Abstract
Previous literature has reported that patients with diabetes in pregnancy (DIP) are at risk of developing antepartum depression but the results have been inconsistent in cohort studies. We conducted a systematic review and performed a meta-analysis to quantify the association between DIP and risk of antepartum depression in cohort studies. Medline, Cinahl, and PubMed databases were searched for studies investigating DIP involving pregnant women with pre-existing diabetes and gestational diabetes mellitus and their risk of antepartum depression that were published in journals from inception to 27 December 2019. We derived the summary estimates using a random-effects model and reported the findings as pooled relative risks (RR) and confidence interval (CI). Publication bias was assessed using a funnel plot and was quantified by Egger and Begg’s tests. Ten studies, involving 71,036 pregnant women were included in this meta-analysis. The pooled RR to develop antepartum depression was (RR = 1.430, 95% CI: 1.251–1.636) among women with gestational diabetes mellitus. Combining pregnant women with pre-existing diabetes mellitus and gestational diabetes mellitus, they had a significant increased risk of developing antepartum depression (RR = 1.431, 95% CI: 1.205–1.699) compared with those without it. In comparison, we found no association between pre-existing diabetes mellitus in pregnancy (RR = 1.300, 95% CI: 0.736–2.297) and the risk of developing antepartum depression. This study has a few limitations: first, different questionnaire and cut-off points were used in evaluation of depression across the studies. Second, there was a lack of data on history of depression prior to pregnancy, which lead to confounding bias that could not be solved by this meta-analysis. Third, data were dominated by studies in Western countries; this is due to the studies from Eastern countries failing to meet our inclusion criteria for statistical analysis. Women with gestational diabetes mellitus have an increased risk of developing antepartum depression compared to those without the disease. Therefore, more attention on the mental health status should be given on pregnant women diagnosed with pre-existing diabetes mellitus and gestational diabetes mellitus.
Keywords: antepartum depression, gestational diabetes, pre-existing diabetes, diabetes in pregnancy
1. Background
Depression is a common illness worldwide [1,2] and women are about twice as likely than men to develop depression during their lifetime [3]. Without doubt, pregnancy is a major life event that is usually accompanied by hormonal changes and it is a time of extreme increased vulnerability for having antepartum depression [4,5]. Studies have reported that the prevalence of antepartum depression was higher in the second and third trimesters (12.0%–12.8%) as compared with the first trimester (7.4%) [6,7,8].
Based on the existing systematic review conducted among the Indian women, Arora and Aeri in 2019 summarized that the significant risk factors for antenatal depression are unplanned pregnancy, being a multigravida, having a history of abortion, advancing age, lower socio-economic status, lower educational status, unemployment, bad relationship with her in-laws, male gender preference, and excessive demand for dowry [9]. However, diabetes in pregnancy (DIP) was not included in that systematic review. In fact, there has been literature reporting data on the occurrence of antepartum depression among women with and without DIP [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. Furthermore, DIP could be associated with the onset of antepartum depression.
On the other hand, most of the existing literature focused on the association between DIP and postpartum depression, for example a meta-analysis by Arafa and Dong [29] that reported that GDM is a significant risk factor for postpartum depression (pooled relative risk (RR) = 1.32). Another meta-analysis by Azami et al. found a similar pooled RR of 1.59 based on observational studies [30]. Indeed, postpartum depression has a drawn out ramifications for women and their children [31]. Nevertheless, studies have reported that the prevalence of antepartum depression (that ranged from 6.5% to 12.9%) [32] and postpartum depression (that ranged from 6.6% to 8.5%) were actually comparable to each other [33]. In fact, antepartum depression was also associated with postpartum depression [34].
Women with GDM have an increased risk of developing type 2 diabetes (with a RR of 7.43) compared to pregnant women who are normo-glycemic [35]. As it is well known, pregnant mothers with pre-existing diabetes mellitus (DM) are at a high risk for adverse pregnancy outcomes such as unplanned caesarean section, abnormal fetal birth weight, and congenital anomalies in the offspring [36,37]. Therefore, DIP (pre-existing DM and GDM) is known to be associated with increased risk of maternal and neonatal morbidity and mortality [7,38]. In mothers facing the dual challenge of pregnancy and upcoming motherhood, the association of DIP and depression imposes important health concerns. Currently, the relationship between these conditions remains indistinct due to the reason that the existing systematic review on the association between depression and DIP included all observational studies, whereby the causal relationship between DIP and depression was difficult to determine from the study design itself. Furthermore, some of the studies had the diagnosis of depression confirmed in the study’s participants even before the diagnosis of diabetes was made [39]. Therefore, we conducted a systematic review with meta-analysis to determine the association between DIP and the risk of antepartum depression only among the available cohort studies.
2. Methods
The present study was registered with the National Medical Research Register, Ministry of Health Malaysia (registration number: NMRR-20-674-53879). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria when conducting this meta-analysis and reporting its results [40].
2.1. Literature Search
Two investigators (K.W.L. and S.C.C.) independently searched Medline, Cinahl, and PubMed databases for potential studies published in journals from inception to 27 December 2019. We considered any relevant studies in the search as long as it was published before or on 27 December 2019. We also did not impose a limitation on the years of publication on the studies identified from reverse–forward citation tracking. We used a combination of search terms: (mood disorder OR unipolar depress* OR depress* OR depress* disorder OR major depress* OR major depress* disorder OR atypical depress* OR melancholi* OR melancholi* depress* OR melancholi* feature OR peripartum depress* OR persistent depress* disorder OR dysthymic disorder OR dysthymi*) AND (gestational diabetes OR diabetic pregnancy OR diabetes mellitus OR type 1 diabetes mellitus OR type 2 diabetes mellitus OR NIDDM OR non-insulin dependent diabetes mellitus OR insulin dependent diabetes OR pregnancy diabetes mellitus) for related studies. The search strategies are shown in Table S1.
2.2. Study Selection
Firstly, relevant articles identified through the databases were imported into Endnote program X5 version and any duplicate publications were removed. This step was performed by two investigators (K.W.L. and S.Y.L.) independently. Secondly, two investigators (K.W.L. and S.Y.L.) independently screened the titles and abstracts of those articles for suitability based on the search strategies mentioned above. Thirdly, full-text articles were assessed based on the inclusion criteria mentioned below by two investigators (K.W.L. and S.Y.L.) independently. Any disagreements were resolved by discussion before commencing the quantitative analysis. In addition, we manually performed reverse–forward citation tracking of the identified studies. This step was also performed by two investigators (K.W.L. and S.Y.L.) independently.
2.3. Inclusion Criteria
Cohort studies were eligible for quantitative analysis if the study’s participants consisted of those with and without DIP. The studies were also required to present data of antepartum depression screened or diagnosed at either the second or third trimester as a primary or secondary outcome. The studies must have been published in an English peer-reviewed journal. Studies were excluded if the samples size was less than 100 or there was no information on which trimester the depression assessment was conducted. We also excluded studies that did not show any data relevant to a correlation between DIP and antepartum depression; these studies were categorized as “insufficient data” in PRISMA flowchart.
2.4. Data Extraction
The following data were extracted by two reviewers (K.W.L. and S.Y.L.): the last name of the first author, year of publication, country, ethnic origin, mean age or median of participants, number of participants with diagnosis in pregnancy among those with or without depression symptoms, study tool for assessment of depression, cut-off value for diagnosis of depression, and trimester where depression assessment was done. Data extraction was conducted independently, and the results of data extraction were compared between the two reviewers to ensure no errors.
2.5. Exposure and Outcomes Measures
Data regarding exposure to pre-existing DM are referred as pre-gestational diabetes (type 1 or type 2 DM diagnosed before pregnancy) [41]. GDM is defined as glucose intolerance of variable degree with onset or first recognition during pregnancy [42]. Diabetes in pregnancy (DIP) could refer to pre-existing DM and/or GDM.
Measures of exposure for DIP were derived in three ways. First, the number of DIPs was calculated by summing the number of pregnant women with pre-existing DM and GDM if both data were available separately in original articles. Second, if pre-existing DM and GDM were presented as diabetic pregnant women in original articles in which differentiating the data between pre-existing DM and GDM could never be possible, we used the number of diabetic pregnant women in calculation of the number of DIPs. Third, if the articles indicated the numbers of pregnant women with either pre-existing DM and GDM, the data of available groups (either pre-existing DM or GDM) were used in calculation for the numbers of DIPs and its risk for antepartum depression.
The outcome was the presence of antepartum depression, where it could be determined either with a confirmed diagnosis or use of screening tools. Any diagnostic guidelines or screening cut-off value for depression was acceptable for data synthesis in the meta-analysis. Measures of outcomes were the number of pregnant women with antepartum depression.
2.6. Data Synthesis
We used the relative risk (RR) and the corresponding 95% confidence interval (CI) to quantify the association between DIP and depression for observational studies. The meta-analyses were performed using a random-effects model of DerSimonian and Laird, which incorporates both within and between-study variability, as we anticipated between-study heterogeneity. Heterogeneity across studies was assessed using the I2 index (low was <25%, moderate 25%–50%, and high >50%), that indicated the total per cent of discrepancy due to studies variation [43].
2.7. Quality Assessment
The quality of the individual studies was determined using the checklist Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [44]. Two investigators (H.A.H. and N.K.D.) individually assessed the studies quality, and any discrepancies were resolved by discussion with the third investigator (S.M.C.). Studies were nevertheless included in analysis regardless of the STROBE score and grading.
2.8. Statistical Analysis
A random-effects (DerSimonian and Laird Method) meta-analysis was used throughout the analysis to compute the pooled RRs and their 95% CI [45,46]. We also examine potential publication bias by funnel plot, Begg’s test, and Egger’s test [47], and excluded those studies with high risk of publication bias from meta-analysis, which might be the source of heterogeneity. Heterogeneity across studies was assessed using the I2 index (low was <25%, moderate 25%–50%, and high >50%) [46]. A sensitivity analysis was conducted using leave-one-out meta-analysis to examine how each individual study affects the overall estimate of the rest of the studies. All analyses were performed using Open Meta(Analyst) software, this software can be accessed and downloaded from http://www.cebm.brown.edu/openmeta/index.html [48].
3. Results
3.1. Description of Included Studies
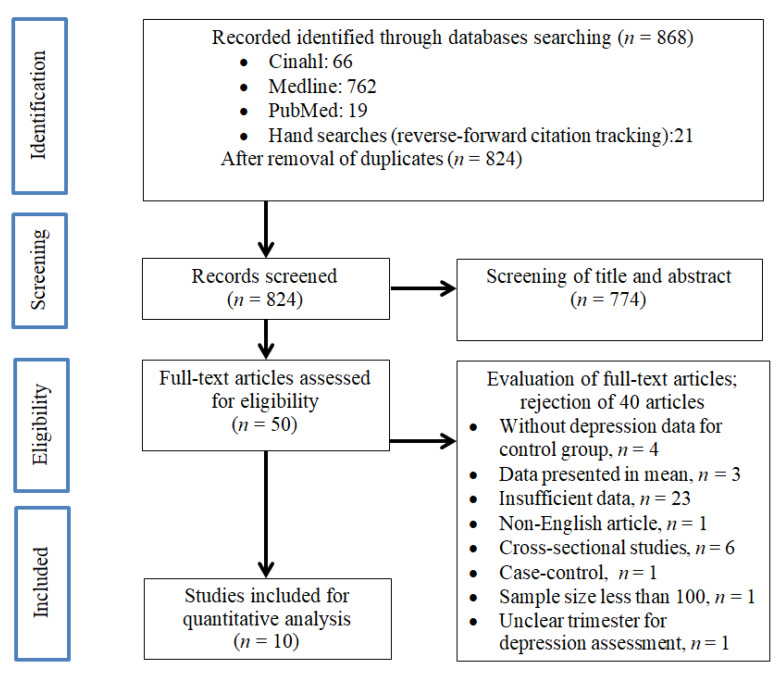
Our literature search identified 868 articles in the initial screening as shown in Figure 1. After removal of duplicate articles (n = 44), a total of 824 studies were retrieved for review of title and abstract. After screening for its suitability through title and abstract, 50 studies were subjected to full-text assessment for inclusion criteria. After careful evaluation of the 50 articles, 10 studies were eligible for quantitative analysis in this study.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRIMSA) flow diagram of the literature screening process.
3.2. Characteristics of Included Studies
The characteristics of the included studies are summarized in Table 1. A total sample of 71,036 pregnant women were included in the analyses. Among the 10 studies, six studies were conducted in USA [15,18,20,22], two studies were conducted in Australia [16,26], and one study conducted each in Brazil [11], Canada [24], Greece [27] and Ireland [17], respectively.
Table 1.
Characteristics of the included studies in meta-analysis which comprising 73,845 pregnant women whom depression was assessed in second or third trimester.
| Author, Year | Country | Ethnic Origin | Mean Age ± SD; Median (Range) | Study Tool for Assessment of Depression (Depression Type) | Cut Point for Diagnosis of Depression | Enrolment Trimester for Depression Assessment † | Study Conclusion | Quality * |
|---|---|---|---|---|---|---|---|---|
| Benute et al., 2010 [11] | Brazil | N/A | 30.2 ± 7.1 | Primary care evaluation of mental disorders (major depressive disorder) | Presence of 4–6 depressive symptoms | 28.2 week’s gestation ± 10.5 | Unplanned pregnancy in women with a medical disorder was identified as a risk factor for major depression during gestation. Major depression during pregnancy in women with a medical disorder should be routinely investigated using specific methods. | Poor |
| Cripe et al., 2011 [15] | USA | N/A | N/A | Assessment tool was not mentioned (depression) | N/A | <20 week’s gestation | Pregnant women with a history of migraine may benefit from screening for depression during prenatal care and vigilant monitoring, especially for women with co-morbid mood and migraine disorders. | Good |
| Daniells et al., 2003 [16] | Australia | N/A | N/A | Mental Health Inventory form—5 items (major depression) | >16 | 30 week’s gestation) | There were no sustained increased levels of anxiety for women diagnosed with Gestational diabetes mellitus (GDM). Concerns expressed about causing sustained maternal anxiety by testing for GDM could not be substantiated. | Good |
| Egan et al., 2017 [17] | Ireland | Type 1 diabetes mellitus group (Caucasian, 96.9%; non-Caucasian, 3.1%); GDM group (Caucasian, 89.7%; non-Caucasian, 10.3%); Control group (Caucasian, 98.1%; non-Caucasian, 1.9%) | N/A | Depression anxiety stress scale—21 items (clinically significant depression: moderate–extremely severe) | ≥14 | Third trimester | This work highlights a potential role for targeted psychological interventions to address and relieve symptoms of anxiety and depression among pregnant women with diabetes. | Good |
| Huang et al., 2015 [18] | USA | White, African American, Asian and others | N/A | Edinburgh Postnatal Depression Score—10 items (depressive symptoms) | ≥13 | ≤22 week’s gestation) | Pregnancy hyperglycaemia was cross-sectionally associated with higher risk of prenatal depressive symptoms, but not with postpartum depressive symptoms. | Good |
| Kozhimannil et al., 2009 [20] | USA | With diabetes mellitus group (White, 36.4%; African American, 46%; Other, 17.5%); Control group (White, 42.3%; African American, 45.3%; Other, 12.4%) | N/A | International Classification of Disease, ninth revision (depressive symptoms) | N/A | <37 week’s gestation) | Prepregnancy or gestational diabetes was independently associated with perinatal depression, including new onset of postpartum depression, in our sample of lowincome new mothers. | Good |
| Miller et al., 2020 [22] | USA | N/A | N/A | Patient Health Questionnaire—9 items (depression symptoms) | N/A | 18–28 week’s gestation) | The diagnosis of GDM was associated with an elevated risk of concomitant pregnancy diagnosis of depression. Given the elevated risk to patients diagnosed with GDM, a more frequent depression screening interval could be considered during the remainder of the pregnancy, such as each prenatal visit. | Good |
| Pace et al., 2018 [24] | Canada | N/A | (20–44) | International Classification of Disease, ninth revision (depressive symptoms) | N/A | 24–28 week’s gestation) | GDM is associated with an increased risk of depression in women particularly during pregnancy highlighting the need to screen for depression and provide supportive interventions during this period. | Good |
| Rumbold and Crowther, 2002 [26] | Australia | Caucasian, 90%; Asian, 5%; Aboriginal, 1% | 29.0 ± 5.0 | Edinburgh Postnatal Depression Score—36 items (depressive symptoms) | ≥12 | Third trimester (36 week’s gestation) | Screening for GDM had an adverse impact on women’s perceptions of their own health. | Poor |
| Varela et al., 2017 [27] | Greece | Greek, 93.2%; Other, 6.8% | N/A | Edinburgh Postnatal Depression Score—10 items (probably major depression) | ≥13 | Third trimester | GDM appears to be associated with depressive symptoms in the first week postpartum. Clinical implications and recommendations for future research are discussed, emphasizing the importance of closely monitoring women with GDM who seem more vulnerable to developing depressive symptomatology during the postnatal period. | Poor |
Note: N/A, Not available; SD, standard deviation. * The quality of the individual studies was determined using the checklist of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE), the assessment of study quality of included studies by STROBE checklist is shown in Table S2. † Unit used in enrolment trimester for depression assessment varies across studies, which data were presented either in precise week’s gestation, range of week’s gestation, mean of weeks’ gestation ± SD, or only trimesters.
In terms of screening for depression, Edinburg Postnatal Depression Score was the most commonly used assessment tool [18,26,27]. In addition, different cut-off points at 12 and 13 were used in Edinburgh Postnatal Depression Score, which differed across three studies. Other screening tools such as the Depression Anxiety Stress Scale [17], Mental Health Inventory Form [16], and Primary care evaluation of Mental disorders [11] were used in some of the studies. For diagnostic purposes, the International Classification of Disease [20,24] and Patient Health Questionnaire [22] were used. There were also studies [15] in which the screening tool for depression was not mentioned.
Half of the included studies provided data of respondent ethnicity composition. As we could see that most of the respondents comprised of Caucasians. The mean age range was within 29 to 30.2 years old, however these values merely came from two studies that reported this value [11,26], and majority of the studies did not report mean age of respondent. In regard to quality of studies, the majority of studies had a score of 14 or above [15,16,17,18,20,22,24] except for three studies [11,26,27].
3.3. DIP and Risk of Antepartum Depression
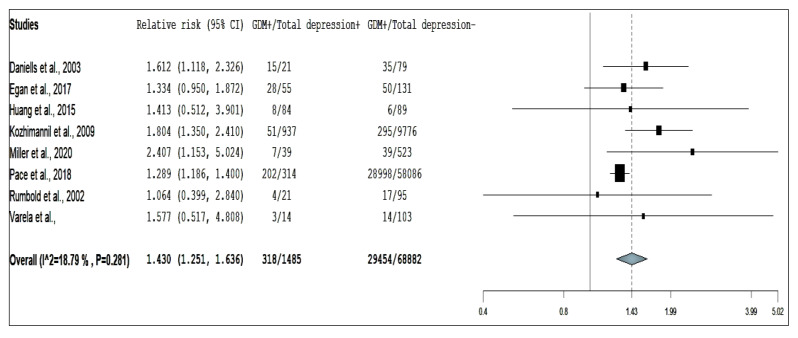
Eight studies reporting on the association between risk of antepartum depression and GDM, three studies for pre-existing DM, and nine studies for DIP were included for the overall analysis. The pooled RR using random-effect models are presented in Figure 2, Figure 3 and Figure 4.
Figure 2.
Forest plot of gestational diabetes mellitus and risk of antepartum depression.
Figure 3.
Forest plot of pre-existing diabetes mellitus and risk of antepartum depression.
Figure 4.
Forest plot of diabetes in pregnancy and risk of antepartum depression.
The results suggest that women with GDM have a statistically significant 43% increase in risk of developing antepartum depression (pooled RR = 1.430, 95% CI: 1.251–1.636; Figure 2). There was low degree of heterogeneity across the included studies (I2 = 18.8, p = 0.281). The funnel plot, Egger’s test (p = 0.882) and Begg’s test (p = 0.621) suggested that there was no publication bias (Figure S1 and Table S3). Nevertheless, sensitivity analysis identified all studies had substantial influences on the overall relative risk, which cause variation in pooled RRs ranging from 1.313 to 1.605 [16,17,18,20,22,24,26,27].
Our study showed that pregnant women with pre-existing DM, compared with those without diabetes, had an insignificant pooled RR of 1.300 (95% CI: 0.736–2.297) and I2 for heterogeneity was 68.0% (p = 0.044; Figure 3). The test for the small-study effect suggests that there was evidence present based on Begg’s test (p Value= 0.117) but not on funnel plots and Egger’s test (p Value = 0.216; Figure S2 and Table S4) after the study by Cripe et al. [15] was excluded from analysis. The study by Cripe et al. [15] was removed from the analysis because it caused a high degree of heterogeneity (I2 = 92.3%, p < 0001) and the test for the small-study effect suggested that this study [15] may have publication bias, of which there was evidence present based on funnel plot and Egger’s test (p = 0.076) but not in Begg’s test (p = 1.000). Sensitivity analysis of all studies had substantial influences on the overall relative risk, which cause variation in pooled RRs ranging from 1.300 to 6.778 [11,15,17,20].
The association between DIP and antepartum depression was significant compared with those without DIPs (pooled RR = 1.601, 95% CI: 1.190–2.153, I2 = 82.5, p <0.001 for heterogeneity). Funnel plot and Egger’s test (p = 0.091) but not Begg’s test (p = 0.655) indicated that the study by Cripe et al. [15] may have had publication bias. Overall, all studies [11,15,16,17,18,20,22,24,26,27] affected the pooled RRs, causing it to vary from 1.431 to 1.779 after combining the number of pregnant women with pre-existing DM and GDM compared with those without diabetes. Due to the high heterogeneity and publication bias, we removed the study by Cripe et al. [15] from the meta-analysis. After the study by Cripe et al. [15] was excluded from analysis (Figure 4), the pooled RR was 1.431 (95% CI: 1.205–1.699) and the I2 reduced to 50.0% (p = 0.043). We also did not find any evidence of publication bias when we reassessed the funnel plot, Egger’s (p = 0.462) and Begg’s test (p = 0.532; for publication bias, both p > 0.20; Figure S3 and Table S5) after performing this crucial step [15].
3.4. Sensitivity and Publication Bias Analysis
Sensitivity analysis revealed that excluding any of the studies could cause significant changes to the pooled relative risk. The decision whether to exclude any study from the meta-analyses was made after considering the publication bias analysis as well as the heterogeneity prior to excluding any of the eligible studies. Based on the funnel plot, Egger’s test and Begg’s test, there was no evidence of publication bias in the meta-analysis of GDM. Therefore, we did not exclude any studies from the meta-analysis.
On the other hand, we found that the study by Cripe et al. [15] may have contributed to publication bias in meta-analysis for pre-existing DM and DIP and risk of antepartum depression. After removing the study by Cripe et al. [15] from the meta-analysis for pre-existing DM and risk of antepartum depression, the pooled RRs were reduced from 3.433 (95% CI: 0.988–11.927) to a RR of 1.300 (95% CI: 0.736–2.297) and heterogeneity was also greatly reduced from 92.3% to 68.0%.
Similar observation was also seen in the association between DIP and the risk of antepartum depression, in which the pooled RRs also declined (from pooled RR = 1.601 to pooled RR = 1.431 by excluding the study by Cripe et al. [15] and heterogeneity was reduced by nearly half from I2 = 82.5% to I2 = 50.0, which once again proved that the study by Cripe et al. [15] could have contributed to the publication bias (as shown by the funnel plot and Egger’ test, p = 0.091).
4. Discussion
To our knowledge, this is the first meta-analysis to comprehensively summarize the association between DIP and the risk of antepartum depression. This study aimed to assess whether pregnant women with pre-existing DM or GDM are indeed at a higher risk of developing antepartum depression.
In the present meta-analysis, it was demonstrated that the presence of GDM correlated with a 43% increased risk of having antepartum depression, and DIP presence also indicated a similar result in its association with antepartum depression. Even though this meta-analysis showed significant increased risk of antepartum depression in women with GDM, it would be too premature to say that DIP and antepartum depression have a strong association due to the individual biases of the studies and limitation of this study. Therefore, more studies are needed to look into this association. Having said that, a possible physiologic mechanism for this significant association could be linked to the secretion of cortisol and expression of certain inflammation markers in pregnancy [49], that are in turn associated with hyperglycemia and insulin resistance [50]. Therefore, the abnormal secretion of these stress hormones could be exacerbated in the presence of hyperglycemia and insulin resistance in pregnancy [50], which might lead to a heightened inflammatory response that is common among those with depression [49]. Another psychological explanation could be linked indirectly to fears and worries of the developing obstetrics complications among women with GDM, especially about the possible consequences for their unborn child and also resultant poor maternal health and distress that could lead to maternal depression [16,51,52].
Surprisingly, our study found a no association between pre-existing DM in pregnancy and the risk of developing antepartum depression. The statistical power could be limited by the mere inclusion of three studies having high heterogeneity for the current meta-analysis. Nevertheless, the lack of association could also be explained by the possibility that women with pre-existing DM were more aware of the importance of physical activity and weight control through various psycho-education or lifestyle modification programs they were exposed to prior to conceiving. This may also help in improving the insulin resistance and preventing the emergence of depressive symptoms [53]. In addition, individuals having a longer duration of diabetes could have better illness perception, and are therefore more able to cope constructively with their disease [54,55]. These facilitate self-efficacious behaviors among pregnant women with pre-existing DM [56], leading to better health outcomes and less depressive symptoms during pregnancy. However, the information on the duration of diabetes illness and the extent of anti-diabetic medication adherence were not available in these included studies. Thus, it was not possible to consider these variables in sub-group analysis.
A prior meta-analysis estimated that GDM significantly increased the risk of postpartum depression by a pooled RR ranging from 1.32 to 1.59 [29,30]. Meanwhile, we estimated that the association between GDM and risk of antepartum depression was statistically significant at with a pooled RR at 1.43. Even though antepartum and postpartum are two distinctive periods, there are similarities in finding of GDM and its risk on antepartum and postpartum depression. It can therefore be assumed that presence of perinatal depression could possibly be related to GDM. However, a prior systematic review and meta-analysis that reported the pooled prevalence [6,8,32] and the risk factors for antepartum depression [9] did not include GDM in the meta-analyses. Therefore, if new study is available in the future, a more detailed conclusion can be drawn. Until then, based on the available studies, this is the first study that shows a possible association between DIP and antepartum depression.
4.1. Implications of This Study
The co-existence of DIP and depression could be a lethal combination. Therefore, it is important to be able to identify pregnant women with diabetes at risk of developing antepartum depression earlier for various reasons. For the mother, antepartum depression is known to cause detrimental effects such as poor self-care, impaired quality of life, increased risk of suicide, and postnatal depression [57]. For the new-born babies, early recognition and intervention on antepartum depression can prevent the associated adverse perinatal outcomes such as preterm delivery, low birth weight, growth retardation, infants having diarrheal diseases or with disrupted cardiorespiratory regulation and feeding problem, as well as long term cognitive and behavioral deficits [58,59].
For healthcare providers, this indicates the need to screen for depression in woman with DIP. For policymakers, the latest clinical practice guidelines should clearly outline the need for those providing antepartum services to do this important screening.
In view of the fact that antepartum depression is a negative psychological effect of DIP, and both conditions are associated with an increased possibility of both maternal and neonatal adverse outcome [60,61], it is therefore pertinent to acknowledge DIP as one of the associated factor for antepartum depression.
4.2. Strength and Limitations
This is the first systematic review and meta-analysis that reported a significant association between GDM, DIP, and antepartum depression, in which it estimated the relative risk based on 10 cohort studies comprising of more than 71,000 pregnant women.
Our meta-analysis has a number of potential limitations. First, the questionnaire used in evaluation of depression varied across studies. Furthermore, we notice that different cut-off points at 12 and 13 were used in the Edinburgh Postnatal Depression Score, which differed across three studies. In a one of the studies the questionnaire used for assessment of depression was not even mentioned, which may have increased the risk of information bias. Second, data on the history of depression prior to pregnancy have been particularly helpful for subgroup analysis. However, the availability of these data was very limited leading to an increased risk of confounding bias that could not be solved by this meta-analysis. Third, data of the current study were dominated by studies in Western countries, and less so from Asian and African countries. Therefore, the finding of this study should be interpreted with caution. In fact, there are studies on the correlation between DIP and antepartum depression that have been reported from Eastern countries, but they were conducted with a cross-sectional design. We choose cohort study design as one of our inclusion criteria because it demonstrates a more causal relationship than cross-sectional study design. Therefore, many studies from Eastern countries were not eligible for statistical analysis.
5. Conclusions
In summary, our study suggested that the presence of GDM significantly increased the risk of developing antepartum depression. Given the appreciable relative risk of antepartum depression among those with DIP, more attention on the mental health status should be given to pregnant women diagnosed with pre-existing DM and GDM. Furthermore, more studies from Eastern countries with a well-designed prospective study design are needed to confirm our study findings.
Acknowledgments
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
List of Abbreviations
| GDM | Gestational diabetes mellitus |
| DM | Diabetes mellitus |
| DIP | Diabetes in pregnancy |
| RR | Relative risk |
| CI | Confidence interval |
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/11/3767/s1, Figure S1: Funnel plot of studies evaluating the risk of antepartum depression associated with gestational diabetes mellitus, Figure S2: Funnel plot of studies evaluating the risk of antepartum depression associated with pre-existing diabetes mellitus, Figure S3: Funnel plot of studies evaluating the risk of antepartum depression associated with diabetes in pregnancy, Table S1: Search terms used for final search on 27 December 2019, Table S2: Publication bias was assessed by Egger’s test and Begg’s test for association between GDM and risk of antepartum depression, Table Table S3: Publication bias was assessed by Egger’s test and Begg’s test for association between GDM and risk of antepartum depression. Table S4: Publication bias was assessed by Egger’s test and Begg’s test for association between pre-existing DM and risk of antepartum depression, Table S5: Publication bias was assessed by Egger’s test and Begg’s test for association between diabetes in pregnancy and risk of antepartum depression.
Author Contributions
Conceptualization, K.W.L., S.M.C. and S.C.C.; Data curation, N.K.D., S.C.C., S.Y.L., and H.A.H.; Formal analysis, K.W.L. and H.C.L.; Investigation, S.M.C., N.K.D., S.C.C., and H.A.H.; Methodology, K.W.L. and S.Y.L.; Supervision, S.M.C.; Validation, S.Y.L., H.A.H., and H.C.L.; Visualization, H.A.H.; Writing—original draft, K.W.L., N.K.D., S.C.C., and H.A.H.; Writing—review and editing, K.W.L., S.M.C., N.K.D., S.C.C., and H.C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received its funding from the Universiti Putra Malaysia under Putra Graduate Initiative (UPM/700-2/1/GP-IPS/2018/9593800), High Impact Grant (UPM/800-3/3/1/GPB/2018/9659600) and Graduate Research Fellowship (UPM/SPS/GS48750). The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- 1.Wang J., Wu X., Lai W., Long E., Zhang X., Li W., Zhu Y., Chen C., Zhong X., Lin H., et al. Prevalence of depression and depressive symptoms among outpatients: A systematic review and meta-analysis. BMJ Open. 2017;7:e017173. doi: 10.1136/bmjopen-2017-017173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Westdahl C., Milan S., Magriples U., Kershaw T.S., Rising S.S., Ickovics J.R. Social Support and Social Conflict as Predictors of Prenatal Depression. Obstet. Gynecol. 2007;110:134–140. doi: 10.1097/01.AOG.0000265352.61822.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- 4.Bloch M., Daly R.C., Rubinow D.R. Endocrine factors in the etiology of postpartum depression. Compr. Psychiatry. 2003;44:234–246. doi: 10.1016/S0010-440X(03)00034-8. [DOI] [PubMed] [Google Scholar]
- 5.Llewellyn A.M., Stowe Z.N., Nemeroff C.B. Depression during pregnancy and the puerperium. J. Clin. Psychiatry. 1997;58:26–32. [PubMed] [Google Scholar]
- 6.Bennett H.A., Einarson A., Taddio A., Koren G., Einarson T.R. Prevalence of Depression during Pregnancy: Systematic Review. Obstet. Gynecol. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- 7.Lee K.W., Ching S.M., Hoo F.K., Ramachandran V., Chong S.C., Tusimin M., Nordin N.M. Prevalence and factors associated with depressive, anxiety and stress symptoms among women with gestational diabetes mellitus in tertiary care centres in Malaysia: A cross-sectional study. BMC Pregnancy Childbirth. 2019;19:367. doi: 10.1186/s12884-019-2519-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woody C., Ferrari A., Siskind D., Whiteford H.A., Harris M. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Arora P., Aeri B.T. Burden of antenatal depression and its risk factors in Indian settings: A systematic review. Indian J. Med. Spec. 2019;10:55. [Google Scholar]
- 10.Bennett W.L., Chang H.-Y., Levine D.M., Wang L., Neale D., Werner E.F., Clark J.M. Utilization of Primary and Obstetric Care After Medically Complicated Pregnancies: An Analysis of Medical Claims Data. J. Gen. Intern. Med. 2014;29:636–645. doi: 10.1007/s11606-013-2744-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benute G.R.G., Nomura R.M.Y., Reis J.S., Fraguas Junior R., Lucia MCSd Zugaib M. Depression during pregnancy in women with a medical disorder: Risk factors and perinatal outcomes. Clinics (Sao Paulo, Brazil) 2010;65:1127–1131. doi: 10.1590/S1807-59322010001100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bisson M., Series F., Giguere Y., Pamidi S., Kimoff J., Weisnagel S.J., Marc I. Gestational Diabetes Mellitus and Sleep-Disordered Breathing. Obstet. Gynecol. 2014;123:634–641. doi: 10.1097/AOG.0000000000000143. [DOI] [PubMed] [Google Scholar]
- 13.Byrn M., Penckofer S. The Relationship between Gestational Diabetes and Antenatal Depression. J. Obstet. Gynecol. Neonatal Nurs. 2015;44:246–255. doi: 10.1111/1552-6909.12554. [DOI] [PubMed] [Google Scholar]
- 14.Chazotte C., Freda M.C., Elovitz M., Youchah J. Maternal Depressive Symptoms and Maternal–Fetal Attachment in Gestational Diabetes. J. Women’s Health. 1995;4:375–380. doi: 10.1089/jwh.1995.4.375. [DOI] [Google Scholar]
- 15.Cripe S.M., Frederick I.O., Qiu C., Williams M.A. Risk of preterm delivery and hypertensive disorders of pregnancy in relation to maternal co-morbid mood and migraine disorders during pregnancy. Paediatr. Périnat. Epidemiol. 2011;25:116–123. doi: 10.1111/j.1365-3016.2010.01182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniells S., Grenyer B.F., Davis W.S., Coleman K.J., Burgess J.-A.P., Moses R.G. Gestational diabetes mellitus: Is a diagnosis associated with an increase in maternal anxiety and stress in the short and intermediate term? Diabetes Care. 2003;26:385–389. doi: 10.2337/diacare.26.2.385. [DOI] [PubMed] [Google Scholar]
- 17.Egan A.M., Dunne F.P., Lydon K., Conneely S., Sarma K., E McGuire B. Diabetes in pregnancy: Worse medical outcomes in type 1 diabetes but worse psychological outcomes in gestational diabetes. QJM Int. J. Med. 2017;110:721–727. doi: 10.1093/qjmed/hcx106. [DOI] [PubMed] [Google Scholar]
- 18.Huang T., Rifas-Shiman S.L., Ertel K.A., Rich-Edwards J., Kleinman K., Gillman M.W., Oken E., James-Todd T. Pregnancy Hyperglycaemia and Risk of Prenatal and Postpartum Depressive Symptoms. Paediatr. Périnat. Epidemiol. 2015;29:281–289. doi: 10.1111/ppe.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katon J.G., Russo J., Gavin A.R., Melville J.L., Katon W.J. Diabetes and depression in pregnancy: Is there an association? J. Women’s Health. 2011;20:983–989. doi: 10.1089/jwh.2010.2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kozhimannil K.B., Pereira M.A., Harlow B.L. Association between diabetes and perinatal depression among low-income mothers. JAMA. 2009;301:842–847. doi: 10.1001/jama.2009.201. [DOI] [PubMed] [Google Scholar]
- 21.Lara-Cinisomo S., Swinford C., Massey D., Hardt H. Diabetes, Prenatal Depression, and Self-Rated Health in Latina Mothers. Diabetes Spectr. 2018;31:159–165. doi: 10.2337/ds17-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller N.E., Curry E., Laabs S.B., Manhas M., Angstman K. Impact of gestational diabetes diagnosis on concurrent depression in pregnancy. J. Psychosom. Obstet. Gynecol. 2020;2020:1–4. doi: 10.1080/0167482X.2019.1709816. [DOI] [PubMed] [Google Scholar]
- 23.Natasha K., Hussain A., Khan A.K.A. Prevalence of depression among subjects with and without gestational diabetes mellitus in Bangladesh: A hospital based study. J. Diabetes Metab. Disord. 2015;14:64. doi: 10.1186/s40200-015-0189-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pace R., Rahme E., Da Costa D., Dasgupta K. Association between gestational diabetes mellitus and depression in parents: A retrospective cohort study. Clin. Epidemiol. 2018;10:1827–1838. doi: 10.2147/CLEP.S184319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Räisänen S., Lehto S.M., Nielsen H.S., Gissler M., Kramer M.R., Heinonen S. Risk factors for and perinatal outcomes of major depression during pregnancy: A population-based analysis during 2002–2010 in Finland. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-004883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rumbold A.R., Crowther C.A. Women’s experiences of being screened for gestational diabetes mellitus. Aust. N. Z. J. Obstet. Gynaecol. 2002;42:131–137. doi: 10.1111/j.0004-8666.2002.00131.x. [DOI] [PubMed] [Google Scholar]
- 27.Varela P., Spyropoulou A.C., Kalogerakis Z., Vousoura E., Moraitou M., Zervas I.M. Association between gestational diabetes and perinatal depressive symptoms: Evidence from a Greek cohort study. Prim. Health Care Res. Dev. 2017;18:1–7. doi: 10.1017/S1463423617000317. [DOI] [PubMed] [Google Scholar]
- 28.Zain S., Raghib M.F., Khan H.A., Mustafa S.F., Fatima S.S. Relationship between Diabetes and Depression Severity in Pregnant Females. J. Pioneer. Med. Sci. 2016;6:22–26. [Google Scholar]
- 29.Arafa A., Dong J.-Y., Ahmed A. Gestational diabetes and risk of postpartum depressive symptoms: A meta-analysis of cohort studies. J. Affect. Disord. 2019;253:312–316. doi: 10.1016/j.jad.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Azami M., Badfar G., Soleymani A., Rahmati S., Solemani A. The association between gestational diabetes and postpartum depression: A systematic review and meta-analysis. Diabetes Res. Clin. Pr. 2019;149:147–155. doi: 10.1016/j.diabres.2019.01.034. [DOI] [PubMed] [Google Scholar]
- 31.Radoš S.N., Matijaš M., Anđelinović M., Čartolovni A., Ayers S. The role of posttraumatic stress and depression symptoms in mother-infant bonding. J. Affect. Disord. 2020;268:134–140. doi: 10.1016/j.jad.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 32.Gavin N.I., Gaynes B.N., Lohr K.N., Meltzer-Brody S., Gartlehner G., Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstet. Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 33.Bilszta J.L., Gu Y.Z., Meyer D., Buist A.E. A geographic comparison of the prevalence and risk factors for postnatal depression in an Australian population. Aust. N. Z. J. Public Health. 2008;32:424–430. doi: 10.1111/j.1753-6405.2008.00274.x. [DOI] [PubMed] [Google Scholar]
- 34.Josefsson A., Angelsiöö L., Berg G., Ekström C.-M., Gunnervik C., Nordin C., Sydsjö G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet. Gynecol. 2002;99:223–228. doi: 10.1016/s0029-7844(01)01722-7. [DOI] [PubMed] [Google Scholar]
- 35.Bellamy L., Casas J.-P., Hingorani A.D., Williams D. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet. 2009;373:1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 36.Negrato C.A., Mattar R., Gomes M.B. Adverse pregnancy outcomes in women with diabetes. Diabetol. Metab. Syndr. 2012;4:41. doi: 10.1186/1758-5996-4-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wahabi H., A Esmaeil S., Fayed A., Al-Shaikh G., Alzeidan R. Pre-existing diabetes mellitus and adverse pregnancy outcomes. BMC Res. Notes. 2012;5:496. doi: 10.1186/1756-0500-5-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jensen D.M., Feilberg-Jorgensen N., Westergaard J.G., Beck-Nielsen H., Sørensen B. Maternal and perinatal outcomes in 143 Danish women with gestational diabetes mellitus and 143 controls with a similar risk profile. Diabet. Med. 2000;17:281–286. doi: 10.1046/j.1464-5491.2000.00268.x. [DOI] [PubMed] [Google Scholar]
- 39.Ross G.P., Falhammar H., Chen R., Barraclough H., Kleivenes O., Gallen I. Relationship between depression and diabetes in pregnancy: A systematic review. World J. Diabetes. 2016;7:554–571. doi: 10.4239/wjd.v7.i19.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P.G., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mellitus P.D. Acog Practice Bulletin Summary. Obstet. Gynecol. 2018;132:e228–e248. doi: 10.1097/AOG.0000000000002960. [DOI] [PubMed] [Google Scholar]
- 42.Diabetes I.A., Panel P.S.G.C. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 44.Vandenbroucke J.P., Von Elm E., Altman D.G., Gøtzsche P.C., Mulrow C.D., Pocock S.J., Poole C., Schlesselman J.J., Egger M., Initiative S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 2007;4:e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 46.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman U.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wallace B.C., Dahabreh I.J., Trikalinos T., Lau J., Trow P., Schmid C.H. Closing the Gap between Methodologists and End-Users: R as a Computational Back-End. J. Stat. Softw. 2012;49 doi: 10.18637/jss.v049.i05. [DOI] [Google Scholar]
- 49.Black P.H. The inflammatory consequences of psychologic stress: Relationship to insulin resistance, obesity, atherosclerosis and diabetes mellitus, type II. Med Hypotheses. 2006;67:879–891. doi: 10.1016/j.mehy.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 50.Lustman P.J., Clouse R.E. Depression in diabetic patients: The relationship between mood and glycemic control. J. Diabetes Complicat. 2005;19:113–122. doi: 10.1016/j.jdiacomp.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 51.Lapolla A., Di Cianni G., Di Benedetto A., Franzetti I., Napoli A., Sciacca L., Torlone E., Tonutti L., Vitacolonna E., Mannino D. Quality of Life, Wishes, and Needs in Women with Gestational Diabetes: Italian DAWN Pregnancy Study. Int. J. Endocrinol. 2012;2012:1–6. doi: 10.1155/2012/784726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee K.W., Ching S.M., Hoo F.K., Ramachandran V., Chong S.C., Tusimin M., Nordin N.M., Devaraj N.K., Cheong A.T., Chia Y.C. Neonatal outcomes and its association among gestational diabetes mellitus with and without depression, anxiety and stress symptoms in Malaysia: A cross-sectional study. Midwifery. 2019;81:102586. doi: 10.1016/j.midw.2019.102586. [DOI] [PubMed] [Google Scholar]
- 53.Silva N., Atlantis E., Ismail K. A review of the association between depression and insulin resistance: Pitfalls of secondary analyses or a promising new approach to prevention of type 2 diabetes? Curr. Psychiatry Rep. 2012;14:8–14. doi: 10.1007/s11920-011-0245-8. [DOI] [PubMed] [Google Scholar]
- 54.Knowles S.R., Apputhurai P., O’Brien C.L., Ski C.F., Thompson D.R., Castle D.J. Exploring the relationships between illness perceptions, self-efficacy, coping strategies, psychological distress and quality of life in a cohort of adults with diabetes mellitus. Psychol. Health Med. 2019;25:214–228. doi: 10.1080/13548506.2019.1695865. [DOI] [PubMed] [Google Scholar]
- 55.Zhu T.H., Mooi C.S., Shamsuddin N.H. Diabetes empowerment scores among type 2 diabetes mellitus patients and its correlated factors: A cross-sectional study in a primary care setting in Malaysia. World J. Diabetes. 2019;10:403. doi: 10.4239/wjd.v10.i7.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chew B.H., Shariff-Ghazali S., Fernandez A. Psychological aspects of diabetes care: Effecting behavioral change in patients. World J. Diabetes. 2014;5:796–808. doi: 10.4239/wjd.v5.i6.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Målqvist M., Clarke K., Matsebula T., Bergman M., Tomlinson M. Screening for Antepartum Depression through Community Health Outreach in Swaziland. J. Community Health. 2016;41:946–952. doi: 10.1007/s10900-016-0175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Joshi D., Shrestha S., Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS ONE. 2019;14:e0214992. doi: 10.1371/journal.pone.0214992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schaffir J. Consequences of antepartum depression. Clin. Obstet. Gynecol. 2018;61:533–543. doi: 10.1097/GRF.0000000000000374. [DOI] [PubMed] [Google Scholar]
- 60.Byrn M.A., Penckofer S. Antenatal Depression and Gestational Diabetes: A Review of Maternaland Fetal Outcomes. Nurs. Women’s Health. 2013;17:22–33. doi: 10.1111/1751-486X.12003. [DOI] [PubMed] [Google Scholar]
- 61.Rasmussen-Torvik L.J., Harlow B.L. The Association between Depression and Diabetes in the Perinatal Period. Curr. Diabetes Rep. 2010;10:217–223. doi: 10.1007/s11892-010-0108-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.