Abstract
With the COVID-19 pandemic, the fear among patients of contracting it has made them reluctant to seek medical attention on a timely basis even for emergent conditions. We present a case of post infarction ventricular septal rupture due to delayed presentation as a consequence of the fear of COVID-19. (Level of Difficulty: Intermediate.)
Key Words: chest pain, complication, left-sided catheterization, myocardial infarction, right-sided catheterization, ventricular septal defect
Abbreviations and Acronyms: CAD, coronary artery disease; LAD, left anterior descending; MI, myocardial infarction; PCI, percutaneous coronary intervention; RCA, right coronary artery; RV, right ventricle; VSR, ventricular septal rupture
Graphical abstract

With the COVID-19 pandemic, the fear among patients of contracting it has made them reluctant to seek medical attention on a timely basis even for…
A 72-year-old woman presented with substernal chest heaviness radiating to her back and bilateral upper extremities with associated lightheadedness. At the onset of symptoms, the chest discomfort was severe but she did not come to the hospital for the fear of contracting COVID-19. After 14 h of persistent symptoms, she finally presented to an outside hospital that did not have primary percutaneous coronary intervention (PCI) capability. Vitals were notable for normal temperature, hypotensive with blood pressure of 70/50 mm Hg, pulse of 50 beats/min, and O2 saturations of 95% on room air. Jugular venous distension was not appreciated. Cardiac auscultation revealed no obvious murmur and the initial pulmonary examination revealed scattered crackles. Lower extremities were cool to touch without any pitting edema.
Learning Objectives
-
•
Mechanical complications such as VSR, papillary muscle rupture, or free ventricular wall rupture should be high on the differential in patients who present late with acute MI and are hemodynamically unstable.
-
•
The COVID-19 pandemic and fear among patients of contracting the infection within the hospital is playing a detrimental role in delayed presentation of acute MI, and leading to resurgence of post MI mechanical complications.
-
•
Classic presentation and catheterization findings of post MI VSR include late MI presentation, cardiogenic shock, evidence of contrast filling of the RV on left ventriculogram, prominent “v” waves, and step-up in O2 saturation at the level of RV resulting in increased Qp:Qs ratio.
The patient developed a bradycardic cardiac arrest necessitating brief cardiopulmonary resuscitation with return of spontaneous circulation. During the cardiac arrest, she was intubated for airway protection and was started on multiple vasopressors/inotropes for persistent hypotension. Ultimately, the patient was transferred to our facility for further consideration of emergent cardiac catheterization.
Past Medical History
The patient had hypertension, dyslipidemia, and coronary artery disease (CAD) with prior PCI with stents to the right coronary artery (RCA) in 2002.
Differential Diagnosis
The differential diagnosis includes inferior myocardial infarction (MI) with right ventricle (RV) failure, inferior MI with ventricular septal rupture (VSR), inferior MI with posteromedial papillary muscle rupture with resultant mitral regurgitation, and aortic dissection with involvement of RCA.
Investigations
Initial electrocardiogram at the outside hospital revealed ST-segment elevation in the inferior leads with associated Q waves and reciprocal ST-segment depressions in high lateral leads (Figure 1). The computed tomography angiogram showed no evidence of aortic dissection or pulmonary embolism. Initial troponin I was elevated (>25 ng/ml). On arterial blood gas, pH was noted to be 6.9 with a PCO2 of 52.5 mm Hg and a bicarbonate of 10 mmol/l.
Figure 1.
Presenting Electrocardiogram
Presenting electrocardiogram ST-segment elevation in the inferior leads (II, III, aVF) with associated Q waves and reciprocal ST-segment depression in high lateral leads (I and aVL).
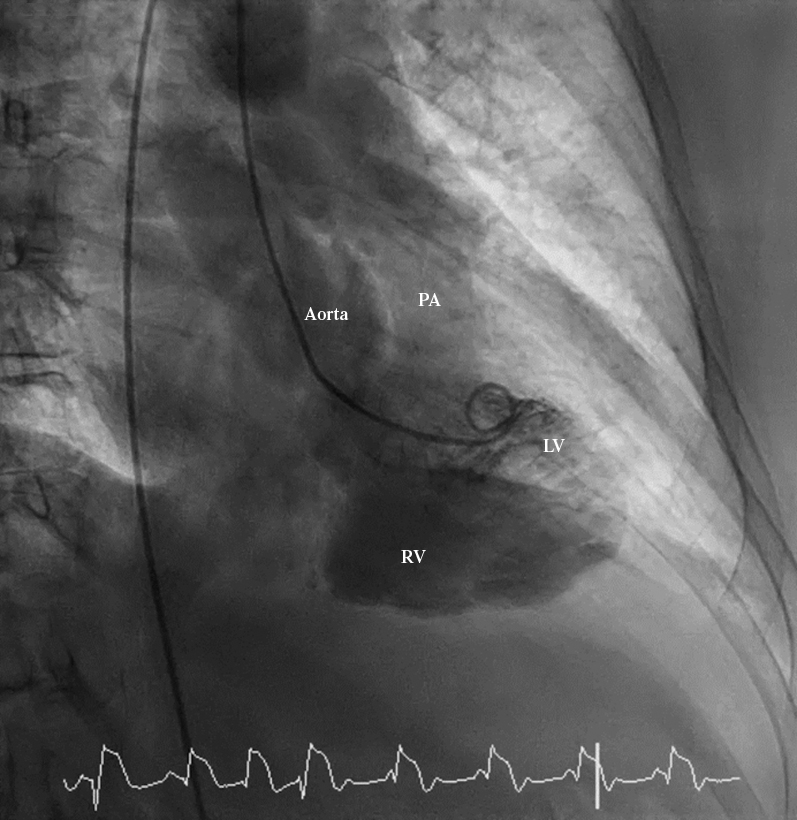
Coronary angiography demonstrated acute thrombotic occlusion of the mid RCA stent (Figure 2) and no obstructive CAD in the left main, left anterior descending (LAD), and left circumflex arteries. The left ventriculogram in right anterior oblique and left anterior oblique projection demonstrated contrast filling of the RV and main pulmonary artery consistent with a VSR and no evidence of mitral regurgitation (Figures 3 and 4, Videos 1 and 2).
Figure 2.

RCA Angiogram
Right coronary artery (RCA) angiogram in left anterior oblique projection demonstrating acute occlusion of the stent in the mid RCA (as indicated by the arrow).
Figure 3.
RAO Left Ventriculogram
Left ventriculogram in anterior oblique (RAO) projection demonstrating contrast filling of right ventricle (RV) and pulmonary artery (PA) from the left ventricle (LV).
Figure 4.

LAO Left Ventriculogram
Left ventriculogram in left anterior oblique (LAO) projection demonstrating contrast filling of the right ventricle (RV) and pulmonary artery (PA) from the left ventricle (LV).
Online Video 1.
Right anterior oblique left ventriculogram.
Online Video 2.
Left anterior oblique left ventriculogram.
Right heart catheterization demonstrated a mean pulmonary capillary wedge pressure of 28 mm Hg associated with significant “v” waves (Figure 5), pulmonary artery pressure of 54/26 mm Hg, and mean right atrial pressure of 23 mm Hg. O2 saturation shunt run revealed a step-up in the RV (O2 saturations: right atrium 55.6%, RV 85.4%, pulmonary artery 75.2%, and systemic arterial 91%). The calculated shunt fraction (Qp:Qs) was 2.2:1 with a cardiac index of 2.2 l/min/m2.
Figure 5.
PCWP Tracing
Elevated pulmonary capillary wedge pressure (PCWP) with prominent “v” waves.
Management
The patient received aspirin and intravenous unfractionated heparin bolus per acute coronary syndrome protocol before cardiac catheterization. The patient underwent percutaneous coronary intervention of the mid RCA with 1 drug-eluting stent. After discussion with cardiac surgery, emergent surgical intervention for the VSR was deemed to be futile. Given the grim prognosis and the patient’s documented wish of not continuing futile life-saving measures, she was made “comfort measures only,” and soon after she died.
Discussion
VSR following acute MI occurs due to ischemic necrosis of the interventricular septum after a transmural infarct. The LAD supplies the anterior portion of the interventricular septum while a dominant RCA usually supplies the inferior portion of the IVS (1). Thus, infarction in the LAD territory may result in an apical VSR, whereas an infarction involving the RCA can result in a basal inferoposterior VSR (1), similar to what was seen in our patient. Before the advent of early reperfusion therapies, VSR occurred at a rate of 1% to 2% after acute MI (2). With contemporary reperfusion therapy, the rate of VSR has decreased significantly to approximately 0.17% to 0.31% (2,3). Despite advancement in percutaneous and surgical techniques, survival in patients with VSR remains poor. Even with early surgical repair, 30-day survival is approximately 60%, with a 5-year survival of only 38% (4), whereas, conservative management resulted in a grim prognosis and a 30-day mortality of 100% (5). Because of this, it is important to minimize the risk of VSR with prompt symptom recognition and presentation for early revascularization.
With the current COVID-19 pandemic, there has been a reorganization of health care and community resources to combat the pandemic. The effects of previously successful awareness campaigns regarding the need for early assessment of acute chest pain have waned in the light of the new campaigns for social distancing and self-isolation (6). There is also hesitancy among the patients about coming to the hospital for the fear of being exposed to COVID-19. As a result of this, there has been a decrease in cardiac catheterization laboratory (cath lab) activations for ST-segment elevation MI by approximately 38% in the United States (7). Furthermore, the likelihood of delayed presentations, such as the one seen in our patient, has increased. Tam et al. (8) showed that the time from symptom onset to first medical contact has increased by approximately 300% during the current COVID-19 pandemic in Asia. In addition to this, extensive donning and doffing protocols in the cath lab have increased cath lab arrival–to–first device time (8). Rescheduling of the “nonemergent” coronary angiograms has resulted in delay in definitive diagnosis and treatment of patients with undefined coronary anatomies. With these factors, we are likely to see an increase in the post MI mechanical complications as well as chronic total occlusions in the coming months.
Although the extremely important campaigns for awareness for COVID-19 and social distancing are ongoing, it is equally important for health care professionals to highlight symptoms and situations for which the patients should urgently seek medical attention without delay. Such awareness should be created both at the individual patient level (through physician offices) as well as at the community level though public health forums and professional medical societies (9).
Conclusions
Our case illustrates the classic presentation and cardiac catheterization findings of post MI VSR associated with a late presentation inferior ST-segment elevation myocardial infarction. More importantly, it also highlights the detrimental role of the COVID-19 pandemic as the cause for delayed presentations, which could result in the resurgence of mechanical complications of acute MI.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Mubarik A., Iqbal A.M. StatPearls; Treasure Island, FL: 2020. Ventricular Septal Rupture. [PubMed] [Google Scholar]
- 2.Singh V., Rodriguez A.P., Bhatt P. Ventricular septal defect complicating ST-elevation myocardial infarctions: a call for action. Am J Med. 2017;130:863.e12. doi: 10.1016/j.amjmed.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Moreyra A.E., Huang M.S., Wilson A.C. Trends in incidence and mortality rates of ventricular septal rupture during acute myocardial infarction. Am J Cardiol. 2010;106:1095–1100. doi: 10.1016/j.amjcard.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Jeppsson A., Liden H., Johnsson P., Hartford M., Rådegran K. Surgical repair of post infarction ventricular septal defects: a national experience. Eur J Cardiothorac Surg. 2005;27:216–221. doi: 10.1016/j.ejcts.2004.10.037. [DOI] [PubMed] [Google Scholar]
- 5.Poulsen S.H., Praestholm M., Munk K., Wierup P., Egeblad H., Nielsen-Kudsk J.E. Ventricular septal rupture complicating acute myocardial infarction: clinical characteristics and contemporary outcome. Ann Thorac Surg. 2008;85:1591–1596. doi: 10.1016/j.athoracsur.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Gori T., Lelieveld J., Münzel T. Perspective: cardiovascular disease and the Covid-19 pandemic. Basic Res Cardiol. 2020;115:32. doi: 10.1007/s00395-020-0792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tam C.F., Cheung K.S., Lam S. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mahmud E., Dauerman H.L., Welt F.G. Management of acute myocardial infarction during the COVID-19 pandemic. J Am Coll Cardiol. 2020 Apr 21 doi: 10.1016/j.jacc.2020.04.039. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]




