Abstract
Objectives
Pandemic COVID-19 has become a seriously public health priority worldwide. Comprehensive strategies including travel restrictions and mask-wearing have been implemented to mitigate the virus circulation. However, detail information on community transmission is unavailable yet.
Methods
From January 23 to March 1, 2020, 127 patients (median age: 46 years; range: 11–80) with 71 male and 56 female, were confirmed to be infected with the SARS-CoV-2 in Taizhou, Zhejiang, China. Epidemiological trajectory and clinical features of these COVID-19 cases were retrospectively retrieved from electronic medical records and valid individual questionnaire.
Results
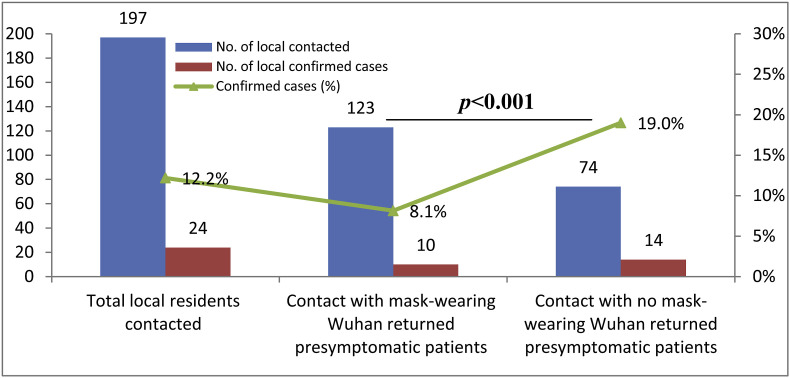
The disease onset was between January 9 to February 14, 2020. Among them, 64 patients are local residents, and 63 patients were back home from Wuhan from January 10 to 24, 2020 before travel restriction. 197 local residents had definite close-contact with 41 pre-symptomatic patients back from Wuhan. 123 and 74 of them contact with mask-wearing or with no mask-wearing pre-symptomatic patients back from Wuhan, respectively. Data showed that incidence of COVID-19 was significantly higher for local residents close-contact with no mask-wearing Wuhan returned pre-symptomatic patients (19.0% vs. 8.1%, p < 0.001). Among 57 close-contact individuals, 21 sequential local COVID-19 patients originated from a pre-symptomatic Wuhan returned couple, indicated dense gathering in congested spaces is a high risk for SARS-CoV-2 transmission.
Conclusions
Our findings provided valuable details of pre-symptomatic patient mask-wearing and restriction of mass gathering in congested spaces particularly, are important interventions to mitigate the SARS-CoV-2 transmission.
Keywords: SARS-CoV-2, COVID-19, Transmission, Community, Mask-wearing, Mass gathering
1. Introduction
As of 4th April, pandemic COVID-19, caused by the coronavirus SARS-CoV-2, has claimed 45 526 lives with an ever-increasing accumulated 896 450 confirmed cases around the world since its outbreak in Wuhan, China during December 2019 [1]. The highly person-to-person contagious SARS-CoV-2 has been reported in various visible and invisible fomite such as droplet, aerosol, feces and even in conjunctival secretions [[2], [3], [4]]. Comprehensive and unprecedented measurements have been implemented to interrupt and mitigate the SARS-CoV-2 transmission by more and more governments as the World Health Organization (WHO) announced a public health emergency of COVID-19 on January 30, 2020.
In addition to virus transmissibility and host susceptibility, environmental settings and personal hygienic behavior are important to spread of the infectious diseases [5]. Under the circumstance of a very limited social distancing and congestive space in Diamond Princess Cruises, nearly 17% (621/3711) of the passengers and crew onboard infected with SARS-CoV-2. The estimated reproductive value for the virus was 11.0, which was rather higher than that of the community-level round 2.2 [6,7]. In this context, lessons and experience learned from very lately occurred pandemic such as 2009 H1N1 and the 2013 MERS, that the implication of mass gathering restriction and social distance in COVID-19 prevention [8].
Indeed, currently implemented public regulations such as travel and mass gathering restrictions, home quarantine and patient isolation, combined with personal hygiene including mask-wearing and hand-washing were necessary and did have delayed and reduced the SARS-CoV-2 transmission [[9], [10], [11]]. In this scenario, WHO has recommended properly use of masks, particularly for confirmed or suspected COVID-19 patients, in the community, during home care and in health care facilities to interrupt the SARS-CoV-2 transmission [12]. However, as Chinazzi et al. reported, without a significant reduction of community spreading, the effects of containing the outbreak of COVID-19 would be limited [13].
Taizhou is a city in Zhejiang province with 6 million residents, near 900 km away from Wuhan, China. The status quo scenario is that many Taizhou residents living, running business or working in Wuhan, and most of them will come back home for family gathering when close to the Chinese traditional holiday, the Spring Festival. From January 10, 2020 to 24, 2020 before travel restriction implemented firstly in Wuhan, 63 individuals returned from Wuhan were confirmed to be infected with the SARS-CoV-2 in our medical center, the only designated medical facility for COVID-19 in Taizhou city. 41 of them were identified to have close-contact 197 local residents, leading 24 local residents infected with SARS-CoV-2.
In this study, we described the epidemiological trajectory and clinical features of these patients, and a cluster of 21 sequential local COVID-19 patients originated from a couple back from Wuhan among 57 close-contact individuals was detailed.
2. Methods
2.1. Patients and design
From January 23, 2020 to March 1, 2020, 127 patients were confirmed to be infected with the SARS-CoV-2 in Taizhou, Zhejiang, China. Among them, 64 patients are local residents, and 63 patients who were back home from Wuhan from January 10 to 24, 2020 before travel restriction. All patients were admitted and treated in the officially designated medical center for COVID-19 patients, Enze Hospital, Taizhou Hospital of Zhejiang Province, Taizhou Enze Medical Center (Groups). All patients were discharged by March 11, 2020.
Throat swab samples were collected and SARS-CoV-2 infection was confirmed by RT-PCR according to the guidelines recommended by the National Health Commission (NHC) of the People's Republic of China. Clinical classification of COVID-19 cases was based on the Diagnosis and Treatment Plan of Corona Virus Diseases 2019 (Tentative Sixth Edition), National Health Commission (NHC) of the People's Republic of China [14].
Demographic information and epidemiological trajectory for each patient (both back from Wuhan and local residents) was collected with an epidemics of COVID-19 questionnaire survey by interviews of the cases (suppl. Figure 1). The contents of the questionnaire mainly focused on the transmission route, wearing masks or not, close-contact or exposure history. Up to 10 close-contacted individuals’ detail information and relationship to surveyed COVID-19 cases (such as couple, family members, relatives, friends, villagers and others) are required to be provided. Clinical features, and medical history of the patients were retrospectively retrieved from electronic medical records. The validity of questionnaire survey was assured with the cross-checked demographic information and epidemiological trajectory from COVID-19 cases admitted in our medical center.
Fig. 1.
Distribution of Taizhou local residents close-contact with 41 Wuhan returned COVID-19 pre-symptomatic patients (a); distribution of Taizhou local residents close-contact with 28 mask-wearing Wuhan returned COVID-19 pre-symptomatic patients (b), distribution of Taizhou local residents close-contact with 13 no mask-wearing Wuhan returned COVID-19 pre-symptomatic patients (c).
A community-level cluster of 21 sequential local COVID-19 patients originated from a couple back from Wuhan among 57 close-contact individuals was based on the timeline of close-contact, exposure history and events within 14 days. Of 21 local COVID-19 patients in this cluster, 5 clinically diagnosed but without SARS-CoV-2 confirmed cases who were admitted and treated in other hospitals were validated by telephone interview.
The protocol of this study was reviewed and approved by the institutional ethics committee (#K20200111), and written consent was obtained from all patients or the guardians.
2.2. Statistical methods
General description or group comparison with variables was analyzed. Mann-Whitney U test for continuous variables, and χ2 test with Fisher's exact probability for categorical variables was performed. Statistical analysis was performed with SPSS v.13.0 (SPSS, Inc. Chicago, IL, USA). A two-sided p < 0.05 means statistical significance.
3. Results
3.1. Clinical baseline of the COVID-19 patients
The details of the clinical baseline of the COVID-19 patients were shown in Table 1 . From January 23, 2020 to March 1, 2020, 127 patients (109 ordinary and 18 severe cases) were confirmed to be infected with the SARS-CoV-2 in Taizhou, Zhejiang, China. Among them, 64 patients are local residents, and 63 patients who were back home from Wuhan from January 10 to 24, 2020 before travel restriction. There are 71 male and 56 female with the median age of 46.0 years (range: 11 years–80 years). Median of onset day is January 25, 2020. Data showed that median of the onset time is 6 days later (January 28 vs. January 22) for the local patients than that for patients returned from Wuhan. Our finding is in line with the median incubation period of COVID-19 patients that is round 4–7 days as reported in recent studies [[15], [16], [17]].
Table 1.
Clinical baseline of the COVID-19 patients in Taizhou City.
| Variables | Total | Wuhan returned | Taizhou local | p value |
|---|---|---|---|---|
| COVID-19 cases | 127 | 63 | 64 | 0.900 |
| Male/female | 71/56 | 30/33 | 41/23 | 0.062 |
| Age | 46.0 (11–80) | 46.0 (11–75) | 46.0 (12–80) | 0.659 |
| Body mass index | 24.4 (18.9–31.3) | 24.1 (18.9–31.3) | 24.5 (19.2–30.7) | 0.349 |
| Severe (yes/no) | 18/109 | 7/56 | 11/53 | 0.326 |
| Return day | / | Jan 10~Jan 24 | / | / |
| Onset day | Jan 9~ Feb 14 | Jan 9~ Feb 4 | Jan 12~ Feb 14 | / |
| Median Onset day | Jan 25 | Jan 22 | Jan 28 | / |
| Signs on admission | ||||
| fever (yes/no) | 91/36 | 47/16 | 44/20 | 0.464 |
| body temperature | 36.9 (36.0–39.0) | 37.0 (36.0–38.6) | 36.9 (36.0–39.0) | 0.137 |
| sputum production | 40 | 22 | 18 | 0.085 |
| poor appetite | 38 | 17 | 21 | 0.473 |
| Cough | 37 | 18 | 19 | 0.890 |
| Fatigue | 34 | 7 | 27 | <0.001 |
| Chills | 22 | 12 | 10 | 0.610 |
| Headache | 18 | 13 | 5 | 0.038 |
| sore throat | 17 | 12 | 5 | 0.063 |
| chest suppression | 14 | 4 | 10 | 0.095 |
| Diarrhea | 13 | 5 | 8 | 0.396 |
| nasal congestion/runny | 11 | 8 | 3 | 0.109 |
| nausea or vomiting | 5 | 0 | 5 | / |
| Myalgia | 5 | 5 | 0 | / |
| Hemoptysis | 1 | 0 | 1 | / |
| shortness of breath | 1 | 1 | 0 | / |
| Pre-existing disorders | / | |||
| yes/no | 75/52 | 36/27 | 39/25 | 0.664 |
| Hypertentsion | 18 | 9 | 9 | 0.971 |
| Diabetes | 17 | 8 | 9 | 0.821 |
| chronic liver disease | 9 | 3 | 6 | 0.311 |
| chronic lung disease | 8 | 4 | 4 | 0.982 |
| chronic renal disease | 2 | 0 | 2 | / |
| Cancers | 3 | 3 | 0 | / |
| chronic heart disease | 1 | 0 | 1 | / |
| HBV histroy | 7 | 2 | 5 | 0.252 |
| HCV histroy | 1 | 0 | 1 | / |
| others disorders | 41 | 18 | 23 | 0.375 |
No significant difference for demographic and epidemiological features was found between the COVID-19 patients returned from Wuhan and local cases. Onset signs such as fever, mild sputum production, cough, poor appetite, fatigue and chills, and pre-existing disorders such as hypertension and diabetes are frequently observed. Among onset symptoms, fatigue are significantly common in Taizhou local patients (p < 0.001), while headache are much higher in patients returned from Wuhan (p = 0.038).
3.2. Distribution of local residents close-contact with Wuhan returned patients
During January 10, 2020 to January 24, 2020 before the travel restriction, 63 individuals returned from Wuhan were consecutively diagnosed as laboratory confirmed COVID-19 patients. Of these 63 Wuhan returned COVID-19 patients, 41 of them provided a valid demographic information and epidemiological trajectory, and close-contact with definite local residents to the questionnaire survey. Before diagnosed, these 41 COVID-19 pre-symptomatic patients (13 without wearing masks and 28 is wearing masks), had closely contacted with 197 local residents including couple, family members, relatives, friends, villagers, or card playing partners, leading 24 of them infected with SARS-CoV-2 (Fig. 1 a).
Few Taizhou local residents were aware of the serious situation of COVID-19 outbreak in Wuhan until the travel restriction was announced on January 23, 2020, and Taizhou city followed on January 24, 2020. Before then, few Taizhou local people were masking. During the period of close-contacting, 28 out of 41 Wuhan returned COVID-19 pre-symptomatic patients wearing masks and closely contacted with 123 local residents (Fig. 1b), leading to 10 local residents infected with SARS-CoV-2. Meanwhile, 13 of them are not wearing masks and closely contacted with 74 local residents, leading to 14 local residents infected with SARS-CoV-2 (Fig. 1c). When compared, the percentage of local residents infected with SARS-CoV-2 was dramatically lower in the group who closely contacted with Wuhan returned mask-wearing COVID-19 pre-symptomatic patients than that of those contacted with the pre-symptomatic patients without mask-wearing (8.1% vs. 19.0%; p < 0.001; Fig. 2 ). Our finding indicated that, as WHO recommended, symptomatic and suspected individuals should wear mask to prevent the human-to-human transmission of SARS-CoV-2 [12].
Fig. 2.
Comparison of the incidence of local COVID-19 patients after close-contact between mask-wearing and without mask-wearing Wuhan returned COVID-19 pre-symptomatic patients (p < 0.001).
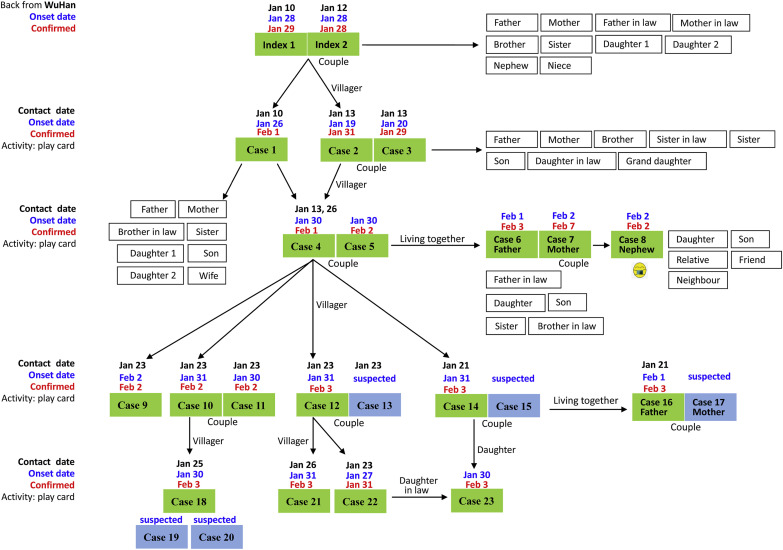
3.3. Epidemiological trajectory of a community-level cluster of 21 sequential local COVID-19 patients
Details of epidemiological trajectory and events of the cluster of 21 sequential local COVID-19 patients originated from a couple back from Wuhan was presented in Fig. 3 . A couple returned from Wuhan on January 10, and 12, 2020, respectively. The person-to-person transmission of SARS-CoV-2 is majorly during the activity of playing cards in a space limited Chess and Card Room.
Fig. 3.
Timeline of epidemiological trajectory of a cluster of 21 sequential local COVID-19 patients originated from a Wuhan returned pre-symptomatic couple in a community.
On January 10 and 13, Cases index 1 and 2 were playing cards with case #1 and case #2, respectively. On January 13, case #1 and case #2 were playing cards with case #4. On January 23, case #4 was playing cards with cases #9, #10, #11 and #12; and on January 21, case #4 was also playing cards with case #14. Then, on January 25, case #10 was playing cards with case #18, and case #12 was playing cards with case #21 and #22 on January 26 and 23, respectively. Moreover, 8 spouse or family members living together were also subsequently diagnosed as COVID-19, and 5 more were suspected with clinically diagnosed. Be noted, 36 close-contacted family members but not living together in 5 families were not infected. During the period, only case #8 was wearing masks.
4. Discussion
Tragedy of the pandemic of COVID-19 is of massive destruction in all aspects of life. An ever-increasing cases confirmed and deaths claimed by the disease is deeply concerning around the world. Great efforts and measurements have been made to fight against the COVID-19; however, no clear evidence has so far shown that the situation have been changed for better. Without effective medical treatment currently and vaccine is still on the road, and high human-to-human transmission potential of the SARS-CoV-2 from symptomatic, pre-symptomatic and even asymptomatic patients, raising the physical quarantine and personal behavior change is vital to mitigate the COVID-19 crisis [[18], [19], [20]].
Taizhou is nearly 900 km away from Wuhan where the COVID-19 firstly emerged. From January 23, 2020 to March 1, 2020, 127 patients were confirmed to be infected with the SARS-CoV-2 in Taizhou, Zhejiang, China. Half of them came back from Wuhan during January 10, 2020 to January 24, 2020, just before the travel restriction was announced in Taizhou city. As out data revealed, among 197 local individuals closely contacted with the Wuhan returned patients, 12.2% (24/197) of them with SARS-CoV-2 infected, indicating that the travel restriction could have dramatically decreased local COVID-19 incidence by reducing the scale of returned personnel. Our observation is agreement with recent reports that the spread of COVID-19 dramatically decreased by the drastic control measures for human mobility, and isolation of suspected or diagnosed cases is necessary to interrupt secondary transmission of the disease [10,21].
Our data also showed that, the incidence of COVID-19 was doubled (19.0% vs. 8.1%) for local residents who had closely contacted with Wuhan returned, without mask-wearing pre-symptomatic COVID-19 patients. Usage of face masks in the general community public is under debating due to not only absence of protective evidence as WHO addressed, but different culture paradigms [12,22]. However, a rather high proportion of COVID-19 patients is pre-symptomatic or asymptomatic, virus shedding and spreading COVID-19 have been reported in various circumstances [18,23]. In our opinion, universal use of masks in general public and community should be recommended if supply permits.
It has been well acknowledged that dense gathering, particularly in a limited space or social distancing, is a high risk factor for respiratory infectious disease transmission [8]. In addition to mass gathering such as the Olympics, passengers, familial members are susceptible to SARS-CoV-2 infection [6,24,25]. In this study, a cluster of 21 local COVID-19 patients originated from a Wuhan returned couple by playing cards sequentially in a space limited Chess and Card Room or living together for a long-time exposure from pre-symptomatic or asymptomatic relatives. Our observation underscores limited social distancing and staying in congested spaces or living together with pre-symptomatic or suspected COVID-19 patients will render a high risk for the transmission of the SARS-CoV-2.
A comprehensive bundling of stringent measurements have been implemented to fight against spreading of the COVID-19; however, a synergistic effect could be achieved by the reduction of community infection [13]. In this context, our findings provided valuable information on mask-wearing, restriction of mass gathering are important interventions to mitigate the SARS-CoV-2 transmission in community.
Authors’ contributions
Lu-Xiao Hong, Ze-Bao He, Hai-Hong Zhao, Chao Zhang, Ling-Jun Ying, Zheng-Ming Ge, Jian-Sheng Zhu and Hai-Xiao Chen had roles in patient recruitment, clinical management, data collection, and data interpretation. Jian-Sheng Zhu, Hai-Xiao Chen and Wei-Hua Yan had roles in the study design, data interpretation. Aifen Lin, Jian-Gang Zhang, Xia Zhang, Qiu-Yue Han, Qiong-Yuan Chen, and Yao-Han Ye had roles in data collection. Aifen Lin and Wei-Hua Yan had roles in data analysis, literature search, data interpretation, and writing of the manuscript.
CRediT authorship contribution statement
Lu-Xiao Hong: Data curation, Conceptualization, Methodology, Investigation, Validation, Formal analysis. Aifen Lin: Conceptualization, Data curation, Formal analysis, Writing - review & editing, Funding acquisition. Ze-Bao He: Conceptualization, Data curation, Methodology, Investigation, Validation. Hai-Hong Zhao: Data curation, Investigation, Resources. Jian-Gang Zhang: Data curation, Resources. Chao Zhang: Investigation, Resources. Ling-Jun Ying: Investigation, Resources. Zheng-Ming Ge: Investigation, Resources. Xia Zhang: Data curation, Resources. Qiu-Yue Han: Data curation, Resources. Qiong-Yuan Chen: Data curation, Resources. Yao-Han Ye: Data curation, Resources. Jian-Sheng Zhu: Conceptualization, Supervision, Investigation, Validation. Hai-Xiao Chen: Conceptualization, Project administration, Supervision. Wei-Hua Yan: Conceptualization, Methodology, Data curation, Formal analysis, Validation, Writing - original draft, Funding acquisition.
Declaration of competing interest
We declare no competing interests.
Acknowledgements
This work was supported by grants from Project of Taizhou Science and Technology Bureau, Zhejiang, China (1901ky01; 1901ky04).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2020.101803.
Appendix A. Supplementary data
The following are the supplementary data to this article:
Suppl. Fig. 1.
Schematic protocol of epidemiological survey questionnaire for COVID-19.
References
- 1.Coronavirus disease 2019 (COVID-19) situation report – 73. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200402-sitrep-73-covid-19.pdf?sfvrsn=5ae25bc7_2
- 2.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu P., Duan F., Luo C. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in hubei province, China. JAMA Ophthalmol. 2020;138(5):575–578. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen C., Gao G., Xu Y. SARS-CoV-2-Positive sputum and feces after conversion of pharyngeal samples in patients with COVID-19. Ann Intern Med. 2020;172(12):832–834. doi: 10.7326/M20-0991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frieden T.R., Lee C.T. Identifying and interrupting superspreading events-implications for control of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(6):1059–1066. doi: 10.3201/eid2606.200495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mizumoto K., Chowell G. Transmission potential of the novel coronavirus (COVID-19) onboard the diamond Princess Cruises Ship, 2020. Infect Dis Model. 2020;5:264–270. doi: 10.1016/j.idm.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebrahim S.H., Ahmed Q.A., Gozzer E., Schlagenhauf P., Memish Z.A. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020;368:m1066. doi: 10.1136/bmj.m1066. [DOI] [PubMed] [Google Scholar]
- 8.Ebrahim S.H., Memish Z.A. COVID-19 - the role of mass gatherings. Trav Med Infect Dis. 2020;34:101617. doi: 10.1016/j.tmaid.2020.101617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung C.C., Lam T.H., Cheng K.K. Mass masking in the COVID-19 epidemic: people need guidance. Lancet. 2020;395(10228):945. doi: 10.1016/S0140-6736(20)30520-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraemer M.U.G., Yang C.H., Gutierrez B. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin C., Braund W.E., Auerbach J. Policy decisions and use of information Technology to fight 2019 novel coronavirus disease, taiwan. Emerg Infect Dis. 2020;26(7):1506–1512. doi: 10.3201/eid2607.200574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak: interim guidance. 29 January 2020. https://www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak
- 13.Chinazzi M., Davis J.T., Ajelli M. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Health Commission (NHC) of the PRC . People’s Meidcal Publishing House; Beijing, China: 2020. National Administration of Traditional Chinese Medicine of the PRC. Guidance for corona virus disease 2019. Prevention, control, diagnosis and management. [Google Scholar]
- 15.Guan W.J., Ni Z.Y., Hu Y. China medical treatment expert group for covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jia J., Hu X., Yang F. Epidemiological characteristics on the clustering nature of COVID-19 in Qingdao City, 2020: a descriptive analysis. Disaster Med Public Health Prep. 2020:1–5. doi: 10.1017/dmp.2020.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian S., Hu N., Lou J. Characteristics of COVID-19 infection in beijing. J Infect. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li C., Ji F., Wang L. Asymptomatic and human-to-human transmission of SARS-CoV-2 in a 2-family cluster, Xuzhou, China. Emerg Infect Dis. 2020;26(7):1626–1628. doi: 10.3201/eid2607.200718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kimball A., Hatfield K.M., Arons M. Public health – seattle & king county; CDC COVID-19 investigation team. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility - king county, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wölfel R., Corman V.M., Guggemos W. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 21.Giovanetti M., Benvenuto D., Angeletti S., Ciccozzi M. The first two cases of 2019-nCoV in Italy: where they come from? J Med Virol. 2020;92(5):518–521. doi: 10.1002/jmv.25699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8(5):434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020;369:m1375. doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J., Tian S., Lou J., Chen Y. Familial cluster of COVID-19 infection from an asymptomatic. Crit Care. 2020;24(1):119. doi: 10.1186/s13054-020-2817-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qian G., Yang N., Ma A.H.Y. A COVID-19 Transmission within a family cluster by presymptomatic infectors in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]