Summary
Background
The WHO estimates 10–30% of hospital admissions are associated with poor infection prevention and control (IPC). There are no reliable data on IPC status in Tanzanian healthcare facilities; hence the Star Rating Assessment (SRA) was established to address this. This study compared the health facility performances on adherence to IPC principles using baseline and reassessment data of SRA.
Methods
A retrospective analysis of data from eight randomly selected regions across Tanzania. Data was gathered from an SRA database in which records of baseline assessments (2015/16) and reassessments (2017/18) were documented. Each healthcare facility's ownership and service level were investigated as independent variables.
Results
A total of 2,131 healthcare facilities at baseline and 2,185 at reassessment were analysed. Median adherence to IPC principles increased from 31% (IQR: 20%, 46%) to 57% (IQR: 41.4%, 73.2%) after interventions (p<0.001).
Privately-owned facilities had higher adherence to IPC principles compared to publicly-owned facilities during baseline (p<0.001) however, the difference was not significant after intervention (p=0.751). On average, hospitals scored highest followed by health centres and then dispensaries during both assessments.
Being a privately-owned facility was a predictor of attaining a recommended IPC score of 80% at baseline (POR=1.92 CI=1.06–3.48) but not after the intervention. Facility level was not a predictor during baseline assessment; however after intervention hospitals were twice as likely to attain the recommended score compared to dispensaries (POR=2.27 CI=1.15–4.45).
Conclusion
Assessment and rating of quality and organization of health services plus management support to healthcare facilities, leads to improved adherence to IPC principles.
Keywords: Star Rating Assessment, Primary healthcare facilities, Quality improvement, Infection prevention and control
Introduction
Infection prevention and control (IPC) is defined as a scientific approach and practical solution designed to prevent harm caused by infection to patients and health workers. [1] The World Health Organization (WHO) estimates 10–30% [2] of all admissions result in healthcare-associated infections (HAIs) and 1.4 million people at any given time have HAIs. [3].
The magnitude of HAIs in developing countries is usually underestimated or unknown because the diagnosis of HAIs is complex and experts and resources needed in surveillance activities to guide interventions are inadequate. [2,4] The problem in resource-constrained countries is three to twenty times greater, compared to developed ones. [5] HAIs are responsible for excess deaths, long term disability, additional financial burden and cost to the government, patients and families. [2,6] In Africa, the prevalence of HAI varies between 2.5% and 14.8%. [2,7] An earlier study in Tanzania revealed an overall prevalence of 14.8% [8], making it one of the most affected countries in Africa.
Currently, there are no reliable data on IPC in Tanzania. However in 2014, the Ministry of Health (in collaboration with the President's Office, Regional Administration, Local Government and other stakeholders) developed a Star Rating Assessment (SRA) initiative as part of the “Big Results Now” implementation in the health sector. [9,10] The SRA initiative aimed at assessing all the primary healthcare facilities across the country and assign a star rating according to the quality of services provided based on a set of tools for dispensaries, health centres, and level 1 hospitals. [9].
The SRA tool is arranged into 12 service areas, which are: Legality (Licensing and Certification), Health Facility Management, Use of Facility Data for Planning and Service Improvement, Staff Performance Assessment, Organization of Services, Handling Emergencies and Referral, Client Focus, Social Accountability, Facility Infrastructure, Infection Prevention and Control (IPC), Clinical Services, and Clinical Support Services. The service areas are defined in Table I.
Table I.
Definitions of the 12 Assessment Areas used during Star Rating Assessments of 2015/16 and 2017/18 in Tanzania
| Assessment area | Percentage points for assessment area | Definition of the area | |
|---|---|---|---|
| 1 | Legality (Licensing and Certification), | 0a | Facilities were supposed to be legally registered and have a license to provide service |
| 2 | Health Facility Management | 10 | Availability of skilled healthcare workers, organization structure, staff attendance, Health Facility Management Teams (HFMTs) and Quality Improvement Teams (QITs), facility planning and budgeting, operating bank accounts and housing and housing allowances |
| 3 | Use of Facility Data for Planning and Service Improvement | 5 | Availability and proper use of Health Management Information Systems (HMIS), use of data for planning, and medical records |
| 4 | Staff Performance Assessment | 5 | Availability of staff open performance review and appraisal system (OPRAS) and job descriptions |
| 5 | Organization of Services | 10 | Proper flow of services in each of the service points from entry to exit, display of services provided and prices, and health promotion and outreach services. |
| 6 | Handling Emergencies and Referral | 5 | Availability of emergency medicines and equipment, staff training on emergency and proper referral system. |
| 7 | Client Focus | 5 | Availability of proper mechanisms for handling clients' complaints such as suggestion box, client help desk, display of contact details for phone or SMS feedback. |
| 8 | Social Accountability | 10 | Partnership between the health facility and community and participation of community through Health Facility Governing Committees (HFGC). |
| 9 | Facility Infrastructure | 10 | Presence of Planned Preventive Maintenance (PPM), the status of the buildings, amenities (electricity and water), disability friendly facilities and adequacy of furniture and equipment in each of the service delivery points. |
| 10 | Infection Prevention and Control (IPC) | 10 | Adherence to proper ways of implementing IPC in health facilities such as the use of PPE, PEP, standard base precautions, processing equipment, laundry services, and healthcare waste management. |
| 11 | Clinical Services | 15 | Proper adherence to treatment guidelines and RMNCH services |
| 12 | Clinical Support Services | The clinical support services included Pharmaceutical services, Laboratory, Radiology and Imaging, Operating Theatre, Food Services, and Mortuary. |
Source: SRT for Dispensary, Health Centre and Hospitals at Council level (2015).
No score was provided for this area, however, for the facilities found unregistered; authorities were informed to close the facility pending legal procedures.
The tenth service area of IPC is routinely affected by non-adherence with poor standard precautions, improper handling of healthcare waste, lack of training and knowledge on IPC, understaffing and overcrowding, improper antibiotic use and lack of microbiological information, low-risk perception and financial constraints to handle IPC related health needs. [4,11,12].
The SRA uses the certification system to assess and rate technical aspects of quality, organization of services and assessment of management and governance at healthcare facilities. It is used to develop facility-specific quality improvement (QI) plans based on gaps identified from the assessment. The performance on adherence to IPC by the SRA across different primary healthcare facilities has rarely been documented and compared with different timelines. The SRA was conducted in 6,993 primary healthcare facilities (public and private) between 2015 and 2016. Of the assessed facilities; 219 were hospitals, 741 were health centres, 6,030 were dispensaries and 3 were unrecorded healthcare facilities. As per results obtained; reassessment was done between 2017 and 2018 whereby 6,243 dispensaries, 799 health centres and 247 hospitals were assessed (a total of 7,289 health facilities). [9] During assessments; data were collected using SRA tools and then the scores from the tools were transcribed into Excel spreadsheets.
The main objective of the study was to compare the SRA IPC performance scores of primary healthcare facilities using the data from baseline assessment (2015/2016) and reassessment (2017/2018). Specifically, to measure:
-
•
the average adherence to IPC principles during SRAs;
-
•
the difference in adherence to IPC principles between baseline assessment and reassessment;
-
•
the association between attaining a recommended IPC status and the characteristics of a healthcare facility; and
-
•
(assess) any spatial distribution of adherence to IPC performance during SRAs.
Methods
Study design
A retrospective analytical study of adherence to IPC principles by ownership and service level of healthcare facilities was performed. Data was gathered from the database produced during baseline SRA held in fiscal year 2015/2016. The database was used in subsequent supportive supervision and during the reassessment in fiscal year 2017/2018.
Study population
All healthcare facilities which were assessed during baseline and reassessment were included in the study population and were units of analysis. [9,13].
Intervention
The SRA system set criteria for minimum standards of quality of care needed to be achieved by all primary healthcare facilities. The performance of the facilities was rated from zero to five stars. [9] Facilities scoring 60% and above in all the four domains (management of health facility and staff performance; fulfilment of services charters and accountability; safe and conducive facilities; and quality of care) were regarded as good performers, while those scoring below 20% in any of the domains were considered unsafe and unfit for providing services and were advised to be closed. [9] Development of a stepwise certification and accreditation system and linkage of quality of service provided by these facilities to insurance payments was designed to enhance compliance with Standard Operating Procedures (SOPs) and healthcare standards. Healthcare facilities scoring below 20% were supported by respective Local Governments to bring them up to the desired standard, such support included (but was not limited to) refurbishment of infrastructure, recruitment of additional staff, training, mentoring and supportive supervision.
Supervision sessions were conducted quarterly by Council Health Management Teams (CHMTs) equally to all facilities to assess the implementation of facilities' Quality Improvement Plans (QIPs). [14] Healthcare facility management teams and staff performance were continually assessed to enhance accountability to social and local government structures. [15] Also, the SRA system set a target for the Tanzanian health system performance, in which the goal was by the end of the fiscal year 2017/18, 80% of primary health care facilities to be rated three star (60–79% in all domains) or above. [9,15].
Target population
All operating primary healthcare facilities in the Council (dispensaries, health centres and level 1 hospitals [i.e.at Council level]) regardless of their ownership, i.e., public (Local Government Authority, military, police, prisons, parastatals and other ministries, departments and agencies) or private (faith-based organisations, private for-profit).
Inclusion criteria
All facilities which participated in baseline assessment in fiscal year 2015/17 or reassessment in 2017/18; whose performance and characteristics were able to be identified from SRA database.
Exclusion criteria
Facilities which did not participate in both assessments were excluded during comparison analysis.
Sampling procedure
Tanzania mainland has 26 regions and 8 zones. Using simple probability sampling, one region from each zone was selected. All facilities in the selected regions were included in the analysis.
Data sources and collection
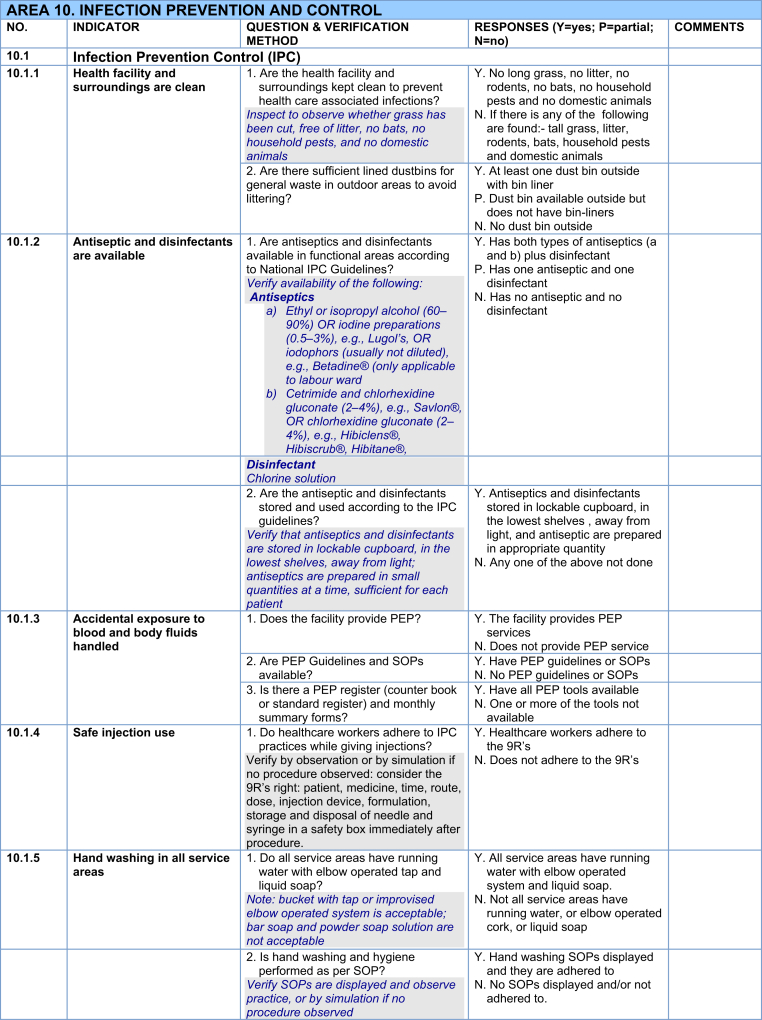
The SRA tool is divided into 12 service areas; each with different weight ranging from 5% to 15% (to total 100%). [9] The IPC service area had 10% weight. As depicted in Table II, the IPC service area was further divided into 11 indicators. Questions were used to assess the indicators. Each question had up to three responses: ‘Yes’ (score=1) or ‘No’ (score=0) or ‘Partial’ (score=0.5). The sum scored was divided by the maximum possible score for the questions, times by 100 to give the percentage score for the indicator. The sum of percentages scored from each indicator then made up the scores in the IPC quality assessment area. QIPs were formulated from indicators which did not attain full scores.
Table II.
Description of the 11 indicators of IPC and how were assessed and scored in primary healthcare facilities in Tanzania for both baseline (2015/16) and reassessment (2017/18).
During assessments, data collection from each healthcare facility was done by using the SRA tools and the scores were entered in MS Excel spreadsheet which produced scores per service area, including IPC. The data from sheets were cleaned and compiled at district level immediately to ensure correctness, accuracy and timeliness of the information. A database at the national level was managed by Health Services Inspectorate and Quality Assurance Section of the then Health Quality Assurance Division, which is currently Health Quality Assurance Unit (HQAU) of the Ministry responsible for health. [16] Data was presented as aggregate percentage scores at the level of service areas for each healthcare facility assessed. The database grouped districts' Excel sheets into respective administrative regions to form a regional scorecard. There were 185 district councils in 26 Tanzanian mainland regions. The 26 regions are further grouped in 8 zones.
For the current study, eight regions (consisting of 51 districts) from all of the country's 8 zones were involved. These were selected through simple random sampling carried out by the IPC sub-unit of HQAU (where one region from a list of regions in each specific zone was drawn).
Each region had two scorecards, one for baseline assessment and another for the reassessment; therefore there was a total of 16 regional scorecards for 8 regions. Before analysis, data were coded and filtered based on healthcare facility service level, type of ownership and name of the district the facility belongs to.
Study variables
The independent variables studied were; facility ownership status and healthcare facility service level. The outcome variables were baseline assessment rate and reassessment rate.
Data management and analysis
Adherence to IPC principles was assessed and rated based on 11 pre-determined indicators; namely cleanliness of healthcare facility and surroundings, availability of antiseptics and disinfectants, handling of accidental exposure to blood and body fluids, use of safe injection, availability of handwashing facilities in all service areas and instrument sterilisation or high-level disinfection. Others were the use of personal protective equipment, laundry services, healthcare waste disposal facilities, training of staff on healthcare waste management and availability of waste segregation equipment and supplies.
Scores for IPC were tested for normality by using the Shapiro-Wilk test. Descriptive analysis was performed to compare adherence to IPC principles based on different characteristics of healthcare facilities. For comparison analysis, only facilities involved in both baseline and reassessment were included. We used a Wilcoxon signed-rank test for related samples to determine whether the differences between baseline IPC performance and reassessment were statistically significant. Comparisons for unrelated samples were performed using a Mann-Whitney U test or a Kruskal-Wallis test. The Mann-Whitney U test was used to compare differences between private and public scores in IPC during baseline and reassessment while Kruskal-Wallis test was used to determine whether there was a significant difference in performance scores across different healthcare facility service levels (i.e. dispensaries, health centres and hospitals) at baseline and reassessment. Healthcare facilities which scored below 80% were considered as poorly compliant to IPC principles while those scoring 80% and above were considered as compliant to the principles. The used cut-off points were provided by the National Guidelines for Recognition of Implementation Status of Quality Improvement Initiatives in Health Facilities. [17].
Data analysis was done using Epi Info version 7.2.2.6 [18]. Descriptive statistics, tables and charts were used to summarize the data. Logistic regression was used to determine the association between attaining recommended IPC status and independent variables; results were considered significant at p < 0.05. GIS software version 2.8.6 was used to display the spatial distribution of IPC performance per districts under study.
Results
Description of the healthcare facilities
We analysed 2,131 healthcare facilities from the baseline assessment data set. Out of these facilities, 55 (2.6%) were hospitals, 187 (8.8%) were health centres, 1,699 (79.7%) were dispensaries and 190 (8.9%) had unrecorded status. Based on the type of ownership; 1,566 (73.5%) were public facilities and 397 (18.6 %) were privately owned.
From reassessment data sets, we included 2,185 healthcare facilities of which 56 (2.6%) were hospitals, 220 (10.1%) health centres and 1,909 (87.4%) were dispensaries. Based on the type of ownership; 1,731 (79.2%) were public facilities and 454 (20.8%) were privately owned. Details are summarized in Table III. Total districts involved were 51 from eight regions falling within all eight zones of the country.
Table III.
Characteristics of healthcare facilities at baseline assessment (2015/16) and reassessment (2017/18) in Tanzania
| Baseline assessment (2015/2016) |
Reassessment (2017/18) |
|||
|---|---|---|---|---|
| Variable | Number | Percentage (%) | Number | Percentage (%) |
| Health Facility Level | ||||
| Dispensary | 1699 | 79.7 | 1909 | 87.4 |
| Health Centre | 187 | 8.8 | 220 | 10.1 |
| Hospital | 55 | 2.6 | 56 | 2.6 |
| Unrecorded | 190 | 8.9 | 0 | 0.0 |
| Total | 2,131 | 100.0 | 2185 | 100.0 |
| Ownership status | ||||
| Public | 1566 | 73.5 | 1731 | 79.2 |
| Private | 397 | 18.6 | 454 | 20.8 |
| Unrecorded | 168 | 7.9 | 0 | 0.0 |
| Total | 2131 | 100.0 | 2185 | 100.0 |
Adherence to IPC principles during Star Rating baseline and re-assessment
The median score of adherence to IPC principles was found to be 31.0% (IQR: 20%, 46%) and 56.6% (IQR: 41.4%, 73.2%) during baseline assessment and reassessment respectively.
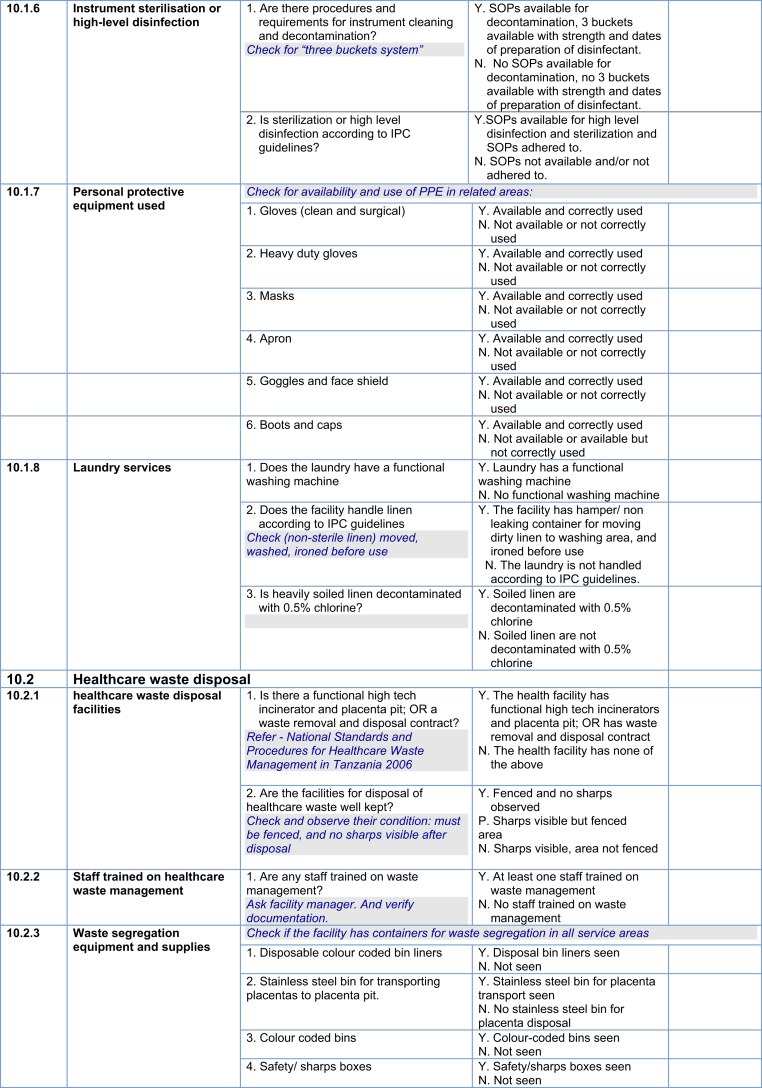
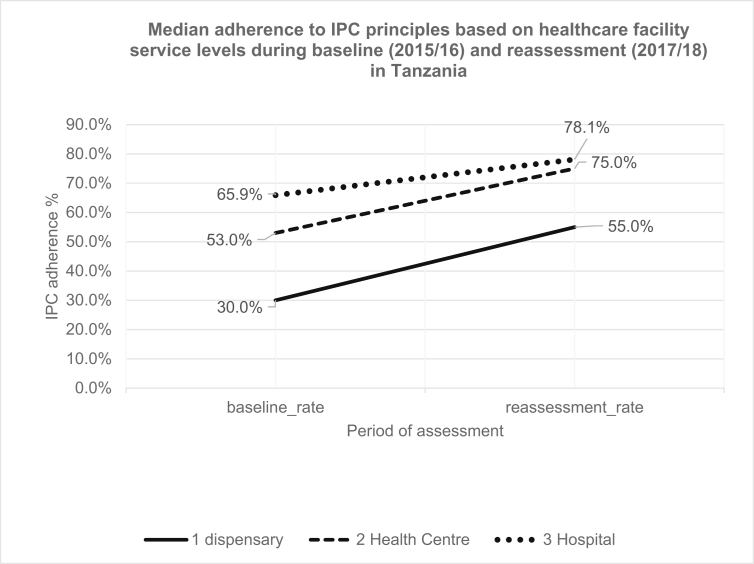
Of all facilities analysed, 1,908 qualified for comparison tests for baseline assessment and reassessment. As Table IV shows, the distribution of IPC scores during baseline and reassessment was statistically different (p<0.001). Figure 1, Figure 2 show the trends in median adherence to IPC principles among different characteristics of healthcare facilities.
Table IV.
Adherence to IPC principles based on characteristics of healthcare facilities during Baseline (2015/16) and Reassessment (2017/18) in Tanzania
| Baseline assessment median, (range) |
P-value | Reassessment median, (range) |
P-value | |
|---|---|---|---|---|
| All facilities (n=1908) | 31.0% (0,100%) | 56.6 % (0,100%) | <0.001a | |
| facility service level | ||||
| Dispensaries | 30.0% (0,100%) | 0.018c | 55.0% (0,100%) | 0.090c |
| Health centre | 53.0% (0,100%) | 75.0% (0,100%) | ||
| Hospital | 65.9% (15, 97%) | 78.1% (0,100%) | ||
| Facility ownership | ||||
| Public | 29.0% (0, 93%) | <0.001b | 56.7% (0,100%) | 0.751b |
| Private | 45.0% (0,100%) | 58.7% (0,100%) | ||
| Unrecorded | 27.0% (0, 71%) | 0 (0,0) | ||
values calculated using Wilcoxon Signed-Ranks.
Mann-Whitney U test for comparison of values.
Kruskal-Wallis test for comparison of values.
Figure 1.
Median Adherence to IPC principles based on Health Facility Service Levels during Baseline (2015/16) and Reassessment (2017/18) in Tanzania.
Figure 2.
Median Adherence to IPC Based Facility Ownership Status during Baseline (2015/16) and Reassessment (2017/18) in Tanzania.
There was a significant difference in IPC adherence among public and privately owned healthcare facilities during baseline assessment (p <0.001, Mann Whitney U); however the significance was lost during reassessment (p =0.751, Mann Whitney U). Furthermore, the analysis showed the significant difference in IPC adherence across different healthcare facility service levels (i.e. hospitals, health centres and dispensaries) at baseline assessment (p =0.018, Kruskal-Wallis); however, the significance was lost during the reassessment (p =0.090, Kruskal-Wallis) as it is presented in Table IV.
The association between attaining a recommended IPC status and characteristics of healthcare facilities
The association between ownership status and IPC performance status were tested separately for baseline and reassessment. The findings showed a significant association between ownership status and IPC performance status during baseline assessment whereby private facilities had nearly two times the odds of achieving a recommended IPC status compared to public ones [POR=1.92, CI (1.06–3.48) p=0.031]. On the other hand, there was no significant association between ownership status and recommended IPC status during re-assessment [POR= 1.10, CI (0.79–1.53) p= 0.55].
Furthermore, the association between healthcare facility service level and attaining of IPC performance status was tested for both baseline and reassessment. There was no significant association between healthcare facility service level and attaining recommended IPC status during baseline assessment. At this time, hospitals were 67% more likely to achieve recommended status compared to dispensaries [POR=1.67, CI (0.39–7.11), p=0.487), and 4% more likely to achieve recommended status when compared to health centres [POR=1.04, CI=0.21–5.20, p=0.99]. During the reassessment period, a significant association was observed between healthcare facility level and attaining recommended IPC status considering hospital level as a reference [POR=2.27, CI=1.15–4.45, p=0.018]; but not with health centre level [POR=1.69, CI=0.79–3.67, p=0.178]. The above results are presented in Table V.
Table V.
Association of healthcare facility characteristics and attaining of recommended IPC status during baseline (2015/16) and reassessment (2017/18) in Tanzania
| Variable |
Baseline assessment |
Reassessment |
||||
|---|---|---|---|---|---|---|
| Facility service level | Good n=55 | Poor n=1853 | POR (95%CI) |
Good n=276 | Poor n=1632 | POR (95%CI) |
| Dispensary | 46 | 1653 | 1.67 (0.39–7.11) |
235 | 1464 | 2.27 (1.15–4.45)∗ |
| Health centre | 7 | 157 | 1.04 (0.21–5.20) |
29 | 135 | 1.69 (0.79–3.67) |
| Hospital | 2 | 43 | 1 | 12 | 33 | 1 |
| Facility Ownership | ||||||
| Private | 16 | 326 | 1.92 (1.06–3.48)∗ |
53 | 289 | 1.10 (0.79–1.53) |
| Public | 39 | 1527 | 1 | 223 | 1,343 | 1 |
POR Prevalence Odds Ratio ∗(P < 0.05).
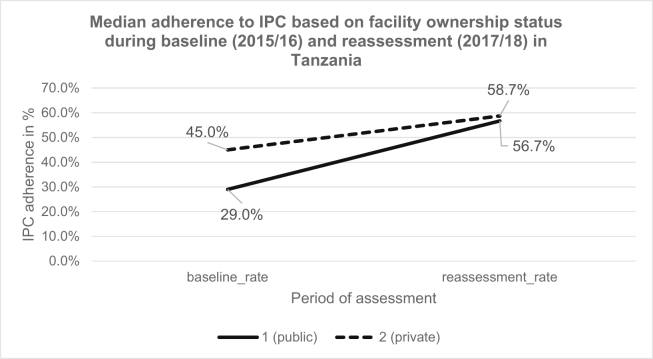
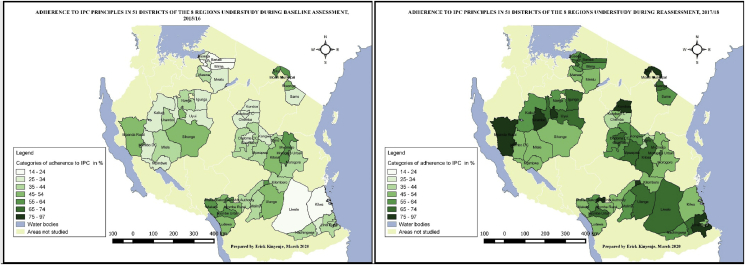
Spatial distribution of adherence to IPC principles per district understudy during SRAs
Representation of adherence to IPC principles by districts understudy before and after the intervention is presented in Figure 3 whereby worst performance was observed in Kilwa district (14%) during baseline and Chemba district (41%) during reassessment. The best adherence was observed from Moshi District (66%) during baseline and Kondoa district (84%) during reassessment. Over the intervention period, the average performance dropped at three districts; namely Sikonge, Makete and Mvomero. While none of the 51 districts attained the recommended average performance of 80% during baseline [17]; seven districts attained the scores during the reassessment period.
Figure 3.
Geographical representation of adherence to IPC principles by time of assessment and District in 51 Districts of 8 Regions Understudy.
Discussion
Our study in Tanzania demonstrates an increasing IPC adherence from baseline 31% (IQR: 20%, 46%) to 57% (IQR: 41.4%, 73.2%) during reassessment period. However, this is not enough, based on high demand for IPC adherence, especially given the current issues of emerging and re-emerging infectious diseases. Tanzanian facilities now have a better understanding of which, in what combination, and in what context, implementation strategies should be best utilized to ensure their safety and that of their patients. [19] The findings are in congruence with those obtained from a before and after comparison study done during the Ebola disease outbreak in a neighbouring country of the Democratic Republic of Congo (DRC) whereby the aggregate mean IPC score rose from 4.41% to 39.51%. [20] The study was conducted around the same period (2018) however, the number of participating healthcare facilities was very few compared to ours. Through both studies, we learned that healthcare facilities from higher service levels had a relatively higher proportion of IPC scores at baseline. Interestingly, low-level facilities in Tanzania had higher improvement in scores compared to those from higher service level to the extent that there was no significant difference after the intervention. Most facilities that scored below 20% during baseline were facilities from a low service level. Based on the results, it is clear that the implementation of IPC in Tanzania requires additional research from an implementation science-specific perspective to promote IPC protocols for healthcare workers. [19].
The median adherence to IPC during reassessment was 26% higher than the baseline assessment scores. The improvement was tested and found to be statistically significant. Despite the improvement, the median adherence to IPC was still below a recommended value of 80%. This poses a threat to controlling diseases like Ebola [21,22] and Coronavirus disease of 2019 (COVID-19). [23] These kinds of highly infectious diseases may be spread by asymptomatic individuals who first seek care at general healthcare facilities, which often have insufficient IPC capacity, causing the spread of the illness. [24,25] Nevertheless, since the scores for IPC adherence doubled; Tanzanian healthcare facilities are now better equipped to prevent the spread of emerging infectious diseases than ever before.
SRA was successful and worth the resource investment because during facility assessments, gaps were identified and subsequent measures were taken to address them. Financial measures were incorporated into Comprehensive Council Health Plans (CCHP). [10] SRAs facilitated the training of healthcare workers on Quality Improvement methodology and how to conduct supervisions that are data-driven. Quality data are now used at various healthcare facilities for planning and budgeting and measurement of progress. SRA enabled harmonization of IPC and regular supportive supervision checklists and in so doing; other areas which were usually not assessed were now included in regular assessments. Therefore, the success of the program mostly depended on the implementation of QIPs. Local authorities ensured the plans were implemented through quarterly supervision to all facilities. However, some unpublished reports show that there were some facilities which did not implement the QIPs effectively. [14,26] The challenges to achieve effective QIPs included lack of skilled staff, [27] lack of commitment and the language used in the assessment tools and QIPs. English was used instead of a common national language (Kiswahili) and therefore staff (especially those in lower cadres) experienced difficulty in understanding the tools and the QIPs developed during the assessment. [26] The facilities which did not submit the QIPs were penalized during the assessments, while those which did not meet the plan identified the gaps which were rescheduled for the subsequent supervisions and assessments.
It was important to determine whether being a private or public facility had an effect on performance in IPC during assessments. The effect of the facility's ownership on adherence to IPC was significant during the baseline assessment; however, this was not the case during the reassessment period. This finding corroborates well with the findings in the study by Bedoya et al. (2017) in Kenya, in which adherence to recommended IPC measures was weakly associated with facility ownership (public or private). [28] The current findings might be influenced by the effect of intervention activities. During the intervention period (which lasted for about two years); the facilities were required to prepare QIPs and work on them before reassessment. Items in QIPs included non-financial and financial items. Only poorly performing public facilities were provided with a fixed amount of money (ten million Tanzanian Shillings each) to improve the financially demanding items. The much improved public facilities could be attributed to the financial package provided to them. This is similar to the findings in Nigeria by Boxton and colleagues; where financial, equipment and human resource constraints were obstacles to effective implementation of IPC in labour and delivery wards. [29] Additionally, intervention packages, such as the refurbishment of infrastructure and recruitment of additional staff, were mainly implemented in public facilities and this could be the reason for greater improvement amongst public facilities. The owners of the private facilities were also required to improve the non-financial and financially demanding QIP items for patients and their benefits. The higher the score amongst the facilities (regardless of the facility's ownership) meant the facility had a higher quality of care and therefore the higher reputation within the community. Much improved publicly-owned facilities resulted in no significant difference in the likelihood of achieving the recommended IPC status between private and public owned facilities at reassessment. Whilst public healthcare facilities had limited funding for financially demanding items; private facilities were composed of a mixture of facilities; those whose owners could address the demands and others whose owners were either reluctant or had no budget to act upon the demands. We suggest that the financially related intervention provided by the government to public facilities (e.g. intervention such as facilities' renovation and staff recruitment) were good enough to improve the situation within two years.
In our evaluation dispensaries performed poorest in IPC adherence compared to other levels of healthcare service delivery during both assessments. The median performance increased as the level of service delivery increases and the change was found to be statistically significant for the baseline assessment. On the other hand, the change was not significant at the reassessment period and this might be attributed to relatively greater improvement in facilities from lower service level compared to those from a higher level. Improvement was more likely for lower-level public facilities because they were given the same amount of money for improvement as that which was given to hospitals and health centres. The higher-level facilities would require more expenses in making infrastructure for IPC. Nevertheless, since dispensaries had a median score of 30% at baseline assessment, a limited improvement was not good enough to attain recommended scores as compared to hospitals and health centres. Further studies (using more effective IPC improvement tools such as the IPC assessment framework to support the World Health Organization Guidelines on IPC Core Components implementation in acute health care facilities) might be needed to validate this potential finding. [30].
At baseline assessment, we didn't find any significant association between attaining a recommended IPC status and healthcare facility level. However, after interventions, hospitals became nearly twice as likely to achieve the recommended IPC status (of 80%) compared to dispensaries. Hospitals and health centres were less differentiated compared to dispensaries regarding attaining recommended IPC status. The current results are in-line with those from the DRC, which showed that hospitals were nearly twice as good as lower healthcare facilities, i.e., medical centres and health centres. [20] Unlike in Tanzania where changes in IPC practices were observed over two years; the changes in the DRC were followed for two months only. The two month period could be a short time for lower facilities (with poor infrastructure and resources) to attain significant changes. We have therefore provided this locally generated evidence to guide strengthening leadership and institutionalisation of IPC programmes in lower primary healthcare facilities of sub-Saharan African countries (as recommended by Avortri and colleagues in the Global call for action on infection prevention and control focusing in low-income countries). [31].
When we studied the spatial distribution of adherence to IPC principles, we found no distinct difference across the districts understudy. Regions and zones could have districts with both poor and good performance. Generally, districts improved in performance. Whilst the lowest score in baseline was 14%, there was no score below 41% during reassessment. The sustainability of the achieved performance needs the participation of healthcare workers who are well trained in IPC, who share experience among themselves through hands-on practices. [32].
Limitation
Data sets had a limited number of variables to allow assessment of the contribution of other factors in IPC analysis for both baseline and assessment. Additionally, the SRA was designed to be repeated after every one to two years. However, since 2015 only two assessments had been conducted.
Conclusion and recommendation
There was a remarkable increase in the adherence to IPC guidelines in Tanzania even though the majority of the facilities did not reach a recommended status. Much improvement in adherence to IPC guidelines was observed among publicly-owned healthcare facilities and facilities from the dispensary level. However, health centres and hospitals were likely to attain the recommended status after the intervention. The findings showed the progression of the healthcare facilities towards recommended status.
Besides improving adherence to IPC principles; SRAs transformed the mind-sets of healthcare workers and they began thinking about the quality of care during healthcare provision. [9] It has been the basis for a result-based financing program whereby facilities strive to improve quality of care to acquire additional funds. Furthermore, the SRA system facilitated guided and structured supportive supervision for healthcare workers on IPC guideline adherence. Some facilities now use SRA assessment tools for internal supervision and appraisal.
Funding
No official funding was received by the authors for the study, FELTP Program supported EK to collect and analyze data as part of the Training.
Conflict of interest statement
The authors declared no conflict of interest. During the time of baseline and reassessment as well as during write up of the study – JH, EE and TY were with the Health Quality Assurance Division (now called Health Quality Assurance Unit) and were responsible for the implementation of SRA and QIPs follow-up.
Ethical approval
For this type of study formal consent is not required, however, prior permission from the Ministry of Health, Community Development, Gender, Elderly and Children was sought before use of the dataset.
CRediT authorship contribution statement
Erick Kinyenje: Conceptualization, Writing - original draft, Methodology, Formal analysis. Joseph Hokororo: Conceptualization, Writing - review & editing, Validation. Eliudi Eliakimu: Writing - review & editing. Talhiya Yahya: Data curation. Bernard Mbwele: Writing - review & editing. Mohamed Mohamed: Supervision. Gideon Kwesigabo: Validation, Writing - review & editing, Supervision.
Acknowledgement
The authors are passing their sincere gratitude to the Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) especially, the Health Quality Assurance Unit for granting us permission to use the Star Rating Assessment data. Our sincere appreciation also goes to TFELTP team especially Dr. Janeth Mghamba, Dr. Rogath Kishimba, Dr. Ahmed Abade and Ms. Loveness John for continual technical and managerial support.
The key partners in the implementation of the Star Rating system includes directorates and units of MoHCDGEC (Health Quality Assurance Division [now a Unit], Curative Services Division, Information Communication and Technology Unit, Preventive Services Division, and Pharmaceutical Services Unit) and the Health Directorate of the President's Office - Regional Administrative and Local Government (PO-RALG). Other development partners like the World Bank, Centres for Disease Control and Prevention (CDC), Danish International Development Agency (DANIDA), The World Health Organization, other members of the Development Partners in Health-Group (DPG-H), PharmAccess, Association of Private Health facilities (APHTA), Christian Social Services Commission (CSSC), and communities of the facilities visited are appreciated.
References
- 1.World Health Organization . WHO; 2019. Infection prevention and control.https://www.who.int/gpsc/ipc/en/ [PubMed] [Google Scholar]
- 2.Nejad S.B., Allegranzi B., Syed S.B., Ellis B., Pittet D. Health-Care-Associated Infection in Africa: A Systematic Review. Bull World Health Organ. 2011;89:757–765. doi: 10.2471/BLT.11.088179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . 2019. Evidence for hand hygiene guidelines.https://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/ [Google Scholar]
- 4.World Health Organization . 2011. Report on the burden of endemic health care-associated infection worldwide. [Google Scholar]
- 5.Zaidi A.K., Huskins W.C., Thaver D., Bhutta Z.A., Abbas Z., Goldmann D.A. Hospital-Acquired Neonatal Infections in Developing Countries. Lancet. 2005;365(9465):1175–1188. doi: 10.1016/S0140-6736(05)71881-X. [DOI] [PubMed] [Google Scholar]
- 6.Ali S., Birhane M., Bekele S., Kibru G., Teshager L., Yilma Y. Healthcare Associated Infection and its Risk Factors Among Patients Admitted to a Tertiary Hospital in Ethiopia: Longitudinal Study. Antimicrobial Resistance & Infection Control. 2018;7(1):2. doi: 10.1186/s13756-017-0298-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allegranzi B., Sax H., Bengaly L., Riebet H., Minta D.K., Chraiti M.N. Successful Implementation of the World Health Organization Hand Hygiene Improvement Strategy in a Referral Hospital in Mali, Africa. Infect Control Hospital Epidemiol. 2010;31(2):133–141. doi: 10.1086/649796. [DOI] [PubMed] [Google Scholar]
- 8.Gosling R., Mbatia R., Savage A., Mulligan J.-A., Reyburn H. Prevalence of Hospital-Acquired Infections in a Tertiary Referral Hospital in Northern Tanzania. Annal Tropical Med Parasitol. 2003;97(1):69–73. doi: 10.1179/000349803125002724. [DOI] [PubMed] [Google Scholar]
- 9.Yahya T., Mohamed M. Raising a Mirror to Quality of Care in Tanzania: the Five-Star Assessment. Lancet Global Health. 2018;6(11):e1155–e1157. doi: 10.1016/S2214-109X(18)30348-6. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health and Social Welfare Big Results Now (BRN) - Tanzania Development Vision 2025. http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/health/Sub_Sector_Group/BRN_documents/Tanz_Healthcare_Lab_Report_Part_1_0212_RH_-_v21__Final_Lab_Report_.pdf BRN Healthcare NKRA Lab: Lab Report – Part I.
- 11.Allegranzi B., Nejad S.B., Combescure C., Graafmans W., Attar H., Donaldson L. Burden of Endemic Health-Care-Associated Infection in Developing Countries: Systematic Review and Meta-Analysis. The Lancet. 2011;377(9761):228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 12.Raza M., Kazi B., Mustafa M., Gould F. Developing Countries Have Their Own Characteristic Problems With Infection Control. J Hosp Infect. 2004;57(4):294–299. doi: 10.1016/j.jhin.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 13.The United Republic of Tanzania - Ministry of Health Community Development, Gender, Elderly and Children; and World Health Organisation . Experiences, best practices and challenges. November 2019. Documentation of Lessons Learnt from Partnership through Health Sector Wide Approach in Tanzania:2016-2019.http://www.tzdpg.or.tz/dpg-website/sector-groups/cluster-2/health/document-library.html Available at: [Google Scholar]
- 14.The United Republic of Tanzania - Ministry of Health Community Development G, Elderly and Children . Dar es Salaam. 2017. Supportive Supervision for Facilities with Zero Stars which Received 10 millions in Kigoma, Dodoma, Singida and Tanga. [Google Scholar]
- 15.United Republic of Tanzania Ministry of Health and Social Welfare . 2015. Health sector strategic plan july 2015 –june 2020 (HSSP IV): reaching all households with quality health care.http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/health/Key_Sector_Documents/Induction_Pack/Final_HSSP_IV_Vs1.0_260815.pdf [Google Scholar]
- 16.President’s Office – public service management and good governance. The approved functions and organisation structure of the Ministry of health. 2018. http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/health/Key_Sector_Documents/Induction_Pack/MUUNDO_-AFYA_July_2018.pdf Community Development, Gender, Elderly and Children (Approved by the President on 7th July, 2018) [Google Scholar]
- 17.United Republic of Tanzania - Ministry of Health and Social Welfare . January 2014. National guidelines for recognition of implementation status of quality improvement initiatives in health facilities.http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/health/Sub_Sector_Group/Quality_Assurance/12_Recognition-Guidelines.pdf Available at: [Google Scholar]
- 18.Centers for Disease Control and Prevention Epi Info™ Downloads. 2019. https://www.cdc.gov/epiinfo/support/downloads.html Available at:
- 19.Barrera-Cancedda A.E., Riman K.A., Shinnick J.E., Buttenheim A.M. Implementation Strategies for Infection Prevention and Control Promotion for Nurses in Sub-Saharan Africa: A Systematic Review. Implementation Science. 2019;14(1):111. doi: 10.1186/s13012-019-0958-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ousman K., Kabego L., Talisuna A., Diaz J., Mbuyi J., Houndjo B. The Impact of Infection Prevention and Control (IPC) Bundle Implementation on IPC Compliance during the Ebola Virus Outbreak in Mbandaka/Democratic Republic of the Congo: A Before and After Design. BMJ Open. 2019;9(9) doi: 10.1136/bmjopen-2019-029717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cenciarelli O., Pietropaoli S., Malizia A., Carestia M., Fabrizio D’Amico F., Alessandro Sassolini A. Ebola virus disease 2013-2014 outbreak in west Africa: an analysis of the epidemic spread and response. International Journal of Microbiology. 2015;2015 doi: 10.1155/2015/769121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coltart C.E., Lindsey B., Ghinai I., Johnson A.M., Heymann D.L. The Ebola outbreak, 2013–2016: old lessons for new epidemics. Phil Transact Royal Soc B: Biol Sci. 2017;372(1721):20160297. doi: 10.1098/rstb.2016.0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Selvaraj S.A., Lee K.E., Harrell M., Ivanov I., Allegranzi B. Infection rates and risk factors for infection among health workers during Ebola and Marburg virus outbreaks: a systematic review. J Infect Dis. 2018;218(suppl_5):S679–S689. doi: 10.1093/infdis/jiy435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Furukawa N., Brooks J., Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic. Emerg Infect Dis. 2020;26(7) doi: 10.3201/eid2607.201595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Justine C. Morogoro: School of Public Administration and Management, Mzumbe University; 2019. Evaluation of implementation Process of star rating Assessment and quality improvement Plans in primary healthcare Facilities in Tanzania-Case of Kibaha Town and Rufiji District Councils [Dissertation] [Google Scholar]
- 27.Sirili N., Frumence G., Kiwara A., Mwangu M., Goicolea I., Hurtig A.-K. “Doctors ready to be posted are jobless on the street…” the deployment process and shortage of doctors in Tanzania. Human Resour Health. 2019;17(1):11. doi: 10.1186/s12960-019-0346-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bedoya G., Dolinger A., Rogo K., Mwaura N., Wafula F., Coarasa J. Observations of Infection Prevention and Control Practices in Primary Health Care, Kenya. Bull World Health Organ. 2017;95(7):503. doi: 10.2471/BLT.16.179499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buxton H., Flynn E., Oluyinka O., Cumming O., Mills J.E., Shiras T. Barriers and Opportunities Experienced by Staff When Implementing Infection Prevention and Control Guidelines During Labour and Delivery in Healthcare Facilities in Nigeria. J Hospital Infect. 2019;103(4):428–434. doi: 10.1016/j.jhin.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 30.Tomczyk S., Aghdassi S., Storr J., Hansen S., Stewardson A.J., Bischoff P. Testing of the WHO Infection Prevention and Control Assessment Framework at Acute Healthcare Facility Level. J Hospital Infect. 2020;105(1):83–90. doi: 10.1016/j.jhin.2019.12.016. [DOI] [PubMed] [Google Scholar]
- 31.Avortri G.S., Nabyonga-Orem J. The Global Call for Action on Infection Prevention and Control. Int J Health Care Qual Assur. 2019;32(6):927–940. doi: 10.1108/IJHCQA-03-2018-0063. [DOI] [PubMed] [Google Scholar]
- 32.Tartari E., Fankhauser C., Masson-Roy S., Márquez-Villarreal H., Moreno I.F., Navas M.L. Train-The-Trainers in Hand Hygiene: A Standardized Approach to Guide Education in Infection Prevention and Control. Antimicrob Resist Infect Control. 2019;8(1):206. doi: 10.1186/s13756-019-0666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]