Abstract
Background
A growing gap has emerged between people with mental illness and health care professionals, which in recent years has been successfully closed through the adoption of peer support services (PSSs). Peer support in mental health has been variously defined in the literature and is simply known as the help and support that people with lived experience of mental illness or a learning disability can give to one another. Although PSSs date back to several centuries, it is only in the last few decades that these services have formally evolved, grown, and become an integral part of the health care system. Debates around peer support in mental health have been raised frequently in the literature. Although many authors have emphasized the utmost importance of incorporating peer support into the health care system to instill hope; to improve engagement, quality of life, self-confidence, and integrity; and to reduce the burden on the health care system, other studies suggest that there are neutral effects from integrating PSSs into health care systems, with a probable waste of resources.
Objective
In this general review, we aimed to examine the literature, exploring the evolution, growth, types, function, generating tools, evaluation, challenges, and the effect of PSSs in the field of mental health and addiction. In addition, we aimed to describe PSSs in different, nonexhaustive contexts, as shown in the literature, that aims to draw attention to the proposed values of PSSs in such fields.
Methods
The review was conducted through a general search of the literature on MEDLINE, Google Scholar, EMBASE, Scopus, Chemical Abstracts, and PsycINFO. Search terms included peer support, peer support in mental health, social support, peer, family support, and integrated care.
Results
There is abundant literature defining and describing PSSs in different contexts as well as tracking their origins. Two main transformational concepts have been described, namely, intentional peer support and transformation from patients to peer support providers. The effects of PSSs are extensive and integrated into different fields, such as forensic PSSs, addiction, and mental health, and in different age groups and mental health condition severity. Satisfaction of and challenges to PSS integration have been clearly dependent on a number of factors and consequently impact the future prospect of this workforce.
Conclusions
There is an internationally growing trend to adopt PSSs within addiction and mental health services, and despite the ongoing challenges, large sections of the current literature support the inclusion of peer support workers in the mental health care workforce. The feasibility and maintenance of a robust PSS in health care would only be possible through collaborative efforts and ongoing support and engagement from all health care practitioners, managers, and other stakeholders.
Keywords: peer support, peer support workers, mental illness and addiction, social support, literature review
Introduction
Peer support services (PSSs) are novel interventions recently adopted in mental health systems worldwide. It is believed, however, that PSSs date back to more than three centuries to the moral treatment era [1], albeit on an informal basis. Diverse definitions and classifications for PSSs have been provided in the literature [2-4], and numerous reports have praised and supported the service provided by peer support workers (PSWs) [5-8]. However, other literature suggests the neutral effects of PSSs, with weak associated evidence to support such services [9,10]. The potential impact of PSWs on their peers [11-14] has received considerable attention in the literature.
PSSs have been introduced in different contexts, such as family PSWs [15-19], the forensic field [20,21], and online PSSs. A considerable number of strategies were proposed to generate an effective PSS in the mental health field amid a number of associated concerns and challenges [22-25].
Methods
This general review sheds light on PSWs’ experiences, benefits, challenges, opportunities to expand access to quality addiction, and mental health care using PSSs. The review was conducted through a general search of the literature on MEDLINE, Google Scholar, EMBASE, Scopus, Chemical Abstracts, and PsycINFO. Search terms included peer support, peer support in mental health, social support, peer, family support, and integrated care. We began the review with an examination of the definitions, origins, and types of peer support contributions and within different clinical contexts, aiming at deepening the view to the diverse effects of such a workforce. We then continued with examining the transition from a patient role to a PSW role and their incorporation into mental health systems. Thereafter, we provided a conceptual framework for the effects of peer support and stigma in relation to PSWs. We concluded the review by examining the benefits and challenges associated with PSSs and provided a commentary on future directions for PSSs in mental health.
Results
Definitions
Peer support has diverse meanings in the literature. For example, it is a system of giving and receiving help founded on key principles of respect, shared responsibility, and an agreement of what is helpful [26]. A peer is defined as an equal, someone with whom one shares demographic or social similarities, whereas support refers to “the kind of deeply felt empathy, encouragement, and assistance that people with shared experiences can offer one another within a reciprocal relationship” [3]. The Mental Health Foundation in the United Kingdom defined peer support in mental health as “the help and support that people with lived experience of a mental illness or a learning disability can give to one another” [27]. Peer employees were also defined as “individuals who fill designated unique peer positions as well as peers who are hired into traditional MH positions” [28]. In 1976, authors defined self-help groups as “voluntary small group structures for mutual aid in the accomplishment of a specific purpose...usually formed by peers who have come together for mutual assistance in satisfying a common need, overcoming a common handicap or life-disrupting problem, and bringing about desired social and/or personal change” [28]. Although the mutual relationship was sometimes overlooked and rather described as an asymmetric or nearly one-directional relationship [29], it is emphasized upon as 1 of the 4 main tasks for peer support accomplishments, which are mutuality, connection, worldwide, and moving toward rather than moving away [30].
Origin and Growth of Peer Support
Davidson et al [11] have expressed the paradigm that calls for new models of community-based practice, which turned away from case management and from conceptualizing old practices under new terms. In the 1990s, peer support was formally introduced as a service in community mental health care. However, there is evidence of its practice throughout history, including during the moral treatment era in France at the end of the 18th century [1]. Recently, peer support has been rapidly growing in many countries and could attract a considerable amount of research [22]. Although Lunatic Friends’ Society is known as the earliest peer support group in mental health, which was founded in England in the middle of the 19th century [31], self-help groups were described as the oldest and most pervasive of peer support types [28]. Some peer-run groups also formed in Germany in the late 19th century, which protested on involuntary confinement laws. In addition to this, several individuals in the 18th and 19th centuries publicized their protests about their treatment in autobiographies and petitions [32]. The origin of peer support even reaches further back than the earliest asylums [33]. Some authors suggest that peer support is not based on psychiatric models and diagnostic criteria [3]; however, it is about “understanding another’s situation empathically through the shared experience of emotional and psychological pain” [34]. In the United States, the start of legitimacy for peer support was ignited in 2007 by considering the conditions under which PSSs could be reimbursed by Medicaid [35]. Although this reform was entailing a recovery model, which has been adopted by health care providers and stakeholders in many “English-speaking” countries, it was not the case in many other countries, in which this reform was yet to be well formulated [36].
Transformational Concepts in Peer Support Service
Intentional Peer Support: Informal to Formal Peer Support Evolution
Intentional peer support (IPS) is described as a philosophical descendant of the informal peer support of the ex-patients’ movement in the 1970s [3]. It depends on a way of communication that immerses the provider into the recipient experience by stepping back from one’s story and being eagerly open to others’ stories [30]. In the field of psychiatry, trauma is blamed for playing a pivotal role in the experience, diagnosis, and treatment, and peer support is described as the logical environment for disseminating trauma-informed care (TIC) or service, which enables building relationships based on mutuality, shared power, and respect [37]. In the same context, trauma-informed peer support usually begins with the main question, “What happened to you?” instead of “What is wrong with you?” [30]. TIC is an explanatory model that identifies PSWs sharing lived experiences, ensuring safety and functioning as an advocate, and a liaison to patient management plans, where empowerment and intervention models are strongly emphasized upon [38,39]. The shift from a traditional biomedical model to recovery-oriented practice is meant to perceive trauma as a coping mechanism rather than a pathology [38,40]. This clearly entails training of all service providers for better acknowledgment and comfort in dealing with trauma survivors, with an understanding of trauma as an expectation rather than an exception [41]. Although the TIC concept has evolved over the years, it still lacks guidance, training, staff knowledge, and governmental support, which are necessary to ensure successful policy implementation [40]. The role of PSWs also extended to support those at risk of trauma events because of the nature of their work, including child protection workers, who are at risk of posttraumatic stress disorder or anxiety disorder [42]. Although IPS grew from the informal practices of grassroots-initiated peer support, it differs from earlier approaches because it is a theoretically based, manualized approach with clear goals and a fidelity tool for practitioners [14]. It instead focuses on the nature and purpose of the peer support relationship and its attention to skill building to purposefully engage in peer support relationships that promote mutual healing and growth [3]. Transitioning from informal to formal roles provides not only well-formulated expectations of the role but also a better chance to identify the potential conflict of the PSWs’ mixed identity [43].
Research conducted on PSWs has been conceptualized throughout history [22]. Starting with feasibility studies, at the initial stage, it is followed by studies comparing peer staff with nonpeer staff and, finally, the studies that answer questions such as the following:
Do interventions provided by peers differ from those provided by nonpeers?
What makes peer support a unique form of service delivery?
If so, to the previous question, what are the active ingredients of these aspects of peer support, and what outcomes can they produce?
Studies that provide answers to the latter set of questions are expected to provide a deeper understanding of the philosophical underpinnings of the IPS concept for PSSs.
The Transformation From Patient to Peer Support Providers
The shift from being a service recipient to a service provider has been contributing as a driving force to restore fundamental human rights, especially among those with serious mental illnesses (SMIs) [22]. Telling the personal lived experience leads to a profound shift, from telling an “illness story” to a “recovery story” [4]. This involved an identity transformation from being perceived as a victim or a patient to a person fully engaged in life with various opportunities ahead [4]. This transition is seen as a gradual process and one that is supported by several other personal changes with expected challenges [44]. Moving a full circle to include PSWs as the service provider has been undertaken by mental health services to further exceed the transformational role, which was primarily the main aim of providing such a service [45]. A liminal identity was given for PSWs as laying between several roles, being service users, friends, and staff. Thus, the professionalism of the PSW role might not be a successful way to ensure individual well-being or to promote the peer support initiative [46]. Thus, successful transitioning from the patient to PSW role involves fundamental functional shifts achieved through overcoming multiple barriers at the personal, health system, and societal levels.
Effects of Peer Support Service in Different Contexts
Trained PSWs or mentors can use communication behaviors useful to different client groups. Many studies showed the effectiveness and feasibility of applying for peer support as follows:
Severe or Serious Mental Illness
Generally, the evidence for peer support interventions for people with SMIs has been described as moderate to limited with mixed intervention effects [2,47]. On the one hand, adding PSSs to intensive case management teams proved to improve activation in terms of knowledge, skills, confidence, and attitudes for managing health and treatment. Hence, patients become healthier, report better quality of life (QOL), engage in more health care practices, and report more treatment satisfaction [48,49]. On the other hand, a systematic review of randomized controlled trials (RCTs) involving adults with SMIs, while showing some evidence of positive effects on measures of hope, recovery, and empowerment at and beyond the end of the PSS intervention in this review, did not show any positive effects on hospitalization, satisfaction, or overall symptoms [10]. Similarly, a Cochrane systematic review of PSSs for people with schizophrenia found inconclusive results, with a high risk of bias in most of the studies and insufficient data to support or refute the PSS for this group [50].
Addiction and Drug Users
In recent years, peer recovery support services have become an accepted part of the treatment for substance use disorders, providing a more extensive array of services that are typically associated with the mutual supportive intervention [51]. This is in contrast to the use of peer support for SMIs where evidence is still developing. The Substance Abuse and Mental Health Services Administration (SAMHSA) defined peer recovery support for substance use disorders as “a set of nonclinical, peer-based activities that engage, educate, and support individuals so that they can make life changes that are necessary to recover from substance use disorders” [51]. Despite the long-term nature of substance abuse, immersion in peer support groups and activities and active engagement in the community are considered the 2 critical predictors of recovery for more than half the dependent substance users [52].
A number of trials studied the peer support effect on drug users, especially in the emergency department [53,54]. Another randomized trial found that a socially focused treatment can affect change in the patient’s social network and hence increase support for abstinence, for example, an increase of one nondrinking friend in the social network is translated into a 27% increase in the probability of reporting abstinence on 90% of days or more at all follow-up visits, which extended to 15 months [55].
Forensic Peer Support Service
The forensic peer system refers to the engagement of peer specialists who have histories of mental illness as well as criminal justice involvement and who are trained to help other patients sharing similar accounts [20]. As referred to by Davidson and Rowe [20], “Forensic Peer Specialists embody the potential for recovery for people who confront the dual stigmas associated with SMI and criminal justice system involvement.”
They offer day-to-day support for those released early from jail by accompanying them to initial probation meetings or treatment appointments and referring them to potential employers and landlords, helping people to negotiate and minimize continuing criminal sanctions and training professional staff on engaging consumers with criminal justice history [20,21]. PSWs with incarceration histories could successfully identify the liminal space in being supportive rather than providing support for the criminal offense, in contrast with the conventional methods that directly confront criminality [56]. In fact, having criminal history is the “critical component” for achieving recovery [56]. Multiple initiatives have been introduced to facilitate a reentry process for people recently released from incarceration, including Forensic Assertive Community Treatment, Assertive Community Treatment, Critical Time Intervention, and Women’s Initiative Supporting Health Transitions Clinic, through diverse community support groups involving PSWs [57,58].
Old Adults
A peer support program undertaken by older community volunteers was effective in improving general and physical health, social functioning, depression parameters, and social support satisfaction, especially in socially isolated, low-income older adults [59]. The Reclaiming Joy Peer Support intervention (a mental health intervention that pairs an older adult volunteer with a participant) has the potential for decreasing depression symptoms and improving QOL indicators for both anxiety and depression [60]. Engaging the community in health research could be of a high value in acknowledging their own health needs [61].
Youth and Adolescents
Peer support programs are mostly needed for university students, where challenges with loneliness and isolation are well recognized [62]. Hence, a need emerged for training peers to support their peer adolescents with the prospective challenges at this age [63]. Trained peer support students without necessarily having a lived experience were also examined in England [64]. The study included university students measuring the acceptability and impact of the volunteer peer support program through 6 weekly sessions. Students with lower mental well-being were more likely to complete the course, and an improvement in mental well-being was recorded for those who attended more frequently. Overall, peers remain to be an essential source of support for young people experiencing mental health and substance use problems [65].
Medically and Socially Disadvantaged Subgroups
A peer-led, medical self-management program intervention has been beneficial for medically and socially disadvantaged subgroups [60]. The Reclaiming Joy Peer Support intervention has the potential for increasing QOL and reducing depression in low-income older adults who have physical health conditions [60]. Similarly, for those who are “hardly reached,” it was indicated that the PSS provided is even more effective in these marginalized populations [66]. A Health and Recovery Peer program was delivered by mental health peer leaders for people with SMIs, resulting in an improvement in the physical health–related QOL parameters such as physical activity and medication adherence [49]. Peer-delivered and technology-supported interventions are feasible and acceptable and are associated with improvements in psychiatric, medical self-management skills, QOL, and empowerment of older adults with SMIs and or chronic health conditions [67,68].
Persons With Disabilities
The United Nations’ Convention on the Rights of Persons with Disabilities (CRPD) was adopted in 2007 and stated that “persons with disabilities should have equal recognition before the law and the right to exercise their legal capacity” [69-71]. Therefore, a positive emphasis upon the supported decision making and the fight against discrimination is evident through the convention. Nevertheless, these initiatives have been perceived as incomplete considering many challenges such as the community social status and ongoing perceived stigma of people with disabilities (PWDs) [70,72]. “Circle of support” is an elaborate example of an applicable peer support model for PWDs that has helped in decision making and facilitating communication [70,73,74]. This is clearly aligned with the paradigm shift from the biomedical to the socially supportive model of disability, which was provided by CRPD [70].
Peer Support for Families
Families may act either as sources of understanding and support or stigmatization through ignorance, prejudice, and discrimination, with subsequent negative impact [19]. In addition, the distress and burden associated with caring for a family member with mental illness are evident, where 29% to 60% endure significant psychological distress [17]. Family support can be financial or emotional; however, moral support was perceived as the substantial motivating factor for relatives who are ill [19]. In the last few decades, consistent and growing evidence that supports the inclusion of family members in the treatment and care of their misfortunate relatives has been developed. This has been mainly evident in the youth mental health system that urged the transformation change, which incorporates family members in the health care service provided to their youth [18,75]. Many PSWs have been engaged in family psychoeducation as family peers or parent partners, especially for those with the first episode of psychosis [76]. Although familial education is crucial and needs to be provided through different scales [19], an extensive matching of PSWs and the caregivers has not been perceived as a necessity to create a successful volunteer mentoring relationship [77]. Multiple initiatives have taken place all over the world. In India, a program titled “Saathi” was established for family members of residential and outpatient mental health service users that had dual goals of offering information and developing a peer support mechanism for family members of people with different mental health conditions [19]. In Melbourne, Australia, “Families Helping Families” was developed, where family PSWs are positioned in the service assessment area and in the inpatient unit to ensure early involvement [18]. An impressive peer support guide for parents of children or youth with mental health problems is provided by the Canadian Mental Health Association, British Colombia Division [15]. In Ontario, family matters programs are provided through provincial peer support programs [16].
The term “transforming mental health care” entails active involvement of families in orienting the mental health system toward recovery [78]. Family members are to have access to timely and accurate information that promotes learning, self-monitoring, and accountability [79]. The inclusion of family members as partners of the medical service is the new philosophy, with a subsequent shift from the concept of clinic-based practice to a community-based service approach [78].
Peer Support Service in Low- and Middle-Income Countries
Several initiatives took place in low- and middle-income countries, such as in rural Uganda, where a trained peer-led team provided 12 successful training sessions of perinatal service for a group of parents over a 6-month period, which resulted in better maternal well-being and child development, compared with another control group [80]. Similarly, successful community peer groups were conducted in rural India and Nepal, with high feasibility and effectiveness rates, and perceived as “potential alternative to health-worker-led interventions” [81-83]. In addition, adding counseling and social support groups entailing PSWs to the conventional medication treatment for patients with psychotic disorders was tried in a cohort study in Uganda; however, the results were not significantly different from those who received only medications [84]. This might be because of the underpowering of community services offered, compared with the robust medication regimens [85].
It is evident from the aforementioned information that there is mixed evidence on the effectiveness of PSW interventions in different contexts. For example, for patients with SMIs, systematic reviews suggest that there is some evidence of positive effects on measures of hope, recovery, and empowerment but no positive effects on hospitalization, satisfaction, or overall symptoms [10]. Similarly, for patients with addiction issues, although being involved in a peer network did not reduce social assistance for alcohol, they somewhat increased behavioral and attitudinal support for abstinence as well as involvement with Alcoholics Anonymous [55]. Furthermore, although many observational studies support the PSW role in the other contexts described above, there is a current dearth of literature involving RCTs and systematic reviews reporting on the effectiveness of PSWs in these specific contexts. Thus, there exist opportunities for conducting RCTs in the described contexts.
The Conceptual Framework for the Effects of Peer Support Service
The conceptual framework is based on empirical evidence, suggesting that the impact of PSWs reflects upon the recipients of such a service [4,76,86-90], the global health system [22,47,76,86,91,92], and the PSWs themselves [13,28,76,93], as shown in Figure 1. The framework has, therefore, been developed by authors through a general review of the literature that examines the effects of PSSs on patients, health care systems, and also PSWs themselves so as to provide evidence-based material supporting all possible effects of PSW roles.
Figure 1.
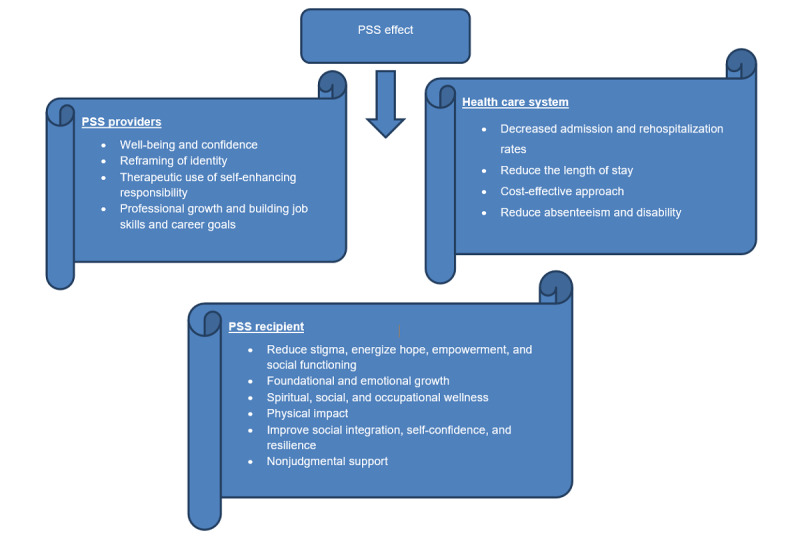
The conceptual framework for the impact of peer support workers in mental health. MH: mental health; PSS: peer support service; PSW: peer support worker.
Supportive social relationships can have a dual opposing effect on individuals’ lives, either as a family member or as social and professional networks through sharing their disappointments and pains or their joy and successes [11]. Useful roles for PSSs are identified in many studies. For example, adding 3 peer specialists to a team of 10 intensive case managers provided better QOL with greater satisfaction [12], stigma reduction, and less health service utilization [89,91]. The economic impact of PSSs has been extensively studied in the literature, concluding cost containment for the health care system in terms of reduction of readmission rates, emergency visits, and fewer hospital stays, which altogether substantially exceed the cost of running a peer support program [92]. Moreover, PSWs are looked at as providers of a service at a cheaper cost compared with other health care providers [94,95]. For example, about US $23,000 is paid to PSWs in the United States compared with around US $100,000 for a nurse practitioner [96]. However, a PSS is not posited as a substitute for clinical services, rather it is perceived as an intrapersonal and social service that provides a dual role of effective service and with humanizing care and support [14,26,97]. This role extends to cover PSWs themselves, in terms of improved overall well-being and self-confidence, reframing identity, and enhancing responsibility either toward themselves or their peers [13,93].
Although PSWs can play a variety of tasks, managers who hire them may want to ensure that improving patient activation is included in their range of duties [48]. In 2 concurrent studies, a significant increase in QOL satisfaction, reduction of rehospitalization rates, and reduction in the number of hospital days were recorded when adding PSSs to usual care [22,98]. In another study engaging 31 peer providers in diverse mental health, agencies identified 5 broad domains of wellness, including foundational, emotional, growth and spiritual, social, and occupational wellness [4]. In a systematic literature review for people with SMIs, peer-navigator interventions and self-management were the most promising interventions [47]. PSWs’ effects are diversified through sharing in different contexts. For example, positive impacts on the physical health of their peers have been recorded [49]. Peer-based approaches have been used to deliver behavioral weight loss interventions [90]. For young students, structured peer support for depression may have benefits in improving students’ mental well-being [64]. In the case of crisis houses, greater satisfaction was achieved through a provided informal PSS [99]. Robust studies, therefore, recommend implementing peer support programs [10,18].
On the other hand, authors found that PSSs met moderate levels of evidence and that effectiveness varied across service types, for example, with “peers in existing clinical roles” was described as being less effective than the “peer staff added to traditional services” and “peer staff delivering structured curricula” [3]. Other reviews suggested that current evidence does not support recommendations or mandatory requirements from policy makers to offer programs for peer support [9,10].
Peer Support Workers’ Satisfaction and Challenges
PSWs experience different problems alongside their diverse job roles, including low pay, stigma, unclear work roles, alienation, struggling with skill deficits, lack of training opportunities, emotional stress in helping others, and, on top of that, maintaining their personal physical and mental health wellness [100,101]. Researchers found that PSWs experience discrimination and prejudice from nonpeer workers, in addition to the encountered difficulties of how to manage the transition from being a patient to a PSW. As a result, high attrition rates were noted among PSWs in mental health settings [102,103]. Peer job satisfaction is strongly dependent on several factors [100,104,105]. Role clarity and psychological empowerment, organizational culture, and working partnership with peers were the most significant predictors of PSW job satisfaction, while professional prejudice was not perceived as a significant predictor [106,107]. Other studies noted that the main problems were experiencing marginalization, lack of understanding, and a sense of exclusion [108-110]. Payment could also contribute to the amount of satisfaction of PSWs [76], as compensation helps through facilitation and engagement motivation [109]. Nevertheless, it seems that not the payment, which ranged from US $10 to US $20 per hour, but the lack of recognition and acknowledgment are the causes for job nonsatisfaction [104].
An interesting literature review grouped these challenges and barriers facing PSWs during fulfilling their assigned roles into 6 main categories: nature of the innovation, individual professional, service user, social context, organizational context, and economic and political contexts [111].
It is evident from the abovementioned information that the PSW role is challenged at multiple levels, including at the personal, societal, and organizational levels. These challenges have a direct bearing on PSW satisfaction, and the successful integration of the PSW role into the health care system depends to a great extent on how these challenges are overcome.
Novel Technology in Peer Support Service (Online and Telephone)
Online support groups are usually conducted through bulletin boards, emails, or live chatting software [28]. Online groups are familiar with people whose illnesses are similar to SMIs or affecting the body shape that have forced them to experience embarrassment and social stigmatization [23,24]. Therefore, they split from the social contexts and redirect toward novel ways of help, such as PSWs and online support groups, and web-based communities provided a suitable medium for people with SMIs by following and learning from their peers on the web, which positively helped them to fight against stigma, instilling hope and gaining insight and empowerment for better health control [25]. Increasingly, social media grew as a target for individuals with SMIs, such as schizophrenia, schizoaffective disorder, or bipolar disorder, seeking advice and supporting each other [112-114]. For someone with SMIs, the decision to reach out and connect with others typically occurs at a time of increased instability or when facing significant life challenges [115]. In a qualitative study, popular social media, such as YouTube, appeared useful for allowing people with SMIs to feel less alone, find hope, support each other, and share personal experiences and coping strategies with day-to-day challenges of living with mental illness through listening and posting comments [114]. Mobile phone–based peer support was found to be a feasible and acceptable way to the youngsters during their pregnancy as well as in the postpartum period [116]. In addition, when coupled with frequent face-to-face meetings with PSWs and with “text for support,” it could be of high value for patients with different mental illnesses [117]. Although online peer networks actively fight against discrimination and stigma, their accessibility to diverse patients’ sectors regarding their income and ethnicity is still questionable [25].
Future of Peer Support Services
Potential new roles, such as community health workers, peer whole health coaches, peer wellness coaches, and peer navigators, have been suggested for such a workforce [76]. They are described as an “ill-defined potential new layer of professionals” [118]. Through an initiative undertaken by SAMHSA via its “Bringing Recovery Supports to Scale Technical Assistance Center Strategy,” a successful identification of abilities and critical knowledge necessarily required for PSWs who provide help and support for those recovering from mental health and substance abuse was noted [76]. At present, peer support is seen as a growing paradigm in many countries, including the United Kingdom, Canada, New Zealand, France, and the Netherlands [103,119]. As an evolving culture, peer support has the opportunity to forge not just mental health system change but social change as well [37]. A novel peer support system termed “Edmonton peer support system” (EPSS) is currently being tested in a randomized controlled pilot trial [117]. In this study, investigators are evaluating the effectiveness of an innovative peer support program that incorporates leadership training, mentorship, recognition, and reward systems for PSWs, coupled with automated daily supportive text messaging, which has proven effectiveness in feasibility trials involving patients with depression and alcohol use disorders [120,121]. Previous studies have examined the effect of PSSs in different contexts, including outpatient departments [122], emergency departments [53,54], community mental health clinics [123,124], and inpatient sites [125]. On the contrary, the EPSS study focuses on patients who have been discharged from acute care hospitals. These patients are being randomized into 1 of the 4 main groups: enrollment in a peer support system, enrollment in a peer support system plus automated daily supportive and reminder text messages, enrollment in automated daily supportive and reminder text messages alone, or treatment as usual follow-up care. The research team hypothesizes that patients who are assigned to a peer support system plus automated daily supportive and reminder text messages will show the best outcome.
Organizations may facilitate peer support through their values, actions, and oversight [119] and through a robust supervision system with available educational access, which could be the adequate path for creating a positive and risk-free environment for PSWs throughout their complex workloads [126]. On the other hand, ethics committees play essential roles in the inclusion of PSWs in applied research studies by avoiding repetition of the work of other trusted agencies and considering the ethical validity of consent procedures for peer support interventions [127].
Discussion
There is an internationally growing trend to adopt PSSs within addiction and mental health services, and despite the ongoing challenges, large sections of the current literature support the inclusion of the PSWs into the mental health care workforce. The literature suggests that the benefits of PSSs impact not only the recipients of mental health services but also extend to the PSWs and the whole health care system. Although the expected benefits of PSSs might be directly measured in terms of service utilization or patient improvement indicators, this could also extend to include wellness and empowerment for PSWs, who may still be fragile, vulnerable, and in need of ongoing acknowledgment and recognition. Thus, the potential for PSSs to be embedded into routine care and the opportunities for the development of innovative models of care for addiction and mental health patients such as the EPSS, which incorporates PSSs and supportive text messaging [117], are evidently a high valued priority. However, the feasibility and maintenance of a robust PSS in health care would only be possible through collaborative efforts and ongoing support and engagement from all health care practitioners, managers, and other stakeholders.
This literature review has several limitations. First, the review is not a systematic review or meta-analysis, and as such, there were no well-defined inclusion or exclusion criteria of studies, which potentially could lead to the exclusion of some essential related studies. Second, the search was conducted in English publications only. Consequently, there is a high probability of missing critical related publications published in non-English languages. Finally, as the review depended mainly on the available literature from the aforementioned sources, which showed marked variability in their design and covered diverse ideas under the central theme, the different weights for each idea throughout the review could be noted.
Acknowledgments
This work was supported by Douglas Harding Trust Fund and Alberta Health Services.
Abbreviations
- CRPD
Convention on the Rights of Persons with Disabilities
- EPSS
Edmonton peer support system
- IPS
intentional peer support
- PSS
peer support service
- PSW
peer support worker
- PWD
people with disability
- QOL
quality of life
- RCT
randomized controlled trial
- SAMHSA
Substance Abuse and Mental Health Services Administration
- SMI
serious mental illness
- TIC
trauma-informed care
Footnotes
Conflicts of Interest: None declared.
References
- 1.Weiner DB. The apprenticeship of Philippe Pinel: a new document, 'observations of Citizen Pussin on the insane'. Am J Psychiatry. 1979 Sep;136(9):1128–34. doi: 10.1176/ajp.136.9.1128. [DOI] [PubMed] [Google Scholar]
- 2.Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, Delphin-Rittmon ME. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. 2014 Apr 1;65(4):429–41. doi: 10.1176/appi.ps.201300244. [DOI] [PubMed] [Google Scholar]
- 3.Penney D. Advocates for Human Potential. 2018. [2019-03-30]. Defining 'Peer Support': Implications for Policy, Practice, and Research https://www.ahpnet.com/AHPNet/media/AHPNetMediaLibrary/White%20Papers/DPenney_Defining_peer_support_2018_Final.pdf.
- 4.Moran GS, Russinova Z, Gidugu V, Yim JY, Sprague C. Benefits and mechanisms of recovery among peer providers with psychiatric illnesses. Qual Health Res. 2012 Mar;22(3):304–19. doi: 10.1177/1049732311420578. [DOI] [PubMed] [Google Scholar]
- 5.Clarke GN, Herinckx HA, Kinney RF, Paulson RI, Cutler DL, Lewis K, Oxman E. Psychiatric hospitalizations, arrests, emergency room visits, and homelessness of clients with serious and persistent mental illness: findings from a randomized trial of two ACT programs vs. usual care. Ment Health Serv Res. 2000 Sep;2(3):155–64. doi: 10.1023/a:1010141826867. [DOI] [PubMed] [Google Scholar]
- 6.Davidson L, Shahar G, Stayner DA, Chinman MJ, Rakfeldt J, Tebes JK. Supported socialization for people with psychiatric disabilities: lessons from a randomized controlled trial. J Commun Psychol. 2004;32(4):453–77. doi: 10.1002/jcop.20013. [DOI] [Google Scholar]
- 7.O'Donnell M, Parker G, Proberts M, Matthews R, Fisher D, Johnson B, Hadzi-Pavlovic D. A study of client-focused case management and consumer advocacy: the Community and Consumer Service Project. Aust N Z J Psychiatry. 1999 Oct;33(5):684–93. doi: 10.1080/j.1440-1614.1999.00629.x. [DOI] [PubMed] [Google Scholar]
- 8.Solomon P, Draine J. The efficacy of a consumer case management team: 2-year outcomes of a randomized trial. J Ment Health Adm. 1995;22(2):135–46. doi: 10.1007/bf02518754. [DOI] [PubMed] [Google Scholar]
- 9.Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, Berends L. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013 Mar 28;(3):CD004807. doi: 10.1002/14651858.CD004807.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, Johnson S, Kendall T. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014 Feb 14;14:39. doi: 10.1186/1471-244X-14-39. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-14-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davidson L, Tondora J, Staeheli M, Martha C, Maria F, Jennifer M, Chinman M. Recovery guides: an emerging model of community-based care for adults with psychiatric disabilities. In: Lightburn A, Sessions P, editors. Handbook Of Community-based Clinical Practice. London: Oxford University Press; 2005. pp. 476–501. [Google Scholar]
- 12.Felton CJ, Stastny P, Shern DL, Blanch A, Donahue SA, Knight E, Brown C. Consumers as peer specialists on intensive case management teams: impact on client outcomes. Psychiatr Serv. 1995 Oct;46(10):1037–44. doi: 10.1176/ps.46.10.1037. [DOI] [PubMed] [Google Scholar]
- 13.Beales A, Wilson J. Peer support – the what, why, who, how and now. J Ment Health Train Educ Prac. 2015;10(5):314–24. doi: 10.1108/JMHTEP-03-2015-0013. [DOI] [Google Scholar]
- 14.MacNeil C, Mead S. A narrative approach to developing standards for trauma-informed peer support. Am J Eval. 2016;26(2):231–44. doi: 10.1177/1098214005275633. [DOI] [Google Scholar]
- 15.Canadian Mental Health Association. Canadian Mental Health Association, BC Division; 2007. [2020-02-29]. Peer Support Guide: For Parents of Children or Youth with Mental Health Problems https://cmha.bc.ca/wp-content/uploads/2016/07/ParentPeerSupportGuide.pdf. [Google Scholar]
- 16.Mood Disorders Association of Ontario. [2020-02-29]. Family Matters Peer Support and Recovery Program https://www.mooddisorders.ca/family-matters-programs.
- 17.Quinn J, Barrowclough C, Tarrier N. The Family Questionnaire (FQ): a scale for measuring symptom appraisal in relatives of schizophrenic patients. Acta Psychiatr Scand. 2003 Oct;108(4):290–6. doi: 10.1034/j.1600-0447.2003.00156.x. [DOI] [PubMed] [Google Scholar]
- 18.Leggatt M, Woodhead G. Family peer support work in an early intervention youth mental health service. Early Interv Psychiatry. 2016 Oct;10(5):446–51. doi: 10.1111/eip.12257. [DOI] [PubMed] [Google Scholar]
- 19.Mahomed F, Stein MA, Chauhan A, Pathare S. 'They love me, but they don't understand me': Family support and stigmatisation of mental health service users in Gujarat, India. Int J Soc Psychiatry. 2019 Feb;65(1):73–9. doi: 10.1177/0020764018816344. [DOI] [PubMed] [Google Scholar]
- 20.Davidson L, Rowe M. The Family-Run Executive Director Leadership Association (FREDLA) 5600 Fishers Ln, Rockville, MD 20857: The CMHS National GAINS Center; 2008. May, [2020-03-01]. Peer Support within Criminal Justice Settings: The Role of Forensic Peer Specialists https://fredla.org/wp-content/uploads/2016/01/davidsonrowe_peersupport1.pdf. [Google Scholar]
- 21.Short R, Woods-Nyce K, Cross SL, Hurst MA, Gordish L, Raia J. The impact of forensic peer support specialists on risk reduction and discharge readiness in a psychiatric facility: A five-year perspective. Int J Psychosoc Rehabil. 2012;16(2):3–10. http://wacodtx.org/wp-content/uploads/2016/09/Clifford-Thurston-1-of-10.pdf. [Google Scholar]
- 22.Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry. 2012 Jun;11(2):123–8. doi: 10.1016/j.wpsyc.2012.05.009. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1723-8617&date=2012&volume=11&issue=2&spage=123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berger M, Wagner TH, Baker LC. Internet use and stigmatized illness. Soc Sci Med. 2005 Oct;61(8):1821–7. doi: 10.1016/j.socscimed.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 24.Highton-Williamson E, Priebe S, Giacco D. Online social networking in people with psychosis: a systematic review. Int J Soc Psychiatry. 2015 Feb;61(1):92–101. doi: 10.1177/0020764014556392. [DOI] [PubMed] [Google Scholar]
- 25.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci. 2016 Apr;25(2):113–22. doi: 10.1017/S2045796015001067. http://europepmc.org/abstract/MED/26744309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J. 2001;25(2):134–41. doi: 10.1037/h0095032. [DOI] [PubMed] [Google Scholar]
- 27.Mental Health Foundation. [2020-02-29]. Peer Support https://www.mentalhealth.org.uk/a-to-z/p/peer-support.
- 28.Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. 2004;27(4):392–401. doi: 10.2975/27.2004.392.401. [DOI] [PubMed] [Google Scholar]
- 29.Davidson L, Chinman M, Sells D, Rowe M. Peer support among adults with serious mental illness: a report from the field. Schizophr Bull. 2006 Jul;32(3):443–50. doi: 10.1093/schbul/sbj043. http://europepmc.org/abstract/MED/16461576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mead S. Intentional Peer Support: An Alternative Approach. West Chesterfield, NH: Intentional Peer Support; 2014. [Google Scholar]
- 31.Sunderland K, Mishkin W, Peer Leadership Group. Mental Health Commission of Canada Mental Health Commission of Canada. 2013. [2020-02-29]. Guidelines for the Practice and Training of Peer Support https://www.mentalhealthcommission.ca/sites/default/files/peer_support_guidelines.pdf.pdf.
- 32.Peterson D. A Mad People’s History of Madness. Pittsburgh, PA: University Of Pittsburgh Press; 1981. [Google Scholar]
- 33.Shaw C. Together: A leading UK mental health charity. 2014. [2020-02-28]. Peer Support in Secure Services: Final Report https://www.together-uk.org/wp-content/uploads/downloads/2014/11/Peer-Support-in-Secure-Settings-Final-Report-4-Nov-14.pdf.
- 34.Mead S. Defining Peer Support. 2003. Mar, [2020-02-29]. http://164.156.7.185/parecovery/documents/DefiningPeerSupport_Mead.pdf.
- 35.Ostrow L, Steinwachs D, Leaf PJ, Naeger S. Medicaid reimbursement of mental health peer-run organizations: results of a national survey. Adm Policy Ment Health. 2017 Jul;44(4):501–11. doi: 10.1007/s10488-015-0675-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stratford AC, Halpin M, Phillips K, Skerritt F, Beales A, Cheng V, Hammond M, O'Hagan M, Loreto C, Tiengtom K, Kobe B, Harrington S, Fisher D, Davidson L. The growth of peer support: an international charter. J Ment Health. 2019 Dec;28(6):627–32. doi: 10.1080/09638237.2017.1340593. [DOI] [PubMed] [Google Scholar]
- 37.Mead S. Google Docs. PO Box 259, West Chesterfield, NH 03466: Intentional Peer Support; 2001. [2020-02-28]. Peer Support as a Socio-Political Response to Trauma and Abuse https://docs.google.com/document/d/1trJ35i4dXX5AIWRnbg78OaT7-RfPE9_DbPm5kSST9_Q/edit. [Google Scholar]
- 38.Wilson AM, Hutchinson M, Hurley J. Literature review of trauma-informed care: implications for mental health nurses working in acute inpatient settings in Australia. Int J Ment Health Nurs. 2017 Aug;26(4):326–43. doi: 10.1111/inm.12344. [DOI] [PubMed] [Google Scholar]
- 39.Goetz SB, Taylor-Trujillo A. A change in culture: violence prevention in an acute behavioral health setting. J Am Psychiatr Nurses Assoc. 2012;18(2):96–103. doi: 10.1177/1078390312439469. [DOI] [PubMed] [Google Scholar]
- 40.Ashmore TR. Massey University. 2013. [2020-02-29]. The Implementation of Trauma Informed Care in Acute Mental Health Inpatient Units: A Comparative Study https://mro.massey.ac.nz/bitstream/handle/10179/5855/02_whole.pdf.
- 41.Brown VB, Harris M, Fallot R. Moving toward trauma-informed practice in addiction treatment: a collaborative model of agency assessment. J Psychoactive Drugs. 2013;45(5):386–93. doi: 10.1080/02791072.2013.844381. [DOI] [PubMed] [Google Scholar]
- 42.Guay S, Tremblay N, Goncalves J, Bilodeau H, Geoffrion S. Effects of a peer support programme for youth social services employees experiencing potentially traumatic events: a protocol for a prospective cohort study. BMJ Open. 2017 Jun 24;7(6):e014405. doi: 10.1136/bmjopen-2016-014405. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28647721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gillard SG, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res. 2013 May 24;13:188. doi: 10.1186/1472-6963-13-188. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-13-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tookey P, Mason K, Broad J, Behm M, Bondy L, Powis J. From client to co-worker: a case study of the transition to peer work within a multi-disciplinary hepatitis c treatment team in Toronto, Canada. Harm Reduct J. 2018 Aug 14;15(1):41. doi: 10.1186/s12954-018-0245-7. https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-018-0245-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stastny P, Brown C. [Peer specialist: origins, pitfalls and worldwide dissemination] Vertex. 2013;24(112):455–9. [PubMed] [Google Scholar]
- 46.Simpson A, Oster C, Muir-Cochrane E. Liminality in the occupational identity of mental health peer support workers: a qualitative study. Int J Ment Health Nurs. 2018 Apr;27(2):662–71. doi: 10.1111/inm.12351. http://europepmc.org/abstract/MED/28548455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cabassa LJ, Camacho D, Vélez-Grau CM, Stefancic A. Peer-based health interventions for people with serious mental illness: a systematic literature review. J Psychiatr Res. 2017 Jan;84:80–9. doi: 10.1016/j.jpsychires.2016.09.021. [DOI] [PubMed] [Google Scholar]
- 48.Chinman M, Oberman RS, Hanusa BH, Cohen AN, Salyers MP, Twamley EW, Young AS. A cluster randomized trial of adding peer specialists to intensive case management teams in the Veterans Health Administration. J Behav Health Serv Res. 2015 Jan;42(1):109–21. doi: 10.1007/s11414-013-9343-1. http://europepmc.org/abstract/MED/23657754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Druss BG, Zhao L, von Esenwein SA, Bona JR, Fricks L, Jenkins-Tucker S, Sterling E, Diclemente R, Lorig K. The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr Res. 2010 May;118(1-3):264–70. doi: 10.1016/j.schres.2010.01.026. http://europepmc.org/abstract/MED/20185272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chien W, Clifton AV, Zhao S, Lui S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst Rev. 2019 Apr 4;4:CD010880. doi: 10.1002/14651858.CD010880.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Salim O, Delphin-Rittmon ME. Peer recovery support for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. 2014 Jul;65(7):853–61. doi: 10.1176/appi.ps.201400047. [DOI] [PubMed] [Google Scholar]
- 52.Best DW, Lubman DI. The recovery paradigm - a model of hope and change for alcohol and drug addiction. Aust Fam Physician. 2012 Aug;41(8):593–7. [PubMed] [Google Scholar]
- 53.Watson DP, Brucker K, McGuire A, Snow-Hill NL, Xu H, Cohen A, Campbell M, Robison L, Sightes E, Buhner R, O'Donnell D, Kline JA. Replication of an emergency department-based recovery coaching intervention and pilot testing of pragmatic trial protocols within the context of Indiana's Opioid State Targeted Response plan. J Subst Abuse Treat. 2020 Jan;108:88–94. doi: 10.1016/j.jsat.2019.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McGuire AB, Powell KG, Treitler PC, Wagner KD, Smith KP, Cooperman N, Robinson L, Carter J, Ray B, Watson DP. Emergency department-based peer support for opioid use disorder: emergent functions and forms. J Subst Abuse Treat. 2020 Jan;108:82–7. doi: 10.1016/j.jsat.2019.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Litt MD, Kadden RM, Kabela-Cormier E, Petry N. Changing network support for drinking: initial findings from the network support project. J Consult Clin Psychol. 2007 Aug;75(4):542–55. doi: 10.1037/0022-006X.75.4.542. [DOI] [PubMed] [Google Scholar]
- 56.Barrenger SL, Hamovitch EK, Rothman MR. Enacting lived experiences: peer specialists with criminal justice histories. Psychiatr Rehabil J. 2019 Mar;42(1):9–16. doi: 10.1037/prj0000327. [DOI] [PubMed] [Google Scholar]
- 57.Angell B, Matthews E, Barrenger S, Watson AC, Draine J. Engagement processes in model programs for community reentry from prison for people with serious mental illness. Int J Law Psychiatry. 2014;37(5):490–500. doi: 10.1016/j.ijlp.2014.02.022. http://europepmc.org/abstract/MED/24650496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thomas K, Wilson JL, Bedell P, Morse DS. 'They didn't give up on me': a women's transitions clinic from the perspective of re-entering women. Addict Sci Clin Pract. 2019 Apr 2;14(1):12. doi: 10.1186/s13722-019-0142-8. https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-019-0142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim SH. [Effects of a volunteer-run peer support program on health and satisfaction with social support of older adults living alone] J Korean Acad Nurs. 2012 Aug;42(4):525–36. doi: 10.4040/jkan.2012.42.4.525. [DOI] [PubMed] [Google Scholar]
- 60.Chapin RK, Sergeant JF, Landry S, Leedahl SN, Rachlin R, Koenig T, Graham A. Reclaiming joy: pilot evaluation of a mental health peer support program for older adults who receive Medicaid. Gerontologist. 2013 Apr;53(2):345–52. doi: 10.1093/geront/gns120. [DOI] [PubMed] [Google Scholar]
- 61.Ahmed SM, Palermo AS. Community engagement in research: frameworks for education and peer review. Am J Public Health. 2010 Aug;100(8):1380–7. doi: 10.2105/AJPH.2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Student Minds. 2014. [2020-02-29]. Grand Challenges in Student Mental Health https://www.studentminds.org.uk/uploads/3/7/8/4/3784584/grand_challenges_report_for_public.pdf.
- 63.Davies EB, Wardlaw J, Morriss R, Glazebrook C. An experimental study exploring the impact of vignette gender on the quality of university students' mental health first aid for peers with symptoms of depression. BMC Public Health. 2016 Feb 25;16:187. doi: 10.1186/s12889-016-2887-2. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-2887-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Byrom N. An evaluation of a peer support intervention for student mental health. J Ment Health. 2018 Jun;27(3):240–6. doi: 10.1080/09638237.2018.1437605. [DOI] [PubMed] [Google Scholar]
- 65.Lubman DI, Cheetham A, Jorm AF, Berridge BJ, Wilson C, Blee F, Mckay-Brown L, Allen N, Proimos J. Australian adolescents' beliefs and help-seeking intentions towards peers experiencing symptoms of depression and alcohol misuse. BMC Public Health. 2017 Aug 16;17(1):658. doi: 10.1186/s12889-017-4655-3. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sokol R, Fisher E. Peer support for the hardly reached: a systematic review. Am J Public Health. 2016 Jul;106(7):e1–8. doi: 10.2105/AJPH.2016.303180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fortuna KL, DiMilia PR, Lohman MC, Bruce ML, Zubritsky CD, Halaby MR, Walker RM, Brooks JM, Bartels SJ. Feasibility, acceptability, and preliminary effectiveness of a peer-delivered and technology supported self-management intervention for older adults with serious mental illness. Psychiatr Q. 2018 Jun;89(2):293–305. doi: 10.1007/s11126-017-9534-7. http://europepmc.org/abstract/MED/28948424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Whiteman KL, Naslund JA, DiNapoli EA, Bruce ML, Bartels SJ. Systematic review of integrated general medical and psychiatric self-management interventions for adults with serious mental illness. Psychiatr Serv. 2016 Nov 1;67(11):1213–25. doi: 10.1176/appi.ps.201500521. http://europepmc.org/abstract/MED/27301767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pathare S, Shields LS. Supported decision-making for persons with mental illness: a review. Pub Health Rev. 2012;34(15) doi: 10.1007/bf03391683. [DOI] [Google Scholar]
- 70.Mahomed F, Stein MA, Patel V. Involuntary mental health treatment in the era of the United Nations Convention on the Rights of Persons with Disabilities. PLoS Med. 2018 Oct;15(10):e1002679. doi: 10.1371/journal.pmed.1002679. http://dx.plos.org/10.1371/journal.pmed.1002679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morrissey F. The United Nations Convention on the Rights of Persons with Disabilities: a new approach to decision-making in mental health law. Eur J Health Law. 2012 Dec;19(5):423–40. doi: 10.1163/15718093-12341237. [DOI] [PubMed] [Google Scholar]
- 72.Szmukler G. 'Capacity', 'best interests', 'will and preferences' and the UN Convention on the Rights of Persons with Disabilities. World Psychiatry. 2019 Feb;18(1):34–41. doi: 10.1002/wps.20584. doi: 10.1002/wps.20584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jeste DV, Eglit GM, Palmer BW, Martinis JG, Blanck P, Saks ER. Supported decision making in serious mental illness. Psychiatry. 2018;81(1):28–40. doi: 10.1080/00332747.2017.1324697. http://europepmc.org/abstract/MED/29494793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Craigie J. A fine balance: reconsidering patient autonomy in light of the UN convention on the rights of persons with disabilities. Bioethics. 2015 Jul;29(6):398–405. doi: 10.1111/bioe.12133. [DOI] [PubMed] [Google Scholar]
- 75.Henderson JL, Cheung A, Cleverley K, Chaim G, Moretti ME, de Oliveira C, Hawke LD, Willan AR, O'Brien D, Heffernan O, Herzog T, Courey L, McDonald H, Grant E, Szatmari P. Integrated collaborative care teams to enhance service delivery to youth with mental health and substance use challenges: protocol for a pragmatic randomised controlled trial. BMJ Open. 2017 Feb 6;7(2):e014080. doi: 10.1136/bmjopen-2016-014080. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=28167747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gagne CA, Finch WL, Myrick KJ, Davis LM. Peer workers in the behavioral and integrated health workforce: opportunities and future directions. Am J Prev Med. 2018 Jun;54(6 Suppl 3):S258–66. doi: 10.1016/j.amepre.2018.03.010. https://linkinghub.elsevier.com/retrieve/pii/S0749-3797(18)31637-4. [DOI] [PubMed] [Google Scholar]
- 77.Smith R, Greenwood N. The impact of volunteer mentoring schemes on carers of people with dementia and volunteer mentors: a systematic review. Am J Alzheimers Dis Other Demen. 2014 Feb;29(1):8–17. doi: 10.1177/1533317513505135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Huang L, Stroul B, Friedman R, Mrazek P, Friesen B, Pires S, Mayberg S. Transforming mental health care for children and their families. Am Psychol. 2005 Sep;60(6):615–27. doi: 10.1037/0003-066X.60.6.615. [DOI] [PubMed] [Google Scholar]
- 79.Hogan MF. The President's New Freedom Commission: recommendations to transform mental health care in America. Psychiatr Serv. 2003 Nov;54(11):1467–74. doi: 10.1176/appi.ps.54.11.1467. [DOI] [PubMed] [Google Scholar]
- 80.Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: a community-based, cluster randomised trial. Lancet Glob Health. 2015 Aug;3(8):e458–69. doi: 10.1016/S2214-109X(15)00099-6. https://linkinghub.elsevier.com/retrieve/pii/S2214-109X(15)00099-6. [DOI] [PubMed] [Google Scholar]
- 81.Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, Tamang S, Thapa S, Shrestha D, Thapa B, Shrestha JR, Wade A, Borghi J, Standing H, Manandhar M, Costello AM, Members of the MIRA Makwanpur trial team Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet. 2004;364(9438):970–9. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 82.Balaji M, Andrews T, Andrew G, Patel V. The acceptability, feasibility, and effectiveness of a population-based intervention to promote youth health: an exploratory study in Goa, India. J Adolesc Health. 2011 May;48(5):453–60. doi: 10.1016/j.jadohealth.2010.07.029. http://europepmc.org/abstract/MED/21501803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tripathy. Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, Rath S, Gope R, Mahto D, Sinha R, Lakshminarayana R, Patel V, Pagel C, Prost A, Costello A. Effect of a participatory intervention with women's groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010 Apr 3;375(9721):1182–92. doi: 10.1016/S0140-6736(09)62042-0. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(09)62042-0. [DOI] [PubMed] [Google Scholar]
- 84.Jordans MJ, Aldridge L, Luitel NP, Baingana F, Kohrt BA. Evaluation of outcomes for psychosis and epilepsy treatment delivered by primary health care workers in Nepal: a cohort study. Int J Ment Health Syst. 2017;11:70. doi: 10.1186/s13033-017-0177-8. https://ijmhs.biomedcentral.com/articles/10.1186/s13033-017-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kohrt B, Asher L, Bhardwaj A, Fazel M, Jordans M, Mutamba B, Nadkarni A, Pedersen G, Singla D, Patel V. The role of communities in mental health care in low- and middle-income countries: a meta-review of components and competencies. Int J Environ Res Public Health. 2018 Jun 16;15(6):pii: E1279. doi: 10.3390/ijerph15061279. http://www.mdpi.com/resolver?pii=ijerph15061279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Arnold I. Workplace Strategies for Mental Health. 2005. [2020-02-29]. Peer Support Programs https://www.workplacestrategiesformentalhealth.com/job-specific-strategies/peer-support-programs.
- 87.Bartels SJ, DiMilia PR, Fortuna KL, Naslund JA. Integrated care for older adults with serious mental illness and medical comorbidity: evidence-based models and future research directions. Psychiatr Clin North Am. 2018 Mar;41(1):153–64. doi: 10.1016/j.psc.2017.10.012. http://europepmc.org/abstract/MED/29412843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bates A, Kemp V, Isaac M. Peer support shows promise in helping persons living with mental illness address their physical health needs. Can J Commun Ment Health. 2008;27(2):21–36. doi: 10.7870/cjcmh-2008-0015. [DOI] [Google Scholar]
- 89.Hardy S, Hallett N, Chaplin E. Evaluating a peer support model of community wellbeing for mental health: a coproduction approach to evaluation. Ment Health Prev. 2019;13(7):149–58. doi: 10.1016/j.mhp.2019.01.007. http://journal.waocp.org/?sid=Entrez:PubMed&id=pmid:22126570&key=2011.12.7.1807. [DOI] [Google Scholar]
- 90.Cabassa LJ, Stefancic A, O'Hara K, El-Bassel N, Lewis-Fernández R, Luchsinger JA, Gates L, Younge R, Wall M, Weinstein L, Palinkas LA. Peer-led healthy lifestyle program in supportive housing: study protocol for a randomized controlled trial. Trials. 2015 Sep 2;16:388. doi: 10.1186/s13063-015-0902-z. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-015-0902-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health. 2011 Aug;20(4):392–411. doi: 10.3109/09638237.2011.583947. [DOI] [PubMed] [Google Scholar]
- 92.Fisher EB, Coufal MM, Parada H, Robinette JB, Tang PY, Urlaub DM, Castillo C, Guzman-Corrales LM, Hino S, Hunter J, Katz AW, Symes YR, Worley HP, Xu C. Peer support in health care and prevention: cultural, organizational, and dissemination issues. Annu Rev Public Health. 2014;35:363–83. doi: 10.1146/annurev-publhealth-032013-182450. [DOI] [PubMed] [Google Scholar]
- 93.MacLellan J, Surey J, Abubakar I, Stagg HR. Peer support workers in health: a qualitative metasynthesis of their experiences. PLoS One. 2015;10(10):e0141122. doi: 10.1371/journal.pone.0141122. http://dx.plos.org/10.1371/journal.pone.0141122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fisher EB, Boothroyd RI, Coufal MM, Baumann LC, Mbanya JC, Rotheram-Borus MJ, Sanguanprasit B, Tanasugarn C. Peer support for self-management of diabetes improved outcomes in international settings. Health Aff (Millwood) 2012 Jan;31(1):130–9. doi: 10.1377/hlthaff.2011.0914. http://europepmc.org/abstract/MED/22232103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Singh P, Chokshi DA. Community health workers--a local solution to a global problem. N Engl J Med. 2013 Sep 5;369(10):894–6. doi: 10.1056/NEJMp1305636. [DOI] [PubMed] [Google Scholar]
- 96.Kangovi S, Long JA, Emanuel E. Community health workers combat readmission. Arch Intern Med. 2012 Dec 10;172(22):1756–7. doi: 10.1001/2013.jamainternmed.82. [DOI] [PubMed] [Google Scholar]
- 97.Fisher EB, Ayala GX, Ibarra L, Cherrington AL, Elder JP, Tang TS, Heisler M, Safford MM, Simmons D, Peers for Progress Investigator Group Contributions of peer support to health, health care, and prevention: papers from peers for progress. Ann Fam Med. 2015 Aug;13(Suppl 1):S2–8. doi: 10.1370/afm.1852. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=26304968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tondora J, O'Connell M, Miller R, Dinzeo T, Bellamy C, Andres-Hyman R, Davidson L. A clinical trial of peer-based culturally responsive person-centered care for psychosis for African Americans and Latinos. Clin Trials. 2010 Aug;7(4):368–79. doi: 10.1177/1740774510369847. http://europepmc.org/abstract/MED/20571133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sweeney A, Fahmy S, Nolan F, Morant N, Fox Z, Lloyd-Evans B, Osborn D, Burgess E, Gilburt H, McCabe R, Slade M, Johnson S. The relationship between therapeutic alliance and service user satisfaction in mental health inpatient wards and crisis house alternatives: a cross-sectional study. PLoS One. 2014;9(7):e100153. doi: 10.1371/journal.pone.0100153. http://dx.plos.org/10.1371/journal.pone.0100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mancini MA. An exploration of factors that effect the implementation of peer support services in community mental health settings. Community Ment Health J. 2018 Feb;54(2):127–37. doi: 10.1007/s10597-017-0145-4. [DOI] [PubMed] [Google Scholar]
- 101.Ahmed AO, Hunter KM, Mabe AP, Tucker SJ, Buckley PF. The professional experiences of peer specialists in the Georgia Mental Health Consumer Network. Community Ment Health J. 2015 May;51(4):424–36. doi: 10.1007/s10597-015-9854-8. [DOI] [PubMed] [Google Scholar]
- 102.Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J. 2013 Mar;36(1):28–34. doi: 10.1037/h0094744. [DOI] [PubMed] [Google Scholar]
- 103.Villani M, Kovess-Masféty V. [Peer support programs in mental health in France: Status report and challenges] Encephale. 2018 Nov;44(5):457–64. doi: 10.1016/j.encep.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 104.Cronise R, Teixeira C, Rogers ES, Harrington S. The peer support workforce: results of a national survey. Psychiatr Rehabil J. 2016 Sep;39(3):211–21. doi: 10.1037/prj0000222. [DOI] [PubMed] [Google Scholar]
- 105.Corrigan PW, Kosyluk KA, Rüsch N. Reducing self-stigma by coming out proud. Am J Public Health. 2013 May;103(5):794–800. doi: 10.2105/AJPH.2012.301037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Davis JK. Predictors of job satisfaction among peer providers on professional treatment teams in community-based agencies. Psychiatr Serv. 2013 Feb 1;64(2):181–4. doi: 10.1176/appi.ps.001452012. [DOI] [PubMed] [Google Scholar]
- 107.Clossey L, Solomon P, Hu C, Gillen J, Zinn M. Predicting job satisfaction of mental health peer support workers (PSWs) Soc Work Ment Health. 2018;16(6):682–95. doi: 10.1080/15332985.2018.1483463. [DOI] [Google Scholar]
- 108.Kemp V, Henderson AR. Challenges faced by mental health peer support workers: peer support from the peer supporter's point of view. Psychiatr Rehabil J. 2012;35(4):337–40. doi: 10.2975/35.4.2012.337.340. [DOI] [PubMed] [Google Scholar]
- 109.Greer AM, Amlani A, Burmeister C, Scott A, Newman C, Lampkin H, Pauly B, Buxton JA. Peer engagement barriers and enablers: insights from people who use drugs in British Columbia, Canada. Can J Public Health. 2019 Apr;110(2):227–35. doi: 10.17269/s41997-018-0167-x. http://europepmc.org/abstract/MED/30610564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Clossey L, Gillen J, Frankel H, Hernandez J. The experience of certified peer specialists in mental health. Soc Work Ment Health. 2015;14(4):408–27. doi: 10.1080/15332985.2015.1038412. [DOI] [Google Scholar]
- 111.Vandewalle J, Debyser B, Beeckman D, Vandecasteele T, Van Hecke A, Verhaeghe S. Peer workers' perceptions and experiences of barriers to implementation of peer worker roles in mental health services: A literature review. Int J Nurs Stud. 2016 Aug;60:234–50. doi: 10.1016/j.ijnurstu.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 112.Gowen K, Deschaine M, Gruttadara D, Markey D. Young adults with mental health conditions and social networking websites: seeking tools to build community. Psychiatr Rehabil J. 2012;35(3):245–50. doi: 10.2975/35.3.2012.245.250. [DOI] [PubMed] [Google Scholar]
- 113.Miller BJ, Stewart A, Schrimsher J, Peeples D, Buckley PF. How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Res. 2015 Feb 28;225(3):458–63. doi: 10.1016/j.psychres.2014.11.067. [DOI] [PubMed] [Google Scholar]
- 114.Naslund JA, Grande SW, Aschbrenner KA, Elwyn G. Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One. 2014;9(10):e110171. doi: 10.1371/journal.pone.0110171. http://dx.plos.org/10.1371/journal.pone.0110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Perry BL, Pescosolido BA. Social network activation: the role of health discussion partners in recovery from mental illness. Soc Sci Med. 2015 Jan;125:116–28. doi: 10.1016/j.socscimed.2013.12.033. http://europepmc.org/abstract/MED/24525260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chyzzy B, Dennis C. 16. Mobile phone-based peer support in the prevention of postpartum depression among adolescent mothers: a pilot randomized controlled trial. J Adolesc Health. 2019;64(2):S8–9. doi: 10.1016/j.jadohealth.2018.10.030. [DOI] [Google Scholar]
- 117.Urichuk L, Hrabok M, Hay K, Spurvey P, Sosdjan D, Knox M, Fu A, Surood S, Brown R, Coulombe J, Kelland J, Rittenbach K, Snaterse M, Abba-Aji A, Li X, Chue P, Greenshaw AJ, Agyapong VI. Enhancing peer support experience for patients discharged from acute psychiatric care: protocol for a randomised controlled pilot trial. BMJ Open. 2018 Aug 17;8(8):e022433. doi: 10.1136/bmjopen-2018-022433. http://bmjopen.bmj.com/cgi/pmidlookup?view=long&pmid=30121611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hurley J, Cashin A, Mills J, Hutchinson M, Graham I. A critical discussion of Peer Workers: implications for the mental health nursing workforce. J Psychiatr Ment Health Nurs. 2016 Mar;23(2):129–35. doi: 10.1111/jpm.12286. [DOI] [PubMed] [Google Scholar]
- 119.Burke EM, Pyle M, Machin K, Morrison AP. Providing mental health peer support 1: A Delphi study to develop consensus on the essential components, costs, benefits, barriers and facilitators. Int J Soc Psychiatry. 2018;64(8):799–812. doi: 10.1177/0020764018810299. [DOI] [PubMed] [Google Scholar]
- 120.Agyapong VI, Juhás M, Mrklas K, Hrabok M, Omeje J, Gladue I, Kozak J, Leslie M, Chue P, Greenshaw AJ. Randomized controlled pilot trial of supportive text messaging for alcohol use disorder patients. J Subst Abuse Treat. 2018 Nov;94:74–80. doi: 10.1016/j.jsat.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 121.Agyapong VI, Ahern S, McLoughlin DM, Farren CK. Supportive text messaging for depression and comorbid alcohol use disorder: single-blind randomised trial. J Affect Disord. 2012 Dec 10;141(2-3):168–76. doi: 10.1016/j.jad.2012.02.040. [DOI] [PubMed] [Google Scholar]
- 122.Gill K. New Moves: Targeting physical and mental illness well-being in people with mental illness. Health Issues J. 2012;108(1):18–23. doi: 10.13140/2.1.3918.1447. https://www.researchgate.net/publication/264547577_New_Moves_Targeting_physical_and_mental_illness_well-being_in_people_with_mental_illness. [DOI] [Google Scholar]
- 123.Martin M, Martin SL. Healthy Amistad: improving the health of people with severe mental illness. Issues Ment Health Nurs. 2014 Oct;35(10):791–5. doi: 10.3109/01612840.2014.915898. [DOI] [PubMed] [Google Scholar]
- 124.Lorig K, Ritter PL, Pifer C, Werner P. Effectiveness of the chronic disease self-management program for persons with a serious mental illness: a translation study. Community Ment Health J. 2014 Jan;50(1):96–103. doi: 10.1007/s10597-013-9615-5. [DOI] [PubMed] [Google Scholar]
- 125.Bouchard L, Montreuil M, Gros C. Peer support among inpatients in an adult mental health setting. Issues Ment Health Nurs. 2010 Sep;31(9):589–98. doi: 10.3109/01612841003793049. [DOI] [PubMed] [Google Scholar]
- 126.Hurley J, Cashin A, Mills J, Hutchinson M, Kozlowski D, Graham I. Qualitative study of peer workers within the 'Partners in Recovery' programme in regional Australia. Int J Ment Health Nurs. 2018 Feb;27(1):187–95. doi: 10.1111/inm.12308. [DOI] [PubMed] [Google Scholar]
- 127.Simmons D, Bunn C, Nakwagala F, Safford MM, Ayala GX, Riddell M, Graffy J, Fisher EB. Challenges in the ethical review of peer support interventions. Ann Fam Med. 2015 Aug;13(Suppl 1):S79–86. doi: 10.1370/afm.1803. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=26304976. [DOI] [PMC free article] [PubMed] [Google Scholar]


