Abstract
Atopic dermatitis (AD), a prevalent chronic skin disease in children, has been associated with psychosocial illness and reduced quality of life because of severe itching and sleep deprivation. Previous studies have found a consistent association between AD and attention deficit hyperactivity disorder (ADHD). However, little is known about this relationship in Chinese children with AD.
To investigate co-occurrence of ADHD symptoms, oppositional defiant disorder (ODD) symptoms, and the relevant risk factors of AD, as well as its impact on the quality of life in Chinese school-aged children with AD.
Outpatients aged 6 to 12 years with confirmed AD and healthy controls matched for age were randomly included in this study from October 2018 to October 2019. AD severity was evaluated using the Severity Scoring of Atopic Dermatitis scale (SCORAD). Inattention, hyperactivity, and oppositional defiant symptoms were evaluated by using the Swanson, Nolan and Pelham IV Teacher and Parent 26-Item Rating Scale (SNAP-IV) questionnaires and quality of life was evaluated using the Children's Dermatology Life Quality Index (CDLQI).
The study included 89 AD patients and 184 healthy controls. AD patients were more likely to have ADHD symptoms (10.1% vs. 3.8%; P = .04) and ODD symptoms (5.6% vs 0%; P < .001) than controls, especially hyperactive/impulsive (P = .03). The severity of itching and sleep loss in AD patients were positively correlated with inattention (P = .03; P < .001), hyperactivity/impulsiveness (P = .01; P = .03), and oppositional defiance scores (P < .01; P = .04). Sleep loss in AD patients was independently associated with an increased risk of ADHD symptoms (OR, 1.78; 95% CI, 1.07–2.98; P = .03). The mean CDLQI scores of AD patients were 6.98 ± 5.02, and CDLQI scores were significantly higher in AD patients with ADHD symptoms than in those without ADHD symptoms (11.44 vs. 6.48; P = .01).
AD is a prevalent chronic condition associated with an increased likelihood of ADHD symptoms and ODD symptoms in school-aged children. Sleep deprivation caused by AD may be a risk factor for ADHD. AD affects quality of life, especially in patients with ADHD symptoms. AD patients with symptoms of inattention and hyperactivity should be evaluated for ADHD.
Keywords: atopic dermatitis, attention deficit hyperactivity disorder, children, quality of life
1. Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin disease mainly affecting children, with a prevalence of 15% to 20%, compared with 1% to 3% in adults.[1] The main symptoms of AD include intense itching, eczema-like rashes, and sleep loss. Children of primary school age are in a key period of growth, development, and interpersonal communication. AD skin lesions in exposed areas, severe pruritus, and sleep deprivation may affect children's mental health, with many of these children experiencing psychological and behavioral problems, such as attention deficit hyperactivity disorder (ADHD), anxiety, and depression.[2]
ADHD is one of the most common childhood-onset psychiatric disorders, with a worldwide prevalence greater than 5%.[3] Its characteristic symptoms include being unable to concentrate on one task, looking around frequently, excitability and hyperactivity, tantrums and aggressive behavior, recklessness, lack of patience, and frequent conflicts with teachers and classmates. However, its etiology is not fully understood. ADHD is sometimes associated with oppositional defiant disorder. Both AD and ADHD impose high financial burdens on social services. AD can cause distraction and difficulties with attention and concentration. Although AD in children is closely associated with the occurrence of ADHD,[4,5] little is known about the relationship between AD and ADHD in Chinese children. We hypothesized that AD in school-aged children is independently associated with an increased risk of ADHD symptoms and oppositional defiant disorder (ODD) symptoms, and that the severity of AD and sleep deprivation together increase the risk of ADHD symptoms. Therefore, this study was designed to evaluate the co-occurrence of ADHD symptoms and the relevant risk factors of AD, and to determine its impact on the quality of life of Chinese school-aged children with AD.
2. Materials and methods
2.1. Study design and participants
A cross-sectional study was conducted on 6 to 12 years old children who visited the Children's Hospital of Chongqing Medical University, China, from October 2018 to October 2019. AD patients were diagnosed according to UK criteria and randomly included in the study.[6–8] Children with other major illnesses, such as psoriasis, epilepsy, and stunting, were excluded. In addition, healthy controls were selected by performing clustering sampling on children evaluated in the Department of Physical Examination of the Children's Hospital of Chongqing Medical University. Inclusion criteria were 6 to 12 years of age and volunteering to participate in the study. Exclusion criteria included physical and mental disorders. The cluster method was conducted according to age. The study protocol was approved by the Ethics Committee of the Children's Hospital of Chongqing Medical University, China, and all participants and their parents provided written informed consent.
2.2. AD symptom score
AD symptom scores were assessed by a dermatologist using the Severity Scoring of Atopic Dermatitis (SCORAD) index.[9] The SCORAD index consists of 3 subscales: interpretation of the extent of the disorder (subscale A; 20% of the total score); intensity of 6 symptoms, erythema, edema/papules, scratches, oozing/crust formation, lichenification, and dryness, with each item graded 0–3 (subscale B; 60% of the score); and subjective symptoms including pruritus and sleeplessness (subscale C; 20% of the score). The distribution of the score was calculated using the formula A|5 + 7B|2 + C. The maximum possible score was 103. Patients were classified by SCORAD score as having mild (<25), moderate (∼25–50), or severe (>50) AD.
2.3. Behavioral assessments
Parents assessed their children's inattention, hyperactivity, and oppositional defiance symptoms using Swanson, Nolan and Pelham IV Teacher and Parent 26-Item Rating Scale (SNAP-IV) questionnaires. The SNAP-IV is a widely used scale that measures the core symptoms of ADHD. It consists of 9 items evaluating symptoms of inattention (IA, items 1–9) and hyperactivity/impulsivity (HI, items 10–18), and 8 items (items 19–26) evaluating oppositional symptoms of oppositional defiant disorder. Each item was rated on a 4-point scale, with 0 = not at all, 2 = just a little, 3 = quite a bit, and 4 = very much.[10] The Chinese version of SNAP-IV was shown to be a reliable and valid instrument for rating ADHD-related symptoms both clinically and in the community.[11]
2.4. Quality of life assessment
Parents evaluated children's quality of life using the Children's Dermatology Life Quality Index (CDLQI), a dermatology-specific questionnaire that measures quality of life in children aged 4 to 16 years. The CDLQI, which measures the degree to which a skin problem affected patient quality of life during the previous 7 days, consists of 10 questions, each having 4 possible responses, identical to those of the SNAP-IV. Total scores ranged from 0 to 30. CDLQI scores were subclassified as 0–1 (no effect on quality of life), 2–6 (little effect), 7–12 (moderate effect), 13–18 (very large effect), or 19–30 (extremely large effect).[12]
2.5. Statistical analysis
Continuous variables were reported as mean ± SD and compared by the Mann–Whitney U test, and categorical variables were reported as number (percent) and compared by the χ2 test. Correlations were analyzed using Spearman correlation coefficient correlation analysis. Univariate and multivariate logistic regression analyses were performed to assess independent variables. All statistical analyses were performed using Statistical Package for Social Science (SPSS) software (version 25), with P < .05 defined as statistically significant.
3. Results
3.1. Participants
A total of 114 patients with AD and 201 nonatopic age-matched controls were included in this study. Eighty-nine patients (mean age, 8.30 ± 1.69 years; 61.8% male) and 184 controls (mean age, 8.29 ± 1.99 years; 63% male) completed the study. The SCORAD of the AD group was 44.09 ± 13.15, of whom 5.6% had mild, 66.3% had moderate, and 25% had severe AD. In addition, 44 (49.4%) of the AD patients had allergic rhinitis and 23 (25.8%) had asthma. 44 (40.9%) patients had a first-degree relative with a history of atopy. The other characteristics of the 2 groups are shown in Table 1.
Table 1.
Characteristics of children with atopic dermatitis, and age- and sex-matched controls.

3.2. Co-occurrence of ADHD symptoms and ODD symptoms in AD patients and controls
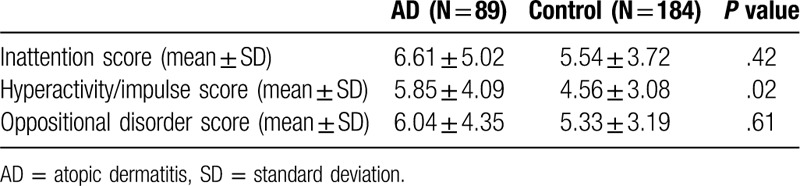
Hyperactivity/impulse score was significantly higher in the AD than in the control group (P = .02). There was no significant difference between the AD group and the control group in the scores of inattention (P = .42) and oppositional defiance (P = .61) (Table 2).
Table 2.
Behavioral assessment of atopic dermatitis patients and controls using the SNAP-IV Parental Rating Scale.
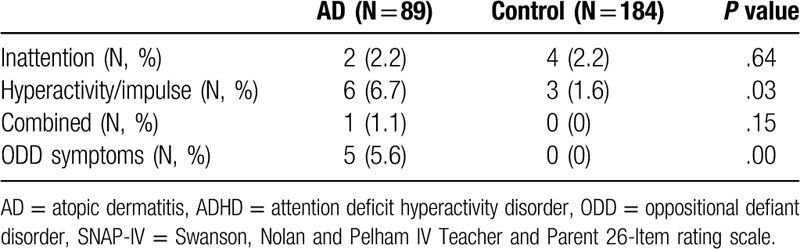
Children with AD were more likely to have ADHD symptoms (10.1% vs. 3.8%; P = .04) and ODD symptoms (5.6% vs 0%; P < .001) than children without AD, especially hyperactive/impulsive symptoms (P = .03) (Table 3).
Table 3.
ADHD subtype and ODD assessment of AD patients and controls using the SNAP-IV parent rating scale.
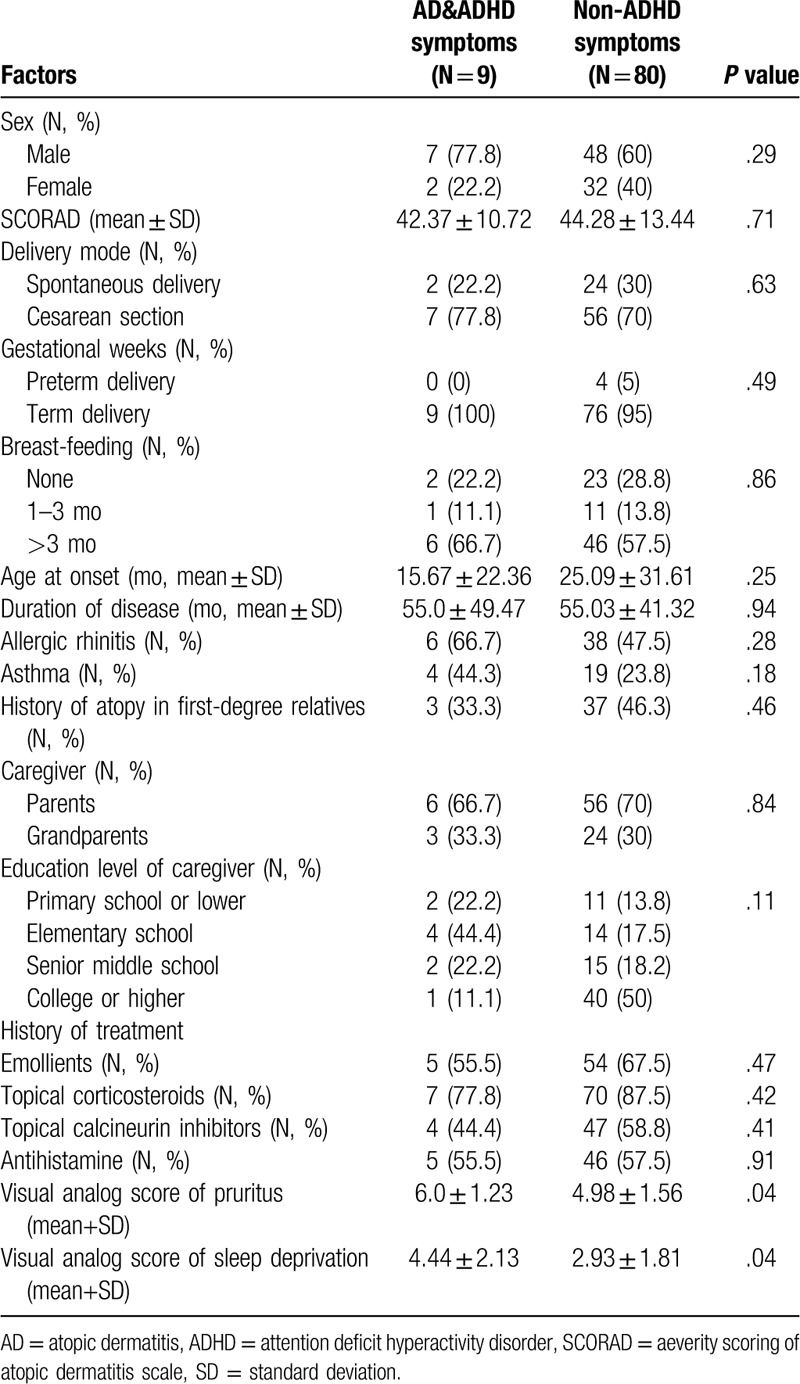
3.3. Differences in relevant factors between AD with and without ADHD symptoms
Gender, severity of AD, delivery mode, gestational weeks, breast feeding, age at onset and duration of AD, history of allergic rhinitis and asthma, familial history of atopy, education level of caregiver, and a history of use of emollients, topical glucocorticoids, topical calcineurin inhibitors, and oral antihistamines were not significantly different between the 2 groups (Table 4).
Table 4.
Comparison of the general characteristics of patients in the AD group with and without ADHD symptoms.
The scores of inattention, hyperactivity/impulse, and oppositional defiance were positively associated with pruritus (r = .24, P = .03; r = .27, P = .01; r = .30, P < .001, respectively) and sleep deprivation (r = .30, P = .00; r = .23, P = .03; r = .22, P = .04, respectively) in the AD group (Fig. 1).
Figure 1.
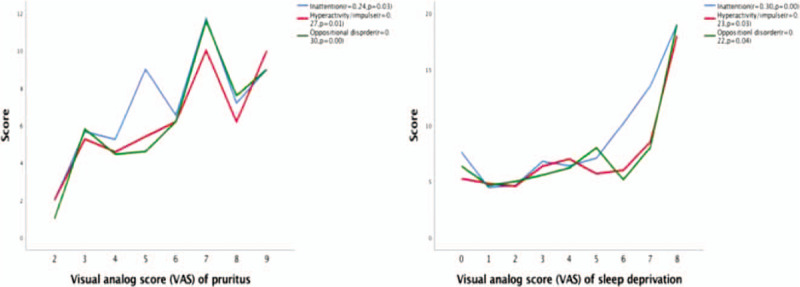
Correlation between inattention, hyperactivity/impulse, oppositional disorder scores and visual analog scores of pruritus and sleep deprivation in atopic dermatitis patients.
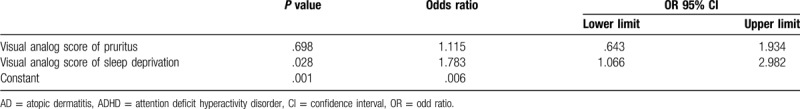
Multivariable analysis showed that sleep deprivation (odds ratio [OR], 1.78; 95% confidence interval [CI], 1.07–2.98; P = .03) was independently associated with an increased risk of ADHD symptoms (Table 5).
Table 5.
Comparison of the effect of extent of pruritus and sleep deprivation on the risks of ADHD symptoms in AD patients.
3.4. The quality of life of children with AD
The CDLQI score of AD patients was 6.98 ± 5.02. There was a strong correlation between SCORAD and CDLQI (r = .42, P < .001), and quality of life decreased with increases in AD severity. In addition, the mean CDLQI score was significantly higher in AD patients with ADHD symptoms than in those without ADHD symptoms (11.44 vs. 6.48; P = .01). CDLQI also showed statistically significant positive correlations with attention deficit score (r = .41, P < .001), hyperactivity/impulse score (r = .28, P < .001), and oppositional defiant score (r = .34, P = .00).
4. Discussion
Atopic dermatitis is a chronic skin disease characterized by pruritus and eczematous skin lesions. Epidemiological studies indicate that AD is not only associated with other atopic conditions, but also with a broad spectrum of emotional and behavioral problems.[13–16] Previous studies found that 68.8% of patients with AD have at least 1 psychiatric disorder, such as attachment disorder, conduct disorder, anxiety disorder, eating disorder, and tic disorder, as well as ADHD and enuresis. These disorders are significantly more frequent in patients with AD than in those without AD.[17] Children with AD are more likely to have ADHD than children without AD.[18] The present study found that although AD was associated with an increased likelihood of ADHD symptoms and ODD symptoms, it showed greater association with hyperactivity/impulse symptoms than with inattention. This may be due to the scratching caused by AD and the greater tolerance parents show toward children with AD. Previous studies found that AD is closely related to the occurrence of ADHD, but few studies have shown that AD is mainly associated with inattention or hyperactivity.[19–21]
In addition, some other characteristics of AD could influence the risk of ADHD symptoms. The extent of pruritus also contributed to ADHD symptoms. Sleep deprivation (odds ratio = 1.78) was associated with a higher risk of ADHD symptoms. Chronic sleep loss can also affect children's brain development. Pruritus, scratching, and lack of sleep can lead to behavior changes, difficulty concentrating, and difficulty in remembering daily tasks. Oral melatonin was found to significantly improve sleep-onset latency and disease severity in children and adolescents with AD, and these effects were comparable to those of melatonin in ADHD children with impaired sleep-onset.[22] These findings indicated that sleep problems may be an effect modifier in the relationship between AD and ADHD. It is also unclear whether the observed association is due to a common cause or is a secondary phenomenon of AD. For example, pruritus, sleep problems, and psychosocial disorders may exacerbate ADHD symptoms in patients with AD, resulting in AD symptoms being misclassified as ADHD. Further research on the causal relationships between AD and ADHD is required.
However, AD accompanied by allergic rhinitis or asthma did not correlate with ADHD symptoms. Asthma and medications used to treat asthma have also been reported to increase the likelihood of ADHD symptoms in children.[23] Moreover, another study found that a large percentage of children with ADHD have allergic rhinitis.[24] Although allergic rhinitis and asthma combined with AD significantly increased the risk of ADHD symptoms, allergic rhinitis and asthma unaccompanied by AD did not correlate with ADHD.[25] Allergies may play a role in ADHD by inducing an imbalance in central nervous system cholinergic/adrenergic activity, leading to poor regulation of arousal and ADHD behavior.[26]
We also found that AD was associated with reduced quality of life in children, with duration of AD, continuous scratching, and sleep disorders having a significant impact on patient quality of life. Among all common chronic diseases, AD has the second highest impact on quality of life behind cerebral palsy,[27] and its negative impact on quality of life is proportional to the severity of AD.[28] Children with ADHD were reported to have a lower quality of life than children with asthma and healthy controls.[29] Our study showed that children with AD and ADHD symptoms have a lower quality of life than children with AD and no ADHD symptoms. Furthermore, inattention score, hyperactivity/impulse score, and oppositional defiance score were related to CDLQI, indicating that ADHD is more deleterious to quality of life than allergic diseases.
The strengths of this study include a valid assessment of the extent of pruritus and sleep deprivation and it is the first study to report a significant relationship between AD and ADHD symptoms in the Chinese population. However, this study had several limitations, including its relatively small sample size. Moreover, symptoms of AD were based solely on parental reports, which may limit the validity and reliability of the data, and the interpretation of results. Further studies are needed, including studies analyzing the mechanism of the relationship between AD and ADHD.
5. Conclusion
Atopic dermatitis is a chronic disease with recurrent findings that are associated with ADHD symptoms and ODD symptoms in school-age children. Sleep problems independently contribute to an increased risk of ADHD symptoms. Itching and sleep deprivation were associated with attention deficit symptoms, hyperactivity/impulse symptoms, and oppositional defiance symptoms in patients with AD. Children with AD and ADHD symptoms have a lower quality of life than children with AD unaccompanied by ADHD symptoms. Patients with AD who present with signs of inattention and hyperactivity should be assessed for ADHD and, if necessary, provided with appropriate support.
Acknowledgments
The authors thank all patients who took part in this study.
Author contributions
Conceptualization: Xiao-yan Luo, Hua Wang.
Data curation: Ling-jie Feng.
Formal analysis: Ling-jie Feng.
Investigation: Ling-jie Feng, An-wei Chen, Xiao-yan Luo.
Methodology: Hua Wang.
Supervision: Hua Wang.
Writing – original draft: Ling-jie Feng.
Writing – review & editing: Hua Wang.
Footnotes
Abbreviations: AD = atopic dermatitis, ADHD = attention deficit hyperactivity disorder, CDLQI = children's dermatology life quality index, CI = confidence interval, ODD = oppositional defiant disorder, OR = odd ratio, SCORAD = severity scoring of atopic dermatitis scale, SD = standard deviation, SNAP-IV = Swanson, Nolan and Pelham IV Teacher and Parent 26-Item rating scale, VAS = visual analog score.
How to cite this article: Feng Lj, Chen Aw, Luo Xy, Wang H. Increased attention deficit/hyperactivity and oppositional defiance symptoms of 6–12 years old Chinese children with atopic dermatitis. Medicine. 2020;99:25(e20801).
This study was approved by the Ethics Committee of Children's Hospital of Chongqing Medical University.
The authors received no specific funding for this work.
For the participants, both caregivers had understood the foreseeable risks, potential benefits, and consequences of participating in the study and provided written consent.
The dataset analyzed during the current study is not publicly available due to reasons of confidentiality and the need to protect the privacy of participants.
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab 2015;66:8–16. [DOI] [PubMed] [Google Scholar]
- [2].Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity in patients with atopic dermatitis. J Allergy Clin Immunol 2013;131:428–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164:942–8. [DOI] [PubMed] [Google Scholar]
- [4].Hak E, de Vries TW, Hoekstra PJ, et al. Association of childhood attention-deficit/hyperactivity disorder with atopic diseases and skin infections? A matched case-control study using the General Practice Research Database. Ann Allergy Asthma Immunol 2013;111:102–6.e2. [DOI] [PubMed] [Google Scholar]
- [5].Strom MA, Fishbein AB, Paller AS, et al. Association between atopic dermatitis and attention deficit hyperactivity disorder in U.S. children and adults. Br J Dermatol 2016;175:920–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Williams HC, Jburney PG, Hay RJ, et al. The U. K. Working Party's Diagnostic Criteria for Atopic Dermatitis. I. Derivation of a minimum set of discriminators for atopic dermatitis. Br J Dermatol 1994;131:383–96. [DOI] [PubMed] [Google Scholar]
- [7].Williams HC, Jburney PG, Strachan D, et al. The U. K. Working Party's Diagnostic Criteria for Atopic Dermatitis II. Observer variation of clinical diagnosis and signs of atopic dermatitis. Br J Dermatol 1994;131:397–405. [DOI] [PubMed] [Google Scholar]
- [8].Williams HC, Jburney PG, Pembroke AC, et al. The U. K. Working Party's Diagnostic Criteria for Atopic Dermatitis. III. Independent hospital validation. Br J Dermatol 1994;131:406–16. [DOI] [PubMed] [Google Scholar]
- [9].Oranje AP, Glazenburg EJ, Wolkerstorfer A, et al. Practical issues on interpretation of scoring atopic dermatitis: the SCORAD index, objective SCORAD and the three-item severity score. Br J Dermatol 2007;157:645–8. [DOI] [PubMed] [Google Scholar]
- [10].Swanson JM, Kraemer HC, Hinshaw SP, et al. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 2001;40:168–79. [DOI] [PubMed] [Google Scholar]
- [11].Gau SS-F, Shang C-Y, Liu S-K, et al. Psychometric properties of the Chinese version of the Swanson, Nolan, and Pelham, version IV scale—parent form. Int J Methods Psychiatr Res 2008;17:35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lewis-Jones MS, Finlay AY. The Children's Dermatology Life Quality Index (CDLQI): initial validation and practical use. Br J Dermatol 2010;132:942–9. [DOI] [PubMed] [Google Scholar]
- [13].Simpson EL. Comorbidity in atopic dermatitis. Curr Dermatol Rep 2012;1:29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Schmitt J, Chen C-M, Apfelbacher C, et al. Infant eczema, infant sleeping problems, and mental health at 10 years of age: the prospective birth cohort study LISAplus: infant eczema, sleep problems & mental health at age 10. Allergy 2011;66:404–11. [DOI] [PubMed] [Google Scholar]
- [15].Schmitt J, Apfelbacher C, Chen C-M, et al. Infant-onset eczema in relation to mental health problems at age 10 years: results from a prospective birth cohort study (German Infant Nutrition Intervention plus). J Allergy Clin Immunol 2010;125:404–10. [DOI] [PubMed] [Google Scholar]
- [16].Wan J, Takeshita J, Shin DB, et al. Mental health impairment among children with atopic dermatitis: a U.S. population-based cross-sectional study of the 2013-2017 National Health Interview Survey. J Am Acad Dermatol 2019;S0190962219329020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Catal F, Topal E, Soylu N, et al. Psychiatric disorders and symptoms severity in preschool children with atopic eczema. Allergol Immunopathol 2016;44:120–4. [DOI] [PubMed] [Google Scholar]
- [18].Roth N, Beyreiss J, Schlenzka K, et al. Coincidence of attention deficit disorder and atopic disorders in children: empirical findings and hypothetical background. J Abnorm Child Psych 1991;19:1–3. [DOI] [PubMed] [Google Scholar]
- [19].Romanos M, Gerlach M, Warnke A, et al. Association of attention-deficit/hyperactivity disorder and atopic eczema modified by sleep disturbance in a large population-based sample. J Epidemiol Community Health 2010;64:269–73. [DOI] [PubMed] [Google Scholar]
- [20].Schmitt J. Atopic eczema and attention-deficit/hyperactivity disorder in a population-based sample of children and adolescents. JAMA 2009;301:724. [DOI] [PubMed] [Google Scholar]
- [21].Schmitt J, Buske-Kirschbaum A, Tesch F, et al. Increased attention-deficit/hyperactivity symptoms in atopic dermatitis are associated with history of antihistamine use. Allergy 2018;73:615–26. [DOI] [PubMed] [Google Scholar]
- [22].Chang Y-S, Lin M-H, Lee J-H, et al. Melatonin supplementation for children with atopic dermatitis and sleep disturbance: a randomized clinical trial. JAMA Pediatr 2016;170:35–42. [DOI] [PubMed] [Google Scholar]
- [23].Yuksel H, Sogut A, Yilmaz O. Attention deficit and hyperactivity symptoms in children with asthma. J Asthma 2008;45:545–7. [DOI] [PubMed] [Google Scholar]
- [24].Brawley A, Silverman B, Kearney S, et al. Allergic rhinitis in children with attention-deficit/hyperactivity disorder. Ann Allergy Asthma Immunol 2004;92:663–7. [DOI] [PubMed] [Google Scholar]
- [25].Lee C-Y, Chen M-H, Jeng M-J, et al. Longitudinal association between early atopic dermatitis and subsequent attention-deficit or autistic disorder: a population-based case-control study. Medicine 2016;95:e5005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Marshall P. Attention deficit disorder and allergy: a neurochemical model of the relation between the illnesses. Psychol Bull 1989;106:434–46. [DOI] [PubMed] [Google Scholar]
- [27].Beattie PE, Lewis-Jones MS. A comparative study of impairment of quality of life in children with skin disease and children with other chronic childhood diseases. Br J Dermatol 2006;155:145–51. [DOI] [PubMed] [Google Scholar]
- [28].Holm JG, Agner T, Clausen M-L, et al. Quality of life and disease severity in patients with atopic dermatitis. J Eur Acad Dermatol 2016;30:1760–7. [DOI] [PubMed] [Google Scholar]
- [29].Escobar R. Worse quality of life for children with newly diagnosed attention-deficit/hyperactivity disorder, compared with asthmatic and healthy children. Pediatrics 2005;116:e364–9. [DOI] [PubMed] [Google Scholar]


