Abstract
Purpose
The guidelines for pathological evaluation of early gastric cancer (EGC) recommend wider section intervals for surgical specimens (5–7 mm) than those for endoscopically resected specimens (2–3 mm). Studies in surgically resected EGC specimens showed not negligible lymph node metastasis risks in EGCs meeting the expanded criteria for endoscopic submucosal dissection (ESD).
Materials and Methods
This retrospective study included 401 EGC lesions with an endoscopic size of ≤ 30 mm detected in 386 patients. Pathological specimens obtained by ESD or surgery were cut into 2-mm section intervals for reference. Submucosal or lymphovascular invasion (LVI) was evaluated arbitrarily in 4- or 6-mm section intervals. McNemar's tests compared the differences between submucosal and LVI.
Results
Submucosal invasion was detected in 29.2% (117/401) and LVI in 9.5% (38/401) at 2-mm interval. The submucosal invasion detection rates in 4-mm intervals decreased to 88.0% or 90.6% (both P<0.001), while the LVI detection rates decreased to 86.8% or 57.9% (P=0.025 and P<0.001, respectively). In 6-mm intervals, the submucosal and LVI detection rates decreased further to 72.7–80.3% (P<0.001 for all three sets) and 55.3–63.2% (P<0.001 for all three sets), respectively. Among 150 out-of-indication cases at 2-mm interval, 4–10 (2.7%–6.7%) at 4-mm intervals, and 10–17 (6.7%–11.3%) at 6-mm intervals were misclassified as lesions meeting the curative resection criteria due to the underestimation of submucosal or LVI.
Conclusions
After ESD, the 2-mm wide section interval was suitable for the pathological evaluation of focal submucosal or LVI. Thus, if an EGC lesion meets the expanded criteria for the ESD specimen pathological evaluation, it could be safely followed up.
Keywords: Stomach neoplasm, Endoscopic submucosal dissection, Submucosal invasion, Lymphovascular invasion
INTRODUCTION
Endoscopic resection is a standard treatment for early gastric cancer (EGC), which has minimal risk of lymph node metastasis [1,2,3]. Current endoscopic resection criteria for EGC are based on a previous study that evaluated the incidence of lymph node metastasis in a large number of surgically resected EGC specimens [4]. Endoscopic resection criteria were proposed for EGC lesions with no lymph node metastasis [4]. However, several studies suggested that lymph node metastasis risks were not negligible, especially in EGC lesions meeting the expanded criteria [5,6,7]. A meta-analysis of 12 studies including patients with EGC who underwent surgery showed that lymph node metastasis risk was significantly higher in lesions meeting the expanded criteria (relative risk, 2.54; 95% confidence interval, 1.29–5.01) than those in the absolute criteria [8]. In addition, extra-gastric recurrences have been reported after curative endoscopic resection of EGCs, especially in cases with minute submucosal invasion [9,10] or missed lymphovascular invasion (LVI) in the resected specimen [11].
Submucosal and LVI are significant risk factors associated with lymph node metastasis in EGC [4,12]. Recommended guidelines for section intervals in pathological evaluations were 5- to 7-mm intervals for surgical specimens and 2- to 3-mm intervals for endoscopic resection specimens [3,13,14]. However, the submucosal or LVI could be detected in a very focal area of the resected specimens [11,15,16]. Thus, the focal submucosal or LVI might be missed in surgically resected specimens because of wider section intervals.
In the present study, we aimed to evaluate whether the submucosal and LVI detection rates are affected by the width of the section intervals used in the pathological examination.
MATERIALS AND METHODS
Patients
This retrospective study included 414 patients with 429 EGC lesions with an estimated size of 30 mm or less as determined by diagnostic endoscopy. The EGC lesions were treated by endoscopic submucosal dissection (ESD) or surgical resection at the National Cancer Center, Korea, from April 2012 to December 2013. Patients with noninvasive carcinoma and those with tumor invasion in the proper muscle on final pathological evaluations were excluded. The baseline demographic data and tumor characteristics were obtained from the medical records of patients.
The Institutional Review Board of the National Cancer Center, Korea (IRB number: NCC2016-0060), approved this study, and the requirement for informed consent waived.
EGC Treatment
ESD was performed in patients with EGC who clinically met the clinical absolute indication criteria for endoscopic resection following the gastric cancer treatment guidelines [1,2]. EGC cases that met the clinically expanded indication, the choice of ESD vs. surgery were determined after a thorough review of the cases in multidisciplinary conferences. The ESD procedure details were as described earlier [17]. The surgical treatment included laparoscopic or robot-assisted radical gastrectomy with lymph node dissection. The extent of lymph node dissection was D1+ or more following the gastric cancer treatment guidelines [2].
Pathological evaluations
The resected EGC specimens from ESD and surgery were stretched and pinned on a flat board and fixed in 10% buffered formalin solution. The samples were sliced serially at 2-mm intervals parallel to the reference cutting line in the center of the specimen. Each 2-mm interval sections were numbered serially from the proximal to the distal end [13].
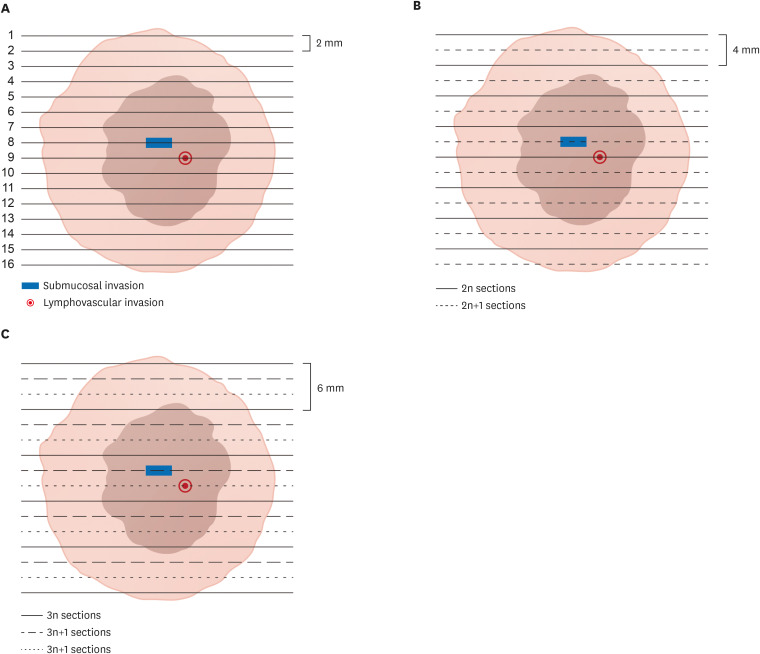
The pathological findings of the presence of submucosal and LVI in the 2-mm sections served as the reference (Fig. 1A). The 4- and 6-mm interval sections were used to evaluate detection rates in wider interval sections. The pathological findings in the 4-mm interval sections were evaluated in even (2n) or odd (2n+1) numbered sets (Fig. 1B). Evaluation of the 6-mm interval sections was performed in three sets (3n, 3n+1, or 3n+2 numbered section sets) (Fig. 1C). The results were evaluated by a pathologist specializing in gastric cancer (MC Kook). Tumor histologic types were classified following the World Health Organization classification system [18] and categorized into differentiated and undifferentiated histologic types following the gastric cancer treatment guidelines [2].
Fig. 1. Section cut and reconstruction of a resected specimen. Light brown color indicates the resected specimen, while dark brown color indicates the tumor area. (A) Reference 2-mm section interval. (B) Two 4-mm section interval sets. (C) Three 6-mm section interval sets.
Study outcomes
Primary outcome variables were differences in submucosal and LVI detection rates in the wider interval (4- and 6-mm) compared to 2-mm interval sections. Secondary outcomes were changes in final pathological curability criteria for endoscopic resection using wider intervals.
The absolute criteria were as follows: mucosal tumors, differentiated histologic type, and tumor sizes of ≤ 2-cm without ulceration, and LVI. The expanded criteria were as follows: 1) mucosal tumors, differentiated histologic type, and tumor sizes of > 2-cm without ulceration (criteria I); 2) mucosal tumors, differentiated histologic type, and tumor sizes of ≤ 3-cm with ulceration (criteria II); 3) mucosal tumors, undifferentiated histologic type, and tumor sizes of ≤ 2-cm without ulceration (criteria III); or 4) tumors with minute submucosal invasion (< 500 µm from the muscularis mucosae), differentiated histologic type, and tumor sizes of ≤ 3-cm (criteria IV). All tumors meeting the expanded criteria should have no LVI [1,2]. EGC lesions that did not meet the expanded criteria were defined as out-of-indication cases.
Statistical analysis
Continuous variables are described as median with interquartile range (IQR) or mean with standard deviation, while categorical variables as percentages. The McNemar's tests were used to compare differences in submucosal and LVI between 2-mm and wider interval sections (4- or 6-mm intervals). Changes in curability criteria for endoscopic resection according to section intervals, were compared using the McNemar-Bowker's symmetry tests [19]. P-values of <0.05 were considered significant. All data were analyzed using STATA 13.1 (StataCorp, College Station, TX, USA).
RESULTS
Baseline characteristics
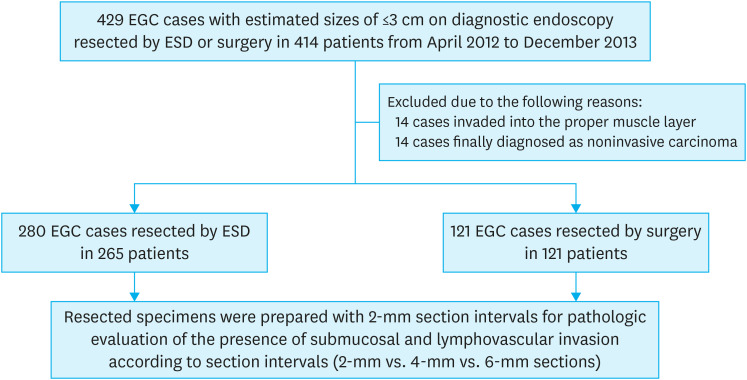
We excluded 14 muscle-invasive and 14 non-invasive carcinoma cases as diagnosed by pathological evaluation of the 429 EGC lesions from 414 patients. A total of 401 EGC lesions from 386 patients who underwent ESD or surgery were included in our study. Among them, 280 EGC lesions from 265 patients, and 121 EGC lesions from 121 patients were treated by ESD and surgical resection, respectively (Fig. 2).
Fig. 2. Study flow.
EGC = early gastric cancer; ESD = endoscopic submucosal dissection.
The baseline patient data and tumor characteristics evaluated in 2-mm interval sections are presented in Table 1. The median age of the included patients was 63 years (IQR, 54–72 years). In the reference 2-mm interval sections, we detected the submucosal invasion in 117 cases (29.2%), while the LVI was detected in 38 cases (9.5%). Among the 117 submucosal invasion cases, 24 cases (20.5%) were identified in one section, 23 cases (19.7%) in two sections, and 70 cases (59.8%) in three or more sections. Of the 38 LVI cases, 18 cases (47.4%) were detected in one section, 7 cases (18.4%) in two sections, and 13 cases (34.2%) in three or more sections.
Table 1. Patient and tumor characteristics.
| Characteristics | Total | Treatment | ||||
|---|---|---|---|---|---|---|
| ESD | Surgery | |||||
| Patient characteristics | ||||||
| No. of patients | 386 | 265 | 121 | |||
| Age (yr) | 63 (54–72) | 66 (58–74) | 55 (50–65) | |||
| Sex | ||||||
| Female | 122 (31.6) | 72 (27.2) | 50 (41.3) | |||
| Male | 264 (68.4) | 193 (72.8) | 71 (58.7) | |||
| No. of EGC lesion | ||||||
| One | 372 (96.4) | 251 (94.7) | 121 (100) | |||
| Two | 13 (3.4) | 13 (4.9) | 0 (0) | |||
| Three | 1 (0.3) | 1 (0.4) | 0 (0) | |||
| Tumor characteristics | ||||||
| No. of tumors | 401 | 280 | 121 | |||
| Tumor location | ||||||
| Upper third | 23 (5.7) | 13 (4.6) | 10 (8.3) | |||
| Middle third | 165 (41.2) | 91 (32.5) | 74 (61.2) | |||
| Lower third | 213 (53.1) | 176 (62.9) | 37 (30.6) | |||
| Tumor size (cm) | 1.96±1.09 | 1.82±1.07 | 2.28±1.07 | |||
| Tumor histology | ||||||
| Differentiated type | 315 (78.6) | 274 (97.9) | 40 (33.1) | |||
| Undifferentiated type | 86 (21.5) | 6 (2.1) | 81 (66.9) | |||
| Ulcer finding | ||||||
| Absence | 241 (60.1) | 182 (65.0) | 59 (48.8) | |||
| Presence | 160 (39.9) | 98 (35.0) | 62 (51.2) | |||
| Tumor depth | ||||||
| Mucosa | 284 (70.8) | 215 (76.8) | 69 (57.0) | |||
| Submucosa | 117 (29.2) | 65 (23.2) | 52 (43.0) | |||
| Submucosa <500 µm | 47 (11.7) | 30 (10.7) | 17 (14.1) | |||
| Submucosa ≥500 µm | 70 (17.5) | 35 (12.5) | 35 (28.9) | |||
| LVI | ||||||
| Absence | 363 (90.5) | 260 (92.9) | 103 (85.1) | |||
| Presence | 38 (9.5) | 20 (7.1) | 18 (14.9) | |||
| Lymph node metastasis* | ||||||
| Absence | 394 (98.3) | - | 114 (94.2) | |||
| Presence | 7 (1.7) | - | 7 (5.8) | |||
Pathology evaluation findings from 2-mm interval sections were presented. Values are presented as number of patients (%), median (interquartile range), or mean±standard deviation.
EGC = early gastric cancer; ESD = endoscopic submucosal dissection; LVI = lymphovascular invasion.
*Status of lymph node metastasis was evaluated only in patients with EGC who underwent resection.
Detection rates of submucosal invasion based on section intervals
Compared to the 100% detection rates of the 117 submucosal invasive EGC cases in the reference 2-mm interval section, the detection rates of submucosal invasion in the 4-mm interval sections decreased significantly to 88.0% in even-numbered (2n) sections, and 90.6% in odd-numbered (2n+1) sections (both P<0.001 by McNemar's test, each compared to the reference 2-mm interval). The submucosal invasion was detected in 78.6% (92/117) of cases, consistently in both sets of the 4-mm interval sections.
In the 6-mm sections, the detection rates decreased further to 76.9% in 3n-, 80.3% in 3n+1, and 72.7% in 3n+2 sections (all three P<0.001 by McNemar's test, as compared with the reference 2-mm interval). In 52.1% (61/117) of cases, the submucosal invasion was detected consistently in all three sets of the 6-mm interval sections (Table 2).
Table 2. Submucosal and LVI detection rates in 401 EGC lesions according to section intervals of resected specimen.
| Variables | Submucosal invasion | LVI | |||
|---|---|---|---|---|---|
| No. (%) | P* | No (%) | P* | ||
| Reference 2-mm interval section | 117 (100.0) | - | 38 (100.0) | - | |
| 4-mm interval section | |||||
| 2n | 103 (88.0) | 0.0002 | 33 (86.8) | 0.0253 | |
| 2n+1 | 106 (90.6) | 0.0009 | 22 (57.9) | 0.0001 | |
| Detected in all sections | 92 (78.6) | - | 17 (44.7) | - | |
| 6-mm interval section | |||||
| 3n | 90 (76.9) | <0.0001 | 21 (55.3) | <0.0001 | |
| 3n+1 | 94 (80.3) | <0.0001 | 22 (57.9) | 0.0001 | |
| 3n+2 | 85 (72.7) | <0.0001 | 24 (63.2) | 0.0002 | |
| Detected in all sections | 61 (52.1) | - | 9 (23.7) | - | |
LVI = lymphovascular invasion; EGC = early gastric cancer
*P-values calculated using McNemar's test compared to results from the reference 2-mm interval sections.
Detection rates of LVI according to section intervals
LVI was present in 38 EGC cases (100%) in the reference 2-mm interval sections. In the 4-mm sections, the detection rates were 86.8% in 2n (P = 0.025 by McNemar's test), and 57.9% in 2n+1 sections (P<0.001 by McNemar's test). LVI was detected consistently in only 44.7% (17/38) of cases in both 4-mm interval sets (Table 2).
In the 6-mm sections, the detection rates decreased further to 55.3%, 57.9%, and 63.2% in 3n, 3n+1, and 3n+2 sections, respectively, (all P<0.001 by McNemar's test, each compared to the reference sections). LVI was detected consistently only in 23.7% (9/38) of cases in all three 6-mm interval sets (Table 2).
Curability criteria distribution following the section interval width
In the reference 2-mm interval sections, 102 (25.4%) EGC cases met the absolute criteria, while 149 (37.2%) met the expanded criteria. The remaining 150 cases (37.4%) were classified as out-of-indication cases (Supplementary Fig. 1A).
In the 4-mm interval sections, misclassification of the curability criteria was noted for seven cases (1.7%, 7/401 cases) in even-numbered (2n) sections. Of these, three cases were misclassified from expanded criteria to absolute criteria due to missed detection of submucosal invasion (Table 3). Due to the missed detection of submucosal or LVI, four (2.7%, 4/150) out-of-indication cases were misclassified as curative resection cases. Changes in the curability criteria were not significant in even-numbered sections compared to the reference interval (P=0.101 by McNemar-Bowker's symmetry test). In the odd-numbered (2n+1) sections, curability criteria were misclassified in 13 cases (3.2%, 13/401 cases). Among the 150 out-of-indication cases in the 2-mm interval sections, ten (6.7%) were misclassified as curative resection cases due to the missed detection of submucosal (2 cases) or LVI (8 cases) (Table 3). Compared to the 2-mm interval sections, the curability criteria distributions changed significantly (P=0.043 by McNemar-Bowker's symmetry test) (Supplementary Fig. 1A).
Table 3. Misclassification in wide interval sections compared the 2-mm interval sections for endoscopic resection criteria.
| Variables | Section intervals | ||||||
|---|---|---|---|---|---|---|---|
| 4-mm interval | 6-mm interval | ||||||
| 2n | 2n+1 | 3n | 3n+1 | 3n+2 | |||
| Expanded criteria in 2-mm interval sections (n=149) | |||||||
| Change from expanded to absolute criteria | 3/149 (2.0) | 3/149 (2.0) | 6/149 (4.0) | 4/149 (2.7) | 2/149 (1.3) | ||
| Missed submucosal invasion | 3 | 3 | 6 | 4 | 2 | ||
| Out-of-indication cases in 2-mm interval sections (n=150) | |||||||
| Change from out-of-indication to absolute criteria | 1/150 (0.7) | 2/150 (1.3) | 4/150 (2.7) | 2/150 (1.3) | 5/150 (3.3) | ||
| Missed submucosal invasion | 1 | 1 | 3 | 1 | 4 | ||
| Missed LVI | 0 | 1 | 1 | 1 | 1 | ||
| Change from out-of-indication to expanded criteria | 3/150 (2.0) | 8/150 (5.3) | 6/150 (4.0) | 8/150 (5.3) | 12/150 (8.0) | ||
| Missed submucosal invasion | 1 | 1 | 3 | 2 | 7 | ||
| Missed LVI | 2 | 7 | 3 | 6 | 5 | ||
LVI = lymphovascular invasion.
In the 6-mm interval sections, the curability criteria for 16 cases (4.0%, 16/401 cases) were misclassified in 3n, 14 (3.5%, 14/401 cases) in 3n+1, and 19 (4.7%, 19/401 cases) in 3n+2 sections compared to the reference 2-mm interval sections (Supplementary Fig. 1B). The distribution of curability criteria changed significantly in all three section numbers in the 6-mm interval (P=0.003 for 3n, P=0.008 for 3n+1, and P=0.002 for 3n+2 sections by McNemar-Bowker's symmetry test). Compared to the 150 out-of-indication cases at 2-mm interval, ten (6.7%, 10/150) to 17 (11.3%, 17/150) cases were misclassified from non-curative resection to curative resection cases in the 6-mm intervals due to the undetected submucosal invasion or LVI (Table 3).
Misclassification of endoscopic resection criteria in cases with lymph node metastasis
Lymph node metastasis was detected in seven (1.7%) of 121 surgically treated patients. In the reference 2-mm interval sections, all seven patients had out-of-indication tumors, and one patient misclassified as meeting the expanded criteria in both 4- and 6-mm interval sections due to missed LVI.
DISCUSSION
The current guidelines for the pathologic evaluation of EGC lesions recommend different section intervals: 2–3-mm intervals for endoscopic resection, and 5–7-mm intervals for surgical specimens [3,13,14]. We speculated that wide resection interval in surgical specimens might affect the detection of lymph node metastasis risk factors. In this study, pathological evaluation of endoscopically or surgically resected 401 EGC lesions was performed using 2-mm interval sections as a reference following the specimen handling guidelines for endoscopic resection. For wide interval sections, we arbitrarily chose 4- and 6-mm sections, and the risk of missed submucosal and LVI detection was high. Thus, the under-detection of submucosal and LVI in wider interval sections might result in the misclassification of curability criteria for endoscopic resection of EGC.
LVI is the most important risk factor for lymph node metastasis in patients with EGC [4,12,20]. The rate of lymph node metastasis of 25.7%–32.1% observed in patients exhibiting LVI was much higher compared to those without LVI (1.5%–2.3%) [4,20,21]. The LVI might be very focal, and the distribution of lymphatic vessels varies according to tumor depth and histologic types [16]. LVI prediction methods before endoscopic resection are not yet available, and detection of LVI could be missed even after pathologic evaluation of endoscopically resected specimens at 2-mm interval [11]. We found that 47.4% (18 of the 38 cases) of LVI cases were focal, and detected only in one section of the reference 2-mm interval. Thus, LVI detection rates decreased significantly in wide interval sections, and the detection rates in all section sets were consistently lower at 4-mm (44.7%, 17 of the 38 cases) and 6-mm intervals (23.7%, 9 of the 38 cases). Wider interval sections recommended for surgical specimens method could result in frequent under-detection of LVI. Due to the under-detection of LVI in wider interval sections, misclassification of curability criteria might occur in patients undergoing ESD.
Submucosal invasion is another important risk factor for lymph node metastasis in patients with EGC [4,12]. Similar to the LVI, the very focal submucosal invasion might be detected frequently in EGC lesions. In a study investigating lymph node metastasis risk in patients with minute submucosal EGC (submucosal invasion depth ≤500 µm), the width of the submucosal invasion was 1-mm or less in 188 of the 278 patients (67.6%) [15]. In our study, 20.5% (24/117) of submucosal invasion cases were detected only in one of the reference 2-mm interval sections. The submucosal invasion was detected consistently in 92 of the 117 (78.6%) cases in both 4-mm interval section sets and 61 of the 117 (52.1%) cases in all three 6-mm interval section sets. These findings suggest the possibility that the curability criteria after endoscopic resection of EGC cases could be misclassified from non-curative to curative resection if the section intervals of EGC specimens are wider than those recommended for endoscopically resected specimens. Further studies are needed to determine whether the deepest portion of submucosal invasion (especially deeper than 500 µm) is detectable in wider (4- and 6-mm) interval sections.
Studies from countries outside of Japan have reported that lymph node metastasis rates were not negligible, especially in patients with EGC who met the expanded criteria [5,6,7,22]. Chung et al. [5] found that lymph node metastasis rates were 0.23%–1.15% in patients with mucosal EGC meeting the expanded criteria. Kim et al. [6] also reported the incidence rates for lymph node metastasis of 0.29%–1.55% in patients with mucosal EGC who met the expanded criteria. Western studies reported higher lymph node metastasis rates in patients with EGC who met the expanded criteria, and the reported lymph node metastases were 7.5% and 2.9% in the US and Brazilian studies, respectively [7,22]. A recent systematic review reported a higher lymph node metastasis rate (4.0%) in minute submucosal lesions meeting the expanded criteria in studies conducted outside of Japan [23]. They emphasized the standardization of specimen processing and histological evaluation so that the Japanese study results could apply to other countries [23]. Our results indicated that the differences in pathology specimen processing could explain the incidence rate discrepancies in lymph node metastasis between studies.
Our study results showed that the risk of misclassification of the final pathology curability criteria for endoscopic resection of EGC was higher in wider interval sections compared to the 2-mm interval sections. Nearly 6.7% of non-curative cases and 11.3% of non-curative cases identified from 4- and 6-mm interval sections, respectively, were misclassified as meeting the final curability criteria and thus were indicated for curative resection. Moreover, among the seven lymph node metastasis cases classified as out-of-indication EGCs based on 2-mm interval sections, one was erroneously classified as a lesion meeting the expanded criteria in wider intervals. Thus, the current criteria for the endoscopic resection should be updated to using pathology data obtained from 2-mm interval surgical specimen sections for evaluating the risk factors for lymph node metastasis. However, surgically resected specimen processing at 2-mm interval sections is not cost-effective because lymph node metastasis is assessed in all patients.
Currently, endoscopic resection for EGC meeting the expanded criteria is performed routinely in selected patients [1,2,3]. Long-term outcomes after curative resection of endoscopic resection in patients meeting the expanded criteria were as favorable as in those who met the absolute criteria [24,25,26]. The long-term overall survival rates of patients who underwent endoscopic resection were not different compared to those who underwent surgery for EGC meeting the curative resection criteria reported in studies performed using the propensity score matching [27,28,29,30]. Thus, if a lesion met the absolute or expanded criteria after pathological evaluation of a 2-mm interval ESD specimen section, it should be considered as a curative resection case since a thorough risk factor evaluation was undertaken.
There are several limitations to our study. First, selection bias might exist due to the inclusion of lesions with an endoscopic size of 3-cm or less. Second, we included patients who underwent endoscopic resection, and lymph node metastasis was evaluated only in patients who underwent surgery. Third, we could not assess long-term clinical outcomes, including overall mortality and cancer recurrence based on changes in section intervals due to this being a cross-sectional study. Fourth, the underestimation of lymphovascular or submucosal invasion in 4- and 6-mm interval sections might not affect decision making for additional chemotherapy of patients who underwent surgery since lymph node metastasis in the resected lymph nodes was assessed. Finally, the pathological evaluation of all study specimen was conducted with 2-mm interval sections. Hence, the detection rates for the lymphovascular and submucosal invasion could not be determined using a 3-mm interval sections as recommended by the ESD specimen handling guidelines [3,14].
In conclusion, wide interval sections recommended for surgical specimen handling might underestimate lymphovascular and submucosal invasion. This finding might explain the increased risk of lymph node metastasis in EGC lesions meeting the expanded criteria reported in the literature, which investigated lymph node metastasis risk using surgically resected specimens. Thus, if an EGC lesion meets expanded criteria after the pathological evaluation of ESD specimens, the lesion can be safely followed up.
Footnotes
Funding: The National Cancer Center (grant numbers: 1610180 and 1910270) supported this work.
- Conceptualization: C.I.J.
- Data curation: K.M.C., L.J.Y., K.C.G., E.B.W., Y.H.M., R.K.W., K.Y.W., C.I.J.
- Formal analysis: K.Y.I., K.M.C., C.I.J.
- Writing - original draft: K.Y.I., C.I.J.
- Writing - review & editing: K.Y.I., K.M.C., C.J.E., L.J.Y., K.C.G., E.B.W., Y.H.M., R.K.W., K.Y.W., C.I.J.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIAL
Comparison of the curability criteria distribution according to the section intervals. (A) Curability criteria between 2-mm section interval and 4-mm section interval. (B) Curability criteria between 2-mm section interval and 6-mm section interval.
References
- 1.Guideline Committee of the Korean Gastric Cancer Association (KGCA), Development Working Group & Review Panel. Korean practice guideline for gastric cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019;19:1–48. doi: 10.5230/jgc.2019.19.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4) Gastric Cancer. 2017;20:1–19. doi: 10.1007/s10120-016-0622-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ono H, Yao K, Fujishiro M, Oda I, Nimura S, Yahagi N, et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer. Dig Endosc. 2016;28:3–15. doi: 10.1111/den.12518. [DOI] [PubMed] [Google Scholar]
- 4.Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 5.Chung JW, Jung HY, Choi KD, Song HJ, Lee GH, Jang SJ, et al. Extended indication of endoscopic resection for mucosal early gastric cancer: analysis of a single center experience. J Gastroenterol Hepatol. 2011;26:884–887. doi: 10.1111/j.1440-1746.2010.06611.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim YI, Lee JH, Kook MC, Lee JY, Kim CG, Ryu KW, et al. Lymph node metastasis risk according to the depth of invasion in early gastric cancers confined to the mucosal layer. Gastric Cancer. 2016;19:860–868. doi: 10.1007/s10120-015-0535-7. [DOI] [PubMed] [Google Scholar]
- 7.Hanada Y, Choi AY, Hwang JH, Draganov PV, Khanna L, Sethi A, et al. Low frequency of lymph node metastases in patients in the United States with early-stage gastric cancers that fulfill Japanese endoscopic resection criteria. Clin Gastroenterol Hepatol. 2019;17:1763–1769. doi: 10.1016/j.cgh.2018.11.031. [DOI] [PubMed] [Google Scholar]
- 8.Abdelfatah MM, Barakat M, Lee H, Kim JJ, Uedo N, Grimm I, et al. The incidence of lymph node metastasis in early gastric cancer according to the expanded criteria in comparison with the absolute criteria of the Japanese Gastric Cancer Association: a systematic review of the literature and meta-analysis. Gastrointest Endosc. 2018;87:338–347. doi: 10.1016/j.gie.2017.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Oya H, Gotoda T, Kinjo T, Suzuki H, Yoshinaga S, Taniguchi H, et al. A case of lymph node metastasis following a curative endoscopic submucosal dissection of an early gastric cancer. Gastric Cancer. 2012;15:221–225. doi: 10.1007/s10120-011-0111-8. [DOI] [PubMed] [Google Scholar]
- 10.Abe S, Oda I, Nakajima T, Suzuki H, Nonaka S, Yoshinaga S, et al. A case of local recurrence and distant metastasis following curative endoscopic submucosal dissection of early gastric cancer. Gastric Cancer. 2015;18:188–192. doi: 10.1007/s10120-014-0341-7. [DOI] [PubMed] [Google Scholar]
- 11.Hirasawa T, Fujisaki J, Fukunaga T, Yamamoto Y, Yamaguchi T, Katori M, et al. Lymph node metastasis from undifferentiated-type mucosal gastric cancer satisfying the expanded criteria for endoscopic resection based on routine histological examination. Gastric Cancer. 2010;13:267–270. doi: 10.1007/s10120-010-0577-9. [DOI] [PubMed] [Google Scholar]
- 12.Kwee RM, Kwee TC. Predicting lymph node status in early gastric cancer. Gastric Cancer. 2008;11:134–148. doi: 10.1007/s10120-008-0476-5. [DOI] [PubMed] [Google Scholar]
- 13.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 14.Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma: 15th Japanese Edition. Tokyo: Kanehara & Co. Ltd.; 2017. [DOI] [PubMed] [Google Scholar]
- 15.Choi JY, Park YS, Jung HY, Son DH, Ahn JY, Han S, et al. Identifying predictors of lymph node metastasis after endoscopic resection in patients with minute submucosal cancer of the stomach. Surg Endosc. 2015;29:1476–1483. doi: 10.1007/s00464-014-3828-8. [DOI] [PubMed] [Google Scholar]
- 16.Sako A, Kitayama J, Ishikawa M, Yamashita H, Nagawa H. Impact of immunohistochemically identified lymphatic invasion on nodal metastasis in early gastric cancer. Gastric Cancer. 2006;9:295–302. doi: 10.1007/s10120-006-0396-1. [DOI] [PubMed] [Google Scholar]
- 17.Lee JY, Choi IJ, Cho SJ, Kim CG, Kook MC, Lee JH, et al. Routine follow-up biopsies after complete endoscopic resection for early gastric cancer may be unnecessary. J Gastric Cancer. 2012;12:88–98. doi: 10.5230/jgc.2012.12.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kleihues P, Sobin LH. Pathology and Genetics of Tumours of the Digestive System. Lyon: IARC Press; 2000. [Google Scholar]
- 19.May WL, Johnson WD. Symmetry in square contingency tables: tests of hypotheses and confidence interval construction. J Biopharm Stat. 2001;11:23–33. doi: 10.1081/BIP-100104195. [DOI] [PubMed] [Google Scholar]
- 20.Kim H, Kim JH, Park JC, Lee YC, Noh SH, Kim H. Lymphovascular invasion is an important predictor of lymph node metastasis in endoscopically resected early gastric cancers. Oncol Rep. 2011;25:1589–1595. doi: 10.3892/or.2011.1242. [DOI] [PubMed] [Google Scholar]
- 21.Lee SY, Yoshida N, Dohi O, Lee SP, Ichikawa D, Kim JH, et al. Differences in prevalence of lymphovascular invasion among early gastric cancers between Korea and Japan. Gut Liver. 2017;11:383–391. doi: 10.5009/gnl16281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pessorrusso FC, Felipe-Silva A, Jacob CE, Ramos MF, Ferreira VA, de Mello ES, et al. Risk assessment of lymph node metastases in early gastric adenocarcinoma fulfilling expanded endoscopic resection criteria. Gastrointest Endosc. 2018;88:912–918. doi: 10.1016/j.gie.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 23.Abdelfatah MM, Barakat M, Othman MO, Grimm IS, Uedo N. The incidence of lymph node metastasis in submucosal early gastric cancer according to the expanded criteria: a systematic review. Surg Endosc. 2019;33:26–32. doi: 10.1007/s00464-018-6451-2. [DOI] [PubMed] [Google Scholar]
- 24.Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58:331–336. doi: 10.1136/gut.2008.165381. [DOI] [PubMed] [Google Scholar]
- 25.Ahn JY, Jung HY, Choi KD, Choi JY, Kim MY, Lee JH, et al. Endoscopic and oncologic outcomes after endoscopic resection for early gastric cancer: 1370 cases of absolute and extended indications. Gastrointest Endosc. 2011;74:485–493. doi: 10.1016/j.gie.2011.04.038. [DOI] [PubMed] [Google Scholar]
- 26.Kim SG, Park CM, Lee NR, Kim J, Lyu DH, Park SH, et al. Long-term clinical outcomes of endoscopic submucosal dissection in patients with early gastric cancer: a prospective multicenter cohort study. Gut Liver. 2018;12:402–410. doi: 10.5009/gnl17414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi IJ, Lee JH, Kim YI, Kim CG, Cho SJ, Lee JY, et al. Long-term outcome comparison of endoscopic resection and surgery in early gastric cancer meeting the absolute indication for endoscopic resection. Gastrointest Endosc. 2015;81:333–41.e1. doi: 10.1016/j.gie.2014.07.047. [DOI] [PubMed] [Google Scholar]
- 28.Kim YI, Kim YW, Choi IJ, Kim CG, Lee JY, Cho SJ, et al. Long-term survival after endoscopic resection versus surgery in early gastric cancers. Endoscopy. 2015;47:293–301. doi: 10.1055/s-0034-1391284. [DOI] [PubMed] [Google Scholar]
- 29.Shin DW, Hwang HY, Jeon SW. Comparison of endoscopic submucosal dissection and surgery for differentiated type early gastric cancer within the expanded criteria. Clin Endosc. 2017;50:170–178. doi: 10.5946/ce.2016.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pyo JH, Lee H, Min BH, Lee JH, Choi MG, Lee JH, et al. Long-term outcome of endoscopic resection vs. surgery for early gastric cancer: a non-inferiority-matched cohort study. Am J Gastroenterol. 2016;111:240–249. doi: 10.1038/ajg.2015.427. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of the curability criteria distribution according to the section intervals. (A) Curability criteria between 2-mm section interval and 4-mm section interval. (B) Curability criteria between 2-mm section interval and 6-mm section interval.