Abstract
Improved understanding of how three-dimensional (3-D) femoral head coverage changes as the pelvic sagittal inclination (PSI) is altered would advance clinical diagnosis of hip pathoanatomy. Herein, we applied computer modeling of 3-D computed tomography reconstructions of the pelvis and proximal femur to quantify relationships between the PSI and regional 3-D femoral head coverage. Eleven healthy, young adult participants with typically developed hip anatomy were analyzed. The orientation of the pelvis was altered to define a PSI of −30° to 30° at 1° increments. Hip adduction and rotation were fixed in a standing position, which was measured by direct in-vivo imaging of the pelvis and femur bones using dual fluoroscopy. Femoral head coverage was quantified in the anterior, superior, posterior, and inferior regions for each PSI position. Change in coverage was largest in the anterior region (29.8%) and smallest in the superior region (6.5%). Coverage increased linearly in the anterior region as the PSI increased, while a linear decrease was found in the posterior region and the inferior region (all p<0.001). The slope of the regression line for these regions were 0.513, −0.316, and −0.255, respectively. For the superior region, coverage increased when the PSI was altered from −30° to 5° and decreased when the PSI was larger than 5°. Overall, a 1° increase in PSI resulted in an increase of 0.5% in anterior coverage and a decrease of 0.3% in posterior coverage. Our findings provide baseline data that improve understanding of the effect of PSI on femoral coverage.
Keywords: pelvic sagittal inclination, areal head coverage, regional analysis, computational analysis, regression model, acetabulum
Introduction
Consideration of femoral head coverage is important when making a diagnosis of structural hip disease as well as planning surgical procedures such as peri-acetabular osteotomy and total hip arthroplasty. Most often, coverage is assessed from two-dimensional measurements of plain-film radiographs. Caution must be exercised when evaluating femoral head coverage from plain films since measurements are sensitive to the pelvic sagittal inclination (PSI), which varies according to the position of the patient. For example, studies have shown that the difference in PSI between the supine and standing position alters the measurement of head coverage on anteroposterior radiographs, which ultimately can change the diagnosis (Henebry and Gaskill, 2013; Pullen et al., 2014). The PSI has been evaluated in studies of developmental dysplasia of the hip (DDH) (Fukushima et al., 2018; Tachibana et al., 2019), femoroacetabular impingement syndrome (FAIS) (Pullen et al., 2014), and hip osteoarthritis (OA) (Pierrepont et al., 2017; Uemura et al., 2017). Nevertheless, prior research has not quantified how femoral head coverage changes as the PSI is altered, which is an important knowledge gap since orthopaedic procedures aim to modify femoral head coverage through corrective osteotomies and/or debridement of the native anatomy (Sardana et al., 2015; Tanaka et al., 2018).
Clarifying how femoral head coverage changes when the PSI is altered may provide biomechanical context when making a diagnosis and planning treatment. For example, a loss of anterior head coverage as PSI decreases would corroborate previous findings that increased contact stresses in the anterior region of the hip lead to progression of hip OA (Uemura et al., 2017). As another example, quantifying the relationship between PSI and head coverage could assist in planning the degree of rotation necessary when performing procedures such as peri-acetabular osteotomy. Previously, studies have evaluated femoral head coverage using the lateral center-edge angle (LCEA) (Wiberg, 1953) and anterior center-edge angle (Lequesne and de, 1961). However, these 2-D measurements of femoral head coverage are prone to measurement error; research has demonstrated that inter- and intra-observer errors may exceed the clinically relevant difference in these measures due to differences across researchers in how the edge of the acetabular rim is defined (Clohisy et al., 2009). Further, the relationship between 2-D measurements and actual three-dimensional (3-D) coverage for each anatomic region of the femoral head (i.e. anterior, superior, posterior, inferior) has been shown to be weak (Hansen et al., 2012).
The purposes of this study were to: 1) quantify regional 3-D head coverage by altering the PSI, and 2) establish the relationship between regional 3-D head coverage and the PSI. Three-dimensional femoral head coverage has not previously been assessed as a function of PSI. Thus, we focused this study on asymptomatic controls with typically developed hip anatomy to provide reference data necessary to evaluate patients with structural hip disease in the future. We hypothesized: 1) anterior coverage increases with anterior pelvic tilt and decreases with posterior pelvic tilt, and that 2) regional femoral head coverage could be predicted from changes in the PSI.
Materials and Methods
Eighteen asymptomatic participants without a history of injury or surgery to either lower limb provided consent to participate in this Institutional Review Board approved study. An anteroposterior film in the standing position was used to screen participants with morphological abnormalities, including DDH, acetabular retroversion, and deformities found in patients with FAIS. Based on the appearance of their anteroposterior film, seven subjects were excluded, leaving eleven subjects (6 male). For these eleven subjects, the mean ± standard deviation (SD) age and body mass index was 23 ± 2 years and 21 ± 2 kg/m2, respectively. The mean ± SD LCEA, extrusion index, and Tönnis angle on an anteroposterior radiograph was 32.8 ± 5.0°, 11.8 ± 4.6%, and 3.6 ± 3.7°, respectively.
Image preprocessing, definition of the pelvic coordinate system, and calculation of PSI
For eleven subjects enrolled herein, in-vivo hip kinematics were previously analyzed using a combined experimental and computational protocol that included a computed tomography (CT) scan, dual fluoroscopy (DF), and model-based tracking (MBT) (Uemura et al., 2018a; Uemura et al., 2018b). Surface models of the pelvis and femur (i.e., nodes with triangular faces) were first generated by semi-automatic segmentation of CT images using Amira (v.6.0.1, Visage Imaging, San Diego, CA, USA).
To identify the anatomical landmarks necessary to define the coordinate system of the pelvis, a host of candidate nodes on the pelvis that contained the landmark of interest was lassoed manually in Postview (v.2.0, University of Utah, Salt Lake City, UT (Maas et al., 2012)). Then, the single node among the candidate list that represented the landmark of interest was found using Matlab (v.7.10, The MathWorks, Natick, MA). Specifically, the anterior superior iliac spines (ASIS) and the pubic tubercles were selected as the most anterior node. Using the bilateral ASIS and the center of the pubic tubercles, the anterior pelvic plane (APP) was generated (Fig. 1) (McKibbin, 1970; Uemura et al., 2017). The transverse axis was set as the line connecting the two ASIS landmarks. Setting the APP as the neutral position, PSI was defined as the sagittal tilt of the pelvis about the transverse axis (i.e. PSI 0° at APP). Anterior tilt of the pelvis from the APP represents a positive PSI whereas posterior tilt represents a negative PSI (Fig. 2).
Figure 1.
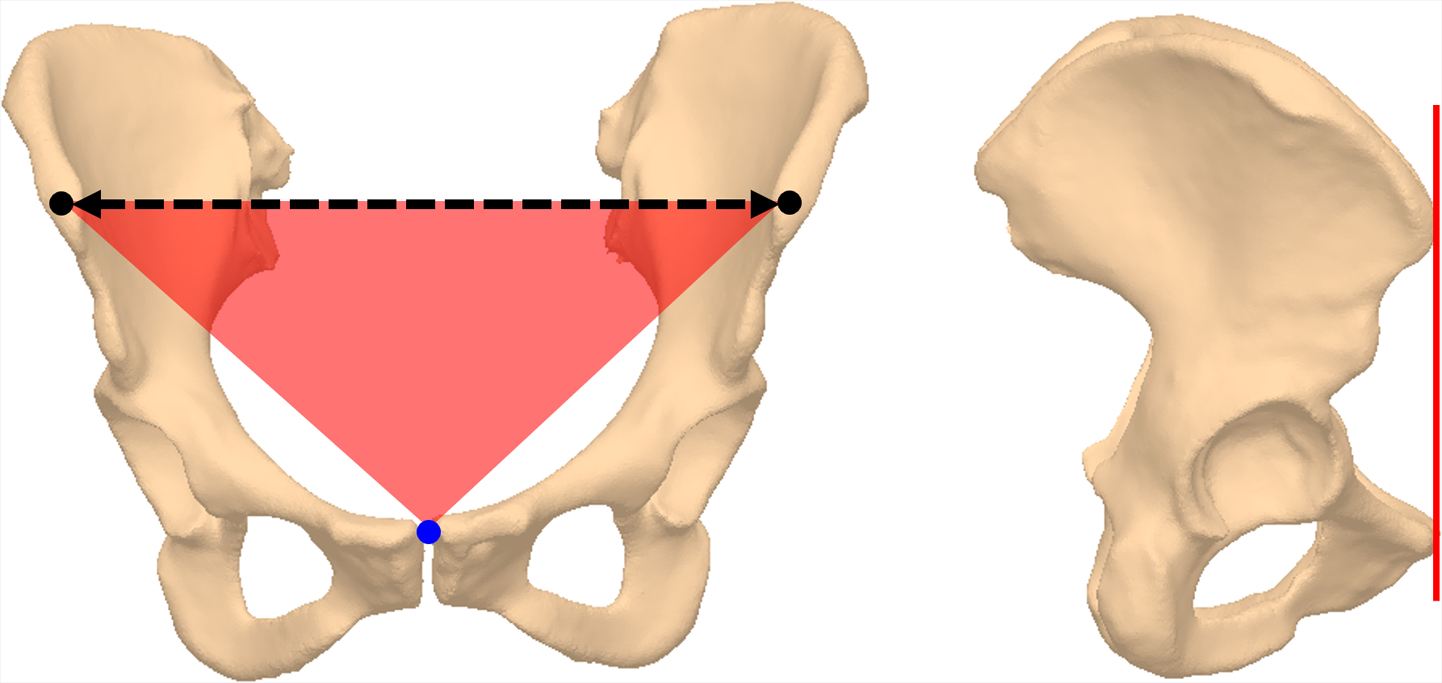
Construction of the anterior pelvic plane (APP) on an anteroposterior view (left) and on a lateral view (right). The APP (red plane) was defined as a plane that included the bilateral anterior superior iliac spines (ASIS, black circle) and the center of the pubic tubercles (blue). The transverse axis of APP (black dotted line) was defined as the line connecting the two ASIS landmarks and was used to rotate the pelvis.
Figure 2.
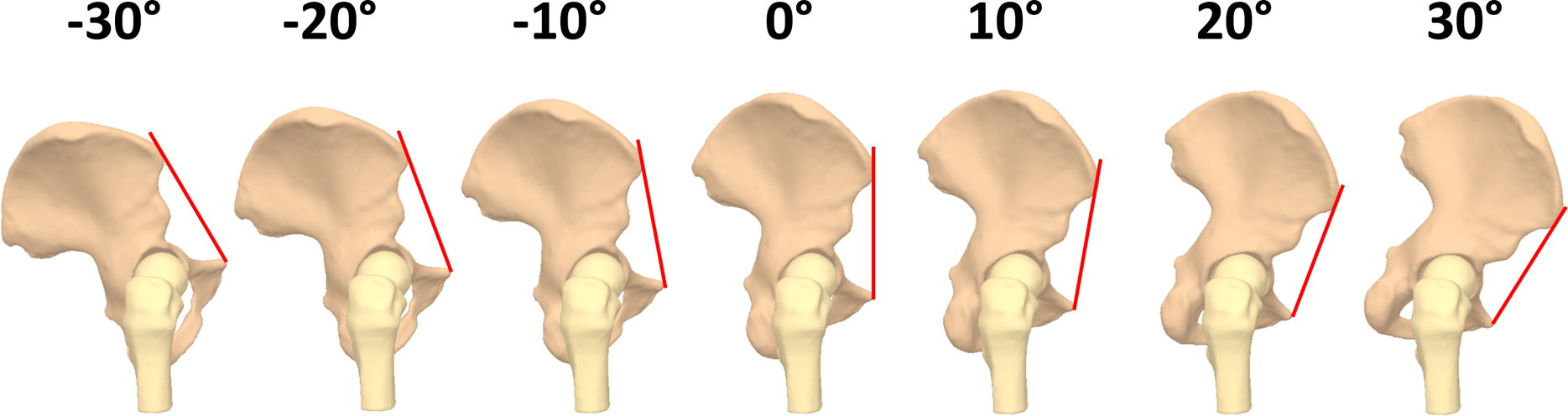
Lateral view of the right hip when the pelvic sagittal inclination (PSI) ranged from −30° to 30°. The anterior pelvic plane (red line) was rotated anteriorly or posteriorly about the axis that included the left acetabular center and was parallel to the transverse axis, which connected the bilateral anterior superior iliac spines. For clarity, pelvic positions are shown at increments of 10° of PSI between −30° and 30°.
Calculation of head coverage and classification of the head surface into four regions
Femoral head coverage was defined as the bony region of the head surface that was covered by the lunate surface of the acetabulum (Uemura et al., 2018b). To quantify coverage, the lunate (Fig. 3a) and head surfaces (Fig. 3b) were first identified using principal curvature in Postview as described previously (Kapron et al., 2014; Uemura et al., 2018b). The 3D coverage of the femoral head was then quantified using the Coverage Tool in Postview (Uemura et al., 2018b). Briefly, surface elements of the femoral head were considered ‘covered’ if they were intersected by the normal projection of any element of the lunate surface. Then, to quantify areal head coverage, the femoral head was divided into four quadrants (anterior, superior, posterior, inferior) in Matlab (Uemura et al., 2018b). Briefly, the nodes of the femoral head were divided into four regions around the neck axis in 90° increments using the femoral head center, knee center, and femoral neck axis (Fig. 3c).
Figure 3.
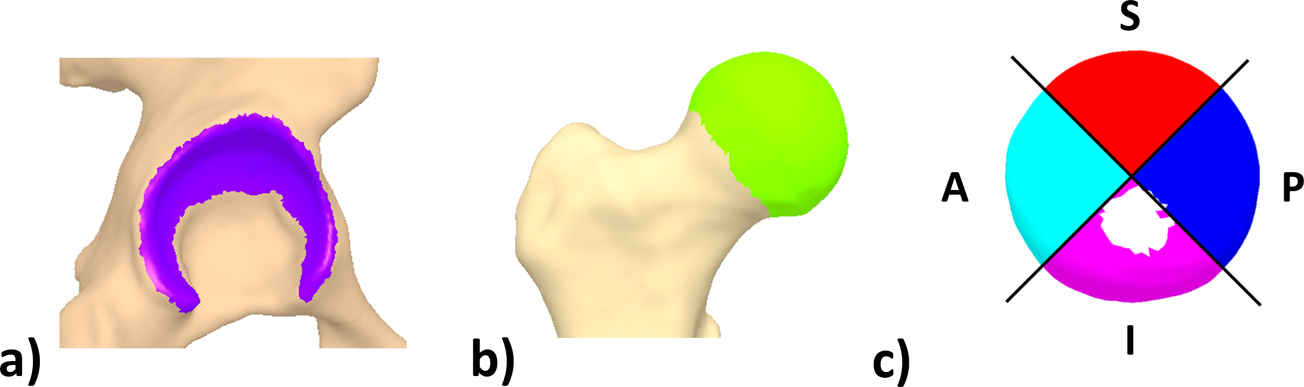
Generation of the three-dimensional surface models of the lunate surface and the quadrants of the femoral head surface shown for a right hip. (a) The lunate surface (purple) was selected from the pelvis surface model using 2nd principle curvature and manual selection. (b) The femoral head (light green) was selected from the femur model using 1st principle curvature. (c) Using the femoral head center, knee center, and femoral neck axis, the nodes of the femoral head were divided into four regions around the neck axis in 90° increments. A, anterior; S, superior; P, posterior; I, inferior.
Definition of the neutral position and calculation of coverage by simulating the PSI
To solely examine the effect of PSI on head coverage, angles of hip rotation and hip adduction were fixed during the simulation analysis. The neutral position of the hip varies across participants (Uemura et al., 2016; Uemura et al., 2018a; Uemura et al., 2018c). Herein, the neutral position was defined based on the relaxed standing position with the toes of the participant pointed forward (Uemura et al., 2018a). With participants in this position, the spatial position of the pelvis and femur was quantified using DF and MBT as described previously (Kapron et al., 2014; Uemura et al., 2018a; Uemura et al., 2018b). Briefly, images were acquired simultaneously from two fluoroscopes that were positioned to image the same region of the hip from two perspectives. Using MBT, images were aligned with the digitally reconstructed radiographs generated from CT images and the in-vivo position of the pelvis and the femur was quantified. Of note, kinematic measurement errors for DF are less than 0.5 mm and 0.6° (Kapron et al., 2014).
To calculate femoral head coverage, the pelvis was rotated anteriorly or posteriorly about the transverse axis of the APP (i.e. axis that includes bilateral ASIS) with the rotation center set as the center of the acetabulum of the examined hip. To include the variation of PSI in the supine and the standing position that has been reported in the literature (Pierrepont et al., 2017; Uemura et al., 2017), the coverage analysis was performed every 1° by altering the pelvic position to represent the PSI range of −30° to 30° (i.e. total of 61 analyses for each subject) (Fig. 2). For each pelvic position (i.e. for each PSI), no overlap occurred between the acetabulum and the femur bone surfaces within the lunate region or acetabular rim, indicating physiologic positioning of the hip joint. The size of the femoral head varied across participants. Thus, areal coverage was represented as percent coverage by dividing the area covered by the total area of each region.
Statistics
Upon confirming a normal distribution using a Kolmogorov-Smirnov test, percent coverage was expressed as mean ± standard deviation (SD). A polynomial regression analysis was employed to fit the data with an appropriate model to clarify the relationship between coverage in each region and the PSI. To be retained in the final model, a component had to be statistically significant at the 0.05 level and account for more than 95% of the variance in percent coverage. Herein, correlation coefficients >0.8 were considered to be very strong (Landis and Koch, 1977; Uemura et al., 2018a). All statistical analyses were performed using SPSS statistical software (v.22, IBM, Armonk, NY, USA).
Results
Areal head coverage changed dynamically for the four regions, with the largest change occurring in the anterior region (29.8%, range in coverage: 11.3% – 41.1%) and the smallest in the superior region (6.5%, range in coverage: 46.8% – 53.3%) (Table 1). Coverage increased gradually as the PSI increased in the anterior region while a gradual decrease was found in the posterior region (Fig. 4a, b). When the relationship between PSI change and change in areal coverage was assessed, a linear model was adopted for the anterior, posterior, and inferior regions (r=0.995, 0.994, and 0.958, respectively; all p<0.001) (Table 2). The slope of the regression line for these regions were 0.513, −0.316, and −0.255, respectively. For the superior region, a quadratic model was adopted (r=0.995, p<0.001) (Table 2). In the superior region, a change of 6.5% (range in coverage: 46.8% – 53.3%) was found when the PSI was between −30 and 30°. Coverage increased when the PSI was altered from −30° to 5° and decreased when the PSI was larger than 5°. Only 0.9% of change (range in coverage: 52.3% – 53.2%) was found when the PSI was changed between −10° and 10°.
Table 1. Maximum and minimum areal head coverage and the corresponding pelvic sagittal inclination at which these occurred.
| Region | Min coverage* PSI at min coverage |
Max coverage* PSI at max coverage |
Change (max coverage - min coverage) |
|---|---|---|---|
| Anterior | 11.3% −30° |
41.1% 30° |
29.7% |
| Superior | 46.8% −30° |
53.3% 5° |
6.5% |
| Posterior | 40.2% 30° |
59.9% −30° |
19.6% |
| Inferior | 6.4% 27° |
20.5% −30° |
14.0% |
data indicate averaged head coverage of eleven subjects
Figure 4.
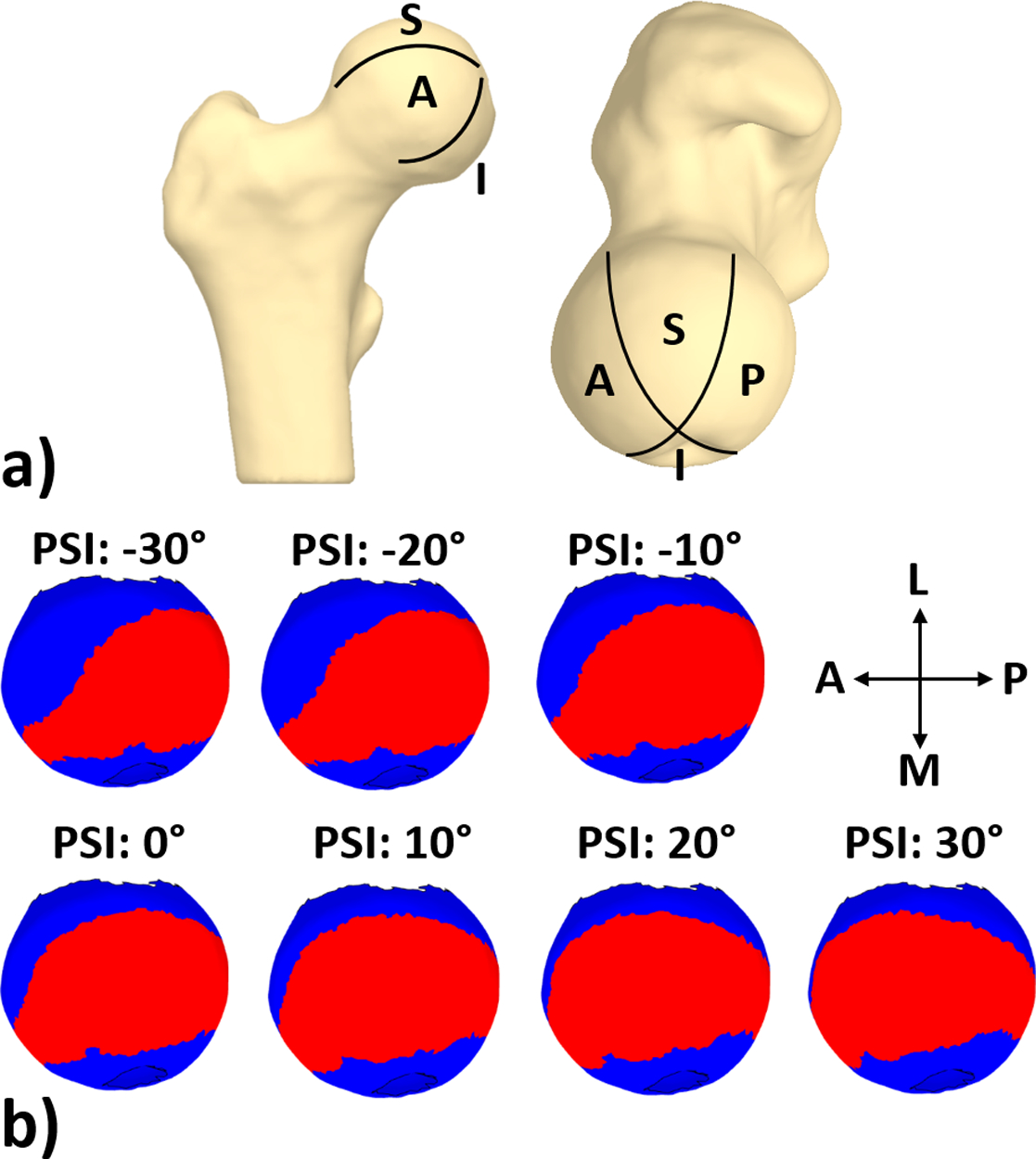
Regions of the femoral head surface covered by the lunate surface at various levels of pelvic sagittal inclination (PSI). a) Surface model of a right proximal femur in an anteroposterior view (left) and a cranial view (right) with the head surface divided into four regions. b) Femoral head surface observed from a cranial view for each PSI. The red area on the femoral head indicates the region that is covered by the lunate surface. For clarity, coverage relative to positions of the lunate surface are shown at increments of 10° of PSI between −30° and 30°. A, anterior; S, superior; P, posterior; I, inferior; M, medial; L, lateral.
Table 2. Relationship between areal head coverage and pelvic sagittal inclination; gray cells indicate a final component which accounted for more than 95% of the variance in percent coverage.
| Component | Anterior | Superior | Posterior | Inferior |
|---|---|---|---|---|
| Linear | R2=0.995 y=0.513x+24.927 |
R2=0.486 y=0.067x+51.794 |
R2=0.994 y=−0.316x+51.017 |
R2=0.958 y=−0.255x+11.762 |
| Quadratic | ΔR2=0.004 y=0.002×2+0.513x +24.293 |
ΔR2=0.504 y=−0.004×2+0.067x +53.143 |
ΔR2=0.005 y=−0.001×2-0.316x+51.472 |
ΔR2=0.037 y=0.003×2-0.255x+10.770 |
| Cubic | ΔR2=0.001 y= −6.303e-5×3+ 0.002×2+0.548x +24.293 |
ΔR2=0.008 y= 3.469e-5×3- 0.004×2+0.048x +53.143 |
ΔR2=0.001 y= −3.393e-5×3-0.001×2-0.297x +51.472 |
ΔR2=0.005 y=7.406e-5×3 +0.003×2-0.296x +10.770 |
All p<0.001.
ΔR2: R square change from the previous component.
Discussion
Femoral head coverage is an important factor used in the diagnosis of hip pathology and planning of surgical procedures. Several studies have quantified how the PSI is altered when the posture changes and reported that the PSI would be smaller in the standing position than supine (Pierrepont et al., 2017; Uemura et al., 2017). However, previous research has not examined how femoral head coverage changes. We found a significant strong positive linear regression between anterior femoral head coverage and the PSI, and a significant strong negative linear regression between the posterior head coverage and the PSI. Thus, our hypothesis that changes in regional femoral head coverage could be predicted from the change in the PSI was confirmed. Our data indicate that the change in regional head coverage can be estimated by the change in the PSI, and thus, the clinical importance of previous reports that measured the PSI in several postures was also confirmed.
Previous computational studies have quantified the relationship between the PSI and cup alignment in total hip arthroplasty (THA). Specifically, studies reported that 1° of change in PSI leads to a change in functional cup anteversion angle (i.e. radiographic anteversion angle (Murray, 1993)) of 0.6°−0.7° (Lembeck et al., 2005; Babisch et al., 2008). These reports support the clinical importance of studies that quantified the PSI in several postures for participants scheduled for THA (Pierrepont et al., 2017; Uemura et al., 2017). On the other hand, the relationship between the PSI and head coverage has not been assessed in patients with FAIS and DDH, making the clinical importance of reports that quantified PSI for these patient groups less certain (Pullen et al., 2014; Fukushima et al., 2018). Previously, studies measured how the change in PSI alters the 2-D measurements of coverage (Henebry and Gaskill, 2013; Ross et al., 2014). For example, one study reported that the LCEA increases 11.7° when PSI increases 15° and decreases 7.0° when PSI decreases 15° (Henebry and Gaskill, 2013). This suggests a diagnosis of DDH based on the LCEA could change as the PSI changes, yet the assessment was made by manual measurements done for every 5° of PSI which may have some inherent measurement error. In this study, a detailed analysis that directly quantified the relationship between coverage and PSI in single degree increments was performed using CT images and computer modelling to eliminate measurement errors inherent with manual, 2-D radiographic measurements.
Herein, we found a linear correlation between the PSI and the 3-D coverage in the anterior and posterior regions. As the slope of the regression model for these regions was 0.513 (anterior) and −0.316 (posterior), it is expected that coverage change in these regions can be calculated from the change in the PSI. For example, if the PSI changes 10° (i.e. 10° of anterior tilt), researchers can anticipate that coverage in the anterior region would increase ~5% and decrease ~3% in the posterior region. For the superior region, coverage increased when the PSI was altered from −30° to 5° and decreased when the PSI was larger than 5°. Interestingly, the raw change in percent coverage was only 0.9% when the PSI ranged between −10° and 10°. As the majority of PSI in the supine and standing position is within −10° and 10° (Uemura et al., 2017), it can be assumed that postural change only has a small effect on the coverage in the superior region and suggests that CT images (i.e. supine position) can be used to predict the superior coverage in the standing position. While this finding may be contrary to previous studies that reported a large change in PSI leading to hip osteoarthritis (Uemura et al., 2017) and dislocation of THA after spine surgery (Sultan et al., 2018), it indicates the effect and importance of anterior coverage on such complications. Collectively, our results indicate that change in regional coverage can be assumed by understanding the change in the PSI and confirmed the clinical importance of previous studies that quantified PSI in several postures for participants with FAIS and DDH. Recently, one study found a small change in PSI in the standing position following peri-acetabular osteotomy as the PSI in supine and standing positions varied (Tani et al., 2019). The authors suggested that the PSI in the standing position should be referenced when developing surgical plans for peri-acetabular osteotomy, which can be supported by our findings that PSI affects head coverage, especially in the anterior region. Further, our findings indicate that 3-D surgical planning of peri-acetabular osteotomy based on CT images may require adjustment of PSI as CT images are acquired in the supine position. However, it is important to note that the analysis herein was based on asymptomatic, morphologically normal subjects. Results could change if patients with FAIS, DDH, and acetabular retroversion were included as these patients often present with hips that are irregular in shape (Harris et al., 2013; Nepple et al., 2017; Gaffney et al., 2019). Future research should clarify the relationship between regional coverage and the PSI. In addition, it would be clinically valuable to develop understanding of the relationship between PSI and hip joint stresses and strains; mechanics could be predicted from patient-specific finite element models that alter PSI.
Limitations
There are some limitations to this study. First, the number of subjects included was relatively small. However, our sample size was comparable to previous reports on coverage (Henebry and Gaskill, 2013). Second, soft tissue such as labrum or cartilage was not included in the analysis of coverage. However, our experiment was consistent with the evaluation of coverage made in a clinical setting, which considers only the bony anatomy. Third, only changes in head coverage from a standing position were examined. While previous studies have reported that PSI in the standing position is generally within the range evaluated in our study (Pierrepont et al., 2017; Uemura et al., 2017), it should be noted that the relationship between PSI and head coverage may not follow the linear trends observed herein if the hip was oriented in more extreme positions (e.g., that produced by end-range-of-motion clinical exams). Finally, the neutral position of the hip and the center of rotation may change in-vivo when the PSI is altered. However, we confirmed that there was no overlap between the lunate surface and the femoral head during the simulated rotations of the pelvis. Additionally, the movement of femoral head center during gait had only a small effect on total femoral head coverage in our previous report (Uemura et al., 2018b). Thus, we believe that our simulation data are clinically relevant.
Conclusions
Regional femoral coverage changed when the PSI was altered. Overall, a 1° increase in PSI resulted in an increase of 0.5% in anterior coverage and a decrease of 0.3% in posterior coverage. Our findings provide baseline data that improve our understanding the effect of PSI on femoral coverage. Future research should clarify the relationship between regional coverage and the PSI for patients with hip pathology.
Figure 5.
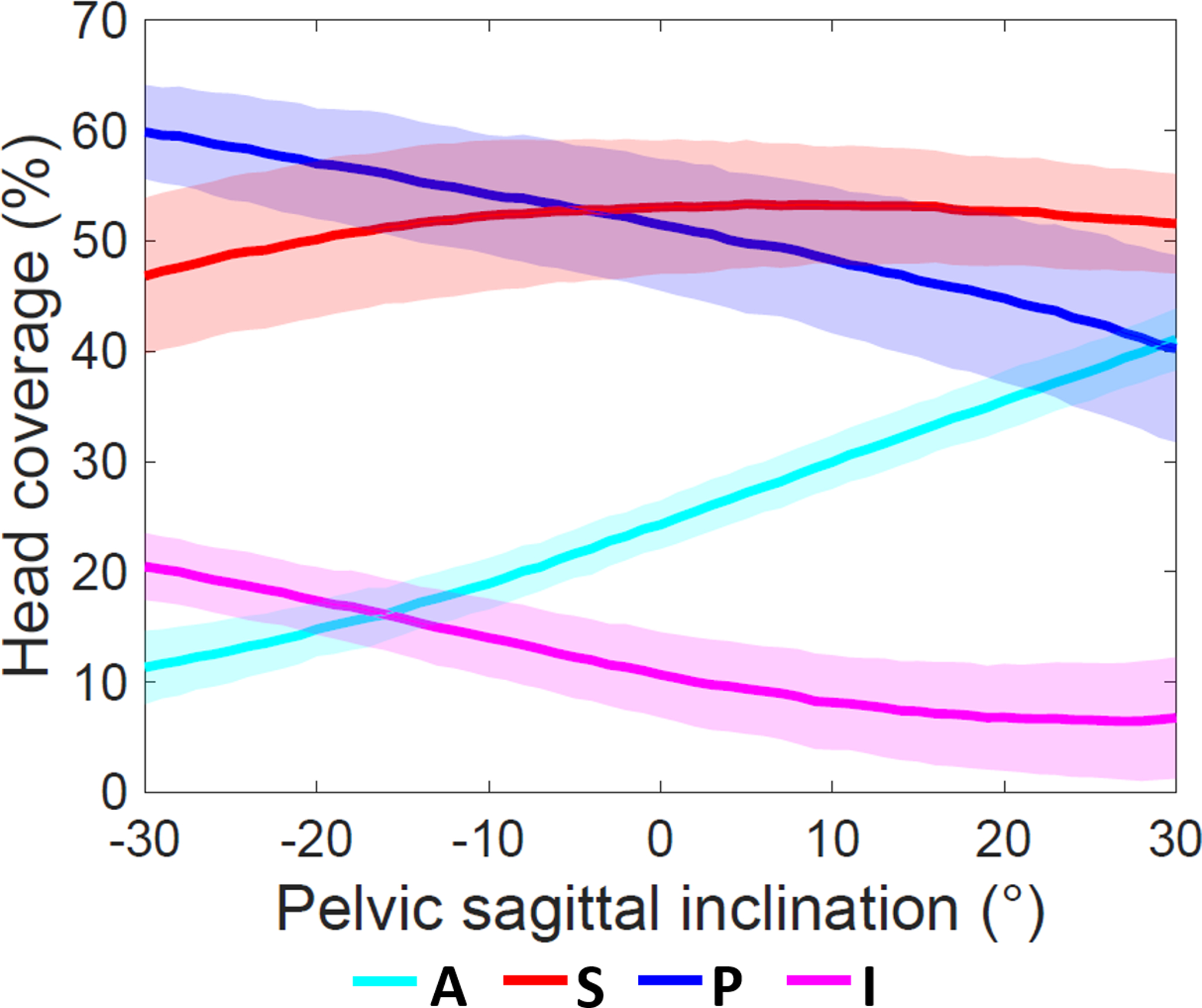
Change in regional head coverage when altering the pelvic sagittal inclination. Percent head coverage for each region is presented as mean (solid line) ± standard deviation (shaded area). A, anterior; I, inferior; P, posterior; S, superior.
Grants
Grant sponsor: National Institutes of Health (NIH); Grant#: R21-AR063844, R01-EB016701, R01-GM083925
Grant sponsor: The LS Peery Discovery Program in Musculoskeletal Restoration; Grant#: N/A
Grant sponsor: The Nakatomi Foundation; Grant#: N/A
Grant sponsor: The Nakatani Foundation for Advancement of Measuring Technologies in Biomedical Engineering; Grant#: N/A
References
- Babisch JW, Layher F, Amiot LP. 2008. The rationale for tilt-adjusted acetabular cup navigation. The Journal of bone and joint surgery American volume 90:357–365. [DOI] [PubMed] [Google Scholar]
- Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, Steger-May K, Schoenecker PL, Millis M. 2009. Radiographic evaluation of the hip has limited reliability. Clinical orthopaedics and related research 467:666–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukushima K, Miyagi M, Inoue G, Shirasawa E, Uchiyama K, Takahira N, Takaso M. 2018. Relationship between spinal sagittal alignment and acetabular coverage: a patient-matched control study. Archives of orthopaedic and trauma surgery 138:1495–1499. [DOI] [PubMed] [Google Scholar]
- Gaffney BMM, Hillen TJ, Nepple JJ, Clohisy JC, Harris MD. 2019. Statistical shape modeling of femur shape variability in female patients with hip dysplasia. Journal of orthopaedic research : official publication of the Orthopaedic Research Society 37:665–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen BJ, Harris MD, Anderson LA, Peters CL, Weiss JA, Anderson AE. 2012. Correlation between radiographic measures of acetabular morphology with 3D femoral head coverage in patients with acetabular retroversion. Acta orthopaedica 83:233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris MD, Reese SP, Peters CL, Weiss JA, Anderson AE. 2013. Three-dimensional quantification of femoral head shape in controls and patients with cam-type femoroacetabular impingement. Annals of biomedical engineering 41:1162–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henebry A, Gaskill T. 2013. The effect of pelvic tilt on radiographic markers of acetabular coverage. The American journal of sports medicine 41:2599–2603. [DOI] [PubMed] [Google Scholar]
- Kapron AL, Aoki SK, Peters CL, Maas SA, Bey MJ, Zauel R, Anderson AE. 2014. Accuracy and feasibility of dual fluoroscopy and model-based tracking to quantify in vivo hip kinematics during clinical exams. Journal of applied biomechanics 30:461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GG. 1977. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374. [PubMed] [Google Scholar]
- Lembeck B, Mueller O, Reize P, Wuelker N. 2005. Pelvic tilt makes acetabular cup navigation inaccurate. Acta orthopaedica 76:517–523. [DOI] [PubMed] [Google Scholar]
- Lequesne M, de S. 1961. [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies]. Revue du rhumatisme et des maladies osteo-articulaires 28:643–652. [PubMed] [Google Scholar]
- Maas SA, Ellis BJ, Ateshian GA, Weiss JA. 2012. FEBio: finite elements for biomechanics. Journal of biomechanical engineering 134:011005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbin B 1970. Anatomical factors in the stability of the hip joint in the newborn. The Journal of bone and joint surgery British volume 52:148–159. [PubMed] [Google Scholar]
- Murray DW. 1993. The definition and measurement of acetabular orientation. The Journal of bone and joint surgery British volume 75:228–232. [DOI] [PubMed] [Google Scholar]
- Nepple JJ, Wells J, Ross JR, Bedi A, Schoenecker PL, Clohisy JC. 2017. Three Patterns of Acetabular Deficiency Are Common in Young Adult Patients With Acetabular Dysplasia. Clinical orthopaedics and related research 475:1037–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierrepont J, Hawdon G, Miles BP, Connor BO, Bare J, Walter LR, Marel E, Solomon M, McMahon S, Shimmin AJ. 2017. Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. The bone & joint journal 99-b:184–191. [DOI] [PubMed] [Google Scholar]
- Pullen WM, Henebry A, Gaskill T. 2014. Variability of acetabular coverage between supine and weightbearing pelvic radiographs. The American journal of sports medicine 42:2643–2648. [DOI] [PubMed] [Google Scholar]
- Ross JR, Nepple JJ, Philippon MJ, Kelly BT, Larson CM, Bedi A. 2014. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. The American journal of sports medicine 42:2402–2409. [DOI] [PubMed] [Google Scholar]
- Sardana V, Philippon MJ, de Sa D, Bedi A, Ye L, Simunovic N, Ayeni OR. 2015. Revision Hip Arthroscopy Indications and Outcomes: A Systematic Review. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association 31:2047–2055. [DOI] [PubMed] [Google Scholar]
- Sultan AA, Khlopas A, Piuzzi NS, Chughtai M, Sodhi N, Mont MA. 2018. The Impact of Spino-Pelvic Alignment on Total Hip Arthroplasty Outcomes: A Critical Analysis of Current Evidence. The Journal of arthroplasty 33:1606–1616. [DOI] [PubMed] [Google Scholar]
- Tachibana T, Fujii M, Kitamura K, Nakamura T, Nakashima Y. 2019. Does Acetabular Coverage Vary Between the Supine and Standing Positions in Patients with Hip Dysplasia? Clinical orthopaedics and related research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka T, Moro T, Takatori Y, Oshima H, Ito H, Sugita N, Mitsuishi M, Tanaka S. 2018. Evaluation of the three-dimensional bony coverage before and after rotational acetabular osteotomy. International orthopaedics 42:2527–2534. [DOI] [PubMed] [Google Scholar]
- Tani T, Takao M, Uemura K, Otake Y, Hamada H, Ando W, Sato Y, Sugano N. 2019. Posterior Pelvic Tilt from Supine to Standing in Patients with Symptomatic Developmental Dysplasia of the Hip. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. [DOI] [PubMed] [Google Scholar]
- Uemura K, Atkins PR, Fiorentino NM, Anderson AE. 2018a. Hip rotation during standing and dynamic activities and the compensatory effect of femoral anteversion: An in-vivo analysis of asymptomatic young adults using three-dimensional computed tomography models and dual fluoroscopy. Gait & posture 61:276–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uemura K, Atkins PR, Maas SA, Peters CL, Anderson AE. 2018b. Three-dimensional Femoral Head Coverage in the Standing Position Represents that Measured In-vivo During Gait Clinical anatomy (New York, NY: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uemura K, Takao M, Otake Y, Koyama K, Yokota F, Hamada H, Sakai T, Sato Y, Sugano N. 2017. Change in Pelvic Sagittal Inclination From Supine to Standing Position Before Hip Arthroplasty. The Journal of arthroplasty 32:2568–2573. [DOI] [PubMed] [Google Scholar]
- Uemura K, Takao M, Otake Y, Koyama K, Yokota F, Hamada H, Sakai T, Sato Y, Sugano N. 2018c. Can Anatomic Measurements of Stem Anteversion Angle Be Considered as the Functional Anteversion Angle? The Journal of arthroplasty 33:595–600. [DOI] [PubMed] [Google Scholar]
- Uemura K, Takao M, Sakai T, Nishii T, Sugano N. 2016. The Validity of Using the Posterior Condylar Line as a Rotational Reference for the Femur. The Journal of arthroplasty 31:302–306. [DOI] [PubMed] [Google Scholar]
- Wiberg G 1953. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. The Journal of bone and joint surgery American volume 35-a:65–80. [PubMed] [Google Scholar]


