Abstract
The assessment of the incubation period, which is the period between the infection and the illness onset, is essential to identify the sufficient isolation period for infectious diseases. In South Korea, a few cases of the coronavirus disease 2019 (COVID-19) were identified after the 14-day self-quarantine program, and the length of this quarantine has raised controversial issues for the Korean public health professionals.
We estimated the COVID-19 incubation period using the log-normal distribution from publicly available data. The data were obtained from the press release of the Busan city department of public health and news reports.
We collected and analysed information for 47 patients with a median age of 30. We estimated that the median incubation period was three days (95% Confidence Interval, 0.6–8.2). We also did not find any significant difference in the incubation period between males and females.
Our findings indicate that a 14-day self-quarantine program should be sufficient to prevent spreading in the infection of suspected individuals with COVID-19 in the community.
Keywords: Coronavirus, Outbreak, Korea, Incubation period, Log-normal distribution
As of the 10th of June 2020, South Korea has experienced the large outbreak of coronavirus disease 2019 (COVID-19) [1]. The first COVID-19 cases were identified on 20 January 2020 from individuals travelling from China to South Korea [2]. Then, superspreading COVID-19 event occurred among a Korean religious group at Daegu-Gyeongsangbuk provincial region mid February 2020 [3].
Busan city, located in the southeast part of the Korean peninsula and with a population of 3.24 million, identified the first COVID-19 case on 22 February 2020. As of 8 March 2020, 89 laboratory-confirmed cases were identified, and 521 individuals were self-quarantined in Busan city [4]. The incubation period, the time between the infection and symptoms onset, plays a key role to determine the period of quarantine for infectious diseases [5]. Recently, several individuals who were exposed to the laboratory-confirmed cases of COVID-19 but tested negative for COVID-19 at the initial assessment were later identified as positive after 14 days of self-quarantine. Therefore, the duration of self-quarantine has raised controversial issues for the public as well as Korean public health professionals [6,7].
The purpose of this study is to estimate an incubation period using the publicly available data and to provide evidence supporting the current 14-day self-quarantine recommendation.
The data was obtained from publicly available sources, such as the press release from Busan city department of public health and news reports [8]. We extracted the information of COVID-19 cases confirmed by real-time reverse transcriptase polymerase chain reactions. The epidemiological information of interest included the year of birth, sex, date of illness onset, exposure date of the infectious source (i.e., the date of the infectee was in contact with the infected patient), the origin of infection, and contact history with other laboratory-confirmed cases. We analysed the incubation period using information from patients with precise contact history with other case-patients.
The incubation period was estimated by fitting log-normal, Weibull, and gamma distributions, and using available data with date of exposure and date of illness onset. We identified the best-fitted model of probabilistic distribution through the Akaike information criterion (AIC). Furthermore, we conducted Wilcoxon signed-rank test to measure the significant difference of incubation periods between males and females. All statistical analyses were performed using R version 3.0.2 (R Foundation for Statistical Computing).
Overall, we obtained a line list of 79 laboratory-confirmed cases reported between 20 February and 3 March 2020. We analysed exposures data for 47 cases with precise information on exposure date and date of illness onset. The overall median age was 30 years (ranging from 17 to 83). The median age of male and female was 34 years (ranging from 6 to 82) and 41 years (ranging from 9 to 83).
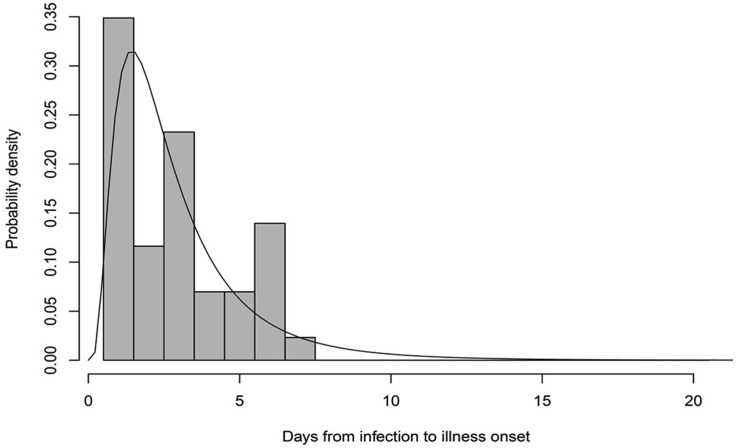
The incubation period estimation model was best fitted with the log-normal distribution which had the lowest AIC (190.9). The AIC for the Weibull and gamma distributions were 192 and 191. The overall estimated median incubation period was 3.0 days (95% Confidence Interval (CI), 0.6–8.2) (Fig. 1 ). We found that the median incubation period for males (2.5 days; 95% CI, 0.5–6.9 days) was shorter than for females (3.3 days; 95% CI, 0.7–8.5 days); however, the difference was not statistically significant (W = 321, p-value = 0.3).
Fig. 1.
Incubation period distribution of COVID-19 for the laboratory-confirmed cases with COVID-19 in Busan, South Korea. The estimated median incubation period was 3.0 (95% Confidence Interval, 0.6–8.2).
The estimation of incubation periods in the early phase of any infectious disease outbreak allows researchers to construct transmission model that can be used to predict future spread in the community and elaborate effective control measure [9]. In this study, the log-normal distribution was the best fitted to our model. This is consistent with a previous review stating that the incubation period of acute respiratory viral infections follows a log-normal distribution [10].
Our estimated median incubation period is shorter than the previous literature (Table 1 ) [[11], [12], [13], [14]]. This indicates that the Korean 14-day self-quarantine program is likely sufficient to prevent spread in the community from individuals with COVID-19. We did not measure any significant difference between the males and the females in our study population for the incubation period. Identifying the impact of the age on the incubation period would be valuable to provide age-specific intervention measures in the community and to conduct epidemiological modelling studies. However, we did not analyse the impact of age on the incubation period because of the small sample size among the different age groups.
Table 1.
The comparison of incubation periods with previous studies.
| Number of cases and place of infection | Median age (range, years) | Fitted distribution | Median incubation period (days) | Range or 95% CI of the incubation period (days) | |
|---|---|---|---|---|---|
| Our study | 47 from Busan, Korea | 30 (17–83) | Log-normal distribution | 3.0 | 95% CI: 0.6–8.2 |
| Ki M et al. [11] | Seven including imported cases in Korea | N/A | N/A | 4.0 | Range: 1-9 |
| Li Q et al. [12]. | 10 from Wuhan, China | 42 (21–62) | Gamma distribution | 5.2 | 95% CI: 4.1–7.0 |
| Linton NM et al. [13]. | 52 from China | N/A (30–59) | Log-normal distribution | 5.6 | 95% CI: 4.4–7.4 |
| Backer JA et al. [14] | 88 travellers from Wuhan, China | N/A (2–72) | Weibull distribution | 6.4 | Range: 2.1–11.1 |
N/A: Not available.
CI: confidence interval.
The probability distribution analysis of the incubation period indicates that the possibility for an infected individual to develop symptoms after 14 days of quarantine is 0.1 percentile, i.e., 1 case in 1000. This information is valuable because it helps the public to better understand the nature of the current public health measures and the epidemiological characteristics of COVID-19. This knowledge can, therefore enhance their compliance with these measures in the community. Previous studies have already described the epidemiological parameters of COVID-19 [2]; however, these parameters can vary in different countries, because of their environment, their medical systems as well as the public behaviour facing health issues [15]. Therefore, the study of epidemiologic parameters should be actively conducted with a specific population and in a specific location to provide the scientific evidence necessary for the establishment of public health measures by the public health authorities and the public.
Our study is the first that estimated the incubation period of COVID-19 in Busan, Korea; however, it presents some limitations. First, our results are based on publicly available data, which were collected from various sources. Second, the number of a sample size used to estimate the incubation period was small. This was due to the number of cases with incomplete information in the line list. Third, we did not consider the demographic characteristics of the patients, which may affect the incubation period.
The median incubation period of COVID-19 was 3.0 days (95% CI, 0.6–8.2), and there was no significant difference in the incubation period between males and females. The current 14-day self-quarantine program is a sufficient public health measure to prevent the transmission of COVID-19 in the community.
Author contributions
All authors meet the ICMJE authorship criteria. SR designed the study. HL, KK, HS, KC, and SH collected the data and conducted analysis. HL, KK, and SR wrote the original draft of manuscript. SR and HS reviewed and edited the manuscript. All authors commented on the manuscript and approved the final version.
Funding
This work was supported by Basic Science Research Program through the National Research Foundation of South Korea funded by the Ministry of Education (NRF-2020R1I1A3066471).
Declaration of Competing Interest
We declare no competing interests.
Acknowledgments
This research was conducted as a part of the project of Community Medicine and Practice at Konyang University College of Medicine, Daejeon, South Korea. The authors thank Minchae Kim, Minhyeok Kim, Hohyup Kim, Chamseul Moon, Yosup Won, Namjung Ryoo, and Hyeongseok Lee for help with data collection, analyses, and interpretation of study results.
References
- 1.Ryu S., Ali S.T., Jang C., Kim B., Cowling B.J. Effect of nonpharmaceutical interventions on transmission of severe acute respiratory syndrome coronavirus 2, South Korea, 2020. Emerg Infect Dis. 2020:26. doi: 10.3201/eid2610.201886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ryu S., Chun B.C., Korean Society of Epidemiology -nCo VTFT An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol Health. 2020;42 doi: 10.4178/epih.e2020006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim H.J., Hwang H.S., Choi Y.H., Song H.Y., Park J.S., Yun C.Y., et al. The delay in confirming covid-19 cases linked to a religious group in korea. J Prev Med Public Health. 2020;53:164–167. doi: 10.3961/jpmph.20.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wonjin Cho. There is no addional cases identified in busan. Seoul, Korea: Sedaily. https://www.sedaily.com/NewsVIew/1Z04B9QJ8R [accessed 29 June 2020].
- 5.Johan Giesecke. CRC Press; New York, NY: 2017. Modern infectious disease epidemiology. [Google Scholar]
- 6.Newsis. Controversy of 14-day incubation period. Seoul, Korea: Newsis. https://newsis.com/view/?id=NISX20200310_0000949953&cID=10201&pID=10200 [accessed 29 June 2020].
- 7.Park H. Is incubation period 14 days? Busan, Korea: Busan Ilbo. http://www.busan.com/view/busan/view.php?code=2020030819354449715 [accessed 29 June 2020].
- 8.Busan metropolitan city. The situation update in busan city. Busan; South Korea: 2020. [Google Scholar]
- 9.Ryu S., Ali S.T., Lim J.S., Chun B.C. Estimation of the excess covid-19 cases in seoul, South Korea by the students arriving from China. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17093113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lessler J., Reich N.G., Brookmeyer R., Perl T.M., Nelson K.E., Cummings D.A. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009;9:291–300. doi: 10.1016/S1473-3099(09)70069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ki M., Task Force for 2019-nCoV Epidemiologic characteristics of early cases with 2019 novel coronavirus (2019-ncov) disease in Republic of Korea. Epidemiol Health. 2020;42:e2020007. doi: 10.4178/epih.e2020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Linton N.M., Kobayashi T., Yang Y., Hayashi K., Akhmetzhanov A.R., Jung S.M., et al. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med. 2020;9 doi: 10.3390/jcm9020538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019-ncov) infections among travellers from wuhan, China, 20–28 january 2020. Euro Surveill. 2020;25:2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., et al. Centre for the mathematical modelling of infectious diseases C-WG, Funk S and Eggo RM. Feasibility of controlling covid-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8:e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]