Abstract
Purpose
Oocyte activation is a fundamental event at mammalian fertilization. In mammals, this process is initiated by a series of characteristic calcium (Ca2+) oscillations, induced by a sperm-specific phospholipase C (PLC) termed PLCzeta (PLCζ). Dysfunction/reduction/deletion of PLCζ is associated with forms of male infertility where the sperm is unable to initiate Ca2+ oscillations and oocyte activation, specifically in cases of fertilization failure. This review article aims to systematically summarize recent advancements and controversies in the field to update expanding clinical associations between PLCζ and various male factor conditions. This article also discusses how such associations may potentially underlie defective embryogenesis and recurrent implantation failure following fertility treatments, alongside potential diagnostic and therapeutic PLCζ approaches, aiming to direct future research efforts to utilize such knowledge clinically.
Methods
An extensive literature search was performed using literature databases (PubMed/MEDLINE/Web of Knowledge) focusing on phospholipase C zeta (PLCzeta; PLCζ), oocyte activation, and calcium oscillations, as well as specific male factor conditions.
Results and discussion
Defective PLCζ or PLCζ-induced Ca2+ release can be linked to multiple forms of male infertility including abnormal sperm parameters and morphology, sperm DNA fragmentation and oxidation, and abnormal embryogenesis/pregnancies. Such sperm exhibit absent/reduced levels, and abnormal localization patterns of PLCζ within the sperm head.
Conclusions
Defective PLCζ and abnormal patterns of Ca2+ release are increasingly suspected a significant causative factor underlying abnormalities or insufficiencies in Ca2+ oscillation-driven early embryogenic events. Such cases could potentially strongly benefit from relevant therapeutic and diagnostic applications of PLCζ, or even alternative mechanisms, following further focused research efforts.
Keywords: Phospholipase C zeta (PLCzeta), Oocyte activation, Fertilization: Sperm, Infertility: Assisted reproductive technology
Introduction
Infertility afflicts ~ 15% of couples, while male infertility is prevalent in ~ 7% of men worldwide, with ~ 50% of such cases remaining unexplained [1–4]. This is a particularly worrying statistic as male infertility is increasingly attributed as the major causative factor underlying infertility [5]. However, assisted reproductive technologies (ART; laboratory techniques such as in vitro fertilization or IVF) have allowed a route for treatment in affected couples, accounting for ~ 7% of total birth rates in some developing countries [5]. However, several conditions of severe male infertility (19–57% of cases of infertility) remain untreatable [6], even following intracytoplasmic sperm injection (ICSI; injection of an individual sperm into the oocyte). Furthermore, up to 1–5% of ICSI treatment cycles fail, largely attributed to a defect in fertilization [5, 7–9].
However, treatment is usually successful following multiple cycles (although this does not preclude a small, but significant, number of cases where cycles are successful on first attempt), potentially due to recurrent implantation failure, which contributes to a significant percentage of infertility following fertility treatments [10]. Indeed, global pregnancy and live birth rates following ART rarely exceeds ~ 40%, while success via IVF or ICSI remains as low as 27% per cycle [11]. Low pregnancy success rates can be attributed to poor embryonic development or competency [12, 13], increasingly correlated with poor sperm parameters [14]. Superior quality sperm selected from a population of generally poor quality tends to improve embryogenic competency compared with without selection in the same infertile couples [15].
Such correlations may be further multifactorial, involving abnormal sperm epigenetics [16–19], abnormal sperm DNA status (DNA fragmentation/aneuploidies; [20–22]), and increasingly altered lifestyles and diets [23–28]. Perhaps one of the major events that sperm components contribute to at fertilization is oocyte activation, a series of processes that are directly influenced by the fertilizing sperm [5, 29]. This review examines the significance of oocyte activation, and how these events can be linked to not only the quality of subsequent embryogenesis but also to potential fertility treatment outcomes. This review also scrutinizes how the sperm initiates oocyte activation through the soluble sperm factor, attempting to connect how recent clinically oriented studies suggest the involvement of such factors in determining fertility treatment outcome. Finally, this review will discuss potential diagnostic and therapeutic approaches based on such associations, with the aim of directing future research efforts to utilize such knowledge clinically.
Oocyte activation, intracellular calcium oscillations, and the sperm factor
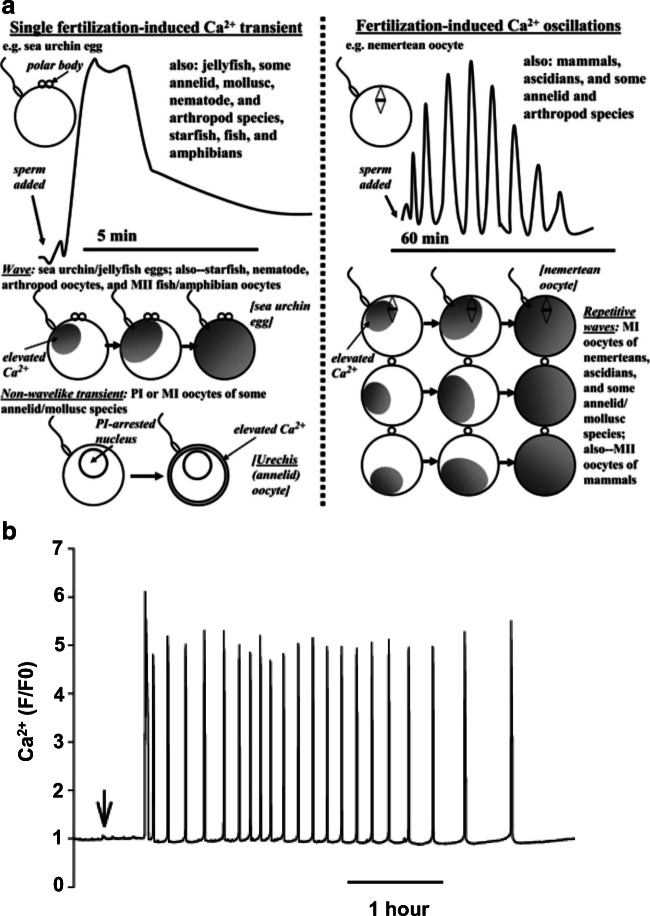
Oocyte activation is a collection of fundamental events at fertilization which culminate in the initiation of embryogenesis in response to changes in intracellular calcium (Ca2+). The eggs of some vertebrates such as echinoderms, frogs, and fish elicit a single Ca2+ wave at fertilization, while mammals and several marine invertebrates elicit a series of repetitive Ca2+ oscillations [5, 30–36], which in mammalian oocytes are a direct consequence of inositol trisphosphate (IP3)-mediated Ca2+ release [5, 9, 35, 37–41]. Patterns of Ca2+ oscillations are species-specific in amplitude, duration, and frequency [42–45], and are essential in all species studies to date (Fig. 1), sufficiently triggering blastocyst development in mice [35, 47]. Inhibiting Ca2+ release prevents fertilization [30, 48], while diminishing IP3 receptors (IP3Rs) in mouse and hamster oocytes inhibited Ca2+ oscillations and oocyte activation [42, 49–51]. Increased IP3 concentrations during fertilization in mammalian oocytes [35] further support the importance of IP3 levels and IP3-mediated Ca2+ release at oocyte activation.
Fig. 1.
a Schematic summary of solitary versus repetitive Ca2+ transients during fertilization across the animal kingdom. Examples of waves versus non-wavelike transients are listed for various animal groups, while also detailing models of Ca2+ transient initiation in each type of model (single versus multiple transients). b A representative recording of intracellular Ca2+ release patterns in a mouse oocyte undergoing in vitro fertilization (IVF) using a Ca2+-sensitive fluorescent dye (Rhod dextran in this case). The fluorescence is expressed as a ratio of the intensity divided by the starting fluorescence value. The arrow indicates time of sperm addition to oocytes. Figure adapted from Kashir et al. [46] and Kashir et al. [45] with permission
The specific profile of Ca2+ release at fertilization may not only be necessary for oocyte activation but also equally important for subsequent embryogenic events. Differential frequencies and amplitudes of Ca2+ release [52, 53] altered protein expression profiles in early mouse embryos and rabbits [43, 44, 54], as well as the efficacy of cell cycle progression and embryogenesis [31, 33, 43, 44]. Considering that such parameters in human embryos is proving an indicator of normal embryogenesis and pregnancy success [55, 56], elucidating the specific mechanisms underlying Ca2+ release at fertilization holds significant scientific and clinical interest.
Most evidence indicates that a specific factor is delivered to the oocyte upon fertilization by the sperm, triggering Ca2+ release from intracellular stores [57]. Indeed, injecting sperm extracts into mammalian oocytes triggered similar patterns of Ca2+ oscillations to those observed at fertilization [32, 57–62], while the global success of ICSI which bypasses most conventional cellular modes of Ca2+ transduction (such as G protein signaling or membrane ligand/receptor mechanisms), provides further support for the sperm factor hypothesis [5, 63]. A number of candidates have been proposed at this “sperm factor,” including a 33 kDa protein (or oscillogen) [64], a truncated form of the c-kit receptor (tr-kit) via activation of phospholipase C (PLC) isoform gamma-1 (PLCγ1) through phosphorylation by a Src-like kinase Fyn [65–67], and more recently, the post-acrosomal sheath WW domain-binding protein (PAWP) [68, 69]. However, the phosphoinositide signaling pathway is an essential component of the Ca2+ oscillations observed, where intracellular IP3 is generated by the hydrolysis of phosphatidylinositol 4,5-bisphosphate (PIP2), binding to IP3Rs on the ER, resulting in Ca2+ release [42, 45, 48, 70–73]. None of the aforementioned factors sufficiently elicit Ca2+ oscillations similar to the pattern observed at fertilization, at least within physiological parameters [9, 45, 46, 74–77]. Intriguingly, although numerous PLC isoforms play specific roles at fertilization in both gametes, data indicated that most previously known PLC isoforms were not directly involved in oocyte activation, failing to elicit Ca2+ release upon injection into mouse oocytes [45, 78–83].
PAWP proposedly mediates effect in oocytes via yes-associated protein (YAP), leading to PLC gamma (PLCγ)-mediated activation similar to Xenopus eggs [84]. Indeed, microinjection of recombinant bovine PAWP seemingly initiated activation of porcine, bovine, macaque, and Xenopus oocytes and eggs as indicated by pronuclear formation [68], while recombinant bovine PAWP injection into Xenopus eggs reportedly exhibited Ca2+ release [69]. Furthermore, recombinant human PAWP protein or cRNA seemingly induced Ca2+ oscillations upon microinjection into mouse and human oocytes, which were blocked by co-injection of a peptide acting as a competitive inhibitor of PAWP [84]. However, the specific molecular mechanisms underlying signal transduction regarding tr-kit and PAWP remain unclear, while it remains unclear whether both tr-kit and PAWP elicit Ca2+ oscillations similar to those observed at fertilization under physiological conditions. Importantly, recent independent in vitro biochemical studies refuted the proposed functional role for PAWP [85–87], while sperm generated from a PAWP-null mouse remained able to initiate Ca2+ induction similar to normal fertilization [88].
Alternative theories have also suggested that mammalian oocyte factors contribute significantly towards oocyte activation. Indeed, oocytes contain multiple PLC isoforms, including beta (β), γ, and delta (δ) [82]. Reduction or overexpression of oocyte-PLCβ1 altered Ca2+ oscillation profiles, but did not prevent activation [82]. A novel PLCδ isoform in sea urchin gametes has also been identified, whose PH domain localized to the plasma membrane of eggs, increasing in intensity at fertilization. However, recombinant sea urchin PLCδ failed to elicit Ca2+ release upon injection into mouse oocytes and sea urchin eggs [81], while the relevance of such populations seem redundant towards oocyte activation at least within mammals whereby Ca2+ oscillations initiate cortically, rather than near the plasma membrane [45]. Furthermore, injection of recombinant PLCβ1, PLCγ1, PLCγ2, PLCδ1, PLCδ3, and PLCδ4 all failed to elicit Ca2+ release upon injection into mouse oocytes, indicating that oocyte PLC isoforms are not directly involved in oocyte activation, but may yet potentially exert effect further downstream of fertilization [45, 80, 82, 83].
The mammalian sperm factor is a distinct PLC, termed phospholipase C zeta
The specific PLC isozyme responsible for mammalian oocyte activation was proposed to be a testis-specific PLC, termed PLCzeta (PLCζ) [89, 90], identified in multiple mammalian species including human, hamster, monkey, and horse [90–94]. PLCζ exhibits characteristic X and Y catalytic domains forming the active site, a single C2 domain, and four tandem EF hand domains [89, 95]. However, PLCζ uniquely lacks either a pleckstrin homology (PH), or Src homology (SH) domain, making PLCζ the smallest known mammalian PLC with a molecular mass of ~ 70 kDa in humans and ~ 74 kDa in mice [89, 90].
Abrogating catalytic domains of PLCζ dissipated Ca2+ release in mouse oocytes [89], while recombinant PLCζ injection downregulated IP3Rs in mouse oocytes, indicative of IP3 binding [96]. PLCζ is extremely sensitive to basal oocyte Ca2+ levels [97, 98], thought to be mediated by its unique domain organization the four EF hand domain exerting significant Ca2+ sensitivity [98–100]. The EF hands along with the C2 domain contribute an important role in PLCζ binding to PIP2 [85], along with the extended PLCζ XY-linker which also regulates enzyme activity [83, 100–103]. The XY-linker region also contains a predicted nuclear localization signal (NLS) sequence, which may regulate at least mouse PLCζ mediated via nuclear shuttling [104, 105]. However, this feature seems to be unique to only the mouse model [5, 105] (Fig. 2a).
Fig. 2.
a Schematic representation of PLCζ, summarizing briefly the functional roles of each domain group. b Schematic illustration of the proposed mechanism of PLCζ action. Following sperm/oocyte fusion, PLCζ diffuses into ooplasm, binding to vesicular-bound PIP2 dispersed throughout the cytoplasm. PIP2 hydrolysis by PLCζ generates IP3, resulting in Ca2+ release from the endoplasmic reticulum (ER). Increased cytosolic Ca2+ then further stimulates the activity of PLCζ, generating more IP3. This positive feedback loop occurs throughout as PLCζ continues to diffuse across the ooplasm. Figure adapted from Swann and Lai [106], with permission
Recombinant PLCζ elicits Ca2+ oscillations similar to physiological fertilization patterns upon injection into mouse oocytes, also supporting blastocyst formation [83, 99]. Sperm extract fractions containing PLCζ-induced Ca2+ oscillations [98, 107, 108] while diminishing PLCζ from such extracts suppressed Ca2+ release [89]. Furthermore, reduction of testicular PLCζ in mice through RNA interference (RNAi) yielded sperm which prematurely ended Ca2+ release before completion of activation, and significantly reduced litter sizes [109]. Finally, sperm extracts and recombinant PLCζ elicit Ca2+ release upon microinjection into eggs and oocytes across and between species [89, 110], while non-mammalian testis-specific PLCζ homologues have also been identified [62, 81, 105, 111], indicating that PLCζ may be a universal feature of oocyte activation, at least within mammals (Fig. 2b).
Hachem et al. [112] and Nozawa et al. [113] recently reported keystone studies involving creation of transgenic knockout (KO) mouse models of PLCζ, both of whom independently concluded that PLCζ is the primary physiological stimulus of Ca2+ oscillations at fertilization [112, 113]. Interestingly, however, both studies also reported that KO males produced offspring, albeit in significantly reduced litter numbers (~ 25% of wild-type litters), indicating subfertility rather than infertility. Puzzlingly, while sperm from such mice failed to induce Ca2+ release following ICSI, IVF resulted in atypical and delayed patterns of Ca2+ oscillations (lower in number and frequency) with a high degree of polyspermy and activation failure [113, 114]. Such results may indicate that PLCζ is not an absolute requirement for natural fertilization, with an additional “primitive” or “cryptic” sperm factor also involved at oocyte activation [113–115].
Perhaps the identity of such a factor could be alternatively proposed sperm factors such tr-kit, citrate synthase, or PAWP, which while not contributing to the majority of Ca2+ release at oocyte activation, may have a contributory function [65, 69, 116]. However, as previously discussed, no other proposed factor apart from PLCζ has been independently and consistently confirmed to elicit Ca2+ release in the specific manner required for oocyte activation, at least at physiological levels of protein present within sperm [45, 86–88], while none of the alternatively proposed sperm factors (apart from PLCζ) involve IP3-mediated Ca2+ release [29, 45]. In addition to sperm contributors towards oocyte activation, the mammalian oocyte cellular machinery involved in Ca2+ signal transduction may also exert significant effect upon the efficacy of oocyte activation [117, 118], with proposed relationships between fertilization failure and the expression profiles of genes involved in oocyte maturation, including growth differentiation factor 9 (GDF9), bone morphogenetic protein 15 (BMP15), BCL2-associated transcription factor 1 (BCLAF1), leiomodin 3 (LMOD3), and F-box protein 5 (FBXO5) [119–123]. In ascidians, sequestration of PLCζ fails to terminate Ca2+ release, which is only achieved following blockage of CDK1, an oocyte protein that promotes IP3 generation in the presence of PLCζ [124]. It would be interesting to examine the role of such factors in the context of PLCζ KO mouse models as well, as to whether such factors could be compensating for lack of PLCζ.
However, both Hachem et al. [112] and Nozawa et al. [113] indicated that sperm lacking PLCζ could not induce Ca2+ release upon microinjection into mouse oocytes, while in vitro fertilization (IVF) with such sperm elicited Ca2+ oscillations lower in number and frequency with a high degree of polyspermy and activation failure [113, 114]. Perhaps the atypical and delayed pattern of Ca2+ release, observed alongside the low number of embryos and offspring, could be spontaneous activation unrelated to Ca2+ release, common in some strains of mice [125]. However, another recent proposition suggested that the low frequency and number of Ca2+ peaks observed could be due to events surrounding actin polymerization or associated IP3-independent events of Ca2+ release (such as influx). Indeed, disruption of starfish egg cytoskeletal arrangements (either age- or heparin-induced) resulted in a delayed pattern of Ca2+, and failed to prevent polyspermy [126–130]. It would be interesting for studies to relate the increasing body of invertebrate animal work with relation to the early influence exerted by the egg/oocyte actin cytoskeleton upon patterns of Ca2+ release and fertilization in mammals. Further studies are urgently required in larger mammalian models to demonstrate whether PLCζ loss resembles the mouse and/or human scenarios and investigating larger issues such as the involvement of the cytoskeleton at activation should constitute at least part of such investigations [130].
Regardless, however, the tremendous work by both Hachem et al. [112] and Nozawa et al. [113] represents keystone studies that both ultimately support the notion that PLCζ is the primary physiological stimulus that triggers the required specific pattern of Ca2+ oscillations, ensuring monospermy and eventually successful oocyte activation and early embryonic development [112, 113]. While numerous studies are still required to fully ascertain the entire picture of players involved at the complex processes of oocyte activation, it would nonetheless seem clear that the presence of an alternative factor in other species and especially in humans is still questionable, particularly taking into consideration all the documented cases of male factor infertility due to PLCζ deficiencies which this review discusses in detail subsequently.
PLCζ in mammalian gametes
Contrary to conventional knowledge, PLCζ does not target the oocyte plasma membrane where PIP2 is sufficiently present in mouse oocytes [131]. Depleting plasma membrane PIP2 had no effect upon PLCζ- or sperm-induced Ca2+ oscillations, while concurrently abolishing PLCδ1-induced Ca2+ release [132]. Indeed, the majority of PIP2 hydrolysis and IP3 generation at mammalian oocyte activation is ooplasmic [45, 56, 133, 134]. Such observations were confirmed by immunocytochemistry experiments [132], which collectively indicated that PLCζ was bound to PIP2-containing vesicles [135]. However, the nature of such vesicles remains to be elucidated [29].
Microinjection experiments alongside mass spectrometry and immunoblotting identified PLCζ in mouse sperm extract fractions containing the ability to elicit Ca2+ release, predominantly within the post-acrosomal sheath component of sperm [107, 135–137]. Immunofluorescence experiments indicated that the pattern of PLCζ localization in mouse sperm was contained to the post-acrosomal region, a component of the post-acrosomal sheath [83, 93, 107], an optimal location within sperm to induce oocyte activation immediately at or after gamete fusion [5, 107]. However, while PLCζ localization in mouse sperm has generally been consistently reported in the literature, the same does not bear true for PLCζ from other mammalian species, particularly in humans.
Populations of PLCζ have been identified in acrosomal and post-acrosomal regions of mouse and porcine sperm, with a tail population also identified in porcine sperm [83, 93, 138, 139]. In equine sperm, PLCζ has been reported at the acrosomal region, equatorial segment, and principle piece of the flagellum [92]. In humans, distinct populations of PLCζ have been identified in the acrosomal, equatorial, and post-acrosomal regions of the sperm head, alongside a tail localization [92, 140–144]. Such distinctly variable populations of PLCζ can perhaps be correlated to species-specific physiological requirements of each organism studied (in terms of PLCζ solubility and/or oocyte calcium response) [45] or are perhaps attributable to specific roles at fertilization. For example, microinjection of equine sperm tails into mouse oocytes resulted in high frequency Ca2+ oscillations, suggesting that the tail does indeed contain functional PLCζ [94]. Indeed, the entirety of the sperm is incorporated into the oocyte during normal fertilization, including the midpiece and tail [145]. Thus, the presence of such potentially contributory populations of PLCζ within the sperm tail would imply functional significance as such tail-PLCζ populations would be eventually delivered to the oocyte in a time-dependent manner in addition to head populations.
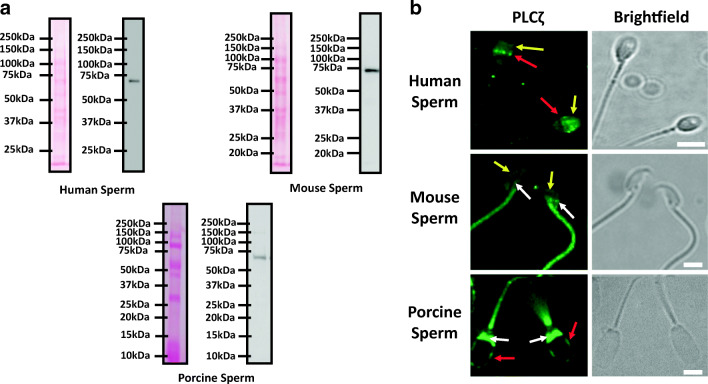
While the most physiologically relevant population of PLCζ within human sperm has traditionally been considered to be the equatorial pattern, acrosomal PLCζ isoforms may also exert a role in capacitation or the acrosome reaction [146]. Indeed, Grasa et al. [140], Young et al. [93], and Mejía-Flores et al. [147] indicated that PLCζ shifted to a dominantly post-acrosomal localization following capacitation in human, mouse/hamster, and bull sperm, respectively. Furthermore, the occurrence of equatorial PLCζ corresponded to sperm with intact acrosomes [93, 140, 141], while Escoffier et al. [148] indicated the presence of PLCζ beneath the acrosomal cap in human sperm following electron microscopy. Thus, such differential populations may serve as additional sources of sperm PLCζ to ensure sufficient requisite levels are delivered to the oocyte for effective oocyte activation. However, such specific assertions require further investigation, particularly within humans where variability in reported localization patterns remains greatest between studies [46]. This is being greatly aided by numerous studies that are utilizing antibodies with confirmed enhanced specificity (Fig. 3a), with which specific assertions can be made about specific patterns of PLCζ localization in mammalian sperm (Fig. 3b).
Fig. 3.
a Representative immunoblotting images of native sperm PLCζ from human, murine, and porcine sperm indicating specific bands corresponding to PLCζ (human 70 kDa; murine 74 kDa; and porcine 72 kDa). Left panels indicated Ponceau-stained membranes following transfer of protein, while right panels indicate antibody-probed membranes. b Representative immunofluorescence images using specific antibodies indicating the immunofluorescence profile of sperm PLCζ in human (top panel), murine (middle panel), and porcine (bottom panel) sperm. PLCζ fluorescence (green) is indicated in the right-most panels, and corresponding brightfield images are indicated in the left-most panels. Red arrows indicate equatorial, yellow arrows indicate acrosomal, and white arrows indicate post-acrosomal localization patterns on PLCζ in the three species of sperm indicated. Images shown are indicative of predominant localization patterns observed throughout the published literature. White scale bars are indicative of 5 μm
Saunders et al. [89] detected PLCζ mRNA as early as the spermatid stage in mice, with similar observations made in porcine, equine, and quail models [91, 94, 139, 149]. Aarabi et al. [150] indicated that PLCζ was incorporated as part of the acrosome during the Golgi phase of human and mouse spermiogenesis, suggesting that levels of PLCζ diminished gradually throughout spermatid elongation. However, these observations have yet to be confirmed independently, with specific localization patterns throughout the various spermatogenic cells within testes remaining elusive within the literature.
Phospholipase C zeta and male infertility
Defective PLCζ or PLCζ-induced Ca2+ can be linked to specific forms of male infertility, or even perhaps subfertility, as a result of defective oocyte activation. Sperm of infertile men which consistently failed to fertilize oocytes following routine IVF or ICSI either failed to produce Ca2+ oscillations upon injection into mouse oocytes or did so with reduced frequency and amplitude [92, 128]. Furthermore, such sperm also exhibit absent/reduced levels, and abnormal localization patterns of PLCζ within the sperm head [5, 92, 141, 142, 144, 151–167], suggesting that defects in sperm PLCζ may underlie such cases of fertilization failure, particularly considering that such fertilization failure can be “rescued” following concurrent microinjection of infertile human sperm with recombinant PLCζ. Clinically, complete fertilization failure is attributed towards defective oocyte activation failure in a sperm-specific manner, more so than any other potential cause [5].
PLCζ mutations
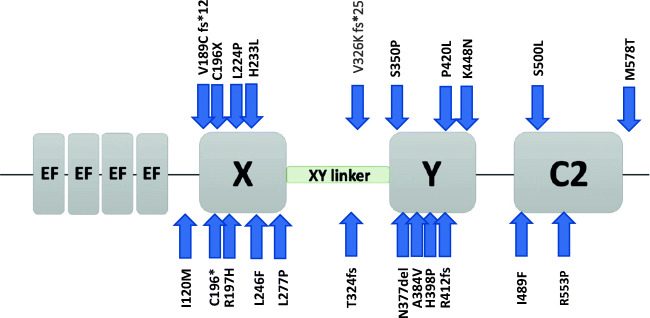
Concurrently, multiple mutations have been identified in the PLCζ gene of such patients by numerous independent groups globally, which result in abrogation of PLCζ activity and/or levels within the sperm [141, 142, 151–162]. Correlative examinations of PLCζ mutation and sperm localization all indicate a common motif of reduced/absent levels of PLCζ in sperm, and/or a severely altered localization profile within the sperm (Fig. 4; Table 1). While such observations are true for patients who can be classified with an oocyte activation deficiency (OAD; where fertilization failure is a repeated outcome), examinations of sperm PLCζ in other motifs of male infertility reveal significant correlations with deficiencies in PLCζ levels and localization patterns. This has been observed for multiple male-specific conditions including abnormal sperm parameters and morphology [5, 46, 148–152], sperm DNA fragmentation and oxidation [165–167], and abnormal embryogenesis/pregnancies [169].
Fig. 4.
Schematic representation of PLCζ indicating where each mutation identified in the literature has thus far been identified as indicated by blue arrows. Each mutation is represented by the original amino acid, followed by the amino acid position number, and then the mutated amino acid
Table 1.
Summary of mutations identified by the scientific literature, detailing the domain affected, the in vitro and in vivo phenotypes detected by various studies, as well as the studies that have investigated and/or reported the corresponding mutations. Mutations are represented as the corresponding amino acid change at the reported amino acid sequence position. OAD, oocyte activation deficiency
| Mutation | Domain affected | In vitro phenotype | In vivo phenotype | Associated studies |
|---|---|---|---|---|
| I120M | EF-X linker | Predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Torra-Massana et al. [158] |
| C196X | X | Predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Dai et al. [157] |
| C196* | X | No recombinant protein produced by mammalian cells; reduced activation success following cRNA injection in mouse oocytes | OAD; reduced/absent PLCζ in patient sperm; low fertilization success | Mu et al. [160]; Yan et al. [161] |
| R197H | X | Predicted alteration of local protein fold | OAD; low fertilization success | Ferrer-Vaquer et al. [153]; Torra-Massana et al. [158] |
| L224P | X | Predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Torra-Massana et al. [158] |
| H233L | X | Reduced expression in mammalian cells; reduced/absent oscillations following cRNA injections in mouse oocytes; reduced embryogenesis in mouse; predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Kashir et al. [142, 151, 152]; Ferrer-Vaquer et al. [153]; Torra-Massana et al. [158] |
| L246F | X | Predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Dai et al. [157] |
| L277P | X | Predicted alteration of local protein fold; reduced activation success following cRNA injection in human oocytes | OAD; reduced/absent PLCζ in patient sperm; low fertilization success | Yan et al. [161] |
| T324fs | X-Y linker | Truncated recombinant protein produced by mammalian cells; reduced activation success following cRNA injection in mouse oocytes | OAD; low fertilization success | Mu et al. [160] |
| V326K fs*25 | X-Y linker | Predicted frameshift truncation of protein | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Torra-Massana et al. [158] |
| S350P | Y | Predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Dai et al. [157] |
| N377del | Y | Predicted alteration of local protein fold; no activation success following cRNA injection in human oocytes | OAD; reduced/absent PLCζ in patient sperm; low fertilization success | Yan et al. [161] |
| A384V | Y | Predicted alteration of local protein fold; no activation success following cRNA injection in human oocytes | OAD; reduced/absent PLCζ in patient sperm; low fertilization success | Yan et al. [161] |
| H398P | Y | Reduced expression in mammalian cells; reduced/absent oscillations following cRNA injections in mouse oocytes; predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Heytens et al. 2009; Kashir et al. [143, 152, 153] |
| R412fs | Y | Truncated recombinant protein produced by mammalian cells; reduced activation success following cRNA injection in mouse oocytes | OAD; low fertilization success | Mu et al. [160] |
| P420L | Y | Reduced recombinant protein produced by mammalian cells; reduced activation success following cRNA injection in mouse oocytes | OAD; low fertilization success | Mu et al. [160] |
| K448N | Y | Predicted alteration of local protein fold; reduced activation success following cRNA injection in human oocytes | OAD; reduced/absent PLCζ in patient sperm; low fertilization success | Yan et al. [161] |
| I489F | C2 | Reduced/absent oscillations following cRNA injections in mouse oocytes; reduced embryogenesis in mouse; predicted alteration of local protein fold; similar enzymatic properties, but dramatically reduced substrate binding | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Escoffier et al. [154]; Nomikos et al. [156] |
| S500L | C2 | Predicted alteration of local protein fold | OAD; reduced/absent PLCζ in patient sperm; abnormal PLCζ localization | Torra-Massana et al. [158] |
| R553P | C2 | Reduced/absent fertilization following cRNA injections in mouse oocytes; predicted alteration of local protein fold; mouse fertilization and embryogenesis comparable following injection of higher levels of mutant cRNA | Comparable levels of PLCζ in patient sperm | Yuan et al. [168] |
| M578T | After C2 | Predicted alteration of local protein fold; No activation success following cRNA injection in human oocytes | OAD; reduced/absent PLCζ in patient sperm; low fertilization success | Yan et al. [161] |
Abnormal embryogenesis
Nikiforaki et al. [169] indicated that an abnormally reduced ability of sperm to induce Ca2+ release in mouse oocytes could be linked to defective embryogenesis in cases of hydatidiform moles; abnormal human pregnancies associated with abnormal fertilization and severely stunted or absent embryonic development, affecting an estimated 0.1–0.3% of pregnancies. Separable into either complete or partial, the etiology for hydatidiform moles is largely unknown, but is attributed to an excess of paternally inherited chromosomes; the risk of occurrence of which is not eliminated by ART [170], suggesting the causative factor persists within gametes. Human sperm previously involved in recurrent cases of partial hydatidiform molar pregnancies did not trigger normal profiles of Ca2+ release upon injection into both mouse and human oocytes, leading to OAD. This is particularly striking as human PLCζ is demonstrably more potent in its activity compared with mouse PLCζ in mouse oocytes [38]. Such results imply either a severely reduced level of PLCζ in such human sperm, or at least PLCζ with a severely diminished capacity for PIP2 hydrolysis.
Indeed, a major causative factor underlying hydatidiform moles is thought to originate from the oocyte’s inability to adequately block polyspermy, a major component of oocyte activation driven by PLCζ [5, 169]. Such suggestions are interesting when viewed in conjunction with the observations of Hachem et al. [112] and Nozawa et al. [113], who as previously discussed reported a decreased profile of Ca2+ release in their transgenic PLCζ knockout mice. In particular, Nozawa et al. [113] also identified a significantly higher rate of polyspermy using sperm from PLCζ KO mice. However, Nikiforaki et al. [169] did not specifically examine levels of PLCζ within sperm of such cases. However, the hallmarks of defective PLCζ were present, and outcomes were strikingly similar to mouse models where PLCζ was defective.
Sperm DNA fragmentation
The integrity of sperm nuclei is emerging as an important consideration for successful reproductive outcomes, with high proportions of damaged or “fragmented” sperm nuclei (either in the form of single- or double-strand breaks) increasingly associated with low fertilization rates, poor embryo implantation, and increased miscarriage rates, particularly following IVF/ICSI, with higher levels of DNA fragmentation associated with poorer sperm parameters [171, 172], and decreased blastocyst formation and live birth rates [20, 173]. Higher miscarriage rates are also seemingly associated with higher rates of sperm DNA fragmentation, regardless of ART methodology used [174, 175].
Considering the increasing relevance of sperm DNA fragmentation to fertility treatment regimens, it is no surprise that studies have begun to generally indicate a significant negative correlation between sperm PLCζ and DNA fragmentation and/or DNA oxidation [165–167, 176]. However, this is currently the extent of the investigations in the literature with no studies yet investigating potential links between PLCζ localization patterns and DNA fragmentation and/or other indicative factors such as protamine status within sperm. Such investigations would be interesting to examine whether a particular pattern of PLCζ could be correlated with extents of DNA fragmentation.
Abnormal sperm parameters and morphology
Defects/deficiencies in PLCζ have been associated with cases of OAD by a large volume of scientific literature [5, 141, 142, 151–154, 158]. However, it is well known that poor sperm parameters as defined by the WHO [177] correlate strongly to lower rates of fertilization and fertility treatment success. Such parameters include sperm motility, concentration, semen volume, and of course sperm morphology. Fertilization rates of sperm exhibiting abnormal parameters are significantly lower compared with normozoospermic parameters, with increasing levels of defects sequentially decreasing success rates further [178, 179]. Injection of morphologically abnormal sperm is associated with lower implantation rates [180], while aneuploidies in resultant preimplantation embryos were correlated with diminished sperm quality [181]. Lower levels of PLCζ have been found in sperm from teratozoospermic (abnormal morphology; [162]), asthenoteratozoospermic (low count and abnormal morphology; [176]), and oligoasthenoteratozoospermic (low count, low motility, and abnormal morphology; [163]). A further negative correlation was also observed between levels of PLCζ and occurrence of varicocele [159].
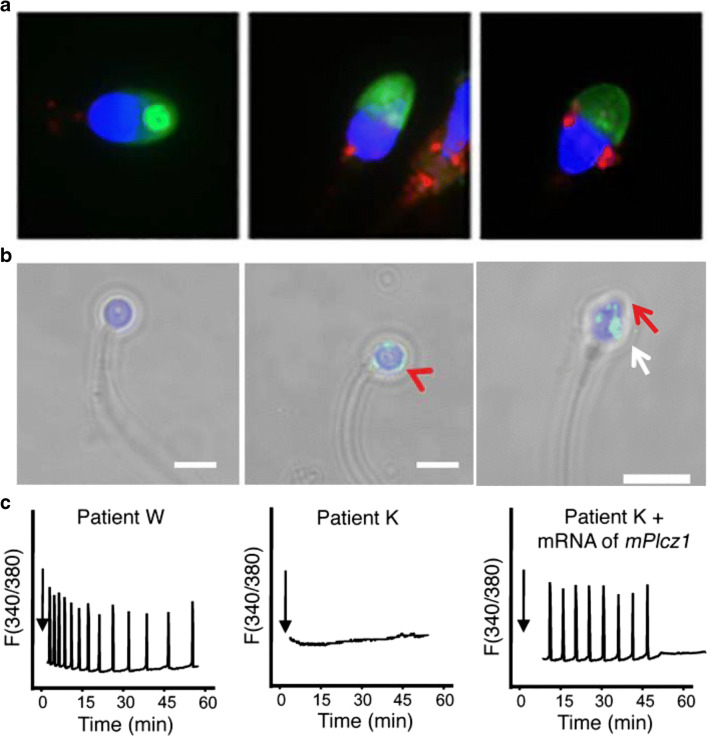
Importantly, there seems to be a significant relationship between specific features of sperm morphology and profiles of PLCζ. The most studied example in relation to PLCζ is that of globozoospermia, a condition characterized by round sperm heads devoid of an acrosome [182]. Some patients present 100% abnormal spermatozoa, while others present a mixture of normal and globozoospermic sperm [148]. Regardless, patients with globozoospermia exhibit low success in oocyte activation without clinical intervention [5, 183], while such sperm exhibit absent/reduced levels of PLCζ with a significantly altered profile of localization, and usually require clinical intervention for ICSI success [5, 183–187] (Fig. 5).
Fig. 5.
Representative immunofluorescence images of sperm from infertile males that were either diagnosed with oocyte activation deficiency, patients from whom PLCζ mutations were identified, or globozoospermic sperm. a Sperm PLCζ is either absent or severely reduced in such sperm with normal morphology or exhibits a significantly abnormal and punctate pattern of localization. b Globozoospermic sperm also exhibits either absent or severely reduced levels of PLCζ. Where some levels of PLCζ are observed, localization patterns are considerably abnormal (red arrowhead). However, in globozoospermic sperm exhibiting an acrosomal bud (red arrow) as selected by motile sperm organelle morphology evaluation (MSOME) using high power magnification, PLCζ is present at higher levels, albeit in abnormal localization conformations (white arrow). White scale bars indicate 5 μm. c Injection of normal human sperm in mouse oocytes exhibited normal Ca2+ oscillatory activity (left-most panel), while injection of sperm from an oocyte activation–deficient male is unable to initiate Ca2+ release following microinjection in mouse oocytes (middle panel). However, injection of sperm from the same patient co-incident with mouse PLCζ mRNA successfully initiated fertilization-like Ca2+ oscillations. Figures adapted from Yoon et al. [92], Kashir et al. [186], and Dai et al. [157] with permission
However, when sperm from a globozoospermic population exhibiting a small acrosomal bud were selected and injected using intracytoplasmic morphologically selected sperm injection (IMSI), pregnancy could successfully be achieved [188]. PLCζ localization in such sperm with an acrosomal bud indicated an acrosomal pattern of localization, while PLCζ exhibited a dispersed pattern of localization in round-headed sperm without an acrosomal bud that resulted in oocyte activation failure [187]. A similar pattern of abnormally localized PLCζ was observed in sperm from a proposed mouse model of globozoospermia (Heytens et al., 2010), indicating that perhaps PLCζ profiles are strongly linked with specific morphological features of sperm. However, the literature currently lacks specific focused studies in this regard.
Azoospermia and round spermatid injection
Perhaps the most severe forms of male infertility involve a complete absence of sperm in the ejaculate, otherwise known as azoospermia, a condition affecting ~ 1% of the global male population and ~ 10–15% of the infertile male population [189]. Characterized as either obstructive or non-obstructive azoospermia, ~ 90–95% of azoospermic men are diagnosed with non-obstructive azoospermia [190]. Microscopic testicular sperm extraction (micro-TESE) is widely used to extract testicular spermatozoa which may be utilized in ART procedures via ICSI in attempts to treat such conditions [190]. However, ~ 30–40% of such patients, who experience more severe forms of spermatogenic arrest, do not present with testicular sperm or late-stage spermatids, instead presenting only round spermatids if at all [190]. To address such cases, a modified version of ICSI is applied, termed round spermatid injection (ROSI).
Hamster and mouse round spermatids form pronuclei in oocytes with the capability of syngamy [186] and successful fertilization and birth following ROSI [191–193]. While ROSI has also been successfully performed in humans [194–198], such reports are few, perhaps due to concerns surrounding the efficiency, safety, and practical value of ROSI in humans [199–201], but mostly due to strikingly low efficacy of human ROSI [190, 202]. Perhaps a reason may be inefficiency of determining cell type following micro-TESE, as human round spermatids (the smallest testicular spermatogenic cells) do not exhibit distinct structural features that would allow identification from other cell types [190]. However, even paying close attention to such detail does not seem to enhance live birth rates, despite slightly increasing pregnancy rates. Astoundingly, rates of miscarriage following such procedures seem quite high, ranging from 55 to 65% [190, 202].
It does seem, however, that human round spermatids contain at least some oocyte-activating ability, which would readily contribute towards activation [203]. Ogonuki et al. [204] demonstrated that mouse ROSI induces small Ca2+ oscillations. Thus, perhaps similar to cases of oocyte activation failure following ICSI, round spermatids may also present with absent/reduced/deficient PLCζ. Indeed, it is interesting that a major structural identifying criterion for round spermatids is the presence of an acrosomal vesicle/cap [190, 204], a structure linked to IMSI success with globozoospermic sperm as previously discussed [186, 188]. In mouse, rabbit, rat, and pig, PLCζ protein has not been detected at the round spermatid stage [91, 94, 139, 149, 150], while rat, mouse, and rabbit ROSI does not necessarily result in efficient oocyte activation without artificial induction, requiring additional stimuli to significantly increase success rates [192, 203, 205–208].
Such experiments suggest that either insufficient PLCζ is present at this stage or somehow requires processing or further modifications. Similar investigations have yet to be performed on humans, but it is worth noting that round spermatids from hamsters and humans are able to successfully elicit Ca2+ oscillations following injection into mouse oocytes [203, 205, 209]. However, this is likely due to increased activity of the human and hamster versions of the enzyme in mouse oocytes. Thus, it is essential that efforts are made to further understand such issues, if such knowledge can be effectively applied within the clinic.
Clinical applications of PLCζ-induced Ca2+ oscillations
Infertile human sperm unable to activate human and mouse oocytes (OAD) can be linked to an inability to elicit effective Ca2+ oscillations, if at all [92]. Furthermore, abrogating PLCζ activity and/or levels within the sperm [92, 141, 142, 144, 148, 151–153, 158] can also be closely correlated with such cases. Indeed, reduced/absent levels of PLCζ are a hallmark of such sperm [5, 92, 141, 210]. However, as discussed previously, growing numbers of male factor conditions affecting sperm DNA integrity, morphology, count, and motility are being associated with similar absent/reduced profiles of PLCζ as with OAD sperm. Perhaps most significantly, abnormalities in levels/localization patterns of PLCζ, or at least the associated profiles of Ca2+ release, are increasingly linked with the efficacy of cell cycle resumption rates and resulting embryogenesis [55, 169].
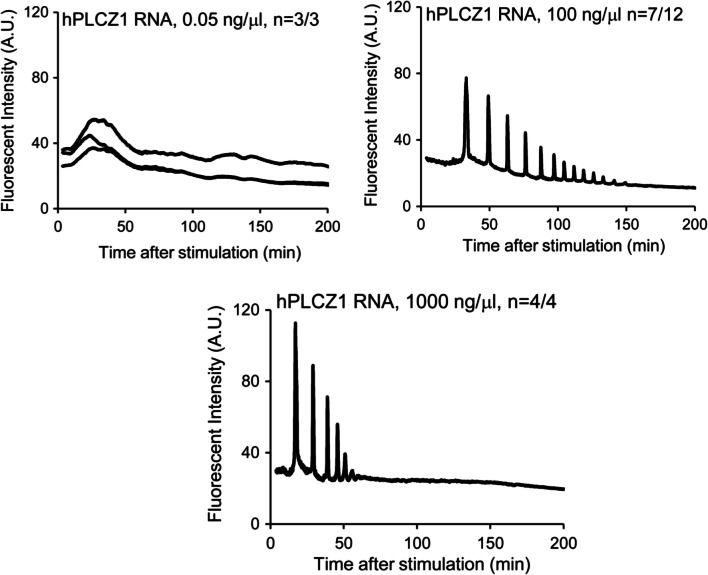
Altering the frequency and/or amplitude of Ca2+ release in mouse oocytes directly affected the efficacy of subsequent embryonic development [43, 44, 211–213]. Furthermore, the specific pattern of Ca2+ release directly affected the number of cells observed in the inner cell mass and trophectoderm in mouse embryos, while post-implantation development was also improved by extending the time of Ca2+ exposure. Collectively, such data suggest that specific profiles of Ca2+ oscillations may exert effect upon long-term embryogenesis in addition to serving as a stimulus for meiotic resumption [214]. However, not all profiles of Ca2+ release yield good-quality embryos [47, 215, 216], making specific amounts of PLCζ (and resultant Ca2+ release profiles) of potential importance for subsequent embryogenic events (Fig. 6). Thus, sperm PLCζ abnormalities may underlie not only infertility directly through fertilization failure but also perhaps cases of male subfertility whereby enough PLCζ may be delivered to oocytes to cause activation, but insufficient for competent embryogenesis. Analysis of PLCζ in human sperm thus represents an attractive diagnostic approach to isolate such cases, to examine whether specific correlations between profiles of PLCζ can be linked to a more general population of males, and not just male factor infertility/subfertility. It is also urgently necessary to examine whether profiles of PLCζ can also be linked to efficacies of resultant embryogenesis.
Fig. 6.
Representative calcium (Ca2+) release patterns in human oocytes induced in response to injections of increasing concentrations of human PLCζ RNA. The point of injection was set as the zero time, while the number of oocytes displaying Ca2+ responses per total number of oocytes examined is also indicated. Figure adapted from Yamaguchi et al. [217], with permission
PLCζ diagnostic approaches
Significant issues remain regarding analysis of PLCζ within human sperm, as most studies have assessed levels of sperm PLCζ RNA rather than protein. Considering that a role for PLCζ RNA at fertilization has yet to be confirmed, such investigations require further evaluation. An alternative approach to indirectly measure sperm PLCζ deficiency has employed microinjection of human sperm into mouse oocytes (known as the mouse oocyte activation test; MOAT), followed by examination of resultant Ca2+ oscillations [5, 215]. However, human PLCζ activity potency is significantly enhanced compared with mouse PLCζ when injected into mouse oocytes [38, 86], with even a significantly diminished level of human PLCζ able to result in high frequency and amplitude Ca2+ oscillations in mouse oocytes. Thus, while such approaches would represent a powerful research and diagnostic tool for specific cases of severe OAD where PLCζ would be completely absent or considerably reduced from sperm, a similar approach would not be able to detect case where a more subtle reduction in PLCζ is present, enough to impact clinical human cases.
Thus far, the most widely used approach is immunocytological analysis of sperm PLCζ protein [5, 92, 141–144, 148, 151, 152, 154, 157, 158, 165, 211, 218, 219]. The existing infrastructure of ART clinics would be well equipped for such analysis, with basic microscopy facilities with which to perform such methods. However, a large number of antibodies employed in humans to study PLCζ exhibit high levels of non-specificity, recognizing multiple protein bands following sperm immunoblotting, in addition to PLCζ. Some antibodies also yield inconsistent results between separate studies ([92, 141, 148, 154]; for detailed review, see Kashir et al. [29]).
This is problematic as most studies have thus far relied solely upon a single antibody with demonstrably low specificity for PLCζ, making it difficult to distinguish between PLCζ and other proteins upon immunocytological analysis. This is particularly concerning for PLCζ localization patterns, where a dominant localization has yet to be related to fertilization/fertility outcome. Such issues may result in most data being artificially skewed, resulting in misleading conclusions by studies which have not paid due attention to such issues. Thus, while PLCζ exhibits great promise as a clinical prognostic factor, research and clinical application has been limited, preventing a methodical analysis of such potential. Such issues would require urgent addressing with specific tools before such examinations can be applied clinically.
PLCζ therapeutic potential
ICSI failure can currently be remedied via assisted oocyte activation (AOA) methodologies, involving an artificial chemical induction of Ca2+ release following application of ICSI protocols. The most commonly applied agents in both research and clinical arenas are Ca2+ ionophores A23187 and strontium chloride [220–222]. Numerous reports demonstrate ICSI combined with AOA significantly enhances fertilization and pregnancy rates (for review, see [29]). However, clinical application of such agents remains limited as human oocytes respond poorly to most individual chemical induction protocols, relying on a combination of chemical treatments coupled with sperm injection. Furthermore, only minor improvements (at best) are observed in fertilization and pregnancy rates [223]. Ca2+ ionophores evoke significantly uncharacteristic single transients of Ca2+ release; with only strontium chloride (Sr2+Cl) thus far reported to produce oscillations in mice, leading to oocyte activation and parthenogenesis [223]. However, Sr2+Cl efficacy in humans remains debatable, wherein no Ca2+ oscillations are observed in most cases examined [29].
Thus, more endogenous clinical treatments need to be developed to overcome the controversial aspects of AOA [29], which could potentially be represented by recombinant PLCζ. Yoon et al. [92] showed that defective sperm PLCζ could be overcome by co-injection with mouse PLCζ, while Rogers et al. [215] demonstrated parthenogenetic generation of blastocysts following PLCζ injection into human oocytes. Furthermore, success rates following PLCζ co-injection with sperm from a mouse model of ICSI failure were comparable with control sperm injections [224]. Indeed, the production of purified and enzymatically active recombinant human PLCζ protein has been widely attempted to varying degrees of success. Following significant efforts by multiple studies that sequentially advanced research efforts [142, 225], Nomikos et al. [226] demonstrated production of purified and highly active recombinant PLCζ protein, able to induce characteristic Ca2+ oscillations upon injection into mouse and human oocytes. This could be done in a reliable and relatively consistent manner, but potential differences in quality of enzymatic activity between batches produced were not extensively examined.
While recombinant PLCζ represents a potentially powerful therapeutic for patients diagnosed with OAD, perhaps such an approach may also be applicable to a wider range of patients where fertilization occurs, but embryogenesis is poor. Indeed, as previously discussed, PLCζ levels within sperm may exert significant and direct effects upon the rate and efficacy of embryogenesis, perhaps underlying numerous cases of recurrent implantation failure attributable to poor embryogenic efficacy. However, generation of purified recombinant PLCζ remains to be routinely utilized in scientific examination. It is not yet clear whether production in bacterial cell lines is also of concern due to lack of physiological biochemical modifications, as a focused set of clinical trials are required.
A further difficulty is that administration of such therapeutic PLCζ would currently require the use of co-injections with sperm and protein directly into oocytes via ICSI. Considering that the amount of PLCζ protein delivered to the oocyte potentially directly determines the quality of embryogenesis, such injection methods could prove unreliable and inaccurate, even with significant expertise and training. Finally, reliable and effective production of purified recombinant PLCζ protein has only been achieved using considerably large purification tags, a necessary measure to prevent protein degradation and inactivation [142, 224, 226], with optimization using more effective and acceptable purification tags required before clinical application can be considered. Thus, while avenues for such a therapeutic are exciting and represent a powerful clinical tool, much research is required before a realistic pathway to clinical application is achieved.
Indeed, previous studies have limited the investigation of the utility for PLCζ as a therapeutic and/or diagnostic intervention for specific cases of severe OAD, with little attention paid to the other conditions of male infertility highlighted in this review which are increasingly being linked with PLCζ abrogation. Considering such emerging connections, perhaps it is prudent to further investigate whether application of PLCζ could potentially increase ART success rates as a whole, and not just “rescue”-specific cases of OAD. Collectively, studies now indicate that the specific dynamics of Ca2+ release at oocyte activation directly impacts upon the efficacy of embryogenesis, the quality of embryos produced, as well as the quality of post-implantation embryogenesis. While it remains to be investigated whether a specific pre-requisite number or profile of Ca2+ release is required for normal development to term, the profiles of Ca2+ release impact most currently known pre-requisites for normal development to term.
Alternative Ca2+-based interventions
Given the potential difficulties associated with PLCζ-based modes of treatment, or direct Ca2+-based interventions such as AOA, perhaps a more modulatory approach could be considered to potentially aid such cases of defective PLCζ-induced Ca2+ release. Recent investigations have indicated that Ca2+ influx, while not directly responsible for meiotic resumption, is an important downstream aspect of oocyte activation, not only involved in maintaining Ca2+ oscillations by replenishing Ca2+ stores but also underlying specific pathways underlying specific events of oocyte activation such as polar body emission and cortical granule exocytosis [226]. Evidence also suggests that defects in such mechanisms potentially also lead to alterations in developmental potential of offspring when mediators of Ca2+ influx including the TRPM7 and CaV3.2 channels are lacking in oocytes, which also exhibit a premature cessation of Ca2+ oscillations [227].
Considering such potential importance underlying influx mechanisms (a sorely understudied area of oocyte activation and Ca2+ regulation at fertilization), perhaps mediation of the mechanisms underlying influx processes could represent an alternative method of treatment for cases of OAD and associated conditions of PLCζ deficiency. Both the TRPM7 and CaV3.2 channels almost completely account for Ca2+ influx in at least mammalian oocytes, while TRPM7 acts as a membrane sensor of extracellular magnesium (Mg2+) and Ca2+ concentrations, modulating the dynamics of the Ca2+ oscillatory response at fertilization [227]. Interestingly, Ozil et al. [228] indicated that altering the extracellular Mg2+:Ca2+ ratio in culture media of mouse oocytes and embryos altered Ca2+ release dynamics in oocytes at fertilization, as well as the developmental capacity of embryos.
Specifically, decreasing the concentration of Mg2+ from culture media increased the frequency and amplitude of Ca2+ release in fertilizing oocytes, suggesting that limiting Mg2+ availability in culture media may represent a potential intervention to increase Ca2+ release in cases where PLCζ-induced Ca2+ release may be defective via influx mechanisms including TRPM7. Indeed, decreased concentrations of Mg2+ during IVF increased embryogenesis efficacy in mice and cats, as well as following ICSI in human embryos (suggesting that such sensitivity to Mg2+ in culture medium during the oocyte-to-embryo transition is conserved in at least mammals [229, 230]. However, focused clinical studies have not yet been undertaken to examine the overall effects of such alterations in culture media, made perhaps more difficult by the reluctance of commercial entities to release the specific composition of commercially available clinical culture media for human embryos. It is thus essential that such investigations be performed to examine whether modulation of Ca2+ influx mechanisms through alteration of culture media composition would improve pregnancy and delivery rates in the clinic, particularly in relation to PLCζ-associated conditions.
Conclusions and future directions
PLCζ has increasingly gained wide acceptance as the pivotal “sperm factor” required for mammalian oocyte activation fertilization. It is increasingly clear that levels and localization patterns of PLCζ are closely linked to specific cases of sperm defects such as abnormal sperm parameters and morphology, high prevalence of DNA fragmentation, and is also potentially associated with cases of abnormal embryogenesis. As numerous clinical reports continue to emerge, it is clear that numerous cases of male infertility in addition to OAD may benefit from the application of PLCζ as a therapeutic and diagnostic measure. Indeed, defective PLCζ and abnormal patterns of Ca2+ release are increasingly being suspected to be a significant causative factor underlying abnormalities or insufficiencies in Ca2+ oscillation-driven early embryogenic events, mediated by abnormalities or insufficiencies in sperm PLCζ. However, despite significant advances in knowledge and data over recent years, particularly on the clinical front, the exact biochemical mechanisms governing PLCζ action and regulation within the fertilizing sperm and oocyte remains elusive. Furthermore, while numerous clinical associations directly link OAD with abrogation of PLCζ, such findings necessitate global efforts to further ascertain the extent of the potential role played by PLCζ in other forms of male infertility, and perhaps also defective embryogenesis and recurrent implantation failure.
Indeed, Kashir et al. [219] demonstrated the necessity of specific antigen unmasking/retrieval (AUM) protocols enhances visualization efficacy of PLCζ in mouse, porcine, and human sperm, purportedly due to strong intra-/inter-molecular interactions with PLCζ of either PLCζ oligomers or other modulatory proteins. Such requirements for AUM perhaps suggest that previously published data regarding PLCζ localization requires re-evaluation [219]. A further conundrum is that levels and localization patterns, especially within human sperm, seem considerably variable between not only infertile patient populations but also within sperm from fertile individuals [46]. Perhaps this may be due to differences between protocols applied between different studies, or perhaps due to limited specificity of the polyclonal antibodies employed thus far [29]. Indeed, multiple studies report differential patterns of PLCζ localization within mouse and human sperm despite using the same antibodies (or antibodies raised against the same peptide sequences) [92, 93, 140–144, 154].
Thus, while encouraging advances have indeed been made, it is imperative that caution is exercised, with current outstanding concerns underlying PLCζ biochemistry and physiology coupled with rigorous clinical trials before routine clinical applications can be recommended. However, while there are indeed numerous questions that remain to be answered, the clinical applications for PLCζ seem to grow with each novel study published, which significantly enhances hope for providing diagnostic measures and therapeutic interventions to enhance existing fertility treatments.
Author contributions
JK conceived, planned, and collated studies for this article, and wrote the final manuscript.
Funding information
JK was supported by a Healthcare Research Fellowship Award (HF-14-16) made by Health and Care Research Wales (HCRW), alongside a National Science, Technology, and Innovation plan (NSTIP) project grant (15-MED4186-20) awarded by the King Abdulaziz City for Science and Technology (KACST).
Compliance with ethical standards
Conflict of interest
The author declares that he has no conflict of interest.
Ethics statement approval of research involving regulated animals
Use of mouse and human sperm cells was performed in accordance with the principles of the Basel Declaration and recommendations of the Animal Care and Use Committee (ACUC) at the Office of Research Affairs (ORA) at the King Faisal Specialist Hospital and Research Center, Riyadh, Kingdom of Saudi Arabia. The protocols utilized for the relevant studies (RAC-2160014 and 2160015) were approved by the ACUC. For the involvement of human subjects, samples were only obtained following informed written consent, and were performed according to the Declaration of Helsinki.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.European IVF-Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE), Calhaz-Jorge C, de Geyter C, Kupka MS, de Mouzon J, Erb K, et al. Assisted reproductive technology in Europe, 2012: results generated from European registers by ESHRE. Hum Reprod. 2016;31(8):1638–52. [DOI] [PubMed]
- 2.Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European Association of Urology guidelines on male infertility: the 2012 update. Eur Urol. 2012;62(2):324–32. [DOI] [PubMed]
- 3.Hotaling JM. Genetics of male infertility. Urol Clin North Am. 2014;41:1–17. doi: 10.1016/j.ucl.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Gunes S, Arslan MA, Hekim GNT, Asci R. The role of epigenetics in idiopathic male infertility. J Assist Reprod Genet. 2016;33:553–569. doi: 10.1007/s10815-016-0682-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kashir J, Heindryckx B, Jones C, De Sutter P, Parrington J, Coward K. Oocyte activation, phospholipase C zeta and human infertility. Hum Reprod Update. 2010;16:690–703. doi: 10.1093/humupd/dmq018. [DOI] [PubMed] [Google Scholar]
- 6.Botezatu A, Socolov R, Socolov D, Iancu IV, Anton G. Methylation pattern of methylene tetrahydrofolate reductase and small nuclear ribonucleoprotein polypeptide N promoters in oligoasthenospermia: a case-control study. Reprod BioMed Online. 2014;28(2):225–231. doi: 10.1016/j.rbmo.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Sousa M, Tesarik J. Fertiliza1tion and early embryology: ultrastructural analysis of fertilization failure after intracytoplasmic sperm injection. Hum Reprod. 1994;9:2374–2380. doi: 10.1093/oxfordjournals.humrep.a138455. [DOI] [PubMed] [Google Scholar]
- 8.Mahutte NG, Arici A. Failed fertilization: is it predictable? Curr Opin Obstet Gynecol. 2003;15(3):211–218. doi: 10.1097/00001703-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Amdani SN, Yeste M, Jones C, Coward K. Phospholipase C zeta (PLCζ) and male infertility: clinical update and topical developments. Adv Biol Regul. 2016;61:58–67. doi: 10.1016/j.jbior.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Polanski LT, Baumgarten MN, Quenby S, Brosens J, Campbell BK, Raine-Fenning NJ. What exactly do we mean by ‘recurrent implantation failure’? A systematic review and opinion. Reprod BioMed Online. 2014;28(4):409–423. doi: 10.1016/j.rbmo.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Dyer S, Chambers GM, de Mouzon J, Nygren KG, Zegers-Hochschild F, Mansour R, et al. International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology 2008, 2009 and 2010. Hum Reprod. 2016;31(7):1588–609. [DOI] [PubMed]
- 12.Fauque P, Léandri R, Merlet F, Juillard JC, Epelboin S, Guibert J, et al. Pregnancy outcome and live birth after IVF and ICSI according to embryo quality. J Assist Reprod Genet. 2007;24(5):159–65. [DOI] [PMC free article] [PubMed]
- 13.Pelinck MJ, Hoek A, Simons AH, Heineman MJ, van Echten-Arends J, Arts EG. Embryo quality and impact of specific embryo characteristics on ongoing implantation in unselected embryos derived from modified natural cycle in vitro fertilization. Fertil Steril. 2010;94:527–534. doi: 10.1016/j.fertnstert.2009.03.076. [DOI] [PubMed] [Google Scholar]
- 14.Loutradi KE, Tarlatzis BC, Goulis DG, Zepiridis L, Pagou T, Chatziioannou E, et al. The effects of sperm quality on embryo development after intracytoplasmic sperm injection. J Assist Reprod Genet. 2006;23(2):69–74. [DOI] [PMC free article] [PubMed]
- 15.Oseguera-López I, Ruiz-Díaz S, Ramos-Ibeas P, Pérez-Cerezales S. Novel techniques of sperm selection for improving IVF and ICSI outcomes. Front Cell Dev Biol. 2019;7:298. doi: 10.3389/fcell.2019.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gannon JR, Emery BR, Jenkins TG, Carrell DT. The sperm epigenome: implications for the embryo. Adv Exp Med Biol. 2014;791:53–66. doi: 10.1007/978-1-4614-7783-9_4. [DOI] [PubMed] [Google Scholar]
- 17.Jenkins TG, Aston KI, James ER, Carrell DT. Sperm epigenetics in the study of male fertility, offspring health, and potential clinical applications. Syst Biol Reprod Med. 2017;63(2):69–76. doi: 10.1080/19396368.2016.1274791. [DOI] [PubMed] [Google Scholar]
- 18.Denomme MM, McCallie BR, Parks JC, Schoolcraft WB, Katz-Jaffe MG. Alterations in the sperm histone-retained epigenome are associated with unexplained male factor infertility and poor blastocyst development in donor oocyte IVF cycles. Hum Reprod. 2017;32(12):2443–2455. doi: 10.1093/humrep/dex317. [DOI] [PubMed] [Google Scholar]
- 19.Carrell DT, Salas-Huetos A, Hotaling J. Increasing evidence of the role of the sperm epigenome in embryogenesis: oligoasthenoteratozoospermia, altered embryo DNA methylation, and miscarriage. Fertil Steril. 2018;110(3):401–402. doi: 10.1016/j.fertnstert.2018.04.042. [DOI] [PubMed] [Google Scholar]
- 20.Alvarez Sedó C, Bilinski M, Lorenzi D, Uriondo H, Noblía F, Longobucco V, et al. Effect of sperm DNA fragmentation on embryo development: clinical and biological aspects. JBRA Assist Reprod. 2017;21(4):343–50. [DOI] [PMC free article] [PubMed]
- 21.Esbert M, Pacheco A, Soares SR, Amorós D, Florensa M, Ballesteros A, et al. High sperm DNA fragmentation delays human embryo kinetics when oocytes from young and healthy donors are microinjected. Andrology. 2018;6(5):697–706. [DOI] [PubMed]
- 22.Borges E, Jr, Zanetti BF, Setti AS, Braga DPAF, Provenza RR, Iaconelli A., Jr Sperm DNA fragmentation is correlated with poor embryo development, lower implantation rate, and higher miscarriage rate in reproductive cycles of non-male factor infertility. Fertil Steril. 2019;112(3):483–490. doi: 10.1016/j.fertnstert.2019.04.029. [DOI] [PubMed] [Google Scholar]
- 23.Kim ST, Moley KH. Paternal effect on embryo quality in diabetic mice is related to poor sperm quality and associated with decreased glucose transporter expression. Reproduction. 2008;136(3):313–322. doi: 10.1530/REP-08-0167. [DOI] [PubMed] [Google Scholar]
- 24.Binder NK, Mitchell M, Gardner DK. Parental diet-induced obesity leads to retarded early mouse embryo development and altered carbohydrate utilisation by the blastocyst. Reprod Fertil Dev. 2012;24(6):804–812. doi: 10.1071/RD11256. [DOI] [PubMed] [Google Scholar]
- 25.Braga DP, Halpern G, Setti AS, Figueira RC, Iaconelli A, Jr, Borges E., Jr The impact of food intake and social habits on embryo quality and the likelihood of blastocyst formation. Reprod BioMed Online. 2015;31(1):30–38. doi: 10.1016/j.rbmo.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Chen Q, Yan M, Cao Z, Li X, Zhang Y, Shi J, et al. Sperm tsRNAs contribute to intergenerational inheritance of an acquired metabolic disorder. Science. 2016;351(6271):397–400. [DOI] [PubMed]
- 27.Sharma U, Conine CC, Shea JM, Boskovic A, Derr AG, Bing XY, et al. Biogenesis and function of tRNA fragments during sperm maturation and fertilization in mammals. Science. 2016;351(6271):391–6. [DOI] [PMC free article] [PubMed]
- 28.Watkins AJ, Sirovica S, Stokes B, Isaacs M, Addison O, Martin RA. Paternal low protein diet programs preimplantation embryo gene expression, fetal growth and skeletal development in mice. Biochim Biophys Acta Mol basis Dis. 2017;1863(6):1371–1381. doi: 10.1016/j.bbadis.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Kashir J, Nomikos M, Lai FA. Phospholipase C zeta and calcium oscillations at fertilization: the evidence, applications, and further questions. Adv Biol Regul. 2018;67:148–162. doi: 10.1016/j.jbior.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 30.Kline D, Kline T. Repetitive calcium transients and the role of calcium in exocytosis and cell cycle activation in the mouse egg. Dev Biol. 1992;149:80–89. doi: 10.1016/0012-1606(92)90265-i. [DOI] [PubMed] [Google Scholar]
- 31.Swann K, Ozil JP. Dynamics of the calcium signal that triggers mammalian egg activation. Int Rev Cytol. 1994;152:183–222. doi: 10.1016/s0074-7696(08)62557-7. [DOI] [PubMed] [Google Scholar]
- 32.Stricker SA. Comparative biology of calcium signalling during fertilization and egg activation in mammals. Dev Biol. 1999;211:57–176. doi: 10.1006/dbio.1999.9340. [DOI] [PubMed] [Google Scholar]
- 33.Miyazaki S, Ito M. Calcium signals for egg activation in mammals. J Pharmacol Sci. 2006;100:545–552. doi: 10.1254/jphs.cpj06003x. [DOI] [PubMed] [Google Scholar]
- 34.Horner VL, Wolfner MF. Transitioning from egg to embryo: triggers and mechanisms of egg activation. Dev Dyn. 2008;237(3):527–544. doi: 10.1002/dvdy.21454. [DOI] [PubMed] [Google Scholar]
- 35.Swann K, Yu Y. The dynamics of calcium oscillations that activate mammalian eggs. Int J Dev Biol. 2008;52:585–594. doi: 10.1387/ijdb.072530ks. [DOI] [PubMed] [Google Scholar]
- 36.Ito J, Parrington J, Fissore RA. PLCζ and its role as a trigger of development in vertebrates. Mol Reprod Dev. 2011;78(10–11):846–853. doi: 10.1002/mrd.21359. [DOI] [PubMed] [Google Scholar]
- 37.Parrington J. Does a soluble sperm factor trigger calcium release in the egg at fertilization? J Androl. 2001;22:1–11. [PubMed] [Google Scholar]
- 38.Swann K, Saunders CM, Rogers NT, Lai FA. PLCzeta (zeta): a sperm protein that triggers Ca2+ oscillations and egg activation in mammals. Semin Cell Dev Biol. 2006;17:264–273. doi: 10.1016/j.semcdb.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 39.Whitaker M. Calcium at fertilization and in early development. Physiol Rev. 2006;86:25–88. doi: 10.1152/physrev.00023.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parrington J, Davis LC, Galione A, Wessel G. Flipping the switch: how a sperm activates the egg at fertilization. Dev Dyn. 2007;236:2027–2038. doi: 10.1002/dvdy.21255. [DOI] [PubMed] [Google Scholar]
- 41.Saunders CM, Swann K, Lai FA. PLCzeta, a sperm-specific PLC and its potential role in fertilization. Biochem Soc Symp. 2007;74:23–36. doi: 10.1042/BSS0740023. [DOI] [PubMed] [Google Scholar]
- 42.Miyazaki S, Shirakawa H, Nakada K, Honda Y. Essential role of the inositol 1,4,5-trisphosphate receptor/Ca2+ release channel in Ca2+ waves and Ca2+ oscillations at fertilization of mammalian eggs. Dev Biol. 1993;158:62–78. doi: 10.1006/dbio.1993.1168. [DOI] [PubMed] [Google Scholar]
- 43.Ducibella T, Huneau D, Angelichio E, Xu Z, Schultz RM, Kopf GS, et al. Egg-to-embryo transition is driven by differential responses to Ca(2+) oscillation number. Dev Biol. 2002;250:280–91. [PubMed]
- 44.Ducibella T, Schultz RM, Ozil JP. Role of calcium signals in early development. Semin Cel Dev Biol. 2006;17:324–332. doi: 10.1016/j.semcdb.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 45.Kashir J, Nomikos M, Lai FA, Swann K. Sperm-induced Ca2+ release during egg activation in mammals. Biochem Biophys Res Commun. 2014;450:1204–1211. doi: 10.1016/j.bbrc.2014.04.078. [DOI] [PubMed] [Google Scholar]
- 46.Kashir J, Deguchi R, Jones C, Coward K, Stricker SA. Comparative biology of sperm factors and fertilization-induced calcium signals across the animal kingdom. Mol Reprod Dev. 2013;80(10):787–815. doi: 10.1002/mrd.22222. [DOI] [PubMed] [Google Scholar]
- 47.Fulton BP, Whittingham DG. Activation of mammalian oocytes by intracellular injection of calcium. Nature. 1978;273:149–151. doi: 10.1038/273149a0. [DOI] [PubMed] [Google Scholar]
- 48.Miyazaki S, Yuzaki M, Nakada K, Shirakawa H, Nakanishi S, Nakade S, et al. Block of Ca2+ wave and Ca2+ oscillation by antibody to the inositol 1,4,5-trisphosphate receptor in fertilized hamster eggs. Science. 1992;257:251–5. [DOI] [PubMed]
- 49.Brind S, Swann K, Carroll J. Inositol 1,4,5-trisphosphate receptors are downregulated in mouse oocytes in response to sperm or adenophostin A but not to increases in intracellular Ca(2+) or egg activation. Dev Biol. 2000;223:251–265. doi: 10.1006/dbio.2000.9728. [DOI] [PubMed] [Google Scholar]
- 50.Jellerette T, He CL, Wu H, Parys JB, Fissore RA. Down-regulation of the inositol 1,4,5-trisphosphate receptor in mouse eggs following fertilization or parthenogenetic activation. Dev Biol. 2000;223:238–250. doi: 10.1006/dbio.2000.9675. [DOI] [PubMed] [Google Scholar]
- 51.Xu Z, Williams CJ, Kopf GS, Schultz RM. Maturation-associated increase in IP3 receptor type 1: role in conferring increased IP3 sensitivity and Ca2+ oscillatory behavior in mouse eggs. Dev Biol. 2003;254:163–171. doi: 10.1016/s0012-1606(02)00049-0. [DOI] [PubMed] [Google Scholar]
- 52.Malcuit C, Kurokawa M, Fissore RA. Calcium oscillations and mammalian egg activation. J Cell Physiol. 2006;206:565–573. doi: 10.1002/jcp.20471. [DOI] [PubMed] [Google Scholar]
- 53.Stitzel ML, Seydoux G. Regulation of the oocyte-to-zygote transition. Science. 2007;316:407–408. doi: 10.1126/science.1138236. [DOI] [PubMed] [Google Scholar]
- 54.Ducibella T, Fissore R. The roles of Ca2+, downstream protein kinases, and oscillatory signaling in regulating fertilization and the activation of development. Dev Biol. 2008;315:257–279. doi: 10.1016/j.ydbio.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wong CC, Loewke KE, Bossert NL, Behr B, De Jonge CJ, Baer TM, et al. Non-invasive imaging of human embryos before embryonic genome activation predicts development to the blastocyst stage. Nat Biotechnol. 2010;28:1115–21. [DOI] [PubMed]
- 56.Yu Y, Saunders CM, Lai FA, Swann K. Preimplantation development of mouse oocytes activated by different levels of human phospholipase C zeta. Hum Reprod. 2008;23:365–373. doi: 10.1093/humrep/dem350. [DOI] [PubMed] [Google Scholar]
- 57.Swann K. A cytosolic sperm factor stimulates repetitive calcium increases and mimics fertilization in hamster eggs. Development. 1990;110:1295–1302. doi: 10.1242/dev.110.4.1295. [DOI] [PubMed] [Google Scholar]
- 58.Kyozuka K, Deguchi R, Mohri T, Miyazaki S. Injection of sperm extract mimics spatiotemporal dynamics of Ca2+ responses and progression of meiosis at fertilization of ascidian oocytes. Development. 1998;125:4099–4105. doi: 10.1242/dev.125.20.4099. [DOI] [PubMed] [Google Scholar]
- 59.Stricker SA. Intracellular injections of a soluble sperm factor trigger calcium oscillations and meiotic maturation in unfertilized oocytes of a marine worm. Dev Biol. 1997;186:185–201. doi: 10.1006/dbio.1997.8594. [DOI] [PubMed] [Google Scholar]
- 60.Dong JB, Tang TS, Sun FZ. Xenopus and chicken sperm contain a cytosolic soluble protein factor which can trigger calcium oscillations in mouse eggs. Biochem Biophys Res Commun. 2000;268:947–951. doi: 10.1006/bbrc.2000.2218. [DOI] [PubMed] [Google Scholar]
- 61.Coward K, Campos-Mendoza A, Larman M, Hibbitt O, McAndrew B, Bromage N, et al. Teleost fish spermatozoa contain a cytosolic protein factor that induces calcium release in sea urchin egg homogenates and triggers calcium oscillations when injected into mouse oocytes. Biochem Biophys Res Commun. 2003;305:299–304. [DOI] [PubMed]
- 62.Coward K, Ponting CP, Chang HY, Hibbitt O, Savolainen P, Jones KT, et al. Phospholipase Czeta, the trigger of egg activation in mammals, is present in a non-mammalian species. Reproduction. 2005;130:157–63. [DOI] [PubMed]
- 63.Nakano Y, Shirakawa H, Mitsuhashi N, Kuwabara Y, Miyazaki S. Spatiotemporal dynamics of intracellular calcium in the mouse egg injected with a spermatozoon. Mol Hum Reprod. 1997;3:1087–1093. doi: 10.1093/molehr/3.12.1087. [DOI] [PubMed] [Google Scholar]
- 64.Parrington J, Swann K, Shevchenko VI, Sesay AK, Lai FA. Calcium oscillations in mammalian eggs triggered by a soluble sperm protein. Nature. 1996;25:364–368. doi: 10.1038/379364a0. [DOI] [PubMed] [Google Scholar]
- 65.Sette C, Bevilacqua A, Bianchini A, Mangia F, Geremia R, Rossi P. Parthenogenetic activation of mouse eggs by microinjection of a truncated c-kit tyrosine kinase present in spermatozoa. Development. 1997;124:2267–2274. doi: 10.1242/dev.124.11.2267. [DOI] [PubMed] [Google Scholar]
- 66.Sette C, Bevilacqua A, Geremia R, Rossi P. Involvement of phospholipase Cgamma1 in mouse egg activation induced by a truncated form of the C-kit tyrosine kinase present in spermatozoa. J Cell Biol. 1998;142:1063–1074. doi: 10.1083/jcb.142.4.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sette C, Paronetto MP, Barchi M, Bevilacqua A, Geremia R, Rossi P. Tr-kit-induced resumption of the cell cycle in mouse eggs requires activation of a Src-like kinase. EMBO J. 2002;21:5386–5395. doi: 10.1093/emboj/cdf553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wu AT, Sutovsky P, Manandhar G, Xu W, Katayama M, Day BN, et al. PAWP, a sperm-specific WW domain-binding protein, promotes meiotic resumption and pronuclear development during fertilization. J Biol Chem. 2007;282:12164–75. [DOI] [PubMed]
- 69.Aarabi M, Qin Z, Xu W, Mewburn J, Oko R. Sperm-borne protein, PAWP, initiates zygotic development in Xenopus laevis by eliciting intracellular calcium release. Mol Reprod Dev. 2010;77:249–256. doi: 10.1002/mrd.21140. [DOI] [PubMed] [Google Scholar]
- 70.Swann K. Different triggers for calcium oscillations in mouse eggs involve a ryanodine-sensitive calcium store. Biochem J. 1992;287(Pt 1):79–84. doi: 10.1042/bj2870079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jones KT, Carroll J, Whittingham DG. Ionomycin, thapsigargin, ryanodine, and sperm induced Ca2+ release increase during meiotic maturation of mouse oocytes. J Biol Chem. 1994;270:6671–6677. doi: 10.1074/jbc.270.12.6671. [DOI] [PubMed] [Google Scholar]
- 72.Kline JT, Kline D. Regulation of intracellular calcium in the mouse egg: evidence for inositol trisphosphate-induced calcium release, but not calcium induced calcium release. Biol Reprod. 1994;50:193–203. doi: 10.1095/biolreprod50.1.193. [DOI] [PubMed] [Google Scholar]
- 73.Nader N, Kulkarni RP, Dib M, Machaca K. How to make a good egg! The need for remodeling of Ca2+ signaling to mediate the egg-to-embryo transition. Cell Calcium. 2013;53:41–54. doi: 10.1016/j.ceca.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 74.Wolosker H, Kline D, Bian Y, Blackshaw S, Cameron AM, Fralich TJ, et al. Molecularly cloned mammalian glucosamine-6-phosphate deaminase localizes to transporting epithelium and lacks oscillin activity. FASEB J. 1998;12:91–9. [DOI] [PubMed]
- 75.Parrington J, Jones KT, Lai FA, Swann K. The soluble sperm factor that causes Ca2+ release from sea urchin egg homogenates also triggers Ca2+ oscillations after injection into mouse eggs. Biochem J. 1999;341:1–4. [PMC free article] [PubMed] [Google Scholar]
- 76.Swann K, Larman MG, Saunders CM, Lai FA. The cytosolic sperm factor that triggers Ca2+ oscillations and egg activation in mammals is a novel phospholipase C: PLCzeta. Reproduction. 2004;127(4):431–439. doi: 10.1530/rep.1.00169. [DOI] [PubMed] [Google Scholar]
- 77.Kashir J, Nomikos M, Swann K, Lai FA. PLCζ or PAWP: revisiting the putative mammalian sperm factor that triggers egg activation and embryogenesis. Mol Hum Reprod. 2015;21(5):383–388. doi: 10.1093/molehr/gav009. [DOI] [PubMed] [Google Scholar]
- 78.Jones KT, Soeller C, Cannell MB. The passage of Ca2+ and fluorescent markers between the sperm and egg after fusion in the mouse. Development. 1998;125:4627–4635. doi: 10.1242/dev.125.23.4627. [DOI] [PubMed] [Google Scholar]
- 79.Jones KT, Matsuda M, Parrington J, Katan M, Swann K. Different Ca2+-releasing abilities of sperm extracts compared with tissue extracts and phospholipase C isoforms in sea urchin egg homogenate and mouse eggs. Biochem J. 2000;346(pt 3):743–749. [PMC free article] [PubMed] [Google Scholar]
- 80.Runft LL, Carroll DJ, Gillett J, Giusti AF, O’Neill FJ, Foltz KR. Identification of a starfish egg PLC-gamma that regulates Ca2+ release at fertilization. Dev Biol. 2004;269:220–236. doi: 10.1016/j.ydbio.2004.01.031. [DOI] [PubMed] [Google Scholar]
- 81.Coward K, Owen H, Tunwell R, Swann K, Parrington J. Phospholipid binding properties and functional characterization of a sea urchin phospholipase Cdelta in urchin and mouse eggs. Biochem Biophys Res Commun. 2007;357:964–970. doi: 10.1016/j.bbrc.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 82.Igarashi H, Knott JG, Schultz RM, Williams CJ. Alterations of PLCbeta1 in mouse eggs change calcium oscillatory behavior following fertilization. Dev Biol. 2007;312:321–330. doi: 10.1016/j.ydbio.2007.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yin X, Eckberg WR. Characterization of phospholipases C beta and gamma and their possible roles in Chaetopterus egg activation. Mol Reprod Dev. 2009;76:460–470. doi: 10.1002/mrd.20961. [DOI] [PubMed] [Google Scholar]
- 84.Aarabi M, Balakier H, Bashar S, Moskovtsev SI, Sutovsky P, Librach CL, et al. Sperm-derived WW domain-binding protein, PAWP, elicits calcium oscillations and oocyte activation in humans and mice. FASEB J. 2014;28:4434–40. [DOI] [PubMed]
- 85.Nomikos M, Sanders JR, Parthimos D, Buntwal L, Calver BL, Stamatiadis P, et al. Essential role of the EF-hand domain in targeting sperm phospholipase Czeta to membrane phosphatidylinositol 4,5-bisphosphate (PIP2). J Biol Chem. 2015;290:29519–30. [DOI] [PMC free article] [PubMed]
- 86.Nomikos M, Sanders JR, Theodoridou M, Kashir J, Matthews E, Nounesis G, et al. Sperm-specific postacrosomal WW-domain binding protein (PAWP) does not cause Ca2+ release in mouse oocytes. Mol Hum Reprod. 2014;20:938–947. doi: 10.1093/molehr/gau056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nomikos M, Sanders JR, Kashir J, Sanusi R, Buntwal L, Love D, et al. Functional disparity between human PAWP and PLCζ in the generation of Ca2+ oscillations for oocyte activation. Mol Hum Reprod. 2015;21:702–710. doi: 10.1093/molehr/gav034. [DOI] [PubMed] [Google Scholar]
- 88.Satouh Y, Nozawa K, Ikawa M. Sperm postacrosomal WW domain-binding protein is not required for mouse egg activation. Biol Reprod. 2015;93. [DOI] [PubMed]
- 89.Saunders CM, Larman MG, Parrington J, Cox LJ, Royse J, Blayney LM, et al. PLC zeta: a sperm-specific trigger of Ca(2+) oscillations in eggs and embryo development. Development. 2002;129:3533–44. [DOI] [PubMed]
- 90.Cox LJ, Larman MG, Saunders CM, Hashimoto K, Swann K, Lai FA. Sperm phospholipase C zeta from humans and cynomolgus monkeys triggers Ca2+ oscillations, activation and development of mouse oocytes. Reproduction. 2002;124:611–623. doi: 10.1530/rep.0.1240611. [DOI] [PubMed] [Google Scholar]
- 91.Yoneda A, Kashima M, Yoshida S, Terada K, Nakagawa S, Sakamoto A, et al. Molecular cloning, testicular postnatal expression, and oocyte-activating potential of porcine phospholipase C zeta. Reproduction. 2006;132:393–401. [DOI] [PubMed]
- 92.Yoon SY, Jellerette T, Salicioni AM, Lee HC, Yoo MS, Coward K, et al. Human sperm devoid of PLC, zeta 1 fail to induce Ca2+ release and are unable to initiate the first step of embryo development. J Clin Invest. 2008;118:3671–81. [DOI] [PMC free article] [PubMed]
- 93.Young C, Grasa P, Coward K, Davis LC, Parrington J. Phospholipase C zeta undergoes dynamic changes in its pattern of localization in sperm during capacitation and the acrosome reaction. Fertil Steril. 2009;91:2230–2242. doi: 10.1016/j.fertnstert.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 94.Bedford-Guaus SJ, McPartlin LA, Xie J, Westmiller SL, Buffone MG, Roberson MS. Molecular cloning and characterization of phospholipase C zeta in equine sperm and testis reveals species-specific differences in expression of catalytically active protein. Biol Reprod. 2011;85:78–88. doi: 10.1095/biolreprod.110.089466. [DOI] [PubMed] [Google Scholar]
- 95.Suh PG, Park JI, Manzoli L, Cocco L, Peak JC, Katan M, et al. Multiple roles of phosphoinositide-specific phospholipase C isozymes. BMB Rep. 2008;41:415–34. [DOI] [PubMed]
- 96.Lee B, Yoon SY, Malcuit C, Parys JB, Fissore RA. Inositol 1 4,5-trisphosphate receptor 1 degradation in mouse eggs and impact on [Ca2+]i oscillations. J Cell Physiol. 2010;222:238–247. doi: 10.1002/jcp.21945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kouchi Z, Fukami K, Shikano T, Oda S, Nakamura Y, Takenawa T, et al. Recombinant phospholipase Czeta has high Ca2+ sensitivity and induces Ca2+ oscillations in mouse eggs. J Biol Chem. 2004;279:10408–12. [DOI] [PubMed]
- 98.Nomikos M, Blayney LM, Larman MG, Campbell K, Rossbach A, Saunders CM, et al. Role of phospholipase C-zeta domains in Ca2+-dependent phosphatidylinositol 4,5-bisphosphate hydrolysis and cytoplasmic Ca2+ oscillations. J Biol Chem. 2005;280:31011–8. [DOI] [PubMed]
- 99.Kouchi Z, Shikano T, Nakamura Y, Shirakawa H, Fukami K, Miyazaki S. The role of EF-hand domains and C2 domain in regulation of enzymatic activity of phospholipase Czeta. J Biol Chem. 2005;280(22):21015–21021. doi: 10.1074/jbc.M412123200. [DOI] [PubMed] [Google Scholar]
- 100.Nomikos M, Kashir J, Swann K, Lai FA. Sperm PLCζ: from structure to Ca2+ oscillations, egg activation and therapeutic potential. FEBS Lett. 2013;587:3609–3616. doi: 10.1016/j.febslet.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 101.Nomikos M, Mulgrew-Nesbitt A, Pallavi P, Mihalyne G, Zaitseva I, Swann K, et al. Binding of phosphoinositide-specific phospholipase C-zeta (PLC-zeta) to phospholipid membranes: potential role of an unstructured cluster of basic residues. J Biol Chem. 2007;282:16644–53. [DOI] [PubMed]
- 102.Nomikos M, Elgmati K, Theodoridou M, Calver BL, Nounesis G, Swann K, et al. Phospholipase Czeta binding to PtdIns(4,5)P2 requires the XY-linker region. J Cell Sci. 2011;124:2582–259. [DOI] [PMC free article] [PubMed]
- 103.Nomikos M, Elgmati K, Theodoridou M, Georgilis A, Gonzalez-Garcia JR, Nounesis G, et al. Novel regulation of PLCzeta activity via its XY-linker. Biochem J. 2011;438:427–32. [DOI] [PMC free article] [PubMed]
- 104.Larman MG, Saunders CM, Carroll J, Lai FA, Swann K. Cell cycle-dependent Ca2+ oscillations in mouse embryos are regulated by nuclear targeting of PLCzeta. J Cell Sci. 2004;117:2513–2521. doi: 10.1242/jcs.01109. [DOI] [PubMed] [Google Scholar]
- 105.Ito M, Shikano T, Oda S, Horiguchi T, Tanimoto S, Awaji T, et al. Difference in Ca2+ oscillation-inducing activity and nuclear translocation ability of PLCZ1, an egg-activating sperm factor candidate, between mouse, rat, human, and medaka fish. Biol Reprod. 2008;78:1081–90. [DOI] [PubMed]
- 106.Swann K, Lai FA. Egg activation at fertilization by a soluble sperm protein. Physiol Rev. 2016;96(1):127–49. [DOI] [PubMed]
- 107.Fujimoto S, Yoshida N, Fukui T, Amanai M, Isobe T, Itagaki C, et al. Mammalian phospholipase Czeta induces oocyte activation from the sperm perinuclear matrix. Dev Biol. 2004;274:370–83. [DOI] [PubMed]
- 108.Kurokawa M, Sato K, Wu H, He C, Malcuit C, Black SJ, et al. Functional, biochemical, and chromatographic characterization of the complete [Ca2+]i oscillation-inducing activity of porcine sperm. Dev Biol. 2005;285:376–92. [DOI] [PubMed]
- 109.Knott JG, Kurokawa M, Fissore RA, Schultz RM, Williams CJ. Transgenic RNA interference reveals role for mouse sperm phospholipase Czeta in triggering Ca2+ oscillations during fertilization. Biol Reprod. 2005;72:992–996. doi: 10.1095/biolreprod.104.036244. [DOI] [PubMed] [Google Scholar]
- 110.Bedford-Guaus SJ, Yoon SY, Fissore RA, Choi YH, Hinrichs K. Microinjection of mouse phospholipase C zeta complementary RNA into mare oocytes induces long-lasting intracellular calcium oscillations and embryonic development. Reprod Fertil Dev. 2008;20:875–883. doi: 10.1071/rd08115. [DOI] [PubMed] [Google Scholar]
- 111.Coward K, Ponting CP, Zhang N, Young C, Huang CJ, Chou CM, et al. Identification and functional analysis of an ovarian form of the egg activation factor phospholipase C zeta (PLCζ) in pufferfish. Mol Reprod Dev. 2011;78:48–56. [DOI] [PubMed]
- 112.Hachem A, Godwin J, Ruas M, Lee HC, Ferrer Buitrago M, Ardestani G, et al. PLCζ is the physiological trigger of the Ca2+ oscillations that induce embryogenesis in mammals but conception can occur in its absence. Development. 2017;14:2914–24. [DOI] [PMC free article] [PubMed]
- 113.Nozawa K, Satouh Y, Fujimoto T, Oji A, Ikawa M. Sperm-borne phospholipase C zeta-1 ensures monospermic fertilization in mice. Sci Rep. 2018;8(1):1315. doi: 10.1038/s41598-018-19497-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Satouh Y, Ikawa M. New insights into the molecular events of mammalian fertilization. Trends Biochem Sci. 2018;43(10):818–828. doi: 10.1016/j.tibs.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Jones KT. Mammalian sperm contain two factors for calcium release and egg activation: phospholipase C zeta and a cryptic activating factor. Mol Hum Reprod. 2018;24(10):465–468. doi: 10.1093/molehr/gay038. [DOI] [PubMed] [Google Scholar]
- 116.Harada Y, Matsumoto T, Hirahara S, Nakashima A, Ueno S, Oda S, et al. Characterization of a sperm factor for egg activation at fertilization of the newt Cynops pyrrhogaster. Dev Biol. 2007;306(2):797–808. [DOI] [PubMed]
- 117.Miyara F, Aubriot FX, Glissant A, Nathan C, Douard S, Stanovici A, et al. Multiparameter analysis of human oocytes at metaphase II stage after IVF failure in non-male infertility. Hum Reprod. 2003;18:1494–503. [DOI] [PubMed]
- 118.Kilani S, Chapman MG. Meiotic spindle normality predicts live birth in patients with recurrent in vitro fertilization failure. Fertil Steril. 2014;101:403–406. doi: 10.1016/j.fertnstert.2013.10.045. [DOI] [PubMed] [Google Scholar]
- 119.Gasca S, Reyftmann L, Pellestor F, Re’me T, Assou S, Anahory T, et al. Total fertilization failure and molecular abnormalities in metaphase II oocytes. Reprod BioMed Online. 2008;17:772–81. [DOI] [PubMed]
- 120.Grøndahl ML, Borup R, Vikesa J, Ernst E, Andersen CY, Lykke-Hartmann K. The dormant and the fully competent oocyte: comparing the transcriptome of human oocytes from primordial follicles and in metaphase II. Mol Hum Reprod. 2013;19:600–617. doi: 10.1093/molehr/gat027. [DOI] [PubMed] [Google Scholar]
- 121.Li Y, Li RQ, Ou SB, Zhang NF, Ren L, Wei LN, et al. Increased GDF9 and BMP15 mRNA levels in cumulus granulosa cells correlate with oocyte maturation, fertilization, and embryo quality in humans. Reprod Biol Endocrinol. 2014;12:81. [DOI] [PMC free article] [PubMed]
- 122.Yeste M, Jones C, Amdani SN, Patel S, Coward K. Oocyte activation deficiency: a role for an oocyte contribution? Hum Reprod Update. 2016;22(1):23–47. doi: 10.1093/humupd/dmv040. [DOI] [PubMed] [Google Scholar]
- 123.Yeste M, Jones C, Amdani SN, Coward K. Oocyte activation and fertilisation: crucial contributors from the sperm and oocyte. Results Probl Cell Differ. 2017;59:213–239. doi: 10.1007/978-3-319-44820-6_8. [DOI] [PubMed] [Google Scholar]
- 124.Levasseur M, Carroll M, Jones KT, McDougall A. A novel mechanism controls the Ca2+ oscillations triggered by activation of ascidian eggs and has an absolute requirement for Cdk1 activity. J Cell Sci. 2007;120:1763–71. [DOI] [PubMed]
- 125.Cheng Y, Zhong Z, Latham KE. Strain-specific spontaneous activation during mouse oocyte maturation. Fertil Steril. 2012;98(1):200–206. doi: 10.1016/j.fertnstert.2012.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Puppo A, Chun JT, Gragnaniello G, Garante E, Santella L. Alteration of the cortical actin cytoskeleton deregulates Ca2+ signaling, monospermic fertilization, and sperm entry. PLoS One. 2008;3(10). [DOI] [PMC free article] [PubMed]
- 127.Santella L, Limatola N, Chun JT. Calcium and actin in the saga of awakening oocytes. Biochem Biophys Res Commun. 2015;460(1):104–113. doi: 10.1016/j.bbrc.2015.03.028. [DOI] [PubMed] [Google Scholar]
- 128.Limatola N, Vasilev F, Chun JT, Santella L. Altered actin cytoskeleton in ageing eggs of starfish affects fertilization process. Exp Cell Res. 2019;381(2):179–190. doi: 10.1016/j.yexcr.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 129.Limatola N, Vasilev F, Chun JT, Santella L. Sodium-mediated fast electrical depolarization does not prevent polyspermic fertilization in Paracentrotus lividus eggs. Zygote. 2019;27(4):241–249. doi: 10.1017/S0967199419000364. [DOI] [PubMed] [Google Scholar]
- 130.Saleh A, Kashir J, Thanassoulas A, Safieh-Garabedian B, Lai FA, Nomikos M. Essential role of sperm-specific PLC-zeta in egg activation and male factor infertility: an update. Front Cell Dev Biol. 2020;8:28. doi: 10.3389/fcell.2020.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Halet G, Tunwell R, Balla T, Swann K, Carroll J. The dynamics of plasma membrane PtdIns(4,5)P2 at fertilization of mouse eggs. J Cell Sci. 2002;115:2139–2149. doi: 10.1242/jcs.115.10.2139. [DOI] [PubMed] [Google Scholar]
- 132.Yu Y, Nomikos M, Theodoridou M, Nounesis G, Lai FA, Swann K. PLCζ causes Ca2+ oscillations in mouse eggs by targeting intracellular and not plasma membrane PI(45)P(2) Mol Biol Cell. 2012;23:371–380. doi: 10.1091/mbc.E11-08-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Swann K, Lai FA. PLCζ and the initiation of Ca(2+) oscillations in fertilizing mammalian eggs. Cell Calcium. 2013;53:55–62. doi: 10.1016/j.ceca.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 134.Yoda A, Oda S, Shikano T, Kouchi Z, Awaji T, Shirakawa H, et al. Ca2+ oscillation-inducing phospholipase C zeta expressed in mouse eggs is accumulated to the pronucleus during egg activation. Dev Biol. 2004;268:245–57. [DOI] [PubMed]
- 135.Perry ACF, Wakayama T, Yanagimachi R. A novel transcomplementation assay suggests full mammalian oocyte activation is coordinately initiated by multiple, submembrane sperm compartments. Biol Reprod. 1999;60:747–755. doi: 10.1095/biolreprod60.3.747. [DOI] [PubMed] [Google Scholar]
- 136.Manandhar G, Toshimori K. Fate of postacrosomal perinuclear theca recognized by monoclonal antibody MN13 after sperm head microinjection and its role in oocyte activation in mice. Biol Reprod. 2003;68:655–663. doi: 10.1095/biolreprod.102.006098. [DOI] [PubMed] [Google Scholar]
- 137.Sutovsky P, Manandhar G, Wu A, Oko R. Interactions of sperm perinuclear theca with the oocyte: implications for oocyte activation, anti-polyspermy defense, and assisted reproduction. Microsc Res Tech. 2003;61:362–378. doi: 10.1002/jemt.10350. [DOI] [PubMed] [Google Scholar]
- 138.Nakai M, Ito J, Sato K, Noguchi J, Kaneko H, Kashiwazaki N, et al. Pre-treatment of sperm reduces success of ICSI in the pig. Reproduction. 2011;142:285–93. [DOI] [PubMed]
- 139.Kaewmala K, Uddin MJ, Cinar MU, Große-Brinkhaus C, Jonas E, Tesfaye D, et al. Investigation into association and expression of PLCz and COX-2 as candidate genes for boar sperm quality and fertility. Reprod Domest Anim. 2012;47:213–23. [DOI] [PubMed]
- 140.Grasa P, Coward K, Young C, Parrington J. The pattern of localization of the putative oocyte activation factor, phospholipase Czeta, in uncapacitated, capacitated, and ionophore-treated human spermatozoa. Hum Reprod. 2008;23:2513–2522. doi: 10.1093/humrep/den280. [DOI] [PubMed] [Google Scholar]
- 141.Heytens E, Parrington J, Coward K, Young C, Lambrecht S, Yoon SY, et al. Reduced amounts and abnormal forms of phospholipase C zeta (PLCzeta) in spermatozoa from infertile men. Hum Reprod. 2009;24:2417–28. [DOI] [PubMed]
- 142.Kashir J, Jones C, Lee HC, Rietdorf K, Nikiforaki D, Durrans C, et al. Loss of activity mutations in phospholipase C zeta (PLCζ) abolishes calcium oscillatory ability of human recombinant protein in mouse oocytes. Hum Reprod. 2011a;26:3372–87. [DOI] [PMC free article] [PubMed]
- 143.Kashir J, Heynen A, Jones C, Durrans C, Craig J, Gadea J, et al. Effects of cryopreservation and density-gradient washing on phospholipase C zeta concentrations in human spermatozoa. Reprod BioMed Online. 2011b;23:263–7. [DOI] [PubMed]
- 144.Kashir J, Jones C, Mounce G, Ramadan WM, Lemmon B, Heindryckx B, et al. Variance in total levels of phospholipase C zeta (PLC-zeta) in human sperm may limit the applicability of quantitative immunofluorescent analysis as a diagnostic indicator of oocyte activation capability. Fertil Steril. 2013;99:107–17. [DOI] [PubMed]
- 145.Ramalho-Santos J. A sperm's tail: the importance of getting it right. Hum Reprod. 2011;26(9):2590–2591. doi: 10.1093/humrep/der200. [DOI] [PubMed] [Google Scholar]
- 146.Bi Y, Xu WM, Wong HY, Zhu H, Zhou ZM, Chan HC, et al. NYD-SP27, a novel intrinsic decapacitation factor in sperm. Asian J Androl. 2009;11(2):229–39. [DOI] [PMC free article] [PubMed]
- 147.Mejía-Flores I, Chiquete-Félix N, Palma-Lara I, Uribe-Carvajal S, de Lourdes Juárez-Mosqueda M. During capacitation in bull spermatozoa, actin and PLC-ζ undergo dynamic interactions. Zygote. 2017;25(5):558–566. doi: 10.1017/S0967199417000260. [DOI] [PubMed] [Google Scholar]
- 148.Escoffier J, Yassine S, Lee HC, Martinez G, Delaroche J, Coutton C, et al. Subcellular localization of phospholipase Cζ in human sperm and its absence in DPY19L2-deficient sperm are consistent with its role in oocyte activation. Mol Hum Reprod. 2015;21:157–68. [DOI] [PMC free article] [PubMed]
- 149.Mizushima S, Takagi S, Ono T, Atsumi Y, Tsukada A, Saito N, et al. Phospholipase Cζ mRNA expression and its potency during spermatogenesis for activation of quail oocyte as a sperm factor. Mol Reprod Dev. 2009;76:1200–7. [DOI] [PubMed]
- 150.Aarabi M, Yu Y, Xu W, Tse MY, Pang SC, Yi YJ, et al. The testicular and epididymal expression profile of PLCζ in mouse and human does not support its role as a sperm-borne oocyte activating factor. PLoS One. 2012;7:e33496. [DOI] [PMC free article] [PubMed]
- 151.Kashir J, Konstantinidis M, Jones C, Lemmon B, Lee HC, Hamer R, et al. A maternally inherited autosomal point mutation in human phospholipase C zeta (PLCζ) leads to male infertility. Hum Reprod. 2012a;27:222–31. [DOI] [PMC free article] [PubMed]
- 152.Kashir J, Konstantinidis M, Jones C, Heindryckx B, De Sutter P, Parrington J, et al. Characterization of two heterozygous mutations of the oocyte activation factor phospholipase C zeta (PLCζ) from an infertile man by use of minisequencing of individual sperm and expression in somatic cells. Fertil Steril. 2012b;98:423–31. [DOI] [PubMed]
- 153.Ferrer-Vaquer A, Barragan M, Freour T, Vernaeve V, Vassena R. PLCζ sequence, protein levels, and distribution in human sperm do not correlate with semen characteristics and fertilization rates after ICSI. J Assist Reprod Genet. 2016;33(6):747–756. doi: 10.1007/s10815-016-0718-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Escoffier J, Lee HC, Yassine S, Zouari R, Martinez G, Karaouzène T, et al. Homozygous mutation of PLCZ1 leads to defective human oocyte activation and infertility that is not rescued by the WW-binding protein PAWP. Hum Mol Genet. 2016;25:878–91. [DOI] [PMC free article] [PubMed]
- 155.Javadian-Elyaderani S, Ghaedi K, Tavalaee M, Rabiee F, Deemeh MR, Nasr-Esfahani MH. Diagnosis of genetic defects through parallel assessment of PLCζ and CAPZA3 in infertile men with history of failed oocyte activation. Iran J Basic Med Sci. 2016;19:281–289. [PMC free article] [PubMed] [Google Scholar]
- 156.Nomikos M, Stamatiadis P, Sanders JR, Beck K, Calver BL, Buntwal L, et al. Male infertility-linked point mutation reveals a vital binding role for the C2 domain of sperm PLCzeta. Biochem J. 2017;474:1003–16. [DOI] [PubMed]
- 157.Dai J, Dai C, Guo J, Zheng W, Zhang T, Li Y, et al. Novel homozygous variations in PLCZ1 lead to poor or failed fertilization characterized by abnormal localization patterns of PLCζ in sperm. Clin Genet. 2019. 10.1111/cge.13636. [DOI] [PubMed]
- 158.Torra-Massana M, Cornet-Bartolomé D, Barragán M, Durban M, Ferrer-Vaquer A, Zambelli F, et al. Novel phospholipase C zeta 1 mutations associated with fertilization failures after ICSI. Hum Reprod. 2019;34(8):1494–504. [DOI] [PubMed]
- 159.Janghorban-Laricheh E, Ghazavi-Khorasgani N, Tavalaee M, Zohrabi D, Abbasi H, Nasr-Esfahani MH. An association between sperm PLCζ levels and varicocele? J Assist Reprod Genet. 2016;33:1649–1655. doi: 10.1007/s10815-016-0802-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Mu J, Zhang Z, Wu L, Fu J, Chen B, Yan Z, et al. The identification of novel mutations in PLCZ1 responsible for human fertilization failure and a therapeutic intervention by artificial oocyte activation. Mol Hum Reprod. 2020. 10.1093/molehr/gaaa003. [DOI] [PubMed]
- 161.Yan Z, Fan Y, Wang F, Yan Z, Li M, Ouyang J, et al. Novel mutations in PLCZ1 cause male infertility due to fertilization failure or poor fertilization. Hum Reprod. 2020. 10.1093/humrep/dez282. [DOI] [PubMed]
- 162.Azad N, Nazarian H, Ghaffari Novin M, Masteri Farahani R, Piryaei A, Heidari MH. Phospholipase C zeta parameters in sperm from polymorphic teratozoospermic men. Ann Anat. 2018;215:63–70. doi: 10.1016/j.aanat.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 163.Azad N, Nazarian H, Ghaffari Novin M, Masteri Farahani R, Piryaei A, Heidari MH, et al. Oligoasthenoteratozoospermic (OAT) men display altered phospholipase C ζ (PLCζ) localization and a lower percentage of sperm cells expressing PLCζ and post-acrosomal sheath WW domain-binding protein (PAWP). Bosn J Basic Med Sci. 2018b;18:178–84. [DOI] [PMC free article] [PubMed]
- 164.Tavalaee M, Nomikos M, Lai FA, Nasr-Esfahani MH. Expression of sperm PLCζ and clinical outcomes of ICSI-AOA in men affected by globozoospermia due to DPY19L2 deletion. Reprod BioMed Online. 2018;36:348–355. doi: 10.1016/j.rbmo.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 165.Park JH, Kim SK, Kim J, Kim JH, Chang JH, Jee BC, et al. Relationship between phospholipase C zeta immunoreactivity and DNA fragmentation and oxidation in human sperm. Obstet Gynecol Sci. 2015;58:232–8. [DOI] [PMC free article] [PubMed]
- 166.Tavalaee M, Kiani-Esfahani A, Nasr-Esfahani MH. Relationship between potential sperm factors involved in oocyte activation and sperm DNA fragmentation with intra-cytoplasmic sperm injection clinical outcomes. Cell J. 2017;18:588–596. doi: 10.22074/cellj.2016.4725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Tavalaee M, Kiani-Esfahani A, Nasr-Esfahani MH. Relationship between phospholipase C-zeta, semen parameters, and chromatin status. Syst Biol Reprod Med. 2017;63:259–268. doi: 10.1080/19396368.2017.1298006. [DOI] [PubMed] [Google Scholar]
- 168.Yuan P, Yang C, Ren Y, Yan J, Nie Y, Yan L, et al. A novel homozygous mutation of phospholipase C zeta leading to defective human oocyte activation and fertilization failure. Hum Reprod. 2020. 10.1093/humrep/dez293. [DOI] [PubMed]
- 169.Nikiforaki D, Vanden Meerschaut F, De Gheselle S, Qian C, Van den Abbeel E, De Vos WH, et al. Sperm involved in recurrent partial hydatidiform moles cannot induce the normal pattern of calcium oscillations. Fertil Steril. 2014;102(2):581–588.e1. [DOI] [PubMed]
- 170.Nickkho-Amiry M, Horne G, Akhtar M, Mathur R, Brison DR. Hydatidiform molar pregnancy following assisted reproduction. J Assist Reprod Genet. 2019;36(4):667–671. doi: 10.1007/s10815-018-1389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Barratt CL, Aitken RJ, Björndahl L, Carrell DT, de Boer P, Kvist U, et al. Sperm DNA: organization, protection and vulnerability: from basic science to clinical applications--a position report. Hum Reprod. 2010;25:824–38. [DOI] [PubMed]
- 172.Nicopoullos J, Vicens-Morton A, Lewis SEM, Lee K, Larsen P, Ramsay J, et al. Novel use of COMET parameters of sperm DNA damage may increase its utility to diagnose male infertility and predict live births following both IVF and ICSI. Hum Reprod. 2019;34(10):1915–23. [DOI] [PubMed]
- 173.Virro MR, Larson-Cook KL, Evenson DP. Sperm chromatin structure assay (SCSA) parameters are related to fertilization, blastocyst development, and ongoing pregnancy in in vitro fertilization and intracytoplasmic sperm injection cycles. Fertil Steril. 2004;81:1289–1295. doi: 10.1016/j.fertnstert.2003.09.063. [DOI] [PubMed] [Google Scholar]
- 174.Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, et al. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012;27:2908–2917. doi: 10.1093/humrep/des261. [DOI] [PubMed] [Google Scholar]
- 175.Osman A, Alsomait H, Seshadri S, El-Toukhy T, Khalaf Y. The effect of sperm DNA fragmentation on live birth rate after IVF or ICSI: a systematic review and meta-analysis. Reprod BioMed Online. 2015;30:120–127. doi: 10.1016/j.rbmo.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 176.Rahimizadeh P, Topraggaleh TR, Nasr-Esfahani MH, Ziarati N, Mirshahvaladi S, Esmaeili V, et al. The alteration of PLCζ protein expression in unexplained infertile and asthenoteratozoospermic patients: a potential effect on sperm fertilization ability. Mol Reprod Dev. 2019. 10.1002/mrd.23293. [DOI] [PubMed]
- 177.WHO laboratory manual for the examination and processing of human semen (2010) (World Health Organization, Geneva). Available at: https://www.who.int/reproductivehealth/publications/infertility/9789241547789/en/ [Accessed January 2, 2020].
- 178.Verza S, Jr, Esteves SC. Sperm defect severity rather than sperm source is associated with lower fertilization rates after intracytoplasmic sperm injection. Int Braz J Urol. 2008;34:49–56. doi: 10.1590/s1677-55382008000100008. [DOI] [PubMed] [Google Scholar]
- 179.Nordhoff V, Fricke RK, Schüring AN, Zitzmann M, Kliesch S. Treatment strategies for severe oligoasthenoteratozoospermia (OAT) (<0.1 million/mL) patients. Andrology. 2015;3(5):856–863. doi: 10.1111/andr.12077. [DOI] [PubMed] [Google Scholar]
- 180.De Vos A, Van De Velde H, Joris H, Verheyen G, Devroey P, Van Steirteghem A. Influence of individual sperm morphology on fertilization, embryo morphology, and pregnancy outcome of intracytoplasmic sperm injection. Fertil Steril. 2003;79:42–48. doi: 10.1016/s0015-0282(02)04571-5. [DOI] [PubMed] [Google Scholar]
- 181.Coban O, Serdarogullari M, Onar Sekerci Z, Bilgin EM, Serakinci N. Evaluation of the impact of sperm morphology on embryo aneuploidy rates in a donor oocyte program. Syst Biol Reprod Med. 2018;64(3):169–173. doi: 10.1080/19396368.2018.1428384. [DOI] [PubMed] [Google Scholar]
- 182.Dam AH, Feenstra I, Westphal JR, Ramos L, van Golde RJ, Kremer JA. Globozoospermia revisited. Hum Reprod Update. 2007;13(1):63–75. doi: 10.1093/humupd/dml047. [DOI] [PubMed] [Google Scholar]
- 183.Taylor SL, Yoon SY, Morshedi MS, Lacey DR, Jellerette T, Fissore RA, et al. Complete globozoospermia associated with PLCζ deficiency treated with calcium ionophore and ICSI results in pregnancy. Reprod BioMed Online. 2010;20:559–64. [DOI] [PMC free article] [PubMed]
- 184.Tejara A, Mollá M, Muriel L, Remohi J, Pellicer A, De Pablo JL. Successful pregnancy and childbirth after intracytoplasmic sperm injection with calcium ionophore oocyte activation in a globozoospermic patient. Fertil Steril. 2008;90:1202.e1–1202.e5. doi: 10.1016/j.fertnstert.2007.11.056. [DOI] [PubMed] [Google Scholar]
- 185.Aghajanpour S, Ghaedi K, Salamian A, Deemeh MR, Tavalaee M, Moshtaghian J, et al. Quantitative expression of phospholipase C zeta, as an index to assess fertilization potential of a semen sample. Hum Reprod. 2011;26:2950–6. [DOI] [PubMed]
- 186.Kashir J, Sermondade N, Sifer C, Oo SL, Jones C, Mounce G, et al. Motile sperm organelle morphology evaluation-selected globozoospermic human sperm with an acrosomal bud exhibits novel patterns and higher levels of phospholipase C zeta. Hum Reprod. 2012;27:3150–60. [DOI] [PubMed]
- 187.Kamali-Dolat Abadi M, Tavalaee M, Shahverdi A, Nasr-Esfahani MH. Evaluation of PLCζ and PAWP expression in globozoospermic individuals. Cell J. 2016;18:438–445. doi: 10.22074/cellj.2016.4572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Sermondade N, Hafhouf E, Dupont C, Bechoua S, Palacios C, Eustache F, et al. Successful childbirth after intracytoplasmic morphologically selected sperm injection without assisted oocyte activation in a patient with globozoospermia. Hum Reprod. 2011;26(11):2944–9. [DOI] [PubMed]
- 189.Esteves SC. Clinical management of infertile men with nonobstructive azoospermia. Asian J Androl. 2015;17(3):459–470. doi: 10.4103/1008-682X.148719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Tanaka A, Nagayoshi M, Takemoto Y, Tanaka I, Kusunoki H, Watanabe S, et al. Fourteen babies born after round spermatid injection into human oocytes. Proc Natl Acad Sci U S A. 2015;112(47):14629–34. [DOI] [PMC free article] [PubMed]
- 191.Ogura A, Matsuda J, Yanagimachi R. Birth of normal young after electrofusion of mouse oocytes with round spermatids. Proc Natl Acad Sci U S A. 1994;91(16):7460–7462. doi: 10.1073/pnas.91.16.7460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kimura Y, Yanagimachi R. Mouse oocytes injected with testicular spermatozoa or round spermatids can develop into normal offspring. Development. 1995;121(8):2397–2405. doi: 10.1242/dev.121.8.2397. [DOI] [PubMed] [Google Scholar]
- 193.Yanagimachi R, Wakayama T, Kishikawa H, Fimia GM, Monaco L, Sassone-Corsi P. Production of fertile offspring from genetically infertile male mice. Proc Natl Acad Sci U S A. 2004;101(6):1691–1695. doi: 10.1073/pnas.0307832100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Tesarik J, Mendoza C. Spermatid injection into human oocytes. I. Laboratory techniques and special features of zygote development. Hum Reprod. 1996;11(4):772–779. doi: 10.1093/oxfordjournals.humrep.a019253. [DOI] [PubMed] [Google Scholar]
- 195.Tesarik J, Rolet F, Brami C, Sedbon E, Thorel J, Tibi C, et al. Spermatid injection into human oocytes. II. Clinical application in the treatment of infertility due to non-obstructive azoospermia. Hum Reprod. 1996;11(4):780–3. [DOI] [PubMed]
- 196.Vanderzwalmen P, Zech H, Birkenfeld A, Yemini M, Bertin G, Lejeune B, et al. Intracytoplasmic injection of spermatids retrieved from testicular tissue: influence of testicular pathology, type of selected spermatids and oocyte activation. Hum Reprod. 1997;12(6):1203–13. [DOI] [PubMed]
- 197.Barak Y, Kogosowski A, Goldman S, Soffer Y, Gonen Y, Tesarik J. Pregnancy and birth after transfer of embryos that developed from single-nucleated zygotes obtained by injection of round spermatids into oocytes. Fertil Steril. 1998;70(1):67–70. doi: 10.1016/s0015-0282(98)00106-x. [DOI] [PubMed] [Google Scholar]
- 198.Gianaroli L, Selman HA, Magli MC, Colpi G, Fortini D, Ferraretti AP. Birth of a healthy infant after conception with round spermatids isolated from cryopreserved testicular tissue. Fertil Steril. 1999;72(3):539–541. doi: 10.1016/s0015-0282(99)00285-x. [DOI] [PubMed] [Google Scholar]
- 199.Van den Veyver IB, Al-Hussaini TK. Biparental hydatidiform moles: a maternal effect mutation affecting imprinting in the offspring. Hum Reprod Update. 2006;12:233–242. doi: 10.1093/humupd/dmk005. [DOI] [PubMed] [Google Scholar]
- 200.Silber SJ, Johnson L. Are spermatid injections of any clinical value? ROSNI and ROSI revisited. Round spermatid nucleus injection and round spermatid injection. Hum Reprod. 1998;13(3):509–515. doi: 10.1093/humrep/13.3.509. [DOI] [PubMed] [Google Scholar]
- 201.Silber SJ, Johnson L, Verheyen G, Van Steirteghem A. Round spermatid injection. Fertil Steril. 2000;73(5):897–900. doi: 10.1016/s0015-0282(00)00488-x. [DOI] [PubMed] [Google Scholar]
- 202.Tanaka A, Suzuki K, Nagayoshi M, Tanaka A, Takemoto Y, Watanabe S, et al. Ninety babies born after round spermatid injection into oocytes: survey of their development from fertilization to 2 years of age. Fertil Steril. 2018;110(3):443–51. [DOI] [PubMed]
- 203.Yazawa H, Yanagida K, Sato A. Human round spermatids from azoospermic men exhibit oocyte-activation and Ca2+ oscillation-inducing activities. Zygote. 2007;15(4):337–346. doi: 10.1017/S0967199407004339. [DOI] [PubMed] [Google Scholar]
- 204.Ogonuki N, Inoue K, Ogura A. Birth of normal mice following round spermatid injection without artificial oocyte activation. J Reprod Dev. 2011;57(4):534–538. doi: 10.1262/jrd.11-008m. [DOI] [PubMed] [Google Scholar]
- 205.Yazawa H, Yanagida K, Sato A. Oocyte activation and Ca(2+) oscillation-inducing abilities of mouse round/elongated spermatids and the developmental capacities of embryos from spermatid injection. Hum Reprod. 2001;16(6):1221–1228. doi: 10.1093/humrep/16.6.1221. [DOI] [PubMed] [Google Scholar]
- 206.Loren J, Lacham-Kaplan O. The employment of strontium to activate mouse oocytes: effects on spermatid-injection outcome. Reproduction. 2006;131(2):259–267. doi: 10.1530/rep.1.00894. [DOI] [PubMed] [Google Scholar]
- 207.Hirabayashi M, Kato M, Hochi S. Factors affecting full-term development of rat oocytes microinjected with fresh or cryopreserved round spermatids. Exp Anim. 2008;57(4):401–405. doi: 10.1538/expanim.57.401. [DOI] [PubMed] [Google Scholar]
- 208.Hirabayashi M, Kato M, Kitada K, Ohnami N, Hirao M, Hochi S. Activation regimens for full-term development of rabbit oocytes injected with round spermatids. Mol Reprod Dev. 2009;76(6):573–579. doi: 10.1002/mrd.20984. [DOI] [PubMed] [Google Scholar]
- 209.Yazawa H, Yanagida K, Katayose H, Hayashi S, Sato A. Comparison of oocyte activation and Ca2+ oscillation-inducing abilities of round/elongated spermatids of mouse, hamster, rat, rabbit and human assessed by mouse oocyte activation assay. Hum Reprod. 2000;15(12):2582–2590. doi: 10.1093/humrep/15.12.2582. [DOI] [PubMed] [Google Scholar]
- 210.Yelumalai S, Yeste M, Jones C, Amdani SN, Kashir J, Mounce G, et al. Total levels, localization patterns, and proportions of sperm exhibiting phospholipase C zeta are significantly correlated with fertilization rates after intracytoplasmic sperm injection. Fertil Steril. 2015;104:561–8.e4. [DOI] [PubMed]
- 211.Ozil JP, Banrezes B, Tóth S, Pan H, Schultz RM. Ca2+ oscillatory pattern in fertilized mouse eggs affects gene expression and development to term. Dev Biol. 2006;300(2):534–544. doi: 10.1016/j.ydbio.2006.08.041. [DOI] [PubMed] [Google Scholar]
- 212.Whitaker M. Calcium signalling in early embryos. Philos Trans R Soc Lond Ser B Biol Sci. 2008;363(1495):1401–1418. doi: 10.1098/rstb.2008.2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Hudmon A, Schulman H. Structure-function of the multifunctional Ca2+/calmodulin-dependent protein kinase II. Biochem J. 2002;364(Pt 3):593–611. doi: 10.1042/BJ20020228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Bos-Mikich A, Whittingham DG, Jones KT. Meiotic and mitotic Ca2+ oscillations affect cell composition in resulting blastocysts. Dev Biol. 1997;182(1):172–179. doi: 10.1006/dbio.1996.8468. [DOI] [PubMed] [Google Scholar]
- 215.Rogers NT, Hobson E, Pickering S, Lai FA, Braude P, Swann K. Phospholipase Czeta causes Ca2+ oscillations and parthenogenetic activation of human oocytes. Reproduction. 2004;128:697–702. doi: 10.1530/rep.1.00484. [DOI] [PubMed] [Google Scholar]
- 216.Rogers NT, Halet G, Piao Y, Carroll J, Ko MS, Swann K. The absence of a Ca(2+) signal during mouse egg activation can affect parthenogenetic preimplantation development, gene expression patterns, and blastocyst quality. Reproduction. 2006;132(1):45–57. doi: 10.1530/rep.1.01059. [DOI] [PubMed] [Google Scholar]
- 217.Yamaguchi T, Ito M, Kuroda K, Takeda S, Tanaka A. The establishment of appropriate methods for egg-activation by human PLCZ1 RNA injection into human oocyte. Cell Calcium. 2017;65:22–30. doi: 10.1016/j.ceca.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 218.Yeste M, Jones C, Amdani SN, Yelumalai S, Mounce G, da Silva SJ, et al. Does advancing male age influence the expression levels and localisation patterns of phospholipase C zeta (PLCζ) in human sperm? Sci Rep. 2016;6:27543. [DOI] [PMC free article] [PubMed]
- 219.Kashir J, Buntwal L, Nomikos M, Calver BL, Stamatiadis P, Ashley P, et al. Antigen unmasking enhances visualization efficacy of the oocyte activation factor, phospholipase C zeta, in mammalian sperm. Mol Hum Reprod. 2017;23:54–67. [DOI] [PubMed]
- 220.Ebner T, Montag M, Oocyte Activation Study Group, Montag M, Van der Ven K, Van der Ven H, et al. Live birth after artificial oocyte activation using a ready-to-use ionophore: a prospective multicentre study. Reprod BioMed Online. 2015 Apr;30(4):359–65. [DOI] [PubMed]
- 221.Heindryckx B, De Gheselle S, Gerris J, Dhont M, De Sutter P. Efficiency of assisted oocyte activation as a solution for failed intracytoplasmic sperm injection. Reprod BioMed Online. 2008;17:662–668. doi: 10.1016/s1472-6483(10)60313-6. [DOI] [PubMed] [Google Scholar]
- 222.Ma SF, Liu XY, Miao DQ, Han ZB, Zhang X, Miao YL, et al. Parthenogenetic activation of mouse oocytes by strontium chloride: a search for the best conditions. Theriogenology. 2005;64:1142–57. [DOI] [PubMed]
- 223.Neri QV, Lee B, Rosenwaks Z, Machaca K, Palermo GD. Understanding fertilization through intracytoplasmic sperm injection (ICSI) Cell Calcium. 2014;55:24–37. doi: 10.1016/j.ceca.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Sanusi R, Yu Y, Nomikos M, Lai FA, Swann K. Rescue of failed oocyte activation after ICSI in a mouse model of male factor infertility by recombinant phospholipase Cζ. Mol Hum Reprod. 2015;21:783–791. doi: 10.1093/molehr/gav042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Yoon SY, Eum JH, Lee JE, Lee HC, Kim YS, Han JE, et al. Recombinant human phospholipase C zeta 1 induces intracellular calcium oscillations and oocyte activation in mouse and human oocytes. Hum Reprod. 2012;27(6):1768–80. [DOI] [PubMed]
- 226.Nomikos M, Yu Y, Elgmati K, Theodoridou M, Campbell K, Vassilakopoulou V, et al. Phospholipase Cζ rescues failed oocyte activation in a prototype of male factor infertility. Fertil Steril. 2013b;99:76–85. [DOI] [PMC free article] [PubMed]
- 227.Miao YL, Stein P, Jefferson WN, Padilla-Banks E, Williams CJ. Calcium influx-mediated signaling is required for complete mouse egg activation. Proc Natl Acad Sci U S A. 2012;109(11):4169–4174. doi: 10.1073/pnas.1112333109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Bernhardt ML, Stein P, Carvacho I, Krapp C, Ardestani G, Mehregan A, et al. TRPM7 and CaV3.2 channels mediate Ca2+ influx required for egg activation at fertilization. Proc Natl Acad Sci U S A. 2018;115(44):E10370–8. [DOI] [PMC free article] [PubMed]
- 229.Ozil JP, Sainte-Beuve T, Banrezes B. [Mg2+]o/[Ca2+]o determines Ca2+ response at fertilization: tuning of adult phenotype? Reproduction. 2017;154(5):675–693. doi: 10.1530/REP-16-0057. [DOI] [PubMed] [Google Scholar]
- 230.Herrick JR, Strauss KJ, Schneiderman A, Rawlins M, Stevens J, Schoolcraft WB, et al. The beneficial effects of reduced magnesium during the oocyte-to-embryo transition are conserved in mice, domestic cats and humans. Reprod Fertil Dev. 2015;27(2):323–31. [DOI] [PubMed]