Abstract
This review aims to locate existing studies on health-seeking behavior of people in Indonesia, identify gaps, and highlight important findings. Articles were retrieved from Medline, Scopus, Web of Science, Academic Search Complete (via Ebsco), and ProQuest with a number of key words and various combinations. Articles from Indonesian journals were also searched for with Google Scholar. A total of 56 articles from peer-reviewed journal databases and 19 articles from Indonesian journals were reviewed. Quantitative designs were applied more frequently than qualitative, and mixed methods designs were used in some studies. The majority gathered retrospective information about people’s behaviors. Communicable diseases and maternity care were the most frequently studied conditions, in contrast to noncommunicable diseases. In terms of geographical distribution, most research was conducted on Java island, with very few in outside Java. Important findings are a model of Indonesian care-seeking pathways, an understanding of determinants of people’s care choices, and the role of sociocultural beliefs. The findings from this narrative review provide insight to what and how Indonesians make decisions to manage their illness and why. This makes an important contribution to understanding the problem of underutilization of medical services despite the government’s extensive efforts to improve accessibility.
Keywords: Concept of health and illness, health-seeking behavior, Indonesia, pathway of seeking care, social determinants of health, traditional medicines, utilization of health care
1. INTRODUCTION
Indonesia is the fourth most populous country in the world with more than 261 million people [1]. The population is spread unevenly, with more than half living on Java, which is only about 6.5% of the total land area [2,3]. Health care in Indonesia is delivered by a mixed system in which government-financed and privately financed health centers coexist. Government health centers consist of community health centers (Puskesmas) at subdistrict level and state hospitals at district and province level [4]. Privately owned health-care services range widely from not-for-profit religious charitable-group-owned health facilities to for-profit non-state health-care facilities including ambulatory clinics and hospital chains [5].
To improve access to medical care, in January 2014 the Indonesian government introduced the Indonesian Universal Health Coverage program, known as the National Social Health Insurance Scheme (Jaminan Kesehatan Nasional, JKN) [6]. The insurance scheme covers most health interventions for people registered under the scheme [6].
Increasing access to health-care services is a key component of improving a nation’s health status. However, at the individual and community level, understanding people’ health-related behaviors is a crucial element in improving community health [7]. Greater understanding of people’s health-related behaviors might shed light on the problems that still exist in the community despite greatly increased access to health services. For example, although the number of deaths from noncommunicable diseases in Indonesia dropped significantly in the last two decades, such diseases including tuberculosis and malaria remain significant health problems [8]. Gaining understanding of people’s health-related behavior is also an important step to establish effective interventions [7,9].
In the Indonesian context, people’s health-related behavior is made more complex due to it being a multicultural, ethnically diverse country with a variety of health providers. As in other low- and middle-income countries, despite wide availability of formal health providers, informal health providers or nonconventional health providers comprise a significant component of health services [10]. In the Indonesian context, these nonformal health providers – known as traditional health providers – are categorized into biologically based therapies (traditional therapies using substances from nature); physical therapies with tools (e.g., acupuncture, acupressure, and cupping therapy); physical therapies without tools (e.g., massage); and mind body therapies (e.g., hypnotherapy and meditation) [11].
With wide availability of these traditional providers, the use of complementary and alternative medicines is also prevalent. This complicates attempts to understand factors driving health-seeking behavior. Health-seeking behavior is defined as “steps taken by an individual who perceives a need for help as he or she attempts to solve a health problem” [12]. It has been the focus of numerous studies in developing countries [13–20]. Other terms with similar meaning include treatment-, care-, and help-seeking behavior [21–23].
This review aims to document existing literature on health-seeking behavior in Indonesia, identify areas and medical conditions that are understudied, and highlight the major findings related to people’s behavior in seeking care.
2. MATERIALS AND METHODS
2.1. Narrative Review
We undertook a narrative review as we aimed to get a deeper understanding of the health-seeking behavior of people in Indonesia. Greenhalgh et al. [24] recommend conducting a narrative review as opposed to a systematic review when the purpose of the review is to get a deeper understanding on the topic. Health-seeking behavior is a broad topic that covers a wide range of health issues. With narrative review, we were able to interpret the patterns of health-seeking behavior among various topics with a wide range of literature available and include literature that may have been excluded with a systematic search. We also aimed to gather as much information as possible from the Indonesian context, so we searched diverse literature sources, including articles in the Indonesian language.
2.2. Data Sources
As health-seeking behavior straddles medical and social sciences, multiple databases were searched in July–August 2017. The databases included: Medline, Scopus, Web of Science, Academic Search Complete (via Ebsco). Anthropological and social sciences databases (via ProQuest) were also used to locate relevant articles. A number of key words and Boolean combinations were applied. The searches used were: “health seeking” OR “help seeking” OR “care seeking” OR “health seeking behavio*r*” OR “treatment seeking behavio*r*” OR “treatment seeking” OR “health behavio*r*” OR “health related behavio*r*” OR “seek medicine*” OR “seek care” OR “delay* treatment” OR “delay* care” OR “self medicat*” OR “self care” OR “self treatment” AND “Indonesia*”. Articles found were assessed for relevance.
We assessed relevance to the topic of health-seeking behavior studies in the Indonesian communities. We found very limited articles when we searched with specific keywords “health-seeking behavior” or “care-seeking behavior”. Therefore, we expanded search to also include a much broader topic “health behavior” as a keyword. With this keyword, we gathered a larger number of papers, but not all were relevant to health-seeking behaviors. We rejected the articles in the scope of health behavior but not relevant to health-seeking behavior.
Further papers identified in reference lists of relevant articles were retrieved. Searches were also carried out of Indonesian journals, using Google Scholar with the same key words translated into Indonesian.
3. RESULTS
3.1. Description of Relevant Literature
Fifty-six peer-reviewed articles were found from 1987 to 2017 [21–23,25–77], and 19 articles from Indonesian journals from 2001 to 2016 [78–96]. Looking at the publication dates, health-seeking behavior in Indonesia drew little attention before 2000, with only six articles before that time.
3.1.1. Methodologies
Quantitative cross-sectional designs (39) were more frequent than qualitative designs (26), with the same pattern for Indonesian journals. Quantitative studies usually used an interviewer-administered questionnaire, possibly to reduce misunderstandings with self-administered questionnaires due to literacy and language issues.
Quantitative studies provide evidence of factors determining people’s behavior, but are limited in their ability to explore the wider narrative of reasons for choosing specific care, which can be explored in qualitative studies. There were also 10 studies that applied mixed methods design [29,43,44,58,61,70,71,92,93,95]. For example, Brooks et al. [29] explored secondary data from the Indonesian Demographic and Health Survey to quantify the effect of the insurance program on maternity services, and explored barriers of the services utilization qualitatively [29].
Most studies were community based. Of those conducted in health-care facilities, Indonesian journals were more likely to carry studies based in traditional medicine clinics. Clinic-based studies exclude people who never seek care [97]. However, recruiting participants with a specific condition from the community means a large number of people need to be screened to find respondents. Some researchers, however, have conducted household surveys to study health-seeking behavior related to acute respiratory illness, tuberculosis, and malaria [21,22,33,62]. Some studies used secondary data from national surveys, revealing patterns of health-care utilization, and sociodemographic determinants [29,52,65,84,89,94,96].
One study asked about a hypothetical scenario [36], but hypothetical behavior can differ from actual behavior. Most other studies gathered retrospective information from people who have a certain illness and asked them to recall what they have done to manage it [98]. This can lead to recall bias. To minimize this, some researchers set up inclusion criteria, for example, newly diagnosed or having symptoms during the last month. In contrast, Utarini et al. [61] used a longitudinal prospective design to explore people’s behavior in seeking care for malaria over 1 year. They detected malaria cases in six endemic malaria villages and what people did during that period. Thus, prospective studies collect more accurate data on health-seeking behavior from the beginning of symptom experiences to the final stage of recovery.
3.1.2. Medical conditions covered
Many studies focused on infectious diseases such as malaria, tuberculosis, and leprosy. Maternity-related health was also common. Tuberculosis, malaria, and mothers’ and infants’ health are important focus areas of the Sustainable Development Goals [99].
Tuberculosis, malaria, and infant health remain significant health problems in Indonesia. Approximately 10% of global tuberculosis patients live in Indonesia with an incidence rate of 399 per 100,000 population in 2016 [100]. Some areas in Indonesia are also endemic to malaria with about 261,617 cases reported in 2018 [101]. In 2015, the maternal mortality and infant mortality rate were recorded as 305 per 100,000 life birth and 22 per 1000 life birth, respectively [4].
Noncommunicable diseases studied included mental illnesses and cancer, but there were fewer studies on stroke, hypertension, and diabetes. The prevalence of noncommunicable diseases in Indonesia is rising and they became major causes of death in 2012 [4,8]. With a prevalence of 47.8%, hypertension has become a leading cause of mortality [102]. The other alarming noncommunicable disease in Indonesia is diabetes. The current diabetes prevalence was 7% with more than a half of them undiagnosed [103,104]. Thus, more studies of health-seeking behavior should focus on chronic diseases.
Other diverse studies included health-seeking behavior of infertility patients and transgender people related to HIV risk [41,47].
3.1.3. Study location
Indonesia is situated between the continents of Asia and Australia, and between the Pacific and Indian Oceans. It is an archipelago of more than 13,000 islands (total land area 1,913,578.68 square kilometers) [2], administratively divided into 34 provinces [2]. It is culturally diverse with more than 1300 ethnic groups and six official religions. Although Islam is the predominant religion, in Bali, Papua, and East Nusa Tenggara, the dominant religions are Hinduism, Protestantism and Catholicism, respectively [105].
Most reviewed studies were on Java, the most populated island of Indonesia, which also includes the capital Jakarta (Figure 1). Java is the most developed region in the country. Within Java, more studies were located in Yogyakarta and Jakarta.
Figure 1.
Coverage of geographical areas in the studies reviewed.
Beyond Java, some studies were performed in Aceh and Bali Provinces. Aceh is located on the far north of Sumatera, whereas Bali is an island to the east of Java. Socioculturally, these provinces are different, most people in Aceh are Muslim and in Bali, Hindu.
More studies need to be conducted outside Java, particularly in the East. This area lags behind western Indonesia in terms of economic activities, infrastructure, and population, including health indicators [4].
3.2. Important Findings
3.2.1. Lay concepts of health and illness
Concepts of health and illness are influenced by people’s sociocultural background [106]. Indonesian people consider themselves healthy if they can perform their everyday activities without disruption. Thus, people generally sought help when symptoms hindered these [21,22,25,28,37,39,42,45,51,56,66,67,71,77]. For example, Eeuwijk [71] described that most older people sought care from health professionals for rheumatism because it hindered their activities. In contrast, they did not seek professional help for problems with eyes, ears, or teeth because there was less impact on their daily lives. Thus, people delayed seeking care until their diseases were severe.
There is also a strong concept of “balance and harmony”, particularly among Javanese. Health is a physical status that cannot be achieved without individuals’ spiritual wellbeing. Life in general should be balanced physically and spiritually, between individual and social life, so that a status of “harmony” can be reached [42,57]. The Indonesian government recognizes six official religions: Islam, Catholicism, Protestantism, Hinduism, Buddhism, and Confucianism [105]. Regardless of specific religion, people tend to believe that health is God’s gift and illness is their fate, sometimes viewed as God’s punishment [28,42,46].
3.2.2. Determinants of health provider choices
Indonesian people’s choice of health providers is determined by complex and interrelated factors: sociodemographic characteristics, influence of significant others, sociocultural beliefs, perception about diseases and their causality, and perception of medical services including accessibility and availability, particularly in rural and areas, and its related cost [23,28–30,34,35,38,40–42,45–48,52,54–57,59,60,64,65,67,72].
3.2.2.1. Sociodemographic characteristics
Age, household size, education, and economic status determine people’s choices of health providers [65,74,94]. Poorer households were more likely to use traditional medicines for treating malaria [25], older people and those in rural areas were more likely to seek traditional and alternative treatment [84,89,96]. Women were also more likely to seek health care for tuberculosis-related symptoms [21]. However, other studies did not find a link between seeking care and sociodemographic characteristics [21,53,75,78,81], suggesting other factors may have greater impact in influencing people’s choices in health providers.
3.2.2.2. Influence of significant others
In most Indonesian communities, seeking care involves not only patients but also family, friends, and other community members [21,28,30,31,34,35,38,45,55,59,64,67,72]. Recommendations from significant others were associated with visiting alternative health-care providers for treating tuberculosis [21] and cancer [28,45]. Religious leaders influenced tuberculosis patients’ choices [30]. The husband and older family members made decisions related to birth attendant choices [34].
3.2.2.3. Sociocultural beliefs
Most women chose to give birth at home, helped by a traditional birth attendant, despite the proximity of health facilities or health professionals, mainly because the birth attendant also performed prayers and other traditional practices and ceremony. People believed that birth is sacred and should be consistent with traditional beliefs [29,34,55].
Cultural beliefs also favored traditional remedies or alternative treatments. These practices have been passed down for generations, and this embedded culture cannot be ignored. They are commonly used for treating most diseases, including malaria [25,44,61,69], tuberculosis [21,39,51,59,67,72], leprosy [46], rheumatoid arthritis [76], cancer [28,38,45], hypertension [93], stroke [56], and diabetes [95]. Traditional remedies are also used for promoting health and preventing disease. For example, women took traditional herbal drinks to stay healthy during pregnancy and breastfeeding [26,49], and some people took bitter-tasting plants to prevent malaria [44,62,69,85,90].
People perceived that biomedicine was failing to cure illness; fear of side effects, dependence on medication, and medical procedures were other common reasons cited for using traditional or alternative treatments [28,32,38,92,93,95]. People viewed full cure as successful treatment. Biomedicine was not believed to cure diabetes and hypertension, leading to the choice of traditional treatment [93,95].
Indonesians regard traditional remedies as safe because they are made from natural resources [87,92]. People also perceived that traditional healers provided comprehensive services as they were also dealing with patients’ feelings [45], and in some cases, payment can be made in kind, for example with food [72].
Many forms of traditional remedies and alternative treatments are available in Indonesia. Jamu, a traditional herbal drink is the most popular [107]. Other popular alternative treatments include traditional Chinese medicines, known as sinshe [87], treatment with animal media such as leeches [79], traditional bone setters [82], cupping therapy [86], and coin scratching [83].
3.2.2.4. Perception of causality
Health-seeking behavior was also influenced by perceptions related to diseases and causality. For example, there were strong beliefs that mental illnesses have supernatural causes, so people first sought care from traditional, spiritual, or religious healers [23,35,64]. In some areas, tuberculosis and leprosy were also believed to be caused by black magic or bad spirits and so people sought help from traditional healers [46,67,72].
Communities commonly have their own local term, description, and interpretation of illnesses or symptoms. For example, tuberculosis was believed to be caused by smoking, stress, sleeping on the floor, or other physical causes [59,67,72]. Thus, early symptoms of tuberculosis were not perceived as serious. People in central Java did not recognize malaria, but the local term katisen has similar symptoms to malaria. Again, katisen is seen as a minor illness, leading to self-medication [69]. Javanese often misidentified heart diseases with masuk angin (wind sickness), using the term angin duduk (sitting wind sickness) for heart disease. Masuk angin is a mild illness caused by over exposure to wind, and people treated it with coin scratching, so heart disease is treated in the same way [57].
3.2.2.5. Perception about health-care systems
Perceptions about medical services also influence health-seeking behavior. Many people were reluctant to go to public health facilities as they experienced complex administrative procedures, one-sided communication style of health professionals, and long waiting times [28,29,35,40,41,67]. Thus, many people choose to go to private health providers [22,33,36,51,59,65,67]. Further reasons driving the choice of private providers include perceived quality of provider, availability of brand name medicines, and short waiting times [36,59,66,67].
3.2.2.6. Health cost and people’s perception of health insurance
Expanding health insurance alone was not enough to increase health-care utilization for people residing in rural areas [52]. Indirect costs of treatment, such as transportation, are barriers to medical treatment [28,34,35,45,54]. In many cases requiring hospitalization, family members accompanied the patient during their stay. Extended families were often a source of finance for extra cost [28,34,35,45]. Therefore, the healthcare cost burdened not only the patients, but also their extended families.
People experienced the insurance scheme as complicated and time consuming, poorly socialized and understood [28,29,55,58]. Therefore, people only applied once they perceived the need for help. People also perceived that health providers offered a low quality of service for the poor under the scheme [28,29,55,58]. This might be true, as from the providers’ perspective there has been incomplete reimbursement and low payment [58].
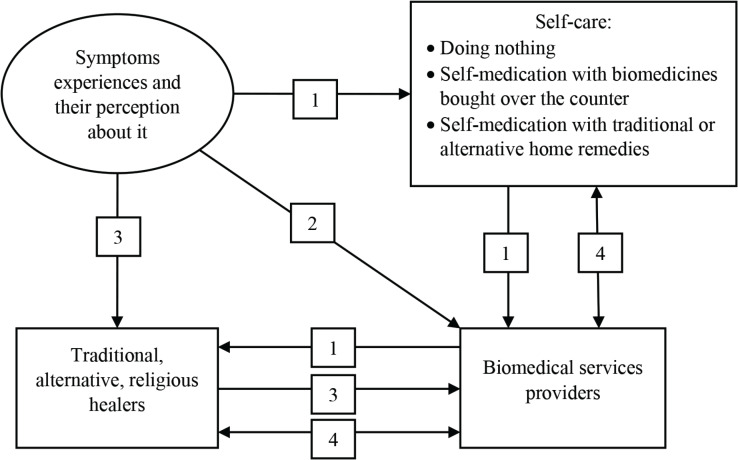
3.2.3. Care pathways
After experiencing symptoms, people generally used self-care: taking rest, self-medicating with medicines bought from drug stores or pharmacies, or taking traditional medicines. If they perceived that the symptoms persisted, they would seek help from formal health care. If that failed, they then would try other traditional or alternative treatments (Figure 2) [28,30,38,43,45,59,62,69,72,73,88,96]. Most then went to either formal or informal health providers, often combining or alternating medicines from different providers [51,67,77,78]. However, if the sick person is a child, going direct to formal health care is common [40,68,73,88,91,96]. A strong belief exists that the effectiveness of treatment is a matter of being “suited to you”, so they would try alternatives to find one that suits [43,69].
Figure 2.
The pathway of seeking care. (1) General process of seeking care. (2) If the sick person is a child. (3) If the disease is strongly attributed to supernatural diseases such as mental illness, or if they perceive that their disease is caused by any supernatural power. (4) Both providers, medical services providers and alternative providers, or type of medications, traditional and biomedicines, are used as an alternate or in combination to find “fit” treatment to them.
Another pathway, as mentioned before, was when people first went to any alternative treatments for illness attributed to supernatural causes, switching to formal health care when they perceived alternative treatments as ineffective [23,35,46,63,64,67,72].
3.2.3.1. Self-medication
Self-medication with biomedicines was a common practice [96]. As with many developing countries, most prescription medicines are available over the counter. People self-medicated with antibiotics for treating a common cold, headache, and other minor symptoms [27,40,50]. People also self-medicated for malaria and tuberculosis [30,39,51,59,61,62,67,69,73,80], and musculoskeletal pain [76]. Many self-medication practices are inappropriate [73].
4. DISCUSSION
This is the first review to look into health-seeking behavior in Indonesia. This review shows that there are significant gaps in the literature about health-seeking behaviors in the Indonesian context. Many studies on health-related behavior focused on a restricted range of health problems. Research on health behavior on child immunization has not been updated for a long time, and very limited studies explored the behavior of people with chronic illnesses such as hypertension and diabetes. Research on the health-seeking behavior of people in Indonesia needs to be conducted in these understudied areas. Understanding people’s behavior related to immunization is particularly important as Indonesia has lower immunization coverage compared with most other countries in the Southeast Asia region [99]. Research suggested that understanding people’s perspectives and behavior related to child immunization is the key to success for immunization programs [108].
Health-seeking behavior studies also need to cover chronic diseases. The prevalence of chronic diseases such as hypertension and diabetes in Indonesia has increased during the past decade [102,103]. Studies in other countries found that people’s behavior in managing chronic illness, for example diabetes, were very complex and influenced by cultural beliefs and values [109–112]. Understanding people’s cultural beliefs and values were key elements for a successful diabetes intervention program [113]. We found that, in terms of geographical areas, most of the studies were conducted within Java island. Some studies outside Java were focused only in particular areas including Aceh and Bali Province. Limited studies were observed from the eastern part of Indonesia. With the wide cultural diversity in Indonesia, research on health-seeking behavior needs to also be expanded to cover understudied areas.
This review also suggests that people’s behavior in seeking care was determined by a range of internal and external factors. The internal factors include individual characteristics and perceptions and beliefs about the disease and its treatments. The external factors may include influence of significant others and perceptions about the health-care and health insurance systems. These findings are similar to studies in other low- and middle-income country contexts [13–16,19,20] and align most with the Kroeger’s model of determinant of choices of health-care services [97]. The Kroeger model incorporates three major factors influencing people’s choices within the wide range of health providers: characteristics of person, characteristics of disorders and their perceptions, and characteristics of the health services system [97].
Health interventions should be developed based on this knowledge on factors determining behavior. This review found that traditional treatments were chosen when people perceived supernatural causes of the disease and when they perceived the biomedical system have failed to cure their chronic diseases, similar to research in Zambia and Kenya [15,20]. The choice of care was also influenced by people’s perception related to the disease and its causality. Therefore, interventions should be made to address misconceptions related to diseases and perceived causality, which hinder people from seeking care. One study attempted to do this through implementing tuberculosis leadership groups within the community, who held meetings to discuss peoples’ perceptions about tuberculosis and to address any misunderstanding found, leading to greater engagement with formal health care [39]. This effort should be expanded to other communities and diseases.
On the other hand, traditional medicine systems are important in developing countries. People value their efficacy, and they are widely accepted. Thus, integrating these into formal health care may be more effective than discouraging them. For example, mothers’ preference for a traditional birth attendant has resulted in collaboration between village midwives and birth attendants in some areas of Indonesia [34]. The Indonesian government has also initiated efforts to ensure the safety and effectiveness of traditional herbal medicines [107]. However, in many cases, the safety and efficacy of techniques used in traditional medication systems are questionable and not scientifically proven. Therefore, their existence should not replace formal health care.
The characteristics of the medical care provider, including availability and cost, also influenced people’s behaviors in seeking care [17,18]. This review shows that the cost mentioned as a barrier to seeking care included transport and other costs related to hospitalizations. The insurance program or the government also need to consider this nonmedical cost as a financial burden to the patients.
Negative past experiences with the public health-care system has made people reluctant to engage. Therefore, improving availability and accessibility may have to be balanced with improving quality of care. Another health system issue is the availability of prescription medicines over the counter, driving increased self-medication.
The other important finding in this review is the pathway of seeking care. Before people in Indonesia seek biomedical help, most of them would self-medicate, including with antibiotics. The government should develop serious efforts to prevent the misuse of antibiotics as the problem of antibiotic resistance in Indonesia and worldwide is alarming. A study in a hospital in Indonesia showed that most bacteria were resistant to the third generation of cephalosporins and quinolone [114]. Worldwide, more than 70% of bacteria were also resistant to most antibiotics available in the market [115].
In summary, studies on health-seeking behavior is important to understand factors determining people’s behavior. This understanding would allow more evidence-based health-care intervention and policy.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
AWW contributed in acquisition and analysis the data and prepared the initial draft of the manuscript. JAG, SH and PN critically reviewed and revised the initial draft.
REFERENCES
- [1].The World Bank World development indicators. 2016 Available from: http://data.worldbank.org/data-catalog/Population-ranking-table (accessed April 17, 2017).
- [2].Indonesia Ministry of Home Affairs The book of administrative code and regions of Indonesia. 2015 Available from: http://www.kemendagri.go.id/media/documents/2015/02/25/l/a/lampiran_i.pdf (accessed June 5, 2016).
- [3].Statistics Indonesia Population distribution by province. Available from: https://www.bps.go.id/linkTableDinamis/view/id/843 (accessed April 19, 2017).
- [4].Indonesia Ministry of Health . Indonesia health profile 2015. Jakarta: Indonesia Ministry of Health; 2016. pp. 25–41. [Google Scholar]
- [5].Hort K, Akhtar AO, Trisnantoro L, Dewi S, Meliala A. The growth of non-state hospitals in Indonesia: implications for policy and regulatory options. Health Policy Health Finance Knowledge Hub. 2011;12:1–17. [Google Scholar]
- [6].Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Taher A, Achadi EL, et al. Universal health coverage in Indonesia: concept, progress, and challenges. Lancet. 2019;393:75–102. doi: 10.1016/S0140-6736(18)31647-7. [DOI] [PubMed] [Google Scholar]
- [7].Glanz K. Health behavior. In: Boslaugh S, editor. Encyclopedia of Epidemiology. Thousand Oaks: SAGE Publications, Inc; 2008. pp. 459–63. [Google Scholar]
- [8].World Health Organization . World Health Organization; 2015. Indonesia: WHO statistical profile. Available from: http://www.who.int/gho/countries/idn.pdf?ua=1 (accessed April 4, 2017). [Google Scholar]
- [9].Glanz K, Rimer BK, Viswanath K. Health behavior and health education theory, research, and practice. 4th ed. Hoboken: Wiley; 2008. [Google Scholar]
- [10].Sudhinaraset M, Ingram M, Lofthouse HK, Montagu D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS One. 2013;8:e54978. doi: 10.1371/journal.pone.0054978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Department of Health Research and Development Indonesia Ministry of Health . Basic Health Research. Jakarta: 2013. pp. 79–80. [Google Scholar]
- [12].Chrisman NJ. The health seeking process: an approach to the natural history of illness. Cult Med Psychiatry. 1977;1:351–77. doi: 10.1007/bf00116243. [DOI] [PubMed] [Google Scholar]
- [13].Sarfo IA, Acquaye VA, Sarfo JO. Existing health seeking behavior in the eastern region of Ghana: the role of traditional and orthodox health systems. Eur J Med. 2016;13:73–80. doi: 10.13187/ejm.2016.13.73. [DOI] [Google Scholar]
- [14].O’Neill S, Gryseels C, Dierickx S, Mwesigwa J, Okebe J, d’Alessandro U, et al. Foul wind, spirits and witchcraft: illness conceptions and health-seeking behavior for malaria in the Gambia. Malar J. 2015;14:167. doi: 10.1186/s12936-015-0687-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Stekelenburg J, Jager BE, Kolk PR, Westen EHMN, van der Kwaak A, Wolffers IN. Health care seeking behavior and utilisation of traditional healers in Kalabo, Zambia. Health Policy. 2005;71:67–81. doi: 10.1016/j.healthpol.2004.05.008. [DOI] [PubMed] [Google Scholar]
- [16].Anwar M, Green J, Norris P. Health-seeking behavior in Pakistan: a narrative review of the existing literature. Public Health. 2012;126:507–17. doi: 10.1016/j.puhe.2012.02.006. [DOI] [PubMed] [Google Scholar]
- [17].Xu JW, Xu QZ, Liu H, Zeng YR. Malaria treatment-seeking behavior and related factors of Wa ethnic minority in Myanmar: a cross-sectional study. Malar J. 2012;11:417. doi: 10.1186/1475-2875-11-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Anselmi L, Lagarde M, Hanson K. Health service availability and health seeking behavior in resource poor settings: evidence from Mozambique. Health Econ Rev. 2015;5:26. doi: 10.1186/s13561-015-0062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Norris P, Fa’alau F, Va’ai C, Churchward M, Arroll B. Navigating between illness paradigms: treatment seeking by Samoan people in Samoa and New Zealand. Qual Health Res. 2009;19:1466–75. doi: 10.1177/1049732309348364. [DOI] [PubMed] [Google Scholar]
- [20].Abubakar A, Van Baar A, Fischer R, Bomu G, Gona JK, Newton CR. Socio-cultural determinants of health-seeking behavior on the Kenyan coast: a qualitative study. PLoS One. 2013;8:e71998. doi: 10.1371/journal.pone.0071998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ahmad RA, Richardus JH, de Vlas SJ. Care-seeking behavior among individuals with TB symptoms in Jogjakarta province, Indonesia: a community-based study. Int Health. 2013;5:51–7. doi: 10.1093/inthealth/ihs002. [DOI] [PubMed] [Google Scholar]
- [22].Karyana M, Devine A, Kenangalem E, Burdarm L, Poespoprodjo JR, Vemuri R, et al. Treatment-seeking behavior and associated costs for malaria in Papua, Indonesia. Malar J. 2016;15:536. doi: 10.1186/s12936-016-1588-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Marchira CR, Supriyanto I, Subandi, Soewadi, Good BJ. The association between duration of untreated psychosis in first psychotic episode patients and help seeking behaviors in Jogjakarta, Indonesia. Int J Cult Ment Health. 2016;9:120–6. doi: 10.1080/17542863.2015.1103276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Greenhalgh T, Thorne S, Malterud K. Time to challenge the spurious hierarchy of systematic over narrative reviews? Eur J Clin Invest. 2018;48:e12931. doi: 10.1111/eci.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Suswardany DL, Sibbritt DW, Supardi S, Pardosi JF, Chang S, Adams J. A cross-sectional analysis of traditional medicine use for malaria alongside free antimalarial drugs treatment amongst adults in high-risk malaria endemic provinces of Indonesia. PLoS One. 2017;12:e0173522. doi: 10.1371/journal.pone.0173522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Probandari A, Arcita A, Kothijah K, Pamungkasari EP. Barriers to utilization of postnatal care at village level in Klaten district, central Java Province, Indonesia. BMC Health Serv Res. 2017;17:541. doi: 10.1186/s12913-017-2490-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kurniawan K, Posangi J, Rampengan N. Association between public knowledge regarding antibiotics and self-medication with antibiotics in Teling Atas Community Health Center, East Indonesia. Med J Indones. 2017;26:62–9. doi: 10.13181/mji.v26i1.1589. [DOI] [Google Scholar]
- [28].Fles R, Bos ACRK, Supriyati, Rachmawati D, Waliyanti E, Tan IB, et al. The role of Indonesian patients’ health behaviors in delaying the diagnosis of nasopharyngeal carcinoma. BMC Public Health. 2017;17:510. doi: 10.1186/s12889-017-4429-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Brooks MI, Thabrany H, Fox MP, Wirtz VJ, Feeley FG, Sabin LL. Health facility and skilled birth deliveries among poor women with Jamkesmas health insurance in Indonesia: a mixed-methods study. BMC Health Serv Res. 2017;17:105. doi: 10.1186/s12913-017-2028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ariyanto Y, Wati DM. Understanding social context on TB cases. J Phys Conf Ser. 2017;801 [Google Scholar]
- [31].Suhariadi F, Zein RA, Alfian IN, Hadi C. The tale of seeking treatment: a qualitative study of pulmonary tuberculosis patients. Psychol Community Health. 2016;5:229–43. doi: 10.5964/pch.v5i3.152. [DOI] [Google Scholar]
- [32].Rahmawati R, Bajorek B. Perspectives on antihypertensive medication: a qualitative study in a rural Yogyakarta province in Indonesia. Drugs Ther Perspect. 2016;32:76–83. doi: 10.1007/s40267-015-0263-4. [DOI] [Google Scholar]
- [33].Praptiningsih CY, Lafond KE, Wahyuningrum Y, Storms AD, Mangiri A, Iuliano AD, et al. Healthcare-seeking behaviors for acute respiratory illness in two communities of Java, Indonesia: a cross-sectional survey. J Epidemiol Glob Health. 2016;6:77–86. doi: 10.1016/j.jegh.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Nasir S, Ahmed R, Kurniasari M, Limato R, Tulloch O, Syafruddin D, et al. Challenges that hinder parturients to deliver in health facilities: a qualitative analysis in two districts of Indonesia. Makara J Health Res. 2016;20:79–87. doi: 10.7454/msk.v20i3.6072. [DOI] [Google Scholar]
- [35].Marthoenis M, Aichberger MC, Schouler-Ocak M. Patterns and determinants of treatment seeking among previously untreated psychotic patients in Aceh Province, Indonesia: a qualitative study. Scientifica (Cairo) 2016;2016:9136079. doi: 10.1155/2016/9136079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kreslake JM, Wahyuningrum Y, Iuliano AD, Storms AD, Lafond KE, Mangiri A, et al. The intersection of care seeking and clinical capacity for patients with highly pathogenic avian influenza A (H5N1) virus in Indonesia: knowledge and treatment practices of the public and physicians. Disaster Med Public Health Prep. 2016;10:838–47. doi: 10.1017/dmp.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Irwan AM, Kato M, Kitaoka K, Kido T, Taniguchi Y, Shogenji M. Self-care practices and health-seeking behavior among older persons in a developing country: theories-based research. Int J Nurs Sci. 2016;3:11–23. doi: 10.1016/j.ijnss.2016.02.010. [DOI] [Google Scholar]
- [38].Handayani K, Sitaresmi MN, Supriyadi E, Widjajanto PH, Susilawati D, Njuguna F, et al. Delays in diagnosis and treatment of childhood cancer in Indonesia. Pediatr Blood Cancer. 2016;63:2189–96. doi: 10.1002/pbc.26174. [DOI] [PubMed] [Google Scholar]
- [39].Dewi C, Barclay L, Passey M, Wilson S. Improving knowledge and behaviors related to the cause, transmission and prevention of Tuberculosis and early case detection: a descriptive study of community led tuberculosis program in Flores, Indonesia. BMC Public Health. 2016;16:740. doi: 10.1186/s12889-016-3448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Widayati A, Suryawati S, de Crespigny C, Hiller JE. Beliefs about the use of nonprescribed antibiotics among people in Yogyakarta City, Indonesia: a qualitative study based on the theory of planned behavior. Asia Pac J Public Health. 2015;27:NP402–NP13. doi: 10.1177/1010539512445052. [DOI] [PubMed] [Google Scholar]
- [41].Prabawanti C, Dijkstra A, Riono P, Hartana G. A survey on HIV-related health-seeking behaviors among transgender individuals in Jakarta, based on the theory of planned behavior. BMC Public Health. 2015;15:1138. doi: 10.1186/s12889-015-2480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Pitaloka D, Hsieh E. Health as submission and social responsibilities: embodied experiences of Javanese women with type II diabetes. Qual Health Res. 2015;25:1155–65. doi: 10.1177/1049732315577607. [DOI] [PubMed] [Google Scholar]
- [43].Seeberg J, Pannarunothai S, Padmawati RS, Trisnantoro L, Barua N, Pandav CS. Treatment seeking and health financing in selected poor urban neighbourhoods in India, Indonesia and Thailand. Soc Sci Med. 2014;102:49–57. doi: 10.1016/j.socscimed.2013.11.039. [DOI] [PubMed] [Google Scholar]
- [44].Murhandarwati EEH, Fuad A, Nugraheni MDF, Sulistyawati, Wijayanti MA, Widartono BS, et al. Early malaria resurgence in pre-elimination areas in Kokap Subdistrict, Kulon Progo, Indonesia. Malar J. 2014;13:130. doi: 10.1186/1475-2875-13-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Iskandarsyah A, de Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, Passchier J. Psychosocial and cultural reasons for delay in seeking help and nonadherence to treatment in Indonesian women with breast cancer: a qualitative study. Health Psychol. 2014;33:214–21. doi: 10.1037/a0031060. [DOI] [PubMed] [Google Scholar]
- [46].Peters RMH, Dadun, Lusli M, Miranda-Galarza B, van Brakel WH, Zweekhorst MBM, et al. The meaning of leprosy and everyday experiences: an exploration in Cirebon, Indonesia. J Trop Med. 2013;2013:507034. doi: 10.1155/2013/507034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Bennett LR, Wiweko B, Hinting A, Adnyana IBP, Pangestu M. Indonesian infertility patients’ health seeking behavior and patterns of access to biomedical infertility care: an interviewer administered survey conducted in three clinics. Reprod Health. 2012;9:24. doi: 10.1186/1742-4755-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Agus Y, Horiuchi S. Factors influencing the use of antenatal care in rural West Sumatra, Indonesia. BMC Pregnancy Childbirth. 2012;12:9. doi: 10.1186/1471-2393-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Wulandari LPL, Whelan AK. Beliefs, attitudes and behaviors of pregnant women in Bali. Midwifery. 2011;27:867–71. doi: 10.1016/j.midw.2010.09.005. [DOI] [PubMed] [Google Scholar]
- [50].Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta City Indonesia: a cross sectional population-based survey. BMC Res Notes. 2011;4:491. doi: 10.1186/1756-0500-4-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Lock WA, Ahmad RA, Ruiter RAC, van der Werf MJ, Bos AER, Mahendradhata Y, et al. Patient delay determinants for patients with suspected tuberculosis in Yogyakarta province, Indonesia. Trop Med Int Health. 2011;16:1501–10. doi: 10.1111/j.1365-3156.2011.02864.x. [DOI] [PubMed] [Google Scholar]
- [52].Erlyana E, Damrongplasit KK, Melnick G. Expanding health insurance to increase health care utilization: will it have different effects in rural vs. urban areas? Health Policy. 2011;100:273–81. doi: 10.1016/j.healthpol.2010.11.008. [DOI] [PubMed] [Google Scholar]
- [53].Ahmad RA, Mahendradhata Y, Utarini A, de Vlas SJ. Diagnostic delay amongst tuberculosis patients in Jogjakarta Province, Indonesia is related to the quality of services in DOTS facilities. Trop Med Int Health. 2011;16:412–23. doi: 10.1111/j.1365-3156.2010.02713.x. [DOI] [PubMed] [Google Scholar]
- [54].Titaley CR, Hunter CL, Heywood P, Dibley MJ. Why don’t some women attend antenatal and postnatal care services?: a qualitative study of community members’ perspectives in Garut, Sukabumi and Ciamis districts of West Java Province, Indonesia. BMC Pregnancy Childbirth. 2010;10:61. doi: 10.1186/1471-2393-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Titaley CR, Hunter CL, Dibley MJ, Heywood P. Why do some women still prefer traditional birth attendants and home delivery?: a qualitative study on delivery care services in West Java Province, Indonesia. BMC Pregnancy Childbirth. 2010;10:43. doi: 10.1186/1471-2393-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Norris M, Allotey P, Barrett G. “I feel like half my body is clogged up”: lay models of stroke in Central Aceh, Indonesia. Soc Sci Med. 2010;71:1576–83. doi: 10.1016/j.socscimed.2010.08.018. [DOI] [PubMed] [Google Scholar]
- [57].Dewi FST, Weinehall L, Öhman A. ‘Maintaining balance and harmony’: Javanese perceptions of health and cardiovascular disease. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].D’Ambruoso L, Byass P, Qomariyah SN. ‘Maybe it was her fate and maybe she ran out of blood’: final caregivers’ perspective on access to care in obstetric emergencies in rural Indonesia. J Biosoc Sci. 2010;42:213–41. doi: 10.1017/S0021932009990496. [DOI] [PubMed] [Google Scholar]
- [59].Rintiswati N, Mahendradhata Y, Suharna, Susilawati, Purwanta, Subronto Y, et al. Journeys to tuberculosis treatment: a qualitative study of patients, families and communities in Jogjakarta, Indonesia. BMC Public Health. 2009;9:158. doi: 10.1186/1471-2458-9-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Mahendradhata Y, Syahrizal BM, Utarini A. Delayed treatment of tuberculosis patients in rural areas of Yogyakarta province, Indonesia. BMC Public Health. 2008;8:393. doi: 10.1186/1471-2458-8-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Utarini A, Nystrom L, Sanusi R, Chandramohan D, Winkvist A. Interactions between malaria workers and clinical malaria patients in Jepara District, Indonesia. Southeast Asian J Trop Med Public Health. 2007;38:959–70. https://www.ncbi.nlm.nih.gov/pubmed/18613535. [PubMed] [Google Scholar]
- [62].Sanjana P, Barcus MJ, Bangs MJ, Ompusunggu S, Elyazar I, Marwoto H, et al. Survey of community knowledge, attitudes, and practices during a malaria epidemic in central Java, Indonesia. Am J Trop Med Hyg. 2006;75:783–9. https://www.ncbi.nlm.nih.gov/pubmed/17123966. [PubMed] [Google Scholar]
- [63].Kurihara T, Kato M, Reverger R, Rai Tirta IG. Pathway to psychiatric care in Bali. Psychiatry Clin Neurosci. 2006;60:204–10. doi: 10.1111/j.1440-1819.2006.01487.x. [DOI] [PubMed] [Google Scholar]
- [64].Kurihara T, Kato M, Reverger R, Rai Tirta IG. Beliefs about causes of schizophrenia among family members: a community-based survey in Bali. Psychiatr Serv. 2006;57:1795–9. doi: 10.1176/ps.2006.57.12.1795. [DOI] [PubMed] [Google Scholar]
- [65].Thind A. Analysis of health services use for respiratory illness in Indonesian children: implications for policy. J Biosoc Sci. 2005;37:129–42. doi: 10.1017/s002193200300645x. [DOI] [PubMed] [Google Scholar]
- [66].Watkins RE, Rouse CR, Plant AJ. Tuberculosis treatment delivery in Bali: a qualitative study of clinic staff perceptions. Int J Tuberc Lung Dis. 2004;8:218–25. https://www.ncbi.nlm.nih.gov/pubmed/15139451. [PubMed] [Google Scholar]
- [67].Watkins RE, Plant AJ. Pathways to treatment for tuberculosis in Bali: patient perspectives. Qual Health Res. 2004;14:691–703. doi: 10.1177/1049732304263628. [DOI] [PubMed] [Google Scholar]
- [68].Simanjuntak CH, Punjabi NH, Wangsasaputra F, Nurdin D, Pulungsih P, Rofiq A, et al. Diarrhoea episodes and treatment-seeking behavior in a slum area of North Jakarta, Indonesia. J Health Popul Nutr. 2004;22:119–29. https://www.ncbi.nlm.nih.gov/pubmed/15473515. [PubMed] [Google Scholar]
- [69].Utarini A, Winkvist A, Ulfa FM. Rapid assessment procedures of malaria in low endemic countries: community perceptions in Jepara district, Indonesia. Soc Sci Med. 2003;56:701–12. doi: 10.1016/s0277-9536(02)00066-7. [DOI] [PubMed] [Google Scholar]
- [70].Susanti NN, Aziz MF, Bachtiar A. An analysis on the delay of cervical cancer patients in seeking medical check up in Dr. Cipto Mangunkusumo National Central General Hospital Jakarta. Med J Indonesia. 2003;12:162–5. doi: 10.13181/mji.v12i3.105. [DOI] [Google Scholar]
- [71].van Eeuwijk P. Urban elderly with chronic illness: local understandings and emerging discrepancies in North Sulawesi, Indonesia. Anthropol Med. 2003;10:325–41. doi: 10.1080/1364847032000133843. [DOI] [PubMed] [Google Scholar]
- [72].Caprara A, Abdulkadir N, Idawani C, Asmara H, Lever P, De Virgilio G. Cultural meanings of tuberculosis in aceh province, Sumatra. Med Anthropol. 2000;19:65–89. doi: 10.1080/01459740.2000.9966169. [DOI] [PubMed] [Google Scholar]
- [73].Sclafer J, Slamet LS, de Visscher G. Appropriateness of self-medication: method development and testing in urban Indonesia. J Clin Pharm Ther. 1997;22:261–72. doi: 10.1046/j.1365-2710.1997.10075100.x. [DOI] [PubMed] [Google Scholar]
- [74].Kaye K, Novell MK. Health practices and indices of a poor urban population in Indonesia. Part I: patterns of health service utilization. Asia Pac J Public Health. 1994;7:178–82. doi: 10.1177/101053959400700306. [DOI] [PubMed] [Google Scholar]
- [75].Sutrisna B, Reingold A, Kresno S, Harrison G, Utomo B. Care-seeking for fatal illnesses in young children in Indramayu, West Java, Indonesia. Lancet. 1993;342:787–9. doi: 10.1016/0140-6736(93)91545-w. [DOI] [PubMed] [Google Scholar]
- [76].Darmawan J, Valkenburg HA, Muirden KD, Wigley RD. Epidemiology of rheumatic diseases in rural and urban populations of Indonesia: a World Health Organization International League Against Rheumatism COPCORD study, stage 1, phase 2. Ann Rheum Dis. 1992;51:525–8. doi: 10.1136/ard.51.4.525. https://www.ncbi.nlm.nih.gov/pubmed/8103880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Berman P, Ormond BA, Gani A. Treatment use and expenditure on curative care in rural Indonesia. Health Policy Plan. 1987;2:289–300. doi: 10.1093/heapol/2.4.289. [DOI] [Google Scholar]
- [78].Widayati A. Health Seeking Behavior di Kalangan Masyarakat Urban di Kota Yogyakarta [Health seeking behavior of people in urban communities of Yogyakarta city] J Pharm Sci Community. 2012;9:59–65. [Google Scholar]
- [79].Safitri EM, Luthviatin N, Ririanty M. Determinan Perilaku Pasien dalam Pengobatan Tradisional dengan Media Lintah [Studi pada Pasien Terapi Lintah di Desa Rengel Kecamatan Rengel Kabupaten Tuban] [Factors determining patients’ seeking care from traditional Leeches therapy - a study of Leeches therapy in Rengel, Tuban] Pustaka Kesehat. 2016;4:181–7. [Google Scholar]
- [80].Ngambut K, Sila O. Faktor lingkungan dan perilaku masyarakat tentang malaria di Kecamatan Kupang Timur Kabupaten Kupang [Environmental and behavioral factors related to malaria in Kupang Timur, Kupang] J Kesehat Masy Nas. 2013;7:271–8. [Google Scholar]
- [81].Kristiono R, Wardani Y. Faktor-faktor yang berhubungan dengan pola pencarian pengobatan ke pelayanan kesehatan alternatif pasien suspek tuberculosis di komunitas [Factors influencing suspected tuberculosis patients’ seeking care behavior from alternative health providers] J Kes Masy. 2013;7 [Google Scholar]
- [82].Kurnia SH, Eli Kosasih C, Prawesti PA. Faktor-faktor yang melatarbelakangi pasien patah tulang berobat ke pengobatan tradisional ahli tulang di Sumedang [Factors influencing bone fracture patients seeking care from traditional bonesetter in Sumedang] Stud e-J. 2012;1:31. [Google Scholar]
- [83].Triratnawati A. Pengobatan tradisional, upaya meminimalkan biaya kesehatan masyarakat desa di Jawa [Traditional medication, an effort to minimize health care cost of Javanese people residing in rural areas] J Manaj Pelayanan Kesehat. 2010;13:69–73. [Google Scholar]
- [84].Supardi S, Susyanty AL. Penggunaan obat tradisional dalam upaya pengobatan sendiri di Indonesia-(analisis data Susenas tahun 2007) [The use of traditional medicines in self-medication in Indonesia-an analysis of National Socio-Economic Survey 2007] Bul Penelit Kesehat. 2010;38:80–9. [Google Scholar]
- [85].Ningsi, Anastasia H, Nurjana MA. Aspek sosial budaya masyarakat berkaitan dengan kejadian malaria di desa Sidoan Kabupaten Parigi Moutong Sulawesi Tengah [Socio cultural aspect among community related and malaria in Sidoan village, Parigi Moutong distric, central Sulawesi] Supplemen Media Penelit Pengemb Kesehat. 2010 [Google Scholar]
- [86].Kamaluddin R. Pertimbangan dan alasan pasien hipertensi menjalani terapi alternatif komplementer bekam di Kabupaten Banyumas [Factors influencing hypertension patients seeking care from complementary and alternative cupping therapy in Banyumas] J Keperawatan Soedirman. 2010;5:95–104. [Google Scholar]
- [87].Jauhari AH, Jauhari MSUH, Utami MS, Padmawati RS. Motivasi dan Kepercayaan Pasien untuk Berobat ke Sinse [Patients’ motivations and beliefs in seeking help from Sinse, traditional Chinese medicines] Ber Kedokt Masy. 2008;24:1. [Google Scholar]
- [88].Budijanto D, Roosihermiatie B. Persepsi sehat-sakit dan pola pencarian pengobatan masyarakat daerah pelabuhan (Kajian Kualitatif Di Daerah Pelabuhan Tanjung Perak) [Health-illness perceptions, and health seeking behavior of people in Port of Tanjung Perak: a qualitative study] Bul Penelit Sist Kesehat. 2006;9:93–9. [Google Scholar]
- [89].Supardi S, Jamal S, Raharni Pola Penggunaan Obat, Obat Tradisional dan Cara Tradisional dalam Pengobatan Sendiri di Indonesia [The pattern of the use of medicine, traditional medicine and traditional methods self-medication] Bul Penel Kesehat. 2005;33:192–8. [Google Scholar]
- [90].Shinta S, Sukowati S, Titik Sapardiyah S. Pengetahuan, sikap dan perilaku masyarakat terhadap malaria di daerah non endemis, di kabupaten Purworejo, Jawa Tengah [Study on knowledge, attitude and practice (KAP) of malaria in the community in non malaria endemic area, Purworejo district, Central Java] J Ekol Kesehat. 2005;4:254–64. [Google Scholar]
- [91].Hendarwan H. Faktor-Faktor Yang Berhubungan Dengan Perilaku Ibu Balita Dalam Pencarian Pengobatan Pada Kasus-Kasus Balita Dengan Gejala Pneumonia di Kabupaten Serang Banten, Tahun 2003. [Factors influencing mothers behavior in seeking care for children with pneumonia symptoms in Serang district] Project report. Pusat Penelit dan Pengemb Ekologi Kesehat. 2005;15 [Google Scholar]
- [92].Zalbawi S, Santoso SS. Pola Pemanfaatan Pengobatan Tradisional oleh Pasien Rematik [Patter of traditional healers visited by rheumatic patient] J Ekol Kesehat. 2002;1:85–93. [Google Scholar]
- [93].Santoso SS, Prasodjo R, Zalbawi S. Faktor-faktor yang mendorong penderita hipertensi ke pengobatan tradisional di DKI Jakarta, Yogyakarta, dan Surabaya [Factors influencing hypertension patients seeking care from traditional and alternative therapies: a study in Jakarta, Yogyakarta, and Surabaya] Media Litbang Kesehat. 2001;11 [Google Scholar]
- [94].Djaja S, Ariawan I, Afifah T. Determinan perilaku pencarian pengobatan infeksi saluran pernafasan atas (ISPA) pada balita [The determinant of health seeking behavior of acute respiratory infection in infant and children under-five years old] Bul Penelit Kesehat. 2001;29 [Google Scholar]
- [95].Santoso SS, Waluyo I, Kasnodiharjo K. Profil penderita diabetes melitus yang berobat ke pengobat tradisional di DKI Jakarta, DI Yogyakarta, dan Surabaya [The profile of diabetes melitus cases coming to the traditional healers in DKI Jakarta, Di Yogyakarta, and Surabaya] Bul Penelit Kesehat. 1999;27 [Google Scholar]
- [96].Handayani L, Siswanto S, Ma’ruf NA, Hapsari D. Pola pencarian pengobatan di Indonesia: analisis data Susenas 2001 [Health seeking behaviour pattern in Indonesia: an analysis of National Socio-Economic survey 2001] Bul Penelit Kesehat. 2003;31:33–47. [Google Scholar]
- [97].Kroeger A. Anthropological and socio-medical health care research in developing countries. Soc Sci Med. 1983;17:147–61. doi: 10.1016/0277-9536(83)90248-4. [DOI] [PubMed] [Google Scholar]
- [98].McKinlay JB. Some approaches and problems in the study of the use of services—an overview. J Health Soc Behav. 1972;13:115–52. https://www.ncbi.nlm.nih.gov/pubmed/4557538. [PubMed] [Google Scholar]
- [99].Regional Office for South-East Asia, World Health Organization . Health in the sustainable development goals: where are we now in the South-East Region? What next? Geneva: World Health Organization; 2016. https://apps.who.int/iris/handle/10665/249536. [Google Scholar]
- [100].World Health Organization . Global tuberculosis report 2015. 20th ed. Geneva: World Health Organization; 2015. https://apps.who.int/iris/handle/10665/191102. [Google Scholar]
- [101].World Health Organization . World Malaria Report 2018. Geneva: World Health Organization; 2018. https://apps.who.int/iris/handle/10665/275867. [Google Scholar]
- [102].Hussain MA, Mamun AA, Reid C, Huxley RR. Prevalence, awareness, treatment and control of hypertension in Indonesian adults aged ≥40 years: findings from the Indonesia Family Life Survey (IFLS) PLoS One. 2016;11:e0160922. doi: 10.1371/journal.pone.0160922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].World Health Organization . Diabetes country profile 2016: Indonesia. Geneva: World Health Organization; p. 2016. https://www.who.int/diabetes/country-profiles/idn_en.pdf?ua=1 (accessed 2 May 2018). [Google Scholar]
- [104].Pramono LA, Setiati S, Soewondo P, Subekti I, Adisasmita A, Kodim N, et al. Prevalence and predictors of undiagnosed diabetes mellitus in Indonesia. Acta Med Indones. 2010;42:216–23. https://www.ncbi.nlm.nih.gov/pubmed/21063043. [PubMed] [Google Scholar]
- [105].Statistics Indonesia . Nationality, ethnic groups, religions and daily languages of people in Indonesia: the result of 2010 census. Jakarta: Statistics Indonesia; 2011. [Google Scholar]
- [106].Calnan M. Health and illness: the lay perspective. London, New York: Tavistock Publications; 1987. [Google Scholar]
- [107].Elfahmi, Woerdenbag HJ, Kayser O. Jamu: Indonesian traditional herbal medicine towards rational phytopharmacological use. J Herb Med. 2014;4:51–73. doi: 10.1016/j.hermed.2014.01.002. [DOI] [Google Scholar]
- [108].Stanton BF. Assessment of relevant cultural considerations is essential for the success of a vaccine. J Health Popul Nutr. 2004;22:286–92. https://www.ncbi.nlm.nih.gov/pubmed/15609781. [PubMed] [Google Scholar]
- [109].Hjelm K, Mufunda E. Zimbabwean diabetics’ beliefs about health and illness: an interview study. BMC Int Health Hum Rights. 2010;10:7. doi: 10.1186/1472-698X-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Hjelm K, Atwine F. Health-care seeking behaviour among persons with diabetes in Uganda: an interview study. BMC Int Health Hum Rights. 2011;11:11. doi: 10.1186/1472-698X-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Henderson LC. Divergent models of diabetes among American Indian elders. J Cross Cult Gerontol. 2010;25:303–16. doi: 10.1007/s10823-010-9128-4. [DOI] [PubMed] [Google Scholar]
- [112].Basity S, Iravani MR. Health seeking behavior of diabetic patients in Koohzar village in Damghan city. Med Arch. 2014;68:384–8. doi: 10.5455/medarh.2014.68.384-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Tucker CM, Lopez MT, Campbell K, Marsiske M, Daly K, Nghiem K, et al. The effects of a culturally sensitive, empowerment-focused, community-based health promotion program on health outcomes of adults with type 2 diabetes. J Health Care Poor Underserved. 2014;25:292–307. doi: 10.1353/hpu.2014.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Radji M, Fauziah S, Aribinuko N. Antibiotic sensitivity pattern of bacterial pathogens in the intensive care unit of Fatmawati Hospital, Indonesia. Asian Pac J Trop Biomed. 2011;1:39–42. doi: 10.1016/S2221-1691(11)60065-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Bérdy J. Thoughts and facts about antibiotics: where we are now and where we are heading. J Antibiot (Tokyo) 2012;65:385–95. doi: 10.1038/ja.2012.27. [DOI] [PubMed] [Google Scholar]