Abstract
This study uses US national survey data to characterize trends in the prevalence of metabolic syndrome among adults in the US between 2011 and 2016.
Metabolic syndrome is associated with increased risk for cardiovascular disease and all-cause mortality.1,2 A previous study reported a prevalence of 33% in adults, which remained stable from 2007 to 2012.3 Understanding current trends in metabolic syndrome prevalence may help identify patients who would benefit from improved screening and optimization of cardiovascular risk profiles. We provide an updated analysis of metabolic syndrome prevalence through 2016.
Methods
Using National Health and Nutrition Examination Survey (NHANES) data from 2011 to 2016, a cross-sectional, stratified, multistage probability sample of the US population, we evaluated trends in metabolic syndrome prevalence among adults (aged ≥20 years). NHANES was approved by the institutional review board at the National Center for Health Statistics and written consent was obtained from participants. From 2011 to 2016, unweighted response rates ranged from 58.7% to 69.5%. Self-reported race/ethnicity was evaluated to determine race-specific differences. Metabolic syndrome was defined based on the National Cholesterol Education Program’s Adult Treatment Panel III as having at least 3 of the following: waist circumference greater than 102 cm in men or 88 cm in women, triglyceride level greater than 150 mg/dL, high-density lipoprotein cholesterol less than 40 mg/dL in men or less than 50 mg/dL in women, systolic blood pressure at least 130 mm Hg or diastolic blood pressure at least 85 mm Hg or taking hypertension medications, or fasting plasma glucose level at least 100 mg/dL or taking diabetes medications. Weighted data were used to estimate the unadjusted prevalence of metabolic syndrome, stratified by age group (20-39, 40-59, and ≥60 years), sex, and race/ethnicity. Tests for trends were assessed, overall and among subgroups, using logistic regression after regressing metabolic syndrome on year (modeled as a continuous predictor). Between-group comparisons used χ2 tests. Statistical significance was met with 2-tailed P <.05. Statistical analyses were performed with Stata, version 15 (StataCorp).
Results
Among 17 048 participants, the weighted metabolic syndrome prevalence was 34.7% (95% CI, 33.1%-36.3% [n = 5885]). Metabolic syndrome prevalence was not significantly different among men and women (35.1% vs 34.3%; P = .47) and was highest among “other” race/ethnicity (39.0%), followed by Hispanic (36.3%) and non-Hispanic white (36.0%) participants (Table). The increase in the overall crude metabolic syndrome prevalence from 2011-2012 to 2015-2016 did not meet statistical significance (from 32.5% [95% CI, 29.0%-36.2%] in 2011-2012 to 36.9% [95% CI, 33.9%-39.9%] in 2015-2016; P = .07 for trend). Over the study period, metabolic syndrome prevalence increased significantly among those aged 20 to 39 years (from 16.2% to 21.3%; P = .02 for trend), women (from 31.7% to 36.6%; P = .04 for trend), Asian participants (from 19.9% to 26.2%; P = .008 for trend), and Hispanic participants (from 32.9% to 40.4%; P = .01 for trend) (Table).
Table. Prevalence of the Metabolic Syndrome by Sex and Race/Ethnicity.
| Characteristics | Unweighted No. (weighted %) [95% CI] | P value for trend | Total unweighted No. (weighted %) [95% CI] | ||
|---|---|---|---|---|---|
| 2011-2012 | 2013-2014 | 2015-2016 | |||
| Crude metabolic syndrome | 1749 (32.5) [29.0-36.2] | 2004 (34.6) [32.8-36.5] | 2132 (36.9) [33.9-39.9] | .07 | 5885 (34.7) [33.1-36.3] |
| Age category, y | |||||
| 20-39 | 316 (16.2) [13.6-19.2] | 398 (21.0) [18.0-24.3] | 411 (21.3) [18.3-24.7] | .02 | 1125 (19.5) [17.8-[21.4] |
| 40-59 | 655 (38.3) [34.7-42.1] | 737 (38.0) [35.0-41.0] | 766 (42.0) [37.2-47.0] | .23 | 2158 (39.4) [37.2-41.7] |
| ≥60 | 778 (46.6) [41.4-52.0] | 869 (48.5) [45.0-51.9] | 955 (50.4) [45.8-54.9] | .29 | 2602 (48.6) [46.0-51.2] |
| Sex | |||||
| Men | 848 (33.3) [29.3-37.6] | 910 (34.6) [31.5-37.8] | 992 (37.2) [33.2-41.4] | .19 | 2750 (35.1) [32.9-37.3] |
| Women | 901 (31.7) [28.2-35.4] | 1094 (34.6) [32.9-36.4] | 1140 (36.6) [33.6-39.7] | .04 | 3135 (34.3) [32.7-36.0] |
| Race/ethnicity | |||||
| Non-Hispanic white | 709 (33.8) [29.4-38.5] | 922 (36.4) [33.8-39.0] | 712 (37.6) [34.5-40.9] | .18 | 2343 (36.0) [34.0-38.0] |
| Non-Hispanic black | 451 (29.5) [26.2-33.1] | 371 (29.6) [27.3-32.1] | 377 (30.0) [26.8-33.5] | .85 | 1199 (29.7) [28.0-31.5] |
| Non-Hispanic Asian | 152 (19.9) [16.7-23.5] | 157 (22.9) [19.5-26.6] | 168 (26.2) [23.4-29.2] | .007 | 477 (23.2) [21.3-25.1] |
| Hispanica | 396 (32.9) [29.6-36.4] | 500 (35.1) [31.6-38.7] | 787 (40.4) [36.0-44.9] | .01 | 1683 (36.3) [34.0-38.6] |
| Otherb | 41 (33.0) [19.5-50.0] | 54 (33.3) [26.2-41.2] | 88 (47.0) [38.6-55.6] | .11 | 183 (39.0) [33.0-45.3] |
Mexican American or other Hispanic race.
Other non-Hispanic races, including non-Hispanic multiracial.
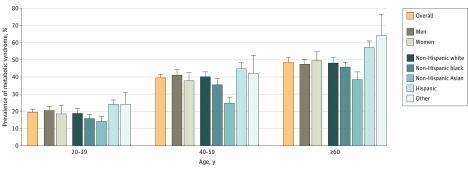
The prevalence of metabolic syndrome significantly increased with increasing age among all subgroups (Figure). Prevalence was 19.5% among those aged 20 to 39 years and increased to 48.6% among those aged at least 60 years. Among each age group, there were no significant differences in metabolic syndrome prevalence between men and women. There were significant differences in prevalence between races/ethnicities among each age group, with the highest prevalence among participants who indicated “other” race/ethnicity who were aged at least 60 years (64.0%), followed by Hispanic participants aged at least 60 years (57.3%).
Figure. Age-Specific Prevalence of Metabolic Syndrome by Sex and Race/Ethnicity, 2011-2016.
Error bars indicate 95% CIs. Hispanic race/ethnicity includes Mexican American or other Hispanic race. Other race/ethnicity includes other non-Hispanic races, including non-Hispanic multiracial. Comparisons of prevalence estimates between age groups among the specified demographic subgroups were performed using χ2 tests. All comparisons yielded P <.001.
Discussion
Although the overall increase in metabolic syndrome prevalence among US adults from 2011-2012 to 2015-2016 did not meet statistical significance, there was a significant increase observed among young adults. Prevalence among those aged 60 years or older remained high.3 The fast-growing prevalence in young adults and Hispanic and Asian individuals is important to note given their increasing population in the US.
With an aging US population and concurrent increases in other chronic conditions and comorbidities,4 increases in the prevalence of metabolic syndrome are concerning. Efforts to implement prevention strategies, including lifestyle modification and use of medications targeted at subgroups at highest risk, may assist in lowering the risk of developing cardiovascular disease.5,6
Limitations inherent in the use of NHANES data, such as nonresponse bias and potential misclassification based on medication use, should be acknowledged. Causal inference could not be drawn due to the cross-sectional nature of the study. No information was available on severity or control of each metabolic syndrome component. Lack of the use of race-specific abdominal obesity cut points may have affected the accuracy of the estimates, particularly for Asian participants. There exists the possibility of insufficient power to detect significant differences between groups or over the study period.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Stepanova M, Rafiq N, Younossi ZM. Components of metabolic syndrome are independent predictors of mortality in patients with chronic liver disease: a population-based study. Gut. 2010;59(10):1410-1415. doi: 10.1136/gut.2010.213553 [DOI] [PubMed] [Google Scholar]
- 2.Isomaa B, Almgren P, Tuomi T, et al. l. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683-689. doi: 10.2337/diacare.24.4.683 [DOI] [PubMed] [Google Scholar]
- 3.Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA. 2015;313(19):1973-1974. doi: 10.1001/jama.2015.4260 [DOI] [PubMed] [Google Scholar]
- 4.Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988-2012. Prev Chronic Dis. 2017;14(3):e24. doi: 10.5888/pcd14.160287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806-814. doi: 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grundy SM, Cleeman JI, Daniels SR, et al. ; American Heart Association; National Heart, Lung, and Blood Institute . Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735-2752. doi: 10.1161/CIRCULATIONAHA.105.169404 [DOI] [PubMed] [Google Scholar]