ABSTRACT
The new coronavirus, COVID-19 was declared a pandemic by the World Health Organization on March 11, 2020. Risk factors associated with this disease are age, sex, and the presence of comorbidities, the most common being hypertension, diabetes, and heart disease. The aim of this meta-analysis was to calculate the prevalence and geographical distribution of comorbidities in all patients admitted to intensive care units (ICUs), and the mortality rate of COVID-19. We selected studies based upon epidemiological and clinical descriptions of the patients and mortality from the disease to determine the pooled prevalence of comorbidities in all patients and in mortality cases due to COVID-19. The pooled prevalence was estimated using the random effects model, and odds ratios were used to measure the probability of death for a patient with a comorbidity. The total prevalence of comorbidities in patients with COVID-19 was 42% (95% CI: 25-60), 61% (95% CI: 42-80) in those admitted to the ICU, and 77% (95% CI: 68-86) among death cases; males were the most affected. Hypertension was the most prevalent comorbidity in all three groups studied, accounting for 32%, 26%, and 35%, respectively. The odds ratio of death for a patient with a comorbidity compared to one with no comorbidity was 2.4 (P < 0.0001). The higher the prevalence of comorbidities the higher the odds that the COVID-19 patient will need intensive care or will die, especially if the pre-existing disease is hypertension, heart disease, or diabetes.
Keywords: COVID-19, SARS-CoV2, Prevalence, Comorbidity, Mortality, Meta-analysis
INTRODUCTION
The 2019 pandemic coronavirus (COVID-19) has affected more than three million people in 211 countries, causing more than two hundred thousand deaths as of the end of April 20201. The etiologic agent of this disease is the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), which is transmitted through contact with infected persons or contaminated fluids2,3.
Several risk factors are associated with this disease. In a multicenter cohort study, advanced age was found to be significantly correlated with overall COVID-19 prevalence, which is consistent with the higher incidence observed in older adults4. The sex is another risk factor as a higher prevalence has been seen in men than women4. Other studies have shown that the presence of any comorbidity increases the chances of COVID-19 infection causing respiratory failure and death in patients5. Another study reports that patients admitted to the intensive care unit (ICU) had a higher number of comorbidities (72.2%) than those not admitted to the ICU (37.3%)6. Hence, comorbidities are considered a risk factor for fatality, and data from other reports show up to a 90% prevalence of comorbidities in fatal cases7, with cardiovascular diseases, diabetes, hypertension, chronic obstructive pulmonary disease being the most prevalent known comorbidities in COVID-19 cases8.
Currently, several published studies describe the epidemiological and clinical characteristics of patients and mortality cases affected by COVID-19 in different parts of the world. For this reason, the aim of this meta-analysis was to estimate the prevalence and geographical distribution of comorbidities in all patients, in those admitted to the ICU, and in mortality cases affected by COVID-19 using the previously published data.
METHODS
The protocol for this systematic review was published in the International Prospective Registry of Systematic Reviews (PROSPERO 2020: CRD42020182479) before its implementation. The protocol and the final report were developed based on the Cochrane Manual of Systematic Reviews of Interventions9.
Review question
What is the prevalence of comorbidities in all patients, patients admitted to the ICU, and in fatal cases affected by the new coronavirus (COVID-19)?
Inclusion criteria
This review considered studies that conducted epidemiological and clinical descriptions in patients and in fatal cases from different parts of the world, in order to determine the prevalence and geographic distribution of comorbidities in patients affected by COVID-19.
Search strategy
An initial search limited to MEDLINE was performed using MeSH index terms and related keywords. This search was followed by an analysis of the words in the text of the title, abstract, and index terms used to describe the articles. A second search using all the identified keywords and index terms was conducted on May 15, 2020 using the following databases: Latin American and Caribbean Health Sciences Literature (LILACS), the bibliographic database of the US National of Medicine (Medline), the Elsevier database (EMBASE), Web of Science and SCOPUS. The MeSH Index Term search included COVID-19, SARS-CoV2, prevalence, and comorbidity. As COVID-19 is a recent topic, thesis and dissertation papers have not yet been published and were not evaluated.
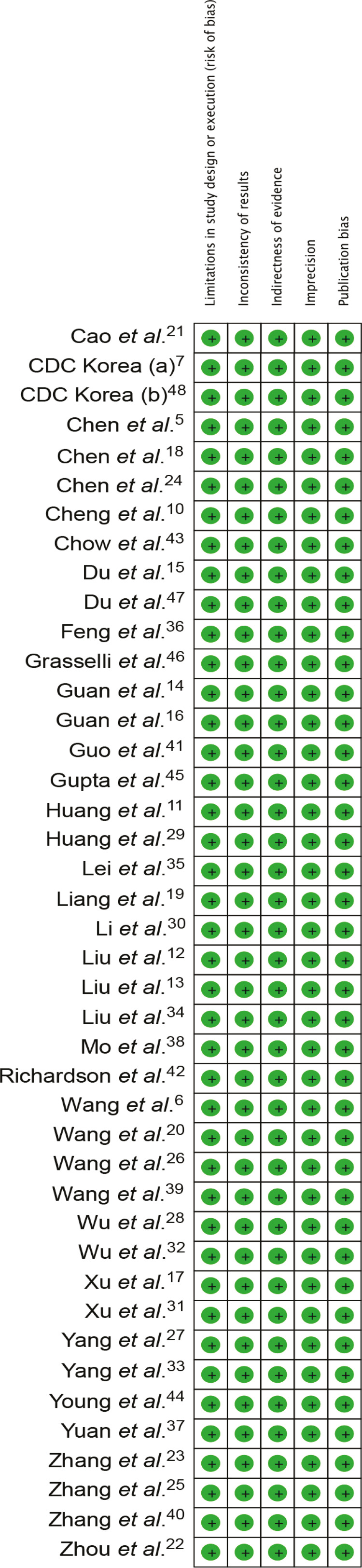
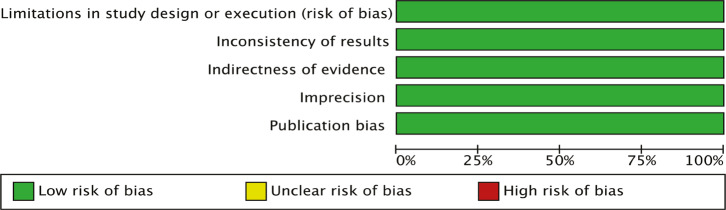
Methodological quality assessment
The articles selected for data recovery were analyzed by two independent reviewers who assessed the methodological validity of each text before their inclusion in this review. The quality of the publications included were evaluated based on the criteria derived from the Grading of Recommendations Assessment, Development and Evaluation method (GRADE). Points were awarded to the studies if they did not present limitations in study design or execution (risk of bias), inconsistency of results, evidence based on indirect data, imprecision, and publication bias. A score of four to five points was considered as high quality, three points as moderate quality, and zero to two points as low quality.
Data extraction
The data were added to the Review Manager (RevMan 5.3) for analysis. A data extraction table was created to assess the quality of demographic data, study location, sample size, number of cases, number of positives and the diagnostic test.
Data synthesis
The random-effect model meta-analysis method was used to analyze the pooled prevalence of comorbidities in patients and in fatal cases affected by COVID-19 in different parts of the world. The heterogeneity among the studies was analyzed using the Higgins test (I2) that shows the percentage of variation among studies. These analyses were compiled by using the STATA software, version 12 (StataCorp LLC, Texas, USA). The Odds Ratio test, with a 95% Confidence Interval (95% CI), was calculated to measure the likelihood of death for a patient with a comorbidity compared to a patient without comorbidities.
RESULTS
Our search resulted in 1,150 manuscripts related to the search strategies used. The search strategy used for each database was: BVS (Comorbidades OR Comorbidities OR Comorbilidades) AND ((“Infecções por Coronavirus” OR “Coronavirus Infections” OR “Infecciones por Coronavirus”) OR (Betacoronavirus OR Betacoronavirus OR Betacoronavirus) OR (COVID-19) OR (SARS-CoV2)); PUBMED (Comorbidity OR Comorbidities) AND (“Coronavirus Infections” OR Betacoronavirus OR COVID-19 OR SARS-CoV2); CINAHL (Comorbidity OR Comorbidities) AND (“Coronavirus Infections” OR Betacoronavirus OR COVID-19 OR SARS-CoV2); EMBASE 2 (‘comorbidity’/exp OR comorbidity OR ‘comorbidities’/exp OR comorbidities) AND (‘coronavirus infection’/exp OR ‘coronavirus infection’ OR ‘betacoronavirus’/exp OR betacoronavirus OR’ COVID 19’/exp OR ‘ COVID 19’ OR ‘sars cov2’); WEB OF SCIENCE (Comorbidit* AND (“Coronavirus Infections” OR Betacoronavirus OR COVID-19 OR SARS-CoV2); SCOPUS (Comorbidit* AND (“Coronavirus Infections” OR Betacoronavirus OR COVID-19 OR SARS-CoV2).
After applying the eligibility exclusion criteria (duplicate texts, articles related to other topics, text excluded by the review criteria or method quality), 42 studies were considered for analyses5-7,10-48. Of them, 39 were used to calculate the total prevalence of comorbidities in patients affected by COVID-19, six were used to calculate the prevalence of comorbidities in patients admitted to the ICU, and 11 were used to calculate the comorbidity prevalence in fatal cases. The characteristics of the studies included in this meta-analysis are shown in Table 1. The results of the search strategy are shown in a PRISMA flow chart (Figure 1). The data extracted from the final selection are shown in the Supplementary Table S1.
Table 1. A summary of the included studies.
| Study | Country | Total | ICU | Death | M | F | Co % | H % | CV % | D % | COPD % |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al. 5 | China | 99 | N.S. | 11 | 67 | 32 | 50.5 | 0.0 | +40 | 0.0 | 1.0 |
| Wang et al.6 | China | 138 | 36 | 6 | 75 | 63 | 46.4 | 31.2 | 14.5 | 10.1 | 2.9 |
| CDC Korea7 | Korea | 54 | N.S. | 54 | 33 | 21 | 90.7 | 0.0 | 59.3 | 29.6 | 13.0 |
| Cheng et al.10 | China | 698 | 138 | 113 | 367 | 331 | 42.6 | 33.4 | 0.0 | 14.3 | 1.9 |
| Huang et al.11 | China | 41 | 13 | N.S. | 30 | 11 | 31.7 | 15.0 | 6.0 | 8.0 | 1.0 |
| Liu et al.12 | China | 137 | 13 | 16 | 61 | 76 | 19.7 | 9.5 | 7.3 | 10.2 | 17.5 |
| Liu et al.13 | China | 12 | 6 | N.S. | 7 | 5 | 58.3 | 25.0 | 33.3 | 16.6 | 8.3 |
| Guan et al. 14 | China | 1099 | 33 | 15 | 640 | 459 | 23.7 | 15.0 | 2.5 | 7.4 | 1.1 |
| Du et al.15 | China | 109 | 51 | 72 | 74 | 35 | 78.0 | 59.6 | +33.9 | 31.2 | 15.6 |
| Guan et al.16 | China | 1590 | 99 | 50 | 904 | 686 | 25.0 | 20.3 | 3.8 | 9.0 | 1.5 |
| Xu et al.17 | China | 63 | 1 | 0 | 36 | 27 | 31.7 | 8.0 | 0.0 | 2.0 | 2.0 |
| Chen et al.18 | China | 203 | N.S. | 26 | 108 | 95 | 43.3 | 12.9 | 3,4 | 2.7 | 3.9 |
| Liang et al.19 | China | 1590 | 90 | 50 | 904 | 674 | 25.1 | 16.9 | 3.7 | 8.2 | 1.5 |
| Wang et al.20 | China | 399 | N.S. | 65 | 226 | 173 | 60.7 | 40.8 | 17.7 | 16.0 | 6.2 |
| Cao et al.21 | China | 102 | N.S. | 17 | 53 | 49 | 46.1 | 27.5 | 4.9 | 10.8 | 9.8 |
| Zhou et al.22 | China | 191 | 50 | 54 | 119 | 72 | 47.6 | 30.0 | 8.0 | 19.0 | 3.0 |
| Zhang et al. 23 | China | 120 | N.S. | 7 | 43 | 77 | 26.7 | 16.0 | 8.0 | 6.0 | 3.0 |
| Chen et al.24 | China | 274 | N.S. | 113 | 171 | 103 | 48.5 | 34.0 | 8.0 | 17 | 7.0 |
| Zhang et al.25 | China | 140 | N.S. | N.S. | 71 | 69 | 64.3 | 30.0 | 5.0 | 12.1 | 1.4 |
| Wang et al. 26 | China | 69 | N.S. | 5 | 32 | 37 | 36.2 | 13.0 | 12.0 | 10.0 | 6.0 |
| Yang et al. 27 | China | 52 | 37 | 32 | 35 | 17 | 40.4 | 0.0 | 10.0 | 17.0 | 8.0 |
| Wu et al.28 | China | 201 | 53 | 44 | 128 | 73 | 32.8 | 19.4 | 4.0 | 10.9 | 2.5 |
| Huang et al. 29 | China | 34 | 8 | N.S. | 20 | 14 | 47.1 | 23.5 | 17.6 | 11.8 | 2.9 |
| Li et al.30 | China | 83 | 6 | N.S. | 44 | 39 | 18.1 | 6.0 | 1.2 | 7.8 | 6.0 |
| Xu et al. 31 | China | 90 | N.S. | N.S. | 39 | 51 | 50.0 | 19.0 | 3.0 | 6.0 | 1.0 |
| Wu et al.32 | China | 80 | 0 | 0 | 39 | 41 | 47.5 | 0.0 | +31.2 | 6.2 | 1.2 |
| Yang et al. 33 | China | 149 | 0 | 0 | 81 | 68 | 34.9 | 0.0 | +18.7 | 6.0 | 0.7 |
| Liu et al. 34 | China | 3 | N.S. | N.S. | 2 | 1 | 33.3 | 0.0 | 0.0 | 33.3 | 33.3 |
| Lei et al. 35 | China | 34 | 15 | 7 | 14 | 20 | 58.8 | 58.8 | 20.6 | 23.5 | 2.9 |
| Feng et al. 36 | China | 476 | N.S. | 38 | 271 | 205 | 43.1 | 0.0 | 8.0 | 10.3 | 4.6 |
| Yuan et al. 37 | China | 27 | N.S. | 10 | 12 | 15 | 48.1 | 19.0 | 11.0 | 22.0 | 0.0 |
| Mo et al. 38 | China | 155 | N.S. | N.S. | 86 | 69 | 45.8 | 23.9 | 9.7 | 9.7 | 3.2 |
| Wang et al. 39 | China | 116 | 11 | 7 | 67 | 49 | 44.0 | 37.1 | 0.0 | 15.5 | 0 |
| Zhang et al. 40 | China | 221 | 23 | 12 | 108 | 113 | 35.3 | 24.4 | 10 | 10 | 2.7 |
| Guo et al. 41 | China | 256 | 45 | 43 | 91 | 165 | 73.0 | 32.6 | 11.2 | 15.0 | 2.1 |
| Richardson et al. 42 | USA | 5700 | 373 | 553 | 3437 | 2263 | 93.9 | 56.6 | 11.1 | 33.8 | 5.4 |
| Chow et al. 43 | USA | 74439 | 1069 | 2112 | N.S. | N.S. | 3.6 | 0.0 | 9.0 | 10.9 | 9.2 |
| Young et al. 44 | Singapore | 18 | 2 | 0 | 9 | 9 | 27.8 | N.S. | N.S. | N.S. | N.S. |
| Gupta et al.45 | India | 21 | N.S. | N.S. | 14 | 7 | 28.6 | 23.8 | 0.00 | 14.2 | 0.0 |
| Grasselli et al.46 | Italy | 1591 | 1591 | N.S. | 1304 | 287 | 65.5 | 49.0 | 21.0 | 17.0 | 4.0 |
| Du et al.47 | China | 85 | N.S. | 85 | 23 | 62 | 68.2 | 37.6 | 11.8 | 22.4 | 2.5 |
| CDC Korea48 | Korea | 7755 | N.S. | 66 | 37 | 29 | 96.8 | 47.6 | 15.9 | 36.5 | 17.5 |
ICU = Intensive Care Unit; M = Male; F = Female; Co. % = Percentage of patients with comorbidities; H % = Percentage of Chronic Heart Disease; CV % = Percentage of Cardiovascular Disease; D % = Percentage of Diabetes; COPD % = Percentage of Chronic Obstructive Pulmonary Disease; CDC = Center for Disease Control and Prevention; + = Cardiovascular and Cerebrovascular Disease; N.S. = Not Specified
Figure 1. A flowchart of the steps performed in the systematic review.
According to the criteria applied based on GRADE, the studies that met the selection criteria presented high methodological quality with a score of five. The I2 test indicated a low heterogeneity among the studies. Publication bias was not evaluated because the currently available methods are not considered useful for studies on proportions. The summaries of methodological quality and bias risk and applicability for each study and among the included studies are shown in the Supplementary Figures S1 and S2.
Overall prevalence of comorbidities
In the 39 studies used to calculate the pooled prevalence of comorbidities, 89,238 patients affected by COVID-19 were analyzed; 11,341 (12.7%) presented one or more comorbidities, 2,172 (2.4%) were admitted to the ICU, and 3,532 (4 %) patients died. The patients age range was 41 to 70 years. Among these studies, only one was conducted in the USA43, and included a large number of patients (74,439) but did not segregate patients according to sex. In the other 38 studies, 14,844 patients were registered with a total of 8,518 (57.4%) males and 6,413 (42.6%) females. The reported comorbidities included hypertension, heart disease, diabetes, cancer, chronic obstructive pulmonary disease, asthma, chronic diseases of the liver, kidneys, digestive system, autoimmune disorders, immunodeficiencies, stroke, and others. Only one study specified which diseases were included in the category “Others”.
Regarding the geographical distribution of the studied patients, 80,139 (88.7%) were in the USA and 9,051 (10.1%) in China. This study also included 21 cases from India, 54 from South Korea, and 18 from Singapore, representing less than 1% of the total patients included.
The analysis of the general population affected by COVID-19 indicated a 42% pooled prevalence of comorbidities (95% CI: 25-60; weight 100%). In China, the geographical distribution analysis showed a 43% prevalence of comorbidities (95% CI: 37-48; weight 89.4%), followed by the USA with 8% (95% CI: 7-8; weight 5.34%), India 29% (95% CI: 14-50; weight 2.59%), and Singapore 28% (95% CI: 12 -51; weight 2.58%) (Figure 2).
Figure 2. Forest plot for a random-effect meta-analysis of comorbidities in all the patients affected by COVID-19.
Among those who had one or more previous diseases, there was a total of 16,222 comorbidities. Hypertension was the most prevalent in 32% (95% CI: 31-33; weight 6.54%), followed by diabetes 22% (95% CI: 21-23; weight 6.57%), heart disease 13% (95% CI: 13-14; weight 6.62%), and Chronic Obstructive Pulmonary Disease (COPD) 8% (95% CI: 7-8; weight 6.65%). In addition to these, other comorbidities were also assessed, such as kidney disease (5%), cancer (3%), asthma (3%), liver disease (2%), stroke (2%), immunodeficiencies (2%), and others (8%). The pooled prevalence with 95% CI values for each disease are shown in Table 2.
Table 2. Overall prevalence of comorbidities, in the group admitted to the ICU and in the fatal cases by COVID-19.
| Comorbidity | Overall Prevalence | ICUs Patients | Fatal Cases | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| PP | 95% CI | W % | PP | 95% CI | W % | PP | 95% CI | W % | |
| Hypertension | 32 | 31 - 33 | 6.54 | 27 | 25 - 29 | 6.86 | 35 | 31- 38 | 8.10 |
| Chronic Heart Disease | 13 | 13 - 14 | 6.62 | 18 | 18 - 19 | 7.15 | 17 | 14 - 20 | 8.61 |
| Diabetes | 22 | 21 - 23 | 6.57 | 17 | 15 -19 | 7.17 | 19 | 16 - 22 | 8.53 |
| Malignancy | 3 | 3 - 4 | 6.68 | 5 | 4 - 6 | 7.81 | 5 | 4 -7 | 9.22 |
| COPD | 8 | 7 - 8 | 6.65 | 7 | 6 - 8 | 7.67 | 9 | 7 -11 | 9.03 |
| Asthma | 3 | 3 - 3 | 6.69 | 0 | 0 - 0 | 0.00 | 0 | 0 - 0 | 0.00 |
| Chronic Kidney Disease | 5 | 5 - 5 | 6.67 | 5 | 6 - 8 | 7.81 | 4 | 3 - 6 | 9.29 |
| Chronic Liver Disease | 2 | 1- 2 | 6.7 | 2 | 4 - 6 | 8.01 | 3 | 2 - 4 | 9.42 |
| Cerebrovascular Accident | 2 | 1- 3 | 6.7 | 1 | 1 - 2 | 8.05 | 6 | 5 - 9 | 9.15 |
| Immunodeficiency | 2 | 2 - 3 | 6.69 | 2 | 1 - 3 | 7.97 | 0 | 0 - 0 | 0.00 |
| Autoimmune Disease | 0 | 0 - 0 | 6.71 | 0 | 0 - 0 | 8.12 | 0 | 0- 1 | 9.57 |
| Cardiovascular and Cerebrovascular Accident | 1 | 1 - 1 | 6.71 | 0 | 0 - 0 | 0.00 | 0 | 0 - 0 | 0.00 |
| Digestive Disease | 0 | 0 - 0 | 6.71 | 0 | 0 - 1 | 8.11 | 0 | 0 - 1 | 9.60 |
| Peripheral Vascular Disease | 0 | 1 - 0 | 6.71 | 0 | 0 -0 | 8.12 | 0 | 0 - 0 | 0.00 |
| Other | 8 | 7 - 8 | 6.65 | 18 | 16 - 19 | 7.15 | 2 | 1 - 3 | 9.48 |
|
| |||||||||
| Overall | 7 | 5 - 8 | 100 | 7 | 6 - 8 | 100 | 9 | 6 - 11 | 100 |
ICU = Intensive Care Unit; PP = Pooled Prevalence; W = Weight; COPD = Chronic Obsctructive Pulmonary Disease; CI = Confidence Interval.
Prevalence of comorbidities in ICU patients
Of the six studies that conducted descriptions of the epidemiological and clinical profiles in patients admitted to the ICU, five divided the data according by sex. In these five studies, 1,661 patients were described6,11,13,36,48. Among these patients, 1,345 (81%) were male, 316 (19%) were female, and the age range was 46 to 63 years. The clinical characteristics of 2,730 patients were also described, indicating that 1,449 (53%) had one or more comorbidities. In total, there were 2,050 comorbidities among patients admitted to the ICU.
The pooled prevalence of comorbidities in ICU patients was 61% (95% CI: 42-80; weight 100%). The geographical distribution analysis showed a 69% prevalence of comorbidities (95% CI: 52-86; weight 61.09%) in China, followed by Italy, with 66% (95% CI: 63-68; weight 19.47%), and the USA, with 33% (95% CI: 31-36; weight 19.44%). The forest plot for a random-effect meta-analysis of comorbidities in patients admitted to ICUs by COVID-19, are shown in the Supplementary Figure S3.
The most prevalent comorbidities in the ICU population were hypertension 26% (95% CI: 25-29; weight 6.86%), heart disease 18% (95% CI: 16-19; weight 7.15%), diabetes 17% (95% CI: 16-19; weight 7.17%), and others 17% (95% CI: 16-19; weight 7.15%). In addition to these diseases, patients with COPD (7%), cancer (5%), kidney disease (5%), liver disease (2%), and stroke (1%) were also evaluated. The pooled prevalence with the 95% CI values for each disease is shown in Table 2.
Prevalence of comorbidities among mortality cases
Eleven studies included descriptions of the epidemiological and clinical profiles of a total of 624 cases of mortality. In these studies, 394 patients were males and 218 females, with an age range between 64 and 70 years. Among the 624 fatal cases, 415 of the patients had one or more previous diseases, totaling 751 comorbidities. The pooled prevalence of comorbidities among the fatal cases was 77% (95% CI: 68-86; weight 100%). Only two countries were analyzed in the geographical distribution: China, with 71% (95% CI: 63-82; weight 76.79%) and Korea, with 92% (95% CI: 87-97; weight 23.21%) (Figure 3).
Figure 3. Forest plot for a random-effect meta-analysis of comorbidities in fatal cases of COVID-19.
The most prevalent comorbidities in this population were hypertension 35% (95% CI: 25-29; weight 8.10%), diabetes 19% (95% CI: 16-22; weight 8.53%), heart disease 17% (95 % CI: 14-20; weight 8.61%), and COPD 9% (95% CI: 7-11; weight 9.22%). In addition to these diseases, patients with cerebrovascular accident (6%), cancer (5%), kidney disease (4%), liver disease (3%), and other (2%) were also evaluated. The pooled prevalence with 95% CI values for each disease is shown in Table 2.
Odds ratio
The probability of a patient with comorbidity of dying from COVID-19, and the significance of this associations using the Fisher’s exact test, were calculated. The number of patients with comorbidities who died and those who survived, in addition to the patients without comorbidities who died and who survived, were used to calculate an odds ratio of 2.4 with 95% CI 1.7-3.3 and in the Fisher’s exact test the value of P < 0.0001.
DISCUSSION
This meta-analysis was based on 42 studies, including a large number of descriptions from China and the United States. Studies conducted in India, Italy, the United Kingdom, South Korea, and Singapore were also analyzed. A higher prevalence of male patients infected with COVID-19 was observed compared to females. This predisposition of the male sex was also observed in the diseases MERS-CoV and SARS-Co, which are also caused by viruses of the coronavirus family49,50.
The pooled prevalence of comorbidities in the general population of patients affected by the new coronavirus (COVID-19) was 42% (95% CI: 26–59). China was the country with the highest prevalence, although there were also more studies analyzed from this country. However, it is important to highlight that two studies from the United States resulted in contrasting prevalence values (4% and 94%). Since the United States is the country that leads the statistics so far with the highest number of confirmed cases (more than one million) and deaths from coronavirus (more than seventy thousand), on May 8, 2020, it is of utmost importance to publish more data on the clinical characteristics of the disease in this country.
The results of this study confirm that the prevalence of comorbidities increases as the patient’s clinical conditions worsens. In the general population affected by COVID-19, the prevalence of comorbidities was 42%, 61% among patients admitted to the ICU, and 77% among fatal cases. Males were the most affected in the three groups. On the other hand, the mean age also increases when we compare the group of patients in general with the group of fatal cases, as previously described among risk factors such as age, sex, and comorbidities4-7.
Regarding comorbidities, in the three groups analyzed (general population, admission to ICU, and fatal cases), hypertension was the most prevalent comorbidity, accounting for 32%, 26%, and 35%, respectively. In the general population, diabetes was the second-most prevalent (22%) comorbidity, followed by heart disease (13%) and COPD (8%). However, in patients admitted to the ICU, diabetes (17%) and heart disease (18%) showed similar values. The same phenomenon was observed in fatal cases, with diabetes (19%), and heart disease (17%) showing similar values. Considering that type 1 diabetes mellitus usually manifests during childhood or adolescence, type 2 diabetes frequently manifests in adults, and heart diseases are more prevalent in older patients, one may think that the earlier onset of diabetes may account for it to rank second among the comorbidities in the general population affected by COVID-19. On the other hand, the group of fatal cases is composed of predominantly older adults, a population in which hypertension, diabetes, and heart disease are prevalent.
The odds ratio for any comorbidity was 2.4 with 95% CI 1.7-3.3 with a statistical significance of P < 0.0001. In other words, a patient with a comorbidity has 2.4 times the chance of dying from COVID-19 compared to a patient without a comorbidity. This may explain the high prevalence of comorbidities among fatal cases,
In developing this study, we encountered several limitations. Firstly, not all studies segregated epidemiological and clinical data (age, sex, percentage of comorbidity, and patients hospitalized in the ICU). Secondly, some studies classified comorbidities in the “Other” category, but only one study described which diseases were comprised in this category. Thirdly, since China is the primary focus of the rise of the pandemic, most of the studies included were from this country. No studies from Africa, Oceania, or Latin America were found. Finally, in meta-analyses, it is recommended that publication bias are always assessed by statistical methods. However, currently available methods, such as the funnel plot and the Egger regression test, are not considered useful tools in studies on proportions51.
One can conclude that the existence of comorbidities increases the probability of dying from COVID-19 by 2.4 times compared to those who do not have pre-existing conditions. The most relevant comorbidities were shown to be hypertension, heart disease, and diabetes. Thus, comorbidities are more prevalent in the group of mortality cases when compared to the general population group. However, these conclusions are based on the evidence obtained, mostly from studies conducted in China. For this reason, studies describing the epidemiological and clinical profiles of COVID-19 cases in Africa, Oceania, and Latin America are recommended to clarify the behavior of this disease in these regions, and, thus, be able to apply effective measures aimed at safeguarding populations at risk.
SUPPLEMENTARY MATERIAL.
Table S1. PRISMA Checklist.
| Section/topic | # | Checklist item | Reported on page # |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | Title |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | Abstract |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | Introduction |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | Introduction and Methods: Review Question. |
| METHODS | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. | Methods |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | Methods: Inclusion Criteria |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | Methods: Search Strategy |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | Methods: Search Strategy |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | Methods: Study Strategy |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | Methods: Data extraction |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | Methods: Data extraction/Quality assessment |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | Additional File. Figure S1. |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | Methods: Data Synthesis |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | Methods: Data Synthesis |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | Additional File. Figure S2. |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | Methods: Data Synthesis |
| RESULTS | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | Results (Figure 1) |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | Results (Table 1) |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | Additional File. Figure S2 and Figure S1. |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | Results. Figure 2, 3 and 4. |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | Results (Figures 2, 3 and 4) |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | Additional File. Figure S2. |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). | Results (Odds Ratio) |
| DISCUSSION | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). | Discussion |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | Discussion |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | Conclusion |
| FUNDING | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | NA |
Figure S1. The methodological quality summary bias risk concern and applicability for each study.
Figure S2. The methodological quality summary bias risk concern and applicability for across the included studies.
Figure S3. The forest plot for a random-effect meta-analysis of comorbidities in patients admited in ICUs.
REFERENCES
- 1.World Health Organization [cited 2020 Jun 13];Coronavirus disease (COVID-19): situation report - 124. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200523-covid-19-sitrep-124.pdf?sfvrsn=9626d639_2
- 2.Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Crosten C, Gulyaeva AA, et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicatingperson-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med. 2020;8:e20. doi: 10.1016/S2213-2600(20)30117-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korean Society of Infectious Diseases. Korea Centers for Disease Control and Prevention Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J Korean Med Sci. 2020;35:e132. doi: 10.3346/jkms.2020.35.e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins JP, Green S, editors, editors. Cochrane handbook for systematic reviews of interventions: version 5.1.0. London: The Cochrane Collaboration; 2011. [cited 2020 Jun 13]. http://handbook-5-1.cochrane.org/ [Google Scholar]
- 10.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020;133:1025–1031. doi: 10.1097/CM9.0000000000000744. Engl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Du RH, Liu LM, Yin W, Wang W, Guan LL, Yuan ML, et al. Hospitalization and critical care of 109 decedents with COVID-19 pneumonia in Wuhan, China. Ann Am Thorac Soc. 2020 doi: 10.1513/AnnalsATS.202003-225OC. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li WM, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen T, Dai Z, Mo P, Li X, Ma Z, Song S, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study. J Gerontol A Biol Sci Med Sci. 2020 doi: 10.1093/gerona/glaa089. glaa089 In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang WH, Guan WJ, Li CC, Li YM, Liang HR, Zhao Y, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicenter) and outside Hubei (non-epicenter): a nationwide analysis of China. Eur Respir J. 2020;55:2000562. doi: 10.1183/13993003.00562-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang L, He W, Yu X, Hu D, Bao M, Liu H, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80:639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cao J, Tu WJ, Cheng W, Yu L, Liu YK, Hu X, et al. Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa243. ciaa243 In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang R, Ouyang H, Fu L, Wang S, Han J, Huang K, et al. CT features of SARS-CoV-2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur Radiol. 2020 doi: 10.1007/s00330-020-06854-1. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen T, Wu D, Chen H, Yan W, Yan D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1111/all.14238. In Press. [DOI] [PubMed] [Google Scholar]
- 26.Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa272. ciaa272 In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang Y, Tu M, Wang S, Chen S, Zhou W, Chen D, et al. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China: a retrospective single center analysis. Travel Med Infect Dis. 2020:101606. doi: 10.1016/j.tmaid.2020.101606. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55:327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J, Liu J, Zhao X, Liu C, Wang W, Wang D, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu Province: a multicenter descriptive study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa199. ciaa199 In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang W, Cao Q, Qin L, Wang X, Cheng Z, Pan A, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80:388–393. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu C, Wu C, Zheng X, Zeng F, Liu J, Wang P, et al. Clinical features and multidisciplinary treatment outcome of COVID-19 pneumonia: a report of three cases. J Formos Med Assoc. 2020 doi: 10.1016/j.jfma.2020.04.008. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feng Y, Ling Y, Bai T, Xie Y, Huang J, Li J, et al. COVID-19 with different severities: a multi-center study of clinical features. Am J Respir Crit Care Med. 2020;201:1380–1388. doi: 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yuan M, Yin W, Tao Z, Tan W, Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS One. 2020;15:e0230548. doi: 10.1371/journal.pone.0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mo P, Xing Y, Xiao Y, Deng L, Zhao Q, Wang H, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa270. ciaa270 In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang L, Li X, Chen H, Yan S, Li D, Li Y, et al. Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. Am J Nephrol. 2020;51:343–348. doi: 10.1159/000507471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang G, Hu C, Luo L, Fang F, Chen Y, Li J, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020:e201017. doi: 10.1001/jamacardio.2020.1017. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chow N, Fleming-Dutra K, Gierke R, Hall A, Hughes M, Pilishvili T, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 — United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Young BE, Ong SW, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323:1488–1494. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gupta N, Agrawal S, Ish P, Mishra S, Gaind R, Usha G, et al. Clinical and epidemiologic profile of the initial COVID-19 patients at a tertiary care centre in India. 1294Monaldi Arch Chest Dis. 2020;90 doi: 10.4081/monaldi.2020.1294. [DOI] [PubMed] [Google Scholar]
- 46.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020;201:1372–1379. doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.COVID-19 National Emergency Response Center. Epidemiology and Case Management Team. Korea Centers for Disease Control and Prevention Coronavirus disease-19: the first 7,755 cases in the Republic of Korea. Osong Public Health Res Perspect. 2020;11:85–90. doi: 10.24171/j.phrp.2020.11.2.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017;198:4046–4053. doi: 10.4049/jimmunol.1601896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murad MH, Chu H, Lin L, Wang Z. The effect of publication bias magnitude and direction on the certainty in evidence. BMJ Evid Based Med. 2018;23:84–86. doi: 10.1136/bmjebm-2018-110891. [DOI] [PMC free article] [PubMed] [Google Scholar]