INTRODUCTION
Maintaining prosthetic fit over the day is a challenge for people with transtibial amputation. Changes in residual limb volume that occur over time alter the distribution of mechanical stress on the limb and adversely affect socket fit.1 These ongoing changes in socket fit can affect the user’s ability to wear the prosthesis, activity level, and quality of life, particularly if he or she has fragile soft tissues.
People wearing prosthetic limbs typically adjust their use of the prosthesis and their practices for accommodating limb volume changes according to how their limb feels. For example, a patient may wear the prosthesis less or even discontinue use of the prosthesis if he or she is in pain.2 A prosthesis user may also make more frequent sock adjustments if fit is not right, or he/she may doff the prosthesis more often or longer to allow fluid volume recovery and offset daily volume loss.
How prosthesis users feel about their socket fit and how they accommodate volume changes is important information for practitioners treating patients with limb loss. Practitioners traditionally use self-report information during clinical visits to educate the patient about accommodation methods, make socket adjustments, and determine when a new prosthesis is needed. However, information collected by self-report may be affected by issues such as recall, perception, and social desirability.3.4 As a result, the practitioner may have to try several different adjustments in order to correct comfort and fit problems. This iterative approach to solving socket fit issues can be time consuming, costly, and potentially detrimental to the prosthesis user’s residual limb health.
Electronic sensors have been developed to monitor prosthesis use and provide practitioners and patients with an objective record of wear.5,6 Proximity sensors mounted to the socket brim or embedded within the socket wall have been used previously to detect the presence of the residual limb within the socket. The sensors produced reliable data but consumed too much power to be practical for long-term field use. The purpose of this study was to extend from prior work and develop a portable sensor that measured when the prostheses was donned and doffed and that was capable of long-term (i.e., 2-wk) monitoring. We tested hypotheses that there would be no significant differences between self-report and electronically recorded start of day, end of day, and day durations, and that weekly prosthesis use would differ from weekend prosthesis use among people with transtibial amputation. We also characterized the frequency of socket releases and their durations, as well as doff durations for sock changes using the electronic sensor. From self-report data, we characterized start-of-day sock thicknesses and frequency of sock changes.
METHODS
Participant inclusion/exclusion criteria
Volunteers with lower-limb loss were recruited using study flyers posted in local prosthetic clinics from 01/2016 to 12/2016. Interested individuals contacted research staff by phone to obtain information about the study. Interested volunteers were screened for eligibility, and if they met inclusion criteria were scheduled for their initial visit. Volunteers were included if they had a transtibial amputation at least one year prior, an activity classification (K-level) of 2 or higher, used a prosthetic limb with an elastomeric liner at least 4 hours/day, and stated that they routinely (i.e., at least once per week) used prosthetic socks to accommodate daily limb volume changes. Participants were required to be free of residual limb skin breakdown. If presenting with skin issues at enrollment, the volunteer was referred to his or her regular practitioner for care and was reconsidered for enrollment once free of skin issues for at least a 2-week period. Exclusion criteria were regular use of an assistive device (e.g., cane), elevated vacuum, or an adjustable socket system (e.g., RevoFit and LIM sockets). Socket release practices using elevated vacuum or an adjustable socket differ from those observed with a traditional prosthesis. All test procedures were approved by an institutional review board. Informed consent was obtained before any study procedures were initiated. Participant selection criteria, including determination of K-level, were verified by the study prosthetist. K-level was determined using the Medicare ambulation definition and observed physical ability.
Instrumentation
The instrumentation to measure socket use consisted of three parts: a low-profile sensor, termed the WAFER, mounted inside the user’s socket; a cloth target affixed to the outside of the participant’s liner; and an electronics enclosure strapped to the lateral aspect of the user’s socket (Figure 1A,B, Figure 2B). Components within each part of the system are listed in Table 1. The WAFER was an inductive antenna and capacitor affixed to a thin polymer shell (Figure 2A). The inductive antenna was custom designed and fabricated using flex-circuit techniques, and the polymer shell was made using additive manufacturing techniques (Objet 30PRO, Stratasys, Eden Prairie, Minnesota). A surface mount thermistor was used for thermal compensation. The cloth target was a conductive metallized nylon fabric coated with a stretchable silver conductor paste and a stretchable protective encapsulant. The target was adhered to the posterior aspect of the prosthetic liner using adhesive (Figure 1B).
FIGURE 1A,B.
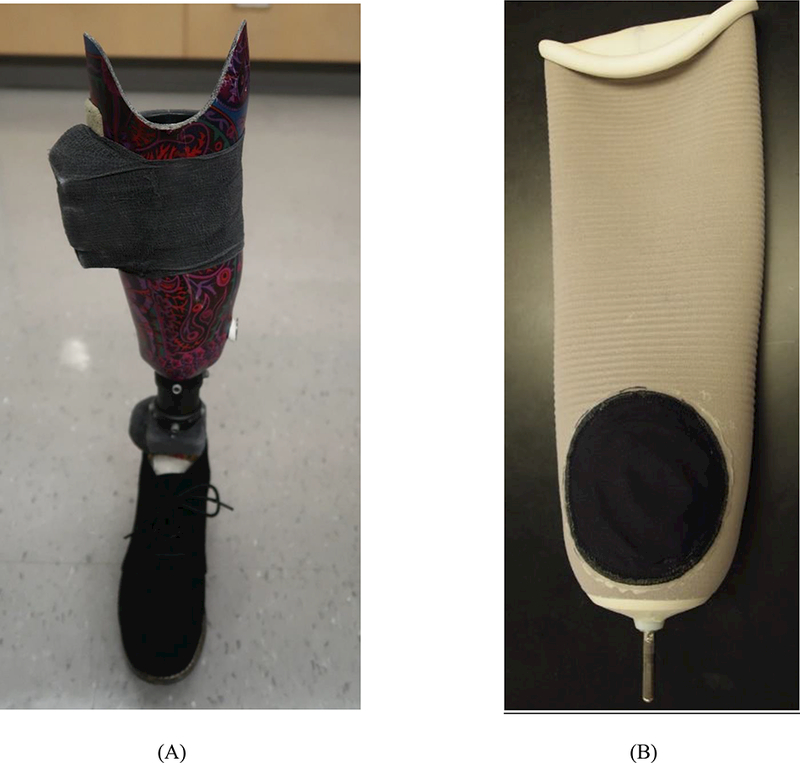
Instrumented socket and liner. (A) Socket instrumented with the WAFER and electronics enclosure ready for two weeks of field data collection. (B) Prosthetic liner with conductive target affixed.
FIGURE 2A,B.
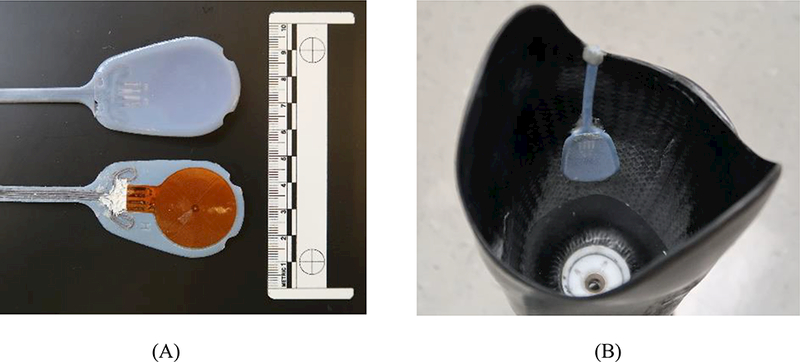
WAFER sensor. (A) The WAFER antenna, thermistor, capacitor, and lead wires were affixed to the back surface of the plastic shell (lower part of image). The inside surface of the shell (upper part of image) faced the liner. (B) Top-view of socket showing WAFER sensor positioned within a socket.
TABLE 1.
Components of the electronic monitoring system.
| Part | Component | Details |
|---|---|---|
| WAFER | Inductive antenna | 30.5 mm diameter |
| Capacitor | 470 pF | |
| Polymer shell | 1.3-mm thickness, flexible, VeroBlue FullCure 840, Stratasys, Eden Prairie, Minnesota | |
| Thermistor | 10 kΩ, 0.1°C resolution | |
| Cloth target | Metalized nylon fabric | 10-cm diameter, Zell, Shieldex by Statex, Palmyra, New York |
| Silver conductive paste | PE873, Dupont, Research Triangle Park, North Carolina | |
| Encapsulant | PE773, Dupont | |
| Adhesive | E600 Permanent Craft Adhesive, Eclectic Products Incorportated, Eugene, Oregon | |
| Electronics enclosure | Inductive sensing chip | LDC1614, Texas Instruments, Dallas, Texas |
| A-D converter | AD7173–8, Analog Devices, Norwood, Massachusetts | |
| Real time clock | DS1374U, Maxim Integrated, San Jose, California | |
| SD card | MB-MP32DA/AM, Samsung, Ridgefield Park, New Jersey | |
| Battery | Adafruit, New York City, New York | |
| Attachment to prosthesis | Double-sided tape | FastCap, Ferndale, Washington |
| Epoxy | FabTech Systems, Everett, Washington | |
| Polyimide tape | Kapton, Torrance, California | |
| Fastening strap | Velcro USA Inc., Manchester, New Hampshire | |
| Vetrap | 3M, St. Paul, Minnesota |
Components within the electronics enclosure powered the WAFER and stored collected data. When powered, the antenna and circuitry within the WAFER sensor served as an LC tank oscillator, creating a local inductive field. When the conductive target was brought near the antenna, eddy currents were induced in the conductive target which reduced the oscillation frequency, and that change in frequency was detected by the inductive sensing chip in the electronics enclosure. The signal was thus a very sensitive measure of the distance between the conductive target and antenna, i.e., distances between the liner and socket. The sensor was calibrated using a bench test apparatus that positioned targets at known distances (0.0 to 30.0 mm, 0.5 mm increments) from the WAFER.6 A thermal compensation curve (temperature vs. WAFER output) was created by placing a WAFER on a flat piece of carbon fiber (socket material), and then heating it in an oven to 50° C while collecting WAFER and temperature data.
Protocol
Each participant came to the lab for an initial visit, where the study was explained and informed consent was obtained. The research practitioner inspected the participant’s residual limb to ensure inclusion criteria were met, obtained general health and demographic information, fit the participant with a duplicate of his or her normal elastomeric prosthetic liner, and provided the participant with four new prosthetic socks (CoolMax, Royal Knit, Lee’s Summit, Missouri). Extra socks were provided if needed. Provided socks were labelled (A – 1 ply, B – 1 ply, C – 3 ply, and D – 5 ply) to help participants log which socks were used each day. Participants were instructed to wear only the liner and socks provided for the study and to notify study staff of any deviations from these instructions.
After using the duplicate liner and study socks for 2 weeks, the participant returned to the lab for the prosthesis to be instrumented. The WAFER was placed inside the socket in the popliteal space between the hamstring tendon insertions, just lateral of midline. It was important to place the WAFER on an inward-sloped portion of the socket (when viewing the socket form above) such that it bore weight when the participant stood or walked. If the WAFER was placed on an outward-sloped area then it might lose contact during standing, making it difficult to distinguish a donned from a doffed socket and resulting in underestimation of socket use. The participant was provided with a charger for the electronics enclosure and instructed how to use it, and was asked to demonstrate plugging in and unplugging the charger properly before leaving the lab. The participant was asked to charge the WAFER nightly during the 2-week study.
The posterior lateral region of the participant’s elastomeric liner was covered with the conductive target (Figure 1B). The center of the target was placed so that it aligned with the center of the WAFER sensor in the socket when the participant wore the prosthesis and stood with equal weight-bearing. Prosthesis weight bearing was measured using a scale mounting flush with the standing surface. The bottom edge of the target was placed just above the umbrella on liners with locking pins to avoid interference with normal donning procedures.
The WAFER and wires were secured to the socket with double-sided tape and small dabs of epoxy. The wires on the exterior of the socket were covered with polyimide tape. A 2.0 cm thick piece of foam was attached to the back of the electronics enclosure, and the enclosure was secured to the socket with a strap. Once functionality was confirmed, the enclosure was secured with several wraps of Vetrap, taking care not to cover the charging port. Participants were instructed how to align the target on the liner with the WAFER while donning, and asked to demonstrate this procedure to the researchers. If the liner did not have external markings, the liner was marked with permanent marker to aid in proper orientation of the target during donning.
Thicknesses of socks (socks A-D noted above) worn by the participant for the past 2 weeks were measured under stance phase walking conditions (101.2 kPa) using a custom instrument developed previously.7 A log to record daily prosthesis donning times, prosthesis doffing times, and sock changes was provided to the participant, 8 and verbal and written instructions were given for how to complete the log. Participants were asked to record in the log the time and sock ply when they first put on their prosthesis during the day and the time and sock ply when they took it off to sleep at night. In addition they were asked to record times and sock plies when they removed the socket to add or remove socks. Additional space was provided to record unusual activities or events. The participant was instructed to return to the lab after 2 weeks.
At the third visit, the log was collected, the instrumentation on the prosthesis was removed, and the data were downloaded from the electronics enclosure. The participant was returned to his or her normal liner and socks. A post-study interview was conducted to ask the participant about any concerns or issues they had wearing the instrument. Participants were then discharged from the study.
Data analysis
After downloading the data, we used the thermal compensation curve to correct WAFER data for thermal drift. The data were then parsed into 24-hour days (12 midnight to next 12 midnight). The first and last days, which were less than 24 hours, were not included in subsequent analyses.
A MATLAB script (Mathworks, Natick, Massachusetts) was written to create figures of WAFER data vs. time and temperature vs. time to facilitate visual identification and verification of dons and doffs. Doffs were identified as sudden decreases in magnitude of measured distance (liner further from the socket) and dons as sudden increases in magnitude of measured distance (liner closer to the socket), which were distinguishable in collected data (Figure 3).
FIGURE 3.
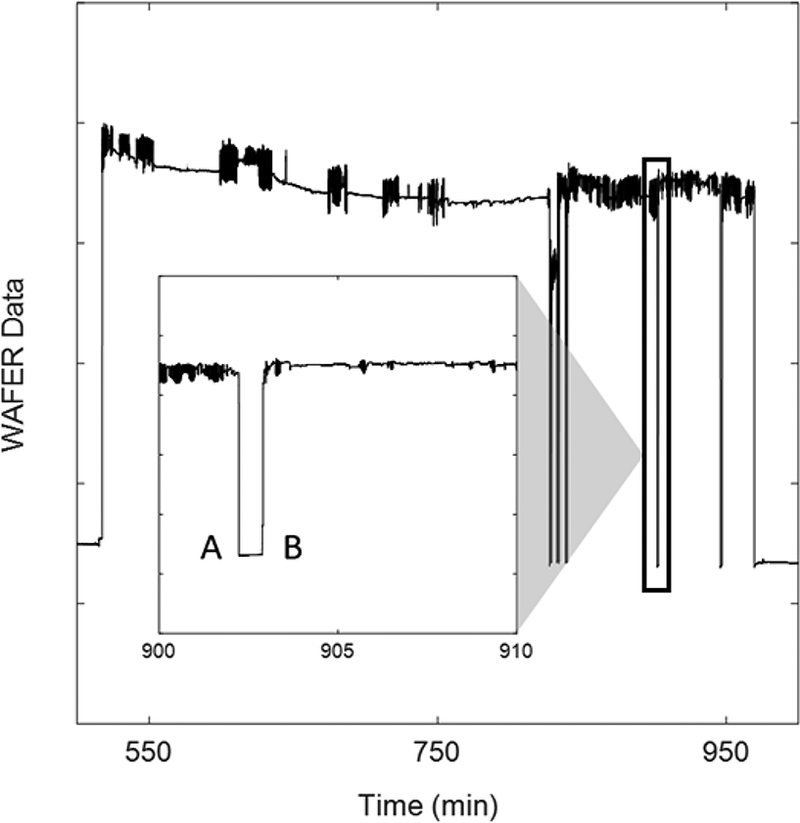
Example WAFER data illustrating multiple don-to-doff and doff-to-don transitions. A=transition to doff. B=transition to don. A don-to-doff and doff-to-don occurring between minutes 902 and 903, is magnified in the inset box. The transitions are clearly visible. Y-axis is in proximity counts with 1.0E6 counts between adjacent tick marks.
The start and end of each day were determined using an objective ruleset intended to capture meaningful socket usage time. The start time of socket use for each day was chosen as the beginning of the first don that was greater than 30 minutes in duration, or was greater than 10 minutes in duration with the next doff less than 1 hour in length (the participant was not just getting up briefly and then returning to prolonged sleep/inactivity). The end time of socket use for each day was chosen as the doff that ensured the elapsed time since the start of socket use for the day met all of the following criteria: included all 20 minute or longer dons since the start time; included every 1 hour window in which 2 dons occurred; and was at the outset of a doff lasting at least 60 minutes (ensuring the participant doffed for a significant amount of time to end the day). If these criteria were not met during a given day due to prolonged socket use, the first doff of the next day that satisfied the third criteria (was at least 60 minutes in duration) was used as the end of the day. Within each day of socket use, the following metrics were calculated: day duration, time that each doff occurred, duration of each doff, total number of doffs, daily donned prosthesis time, and daily doffed prosthesis time. Twenty-four-hour time charts were created to summarize collected data as shown in Figure 4.
FIGURE 4.
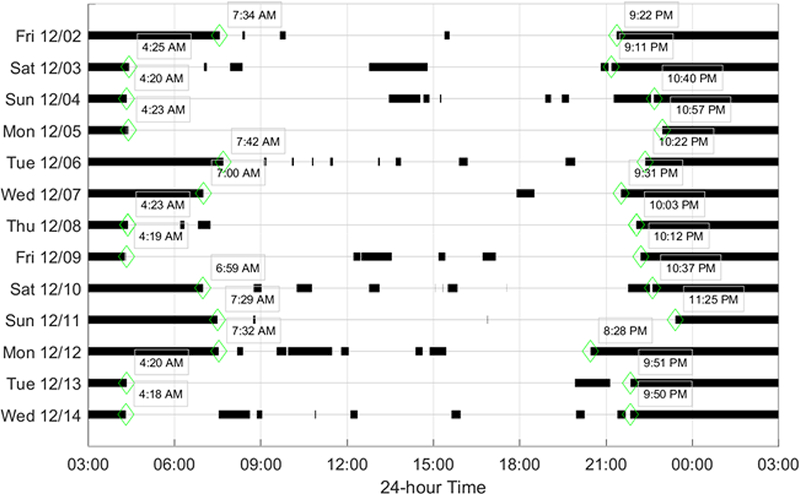
Example of doff data from two weeks of field monitoring. Doffs are shown with black lines. Green diamonds and adjacent time of day numbers indicate beginning-of-day and end-of-day times.
Self-reported prosthesis use data from participants’ logs were transcribed and added to the 24-hour time charts. In instances where participants’ self-report data were contradictory, reasonable inferences were made about socket usage activities. For example, if a participant wrote that he or she ended the day at 10 PM but also noted that he or she doffed the socket that day at 2 PM due to soreness, and the WAFER data showed the socket as being doffed from 2 PM until the next day, the self-reported end of day was revised to 2 PM. The differences between all self-reported start (and end) of day times and their corresponding WAFER start (and end) of day times were calculated in minutes. Similarly, differences in minutes between all sock change reports and their nearest WAFER doff points were calculated. Sock change doff metrics – time of occurrence, and duration – were calculated only for reported sock changes that had a WAFER-detected doff point within 1 hour of occurrence; sock changes reported outside the 1 hour range were determined to be poorly recalled time estimates of sock change and were not included in sock change doff metric calculations.
Normality of all variables was assessed using histograms, quartile-quartile plots, and Shapiro-Wilk tests. Related samples were compared using Wilcoxon signed-rank tests due to the non-normal distribution of most data. Statistical analyses were performed in SPSS Statistics 19 (IBM, Armonk, New York).
RESULTS
Participant characteristics
Twenty-six people with transtibial amputation participated in this study, but only 21 were included in analysis because of instrumentation performance issues. The most common issue was forgetting to recharge the unit (Table 2). Most participants were male (76.2%), middle-age (median of 57.0 years, IQR of 43.0–67.5 years), established prosthesis users (median of 15.6 years post-amputation, IQR of 7.9–31.7 years), unlimited community ambulators (85.7% K-3), and used a PTB prosthesis (81.0%) with lock-and-pin suspension (81.0%) (TABLE 3A,B).
TABLE 2.
Reasons for incomplete or unusable WAFER data.
| Issue | Total Occurrences | No. of Occurrences (Partic. No.) | How Handled in Analysis |
|---|---|---|---|
| Participant did not recharge
the system |
6 | 3 (NA) | Data not included |
| 1 (#11) | Restart | ||
| 1 (#13) | Data for 8 days included | ||
| 1 (#9) | Data for 10 days included | ||
| Participant did not align the
liner target properly with the WAFER sensor |
1 | 1 (NA) | Data not included |
| Electronics hardware failed | 2 | 1 (NA) | Data not included |
| 1 (#10) | Restart | ||
| Electronics enclosure
considered unsightly or socially unacceptable by participant |
2 | 1 (#1) | Wore pants |
| 1 (#6) | Wore alternate prosthesis (1 day) | ||
| Signal degradation late in testing | 3 | 2 (#14,#17) | Data for 11 days included |
| 1 (#4) | Data for 12 days included |
Partic. No. = participant number
NA = not applicable
TABLE 3A.
Participant characteristics.
| Partic. No. | Gender | Age (y) |
BMI (kg/m2) |
Reason for Amput. | Time since Amput. (y) |
Residual Limb Length (cm) |
Mid-Limb Circumference (cm) |
K-Level | Co-Morbidities, Medications,
and General Health Notes |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 35 | 45.5 | trauma | 31 | 16 | 32.4 | 3 | no co-morbidities |
| 2 | M | 56 | 30.6 | trauma | 30 | 10 | 34.8 | 3 | chronic pain, phantom pain meds |
| 3 | M | 31 | 34.6 | trauma | 11 | 18 | 32.6 | 3 | smoker |
| 4 | M | 67 | 25.4 | vascular | 16 | 14 | 31.4 | 2 | Type 2 DM |
| 5 | M | 52 | 30.6 | trauma | 21 | 17 | 30.5 | 3 | smoker, recreational drug use |
| 6 | F | 38 | 27.9 | trauma | 15 | 16 | 26.2 | 3 | no co-morbidities |
| 7 | M | 46 | 29.3 | vascular | 4 | 15 | 26.5 | 3 | DM, HTN |
| 8 | M | 62 | 30.7 | trauma | 16 | 17 | 29.2 | 3 | no co-morbidities |
| 9 | M | 78 | 25.9 | trauma | 42 | 18 | 28.4 | 3 | high cholesterol |
| 10 | M | 75 | 26.1 | trauma | 56 | 18 | 28.6 | 3 | poor balance, antibiotics for allergies |
| 11 | M | 56 | 22.4 | trauma | 33 | 19 | 26.1 | 3 | no co-morbidities |
| 12 | M | 35 | 33.5 | trauma | 8 | 14 | 31.1 | 3 | smoker, antidepressants, bipolar psychiatric meds |
| 13 | F | 60 | 37.4 | trauma | 11 | 17 | 31.4 | 2 | L5-S1 spinal injury |
| 14 | M | 74 | 27.1 | trauma | 46 | 12 | 34.2 | 3 | HTN |
| 15 | M | 61 | 27.9 | vascular | 8 | 13 | 30.2 | 3 | DM, neuropathy, cardiac stent, poor balance |
| 16 | M | 68 | 34.5 | trauma | 49 | 11 | 28.5 | 3 | DM, RA, HepB |
| 17 | F | 76 | 21.8 | congenital | 10 | 12 | 24.4 | 3 | congenital, ankle replacement failure, RA, HTN |
| 18 | F | 68 | 26.3 | vascular | 1 | 11 | 29.3 | 3 | vascular - blood clot |
| 19 | M | 45 | 27.4 | trauma | 2 | 15 | 31.1 | 4 | no co-morbidities |
| 20 | M | 42 | 28.8 | trauma | 4 | 13 | 31.8 | 3 | smoker |
| 21 | M | 46 | 25.4 | trauma | 30 | 17 | 26.9 | 3 | no co-morbidities |
Partic. No. = participant number
BMI = body mass index
Amput.= amputation
M/F = male/female
DM= diabetes mellitus
HTN= hypertension (high blood pressure)
RA= rheumatoid arthritis
HepB= hepatitis B
TABLE 3B.
Prosthesis characteristics.
| Partic. No. | Foot | Suspension | Liner | Type of Socket | Assistive Devices |
|---|---|---|---|---|---|
| 1 | Freedom Innovations Runway | Lock/pin | WillowWood Alpha Classic | PTB | |
| 2 | Össur Vari-Flex | Lock/pin | WillowWood Alpha Classic | PTB | occasional WC use in morning |
| 3 | Freedom Innovations Renegade | Lock/pin | Ossur Iceross STM | PTB | |
| 4 | Össur Sensation | Sleeve | WillowWood Alpha Classic | PTB | cane, WC in challenging environments |
| 5 | Freedom Innovations Renegade | REVO | OttoBockAnatomic 3D liner | PTB | |
| 6 | Össur Cheetah Xplore | Lock/pin | Iceross Sport | PTB | |
| 7 | unknown | Lock/pin | WillowWood Alpha Silicone | PTB | |
| 8 | Otto Bock Triton | Lock/pin | WillowWoodAlphaHybrid | TSB/PTB hybrid | |
| 9 | Freedom Innovation Renegade | Lock/pin | Iceros Synergy, Wave 18 | TSB/PTB hybrid | |
| 10 | Otto Bock Axtion | Suction | WillowWood Cushion | TSB | forearm crutches on challenging terrain |
| 11 | Össur Cheetah | Lock/pin | Iceross Dermo | PTB | |
| 12 | Össur Vari-Flex XC Rotate | Lock/pin | Iceross Synergy Wave | PTB | |
| 13 | Freedom Innovations Senator | Strap | Iceross Synergy Wave | PTB, SCSP | |
| 14 | Ossur Vari-Flex | Lock/pin | WillowWood Alpha Silicone | PTB | |
| 15 | Ability Dynamics RUSH | Lock/pin | ALPS 6 mm | PTB | |
| 16 | Trulife Seattle | Lock/pin | WillowWood Alha Hybrid Custom | PTB | |
| 17 | Trulife Seattle | Lock/pin | Ossur Dermo Uniform | PTB | occasional cane, occasional WC use |
| 18 | Össur Vari-Flex | Lock/pin | Iceross Comfort | PTB | cane, occasional WC use in morning |
| 19 | Freedom Innovations Renegade | Lock/pin | WillowWood Alpha Classic | PTB | |
| 20 | Össur Cheetah modified | Lock/pin | Iceross Synergy Wave | TSB | |
| 21 | Mica Genesis | Lock/pin | WillowWood Alpha Hybrid | PTB |
Partic. No. = participant number
WC= wheelchair
PTB= patellar tendon bearing
SCSP= supracondylar suspension
TSB= total surface bearing
Instrumentation performance
Of the 21 participants, data were collected for the intended 13-day period or longer on 16 of them. Five participants had shorter than 13-day test periods (8 to 12 days) because they forgot to plug in the unit during the second week of testing or because of various instrumentation issues (Table 2).
Participant feedback
Participants generally reported acclimating to the study liner within 3 days (range 2 hours to 3 days). Six of the participants anecdotally reported that the study liner felt less compliant than their usual liner after the conductive target had been installed. Two female participants disliked the appearance of the instrumentation enclosure – one compared it to a GPS monitor (for parolees) and stopped wearing dresses during the study (and wore only pants), the other considered the enclosure unsightly and wore an alternate prosthesis to a formal event she attended during the study period.
Log performance
Of the 21 participants without instrumentation performance issues, three had incomplete log data over the entire study period – one participant wrote down start and end times but did not document sock changes (#21) and two did not complete any of the daily logs (#1 and #3). Incomplete or inconsistent log data were intermittent for the remaining 18 participants (i.e., occurring only on certain days for certain participants), and are summarized in Table 4. In exit interviews participants indicated that they either carried their log with them, recording events as they happened throughout the day, or filled out their log at home at the beginning and end of the day.
TABLE 4.
Occasional issues: reasons for incomplete or unusable self-report data.
| Issue | Total Occurrences | Number of Occurrences (Participant IDs) | How Handled in Analysis |
|---|---|---|---|
| Log page missing |
2 | 1(#5,#19) | Did not include that day in reporting of log data or in comparison with WAFER data |
| Did not report start of day time or
socks |
1 | 1(#20) | Did not include that day in reporting of log data or in comparison with WAFER data |
| Did not report end of day time or
socks |
14 | 1(#7,#16,#19), 2(#5,#15), 3(#11), 4(#9) | Did not include that day in reporting of log data or in comparison with WAFER data |
| Did not report time of midday sock change (e.g., started day with sock A, ended day with socks AB, but no change logged in between) | 7 | 1(#4,#8,#20), 2(#5,#9) | Did not include this as a record of sock change |
| Mistakenly reported a prolonged doff as a sock change (i.e., participant interpreted doffing the prosthesis and socks then resting as a sock change and wrote “0 socks” in the log) | 5 | 1(#5,#8,#14), 2(#4) | Did not include this as a record of sock change |
| Reported a sock change and time but wrote down same thickness as before the sock change | 2 | 1(#12,#14) | Did not include this as a record of sock change |
Duration of day
We defined a “prosthesis day” as the time between prosthesis donning at the outset of the day and prosthesis doffing at the end of the day. Using WAFER data and excluding days in which the instrumented socket was not worn by the participant (four days total for all participants), we determined that participants’ prosthesis days ranged from 9.8 h to 20.1 h, with a median of 14.9 h (IQR of 13.2–15.9 h). Using self-report log data, we found that participants’ prosthesis day durations were comparable, ranging from 10.6 h to 19.5 h, with a median of 15.2 h (IQR of 14.0 to 16.3 h).
Differences between WAFER and sock log prosthesis day reporting appeared to be related to employment or socioeconomic status. Four participants (#5, 12, 18, 20), who reported inconsistent or no current employment, were responsible for 56% (27 out of 48) of the observed discrepancies greater than 60 minutes (Figure 5). One additional participant (#16) was unemployed. Agreement between WAFER and self-report log data were better for start-of-prosthesis-day times (first put on the prosthesis after waking up) than for end-of-prosthesis-day times (take off the prosthesis before going to bed), suggesting that end-of-day records were responsible for much of the difference in prosthesis day duration measured in this study (Appendix 1).
FIGURE 5.
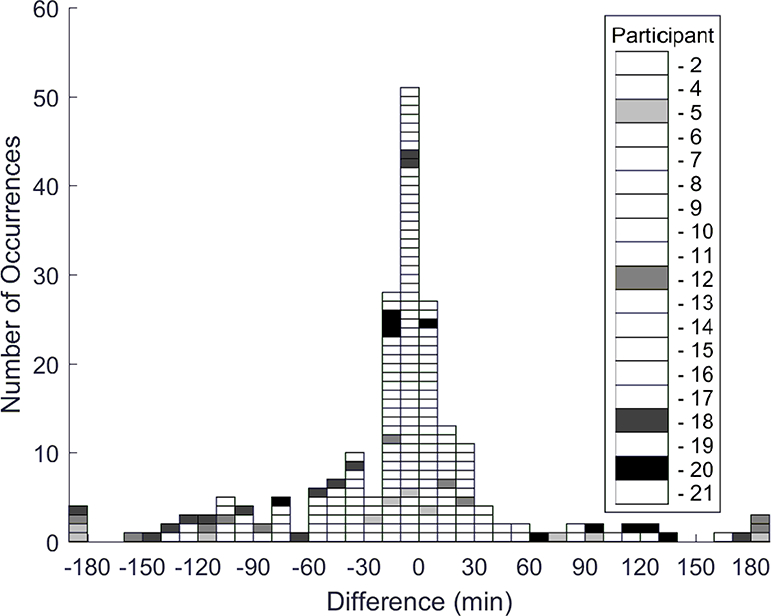
Histogram of day duration differences between WAFER data and participant log records. Four participants (#5, 12, 18, and 20) were responsible for 56% of the differences greater than 60 minutes.
Weekday and weekend data were compared. Prosthesis day durations were longer for weekdays than weekends (median difference of 1.1 h, weekday IQR of 12.7 to 16.1, weekend IQR of 13.2 to 15.5), but differences were not statistically significant (p=0.079).
Prosthesis use
Using WAFER data we calculated the time participants wore their prosthesis within each prosthesis day. Across participants, the median don time was 14.1 h/day (IQR of 12.5–14.9 h/day) and the median doff time was 0.5 h/day (IQR of 0.1–1.2 h/day). Five participants doffed for more than 1.0 h/day (#2, 3, 7, 11, 18). Daily doff percentages for all participants ranged from 0.0% to 41.3% of the participant’s prosthesis day with a median of 3.2% (IQR of 0.9–7.0%). We found no consistent differences between weekday and weekend don and doff durations (Appendix 2).
Noting that participants #2 and #18 had unusually long percentage of doff durations, we queried all participants about wheeled mobility aids. We found these two participants occasionally used a wheelchair for mobility during morning hours and were the only participants who did so.
Sock changes
Eleven of the 18 participants who completed their daily log reported changing socks at least once during the study period. The median number of sock changes per day for these 11 participants was 0.4 (IQR of 0.3–1.0) (Table 5). There were a total of 77 reported sock changes (after exclusion of misreports listed in Table 4), with 53 within plus-or-minus 60 minutes of a doff recorded by the WAFER. Of the 77 sock changes, 56 of them were sock additions and 21 were removals, with 11 of the removals being from one participant (#17). One participant (#8) was responsible for 11 of the 24 sock changes reported more than 60 minutes before or after a doff; two other participants accounted for an additional eight (four each for #4 and #5). Participants’ median difference in time between self-report sock changes and nearest electronic recorded doff was 57.1 minutes (IQR of 6.2–106.9 minutes) (Appendix 3).
TABLE 5.
Sock changes and socket releases.
| Partic. No. |
Sock Changes |
Socket Releases |
|||||
|---|---|---|---|---|---|---|---|
| Total Sock Changes Reported |
Total Sock Changes Within 1.0 h of WAFER Doff |
Median Daily Sock Changes |
Median Sock Change Doff Duration (min) |
Total Socket Releases |
Median Daily Socket Releases |
Median Socket Release Doff Duration (min) |
|
| 1 | NC | NC | NC | 0 | 0.0 | NA | |
| 2 | 1 | 1 | 0.0 | 55.5 | 89 | 5.0 | 18.2 |
| 3 | NC | NC | NC | 27 | 2.0 | 42.2 | |
| 4 | 12 | 8 | 1.0 | 7.8 | 8 | 1.0 | 4.6 |
| 5 | 4 | 1 | 0.0 | 171.5 | 7 | 0.0 | 27.7 |
| 6 | 0 | 0.0 | NA | 2 | 0.0 | 63.7 | |
| 7 | 0 | 0.0 | NA | 111 | 9.0 | 11.6 | |
| 8 | 13 | 2 | 1.0 | 12.0 | 17 | 0.0 | 11.4 |
| 9 | 4 | 1 | 0.0 | 3.3 | 23 | 1.0 | 0.3 |
| 10 | 0 | 0.0 | NA | 83 | 4.5 | 1.9 | |
| 11 | 0 | 0.0 | NA | 55 | 4.0 | 14.7 | |
| 12 | 3 | 2 | 0.0 | 75.5 | 35 | 1.0 | 3.5 |
| 13 | 0 | 0.0 | NA | 0 | 0.0 | NA | |
| 14 | 3 | 2 | 0.0 | 44.9 | 8 | 0.0 | 28.2 |
| 15 | 0 | 0.0 | NA | 1 | 0.5 | 80.6 | |
| 16 | 0 | 0.0 | NA | 10 | 0.0 | 7.2 | |
| 17 | 17 | 17 | 1.0 | 1.4 | 38 | 3.0 | 1.1 |
| 18 | 12 | 12 | 1.0 | 12.5 | 77 | 5.0 | 30.6 |
| 19 | 2 | 2 | 0.0 | 1.0 | 6 | 0.5 | 8.7 |
| 20 | 6 | 5 | 0.5 | 0.6 | 7 | 0.0 | 5.7 |
| 21 | NC | NC | NC | 21 | 1.0 | 11.7 | |
Partic. No. = participant number
STD = standard deviation
NC = noncompliant in filling out sock long
NA = not applicable
When we plotted doff durations for sock changes using the doff closest in time to the self-reported sock change (including only the 53 sock changes within 60 minutes of a doff as recorded by the WAFER), we found considerable variation among participants (Table 5). Median doff duration for sock changes was 14.2 minutes (IQR of 2.0–55.5 minutes).
Three participants started different days with markedly different sock thicknesses (>0.75mm difference between 2 days within the test period) (#2, 4, 12), and each of these three participants reported sock changes. Another seven participants had differences in sock thickness between days of more than 0.00 mm but less than 0.75mm (#7, 8, 9, 10, 14, 17, 20). Two of those seven did not report making sock changes during the day (#7, 10). Eight participants used the same sock thickness at the outset of the day each day (#5, 6, 11, 13, 15, 16, 18, 19). Five of those eight did not report making sock changes during the day (#6, 11, 13, 15, 16).
Socket releases
We calculated the number of doffs each participant made per day that were not for sock changes, and termed these “socket releases.”9 All but two participants (#1, 13) conducted socket releases at least once over the study period (Table 5). Participants most frequently conducted 1.3 socket releases/day (IQR of 0.5–3.8).
Participants’ socket release durations ranged from 4.7 minutes to 80.6 minutes with a mean of 22.4 minutes (SD=34.6 minutes, median= 10.1 minutes). 50.0% (312 of 625) of the socket releases conducted were less than 10 minutes in duration, 34.6% (216 of 625) were between 10 and 30 minutes, 5.4% (34 of 625) were between 30 and 60 minutes, and 10.1% (63 of 625) were over 60 minutes (Table 5).
We investigated at what time of day socket releases were conducted. In general, participants doffed the socket for reasons other than sock changes in the afternoon or early evening (Figure 6). Participants’ median time of a socket release was 4:04 PM (IQR of 2:20–6:18 PM) (Appendix 4).
FIGURE 6.
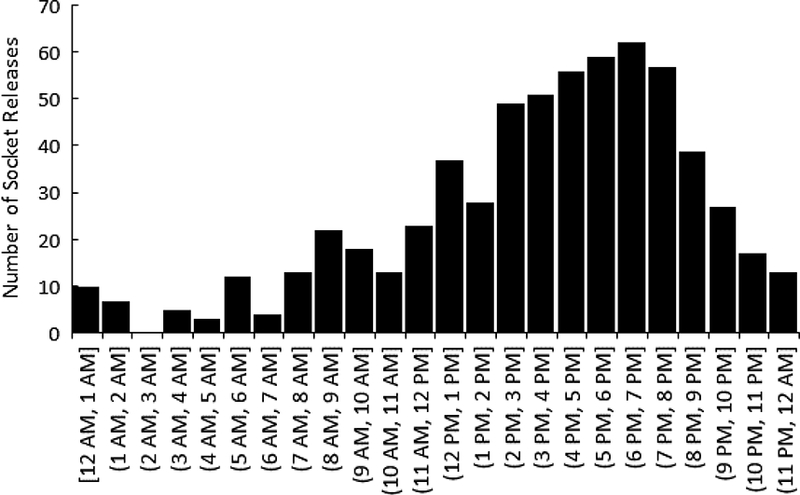
Histogram of time of day socket releases were conducted.
When we plotted number of self-reported sock changes/day vs. number of socket releases/day, we found that participants in general fell into four groups (A-D) (Figure 7). The four groups were arbitrarily defined as: (A) rarely changed socks (<1 sock change every 10 days) and rarely did socket releases (<1 release/day); (B) routinely changed socks (>1 sock change every 10 days), but rarely did socket releases; (C) rarely changed socks, but routinely did socket releases (>1 sock release/day); and (D) routinely did both sock changes and socket releases. There were a comparable number of participants in each group.
FIGURE 7.
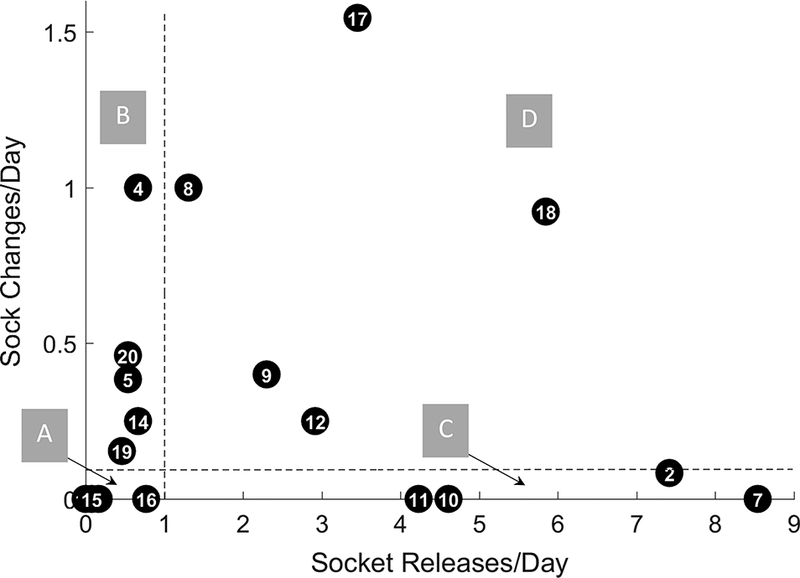
Sock changes per day v. socket releases per day. Region A contains participant #6, 13, 15, and 16. Region B contains participant #4, 5, 14, 19, and 20. Region D contains participant #8, 9, 12, 17, and 18. Region C contains participant #2, 7, 10, and 11. Participant #1, 3, and 21 omitted due to incomplete self-report information. Dashed lines delineating regions are at 0.1 sock changes/day and 1 socket release/day.
DISCUSSION
This research was directed towards evaluation of a novel electronic sensor designed to provide information about socket use and volume accommodation methods outside of clinic or laboratory settings. Results from this study demonstrated no significant differences between electronic and self-reported start-of-day times and prosthesis day durations, but significant differences for end-of-day times. The sensor has the potential to enhance patient care by providing patients and practitioners information about socket wear and residual limb volume management over extended periods of time.
Instrumentation
Most of the instrumentation performance issues in this investigation were associated with practical issues (e.g., battery life, alignment requirements for the liner target and sensor, and bulk of the electronics enclosure) that caused burden to the user, rather than electronic hardware failure. As such, the instrumentation developed for this study did not seamlessly integrate into participants’ normal routines. Key changes that need to be implemented include: reducing the need to recharge the unit daily; simplifying the need to orient the conductive target with the WAFER sensor; and improving cosmesis by reducing the size of the electronics enclosure mounted to the outside of the socket. Issues such as donning, doffing, and appearance are recognized as key factors in the design and acceptance of portable instrumentation such as ambulatory monitors. Users’ acceptance of monitors, such as the WAFER system developed in this study, is therefore likely to improve as these issues are addressed.
We attributed the observed signal degradation noted after 12 or more days in the 2-week monitoring period to mechanical breakdown of the conductive targets that were affixed to the study liners. After completion of the study, we conducted scanning electron microscopy (SEM) imaging to gain insight into physical sources of signal degradation. Results demonstrated that contaminants were deposited between adjacent fibers within the conductive fabric targets (Figure 8A), spreading the fibers apart, which may have reduced conduction and capability to form eddy currents within the fabric target responsible for generating the sensor signal. New unused conductive fabric targets showed minimal contamination (Figure 8B). Changing to a magnetic target, such as iron powder particles embedded within the liner elastomer or fabric backing, rather than using a conductive target, may help to overcome this limitation and allow for longer recording periods.
FIGURE 8A,B.
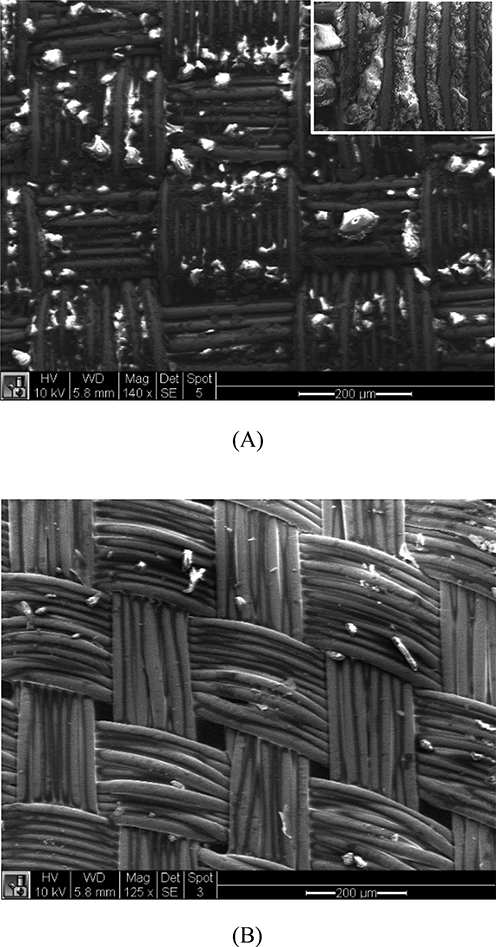
SEM images of fabric targets. (A) Used target showing debris (white). Inset illustrates debris embedded between fibers. (B) Unused target.
Lastly, the instrument developed for this study served exclusively as a prosthesis use monitoring device. Thus it did not recognize when a prosthesis user was active but not weight-bearing on his or her prosthesis, for example, using a wheelchair. Additional sensors, such as accelerometers mounted to the mobility aid, would be needed to make this distinction.
Participant report
Participant reports most closely matched WAFER data for start-of-prosthesis-day time, presumably because most participants placed the log in a location they visited as a part of their normal early day routine, e.g., on a bedside table. The log-reported end-of-prosthesis-day time was less closely matched to WAFER data. However, end-of-prosthesis-day differences may in part reflect limitations in our processing algorithm in properly selecting which late-day doff (most users had several late-day doffs) aligned with the doff that the participant considered his or her last doff of the day.
Participants who were not regularly employed may have had less routine schedules than those with full-time employment, and this may in part explain why differences in their prosthesis day duration between report and WAFER data were greater. Lack of a regular schedule may have caused participants to misplace the sock log, leave it at home, or forget to complete it. Testing on a larger group of participants may help determine if there is a noteworthy pattern in self-report accuracy of prosthesis day times that suggests investigators should consider employment status in future research.
For participants who followed the log instructions, there were still occasional (i.e., once or twice over the testing period) inconsistencies between the log and the WAFER data. It is likely that the long duration of monitoring (~2 weeks) contributed to errors in times or events noted in the log. Such issues may occur when a participant is unable to record log data in real-time and has to recall the timing of an event (e.g., a sock change) later. It may be unrealistic to expect every entry to be accurately recorded in a 2-week log. As such, future studies towards characterizing resolution of self-report measurement of prosthesis use should consider conducting validation studies using an objective sensor like the WAFER used in the present study to quantify potential measurement errors.
Modifications to the log and instructions may improve accuracy and compliance. The log used in this study was developed previously for monitoring sock use in transtibial prosthesis users,8 but has not been tested through rigorous qualitative methods such as cognitive interviewing. Cognitive interviewing is often advocated to maximize clarity, comprehension, and quality of survey items and instructions.11,12 For example, refinement of the log instructions to clarify how the user should differentiate sock changes and socket releases may improve the quality and accuracy of the data. Developing the log into a mobile application may mitigate reporting issues associated with misplacing or forgetting the paper log. As many prosthesis users are likely to carry their mobile phone with them throughout the day, a mobile application would allow users to track sock change or socket release information more readily and avoid misreporting these events based on recall. The mobile application could also prompt users to enter their data based on a practitioner- or user-selected frequency.
Data interpretation
Participants’ prosthesis use (i.e., 14.1 h/day), as recorded by the WAFER, is consistent with prosthesis users’ self-report in other studies. For example, the mean daily use of a prosthesis, as reported by a national sample of 705 transtibial prosthesis users was 12.9 h/day.13 The slightly elevated daily use measured in this study may be due to the higher percentage of trauma versus dysvascular participants in the present study (76.2% as compared to 47.9%). The lack of weekday to weekend differences in prosthesis day durations may reflect the few number of participants (6) who had consistent work schedules. Klute et al. showed significant differences in step activity between weekdays and weekends, but 9 of their 12 analyzed people were fully employed.14 Calculation of percent of the prosthesis day participants donned and doffed their prosthesis, 92.7% and 7.3% in the present study, is a novel measure that may prove useful in future research efforts.
Percentage time donned and doffed
Only 2 of the 21 participants did not doff at all during the day for the entire test period. Some clinical specialists advise that prosthesis users should gradually increase daily prosthesis use, striving for all day wear, i.e., putting on the prosthesis in the morning and taking it off in the evening, like an able-bodied person would do with shoes.15 While all-day use is convenient for the prosthesis user and may limit fit problems for patients prone to edema, in others it may facilitate limb fluid volume loss and necessitate accommodation partway through the day.16 The relatively narrow range of daily doff durations measured in the present study for most of the participants (16 of 21 participants doffed less than 60 minutes/day) sets a starting point for characterization of prosthesis users’ daily doffing frequencies and durations. It also sets a baseline for evaluation of technologies intended to eliminate doffing during the day but still facilitate limb fluid volume recovery (e.g., adjustable sockets and elevated vacuum systems).
Sock Changes
Although we sought to enroll participants who regularly used socks to accommodate residual limb volume fluctuations, only 11 of 18 of the participants who had complete sock logs made sock changes during the 2-week test period. This result is consistent with our prior study that indicated a verbal question (i.e., do you add or change socks throughout the day?) did not well characterize prosthesis users’ habitual sock use, as reported in a daily log.8 Prosthesis use data collected in the present study further challenges the notion that clinical behaviors (e.g., reports of sock use) can be accurately obtained via questions posed in a patient interview.
None of the participants followed a regular daily routine of sock addition, supporting the expectation that participants adjusted sock thickness not by an established daily schedule (set by themselves or their practitioner) but instead by how they felt. This result points to the burden put on the user to continually sense his or her prosthetic fit and decide accordingly what adjustments to make and when to make them. Future studies need to quantify to what degree this burden affects comfort and residual limb health. It may be that a means for detecting the need for accommodation and communicating it to the user reduces the burden, facilitates timely socket adjustments, enhances comfort, and improves residual limb health. A means for detecting the need for accommodation and communicating it to the user may also facilitate education about overcompensation for participants adding a sock after executing an extended doff.
We conducted an additional analysis to investigate if use of the WAFER affected start-of-day sock thickness. Three of the 18 reporting participants started their day with a much different sock thickness than other days (>0.75mm difference). We found that one of these three participants varied start-of-day sock thickness by more than 0.75mm only during the first 7 days of the study, but afterwards did not. This early adjustment may suggest that the participant may have felt the WAFER sensor in her socket and tried to accommodate its presence. The other two participants did not show this trend, and reasons for their day-to-day variability in start-of-day sock thickness remain unknown.
Socket releases
Surprisingly, almost every participant (all but #1 and #13) in the study executed socket releases, i.e., doffs during the day that were not to change socks. Further, of the 19 participants who executed socket releases, nine conducted at least 1 socket release per day while only three conducted at least 1 sock change per day. Reasons for socket releases were not recorded in the present study; thus, it is not known what percentage of socket releases were executed to improve limb comfort or manage socket fit. The two accommodation techniques, sock addition and socket release, operate on different volume adjustment principles. When a prosthesis user adds a sock, the socket’s available volume is reduced and to a lesser extent residual limb fluid volume is reduced (Figure 9A).17 When a prosthesis user executes socket release, socket volume stays the same and limb fluid volume usually increases. Some of the fluid volume is typically retained upon subsequent re-donning, provided the doff duration is long enough (Figure 9B).9 Thus, socket release may reduce peak-to-peak daily limb fluid volume change, which may be more comfortable to the person with limb loss than the alternative strategy of adding a sock.
FIGURE 9A,B.
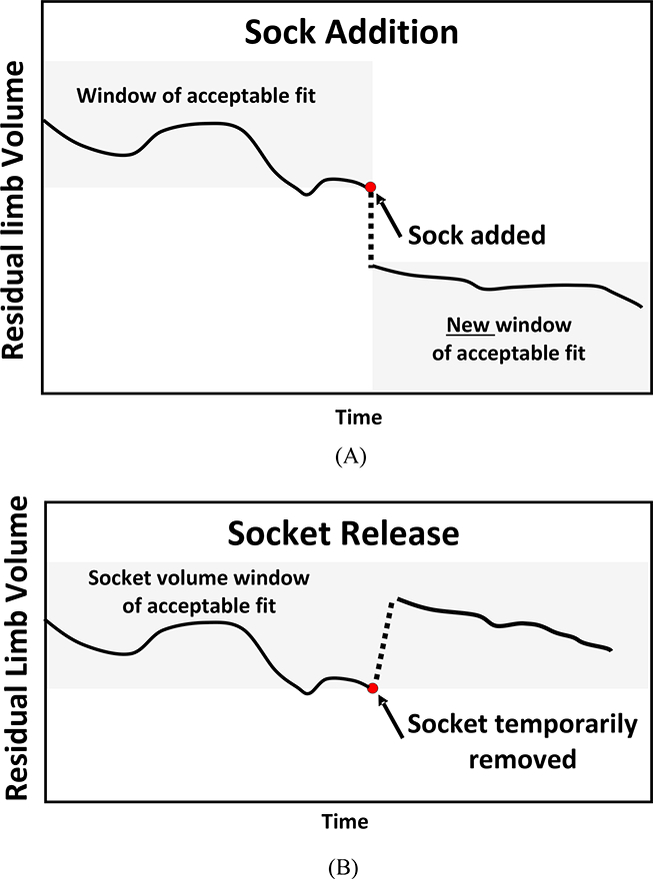
Concept diagrams illustrating residual limb fluid volume changes upon accommodation. (A) From increasing sock thickness. (B) From socket release (temporary doffing).
User classification
When we plotted sock changes/day v. socket releases/day, we found that the data were reasonably well distributed (Figure 7), suggesting that prosthesis users execute a range of strategies to maintain fit. Because we did not find consistent participant or prosthesis characteristics matched to group membership, participant decisions to add socks, execute socket releases, conduct no accommodations, or conduct a combination of sock addition and socket release may have been because of other influences. Possible factors include activity and limb volume change that day and the convenience or inconvenience (social environment) of executing accommodation at the time it was desired. We also noted that several of the individuals who participated in the present study were participants in previous research projects testing socket release in our lab9; thus their prior experience in that study may have influenced their accommodation behavior.
Future research
A next step in instrument development is to enhance sensor functionality and utility to provide additional insight for the practitioner, for example monitoring timings and durations of user activities. During the first several days of wear, the WAFER sensor well distinguished sitting, standing, and walking, in addition to donning and doffing. However, because of signal degradation problems from target deterioration as discussed above, this capability diminished after several days and only donning and doffing could be accurately differentiated. Enhancement of the sensor target using different target materials may overcome this problem and is a next step in this research effort.
A logical clinical extension of this research is to enhance the electronics hardware to communicate with a smartphone via low-power Bluetooth and provide information directly to the patient and/or practitioner.18 The WAFER could monitor patients’ prosthesis use and daily activity relative to practitioner-established recommendations, and communicate with the patient via a mobile application. The application could allow patients to set goals, track prosthesis use and activity, provide reminders to check socket fit after long periods of standing or high activity, or suggest times for socket release. Integration of other behavior change techniques, such as opportunities for social comparison, in the mobile application should also be explored to determine whether they may have a positive effect on users’ health.19 The proposed WAFER notification system could also prompt the user for real-time self-report information (e.g., socket comfort score20 ) that would complement the objective sensor data and help practitioners to better contextualize patient’s day-to-day experiences. Such a tool could also be used to help assess the validity of new self-report measures against a ground-truth reference.
Based on knowledge gained during development of the WAFER and results of this study, we expect the WAFER would initially find practical use as a temporary assessment tool to monitor patients having prosthetic fit problems for a 2–4 week period. The data could facilitate practitioner decision-making for socket modification or replacement. Once a decision was made to replace the socket, sensor antennas could be placed within the new socket wall during fabrication,6 allowing for monitoring at any time assessment may be useful. We have found that mounting the WAFER sensors within the socket wall rather than adhering them to the surface enhances their durability. Continual monitoring with data presentation via smartphone may be attractive and desirable for some prosthesis users and may facilitate understanding of events leading to socket fit problems.
CONCLUSION
The WAFER sensor in general exhibited good performance but had practical issues including limited battery life, alignment requirements for the liner target and sensor, and bulk of the electronics enclosure that should be resolved in further development. There was generally good agreement between self-report and electronic start-of-prosthesis-day times, but not as good agreement for timing of sock changes and end-of-prosthesis-day times. The developed electronic monitor may improve prosthesis use and accommodation recording for some people with limb loss. The daily prosthesis wear durations (median of 14.1 h/day), doff durations (median of 0.5 h/day), sock change frequencies (median of 0.4 changes/day), and socket release frequencies and durations (median of 1.3 releases/day, 21.8 minutes/day) serve as a starting point for characterizing socket wear and accommodation.
Supplementary Material
ACKNOWLEDGMENTS
Assistance from Jarrod LaFountaine during pilot study data collection efforts is gratefully acknowledged. This research was based on work supported by the Institute of Child Health and Human Development of the National Institutes of Health under award number R01HD060585. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Joan E Sanders, University of Washington Department of Bioengineering, Seattle WA.
Christian B Redd, University of Washington Department of Bioengineering, Seattle WA.
Brian G Larsen, University of Washington Department of Bioengineering, Seattle WA.
Andrew C Vamos, University of Washington Department of Bioengineering, Seattle WA.
Jacob T Brzostowski, University of Washington Department of Bioengineering, Seattle WA.
Brian J Hafner, University of Washington Department of Rehabilitation Medicine, Seattle WA.
Katheryn J Allyn, University of Washington Department of Bioengineering, Seattle WA.
Katrina Henrikson, University of Washington Department of Bioengineering, Seattle WA.
Jake B McLean, University of Washington Department of Bioengineering, Seattle WA.
Paul Hinrichs, University of Washington Department of Bioengineering, Seattle WA.
REFERENCES
- 1.Sanders JE, Zachariah SG, Jacobsen AK, Fergason JR. Changes in interface pressures and shear stresses over time on trans-tibial amputee subjects ambulating with prosthetic limbs: comparison of diurnal and six-month differences. J Biomech. 2005; 38(8):1566–73. [DOI] [PubMed] [Google Scholar]
- 2.Schaffalitzky E, Gallagher P, Maclachlan M, Wegener ST. Developing consensus on important factors associated with lower limb prosthetic prescription and use. Disabil Rehabil. 2012;34(24):2085–94. [DOI] [PubMed] [Google Scholar]
- 3.Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003;37(3):197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stone AA, Shiffman S. Capturing momentary, self-report data: a proposal for reporting guidelines. Ann Behav Med. 2002;24(3):236–43. [DOI] [PubMed] [Google Scholar]
- 5.Gardner DW, Redd CB, Cagle JC, Hafner BJ, Sanders JE. Monitoring prosthesis user activity and doffing using an acitivity monitor and proximity sensors. J Prosthet Orthot 2016;28(2):68–77. [Google Scholar]
- 6.Swanson EC, McLean JB, Allyn KJ, Redd CB, Sanders JE. Instrumented socket inserts for sensing interaction at the limb-socket interface: A technical note. Med Eng Phys. 2018, 51:111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cagle JC, Yu AJ, Ciol MA, Sanders JE. Amputee socks: Thickness of multiple socks. Prosthet Orthot Int. 2014; 38(5):405–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Silva K, Hafner BJ, Allyn KJ, Sanders JE. Self-reported prosthetic sock use among persons with transtibial amputation. Prosthet Orthot Int. 2014; 38(4):321–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanders JE, Hartley TL, Phillips RH, Ciol MA, Hafner BJ, Allyn KJ and Harrison DS. Does temporary socket removal affect residual limb fluid volume of trans-tibial amputees? Prosthet Orthot Int. 2016; 40(3): 320–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rueterbories J, Spaich EG, Larsen B, Andersen OK. Methods for gait event detection and analysis in ambulatory systems. Med Eng Phys. 2010;32(6):545–52. [DOI] [PubMed] [Google Scholar]
- 11.Beatty PC, Willis GB. Research synthesis: The practice of cognitive interviewing. Public Opin Q. 2007;71(2):287–311. [Google Scholar]
- 12.Bredart A, Marrel A, Abetz-Webb L, Lasch K, Acquadro C. Interviewing to develop Patient-Reported Outcome (PRO) measures for clinical research: eliciting patients’ experience. Health Qual Life Outcomes. 2014;12(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amtmann D, Morgan SJ, Kim J, Hafner BJ. Health-related profiles of people with lower limb loss. Arch Phys Med Rehabil. 2015;96(8):1474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klute GK, Berge JS, Orendurff MS, Williams RM, Czerniecki JM. Prosthetic intervention effects on activity of lower-extremity amputees. Arch Phys Med Rehabil. 2006;87(5):717–22. [DOI] [PubMed] [Google Scholar]
- 15.Carroll K, Edelstein JE. Prosthetics and Patient Management. SLACK Incorporated, 2006. ISBN 10: 1556426712 ISBN 13: 9781556426711 [Google Scholar]
- 16.Sanders JE, Cagle JC, Allyn KJ, Harrison DS, Ciol MA. How do walking, standing, and resting influence transtibial amputee residual limb fluid volume? J Rehabil Res Dev. 2014; 51(2): 201–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanders JE, Harrison DS, Allyn KJ, Myers TR, Ciol MA and Tsai EC. How do sock ply changes affect residual-limb fluid volume in people with transtibial amputation? J Rehab Res Dev. 2012; 49(2): 241–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hafner BJ, Sanders JE. Considerations for development of sensing and monitoring tools to facilitate treatment and care of persons with lower-limb loss: a review. J Rehabil Res Dev. 2014;51(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Middelweerd A, Mollee JS, van der Wal CN, Brug J, Te Velde SJ. Apps to promote physical activity among adults: a review and content analysis. Int J Behav Nutr Phys Act. 2014;11:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanspal RS, Fisher K, Nieveen R. Prosthetic socket fit comfort score. Disabil Rehabil. 2003;25(22):1278–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


