Abstract
Context
Discordance in prognostic understanding between caregivers of adults with advanced cancer and the oncologist may shape caregivers’ views of the oncologist and bereavement outcomes.
Objectives
We examined prospective associations of caregiver-oncologist discordance with caregiver-oncologist therapeutic alliance and caregiver anxiety following patient death.
Methods
We conducted a secondary analysis of data collected in a cluster randomized controlled trial from August 2012 to June 2014 in Western New York and California. At enrollment, caregivers and oncologists used a 7-point scale to rate their beliefs about the patient’s curability and living ≥2 years: 100%, about 90%, about 75%, about 50/50, about 25%, about 10%, and 0%. Discordance was defined as a difference of ≥2 points. Outcomes at 7 months after patient death included caregiver-oncologist therapeutic alliance [modified 5-item Human Connection (THC) scale] and caregiver anxiety (Generalized Anxiety Disorder-7). We conducted multivariable linear regression models to assess the independent associations of discordance with alliance and anxiety.
Results:
We included 97 caregivers (mean age=63) and 38 oncologists; 41% of caregiver-oncologist dyads had discordant beliefs about the patient’s curability and 63% of caregiver-oncologist dyads had discordant beliefs about living ≥2 years. On multivariate analysis, discordance in beliefs about curability was associated with lower anxiety (β=−2.20, SE=0.77, p=0.005). Discordance in beliefs about length of life was associated with a weaker alliance (β=−5.87, SE=2.56, p=0.02).
Conclusion:
A better understanding of how caregivers understand and come to terms with poor prognoses will guide interventions to improve cancer care delivery and outcomes of cancer treatment.
Keywords: discordance, beliefs about curability, beliefs about length of life, therapeutic alliance, anxiety
1. Introduction
Caregivers play an important role in the care of patients with advanced cancer. They not only accompany patients to medical appointments, offer advice, and provide emotional support, but also are involved in cancer treatment decision-making. Studies have shown that up to 55% of caregivers have a different understanding of the patient’s prognosis relative to their oncologist, most of which are due to caregivers being more optimistic than the oncologist.1,2 Prior research has also shown that poor prognostic understanding among patients with cancer is associated with both poor and good outcomes.3–9 Patients who have poor prognostic understanding are less likely to utilize palliative and hospice care3–5 and more likely to receive aggressive life-prolonging care,10 but they report less anxiety and fewer depressive symptoms.6–9 We are aware of no prior studies examining the relationships between caregiver prognostic understanding and caregiver bereavement outcomes.
Therapeutic alliance is generally described as a collaborative relationship between physicians/oncologists and patients,11,12 but is applicable to caregivers as well, especially in the setting of advanced life-limiting disease. Just as a stronger patient-physician alliance is associated with better patient outcomes (e.g., higher rates of treatment adherence,13 superior patient quality of life, greater illness acceptance, lower likelihood of receiving aggressive care11,14), a stronger caregiver-physician alliance may reflect better satisfaction with cancer care, perhaps as a consequence of clinician communication.15 However, the therapeutic alliance between caregivers and oncologists is infrequently studied.16,17
The objective of this exploratory secondary analysis was to evaluate the associations of caregiver-oncologist discordance in prognostic understanding, in the form of beliefs about curability and length of life, with caregiver-oncologist therapeutic alliance measured 7 months after the patient’s death. In addition, we also evaluated the associations of discordance with caregiver anxiety.
2. Methods
2.1. Study design, setting, and participants
This was an exploratory secondary analysis of a cluster randomized controlled trial [Values and Options in Cancer Care (VOICE); ClinicalTrials.gov, NCT01485627] in Western New York and Northern California (three academic medical centers, three community hospitals, and four community-based cancer clinics). Detailed information on the study has been previously reported.18–20 Briefly, oncologists were randomized to an intervention or a control arm. In the intervention arm, oncologists received individualized communication training using standardized patient-instructors. Their patients (and caregivers if available) participated in an in-person coaching session and up to three follow-up telephone calls with their coach. Oncologists, patients, and/or their caregivers in the control arm received usual care. Participants were recruited from August 2012 to June 2014. All oncologists, patients, and/or their caregivers provided informed consent prior to study enrollment. The study was approved by the Institutional Review Board at each study site.
2.2. Participants and brief description of the primary study
The VOICE trial included medical oncologists who care for patients with non-hematologic malignancies at the participating clinics. Patients of the participating oncologists were recruited. Eligibility criteria for patients included aged ≥21 years, able to understand spoken English, able to provide informed consent, and stage III or IV non-hematologic malignancy (for patients with stage III cancer, their oncologist must affirm that they “would not be surprised” if the patient were to die within 12 months). We excluded hospitalized patients and patients on hospice. For caregivers, patients were asked to identify “a family member, partner, friend, or other individual involved with your health care issues, preferably someone who comes to physician appointments with you”. Caregivers were aged ≥21, able to understand spoken English, and able to provide informed consent. The primary study tracked the patient survival until December 2016. For our analysis, we included caregivers of patients who completed measures 7 months after the patient’s death.
2.3. Measures
Oncologists provided information on their demographics and beliefs about the patient’s chance of cure and length of life at enrollment. For chance of cure, they were asked “what do you believe are this patient’s chances of being cured?” For length of life estimates, they were asked “what do you believe are the chances that this patient will live for 2 years or more?” Response options were 100%, about 90%, about 75%, about 50/50, about 25%, about 10%, 0%, and “don’t know”. These questions and responses were based on the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) measure.21
Caregivers completed an assessment at enrollment which included their demographics, their beliefs about the patient’s chance of cure and length of life (question and response options were same as above), and their perceived therapeutic alliance with the patient’s oncologist. Seven months after the patient’s death, caregivers repeated the assessment on therapeutic alliance and also self-reported their anxiety levels.
2.3.1. Key independent variables: Caregiver-oncologists discordance in beliefs about curability and length of life
Discordance was defined categorically as a difference of two or more levels in response options between the caregiver and oncologist based on a prior study.22 For example, if the caregiver selected 90% and the oncologist selected 50/50, this was considered discordant. If the caregiver selected 90% and the oncologist selected 75%, this was considered concordant.
2.3.2. Key dependent variables: Caregiver-oncologist therapeutic alliance and caregiver anxiety
The dependent variables were assessed approximately seven months after the death of the patient. We selected seven months as it is a common time point in the bereavement literature14,23,24 as the effects of acute grief may last for a few months, and we conducted the assessments after the effects of acute grief were presumed to resolve. Therapeutic alliance was measured using items from The Human Connection (THC) scale.11 The 16-item THC scale was originally developed to assess therapeutic alliance between patients and oncologists.11 Caregivers were asked to answer five adapted questions about the patient’s oncologist with regard to the last months of the patient’s life: 1) How often did the doctor ask you how you were coping with the patient’s illness? 2) How often did the doctor pay close attention to what you were saying? 3) How often did the doctor address your needs as a person? 4) How much did you feel the doctor cared about you? 5) How concerned was the doctor about your quality of life? Each question was rated from 0 (not at all) to 10 (always or completely), and a higher summary score indicated a stronger therapeutic alliance (range 0-50). Anxiety levels over the prior 2 weeks were assessed using the 7-item Generalized Anxiety Disorder-7 (GAD-7).25 Items are rated from 0 (not at all sure) to 3 (nearly every day) and higher scores indicate worse anxiety levels (range 0-21).26 A cut-off score of 5, 10, and 15, respectively, indicate mild, moderate, and severe anxiety.27
2.3.3. Covariates
Covariates included caregiver demographics and study arm. Caregiver demographics included age, gender, race (white vs. non-white), marital status (married vs. not-married), and education (at least some high school vs. some college vs. college graduate or above). We did not include patient demographics in the multivariable analyses due to multicollinearity with caregiver demographics.
2.4. Statistical analyses
After conducting descriptive statistics, we examined the bivariate associations between binary independent variables (caregiver-oncologist discordance in beliefs about curability and length of life) and the two dependent continuous outcomes (THC, GAD-7). We further evaluated adjusted associations in four separate linear regression models. We included caregiver demographics and study arm as covariates. In addition, for adjusted analysis for THC scale, we included baseline value (baseline value for GAD-7 was not collected). We used generalized estimating equations to account for clustering at the oncologist level.28 We performed all analyses using SAS 9.4 (SAS Institute Inc., Cary, NC).
In sensitivity analyses, we included time from the baseline study visit to the patient’s death as a covariate. We then repeated the multivariate analyses.
3. Results
The primary study included caregivers for 204 patients; 127 patients died during the study period, and we collected data 7 months after the patient’s death from 97 caregivers. Detailed information on these caregivers were previously described.20 Mean age of the caregivers was 63.2 (SD 11.6, range 22-83), 65% were female, 93% were white, and 81% were married. Approximately 32% were caregivers of patients with gastrointestinal cancer and 28% were caregivers of patients with lung cancer. Table 1 shows the characteristics of the study sample as well as the 38 oncologists.
Table 1:
Characteristics of the study sample
| Variables | ||
|---|---|---|
| Caregivers (N=97) | ||
| Age, mean (SD) | 63.2 (11.6) | |
| Gender, N (%) | Male | 34 (35.1) |
| Female | 63 (65.0) | |
| Race, N (%)a | White | 87 (92.6) |
| Non-white | 7 (7.5) | |
| Marital Status, N (%) | Married | 79 (81.4) |
| Non-married | 18 (18.6) | |
| Education, N (%) | College degree or above | 39 (40.2) |
| Some college | 31 (32.0) | |
| High school or below | 27 (27.8) | |
| Cancer type (patient), N (%)b | Gastrointestinal | 31 (32.3) |
| Lung | 27 (28.1) | |
| Other | 38 (39.6) | |
| Study arm, N (%) | Control | 49 (50.5) |
| Intervention | 48 (49.5) | |
| Discordance in beliefs about curability, N (%)c | Yes | 38 (39.2) |
| No | 54 (58.7) | |
| Discordance in length of life, N (%)d | Yes | 55 (63.2) |
| No | 32 (36.8) | |
| Therapeutic alliance (THC scale) at baseline, mean (SD)e | 27.5 (12.7) | |
| Oncologist (N=38) | ||
| Age, mean (SD) | 44.3 (9.8) | |
| Gender, N (%) | Male | 26 (68.4) |
| Female | 12 (31.6) | |
| Race, N (%) | White | 20 (52.6) |
| Non-white | 18 (47.4) | |
| Years in practice, mean (SD) | 11.8 (10.4) | |
3 caregivers had missing data
1 patient had missing data
4 patients selection the “don’t know” option and 1 oncologist did not provide response, therefore discordance cannot be determined
9 patients selection the “don’t know” option and 1 oncologist did not provide response, therefore discordance cannot be determined
2 caregivers had missing data
Abbreviation: THC scale, the human connection scale
3.1. Discordance in beliefs about curability and length of life
Figure 1 shows the distribution of beliefs about curability and likelihood of living 2 years; 4% and 9%, respectively, responded “don’t know” when asked about their beliefs about the patient’s chance of cure and length of life. Forty-one percent (38/92) of the caregiver-oncologist dyads were discordant in beliefs about curability (caregivers were more optimistic than the oncologist in all dyads). Almost 63% (55/87) were discordant in beliefs about 2-year survival (caregivers were more optimistic than the oncologist in 94% of the dyads). Thirty-two percent (27/84) the dyads were discordant in both beliefs about curability and 2-year survival.
Figure 1:
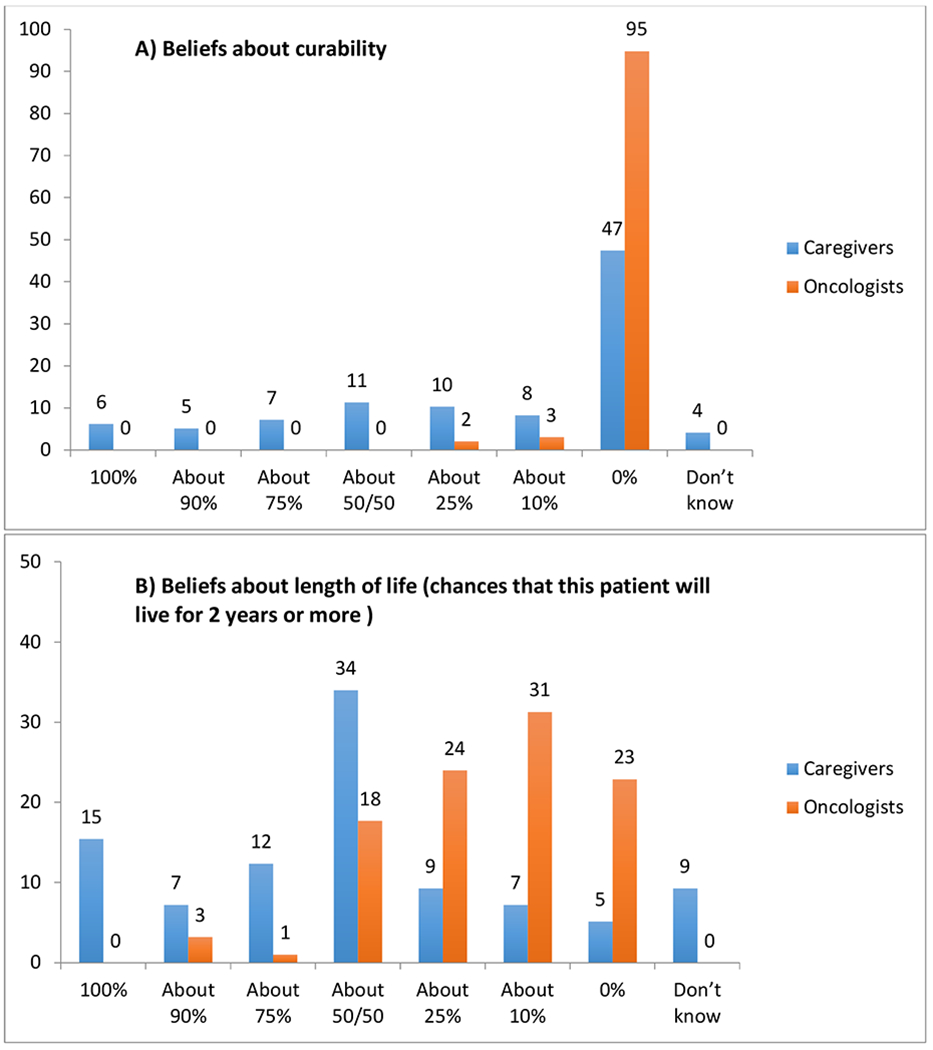
Distribution of caregiver and oncologist A) beliefs about curability and B) beliefs about length of life
3.2. Caregiver-oncologist therapeutic alliance
Mean THC score at 7 months after the patient’s death was 28.2 (SD 15.5, IQR 17-45, range 0-50). No significant differences were observed among dyads that were discordant in beliefs about curability. THC scores were significantly lower in caregiver-oncologist dyads that were discordant in beliefs about 2-year survival at enrollment (24.6 vs. 35.0, p=0.002) (Table 2). On multivariate analysis, discordance in beliefs about 2-year survival was significantly associated with lower THC scores 7 months after the patient’s death (β =−5.87, SE=2.56, p=0.00) (Table 3). In other words, compared to the concordant dyads, caregivers in the discordant dyads had a 5.87 point lower score on the THC scale.
Table 2:
Bivariate analyses of beliefs about curability and length of life with outcomes at 7 months after the patient’s death
| Outcomes at 7 month after the patient’s death | Total | Discordance in beliefs about curability (N=92) | Discordance in beliefs about length of life (N=87) | ||||
|---|---|---|---|---|---|---|---|
| Yes (N=38) | No (N=54) | P-value | Yes (N=55) | No (N=32) | P-value | ||
| Caregiver-oncologist therapeutic alliance (THC scale)a | 28.3 (15.5) | 26.7 (14.7) | 29.2 (16.1) | 0.46 | 24.6 (15.2) | 35.0 (14.0) | 0.002 |
| Caregiver anxiety (GAD-7)b | 2.7 (4.6) | 1.6 (3.2) | 3.4 (5.1) | 0.05 | 2.8 (4.6) | 2.8 (4.7) | 0.98 |
A higher score indicates better caregiver-oncologist therapeutic alliance
A higher score indicates higher caregiver anxiety
Abbreviations: THC scale, the human connection scale; GAD-7, Generalized Anxiety Disorder-7
Table 3:
Multivariate analyses of beliefs about curability and length of life with outcomes at 7 months after the patient’s death
| Outcomes at 7 month after the patient’s death | Discordance in beliefs about curability (N=92) | Discordance in beliefs about length of life (N=87) | ||||
|---|---|---|---|---|---|---|
| Beta Estimate | Standard Error | P-value | Beta Estimate | Standard Error | P-value | |
| Caregiver-oncologist therapeutic alliance (THC scale)a,b | −2.57 | 2.26 | 0.26 | −5.87 | 2.56 | 0.02 |
| Caregiver anxiety (GAD-7)c,d | −2.20 | 0.77 | 0.005 | −0.09 | 1.06 | 0.93 |
A higher score indicates better caregiver-oncologist therapeutic alliance
Adjusted for caregiver age, gender, race, education, marital status, study arm, baseline THC scale, and clustering at the oncologist level
A higher score indicates higher caregiver anxiety
Adjusted for caregiver age, gender, race, education, marital status, study arm, and clustering at the oncologist level
Abbreviations: THC scale, the human connection scale; GAD-7, Generalized Anxiety Disorder-7
3.3. Caregiver anxiety
Mean GAD-7 score at 7 months after the patient’s death was 2.7 (SD 4.6, IQR 0-3, range 0-21). Caregiver anxiety levels were lower in dyads that were discordant in beliefs about curability at enrollment (1.6 vs. 3.4, p=0.05) (Table 2). Caregiver anxiety levels were not different in dyads that were discordant in beliefs about 2-year survival. On multivariate analysis, discordance in beliefs about curability was associated with lower anxiety levels (β =−2.20, SE=0.77, p=0.005) (Table 3). In other words, compared to the concordant dyads, caregivers in the discordant dyads had a 2.20 point lower score on GAD-7.
3.4. Sensitivity analyses
After adjusting for time from baseline study visit to the patient’s death, results were similar. Discordance in beliefs about length of life was associated with lower THC score (β=−6.01, SE=2.61, p=0.01). Discordance in beliefs about curability was associated with lower anxiety levels (β=−2.27, SE=0.76, p=0.003).
4. Discussion
In this analysis, we found that discordance in beliefs about curability and length of life occurred in 41% and 63% of caregiver-oncologist dyads, respectively. The majority of the discordance was due to caregivers being more optimistic than the oncologist. Consistent with prior research, we found that caregiver-oncologist prognostic discordance was associated with both poor outcome (worse alliance) and good outcome (lower anxiety levels). Our findings reflect the need to assess caregiver beliefs about both the patient’s curability and length of life; the latter may be more difficult for caregivers to accept. Caregivers may be less likely to accept a shorter length of life as compared to an incurable cancer, as patients may live a long time irrespective of curability. We are unclear the reasons why discordance in curability and length of life were associated with lower anxiety levels and worse alliance, respectively, but not the other way round. They may be measuring different constructs and therefore more studies are required.29 Factors contributing to discordance are complex, and these include patient-related factors (e.g., race, education, emotional status, social support, fatalism),30 caregiver-related factors (e.g., race, education, caregiver health),30,31 physician-related factors (e.g., clinical experience, comfort with prognostic discussion),30,32,33 and disease-related factors (e.g., cancer type).30 The interplay of these factors and how they contribute to discordance need to be further investigated.
Prognostic understanding is variably defined in existing literature and includes unrealistic belief about prognosis,34,35 overestimation of prognosis relative to their oncologist,2,6,22 and overestimation of prognosis compared to the patient’s actual prognosis.36 While all three constructs are relevant, we chose to study caregiver beliefs about the patient’s prognosis relative to the because this is the most used definition in research. Caregivers are an essential component of patient-centered care as they play a major role in cancer treatment decision-making.37 However, studies of caregiver prognostic understanding are limited. The percentage of discordance between caregivers and oncologists in our study was comparable to that seen in prior studies.1,2 In older patients with advanced cancer seen by community oncologists in the United States, caregiver-oncologist discordance in beliefs about curability was 50%.2 In another study of patients with cancer in South Korea, caregiver-oncologist discordance in beliefs about curability was 45%, discordance about treatment goals was 70%, and discordance about disease stage was 66%.1 These findings emphasize the need to improve communication between oncologist and caregivers.38 Given the central role that caregivers play in treatment decision-making, working to build trust and ensuring they have accurate information may help improve their satisfaction with cancer care. In addition, caregivers may also help patients understand their disease, treatment, and prognosis, especially when many patients are not able to retain/recall information from clinic encounters.39
The importance of caregiver-oncologist therapeutic alliance does not end after the patient’s death. Caregivers’ experiences during the care of their loved ones may shape how they subsequently interact with the healthcare system.40 Caregivers who have had a bad experience may be less likely to seek treatment when needed and cope with bereavement.41 In addition, there is typically little contact between caregivers and oncologists after the patient’s death, which deprives caregivers of a source of support. The positive association between caregiver-oncologist discordance in beliefs about 2-year survival and lower therapeutic alliance underscores the need for research on how discordance undermines the alliance.42 This may help to guide interventions to improve the delivery of prognostic information while strengthening the alliance..43
Compared to other studies, caregivers in our sample reported relatively low levels of anxiety. Mean GAD-7 score was 2.7 compared to 9.0 in caregivers of patients with advanced cancer in the inpatient palliative care setting44 and 4.6-6.1 among patients seen in the primary care setting.27 Nonetheless, caregivers with a different belief about the patient’s curability had even lower anxiety levels after the patient’s death, suggesting that they may be actively defending against negative thoughts and emotions.45 Alternatively, low anxiety might reflect the protective role of optimism. Whether this relationship persists beyond 7 months is unclear and needs to be studied over a longer period of time. In addition, the associations of discordance with other bereavement outcomes such as prolonged grief, physical and mental health, and distress, especially during stressful life events should be further investigated.
Our study has several strengths. First, this was a multicenter study recruited from both academic and community cancer clinics. Second, the study provides a longitudinal relationship of caregiver-oncologist discordance at baseline with caregiver-oncologist therapeutic alliance and caregiver anxiety levels. There are several limitations to our study. First, most of the caregivers were white and well-educated, and therefore our findings may not be generalizable to non-white caregivers and those with lower education levels. Second, patient deaths were tracked for 30 months after the last patient was enrolled onto the study and therefore caregivers of the patients who died after that were not included. Future studies could examine long-term caregiver outcomes and their associations with discordance prior to the patient’s death. In addition, nearly one-third of dyads were excluded from the regression analyses either because caregivers were lost to follow-up 7 months after the patient’s death or because oncologists/caregivers responded “don’t know” with regards to their beliefs about the patient’s chance of cure and prognosis. The latter subgroup may merit further investigations. Third, we did not measure caregiver anxiety levels at baseline. Forth, we used binary classification of prognostic understanding into discordance and concordance, which was commonly used in published studies.6,22,30,46 Prognostic understanding may be dynamic, and we only measured it at enrollment. Future studies should explore degree of and change in discordance. Fifth, the THC scale was validated for use between patients and oncologists,11 but not between caregivers and oncologists. However, a prior study has used the THC scale for caregivers in the intensive care unit setting.16 Therapeutic alliance was also measured at 7-month following patient death and this may be subjected to recall bias. Sixth, we did not collect information on what the oncologist actually communicated to the caregiver in terms of the patient’s cancer curability and length of life. Finally, given this is an exploratory analysis, we did not adjust for multiple testing.
In conclusion, caregiver-oncologist discordance in beliefs about curability and 2-year survival was common. Although caregiver-oncologist discordance may protect against anxiety, it may compromise the caregiver-oncologist therapeutic alliance and potentially caregiver satisfaction with cancer care. A better understanding of how caregivers understand and come to terms with poor prognoses is needed to improve cancer care delivery and outcomes of advanced cancers.
Key Message:
Forty-one percent of caregiver-oncologist dyads had discordant beliefs about the patient’s curability and 63% of caregiver-oncologist dyads had discordant beliefs about living ≥2 years (caregivers were more optimistic in 94% of dyads). Caregiver-oncologist discordance may protect against anxiety but compromise the caregiver-oncologist alliance
Acknowledgments
Funding: The work was funded by the National Cancer Institute (R01 CA140419 to Ronald Epstein and Richard Kravitz; R01 CA168387 to Paul R. Duberstein and Holly G. Prigerson). Dr. Loh is supported by the National Cancer Institute (K99 CA237744) and Wilmot Research Fellowship Award. Dr. Prigerson is supported by the National Cancer Institute (R35 CA197730). Dr. Mohile is supported by the National Cancer Institute (K24 AG056589). Dr. Saeed is supported by the Carl W. Gottschalk Research Scholar Grant. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure/Conflict of Interest: Dr. Loh has served as a consultant to Seattle Genetics and Pfizer. All other authors have no relevant conflicts of interest to report.
Prior presentation: The abstract was accepted as an oral presentation at the 2019 ASCO Supportive Care in Oncology Symposium.
Competing interests: No competing interests
Submission declaration: The manuscript has not been published previously
References
- 1.Shin DW, Cho J, Kim SY, et al. Patients’ and family caregivers’ understanding of the cancer stage, treatment goal, and chance of cure: A study with patient-caregiver-physician triad. Psychooncology. 2018;27(1):106–113. [DOI] [PubMed] [Google Scholar]
- 2.Loh KP, Mohile SG, Lund JL, et al. Beliefs About Advanced Cancer Curability in Older Patients, Their Caregivers, and Oncologists. Oncologist. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010;28(7):1203–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang ST, Liu TW, Chow JM, et al. Associations between accurate prognostic understanding and end-of-life care preferences and its correlates among Taiwanese terminally ill cancer patients surveyed in 2011–2012. Psycho-oncology. 2014;23(7):780–787. [DOI] [PubMed] [Google Scholar]
- 5.Enzinger AC, Zhang B, Schrag D, Prigerson HG. Outcomes of Prognostic Disclosure: Associations With Prognostic Understanding, Distress, and Relationship With Physician Among Patients With Advanced Cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2015;33(32):3809–3816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Jawahri A, Traeger L, Kuzmuk K, et al. Prognostic understanding, quality of life and mood in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant. 2015;50(8):1119–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Jawahri A, Traeger L, Park ER, et al. Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer. 2014;120(2):278–285. [DOI] [PubMed] [Google Scholar]
- 8.Nipp RD, Greer JA, El-Jawahri A, et al. Coping and Prognostic Awareness in Patients With Advanced Cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2017;35(22):2551–2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sato T, Soejima K, Fujisawa D, et al. Prognostic Understanding at Diagnosis and Associated Factors in Patients with Advanced Lung Cancer and Their Caregivers. The oncologist. 2018;23(10):1218–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mack JW, Walling A, Dy S, et al. Patient beliefs that chemotherapy may be curative and care received at the end of life among patients with metastatic lung and colorectal cancer. Cancer. 2015;121(11):1891–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009;115(14):3302–3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allen ML, Cook BL, Carson N, Interian A, La Roche M, Alegria M. Patient-Provider Therapeutic Alliance Contributes to Patient Activation in Community Mental Health Clinics. Adm Policy Ment Health. 2017;44(4):431–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trevino KM, Abbott CH, Fisch MJ, Friedlander RJ, Duberstein PR, Prigerson HG. Patient-oncologist alliance as protection against suicidal ideation in young adults with advanced cancer. Cancer. 2014;120(15):2272–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Jama. 2008;300(14):1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kehl KL, Landrum MB, Arora NK, et al. Association of Actual and Preferred Decision Roles With Patient-Reported Quality of Care: Shared Decision Making in Cancer Care. JAMA Oncol. 2015;1(1):50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huff NG, Nadig N, Ford DW, Cox CE. Therapeutic Alliance between the Caregivers of Critical Illness Survivors and Intensive Care Unit Clinicians. Ann Am Thorac Soc. 2015;12(11):1646–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trevino KM, Maciejewski PK, Epstein AS, Prigerson HG. The lasting impact of the therapeutic alliance: Patient-oncologist alliance as a predictor of caregiver bereavement adjustment. Cancer. 2015;121(19):3534–3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Epstein RM, Duberstein PR, Fenton JJ, et al. Effect of a Patient-Centered Communication Intervention on Oncologist-Patient Communication, Quality of Life, and Health Care Utilization in Advanced Cancer: The VOICE Randomized Clinical Trial. JAMA Oncol. 2017;3(1):92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoerger M, Epstein RM, Winters PC, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer. 2013;13:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duberstein PR, Maciejewski PK, Epstein RM, et al. Effects of the Values and Options in Cancer Care Communication Intervention on Personal Caregiver Experiences of Cancer Care and Bereavement Outcomes. J Palliat Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. Jama. 1998;279(21):1709–1714. [DOI] [PubMed] [Google Scholar]
- 22.Gramling R, Fiscella K, Xing G, et al. Determinants of Patient-Oncologist Prognostic Discordance in Advanced Cancer. JAMA oncology. 2016;2(11):1421–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Breen LJ, Aoun SM, O’Connor M. The effect of caregiving on bereavement outcome: study protocol for a longitudinal, prospective study. BMC Palliat Care. 2015;14:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nielsen MK, Carlsen AH, Neergaard MA, Bidstrup PE, Guldin MB. Looking beyond the mean in grief trajectories: A prospective, population-based cohort study. Soc Sci Med. 2019;232:460–469. [DOI] [PubMed] [Google Scholar]
- 25.Lowe B, Decker O, Muller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. [DOI] [PubMed] [Google Scholar]
- 26.Arroll B, Goodyear-Smith F, Crengle S, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Annals of family medicine. 2010;8(4):348–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 28.Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467–474. [DOI] [PubMed] [Google Scholar]
- 29.Thompson LL, Temel B, Fuh CX, et al. Perceptions of medical status and treatment goal among older adults with advanced cancer. J Geriatr Oncol. 2019. [DOI] [PubMed] [Google Scholar]
- 30.Loh KP, Mohile SG, Lund JL, et al. Beliefs About Advanced Cancer Curability in Older Patients, Their Caregivers, and Oncologists. The oncologist. 2019;24(6):e292–e302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duberstein PR, Chen M, Chapman BP, et al. Fatalism and educational disparities in beliefs about the curability of advanced cancer. Patient education and counseling. 2018;101(1):113–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robinson TM, Alexander SC, Hays M, et al. Patient-oncologist communication in advanced cancer: predictors of patient perception of prognosis. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2008;16(9):1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duberstein PR, Kravitz RL, Fenton JJ, et al. Physician and Patient Characteristics Associated With More Intensive End-of-Life Care. Journal of pain and symptom management. 2019;58(2):208–215. e201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loh KP, Mohile SG, Epstein RM, et al. Willingness to bear adversity and beliefs about the curability of advanced cancer in older adults. Cancer. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol. 2011;29(17):2319–2326. [DOI] [PubMed] [Google Scholar]
- 36.Malhotra K, Fenton JJ, Duberstein PR, et al. Prognostic accuracy of patients, caregivers, and oncologists in advanced cancer. Cancer. 2019;125(15):2684–2692. [DOI] [PubMed] [Google Scholar]
- 37.Shin DW, Cho J, Roter DL, et al. Preferences for and experiences of family involvement in cancer treatment decision-making: patient-caregiver dyads study. Psychooncology. 2013;22(11):2624–2631. [DOI] [PubMed] [Google Scholar]
- 38.Cherlin E, Fried T, Prigerson HG, Schulman-Green D, Johnson-Hurzeler R, Bradley EH. Communication between physicians and family caregivers about care at the end of life: when do discussions occur and what is said? J Palliat Med. 2005;8(6):1176–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jansen J, Butow PN, van Weert JC, et al. Does age really matter? Recall of information presented to newly referred patients with cancer. J Clin Oncol. 2008;26(33):5450–5457. [DOI] [PubMed] [Google Scholar]
- 40.Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff (Millwood). 2010;29(8):1489–1495. [DOI] [PubMed] [Google Scholar]
- 41.Kim Y, Carver CS, Spiegel D, Mitchell HR, Cannady RS. Role of family caregivers’ self-perceived preparedness for the death of the cancer patient in long-term adjustment to bereavement. Psychooncology. 2017;26(4):484–492. [DOI] [PubMed] [Google Scholar]
- 42.Fenton JJ, Duberstein PR, Kravitz RL, et al. Impact of Prognostic Discussions on the Patient-Physician Relationship: Prospective Cohort Study. J Clin Oncol. 2018;36(3):225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ellison NM, Ptacek JT. Physician interactions with families and caregivers after a patient’s death: current practices and proposed changes. J Palliat Med. 2002;5(1):49–55. [DOI] [PubMed] [Google Scholar]
- 44.Ullrich A, Ascherfeld L, Marx G, Bokemeyer C, Bergelt C, Oechsle K. Quality of life, psychological burden, needs, and satisfaction during specialized inpatient palliative care in family caregivers of advanced cancer patients. BMC palliative care. 2017;16(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mund M, Mitte K. The costs of repression: a meta-analysis on the relation between repressive coping and somatic diseases. Health Psychol. 2012;31(5):640–649. [DOI] [PubMed] [Google Scholar]
- 46.Loh KP, Xu H, Back A, et al. Patient-hematologist discordance in perceived chance of cure in hematologic malignancies: A multicenter study. Cancer. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]


