Background: Although antidepressant therapy has been related to increased cardiovascular risk, depression, and its adverse effects on prognosis, is a well-recognised entity among acute coronary syndrome (ACS) patients. The aim of the study was to evaluate prevalence and outcome of antidepressant treatment in a real-world cohort of ACS patients.
Methods: We sought to assess the prevalence of established antidepressant therapy (ADT) and its impact among 2,168 all-comers patients admitted to four Swiss university hospitals for ACS and enrolled in the prospective multicentre SPUM registry (NCT01000701). The primary endpoint was all-cause mortality. The association between ADT and mortality was tested by adjusted multivariable conditional logistic regression.
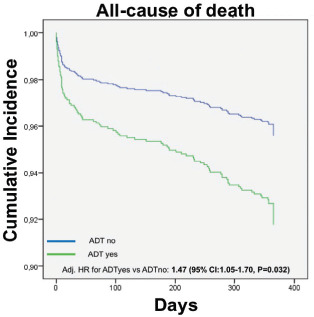
Results: Out of 2,168 ACS patients, 141 patients (6.5%) were on ADT. Compared with the general ACS population, ADT patients were more likely to be unemployed (p=0.001), men (p=0.002), diabetic (p=0.010) and already treated with cardiovascular (CV) preventive therapy with statins or beta-blockers (p<0.001). Patients with ADT had a twofold risk of all-cause mortality (OR 2.2, 95% CI [1.20–4.00[, p=0.009) with a threefold risk of non-CV death (OR 3.24, 95% CI [1.10–9.70], p=0.026) and a 77% not significant higher risk of CV death (OR 1.77, 95% CI [0.83–3.80], p=0.130). This enhanced risk persisted after adjustment for confounding significant baseline characteristics, with a 47% (adjusted HR 1.47, 95% CI [1.05–1.70], p=0.032, Figure 1).
Figure 1.
Conclusion: Among a real-world cohort of ACS patients, ADT is associated with a significantly increased rate of all-cause mortality and non-CV death. These observations should lead clinicians to further individualise ADT, employing newer and safer ADT, generally associated with a lower CV risk.


