Abstract
The objectives of the study were to identify the prevalence of insomnia among a representative sample of the Lebanese population and to assess potential factors associated with insomnia among this group. A cross-sectional study was done in the Lebanese population from August 2017 to April 2018 enrolling 789 participants using a proportionate random sample from all five Lebanese governorates. Participants filled a self-administered Arabic questionnaire. The Athens Insomnia Scale was used to diagnose insomnia. The Hamilton Depression Rating Scale and the Generalized Anxiety Disorder Scale were used to measure depression and anxiety, respectively. The prevalence of insomnia was 47.1% in the population sampled. The mean age of the participants was 37 years (64% females). Death in the family [adjusted odds ratio (aORa) = 1.59], drinking caffeine before sleep more than 2 days per week compared to none (aORa = 1.57), increased stress (aORa = 1.03), increased depression (aORa = 1.14), and anxiety scores (aORa = 1.07) were associated with higher odds of insomnia. The prevalence of insomnia was very high in the Lebanese population, and it was mainly associated with modifiable, treatable risk factors. Improved knowledge and adequate screening for insomnia are needed to promote better sleep quality.
Keywords: Insomnia, prevalence, factors, depression, anxiety
1. INTRODUCTION
Over the years and so far, epidemiologic data suggest a rise in insomnia and sleep difficulties worldwide [1]. According to the Centers for Disease Control and Prevention in the United States, sleep insufficiency is considered a capital public health concern showing an estimated 50–70 million U.S. adults having sleep-related difficulties [1]. Its actual prevalence varies extensively from 10% to 30% of the population [2]. Interestingly, an international survey investigated the prevalence and impact of insomnia in France, Italy, Japan, and the United States, and the estimated prevalence of insomnia ranged between 6.6% (France and Italy) and 37.2% (USA) with a consequential altered daily quality of life [3]. Multiple explanations have been offered for this wide range of prevalence rates related, in part, to the inconsistencies in insomnia definition, diagnostic criteria, and time interval, but to a larger extent to the populations studied [2].
In the Middle East, despite the fact that sleep specialists estimate an increasing number of people suffering from sleep disorders, especially insomnia, studies related to its prevalence, risk factors, and the impairment of quality of life are sparse. In Lebanon, insomnia is now recognized as a major public health concern [4]. Almost all existing publications concern mainly university students and none was carried out at the population level. A study conducted in Lebanon among university students revealed that 37.1% of participants are poor sleepers, with insomnia being the main cause of this poor sleep quality; a strong association between anxiety and insomnia was detected in that study as well [4].
Recently, insomnia has been identified as a disorder as well as a symptom of psychiatric and medical disorders [5]. Insomnia and anxiety often coexisted; especially that a clear overlap in symptoms is present [5]. An early morning awakening is considered a hallmark symptom of depression, and resolution of insomnia is a predictor for a favorable response to depression treatment [6].
Predisposition to insomnia concerns to some degree the person himself and people around him [2]. A precipitating event, a perceived stressful life may contribute to its onset where many predisposing psychological and physiological, behavioral, and lifestyle factors have been incriminated [2]. Previous findings showed that aging, female gender, living alone, maladaptive sleep habits related to hectic work schedules, smoking, stressful life events, chronic pain, and medication use were also incriminated risk factors for insomnia [7–9].
In Lebanon, large general population studies are sparse. That is why our research shows interest in identifying the prevalence and potential factors associated with insomnia complaints among a representative sample of the Lebanese population.
2. METHODOLOGY
2.1. Study Design and Sampling
A cross-sectional study, using a balanced random sampling from all six Lebanese governorates, was carried out over a period from August 2017 and April 2018, recruiting community-dwelling participants. The Central Agency of Statistics in Lebanon provided a list of villages from which we chose two in each caza (stratum) of every governorate. Governorates were proportionally represented. Participants were randomly selected from each village.
2.1.1. Inclusion criteria
Individuals who were 18 years old and more.
2.1.2. Exclusion criteria
(1) Self-reported psychiatric and psychotic problems (self-reported schizophrenia, bipolar disorder), (2) mental retardation or dementia, and (3) refusal to fill the questionnaire. A total of 77 participants were excluded. Individualized interviews were carried out by trained, neutral personnel.
2.2. Minimal Sample Size Calculation
Based on a 12.2% expected frequency of insomnia in the population [10] in the absence of similar studies in Lebanon, the minimal sample size calculated according to the Epi Info software version 7.2 (population survey) was 330 participants to ensure a confidence level of 95%. Of 900 participants who were approached, 756 (84%) accepted to participate. The nonresponse rate was 16%. The reason for oversampling is that this study is part of a big project about insomnia, in which other papers necessitated a bigger sample size.
2.3. Data Collection and Measurement
The preparation of the questionnaire was based on the fact that Arabic is the native language in Lebanon, with an average time between 15 and 20 min needed to complete it. Questions covered different aspects: the first part included sociodemographic characteristics (gender, age, region, marital status, educational level, profession, family income, number of children, work schedules, monthly income). The second part included questions about personal and family history of insomnia, chronic pain, medication, and known, likely, hypothesized risk factors for insomnia.
Since cigarette and Water pipe (WP) dependence are known to increase markedly the likelihood of insomnia [11], we decided to use the Fagerstrom scale [12] (Cronbach’s alpha: 0.889) and the Lebanon Waterpipe Dependence Scale-11 [13] (Cronbach’s alpha: 0.911) to assess dependence to cigarette and WP smoking, respectively.
Mental and psychological distress are evaluated using a Lebanese adapted scale, the Beirut Distress Scale (BDS-22) [14]. Answers were assessed using a Likert scale from 0 (never) to 3 (very much) asking about many symptoms such as depression, feeling of emptiness, anxiety, concentration, and memory issues and other possible health-related consequences of stress. The global score ranged from 0 to 66 and is created by adding all the answers for respective items of the score. A score of 25 or more is indicative for high risk of psychological distress [14]. The Cronbach’s alpha for this scale was 0.939.
The Hamilton Depression Rating Scale, validated among the Lebanese population [15], reposes on 21 items rating the severity of depression in the last week. It pertains to feelings of guilt, suicidal thoughts, insomnia, work and interests, retardation, and many other depressive symptoms. The scoring is based on a 0 (none/absent) to 4 (most severe) spectrum, a 0–3 spectrum, or a 0–2 spectrum, and the total score consists of the sum of the items. A score of 0–7 indicates no depression, 8–13 mild depression, 14–18 moderate depression, and 19–22 severe depression, and a score of 23 and more indicates a very severe depression [16]. The Cronbach’s alpha for this scale was 0.844.
The seven items Generalized Anxiety Disorder Scale (GAD-7), previously validated in Lebanon [17], allows an adequate assessment for anxiety, and it contains seven questions that ask how often during the last 2 weeks participants’ experienced excessive worry, irritability, and difficulty in relaxing [18]. As for the response options, it included “not at all,” “several days,” “more than half the days,” and “nearly every day,” and each one matched respectively 0, 1, 2, and 3. The global score ranges from 0 to 21. Thus, 5, 10, and 15 correspond to three corresponding categories: mild, moderate, and severe levels of anxiety on the GAD-7 scale. The Cronbach’s alpha for this scale was 0.925.
The Athens insomnia scale (AIS), an instrument that was validated in Lebanon [19], is composed of eight items constructed to allow a proper self-assessment of the intensity of sleep difficulty related to International Classification of Diseases (ICD-10) criteria mainly [20]. The presence of insomnia was determined if the total score was 6 or above. The Cronbach’s alpha for this scale was 0.829.
Diagnostic and Statistical Manual of Mental Disorders (DSM-V) insomnia disorder criteria were applied to give a rigorous diagnosis of insomnia. It includes some major touchstones related to sleep quality and quantity satisfaction, sleep difficulties, difficulty initiating sleep, and difficulty maintaining sleep, early morning awakening or a nonrestorative sleep, major repercussions on daily personal functioning caused by the sleep difficulty, for at least three times a week over a period of at least 3 months, despite adequate conditions for sleeping [20]. Insomnia is considered if they answered several times per week for one or more criterion. A lot of questionnaires meet those criteria including ours, making it global and thorough.
Translation of all scales to Arabic was performed by a certified translator and then a second certified translator translated the Arabic version back to English. English versions did not differ significantly; therefore, the translated Arabic version was used as is.
2.4. Statistical Analysis
Statistical analysis was performed using SPSS software version 23 (IBM SPSS Statistics for Windows, Armonk, New York, USA). Weighting to the general population was performed regarding gender, age, and governorate of dwelling. The official numbers of the Ministry of Public Health in Lebanon were used [21]. Means and standard deviations and frequencies and percentages were used to describe continuous and categorical variables, respectively. The Shapiro–Wilk test was used to check for the normal distribution of the sample. Differences between means were done using the Student’s t-test, whereas comparison between categorical variables was done using the Chi-square test.
Association between multiple factors including sociodemographic characteristics of study participants and insomnia was evaluated using both bivariate and multivariable analyses. A multiple logistic regression was carried out using variables that showed a p < 0.2 in the bivariate analysis (Supplementary Table 1) [22], in order to eliminate potential confounders as much as possible [23]. In the multiple logistic regression, the dichotomized presence/absence of insomnia was used as the dependent variable. Significance was defined as a p value less than 0.05. Moreover, the Cronbach’s alphas were calculated for each scale for internal consistency and reliability analysis.
3. RESULTS
The mean age of the participants was 37.00 ± 15.54 years (64% females). More sociodemographic characteristics of the participants can be found in Table 1.
Table 1.
Sociodemographic characteristics of the sample population
| Frequency (%) | ||
|---|---|---|
| Gender | Male | 272 (36.0) |
| Female | 484 (64.0) | |
| Living alone | Yes | 60 (7.9) |
| No | 696 (92.1) | |
| Education level | Primary | 2 (0.3) |
| Complementary | 39 (5.2) | |
| Secondary | 210 (27.8) | |
| University | 505 (66.8) | |
| Family monthly salary | No income | 238 (31.5) |
| <450 USD | 75 (9.9) | |
| 450–1000 USD | 237 (31.3) | |
| 1000–2000 USD | 162 (21.4) | |
| >2000 USD | 44 (5.8) | |
| District | Beirut | 203 (26.9) |
| Mount Lebanon | 460 (60.8) | |
| North Lebanon | 36 (4.8) | |
| South Lebanon | 44 (5.8) | |
| Bekaa | 13 (1.7) | |
| Marital status | Single | 409 (54.1) |
| Married | 292 (38.6) | |
| Divorced | 22 (2.9) | |
| Widowed | 33 (4.4) | |
| Smoking | Yes | 160 (21.2) |
| No | 596 (78.8) | |
| Water pipe | Yes | 175 (23.1) |
| No | 581 (76.9) | |
| Mean ± standard deviation | ||
| Age (years) | 37.00 ± 15.54 | |
| Alcohol to sleep | 0.12 ± 0.89 | |
| Body mass index (kg/m2) | 25.04 ± 4.34 | |
3.1. Prevalence of Insomnia Complaints
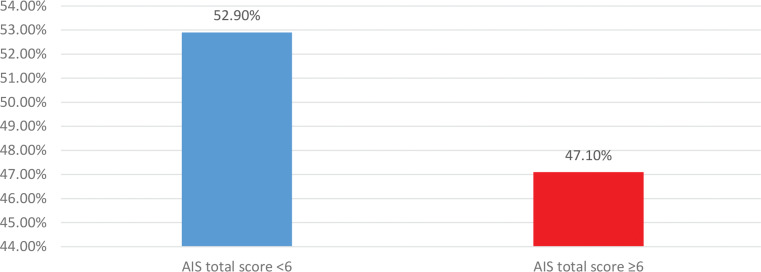
According to the AIS, the prevalence of insomnia in our sample was 47.1%, with 356 participants having an AIS score ≥6 (Figure 1). The mean score was 6.10 ± 4.39, with a 95% confidence interval of 5.78–6.41. The minimum score in our sample was 0 and the maximum score was 23.
Figure 1.
Description of participants with and without insomnia among the Lebanese population. AIS, Athens Insomnia Scale; 95% confidence interval [0.469–0.533]
3.2. Multivariable Analysis
The results of a backward logistic regression, taking the presence/absence of insomnia (Athens score ≥6 and <6, respectively) as the dependent variable, showed that having a death in the family [adjusted odds ratio (aORa) = 1.741], having stressful situations (divorce/unemployment) in one’s life (ORa = 2.292), drinking caffeine before sleep less than once a month (ORa = 2.073) and at least once a week (ORa = 2.964), and eating heavy before sleep 2–6 days a week (ORa = 2.02) were associated with higher odds of insomnia. Moreover, higher stress (ORa = 1.044), depression (ORa = 1.107), and anxiety scores (ORa = 1.056) were associated with higher odds of insomnia. Finally, exercising (ORa = 0.675) was associated with lower odds of insomnia (Table 2).
Table 2.
Multivariable analysis. Logistic regression taking the dichotomous Athens score variable (presence vs absence of insomnia) as the dependent variable
| p-value | ORa | Confidence interval | ||
|---|---|---|---|---|
| Lower bound | Lower bound | |||
| Death in the family last year (yes vs no*) | 0.001 | 1.741 | 1.252 | 2.422 |
| Stressful situations (divorce/unemployment) (yes vs no*) | <0.001 | 2.292 | 1.594 | 3.295 |
| Caffeine before sleep** | 0.008 | |||
| Caffeine before sleep less than once a month | 0.037 | 2.073 | 1.046 | 4.109 |
| Caffeine before sleep at least once a month | 0.776 | 0.880 | 0.365 | 2.124 |
| Caffeine before sleep at least once a week | 0.001 | 2.964 | 1.524 | 5.767 |
| Caffeine before sleep every day | 0.349 | 1.226 | 0.800 | 1.877 |
| Exercise (yes vs no*) | 0.047 | 0.675 | 0.459 | 0.995 |
| Eat heavy before sleep** | 0.069 | |||
| Eat heavy before sleep <2 days weekly | 0.087 | 1.390 | 0.953 | 2.026 |
| Eat heavy before sleep 2–6 days per week | 0.020 | 2.020 | 1.117 | 3.654 |
| Eat heavy before sleep daily | 0.912 | 1.053 | 0.419 | 2.650 |
| Stress score (BDS-22) | <0.001 | 1.044 | 1.023 | 1.064 |
| Depression score (HAM-D) | <0.001 | 1.107 | 1.069 | 1.146 |
| Anxiety score (GAD) | 0.011 | 1.056 | 1.013 | 1.100 |
| Body mass index | 0.024 | 1.046 | 1.006 | 1.088 |
| Number of medications taken per day | 0.098 | 1.124 | 0.979 | 1.291 |
Reference group.
Compared to no caffeine drinking or no heavy eating before sleep. Variables entered: family monthly income, family insomnia problems, death in the family last year, verbal assault, stressful situations (divorce/unemployment), alcohol intake frequency, coffee intake frequency, exercise, family history of psychiatric disorders, chronic pain, psychiatric diseases, caffeine before sleep, eat heavy food before sleep, number of chronic diseases, medications, BDS-22, HAM-D, GAD, body mass index, number of medications taken daily.
BDS, Beirut Distress Scale; GAD, Generalized Anxiety Disorder Scale; HAM-D, Hamilton depression.
4. DISCUSSION
This cross-sectional study, the fourth out of a big project about insomnia in the general Lebanese population, executed on a balanced random sample of Lebanese participants is the first to reflect an estimate of 47.1% of the Lebanese population having insomnia according to AIS. Some risk factors were associated with insomnia, mainly a death in the family last year, caffeine intake before sleep, increased stress, the presence of depression, and anxiety.
4.1. Prevalence of Insomnia
The prevalence of insomnia worldwide varies between 10% and 30% of the population, knowing that in some findings it climbs up to 50–60% [6,24]. It is important to mention that the wide range of estimated prevalence can be explained by the lack of comparable methodology, study design and inconsistencies in definitions, and diagnostic criteria for insomnia. In our present study, we obtained an alarming number going up to a prevalence of 47.1% broadly consistent with the findings of the international survey of sleeping problems in the United States, Europe, and Japan and this survey revealed a prevalence of sleeping problems of 56% in the United States, 31% in Western Europe, and 23% in Japan [25], whereas our study showed a much higher rate compared to a study done in the Family Medicine Outpatient Department at St. Philomena’s Hospital, Bengaluru, where 33% of the adult population sampled had chronic insomnia [26]. This high prevalence might be due to the fact that Lebanon had witnessed a series of wars, local armed combats, and terrorist attacks [27], in addition to a series of crises including clean water penury, electrical power, and waste management had overwhelmed the country [27]. Moreover, a high number of Syrian refugees had led to high levels of unemployment and competition for employment with locals.
4.2. Insomnia Risk Factors
Death in the family is known to cause sleep disturbances [28]. The findings of our study goes hand in hand with a study conducted in Canada, a study that provides supportive evidence of the fact that insomniacs have experienced more negative stressful life events prior to the incidence of insomnia when comparing to good sleepers [2].
Emotional factors have been assessed in multiple studies investigating insomnia because discontent people, individuals going through separation, divorce, and grief are more prone to report chronic insomnia [29]. In our study, higher odds of insomnia were found in divorced and unemployed individuals. It can be explained by disturbed unstable interpersonal relations, interrupted coping mechanisms, and a state of emotional hyper arousal [30]. In terms of low educational and economical level, as well as unemployment, insomnia is more frequently described [31]. It is true that insomnia among other causes of poor mental health increases the risk of job loss but in return unemployment with its high social burden and financial insecurities increases the likelihood of insomnia, highlighted in our study findings.
According to previous findings, excessive caffeine intake has numerous adverse effects not only restricted to the cardiovascular system but also in terms of sleep disturbances [32]. Our study showed that high caffeine intake, especially before sleep, more than 2 days per week was highly correlated with increased risk of developing of insomnia. This comes in line with the reports of Drake et al. [33] which explain about potential caffeine disruptive effects at 0, 3, and 6 h before sleep, concluding that high caffeine intake, particularly in the early evening hours, will have a negative impact on total sleep duration.
Preliminary findings suggest that eating habits and patterns can alter sleep architecture and quality [34]. Shortened sleep duration was described by Tanaka et al. [35] in individuals on high-energy diet, especially fat, carbohydrates, and protein. Despite the fact that epidemiologic data reported that a Mediterranean dietary profile is associated with fewer insomnia symptoms in women [11], our study showed higher odds of insomnia in the Lebanese population, particularly when eating heavy food before sleeping.
Stress-related insomnia has been described as difficulties in falling and staying asleep and short sleep duration because stress in general leads to hyper arousal state [12]. When it comes to predictors of sleep duration and quality of sleep, psychological distress and self-perceived health status are both considered as strong predictors [35]. We were able to describe a strong correlation between psychological distress and insomnia. Our research revealed results synonymous with the DRIVE study that showed a clear association between prevalent psychological distress and self-reported short sleep duration [11].
Depression and anxiety are known to be the most common comorbidities associated with insomnia [13]. Despite that, the extent to which these two medical problems trigger insomnia or represent its consequences remains poorly stated. In fact, Coleman et al. [36] have reported that emotional and mental disorders appear to play an important role in the relevance of this condition. Previous research refers repeatedly to the interrelation between sleep disorders and depression. Attention was drawn to the fact that these two conditions induce poor performance in executive function tasks. For Snyder et al. [37], these roles are highly lessened in major depression but only susceptible to poor sleep according to Shekleton et al. [38]. As already stated within the DSM-IV criteria, poor sleep can be a predictor of another disorder, specifically depression. Additionally, Da Rocha et al. insist on this pertinent association too [26]. Regardless the fact that anxiety is an entity by itself, many potential overlapping symptoms with sleep disturbances and more specifically insomnia were discussed in numerous reports. Hasler et al. [39] suggested that daytime sleepiness secondary to sleep night disturbances mostly is mediated by comorbid anxiety. Furthermore, Johnson et al. [40] found that the rate varies with anxiety profiles. Our study conveys as well a supportive advancing knowledge concerning the previously mentioned comorbidities. It highlights the strong contribution in acquiring these conditions together. So, at the very least, participants should be assessed for the three disorders and thus drawing out the way to prevent it and, if needed, intervene.
Exercise training has a remarkable effect on body clock by causing an increase in body temperature, whereas post exercise, the decrease in body temperature modifies the circadian rhythm and promotes sleep. From here, physiologically speaking, we can say that exercise prevents to some degree insomnia by favoring sleep [41]. Our study results come to support exercising for being among proposed low cost, first-line non-pharmacological approaches to chronic insomnia. The “Sleep in America” poll conducted by the National Sleep Foundation concluded that individuals of 55–84 years of age who exercised more frequently complained about insomnia less than those exercising less than one time per week [42]. Adding to this, a British study added to the evidence that regular physical activity can be considered as preventive approach for late-life insomnia [43].
4.3. Limitations
We acknowledge that with the small sample size, refusal rate, and sample representativeness, our study is not representative of the whole Lebanese population. Additionally, despite the fact that the questionnaire prepared covered most commonly hypothesized potential insomnia risk factors according to the literature, some other risk factors were not included and could be the objectives of future studies. An overestimation of the symptoms and subjective measures might be possible, predisposing us to an information bias. No causality can be inferred from the cross-sectional design of this study. To know the sensitivity and specificity of the AIS and other scales in the Lebanese population, future studies should be conducted taking the physician’s diagnosis into account. However, one of the strength points of this paper is that the data were weighted to account for the multilevel sampling design in terms of total population per governorate and subcategories by age and gender.
5. CONCLUSION
Human life is occupied by an important amount of sleep: one-third. Yet, lacks exist when studying different aspects of neuroscience about sleep. In conclusion, despite some limitations, our present study remains innovative by being the first to assess the prevalence and risk factors of insomnia in the Lebanese population. Standardized diagnostic criteria of insomnia and validated scales allowed assessing for potential risk factors. Our findings stressed on some modifiable risk factors such as high caffeine intake and heavy eating before sleep, where others are treatable underdiagnosed ones like depression and anxiety. An adequate psychological support and an improved knowledge concerning the risk factors of insomnia could guide an effective sleep health assessment, treatment, and the development of public health prevention and intervention programs of sleep–hygiene and stress management measures; this will promote a better sleep quality.
ACKNOWLEDGMENT
The authors would like to thank all the participants who enrolled in the study.
Footnotes
Data availability statement: The data that support the findings of this study are available from the corresponding author [SH], upon reasonable request.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
SH, RH, and PS were involved in the study conceptualization. GAK and SH wrote the manuscript; GAK, DM, and NK were responsible for the data collection and entry. SH and PS analyzed and interpreted the data and SH and RH supervised the project. HS edited the manuscript for English language. All authors reviewed the final draft and approved it.
ETHICAL APPROVAL
The Psychiatric Hospital of the Cross Ethics Committee approved the study protocol (HPC-021-2017). All participants provided a signed informed consent.
SUPPLEMENTARY MATERIAL
Supplementary data related to this article can be found at
.
REFERENCES
- [1].National Center on Sleep Disorders Research (National Heart, Lung, and Blood Institute), Trans-NIH Sleep Research Coordinating Committee . 2003 National sleep disorders research plan. Bethesda, MD, USA: US Dept. of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 2003. [Google Scholar]
- [2].LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32:1027–37. doi: 10.1093/sleep/32.8.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Leger D, Poursain B. An international survey of insomnia: under-recognition and under-treatment of a polysymptomatic condition. Curr Med Res Opin. 2005;21:1785–92. doi: 10.1185/030079905X65637. [DOI] [PubMed] [Google Scholar]
- [4].Choueiry N, Salamoun T, Jabbour H, El Osta N, Hajj A, Rabbaa Khabbaz L. Insomnia and relationship with anxiety in university students: a cross-sectional designed study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0149643. e0149643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36:1059–68. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;37:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- [7].Dollander M. [Etiology of adult insomnia] Encephale. 2002;28:493–502. (In French). https://www.ncbi.nlm.nih.gov/pubmed/12506261. [PubMed] [Google Scholar]
- [8].Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Riemann D. Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety. 2003;17:162–72. doi: 10.1002/da.10101. [DOI] [PubMed] [Google Scholar]
- [9].Kim WJ, Joo WT, Baek J, Sohn SY, Namkoong K, Youm Y, et al. Factors associated with insomnia among the elderly in a Korean rural community. Psychiatry Investig. 2017;14:400–6. doi: 10.4306/pi.2017.14.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Benbir G, Demir AU, Aksu M, Ardic S, Firat H, Itil O, et al. Prevalence of insomnia and its clinical correlates in a general population in Turkey. Psychiatry Clin Neurosci. 2015;69:543–52. doi: 10.1111/pcn.12252. [DOI] [PubMed] [Google Scholar]
- [11].Jaussent I, Dauvilliers Y, Ancelin ML, Dartigues JF, Tavernier B, Touchon J, et al. Insomnia symptoms in older adults: associated factors and gender differences. Am J Geriatr Psychiatry. 2011;19:88–97. doi: 10.1097/JGP.0b013e3181e049b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Han KS, Kim L, Shim I. Stress and sleep disorder. Exp Neurobiol. 2012;21:141–50. doi: 10.5607/en.2012.21.4.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Barbour B, Saadeh N, Salameh PR. Psychological distress in Lebanese young adults: constructing the screening tool ‘BDS-22’. Int J Cult Ment Health. 2012;5:94–108. doi: 10.1080/17542863.2011.563043. [DOI] [Google Scholar]
- [15].Obeid S, Abi Elias Hallit C, Haddad C, Hany Z, Hallit S. Validation of the Hamilton Depression Rating Scale (HDRS) and sociodemographic factors associated with Lebanese depressed patients. L’Encéphale. 2018;44:397–402. doi: 10.1016/j.encep.2017.10.010. [DOI] [PubMed] [Google Scholar]
- [16].Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. https://www.ncbi.nlm.nih.gov/pubmed/14399272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sawaya H, Atoui M, Hamadeh A, Zeinoun P, Nahas Z. Adaptation and initial validation of the Patient Health Questionnaire – 9 (PHQ-9) and the Generalized Anxiety Disorder – 7 questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res. 2016;239:245–52. doi: 10.1016/j.psychres.2016.03.030. [DOI] [PubMed] [Google Scholar]
- [18].Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- [19].Hallit S, Haddad C, Hallit R, Al Karaki G, Malaeb D, Sacre H, et al. Validation of selected sleeping disorders related scales in Arabic among the Lebanese population. Sleep Biol Rhythms. 2019;17:183–9. doi: 10.1007/s41105-018-0196-0. [DOI] [Google Scholar]
- [20].Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48:555–60. doi: 10.1016/s0022-3999(00)00095-7. [DOI] [PubMed] [Google Scholar]
- [21].Central Administration of Statistics Ministry of Social Affairs: Population. Available from: http://www.cas.gov.lb/index.php/demographic-and-social-en/population-en.
- [22].Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923–36. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- [24].Nowicki Z, Grabowski K, Cubała WJ, Nowicka-Sauer K, Zdrojewski T, Rutkowski M, et al. Prevalence of self-reported insomnia in general population of Poland. Psychiatr Pol. 2016;50:165–73. doi: 10.12740/PP/58771. (In English, Polish). [DOI] [PubMed] [Google Scholar]
- [25].Chen LJ, Steptoe A, Chen YH, Ku PW, Lin CH. Physical activity, smoking, and the incidence of clinically diagnosed insomnia. Sleep Med. 2017;30:189–94. doi: 10.1016/j.sleep.2016.06.040. [DOI] [PubMed] [Google Scholar]
- [26].Da Rocha PC, Barroso MT, Dantas AA, Melo LP, Campos TF. Predictive factors of subjective sleep quality and insomnia complaint in patients with stroke: implications for clinical practice. An Acad Bras Cienc. 2013;85:1197–206. doi: 10.1590/S0001-37652013005000053. https://www.ncbi.nlm.nih.gov/pubmed/24068099. [DOI] [PubMed] [Google Scholar]
- [27].Cherri Z, Arcos González P, Castro Delgado R. The Lebanese–Syrian crisis: impact of influx of Syrian refugees to an already weak state. Risk Manag Healthc Policy. 2016;9:165–72. doi: 10.2147/RMHP.S106068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Monk TH, Germain A, Reynolds CF. Sleep disturbance in bereavement. Psychiatr Ann. 2008;38:671–5. doi: 10.3928/00485713-20081001-06. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826218/%23__ffn_sectitle. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- [30].Basta M, Chrousos GP, Vela-Bueno A, Vgontzas AN. Chronic insomnia and the stress system. Sleep Med Clin. 2007;2:279–91. doi: 10.1016/j.jsmc.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Xiang YT, Ma X, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep. 2008;31:1655–62. doi: 10.1093/sleep/31.12.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Nordt SP, Vilke GM, Clark RF, Lee Cantrell F, Chan TC, Galinato M, et al. Energy drink use and adverse effects among emergency department patients. J Community Health. 2012;37:976–81. doi: 10.1007/s10900-012-9549-9. [DOI] [PubMed] [Google Scholar]
- [33].Drake C, Roehrs T, Shambroom J, Roth T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. J Clin Sleep Med. 2013;9:1195–200. doi: 10.5664/jcsm.3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].St-Onge MP, Mikic A, Pietrolungo CE. Effects of diet on sleep quality. Adv Nutr. 2016;7:938–49. doi: 10.3945/an.116.012336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Tanaka E, Yatsuya H, Uemura M, Murata C, Otsuka R, Toyoshima H, et al. Associations of protein, fat, and carbohydrate intakes with insomnia symptoms among middle-aged Japanese workers. J Epidemiol. 2013;23:132–8. doi: 10.2188/jea.je20120101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Coleman RM, Roffwarg HP, Kennedy SJ, Guilleminault C, Cinque J, Cohn MA, et al. Sleep-wake disorders based on a polysomnographic diagnosis. A national cooperative study. JAMA. 1982;247:997–1003. https://www.ncbi.nlm.nih.gov/pubmed/7057593. [PubMed] [Google Scholar]
- [37].Snyder HR, Miyake A, Hankin BL. Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Front Psychol. 2015;6:328. doi: 10.3389/fpsyg.2015.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Shekleton JA, Rogers NL, Rajaratnam SM. Searching for the daytime impairments of primary insomnia. Sleep Med Rev. 2010;14:47–60. doi: 10.1016/j.smrv.2009.06.001. [DOI] [PubMed] [Google Scholar]
- [39].Hasler G, Buysse DJ, Gamma A, Ajdacic V, Eich D, Rössler W, et al. Excessive daytime sleepiness in young adults: a 20-year prospective community study. J Clin Psychiatry. 2005;66:521–9. doi: 10.4088/jcp.v66n0416. [DOI] [PubMed] [Google Scholar]
- [40].Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- [41].Passos GS, Poyares DL, Santana MG, Tufik S, Mello MT. Is exercise an alternative treatment for chronic insomnia? Clinics (Sao Paulo) 2012;67:653–60. doi: 10.6061/clinics/2012(06)17. https://www.ncbi.nlm.nih.gov/pubmed/22760906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10:771–9. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- [43].Morgan K. Daytime activity and risk factors for late-life insomnia. J Sleep Res. 2003;12:231–8. doi: 10.1046/j.1365-2869.2003.00355.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.