Abstract
Objective
The incidence of intravenous drug associated (IVDA) Tricuspid Valve (TV) endocarditis in the United States is rapidly increasing. Our goal was to evaluate the outcomes of isolated TV operations using the Society of Thoracic Surgeon (STS) Adult Cardiac Surgical Database.
Methods
From July 2011 to December 2016, 1,613 IVDA patients underwent isolated TV operations for endocarditis. Patients were stratified based on type of TV operation: valvectomy 119 (7%), repair 532 (33%) and replacement 962 (60%). Risk factors and 30-day outcomes were compared between groups using Kruskal-Wallis and Pearson’s chi-squared tests. Multivariable logistic regression evaluated risk-adjusted operative mortality and morbidity by operative technique.
Results
Age, gender, race and renal function were comparable between groups. Compared to repair and replacement respectively, the valvectomy group had higher rate of acute infection (90% vs. 79%, 84%p<0.01), MELD score (10.17 vs. 8.44, 9.74,p<0.01) and urgent/emergent surgery (91% vs. 75%, 83%, p<0.01). Operative mortality was higher in valvectomy 16% (p<.01) compared to repair 2% or replacement 3%. Following risk-adjustment, valvectomy was associated with higher risk of operative mortality compared to repair (OR=3.82, p<.01), whereas there was no difference in operative mortality between repair and replacement (OR=0.95, p=0.89).
Conclusion
This contemporary series of IVDA TV endocarditis reveals that valvectomy is an independent predictor of operative mortality. When anatomically possible, repair should be the preferred management for TV endocarditis to avoid recurrent valve infection and prosthetic valve degeneration.
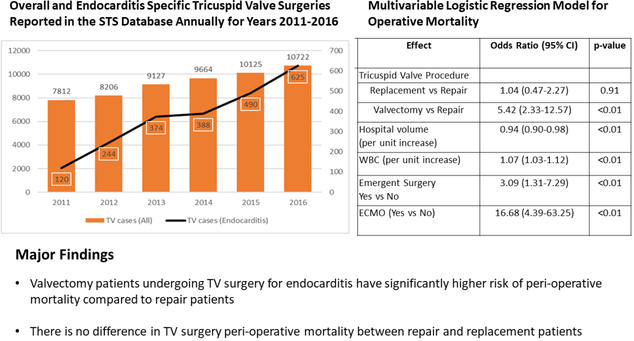
Graphical Abstract
Summarizing Annual Number of Overall and Endocarditis Specific Tricuspid Valve Surgeries Performed, Multivariable Regression Model showing Association of Tricuspid Surgery Type to Operative Mortality as well as Major Findings of the Study
Introduction
The United States (USA) is facing one of the worst opioid crises in its history with approximately 42,000 deaths in year 2016 directly attributed to opioid overdose 1. Certain reports in mid 1980s advocated use of opioid for chronic pain management, starting the ineradicable debate about its benefits, dependence and addiction 2, 3. Sam Quinones in his book “Dreamland: the true tale of America’s opiate epidemic” summarizes several studies from 1990s supporting aggressively treating pain, now considered the 5th vital sign, causing a significant increase in prescription opioid use and consequential dependence 4 To mitigate increasing use of prescription opioids, there has been a rapid rise in physician regulation 4 Center for Disease Control (CDC) data shows that in 2010, there were approximately 6 opioid overdose deaths and 1 heroin overdose death per 100,000 population which has skyrocketed to approximately 15 opioid overdose deaths and 5 heroin overdose deaths per 100,000 population in year 2016 1.
Although, intravenous antibiotics are primary treatment for tricuspid valve (TV) endocarditis, several patients fail the treatment or have residual TV insufficiency requiring operative intervention 5–7 Recent literature, including consensus guidelines from the American Association for Thoracic Surgery recommend TV vegetation debridement and repair of the valve when possible although replacement is still most commonly performed intervention 8–11. Given the high rates of recidivism in the intravenous drug use (IDU) endocarditis population, we aimed to evaluate the early outcomes of isolated TV repair, replacement and valvectomy using the Society of Thoracic Surgeons (STS) adult cardiac surgical database (ACSD).
Methods
Study Population
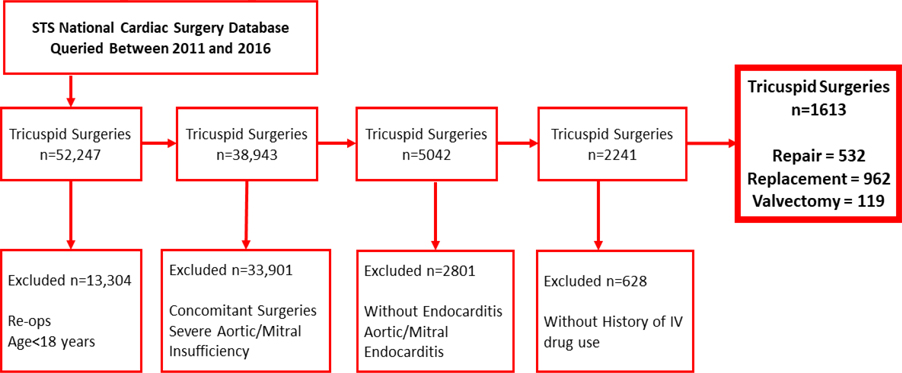
The STS ACSD access and publication committee approved our proposal to access data on adult patients undergoing tricuspid valve surgery for infective endocarditis between years 2011 and 2016. Tricuspid surgery patients undergoing concomitant surgeries, re-operations as well as with severe aortic or mitral insufficiency were excluded. Patients without history of TV endocarditis or IVDA and with history of aortic and mitral valve endocarditis (but not receiving surgery) were also excluded. Figure 1 shows the flow diagram of the study population. The final dataset had 1613 patients undergoing TV surgery of which 119 had valvectomy, 532 had repair and 962 had replacement and were categorized into these corresponding study groups.
Figure 1.
Consort Diagram Describing Inclusion/Exclusion Criteria and Final Study Population
Data Analysis
The TV surgery patients were initially evaluated for their demographic and pre-operative risk factors by the type of surgery. The patients were also evaluated by their pre-operative cardiac risk factors. The primary study outcome was operative mortality. The operative mortality was defined as in-hospital or 30-day post-operative mortality. The secondary study outcomes were in-hospital complications and rates of 30-day readmissions.
The data was analyzed using univariate non-parametric statistical tests. The Kruskal-Wallis test was used for continuous variables and the Pearson’s chi-square estimates were used for categorical variables. The univariate statistics were presented as median (inter quartile range) for continuous variables and N (%) for categorical variables. A multivariable logistic regression model with generalized estimating equations accounting for statistical dependence between patients from the same hospital was generated to evaluate demographic and preoperative factors associated with operative mortality. A variable defined as type of TV surgery (repair, replacement or valvectomy) was forced in the logistic regression model to evaluate association of type of surgery (TV repair used as reference variable) with operative mortality after risk adjusting for multiple pre-operative and demographic variables (Age, Organism (Staph. Aureus vs. Others), Government Payer (Yes vs No), Acute Infection (Active vs Treated), WBC, Hematocrit, MELD Score, Emergent Surgery Yes vs No, NYHA class > II (Yes vs No), ECMO (Yes vs No) and Tricuspid Valve Procedure). We also added TV surgery hospital volume as a co-variate in the regression model as hospital variation could contribute to outcomes. We also performed a hierarchical logistic regression model with site-specific random intercepts (supplement 1 appendix 2). The result from two models are very close hence we only reported results of generalized logistic regression model. We also performed a logistic regression model to evaluate association of type of TV surgery with in-hospital complications (complications were accounted as composite of deep sternal wound infection, operative bleeding, permanent stroke, renal Failure, prolonged ventilation, blood products used postoperatively and continued sepsis/positive cultures). The results of the logistic regression model for complications are reported in the supplement file appendix 1. The results of regression model were reported as odds ratio (OR) and 95% confidence intervals (CI). We excluded patients with missing information from the model. We only used complete cases for multivariable logistics regression. All the analysis was conducted using SAS 9.4 software (SAS Inc., Cary, NC).
Results
Demographic and Risk Factors
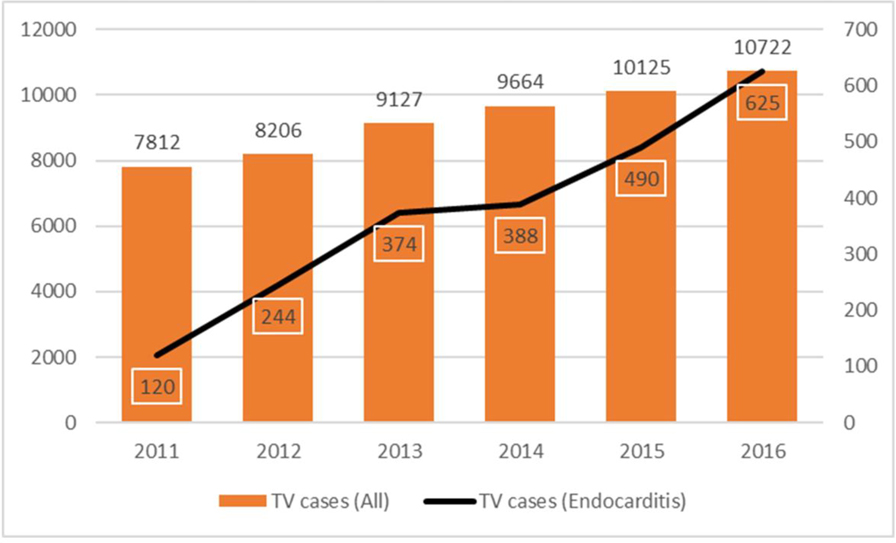
A total of 1613 patients with history of IVDA were operated for isolated tricuspid valve endocarditis between years 2011 and 2016. The TV endocarditis operations due to IVDA increased from 120 in year 2011 to 625 in year 2016 coinciding with the increase in heroin overdose deaths (Figure 2). The median age of the cohort was 30 (26–36) years. There were 968 (60%) females and 1361 (84%) Caucasians. For TV valvectomy, repair and replacement, the median age (29 vs. 30 vs. 31 years, p=0.11), female gender (55% vs. 58% vs. 62%, p=0.19), Caucasian race (85% vs. 84% vs. 85%, p=0.99) and median body mass index (24 vs. 24 vs. 24 kg/m2, p=0.49) were similar between the groups respectively. The valvectomy group had significantly more patients with government sponsored insurance (73% vs. 56% vs. 50%, p<0.01) compared to replacement and repair groups. Table 1 describes the demographic factors by TV surgery.
Figure 2.
Overall and Endocarditis Specific Tricuspid Valve Surgeries Reported in the STS Database Annually for Years 2011–2016
Table 1.
Demographic and Risk Factors by Type of TV Surgery
| Type of Surgery | Overall | Valvectomy | Repair | Replacement | P-value |
|---|---|---|---|---|---|
| (N=1613) | (N=119) | (N=532) | (N=962) | ||
| Demographics | |||||
| Age (years)* | 30 (26–36) | 29 (25–35) | 30 (26–36) | 31 (26–37) | 0.11 |
| Gender (Female) | 968 (60.01) | 65 (54.62) | 310 (58.27) | 593 (61.64) | 0.19 |
| Race (Caucasian) | 1361 (84.38) | 101 (84.87) | 450 (84.59) | 810 (84.2) | 0.99 |
| Payor-Government | 894 (55.42) | 87 (73.11) | 265 (49.81) | 542 (56.34) | <.01 |
| Risk Factors | |||||
| Infectious Endocarditis (Active) | 1332 (82.58) | 107 (89.92) | 418 (78.57) | 807 (83.89) | <.01 |
| Staphylococcus aureus | 1239 (76.81) | 104 (87.39) | 395 (74.25) | 740 (76.92) | 0.02 |
| Tobacco Use (current) | 1220 (75.64) | 98 (82.35) | 394 (74.06) | 728 (75.68) | 0.14 |
| Alcohol Use (>7 drinks/week) | 150 (9.3) | 9 (7.56) | 54 (10.15) | 87 (9.04) | 0.01 |
| Body Mass Index (kg/m2)* | 24 (21–28) | 24 (21–28) | 24 (22–27) | 24 (21–28) | 0.48 |
| Diabetes | 77 (4.77) | 6 (5.04) | 24 (4.51) | 47 (4.89) | 0.94 |
| Dyslipidemia | 108 (6.7) | 11 (9.24) | 43 (8.08) | 54 (5.61) | 0.10 |
| Dialysis | 102 (6.32) | 11 (9.24) | 32 (6.02) | 59 (6.13) | 0.40 |
| Hypertension | 291 (18.04) | 20 (16.81) | 99 (18.61) | 172 (17.88) | 0.88 |
Data presented N (%) and
Median (Inter Quartile Range)
Of all, 1332 patients undergoing TV surgery had active infection (83%) and Staphylococcus Aureus was the most common organism (n=1239, 77%). The valvectomy group had significantly more patients with active infection (90% vs. 84% vs. 79%, p<0.01) and Staphylococcus Aureus organism (87% vs 77% vs. 74%, p=0.02) compared to replacement and repair groups. History of smoking,, diabetes, hypertension, dyslipidemia, and dialysis were statistically similar between the study groups. Table 1 summarizes the risk factors by TV surgery.
Pre-operative Factors
At baseline, valvectomy patients had significantly higher median WBCs (11.9 vs. 10.0 vs. 9.0, p<0.01) as well as MELD score (10.17 vs. 9.74 vs. 8.44, p<0.01) and significantly lower median hematocrit (26.7 vs. 28.0 vs. 29.0, p<0.01) and albumin (1.9 vs. 2.2 vs. 2.5, p<0.01) compared to TV replacement and repair patients. The presence of NYHA class 3 or more heart failure (23% vs. 16% vs. 22%, p=0.04), severe tricuspid insufficiency (72% vs. 62% vs. 64%, p=0.04) and use of pre-operative intravenous inotropes (6% vs. 3% vs. 5%, p=0.03) was significantly higher in the TV replacement group compared to repair and valvectomy groups (Table 2).
Table 2.
Pre-operative and Cardiac Risk Factors by Type of TV Surgery
| Type of Surgery | Overall | Valvectomy | Repair | Replacement | P-value |
|---|---|---|---|---|---|
| (N=1613) | (N=119) | (N=532) | (N=962) | ||
| WBC* | 9.8 (7.1–13.4) | 11.9 (9–16.5) | 9 (6.7–12) | 10 (7.2–13.6) | <.01 |
| Hematocrit* | 28.2 (25.3–32) | 26.7 (24.1–29) | 29 (26.2–33.5) | 28 (25–31.6) | <.01 |
| Last Creatinine Level Preop (mg/dL)* | 0.8 (0.6–1.1) | 0.8 (0.62–1.2) | 0.8 (0.6–1.0) | 0.82 (0.61–1.2) | <.01 |
| Heart failure (>class II) within 2 weeks | 334 (20.71) | 27 (22.69) | 85 (15.98) | 222 (23.08) | <.01 |
| Cardiogenic shock | 41 (2.54) | 3 (2.52) | 9 (1.69) | 29 (3.01) | 0.29 |
| Resuscitation | 12 (0.74) | 2 (1.68) | 3 (0.56) | 7 (0.73) | 0.43 |
| Arrhythmias | 84 (5.21) | 11 (9.24) | 22 (4.14) | 51 (5.3) | 0.07 |
| Inotropic, intravenous | 80 (4.96) | 6 (5.04) | 16 (3.01) | 58 (6.03) | 0.03 |
| Aortic Insufficiency | |||||
| None/Trivial | 1551(96.11) | 113 (94.96) | 520 (97.74) | 918 (95.42) | 0.48 |
| Mild | 28 (1.74) | 2 (1.68) | 5 (0.94) | 21 (2.18) | |
| Moderate | 5 (0.31) | 0 (0.00) | 2 (0.38) | 3 (0.31) | |
| Mitral Insufficiency | |||||
| None/Trivial | 1312 (81.33) | 93 (78.15) | 437 (82.14) | 782 (81.28) | 0.71 |
| Mild | 248 (15.38) | 20 (16.81) | 79 (14.85) | 149 (15.49) | |
| Moderate | 23 (1.43) | 3 (2.52) | 8 (1.50) | 12 (1.25) | |
| Tricuspid Insufficiency | |||||
| Severe | 1098 (68.07) | 76 (63.87) | 328 (61.65) | 694 (72.14) | <.01 |
| Moderate | 330 (20.46) | 24 (20.17) | 135 (25.38) | 171 (17.78) | |
| Mild | 132 (8.18) | 13 (10.92) | 53 (9.96) | 66 (6.86) | |
| Trivial | 26 (1.61) | 3 (2.52) | 9 (1.69) | 14 (1.46) | |
| None | 20 (1.24) | 1 (0.84) | 5 (0.94) | 14 (1.46) | |
| MELD score* | 9.3 (7.5–12.3) | 10.2 (8.4–13.8) | 8.4 (7.4–10.5) | 9.7 (8.3–12.6) | <.01 |
| Total Albumin* | 2.3 (1.8–3) | 1.9 (1.5–2.5) | 2.5 (1.9–3.2) | 2.2 (1.8–2.9) | <.01 |
Data presented N (%) and
Median (Inter Quartile Range)
Outcomes
The valvectomy group had significantly higher unadjusted operative mortality (16% vs. 2% vs. 3%, p<0.01) compared to TV repair and replacement groups however unadjusted mortality between TV repair and replacement (2% vs. 3%, p=0.50) groups was not significantly different. The valvectomy group also had higher rates of in-hospital stroke (2% vs. 1% vs. 0, p<0.01), renal failure (19% vs. 5% vs. 6%, p<0.01) and mechanical ventilation>24hours (43% vs. 14% vs. 20%, p<0.01) compared to repair and replacement groups. Although median ICU stay in the valvectomy group was longer (74 vs. 61 vs. 44 hours, p<0.01), the 30-day readmission rate (10% vs. 6% vs. 9%, p=0.34) was comparable between the study groups (Table 3).
Table 3.
Post-operative Outcomes by Type of TV Surgery
| Type of Surgery | Overall | Valvectomy | Repair | Replacement | P-value |
|---|---|---|---|---|---|
| (N=1613) | (N=119) | (N=532) | (N=962) | ||
| Primary Outcome | |||||
| Operative Mortality | 60 (3.72) | 19 (15.97) | 12 (2.26) | 29 (3.01) | <.01 |
| Secondary Outcomes | |||||
| Post-operative complications | 1029 (63.79) | 85 (71.43) | 304 (57.14) | 640 (66.53) | <.01 |
| Deep sternal infection | 1 (0.06) | 0 (0) | 0 (0) | 1 (0.1) | 0.71 |
| Permanent stroke | 6 (0.37) | 2 (1.68) | 4 (0.75) | 0 (0) | <.01 |
| Renal Failure | 111 (6.88) | 23 (19.33) | 28 (5.26) | 60 (6.24) | <.01 |
| Prolonged ventilation | 324 (20.09) | 51 (42.86) | 76 (14.29) | 197 (20.48) | <.01 |
| Initial ICU hours* | 51.1 (26–120.8) | 74 (38.9–190) | 44 (24–75.5) | 61 (27–139) | <.01 |
| Reop for any reason | 194 (12.03) | 16 (13.45) | 48 (9.02) | 130 (13.51) | 0.03 |
| ReOp for Valvular Dysfunction | 11 (0.68) | 3 (2.52) | 5 (0.94) | 3 (0.31) | 0.01 |
| Sepsis | 44 (2.73) | 3 (2.52) | 9 (1.69) | 32 (3.33) | 0.18 |
| Positive Blood Culture | 38 (2.36) | 2 (1.68) | 8 (1.5) | 28 (2.91) | 0.20 |
| Discharge location Home | 844 (52.32) | 44 (36.97) | 292 (54.89) | 508 (52.81) | 0.42 |
| 30 Day readmission | 125 (7.98) | 10 (9.9) | 31 (5.92) | 84 (8.93) | 0.34 |
Data presented N (%) and
Median (Inter Quartile Range)
Risk-adjusted Mortality
The multivariable logistic regression model, risk-adjusting for demographic and pre-operative variables, showed that the valvectomy group was independently associated with higher risk of operative mortality (OR=5.42, 95% CI=2.33–12.57) compared to the repair group whereas there was no difference in operative mortality between TV replacement and repair groups (OR=1.04, 95% CI=0.47–2.27). Other than valvectomy, emergent indication (OR=3.09, 95% CI=1.31–7.29), peri-operative ECMO requirement (OR=16.68, 95% CI=4.39–63.25) and increase in WBC (OR=1.07,95% CI=1.03–1.12) were associated with increased risk of operative mortality whereas higher TV surgery hospital volume (OR=0.94, 95% CI=0.90–0.98) was associated with decreased operative mortality (Table 4). The multivariate model for the complications showed that type of TV surgery was not associated with composite complications (Appendix 1 supplement file).
Table 4.
Multivariable Logistic Regression Model for Operative Mortality
| Effect | Odds Ratio (95% CI) | p-value |
|---|---|---|
| Age (per unit increase) | 1.01 (0.98–1.04) | 0.26 |
| Organism (Staph. Aureus vs. Others) | 0.67 (0.31–1.44) | 0.31 |
| Government Payer (Yes vs No) | 1.11 (0.61–2.02) | 0.72 |
| Acute Infection (Active vs Treated) | 1.13 (0.37–3.44) | 0.82 |
| WBC (per unit increase) | 1.07 (1.03–1.12) | <0.01 |
| Hematocrit (per unit increase) | 1.00 (0.94–1.06) | 0.95 |
| MELD Score (per unit increase) | 1.03 (0.98–1.07) | 0.14 |
| Emergent Surgery Yes vs No | 3.09 (1.31–7.29) | <0.01 |
| ECMO (Yes vs No) | 16.68 (4.39–63.25) | <0.01 |
| NYHA class > II (Yes vs No) | 1.10 (0.54–2.22) | 0.79 |
| Tricuspid Valve Procedure | ||
| Replacement vs Repair | 1.04 (0.47–2.27) | 0.91 |
| Valvectomy vs Repair | 5.42 (2.33–12.57) | <0.01 |
| Hospital volume (per unit increase) | 0.94 (0.90–0.98) | <0.01 |
CI = Confidence Interval
The leading causes of operative mortality in TV endocarditis patients were infection (33%) and cardiac (27%). Infection was responsible for nearly half of all deaths in the valvectomy group (47%). Infection accounted for 23% and 30% and cardiac causes were responsible for 18% and 25% of all deaths in the TV repair and replacement groups respectively.
Discussion
This analysis of the STS database revealed that the number of TV surgeries have increased by 35% between years 2011 (n=7814) and 2016 (n=10722). This increase was partially due to a 500% increase in the TV surgeries performed for infective endocarditis (120 in 2011 to 628 in 2016) that is temporally congruent with the heroin epidemic. The IVDA population is at higher risk of recidivism following drug dependency treatment, posing a significant dilemma about choosing the best surgical treatment modality for TV endocarditis 12, 13. Although the TV repair is recommended by multiple recent reports 8, 14, we observed that TV replacement is still more commonly performed surgery for the endocarditis. Using a large national registry, this study highlights that the operative mortality between the TV repair and replacement were comparable (2% vs. 3%) and significantly lower than the valvectomy group (16%).
Previous studies corroborate our findings of similar operative mortality between repair and replacement patients in TV endocarditis 9, 10, 14. Protos et al. and Gaca et al. have also reported comparable early mortality between valvectomy and replacement and repair groups for TV endocarditis 9, 14. However, we observed a significantly higher operative mortality with valvectomy patients. Cause of death analysis in the valvectomy group showed that 47% of patients died due to infection which suggests continued infection even after removal of the infected valve. Although, the valvectomy group had more co-morbidities and pre-operative risk such as higher active infection, WBCs and MELD score and lower hematocrit and albumin levels, it was still independently associated with increased operative mortality based on the multivariable regression model. The same regression model, risk-adjusting for multiple variables such as degree of heart failure and TV insufficiency, showed no significant difference in operative mortality between TV repair and replacement.
There are several baseline factors variable across the study groups such as type of insurance, active infection, type of organism, bilirubin levels and MELD score. Higher bilirubin and resultant MELD score certainly make the valvectomy group high risk for operative mortality. Impact of socio-economic status on outcomes following tricuspid valve surgery are inevitable. The data is suggestive that more younger patients with government insurance are treated with valvectomy who are likely to be Medicaid or other state supported insurance patients. This maybe reflective of poor outcomes with poor socio-economic status however we did not have income status and education level of patients making our inferences inconclusive. We included the aforementioned factors in the regression analysis and found that type of insurance (Government), active infection and MELD score were not significantly associated with operative mortality. One of the important finding of our study was that the tricuspid valve surgery performed at a higher volume center was associated with lower mortality risk suggesting that surgeon experience and institutional preference are significant predictors of mortality apart from type of surgical approach.
In addition to mortality, we also observed higher post-operative complications in valvectomy patients compared to other groups. The TV replacement group also had significantly higher overall post-operative complications compared to the repair group (66% vs. 57%) particularly in terms of re-operations (13% vs. 9%), prolonged ventilation (20% vs. 14%) and ICU length of stay (median 61 vs. 44 hours). Although statistically not significant, we also observed higher 30-day readmissions with TV replacement compared to repair (9% vs. 6%). Although not reported here, TV replacement may increase heart block and resultant pacemaker utilization. A previous study similarly reported higher unplanned readmissions with TV replacements at 1-year and supported valvectomy whenever repair is not feasible in this patient population, at high risk of IDU recidivism 9 Other studies with longer term follow-up have not only observed similar in-hospital outcomes with TV repair but also reported lower rates of recurrent infection and resultant readmissions compared to replacement 10, 15–17 Given lower rates of operative mortality, in-hospital complications and recurrent infections, the TV repair is potentially more cost-effective therapy to surgically treat TV endocarditis in IDU patient who are at higher risk of recidivism 10, 18. Although valvectomy has high operative mortality it may still be a favored surgical approach in select drug use patients who have active infection and repair is not feasible, primarily to avoid early prosthetic valve infection due to recidivism and provide the patient the window to rehabilitate and become drug free before replacing the valve in staged re-operation 9.
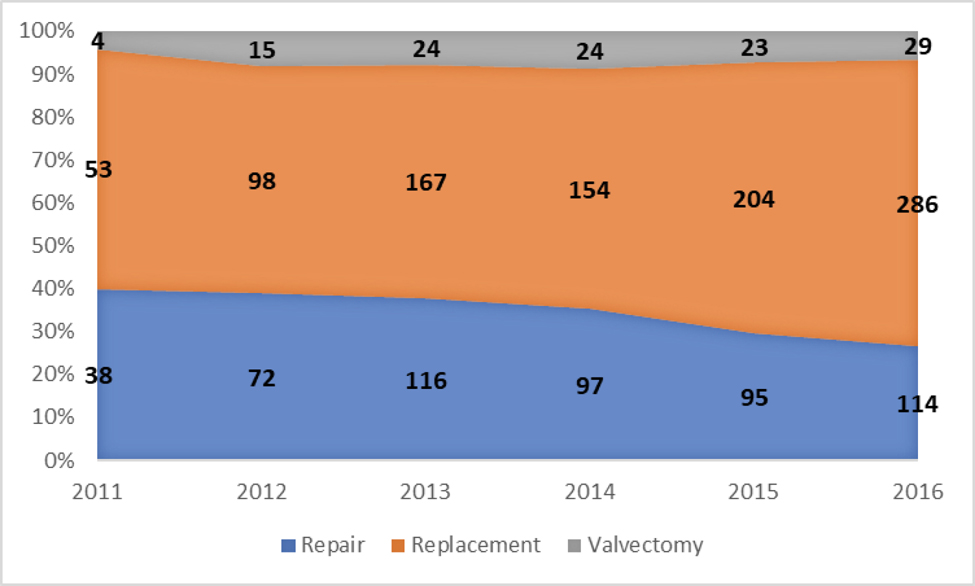
Patients with right heart endocarditis are treated with IV antibiotics as first line of treatment however patients failing the IV antibiotic therapy often need surgical intervention 6. More than 82% patients in our study had an active infection at time of TV surgery with Staphylococcus aureus as most common organism. The requirement for TV endocarditis surgery is likely to follow the trends of heroin epidemic in the USA hence, the survivability of the patients free from recurrent infection and surgery is crucial in collectively countering this high-risk disease. Preserving the native TV is emerging as a favored approach with vegetation debridement followed by repair if feasible however anatomy of the lesion and patient condition such as heart failure may drive decision towards replacement 8. Although, we observed that factors like heart failure class >/=3 are not independently associated with mortality, they may still be critical in clinical decision making. Other than individual clinical factors, decision for TV replacement could also be based on surgeon procedure preference however, with increasing number of IVDA endocarditis, TV repair should become the logical first choice in patients who require surgery. However, our findings not only indicate that the TV replacement has remained the most commonly performed surgery for IV drug use endocarditis, its proportion during the study period increased from 55% in 2011 to 65% in 2016 (Figure 3).
Figure 3.
Tricuspid Valve Surgeries performed Annually by Type of Operation: Replacement, Repair, and Valvectomy
Limitations
This was a retrospective analysis of large registry data at time of surgery hence follow-up beyond 30-days was not available. Consequently, the data is limited by unavailability of longer-term follow-up in this patient population that could be vital to understand rates of recurrent infection, hemodynamic profile of the TV (repaired native or prosthetic), delayed surgical complications like stroke and risk of recidivism. The data about patient selection, clinical decision making on surgical approach and surgeon preferences was also not available that might help understand some of the differences in the outcomes. Despite the use of various characteristics to adjust for potential confounding, residual and/or unmeasured confounding may exist.
Conclusion
This contemporary series of IVDA TV infective endocarditis patients reveals that there was a 500% increase in number of surgeries performed between years 2011 and 2016. Even though valvectomy patients had higher peri-operative risk it was determined to be independent predictor of operative mortality. No statistical difference of operative mortality was observed between TV repair and replacement. However, to potentially avoid recurrent valve infection and prosthetic valve degeneration, whenever anatomically possible, repair should be the preferred management for TV endocarditis. Although valvectomy was found to be high-risk for operative mortality it could not have been prevented in some cases with high risk of recidivism.
Supplementary Material
Central Message.
In the surgical management of isolated tricuspid valve infective endocarditis, operative mortality of repair and replacement are comparable and significantly lower than valvectomy.
Perspective Statement.
This contemporary series of surgical treatment of tricuspid valve infective endocarditis reveals that valvectomy is an independent predictor of mortality. Although operative mortality between repair and replacement are similar, when anatomically possible, repair should be the preferred management for TV endocarditis to potentially avoid recurrent valve infection and prosthetic valve degeneration.
Acknowledgement
The data for this research were provided by The Society of Thoracic Surgeons’ National Database Access and Publications Research Program.
Glossary of Abbreviations
- STS
Society of Thoracic Surgeons
- IVDA
Intravenous Drug User
- TV
Tricuspid Valve
- ACSD
Adult Cardiac Surgical Database
- MELD
Model for End-Stage Liver Disease
- CDC
Center for Disease Control
- WBC
White Blood Cells
- NYHA
New York Heart Association
Footnotes
The Authors of the manuscript have no relevant disclosures or conflict of interest.
References
- 1.Center for Disease Control and Prevention. Drug Overdose Death Data. 2018. 6/26/2018]; Available from: https://www.cdc.gov/drugoverdose/data/statedeaths.html.
- 2.Porter J and Jick H, Addiction rare in patients treated with narcotics. The New England journal of medicine, 1980. 302(2): p. 123. [DOI] [PubMed] [Google Scholar]
- 3.Portenoy RK and Foley KM, Chronic use of opioid analgesics in non-malignant pain: report of 38 cases. Pain, 1986. 25(2): p. 171–186. [DOI] [PubMed] [Google Scholar]
- 4.Quinones S, Dreamland: the true tale of America’s opiate epidemic 2015: Bloomsbury Publishing USA. [Google Scholar]
- 5.Hecht SR and Berger M, Right-sided endocarditis in intravenous drug users: prognostic features in 102 episodes. Annals of internal medicine, 1992. 117(7): p. 560–566. [DOI] [PubMed] [Google Scholar]
- 6.Chambers HF, Miller RT, and Newman MD, Right-sided Staphylococcus aureus endocarditis in intravenous drug abusers: two-week combination therapy. Annals of Internal Medicine, 1988. 109(8): p. 619–624. [DOI] [PubMed] [Google Scholar]
- 7.Nath J, Foster E, and Heidenreich PA, Impact of tricuspid regurgitation on long-term survival. Journal of the American College of Cardiology, 2004. 43(3): p. 405–409. [DOI] [PubMed] [Google Scholar]
- 8.Pettersson GB, Coselli JS, Hussain ST, et al. , 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. The Journal of Thoracic and Cardiovascular Surgery, 2017. 153(6): p. 1241–1258. e29. [DOI] [PubMed] [Google Scholar]
- 9.Protos AN, Trivedi JR, Whited WM, et al. , Valvectomy Versus Replacement for the Surgical Treatment of Tricuspid Endocarditis. Ann Thorac Surg, 2018. 106(3): p. 664–669. [DOI] [PubMed] [Google Scholar]
- 10.Dawood MY, Cheema FH, Ghoreishi M, et al. , Contemporary Outcomes of Operations for Tricuspid Valve Infective Endocarditis. The Annals of Thoracic Surgery, 2015. 99(2): p. 539–546. [DOI] [PubMed] [Google Scholar]
- 11.Wallen TJ, Szeto W, Williams M, et al. , Tricuspid valve endocarditis in the era of the opioid epidemic. Journal of cardiac surgery, 2018. 33(5): p. 260–264. [DOI] [PubMed] [Google Scholar]
- 12.Mori M, Shioda K, Nguemeni Tiako MJ, et al. , Comparable perioperative outcomes and mid-term survival in prosthetic valve endocarditis and native valve endocarditis. Eur J Cardiothorac Surg, 2018. [DOI] [PubMed] [Google Scholar]
- 13.Smyth BP, Barry J, Keenan E, et al. , Lapse and relapse following inpatient treatment of opiate dependence. Ir Med J, 2010. 103(6): p. 176–9. [PubMed] [Google Scholar]
- 14.Gaca JG, Sheng S, Daneshmand M, et al. , Current outcomes for tricuspid valve infective endocarditis surgery in North America. Ann Thorac Surg, 2013. 96(4): p. 1374–1381. [DOI] [PubMed] [Google Scholar]
- 15.Gottardi R, Bialy J, Devyatko E, et al. , Midterm Follow-Up of Tricuspid Valve Reconstruction Due to Active Infective Endocarditis. The Annals of Thoracic Surgery, 2007. 84(6): p. 1943–1948. [DOI] [PubMed] [Google Scholar]
- 16.Baraki H, Saito S, Al Ahmad A, et al. , Surgical treatment for isolated tricuspid valve endocarditis. Circulation Journal, 2013. 77(8): p. 2032–2037. [DOI] [PubMed] [Google Scholar]
- 17.Arbulu A and Asfaw I, Management of infective endocarditis: seventeen years’ experience. The Annals of thoracic surgery, 1987. 43(2): p. 144–149. [DOI] [PubMed] [Google Scholar]
- 18.Kim JB, Ejiofor JI, Yammine M, et al. , Surgical outcomes of infective endocarditis among intravenous drug users. The Journal of Thoracic and Cardiovascular Surgery, 2016. 152(3): p. 832–841.e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.