Abstract
Objective:
To examine the characteristics of interventions to support family caregivers of patients with advanced cancer.
Methods:
Five databases (CINAHL, Medline, PsycINFO, Web of Science, and the Cochrane Library) were searched for English language articles of intervention studies utilizing randomized controlled trials or quasi-experimental designs, reporting caregiver-related outcomes of interventions for family caregivers caring for patients with advanced cancer at home.
Results:
A total of 11 studies met the inclusion criteria. Based on these studies, the types of interventions were categorized into psychosocial, educational, or both. The characteristics of interventions varied. Most interventions demonstrated statistically significant results of reducing psychological distress and caregiving burden and improving quality of life, self-efficacy, and competence for caregiving. However, there was inconsistency in the use of measures.
Conclusions:
Most studies showed positive effects of the interventions on caregiver-specific outcomes, yet direct comparisons of the effectiveness were limited. There is a lack of research aimed to support family caregivers’ physical health.
Practice implications:
Given caregivers’ needs to maintain their wellbeing and given the positive effects of support for them, research examining long-term efficacy of interventions and measuring objective health outcomes with rigorous quality of studies is still needed for better outcomes for family caregivers of patients with advanced cancer.
Keywords: advanced cancer, palliative care, family caregiver, support, outcome
1. Introduction
According to the National Alliance for Caregiving (NAC), approximately 2.8 million Americans provide care to an adult family member or relative with a cancer diagnosis [1]. Cancer is rated by caregivers as the most burdensome condition, followed by surgery and wounds, and a health problem requiring higher-hour caregiving [2]. Throughout the disease trajectory, family caregivers provide care to the individuals with cancer in varied phases: diagnosis, treatments, and palliation near the end of life [3]. Caregivers of patients with advanced cancer are especially challenged physically and emotionally. An estimated 10–60% of caregivers experience negative psychological and physical sequelae including anxiety, depression [4,5], grief [6], and poor physical health [7]. The World Health Organization standards for palliative care highlight the importance of supportive care for caregivers [8], and providing palliative care has positively been associated with reduction in caregiver burden [9,10]. However, support for caregivers is likely to be suboptimal in reality, in contrast to the philosophy of palliative care in which health and psychosocial care for them are deeply ingrained [11].
Recent research has shown that the majority of patients facing advanced illness prefer to receive care and die at home [12,13]. Home care allows the patients to continue their normal daily activities in a familiar environment where they maintain the best quality of life by increasing the chance of dying at home and reducing patients’ diverse symptom burden [13]. Caregivers of patients with advanced cancer also prefer providing care at home [14]. Despite the preference, home care for patients with advanced illness increases caregiving burden, and the burden usually increases over time as the patient’s condition declines [9].
Because of the need for effective ways to support family caregivers, an increasing number of caregiver-focused interventions have been developed and evaluated beyond merely involving family members as a part of the palliative care. Intervention studies for the caregivers can be broadly categorized into three types of interventions—educational or informational, psychosocial supports, or a combination of the two [3]. An educational or informational support program is aimed at providing education on symptom management or problem-solving skills, whereas a psychosocial support program usually includes counseling, telephone conferencing, or cognitive behavioral or interpersonal interventions. These interventions can be delivered to individuals, couples, and groups, in person, over the phone, and via the Internet [15].
Harding et al. conducted an initial systematic review of interventions for caregivers in cancer and palliative care in 2003 and updated while appraising the progress of methods for designing and delivering the interventions in 2011 [16,17]. Together, these systematic reviews cover the relevant studies between 1966 and 2010. They argued that there had been significant growth in the number of intervention studies for supporting caregivers in cancer care and improvement in the study design compared to their first review study [16]. They also pointed out the recurrent challenge and limitation of the large number of outcomes measured in relationship to the limited time period, the lack of diversity in study populations, and the high attrition rate within the palliative care population. In a more recent systematic review covering 2004–2014, Chi et al. synthesized behavioral and educational interventions for caregivers in end-of-life care [18]. They found an impressive expansion of the number of intervention studies specifically targeting caregivers, including randomized controlled trials (RCTs) with large sample sizes. However, they also noted the high attrition rate, short intervention timeframe and short time to follow-up, and a lack of consistent tools to measure caregiver outcomes and cost-effectiveness analysis [18].
The previous review studies did not limit the population or setting of interest, limiting the generalizability of the findings [16–18]. The increasing number of intervention studies targeting caregivers of patients with advanced cancer make it possible to focus on a particular diagnosis and care setting. This may allow more targeted perspectives regarding the caregiver support in unique situations.
Given the increasing demands for family caregivers of home care patients and limited synthesized evidence on supportive interventions that address the needs of caregivers of patients with advanced cancer, this review aims to examine characteristics of interventions for caregivers caring for people diagnosed with advanced cancer at home. Thus, this review is expected to discern the gaps which need further exploration to improve support for caregivers.
2. Method
A review methodology was adopted based on the Cochrane protocol for analysis and the protocol of Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) for reporting findings. This study was conducted to answer the questions: what are the characteristics of interventions supporting family caregivers providing care for patients with advanced cancer at home and what are evidence gaps that need to be further explored using more robust methods? [19]
2.1. Eligibility criteria
2.1.1. Inclusion criteria
English-language articles published between 2007 and 2018 that reported on RCTs and quasi-experimental studies of the effectiveness of an intervention for family caregivers of patients with advanced cancer were included. Caregivers had to be adults providing care in the home to adult patients with Stage III or IV cancer (advanced cancer). In this context, caregivers have been defined as a spouse, adult-child, relative or friend who has a significant relationship with and provides physical, social, and/or psychological assistance to a person with a life-threatening, incurable illness [20]. The intervention had to be explicitly aimed at supporting caregivers of patients with advanced cancer. The primary outcome had to be the psychological or physical effects on the caregivers. Any specific outcomes for searching relevant literature were not limited.
2.1.2. Exclusion criteria
Intervention studies for family caregivers caring for hospitalized patients or ones in nursing homes or assisted living facilities with advanced cancer were excluded. Pilot studies examining only feasibility and acceptability of an intervention and reports on intervention protocols were also excluded. Furthermore, studies focusing solely on patient outcomes and providing a patient-focused care to find the effects on caregivers were excluded to focus on caregiver-specific outcomes. Descriptive or qualitative designs and dissertations were also excluded.
2.2. Information sources
A comprehensive search was conducted using five databases: CINAHL, MEDLINE, PsycINFO, Web of Science, and the Cochrane Library, and through hand searching from reference lists of included articles. The first search was performed in each database in October 2017, and then it was updated in August 2018.
2.3. Search
The search strategy followed the PICO model: (1) Population: family caregivers of advanced cancer patients; (2) Intervention: caregiver support intervention; (3) Comparison: usual care; (4) Outcome: any caregiver outcomes. The following search equation were used: (“family caregivers” OR “informal caregivers”) AND (“advanced cancer” OR “palliative care” OR “hospice care” OR “end-of-life care”) AND (“intervention” OR “program” OR “trial”). The search was restricted to the title, abstract and keywords. English and full-text available peer-reviewed articles were applied in the search as restrictions.
2.4. Study selection and data collection
Study selection and data extraction were performed by one of the authors (SA). The following steps were taken: a) importation of all articles from databases to a reference management program (Mendeley®); b) removal of duplicates; c) initial manual screening of articles by title; d) secondary manual screening by abstract; and e) retrieval of the full text of articles for further evaluation.
2.5. Data items
For each study, the following items were extracted: a) study characteristics (country and year that the study was conducted, the number of participants in control/intervention groups, attrition rate, and study design); b) participant characteristics (gender and race); c) intervention-related aspects (setting for intervention, theory basis for developing the intervention, intervention contents, unit of intervention, provider, duration, follow-up period); and d) outcome-related aspects (outcome measures and the main study findings). The most commonly measured outcomes were synthesized in the analysis.
2.6. Study quality
Methodological quality was scored using the Cochrane Risk of Bias (RoB) tool for RCTs and ROBINS-I (Risk of Bias In Non-randomized Studies-of Interventions) tool for quasi-experimental studies. The Cochrane RoB tool has seven domains: (a) random sequence generation; (b) allocation concealment; (c) selective reporting; (d) blinding of participants and personnel; (e) blinding of outcome measurement; (f) incomplete outcome data; and (g) other bias [21]. Based on each risk of bias judgement, overall risk of bias of a study is evaluated (low risk, high risk, or unclear) [21]. The ROBINS-I tool covers seven domains: (a) bias due to confounding; (b) bias in selection of participants into the study; (c) classification of the intervention; (d) bias due to deviations from intended interventions; e) bias due to missing data; (f) bias in measurement of outcomes; and g) bias in selection of the reported result [22]. Based on the judgement for each domain, overall risk of bias of a study is assessed (low, moderate, serious, critical risk of bias, or no information) [22]. Study screening, review, and quality evaluation was done by the first author (SA) and verified by the other authors (RR, CC).
3. Results
A total of 1,361 potentially relevant articles were identified. After removing duplicates, screening titles and abstracts, and reviewing the full-text, 12 studies met the criteria (Figure 1). Two manuscripts were pooled because they reported on the same intervention study [23,24]. The final sample included 11 studies.
Figure 1. Flow diagram of search.
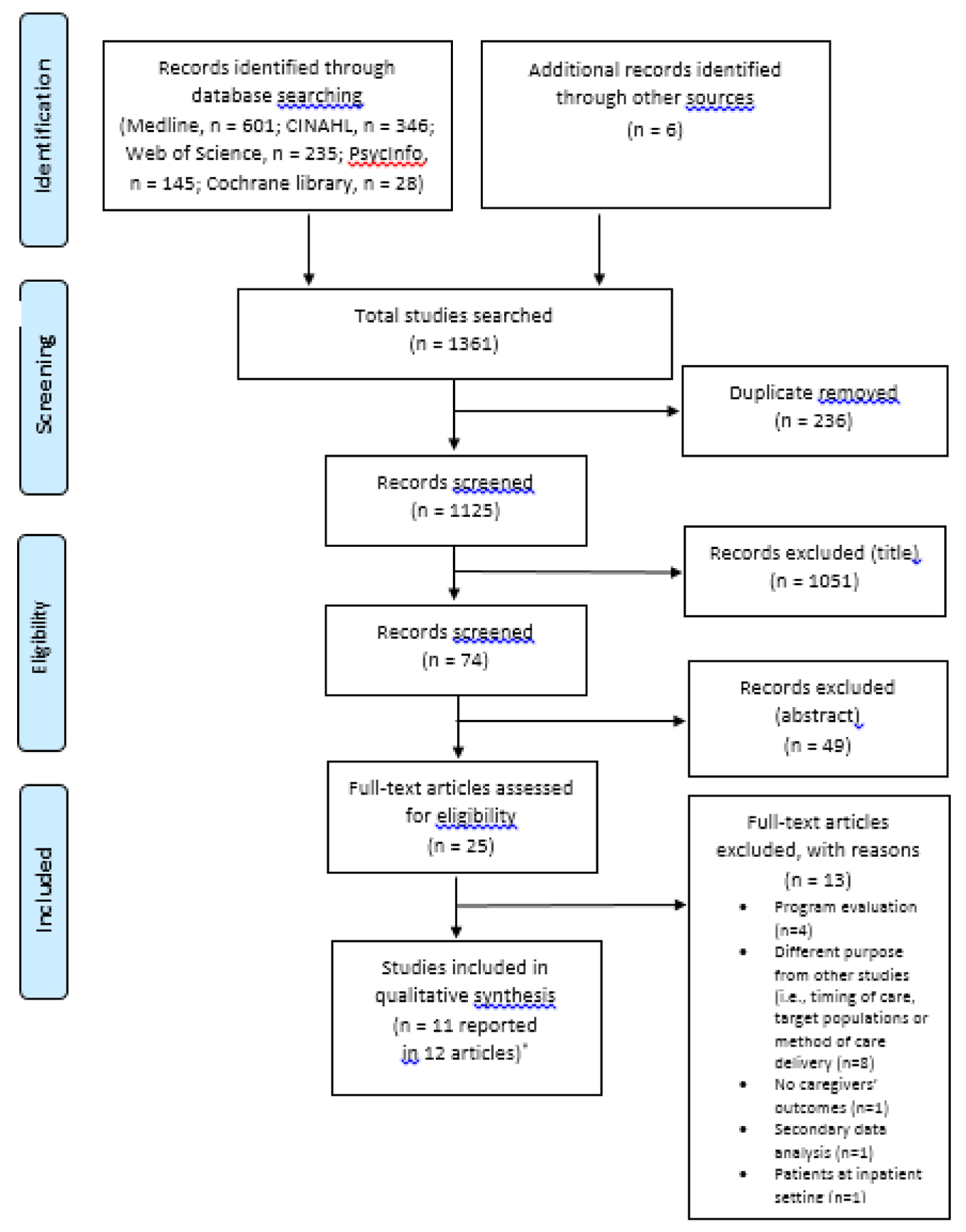
*Hudson et al. (2013) and Hudson et al. (2015) were pooled because reported different articles from the same study
3.1. Study Designs
Study characteristics, including research design, subjects, attrition rates, type of intervention, theoretical basis, and intervention setting are reported in Table 1. The sample included 9 RCTs (two of which were a cluster randomized trial and wait-control design respectively) [25,26] and two quasi-experimental studies [27,28].
Table 1.
Characteristics of included intervention studies for family caregivers of patients with advanced cancer
| Author/Country | Subject | N | Attrition Rate | Type of Intervention | Theoretical Basis | Setting of Intervention | Research Design | Overall Risk of Biasa |
|---|---|---|---|---|---|---|---|---|
| Psychosocial support | ||||||||
| Leow et al. /Singapore [36] | Family caregiver of a person with advanced (stage IV) cancer receiving home hospice care (having a prognosis of at least 3 months) | Con: n=42 Int: n=38 Mean age (years) 47.16±11.76 (range 22–72) Gender Male: n = 26 (32.5%) Female: n = 54 (67.5%) Race Chinese: n = 68 (85%) Malay: n = 8 (10%) Indian: n = 3 (3.8%) Caucasian: n = 1 (1.3%) |
Con: 0% Int: 0% | Int: Psychosocial Con: Routine care for their respective home hospice organization | Self-efficacy theory | Home hospice organizations and Outpatient clinic | RCT | Poor |
| McDonald et al. /Canada [25] | Primary caregivers of patients with stage IV cancer or stage III advanced cancer with poor prognosis (having a prognosis of 6–24 months) | Con: n=88 Int: n=94 Median age (years) Con: 57.0 (22–81) Int: 58.0 (25–83) Gender Male: 63 (34.6%) Female: 119 (65.4%) Race Not described |
Con: 15.9% Int: 18.1% | Int: Psychosocial Con: Standard oncology care | Not indicated | Outpatient Palliative clinic |
Cluster random ized trial | Poor |
| Educational support | ||||||||
| Badr et al. /US [31] | Advanced lung cancer patients and their caregivers (patients within 1 month of treatment initiation) | Con: 19 dyads Int: 20 dyads Mean age (years) 51.10±10.24 (range 35–70) Gender (caregivers) Male: 12 (31%) Female: 27 (69%) Race Not assessed |
Con: 5.2% Int: 0% | Int: Educational Con: Usual medical care | Selfdetermination theory (SDT) | Home | RCT | Poor |
| Dionne-Odom et al. /US [26] | Caregivers of patients with new diagnosis, recurrence, or progression of an advanced- stage cancer within 30–60 days (having a prognosis of 6–24 months) | Con (delayed palliative care group): n = 61 Int (early palliative care group): n = 61 Mean age (years) Con: 57.9±11.9 Int: 61.0±11.6 Gender Male: n = 26 (21.3%) Female: n = 96 (78.7%) Race White: n = 113 (92.6%) Other: n = 5 (4.1%) Missing: n =4 (3.3%) |
32% | Educational | Not indicated | Home | RCT (waitcontrol design) | Fair |
| DuBe nske et al. /US [33] | Primary caregivers of patients with non-small cell lung cancer at stage IIIA, IIIB, or TV (having a prognosis of at least 4 months) |
Con (Internet): n=117 Int (CHESSb): n=121 Mean age (years) 55.56 (range 18–84) Gender Male: 66 (28.2%) Female: 168 (71.8%) Race Not described |
Con: 43. 3% Int:45.8% | Int: Educational Con: Standard care plus a laptop computer with Internet access and a list of lung cancer and palliative care websites. | Not indicated | Home | RCT | Good |
| Holm et al. /Swed en [32] | Family caregivers to cancer patients in specialized palliative home care (having a prognosis longer than 5 weeks) | Con: n= 122 Int: n= 148 Mean age (years) Con: 60.0±14.3 Int: 63±13.4 Gender Male: 65 (33.5%) Female: 129 (66.5%) Race Not described |
Con: 27.9% Int: 39.9% | Int: Educational Con: Standard support from palliative settings | Theoretical framework of relatives’ involvement in palliative care | Home | RCT | Good |
| Psycho-educational support | ||||||||
| Hudson et al. /Australia [23,24] |
Primary family caregivers of patients with advanced cancer receiving home-based palliative care (within 2 weeks of referral) | Con: 148 Int 1 (one visit and three phone calls): 57 Int 2 (two visits and two phone calls): 93 Mean age (years) 59.0–13.9 (range 22–88) Gender Male: n = 85 (28.5%) Female: n = 207(69.5%) Unknown: n = 2 (0.7%) Race Not described |
Con: 48.6% Int 1: 45.6% Int 2: 43.0% | Int: Psychoeducational Con: Usual palliative care | Transaction al model of stress and coping | Home (home visits and phone calls) | RCT | Good |
| Hudson et al. /Australia [27] |
Caregivers of patients with advanced cancer receiving home-based palliative care (having a prognosis of several months) | N = 156 Mean age (years) 58.7±13.5 (range 20–84) Gender Male: n = 46 (30 %) Female: n = 109 (70%) Race Not described |
38% | Psychoeducational | Transaction al model of coping | Home- based palliative care service centers | Quasiexperimental study | Moderate |
| North ouse et al. /US [29] | Patients with advanced breast, colorectal , lung, or prostate cancer (stage III or IV, (having a prognosis of at least 6 months) and their primary family caregivers | Con: n= 163 Extensive Int: n= 162 Brief Int: n= 159 Mean age (years) 56.7±12.6 (range 18–88) Gender (caregivers) Male: 44.2% Female: 55.8% Race (dyads) Caucasian: 82.5% African- American: 13.5% Asian: 1.3% Multi-racial: 0.3% |
Con: 36.2% Extensi ve Int: 38.9% Brief Int: 37.7% |
Int: Psycho- educational Con: Usual care at the cancer center including medical treatment of cancer and symptom management | Stress-Coping Theory |
Home | RCT | Fair |
| Sun et al. /US [28] | Family caregivers of patients with non-small cell lung cancer (Stage IV, 57%) |
Con: n= 163 Int: n=203 (Stage IV: n = 209, 57% of total participants) Mean age (years) Con: 57.23±13.16 Int: 57.54±14.31 Gender(caregivers) Male: n = 139 (38%) Female: n = 227 (62%) Race (caregivers) American Indian n = 2 (0.5%) Asian: n = 41 (11.2%) Black or African American: n = 12 (3.3%) Native Hawaiian or other Pacific Islander: n = 11 (3.0%) White: n = 282 (77%) Other: n = 18 (4.9%) |
Con: 3.7% Int: 3.0% | Int: Psycho- educational Con: Usual care | Combined adult teaching principles, NCCN guidelines, IOM report, NCP guidelines, and the self-care concept |
Hospital | Quasi-experimentalstudy | Moderate |
| Walsh et al. /UK [34] | People who provided informal care to cancer patients newly referred to palliative care (median time to death: 12 weeks) | Con: n=134 Int: n=137 Mean age (years) 56.3±21.0 (range 16–92) Gender Male: n = 56 (21%) Female: n = 215 (79%) Race White: n = 232 (86%) Other: n = 39 (14%) |
Con: 59. 7% Int: 49.6% | Int: Psychoeducational Con: Usual palliative care | Not indicated | Outside of home or at the caregiver’s work place | RCT | Poor |
Abbreviations. Con (Control group); Int (Intervention group).
Cochrane RoB for RCT; ROBINS-I for quasi-experimental studies
The CHESS integrates services to facilitate coping by: (1) providing ready and organized access to information; (2) serving as a channel for communication and support with peers, experts, and users’ social networks; and (3) acting as an interactive coach by gathering information from the user, applying algorithms or decision rules, and providing feedback specifically relevant to the user.
Seven studies (64%) used interventions grounded in a theoretical framework: Smith’s stress and coping theory [23,24,27,29], Bandura’s self-efficacy theory [30], Jones’ self-determination theory [31], and Andershed and Ternestedt’s framework for family identity at the end of life [32]. Sun et al. developed a conceptual framework for the intervention study aimed at improving well-being through family caregiver self-care [28].
3.2. Population and Settings for Intervention
Five studies were conducted in the US [26,28,29,31,33] and two in Australia [23,24,27]. The remaining studies were conducted in Canada [25], Sweden [32], Singapore [30], and the UK [34]. In total, 2,369 participants were included in the 11 studies. In terms of a sample size, six studies had more than 200 participants, with two including 300 and 400 [28,29]. The mean age of participants ranged from 47 to 63 years, and the majority were Caucasian (77 – 93%) and female (56 – 79%). Most of the participants were spouses followed by adult children and parents. Three studies limited participants to caregivers whose patients had lung cancer [28,31,33], whereas the others included participants regardless of cancer type. In six studies, interventions were provided in a home-based setting (face-to-face or over the telephone) [23,24,26,29,31–33], whereas the others took place in an outpatient setting (clinic or home-based palliative care service center).
3.3. Interventions
The description of interventions is shown in Table 2 and include the unit of intervention, provider, length, time to follow-up, and measured outcomes for each study. Eight studies focused only on the caregivers [23–27,30,32–34] while three used the patient-caregiver dyad as the unit of care [28,29,31]. The studies for dyads presented caregiver outcomes distinctly, so that it was possible to extract caregiver-specific findings. Two studies tailored the intervention to patients and caregivers separately, reporting unique outcomes for both [29,31]. One study reporting on patients and caregivers separately utilized a delayed design to prevent treatment effect contamination [28]. Timing of the interventions varied across the disease trajectory. Five studies implemented interventions within a few months of diagnosis or palliative care referral [23,24,26,31,34,35]. Six studies recruited caregivers of patients with a specific prognosis, ranging from 5–24 weeks [25–27,29,32,33,36]. Two studies mentioned that they withheld interventions for caregivers of patients with poor functional status, as this was taken as an indication of imminent death [23,24,31].
Table 2.
Characteristics of interventions for family caregivers of patients with advanced cancer
| Author/Country | Intervention | Unit of Intervention | Intervention Provider | Dose/Duration | Follow-up | Outcomesa | Findings |
|---|---|---|---|---|---|---|---|
| Psychosocial support | |||||||
| Leow et al. /Singap ore [29] | A one-hour face-to-face session, a video clip, two follow-up phone calls, and an invitation to an online social support group. During the session, the caregivers viewed video and developed a care plan with the nurse researcher. | Family caregiver (individual) | Nurse | One hour (20-minute video and 40-minute discussion )/ 6 weeks | Week 4, and week 8 after intervention | QOL Stress and depression Self-efficacy in self-care | -QOL, self-efficacy in self-care↑ -Stress and depression ↓ |
| McDon ald et al. /Canad a [24] | Providing social support, emotional care, and providing resource to assist with care of the patient. Follow-up phone calls a week after each visit; 24-hr telephone support was provided by palliative care physicians. | Family caregiver (individual) | Physicians and nurses | Not indicated | Monthly for 4 months | QOL | -QOL (−) |
| Educational support | |||||||
| Badr et al. /US [30] | The 6-session, standardized, tailored manuals for patients and caregivers were provided (self-care, stress and coping, symptom management, effective communication, problem solving, and maintaining and enhancing relationships) and telephone counseling sessions | Patient/ Caregiver Dyad | A trained intervention ist who had a master’s degree in mental health counseling | 60- minutes, once a week/ 6 weeks | 8 weeks after intervention | Psychological functioning Caregiving burden Competence | - Depression, anxiety, and caregiver burden ↓ (p<0.001) -Caregiver competence ↑ (d≥1.2) |
| Dionne -Odom et al. / US [25] | One-on-one telephone sessions. Sessions addressed taking on the caregiver role, definition of palliative and supportive care, problemsolving, caregiver self-care, effective partnering in patient symptom assessment and management, building of a support them, decision making and support, and advance care planning | Family caregiver (individual) | An advanced- practice palliative care nurse | Once a week 23 minutes on average/ 3 weeks | Every 6 weeks until week 24 and then every 3 months thereafter until the patient’s death or study completion | QOL Depression Caregiving burden |
-Depression ↓ at 3 months (d = −.32, p = .02) in early group -Depression ↓ (d = −.39, p = .02) and stress burden ↓ (d = −.44, p = .01) in decedents’ caregiver of early group) |
| DuBens ke et al. /US [32] | In addition to standard care, received a laptop computer and Internet access and access to the CHESS lung cancer website. support with peers, experts, and users’ social networks | Family caregiver (individual) | E-health system +clinician team | 2 years or 13 months after patient death, whichever came first | Every 2 months | Caregiving burden Negative mood | -Burden ↓ (p=.021, d=.39), -Negative mood ↓ (p=.006,d=.44) |
| Holm et al. /Swede n [31] | Topics included palliative diagnoses and symptom relief, daily care and nutrition problems, and support and existential issues. | Family caregiver (individual) | Health care professionals | 2 hours, once a week/ 3 weeks | Upon completion of the intervention, and 2months afterwards | Competence Caregiving burden Anxiety and depression | -Competence ↑ (in short term) -Burden, anxiety and depression (−) |
| Psycho-educational support | |||||||
| Hudson et al. /Austral ia [22,23] | Each caregiver was allocated a Family Caregiver Support Nurse (FCSN) who assisted the local palliative care service to assess caregiver needs, establish a care plan and provide additional caregiver support. Step1: preparing caregivers for the intervention Step2: assessing caregiver needs and preparing a care plan Step3: reassessing needs and evaluating the care plan |
Family caregiver (individual) | Nurse | 4 weeks | -Time 1 (baseline): within 2 weeks of referral to palliative care -Time 2: 1- week postintervention (5 weeks postrecruitment) -Time 3: 8 weeks postpatient death to assess residual intervention effect | Psychological distress Competence | -Psychological well-being (−) -Unmet needs ↓ -Competence ↑ Intervention 2) -Less worsening in distress between times 1 and 3 in the one visiting intervention group than in the control group (0.28; t(150)=2.97, p=.003) |
| Hudson et al. /Austral ia [26] | Carer Group Education Program (CGEP) was based on the intervention, focusing the typical role of caregivers in the palliative care context, strategies for self-care and for their relative/friend, and strategies for caring for a person when death is approaching and bereavement supports. | Family caregiver (groups, 4–8 in a group) | Healthcare professionals (social workers or nurses) | Three sessions/ 1.5hours each/ 3 weeks | Commencement of the education program, immediately following the education, and 2 weeks flowing the final session. | Competence | -Competence ↑ (Time 1 to Time 2) and maintained throughout the follow up (n2 = .14 p < .01) |
| Northo use et al. /US [28] | FOCUS programb Brief FOCUS: three contacts (two 90-min home visits and one 30- min phone session) Extensive FOCUS: six contacts (four 90-min home visits and two 30- min phone sessions) | Patient/ Caregive r Dyad | Nurse | Brief program, 3.5 hours; extensive program, 7 hours/ 10 weeks | 3 months, 6 months | Risk of developing emotional distress Self-efficacy QOL | -Dyads’ coping (p<0.05), self-efficacy (p<0.05), and social QOL (p<0.01) and in caregivers’ emotional QoL (p<0.05) -Most effects were found at 3 months only. |
| Sun et al. /US [27] | Comprehensive baseline QoL assessment, present interdisciplinary care meeting with recommendations on symptom management and supportive-care referrals and available community resources, 4 Educational sessions with content categorized by the 4 QoL domains | Patient/ Caregive r Dyad | Interdisciplinary team | 4 education sessions (mean: 28 minutes) | 12 weeks after intervention | QOL Caregiving burden Psychological distress | *In the group of stage IV -QOL (Social well-being) ↑ (6.21 vs 6.44; p<.001) - Psychological distress ↓ (4.54 vs 4.23, p=.010), *In groups of all stages -Caregiver burden ↓ (p=.008) |
| Walsh et al. /UK [33] | A comprehensive assessment of domains of need was made; past, present, and future issues were discussed and advice, information and emotional support provided. The intervention was kept to giving advice and support rather than taking action on behalf of caregivers. Sometimes a telephone call took the place of a visit. | Family caregivers (individual) |
Two part-time caregiver advisors with experience in community nursing and social work | Once a week /6 weeks | 4 weeks, 9 weeks, and 12 weeks | Psychological distress Caregiver strain QOL | -Scores of psychological distress fell below the threshold of 5/6 in a third of participants in each trial arm at any follow- up point, but the difference was not significant. -No difference was observed in caregiver strain, QOL |
Only listed five most commonly measured outcomes (psychological distress, quality of life, caregiving burden, self-efficacy, and competence for caregiving)
FOCUS program: Family involvement, Optimistic attitude, Coping effectiveness, Uncertainty reduction, and Symptom management
The interventions could be categorized as psychosocial [25,30], educational [26,31–33], or both (psycho-educational) [23,24,28,29,34]. Two studies used psychosocial interventions [25,30]. McDonald et al. focused on providing caregivers with emotional care and resources to assist with care of the patient by having 24-hour telephone support available [25]. Leow et al. developed an intervention protocol that included information on signs of stress and burnout, self-care strategies, and management of emotions, such as anticipatory grief or frustration, along with making a care plan for caregivers themselves [36]. Four studies focused on educational/informational interventions to improve caregivers’ knowledge and preparedness for care of their patient [26,31–33]. Most interventions included information related to caregivers’ roles, symptom management, nutrition, or caregiving tips based on assessed needs. The remaining majority provided psychoeducational interventions [23,24,27,29,34]. Hudson et al. implemented an intervention providing educational resources to prepare caregivers for their role and including information tailored to each caregiver [23,24,27]. Their aim was to promote psychological wellbeing while also identifying positive aspects of their role and preparing for bereavement [23,24,27]. Northouse et al. conducted a dyadic intervention focusing on five content areas: family involvement, optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management [29]. Their intervention aimed to enhance participants’ abilities to maintain hope and reduce stress, while also satisfying informational needs [29].
The intensity, frequency, and duration of the interventions varied. The frequency of most interventions was generally weekly or every other week [26,31,32,34]. Some studies reported times of contact with participants [28–30], but others did not, only reporting the period of interventions [23–25,33,34]. The duration of the programs varied widely, ranging from three weeks, to two years, or until the patient’s death. Most intervention sessions lasted from 20 to 90 minutes, depending on the manner of delivering the intervention. Nurses provided interventions in five studies [23,24,26,29,30], while interdisciplinary teams were involved in the other six studies
3.4. Outcome Measures and Follow-up
Five main outcomes which had been measured most frequently in the reviewed studies were selected (i.e., psychological distress, quality of life, caregiving burden, self-efficacy, and competence for caregiving). Psychological distress includes each outcome of anxiety, depression, negative mood, or stress although those were measured distinctly according to its definition [37].
All studies evaluated interventions at multiple points. The follow-up assessments started anywhere from the intervention completion to four months, and the follow-up period ranged from two months to two years. One study assessed outcomes after the patient’s death to examine residual effects of the intervention [23,24].
3.5. Effects of Interventions
3.5.1. Psychological distress
Eight studies examined the effectiveness of interventions on psychological distress [23,24,26,28–31,33,34]. Most studies reported positive effects of interventions on decreasing psychological distress. One study found no difference in anxiety or depression between the intervention and control groups at two time-points—the intervention completion and two months after [32]. Two studies found no significant results at 4- and 8-month follow-ups [33,34]. Another study found that psychological distress worsened after the patient’s death, but was significantly lower in the intervention group versus the control, meaning the intervention mitigated the distress [23,24]. This result could be attributed to the fact that the last assessment was carried out during a bereavement phase, which could explain the increase in distress.
3.5.2. Quality of Life (QOL)
Quality of life was assessed in six studies [25,26,28–30,34], three of which showed positive outcomes related to efficacy of the interventions [28–30]. One study found significant improvement in a single QOL domain: physical or social domain [29]. In a dyadic intervention, significant improvement was found in caregivers’ emotional QOL in the intervention group over time (at 3-month and 6-month follow-ups) [29]. In contrast, no significant difference was found among patients in the study.
3.5.3. Caregiving burden
Four researcher teams found statistically significant results [26,28,31,33]. Specifically, those in the intervention group reported fewer problems with objective burden from caregiving roles or with perceived disturbance of the apparent aspects of their life [28]. Yet, the magnitude of effect was not consistent. One study examined the efficacy of a dyadic intervention among advanced lung cancer patients and found a large effect size (d=2.3) [31]. Another study examined the efficacy of e-health support on burden and found that the effect size was low (d=0.2) [33].
3.5.4. Self-efficacy and competence for caregiving
Self-efficacy and perceived competence are often viewed distinctly [38]; however, the reviewed studies used both interchangeably to mean perception of one’s ability to cope with stressful situations related to caregiving roles. Therefore, those are reported as the same in this study. The studies measuring self-efficacy/competence showed positive effects of the intervention, especially educational support, for caregivers [23,24,27,29–32]. Yet, the effect did not last long in that there were no significant improvements at 2 and 6 months [29,30,32]. All of these studies utilized various measures, making cross-study comparisons difficult.
3.6. Fidelity of intervention
Seven studies reported how the researchers accomplished fidelity of the interventions [23,24,26,29–32,34]. In most studies, a protocol or checklist was developed, and intervention providers received training to ensure consistency. In some of the studies, researchers utilized tape-recordings of each session to debrief and discuss adherence to protocols [26,29]. However, the extent of fidelity achieved was reported in only two studies, which found high levels of fidelity, 82.5–98.3% [29,31].
3.7. Study quality assessment
The overall risk of bias is presented in Table 1. Among the 9 RCTs, three studies were evaluated to have good quality [23,24,32,33] with two having fair quality [26,29]. Six RCTs adequately described the methods of randomization and allocation [23–25,30,32–34]. Outcome assessor blinding was reported in eight RCTs [23,24,26,29,30,32–34]. Although the attrition rates in most RCTs were quite high (0–59.7%), their missing outcome data balanced in numbers across intervention groups due to similar reasons (i.e., death of patient, deterioration of patient or follow-up loss). Regarding the nature of clinical environment and possible ethical issues in these studies, it is rarely possible to blind participants and key personnel to allocation. However, it can be assumed that the outcomes are not likely to be influenced by the lack of blinding as long as the effect of interventions is not diluted by contamination between the groups. Two of the quasi-experimental studies were appraised to have a moderate quality. The two studies are likely to be biased in deviations from intended intervention and in missing data [28], and in confounding factors [27], respectively.
4. Discussion and conclusion
4.1. Discussion
The primary aim of this review was to examine characteristics of interventions for family caregivers caring for people diagnosed with advanced cancer and to find gaps in the developed support programs. The review was particularly focused on care provided in the home to understand both the benefits and challenges of the interventions. In spite of the varying effectiveness and study quality, the interventions had positive effects on caregiver-specific outcomes. Specifically, the results consistently report that the interventions were effective in improving psychological distress, QOL, caregiving burden, self-efficacy, and competence for caregiving among the caregivers. These results suggest that caregiver support programs for psychosocial and educational care could ameliorate the negative impact of the caregiving role on caregivers’ wellbeing with respect to factors consistently found to increase strain and lead to poorer health outcomes [39–41].
The results of this review need to be compared with ones of a previous systematic review synthesizing findings from interventional studies of home palliative care for adults with advanced illness [13]. In comparison to patient outcomes showing beneficial effects of home palliative care in the review study, effects on caregiver outcomes were not significant or inconclusive; yet, the studies implementing home palliative care with an additional component of caregiver support (defined as “reinforced home palliative care” in the review) showed more favorable results. Although the beneficial effects were found in limited outcomes, there was evidence that adding the component of caregiver support led to caregivers feeling increased rewards from caregiving and improved distress. The comparison may justify providing support programs targeting caregivers of patients with advanced cancer along with the results of this present review.
In addition, several insights from the reviewed studies can be addressed through this review. First of all, the number of RCTs for support interventions that specifically focused on caregivers caring for patients with advanced cancer has been consistently increasing. In a review by Harding et al., among intervention studies for caregivers of patients with cancer with the publication dates limited from 2001 to 2010, nine RCTs were included [16], and another recent review by Chi included six more RCTs between 2004 and 2014, although it limited the inclusion criteria to educational and behavioral interventions [18]. In the present review, eight RCTs were newly included within the time period from 2007 to 2018 even with a limited population and study setting. Compared with an older review, which had been conducted by Harding et al. in 2003, the change is more obvious [17]. It contributed only two more RCTs of support interventions. This indicates that recognizing the need for and importance of supporting caregivers has been highlighted. In addition to the growth in the number of intervention studies presenting a higher level of evidence (RCTs), the increasing study sample sizes are significant. Seven studies had more than 200 participants, with two other studies including more than 300 participants. This shows a remarkable increase in sample size compared to Harding’s review in which only 27% of the included studies had more than 100 participants. However, the study quality should be scrutinized to see whether there has been improvement and whether previously identified gaps have been filled along with the quantitative growth.
Interventions in the reviewed studies were categorized into three types: psychosocial, educational, and psycho-educational support. The majority consisted of education, either only focusing on informational aspects or accompanying with psychological support. This may reflect that the support programs have weighted meeting caregivers’ informational/educational needs regarding the illness, patient symptoms, and decision making. As shown in the studies, fulfilling the informational needs through education or training for caregivers is likely to lead to positive outcomes, such as improved distress and burden, and competence for caregiving. For this reason, it is plausible that support interventions consisting of both psychosocial and educational components may be more effective to draw favorable outcomes despite the limitation that the efficacy of each intervention type could not be directly compared. Additionally, care for practical and respite care needs were also mentioned in numerous studies [42,43]. However, none of the interventions incorporated those types of support. In contrast to dementia caregiving, relatively little attention is paid to respite care in the cancer caregiving context. As having time away from the caregiving role may enhance physical abilities and reduce psychological distress, further research to examine the effect of practical support is warranted [44,45].
In terms of outcomes measured, the reviewed studies examined a wide range of endpoints using diverse measures, which prevents direct comparisons of the effectiveness of interventions across the studies. Support programs for caregivers are mostly provided holistically as the population tends to have various needs. However, as Harding et al. also argued, it is not desirable to apply a ‘scatter-gun’ approach in a limited time period [16]. Interventions focusing on specific aims and outcomes with some consensus are encouraged so that the effectiveness of interventions can be detected more clearly and allow further research, such as meta-analysis. As most psychological and educational interventions aim to enhance caregivers’ ability for care and cope with problems while maintaining their general health and QOL, future studies need to focus on these outcomes using consistent and reliable measures. Self-efficacy and perceived competence are often used interchangeably in the reviewed studies, as is common interventional studies aimed at promoting adaptive behavior patterns. Despite some points of theoretical congruence, the two concepts are distinct [38]. Self-efficacy is one’s confidence that they can carry out the behavior under challenging circumstances [46], while perceived competence is a one’s perception that they have capability of carrying out a behavior [47].
This review found that the published studies seldom considered physical health as a primary outcome but only as a component of QOL [25,32], although there has been reliable evidence that caregiving burden affects caregivers’ physical health [7,48,49]. Besides the lack of physical health related outcomes, there was no intervention study aimed at improving physical health in this review, despite no limited intervention types applied to the inclusion criteria. This is consistent with Harding’s review in which only one intervention study aiming to support caregiver’s physical health through yoga sessions was included [16]. Given the fact that caregivers’ health problems are related to patient health outcomes as well as burden of the health care system, more intervention research focusing on the effects on caregivers’ physical health problems is needed. Objective measurements could also be utilized to assess the outcomes. Although none of the reviewed studies conducted any biological assessments, these can allow for more reliable findings with participant-reported health outcomes and gather insights into mechanisms by which supportive care affects caregivers’ health outcomes, such as Interleukin-6 (IL-6) and D-dimer for cardiovascular diseases [50], salivary or hair cortisol for chronic stress [51,52], and C-reactive protein (CRP) for endocrine and immune consequences [53].
High attrition rates were noticed in the reviewed studies. The high rate of attrition is commonly problematic when trying to detect genuinely significant effects of interventions involving populations with advanced cancer. Due to the nature of the population, including disease progression and patient death, the challenge regarding and caregiver refusal to continue participation in interventions should be a part of the research. However, methodological research might be needed to find reasonable time points to start interventions and to determine duration of the study. Establishing consensus could help researchers support caregivers in a more appropriate timeframe with lessened burden for them to participate.
Furthermore, lessening the burden to participate may lead caregivers to continue longer in the study even after the patient’s death. Post-death support would allow researchers to track the interventional impacts more longitudinally to find out whether the supports for caregivers affect their bereavement positively. Considering that only one of the reviewed studies evaluated a residual effect of an intervention after the patient deaths [23,24], future research needs to include the evaluation of the effects of support programs on caregivers’ outcomes during a bereavement phase. As caregiver bereavement needs tend to be neglected and support for caregivers after the death of a loved one is generally lacking although bereaved caregivers tend to carry unresolved concerns [54,55], interventions to continuously support from a palliative phase to bereavement phase should be implemented and evaluated.
In terms of dyad studies, the reviewed studies, which had attempted to find interactive effects of dyadic interventions, showed inconsistent results in that some interventions were effective at improving outcomes in both patients and caregivers whereas others brought positive effects on outcomes in a group of caregivers only [29,31]. There is a need to acknowledge patients and caregivers that may have unique needs and possible unwillingness to share their concerns in the presence of each other. There may also be a need for more tailored interventions for patients and caregivers, respectively, while implementing more rigorous dyadic interventions for their shared needs which can be enhanced through the interaction as a unit of family.
It was disclosed that the intervention studies for caregivers of patients with advanced cancer mainly included Caucasians and English speakers. Chi et al. also indicated 60 – 80% of participants in the majority of the reviewed studies were Caucasians and emphasized the need for diverse caregivers to be recruited and targeted for interventions [18]. Recent research has shown that there is no racial/ethnic difference in access and utilization of palliative care services [56,57]. On the other hand, evidence showing disparities in access to the care across all health care settings also exists [58]. This might demonstrate growing needs for benefits from palliative care, which still do not appropriately meet the needs among minorities. Given the culture and beliefs which influence preferences and needs regarding supportive/palliative care among minority patients with advanced cancer and their families, future research particularly targeting specific racial and ethnic populations with cultural sensitivity is required.
There are a number of limitations in this systematic review. The possible reporting bias from the exclusion of grey literature, non-indexed journals, or articles in non-English languages should be considered. In addition, the reviewed studies used different types of study designs and methodological approaches so that it is difficult to compare results between studies and examine the level of evidence as a whole. This can compromise generalizability of the evidence. Lastly, the results of reviewed studies could have been biased by convenience sampling, high rate of attrition, and high risk of performance bias by participants and personnel.
4.2. Conclusion
In this review, regardless of the intervention type, support interventions for the family caregivers of patients with advanced cancer showed great potential for enhancing caregivers’ psychological symptoms, QOL, caregiving burden, self-efficacy, and competence for caregiving. However, the interpretation of the effectiveness was limited due to the inconsistency of measures used in the reviewed studies. Considering the increasing population of patients with cancer and their caregivers who encounter high caregiving demands, which can adversely affect their QOL and general health, more rigorous research is needed in order to achieve stronger evidence of the effectiveness of support programs for caregivers who are providing home care for patients with advanced cancer.
4.3. Research and practice implications
This review provides several implications for future research and practice. First, caregivers have unmet informational, psychological, and social support needs and could benefit from additional support. Second, regarding the strength of tailored interventions based on prior assessments, interventions should be more targeted to the specific needs of participants. Third, considering the lack of evidence about whether caregiver-focused interventions have the potential to yield long-term effectiveness for caregivers, research that tracks the effect of support interventions longitudinally is needed. Fourthly, as the concepts of self-efficacy and perceived competence are related but not synonymous, future researchers will need to unbundle these constructs to develop appropriate measures. Last but not least, acknowledging the growing need for support among minority groups and existing disparities in access to care, more research is needed to include diverse populations and develop more tailored interventions according to cultural contexts. Consideration of these would lead to improvement in quality of the intervention studies for caregivers caring for individuals with advanced cancer.
Highlights.
Most support interventions improve caregivers’ psychological outcomes.
Inconsistency in the use of measures exists.
There is a lack of support interventions for physical health needs of caregivers.
Caregiver outcomes should be assessed in a long-term period.
Further methodologically robust studies are still required.
Acknowledgements
We thank Lauren Catlett, MSN, RN, CNL for language editing on this paper.
Funding
This work was supported by a National Institutes of Health National Institute on Aging Research Supplement to Promote Diversity in Health-Related Research (NIH NIA 3R01AG047897-03S1, Dr. Rafael Romo).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
None declared.
References
- [1].National Alliance for Caregiving, Cancer Caregiving in the U.S.: An Intense, Episodic, and Challenging Care Experience, 2016. https://www.caregiving.org/wp-content/uploads/2016/06/CancerCaregivingReport_FINAL_June-17-2016.pdf (accessed September 29, 2019).
- [2].National Alliance for Caregiving, Caregiving in the U.S, 2015. https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf (accessed March 30, 2019).
- [3].Mcmillan SC, Interventions to Facilitate Family Caregiving at the End of Life, J. Palliat. Med 8 (2005) s-132–s-139. doi: 10.1089/jpm.2005.8.s-132. [DOI] [PubMed] [Google Scholar]
- [4].Ugalde A, Krishnasamy M, Schofield P, The relationship between self-efficacy and anxiety and general distress in caregivers of people with advanced cancer., J. Palliat. Med 17 (2014) 939–941. doi: 10.1089/jpm.2013.0338. [DOI] [PubMed] [Google Scholar]
- [5].Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G, Hidden morbidity in cancer: spouse caregivers., J. Clin. Oncol 25 (2007) 4829–34. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- [6].Ghesquiere A, Haidar YMM, Shear MK, Risks for complicated grief in family caregivers., J. Soc. Work End. Life. Palliat. Care 7 (2011) 216–240. doi: 10.1080/15524256.2011.593158. [DOI] [PubMed] [Google Scholar]
- [7].Kenny P, King MT, Hall J, The physical functioning and mental health of informal carers: evidence of care-giving impacts from an Australian population-based cohort, Health Soc. Care Community. 22 (2014) 646–659. doi: 10.1111/hsc.12136. [DOI] [PubMed] [Google Scholar]
- [8].Foley KM, The past and future of palliative care., Hastings Cent. Rep. Spec No (2005) S42–6. [DOI] [PubMed] [Google Scholar]
- [9].Guerriere D, Husain A, Zagorski B, Marshall D, Seow H, Brazil K, Kennedy J, Burns S, Brooks H, Coyte PC, Predictors of caregiver burden across the home-based palliative care trajectory in Ontario, Canada., Health Soc. Care Community 24 (2016) 428–438. doi: 10.1111/hsc.12219. [DOI] [PubMed] [Google Scholar]
- [10].Barton MK, Structured palliative care program found to be helpful for caregivers of patients with lung cancer, CA. Cancer J. Clin 66 (2016) 5–6. doi: 10.3322/caac.21297. [DOI] [PubMed] [Google Scholar]
- [11].Hudson P, Remedios C, Zordan R, Thomas K, Clifton D, Crewdson M, Hall C, Trauer T, Bolleter A, Clarke DM, Bauld C, Guidelines for the Psychosocial and Bereavement Support of Family Caregivers of Palliative Care Patients, J. Palliat. Med 15 (2012) 696–702. doi: 10.1089/jpm.2011.0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Higginson IJ, Sen-Gupta GJ, Place of care in advanced cancer: a qualitative systematic literature review of patient preferences., J. Palliat. Med 3 (2000) 287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- [13].Gomes B, Calanzani N, Curiale V, McCrone P, Higginson IJ, Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers, Cochrane Database Syst. Rev (2013). doi: 10.1002/14651858.CD007760.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Woodman C, Baillie J, Sivell S, The preferences and perspectives of family caregivers towards place of care for their relatives at the end-of-life. A systematic review and thematic synthesis of the qualitative evidence., BMJ Support. Palliat. Care 6 (2016) 418–429. doi: 10.1136/bmjspcare-2014-000794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW, Interventions with family caregivers of cancer patients: meta-analysis of randomized trials., CA. Cancer J. Clin 60 (2010) 317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Harding R, List S, Epiphaniou E, Jones H, How can informal caregivers in cancer and palliative care be supported? An updated systematic literature review of interventions and their effectiveness, Palliat. Med 26 (2012) 7–22. doi: 10.1177/0269216311409613. [DOI] [PubMed] [Google Scholar]
- [17].Harding R, Higginson IJ, What is the best way to help caregivers in cancer and palliative care? A systematic literature review of interventions and their effectiveness, Palliat. Med 17 (2003) 63–74. doi: 10.1191/0269216303pm667oa. [DOI] [PubMed] [Google Scholar]
- [18].Chi N-C, Demiris G, Lewis FM, Walker AJ, Langer SL, Behavioral and Educational Interventions to Support Family Caregivers in End-of-Life Care, Am. J. Hosp. Palliat. Med 33 (2016) 894–908. doi: 10.1177/1049909115593938. [DOI] [PubMed] [Google Scholar]
- [19].Moher D, Liberati A, Tetzlaff J, Altman DG, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement., PLoS Med. 6 (2009) e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hudson P, Payne S, Family carers in palliative care : a guide for health and social care professionals, Oxford University Press, 2009. [Google Scholar]
- [21].Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials., BMJ. 343 (2011) d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan A-W, Churchill R, Deeks JJ, Hrobjartsson A, Kirkham J, Juni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schunemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP, ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions., BMJ. 355 (2016) i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Hudson P, Trauer T, Kelly B, O’Connor M, Thomas K, Zordan R, Summers M, Reducing the psychological distress of family caregivers of home based palliative care patients: longer term effects from a randomised controlled trial., Psychooncology. 24 (2015) 19–24. doi: 10.1002/pon.3610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hudson P, Trauer T, Kelly B, O’Connor M, Thomas K, Summers M, Zordan R, White V, Reducing the psychological distress of family caregivers of home-based palliative care patients: short-term effects from a randomised controlled trial, Psychooncology. 22 (2013) 1987–1993. doi: 10.1002/pon.3242. [DOI] [PubMed] [Google Scholar]
- [25].McDonald J, Swami N, Hannon B, Lo C, Pope A, Oza A, Leighl N, Krzyzanowska MK, Rodin G, Le LW, Zimmermann C, Impact of early palliative care on caregivers of patients with advanced cancer: cluster randomised trial., Ann. Oncol. Off. J. Eur. Soc. Med. Oncol 28 (2017) 163–168. doi: 10.1093/annonc/mdw438. [DOI] [PubMed] [Google Scholar]
- [26].Dionne-Odom JN, Azuero A, Lyons KD, Hull JG, Tosteson T, Li Z, Li Z, Frost J, Dragnev KH, Akyar I, Hegel MT, Bakitas MA, Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients With Advanced Cancer: Outcomes From the ENABLE III Randomized Controlled Trial., J. Clin. Oncol 33 (2015) 1446–1452. doi: 10.1200/JCO.2014.58.7824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hudson P, Thomas T, Quinn K, Cockayne M, Braithwaite M, Teaching Family Carers About Home-Based Palliative Care: Final Results from a Group Education Program, J. Pain Symptom Manage 38 (2009) 299–308. doi: 10.1016/J.JPAINSYMMAN.2008.08.010. [DOI] [PubMed] [Google Scholar]
- [28].Sun V, Grant M, Koczywas M, Freeman B, Zachariah F, Fujinami R, Del Ferraro C, Uman G, Ferrell B, Effectiveness of an interdisciplinary palliative care intervention for family caregivers in lung cancer, Cancer. 121 (2015) 3737–3745. doi: 10.1002/cncr.29567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, LoRusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL, Kershaw T, Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers., Psychooncology. 22 (2013) 555–63. doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, Hull JG, Li Z, Tosteson TD, Byock IR, Ahles TA, Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial., JAMA. 302 (2009) 741–749. doi: 10.1001/jama.2009.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Badr H, Smith CB, Goldstein NE, Gomez JE, Redd WH, Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: Results of a randomized pilot trial., Cancer. 121 (2015) 150–158. doi: 10.1002/cncr.29009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Holm M, Årestedt K, Carlander I, Fürst C, Wengström Y, Öhlen J, Alvariza A, Short-term and long-term effects of a psycho- educational group intervention for family caregivers in palliative home care—Results from a randomized control trial., Psychooncology. 25 (2016) 795–802. doi: 10.1002/pon.4004. [DOI] [PubMed] [Google Scholar]
- [33].DuBenske LL, Gustafson DH, Namkoong K, Hawkins RP, Atwood AK, Brown RL, Chih M-Y, McTavish F, Carmack CL, Buss MK, Govindan R, Cleary JF, CHESS improves cancer caregivers’ burden and mood: Results of an eHealth RCT., Heal. Psychol 33 (2014) 1261–1272. doi: 10.1037/a0034216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Walsh K, Jones L, Tookman A, Mason C, McLoughlin J, Blizard R, King M, Reducing emotional distress in people caring for patients receiving specialist palliative care, Br. J. Psychiatry 190 (2007) 142–147. doi: 10.1192/bjp.bp.106.023960. [DOI] [PubMed] [Google Scholar]
- [35].Northouse L, Williams A-L, Given B, McCorkle R, Psychosocial care for family caregivers of patients with cancer., J. Clin. Oncol 30 (2012) 1227–34. doi: 10.1200/JCO.2011.39.5798. [DOI] [PubMed] [Google Scholar]
- [36].Leow M, Chan S, Chan MF, A pilot randomized, controlled trial of the effectiveness of a psychoeducational intervention on family caregivers of patients with advanced cancer, Oncol. Nurs. Forum 42 (2015) E63–E72. doi: 10.1188/15.ONF.E63-E72. [DOI] [PubMed] [Google Scholar]
- [37].Drapeau A, Marchand A, Beaulieu-Prevost D, Epidemiology of Psychological Distress, in: Ment. Illnesses - Understanding, Predict. Control, InTech, 2012. doi: 10.5772/30872. [DOI] [Google Scholar]
- [38].Rodgers WM, Markland D, Selzler A-M, Murray TC, Wilson PM, Distinguishing perceived competence and self-efficacy: an example from exercise., Res. Q. Exerc. Sport 85 (2014) 527–39. doi: 10.1080/02701367.2014.961050. [DOI] [PubMed] [Google Scholar]
- [39].Lohne V, Miaskowski C, Rustøen T, The relationship between hope and caregiver strain in family caregivers of patients with advanced cancer., Cancer Nurs. 35 (2012) 99–105. doi: 10.1097/NCC.0b013e31821e9a02. [DOI] [PubMed] [Google Scholar]
- [40].Trevino KM, Prigerson HG, Maciejewski PK, Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder, Psychooncology. 27 (2018) 243–249. doi: 10.1002/pon.4441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kehoe LA, Xu H, Duberstein P, Loh KP, Culakova E, Canin B, Hurria A, Dale W, Wells M, Gilmore N, Kleckner AS, Lund J, Kamen C, Flannery M, Hoerger M, Hopkins JO, Liu JJ, Geer J, Epstein R, Mohile SG, Quality of Life of Caregivers of Older Patients with Advanced Cancer, J. Am. Geriatr. Soc 67 (2019) 969–977. doi: 10.1111/jgs.15862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hudson P, Positive aspects and challenges associated with caring for a dying relative at home., Int. J. Palliat. Nurs 10 (2004). doi: 10.12968/ijpn.2004.10.2.12454. [DOI] [PubMed] [Google Scholar]
- [43].Goldschmidt D, Schmidt L, Krasnik A, Christensen U, Groenvold M, Expectations to and evaluation of a palliative home-care team as seen by patients and carers, Support. Care Cancer 14 (2006) 1232–1240. doi: 10.1007/s00520-006-0082-1. [DOI] [PubMed] [Google Scholar]
- [44].MacDonald G, Massage as a respite intervention for primary caregivers, Am. J. Hosp. Palliat. Med 15 (1998) 43–47. doi: 10.1177/104990919801500109. [DOI] [PubMed] [Google Scholar]
- [45].Barrett M, Wheatland B, Haselby P, Larson A, Kristjanson L, Whyatt D, Palliative respite services using nursing staff reduces hospitalization of patients and improves acceptance among carers., Int. J. Palliat. Nurs 15 (2009) 389–395. doi: 10.12968/ijpn.2009.15.8.43798. [DOI] [PubMed] [Google Scholar]
- [46].Bandura A, Social foundations of thought and action: A social cognitive theory., Prentice-Hall, Inc, Englewood Cliffs, NJ, US, 1986. [Google Scholar]
- [47].Deci EL, Ryan RM, The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior., Psychol. Inq 11 (2000) 227–268. doi: 10.1207/S15327965PLI1104_01. [DOI] [Google Scholar]
- [48].Haley WE, LaMonde LA, Han B, Narramore S, Schonwetter R, Family caregiving in hospice: effects on psychological and health functioning among spousal caregivers of hospice patients with lung cancer or dementia., Hosp. J 15 (2001) 1–18. [DOI] [PubMed] [Google Scholar]
- [49].Pinquart M, Sörensen S, Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis., Psychol. Aging 18 (2003) 250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- [50].Moore RC, Chattillion EA, Ceglowski J, Ho J, von Känel R, Mills PJ, Ziegler MG, Patterson TL, Grant I, Mausbach BT, von Kanel R, Mills PJ, Ziegler MG, Patterson TL, Grant I, Mausbach BT, A randomized clinical trial of Behavioral Activation (BA) therapy for improving psychological and physical health in dementia caregivers: results of the Pleasant Events Program (PEP)., Behav. Res. Ther 51 (2013) 623–632. doi: 10.1016/j.brat.2013.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, Lehman B, Moscoso MS, Kadel R, Le N, Loftus L, Stevens CA, Malafa MP, Shelton MM, A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers., J. Holist. Nurs 30 (2012) 170–185. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- [52].Chen X, Gelaye B, Velez JC, Barbosa C, Pepper M, Andrade A, Gao W, Kirschbaum C, Williams MA, Caregivers’ hair cortisol: a possible biomarker of chronic stress is associated with obesity measures among children with disabilities., BMC Pediatr. 15 (2015) 9. doi: 10.1186/s12887-015-0322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Lovell B, Moss M, Wetherell M, The psychosocial, endocrine and immune consequences of caring for a child with autism or ADHD., Psychoneuroendocrinology. 37 (2012) 534–542. doi: 10.1016/j.psyneuen.2011.08.003. [DOI] [PubMed] [Google Scholar]
- [54].Hudson P, Improving support for family carers: Key implications for research, policy and practice, Palliat. Med 27 (2013) 581–582. doi: 10.1177/0269216313488855. [DOI] [PubMed] [Google Scholar]
- [55].Boerner K, Schulz R, Caregiving, bereavement and complicated grief, Bereave. Care 28 (2009) 10–13. doi: 10.1080/02682620903355382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Worster B, Bell DK, Roy V, Cunningham A, LaNoue M, Parks S, Race as a Predictor of Palliative Care Referral Time, Hospice Utilization, and Hospital Length of Stay: A Retrospective Noncomparative Analysis., Am. J. Hosp. Palliat. Care 35 (2018) 110–116. doi: 10.1177/1049909116686733. [DOI] [PubMed] [Google Scholar]
- [57].Sharma RK, Cameron KA, Chmiel JS, Von Roenn JH, Szmuilowicz E, Prigerson HG, Penedo FJ, Racial/Ethnic Differences in Inpatient Palliative Care Consultation for Patients With Advanced Cancer., J. Clin. Oncol 33 (2015) 3802–3808. doi: 10.1200/JCO.2015.61.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Johnson KS, Racial and ethnic disparities in palliative care., J. Palliat. Med 16 (2013) 1329–1334. doi: 10.1089/jpm.2013.9468. [DOI] [PMC free article] [PubMed] [Google Scholar]


