been reported [2–4].
In this short communication, we describe the cases of five oncological patients without symptoms but with COVID-19 detected at PET/CT imaging and, therefore, potentially able to infect family members, caregivers, and even health-care workers. Indeed, as cancer patients, they need to refer to the health facilities for the course of their treatments. These patients represent the tip of the submerged part of the iceberg and their identification and appropriate management are important for several reasons.
First, these oncological patients might be at increased risk of COVID-19 (owing to their immunosuppressive state caused by the disease and anticancer treatments) and poorer outcome, as reported by Liang et al. [5]. Strategies designed to handle safely both the viral disease and the cancer are necessary, such as considering the postponement of surgery, chemotherapy, or radiotherapy, if possible, and to initiate a careful surveillance of the appearance of SARS-CoV-2 symptoms.
Moreover, the earlier diagnoses of these positive cases can limit the spread of the infection within the population, the exposure of health-care workers, and of their patients.
Additionally, these data are also useful in the epidemiological evaluation of the pandemic, insofar as a better understanding of SARS-CoV-2 spread could lead to evidence-based decisions about control measures, guide the response to the outbreak, and target treatments to maximize benefits [6].
Finally, during an emergency, it is of the utmost importance to allocate resources correctly. SARS-CoV-2-positive asymptomatic patients do not require rapid hospitalization, which is of help in not overloading an already overwhelmed hospital system. In this context, one may also propose avoiding testing for patients with positive imaging. Indeed, as the pandemic progresses, worldwide demand for tests will probably began to exceed supply, creating the need to prioritize patients.
The chest CT has demonstrated high sensitivity for diagnosis of COVID-19 as compared to the reverse-transcription polymerase chain reaction (RT-PCR) test, a test that lacks sensitivity, has insufficient stability and a relatively long processing time [7]. The CT could also be used to follow up the patients during the acute period and the subsequent recovery period, with a low-dose protocol aimed at minimizing radiation exposure [8].
Next to chest CT, FDG PET/CT suggests an unexpected role revealing tracer uptake even in peripheral GGOs, which appear to be typical manifestation of COVID-19 infection, in association with consolidative opacities [9, 10]. Indeed, GGOs are usually manifestation of malignant lesions with low Ki-index and are characterized by absent or low uptake [11].
The FDG positivity of COVID-19 lung lesions is probably correlated with inflammatory burden as reported for Middle East respiratory syndrome or the H1N1 pandemic influenza virus [12].
Our task as radiologists and nuclear medicine physicians is to carefully evaluate the CT and PET/CT exams and to be able to identify and manage patients with imaging findings suggestive of COVID-19. We have a clear contribution to give, even if it may seem minimal.
Acknowledgements
We would like to thank our technical staff for the support with patient care and the acquisition of scans. In addition, the authors wish to thank Dr. Luca Pase and Dr. Fabrizio Mastrilli for their help in patient management and Associate Prof. Gabriella Conti and Mr William Russel Edu for their help with revising the English manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
All patients gave their written informed consent for the use of anonymous personal data extracted from their medical records for research purposes.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Laura Gilardi and Marzia Colandrea have contributed equally to this paper as first authors.
References
- 1.Spina S, Marrazzo F, Migliari M, Stucchi R, Sforza A, Fumagalli R. The response of Milan's Emergency Medical System to the COVID-19 outbreak in Italy. Lancet. 2020;395:e49–e50. doi: 10.1016/S0140-6736(20)30493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020 doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of covid-19—studies needed. N Engl J Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 7.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2019 doi: 10.1148/radiol.20202006422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang Z, Li X, Zhou S. Recommendation of low-dose CT in the detection and management of COVID-2019. Eur Radiol. 2020 doi: 10.1007/s00330-020-06809-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (Lond Engl) 2020 doi: 10.1016/s0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel coronavirus (2019-nCoV) Radiology. 2020;2020:200230. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotaro H, Yoshimichi U, Aya S, Xiao Ming W, Linfeng Xu, Manabu M, et al. Correlation of Glut-1 glucose transporter expression with [18F]FDG uptake in non-small cell lung cancer. Eur J Nucl Med. 2000;27:1778–1785. doi: 10.1007/s002590000367). [DOI] [PubMed] [Google Scholar]
- 12.Jonsson CB, Camp JV, Wu A, Zheng H, Kraenzle JL, Biller AE, et al. Molecular imaging reveals a progressive pulmonary inflammation in lower airways in ferrets infected with 2009 H1N1 pandemic influenza virus. PLoS ONE. 2012;7:e40094. doi: 10.1371/journal.pone.0040094. [DOI] [PMC free article] [PubMed] [Google Scholar]