Abstract
The Transient Receptor Potential Ankyrin 1 (TRPA1) cation channel expressed on capsaicin-sensitive afferents, immune and endothelial cells is activated by inflammatory mediators and exogenous irritants, e.g., endotoxins, nicotine, crotonaldehyde and acrolein. We investigated its involvement in acute and chronic pulmonary inflammation using Trpa1 gene-deleted (Trpa1−/−) mice. Acute pneumonitis was evoked by intranasal Escherichia coli endotoxin (lipopolysaccharide: LPS) administration, chronic bronchitis by daily cigarette smoke exposure (CSE) for 4 months. Frequency, peak inspiratory/expiratory flows, minute ventilation determined by unrestrained whole-body plethysmography were significantly greater, while tidal volume, inspiratory/expiratory/relaxation times were smaller in Trpa1−/− mice. LPS-induced bronchial hyperreactivity, myeloperoxidase activity, frequency-decrease were significantly greater in Trpa1−/− mice. CSE significantly decreased tidal volume, minute ventilation, peak inspiratory/expiratory flows in wildtypes, but not in Trpa1−/− mice. CSE remarkably increased the mean linear intercept (histopathology), as an emphysema indicator after 2 months in wildtypes, but only after 4 months in Trpa1−/− mice. Semiquantitative histopathological scores were not different between strains in either models. TRPA1 has a complex role in basal airway function regulation and inflammatory mechanisms. It protects against LPS-induced acute pneumonitis and hyperresponsiveness, but is required for CSE-evoked emphysema and respiratory deterioration. Further research is needed to determine TRPA1 as a potential pharmacological target in the lung.
Keywords: bronchitis, cigarette smoke, COPD, emphysema, LPS, pneumonitis, whole body plethysmography
1. Introduction
The Transient Receptor Potential Ankyrin 1 (TRPA1) receptor is the sole member of the “ankyrin” subfamily of the Transient Receptor Potential (TRP) receptors in mammals. It is predominantly expressed on capsaicin-sensitive peptidergic sensory nerves densely innervating the lungs [1,2]. TRPA1 is a large transmembrane protein forming a ligand-gated non-selective cation channel [3,4].
TRPA1 is activated by several exogenous stimuli, such as bacterial endotoxin [5] and environmental irritants like acrolein, crotonaldehyde, nicotine and isocyanates [6,7,8,9,10], found in cigarette smoke, wood smoke, diesel exhaust and tear gas [6,7,10,11,12,13]. Moreover, several endogenous mediators produced during inflammation and oxidative stress, such as lipid peroxidation products, e.g., 4-hydroxynonenal (HNE) and 4-oxo-2-nonenal (4-ONE) [14,15,16], reactive oxygen species (ROS) [17], hydrogen sulfide, bradykinin and prostanoids stimulate TRPA1 [18,19,20,21,22]. Electrophilic compounds activate the receptor by covalently binding to the reactive cysteine residues at the intracellular N-terminal region [23,24,25,26]. Bradykinin and prostaglandins sensitize TRPA1 [22,27] through protein kinase A (PKA)-mediated phosphorylation [28,29]. Moreover, TRPA1 is also involved in protease activated receptor 1 (PAR1)/Gq-mediated increase of the intracellular Ca2+-level [30,31].
Pro-inflammatory sensory neuropeptides, e.g., substance P (SP) and calcitonin gene-related peptide (CGRP) are released in response to TRPA1 activation leading to neurogenic inflammation (vasodilatation and plasma protein extravasation) [32]. Simultaneously with these pro-inflammatory mediators, anti-inflammatory neuropeptides, e.g., somatostatin and pituitary adenylate cyclase activating polypeptide are also released from the same terminals counteracting the inflammatory process [33,34].
TRPA1 is also expressed on several non-neuronal cells [35], e.g., keratinocytes, macrophages and CD4+ lymphocytes [36,37,38], epidermal melanocytes, fibroblasts [39,40], urothelial and endothelial cells, as well as primary human osteoarthritic chondrocytes [41,42,43]. In the airways, TRPA1 is expressed on fibroblasts, tracheal, bronchial and alveolar epithelial cells, bronchial smooth muscle cells (SMC), as well as lymphocytes [17,44,45,46,47,48,49,50].
Due to its polymodal chemosensor function and its wide expression pattern, TRPA1 has been addressed as having a key role in physiological and pathophysiological processes, particularly in neuro-immune interactions [51,52,53]. It is suggested to be a particularly important chemical sensor in the respiratory system, playing a role in physiological (protective reflexes, cough and sneeze) and pathophysiological responses (inflammation, bronchial hyperreactivity) [54,55,56]. Although increasing evidence suggests TRPA1 involvement in the pathogenesis of chronic obstructive pulmonary disease (COPD), asthma, chronic cough, cystic fibrosis etc., pointing to the important therapeutic potential of TRPA1 in the pharmacological treatment of chronic pulmonary diseases [26,46,54,57,58,59,60,61,62], there are few in vivo data concerning its function in airway inflammation. Therefore, the results are far from being conclusive and more information is needed to determine the significance of TRPA1 as a possible pharmacological target in inflammatory lung disease, pneumonitis and COPD.
Therefore, in the present study we investigated the involvement of TRPA1 in the in vivo models of endotoxin (lipopolisaccharide: LPS)-induced acute and cigarette smoke exposure-induced chronic pulmonary inflammation with the help of TRPA1 wildtype (Trpa1+/+) and gene-deficient (Trpa1−/−) mice.
2. Results
2.1. Differences in Basal Airway Function Parameters of Trpa1+/+ and Trpa1−/− Mice
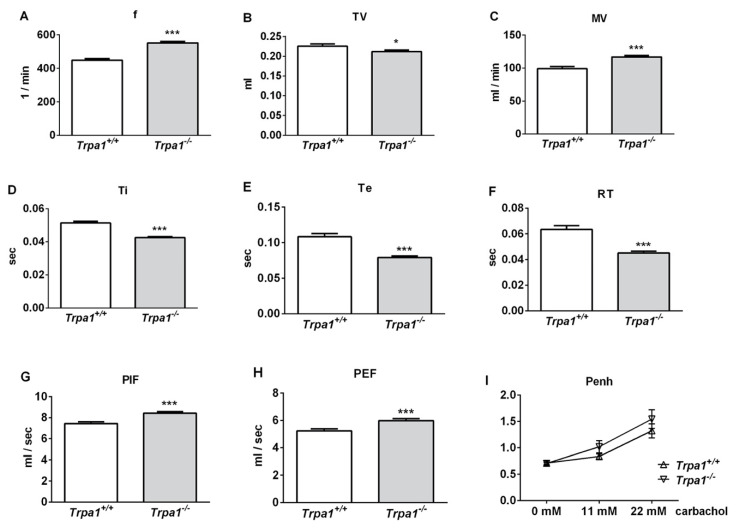
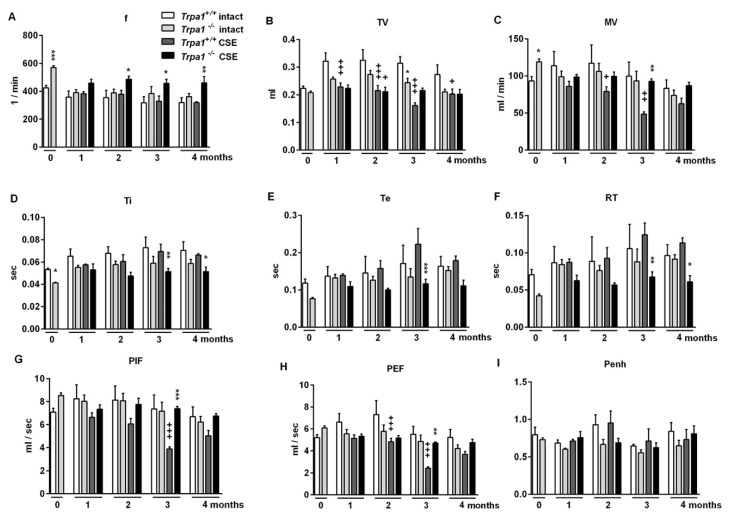
Under intact conditions, frequency (f), minute ventilation (MV), peak inspiratory flow (PIF) and peak expiratory flow (PEF) were significantly greater, tidal volume (TV), inspiratory time (Ti), expiratory time (Te) and relaxation time (RT) were significantly smaller, while no difference was detected in the enhanced pause (Penh) of Trpa1−/− mice compared to their wildtype counterparts, measured by unrestrained whole body plethysmography (WBP) (Figure 1).
Figure 1.
Comparison of the basal airway functions of intact Trpa1+/+ and Trpa1−/− mice measured by unrestrained whole-body plethysmography. (A) Breathing frequency (f), (B) tidal volume (TV), (C) minute ventilation (MV), (D) inspiratory time (Ti), (E) expiratory time (Te), (F) relaxation time (RT), (G) peak inspiratory flow (PIF) and (H) peak expiratory flow (PEF) were measured in conscious, spontaneously breathing mice. (I) Enhanced pause (Penh) correlating with bronchial responsiveness was assessed by the nebulization of the muscarinic receptor agonist, carbachol. Values represent the means ± SEM, n = 30–35 mice/group; Student’s t-test for unpaired comparison; * p < 0.05; *** p < 0.001.
2.2. Endotoxin-Induced Bronchial Hyperreactivity is Greater in Trpa1−/− Mice
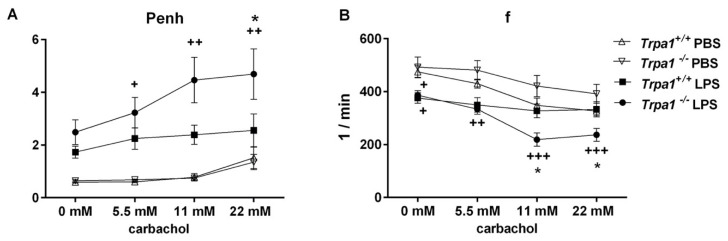
Bronchial responsiveness characterized by the Penh parameter significantly and concentration-dependently elevated in the Trpa1−/− mice in response to increasing concentrations of the muscarinic receptor agonist carbachol 24 h after the administration of intranasal LPS. This indicates the development of inflammatory airway hyperreactivity, which was significantly greater in the TRPA1-deficient mice compared to the LPS-treated wildtypes (Figure 2A).
Figure 2.
Inflammatory airway hyperreactivity: (A) carbachol-induced bronchoconstriction and (B) changes in breathing frequency. Carbachol-evoked bronchoconstriction remarkably increased, and the decrease in breathing frequency was significantly greater in Trpa1−/− mice 24 h after LPS administration, but not in the wildtypes. Values represent the means ± SEM, n = 5–10 mice/group; two-way ANOVA followed by Tukey’s post-test; + p < 0.05, ++ p < 0.005, +++ p < 0.001 vs. PBS-treated respective group; * p < 0.05 vs. LPS-treated Trpa1+/+.
LPS inhalation significantly reduced basal f in both strains. In response to carbachol, f did not change in Trpa1+/+ mice, but it significantly declined in a concentration-dependent manner in the Trpa1−/− ones, being significantly lower compared to the wildtypes at 11 and 22 mM carbachol stimuli (Figure 2B).
Interestingly, the mild, although significant breathing frequency difference between the wildtype and knockout groups found under intact conditions was not observable in this model, most probably because of the different study setting and the use of phosphate buffer saline (PBS) in the control group.
2.3. Endotoxin-Induced Histological Alterations Show No Difference in the Case of TRPA1-Deficiency
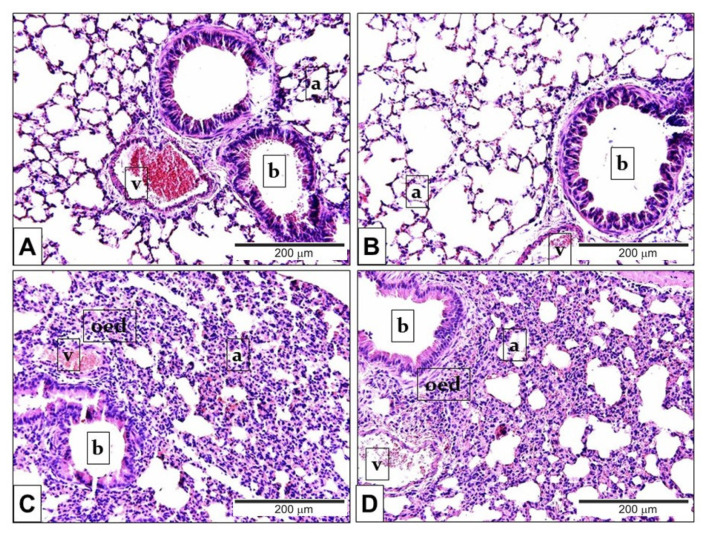
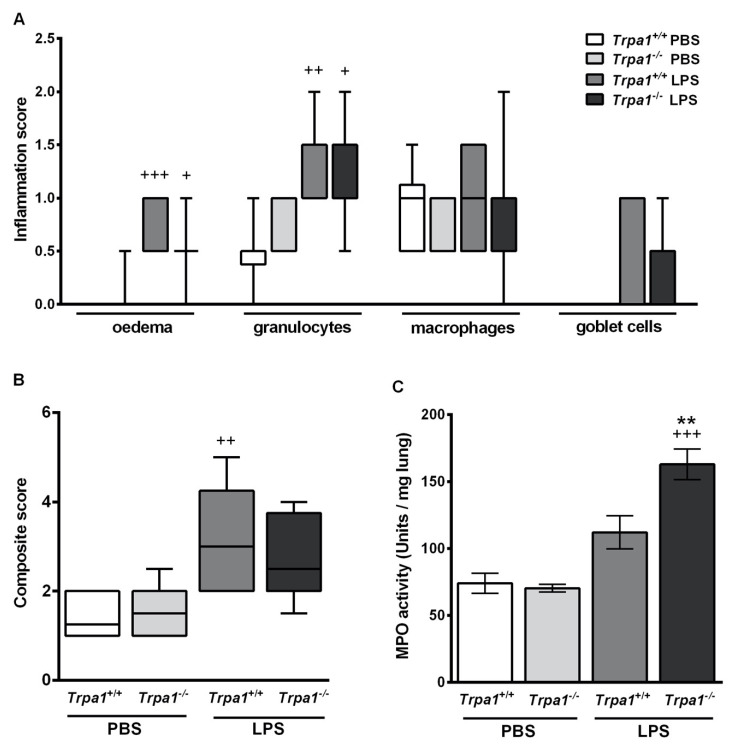
In comparison to the PBS-treated mouse groups (Figure 3A,B) LPS administration induced remarkable oedema formation and inflammatory cell infiltration (Figure 3C,D) in the lung tissue. Based on the semiquantitative histopathological evaluation perivascular/peribronchial oedema and neutrophil granulocyte infiltration (Figure 4A) were significantly higher 24 h after LPS treatment, and the extent of goblet cell hyperplasia also increased, although not significantly. There was no statistical difference in the extent of endotoxin-induced airway inflammation scores between Trpa1+/+ and Trpa1−/− mice (Figure 4A,B).
Figure 3.
Representative histological pictures of LPS-induced pulmonary alterations. Compared to the PBS-treated (A) Trpa1+/+ and (B) Trpa1−/− control groups, the lung tissue of LPS-treated (C) Trpa1+/+ and (D) Trpa1−/− mice exhibited remarkable perivascular and peribronchial oedema, neutrophil granulocyte accumulation, macrophage infiltration and goblet cell hyperplasia (hematoxylin-eosin staining; 200× g magnification; a: alveolus, b: bronchiolus, v: venula, oed: oedema).
Figure 4.
Semiquantitative histopathological evaluation and determination of the myeloperoxidase (MPO) activity of the lung 24 h after LPS inhalation. No significant difference was observed in the (A) detailed and (B) composite scores of histopathological inflammatory parameters between the Trpa1+/+ and Trpa1−/− groups. Boxplots represent the minimum, first quartile, mean, third quartile and maximum values, n = 7–13/group, Kruskal–Wallis followed by Dunn’s post-test; + p < 0.05, ++ p < 0.005, +++ p < 0.001 vs. PBS-treated Trpa1+/+. (C) LPS administration increased myeloperoxidase activity in the lung, which was significantly elevated in Trpa1−/− compared to the wildtypes. Values represent the means ± SEM, n = 5–8 mice/group; one-way ANOVA followed by Bonferroni’s post-test; +++ p < 0.001 vs. PBS-treated respective group; ** p < 0.01 vs. LPS-treated Trpa1+/+.
2.4. Endotoxin-Induced Myeloperoxidase Activity in the Lung is Greater in Trpa1−/− Mice
Myeloperoxidase (MPO) enzyme activity correlating with the activated neutrophil granulocytes and macrophages increased 24 h after LPS-inhalation in both strains, however it was significantly greater in Trpa1−/− mice compared to the wildtypes (Figure 4C).
2.5. Chronic Cigarette Smoke Induces Respiratory Function Alterations in Trpa1+/+, but not in Trpa1−/− Mice
Respiratory functions were measured in a follow-up design before and at the end of each month in the 4-month long protocol of cigarette smoke exposure (CSE). CSE induced a gradual and significant decrease in TV, MV, PIF and PEF in Trpa1+/+ mice with a peak at 3 months, which was not present in the Trpa1−/− animals (Figure 5). The significant differences in f, Ti, Te and RT measured in the Trpa1−/− mice were attributable to the significant differences between the wildtype and gene-deficient mice observed already in the intact animals, before CSE.
Figure 5.
Respiratory functions during the 4 months of cigarette smoke exposure. (B) Tidal volume (TV), (C) minute ventilation (MV), (G) peak inspiratory flow (PIF) and (H) peak expiratory flow (PEF) significantly decreased after CSE with a peak at 3 months in Trpa1+/+ mice. The significant strain differences in (A) frequency, (D) inspiratory time (Ti), (E) expiratory time (Te) and (F) relaxation time (RT) observed already in intact mice were not influenced by CSE. (I) Enhanced pause did not show any differences either by treatment or by strain. Values represent means ± SEM, n = 6–7 mice/group; two-way ANOVA followed by Tukey’s post-test; + p < 0.05, ++ p < 0.005, +++ p < 0.001 vs. PBS-treated respective group; * p < 0.05, ** p < 0.005, *** p < 0.001 vs. LPS-treated Trpa1+/+.
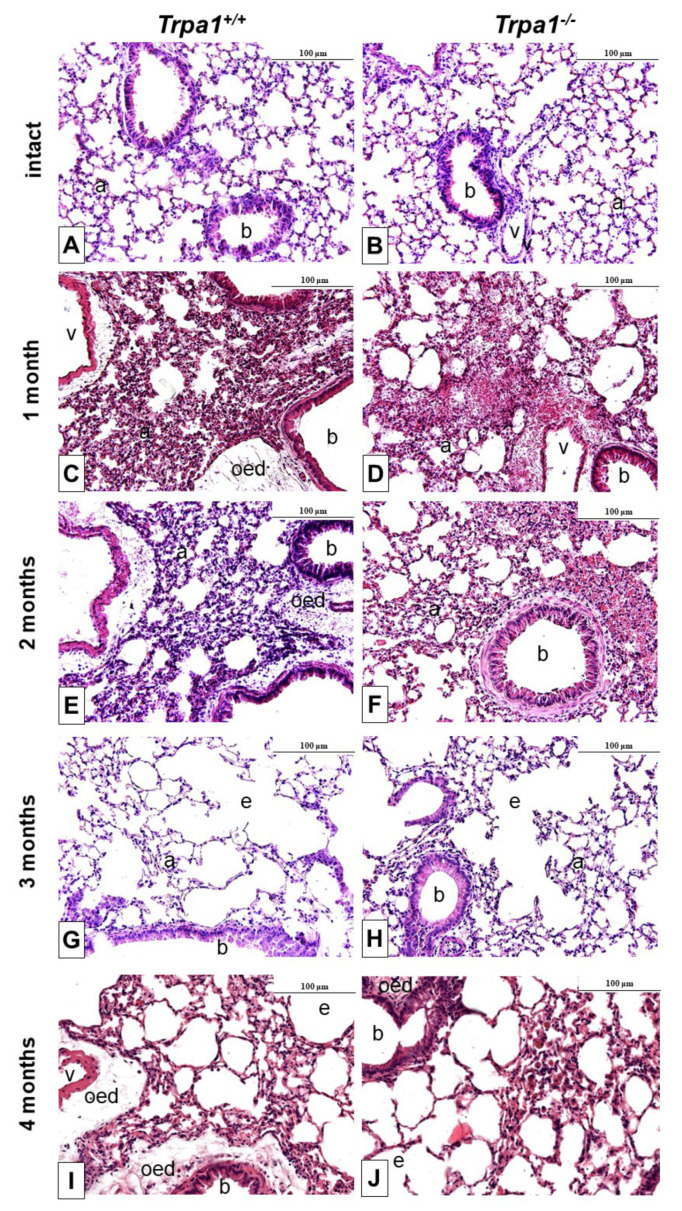
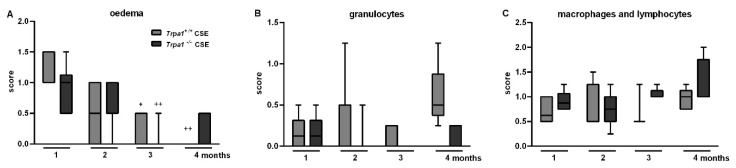
2.6. CSE-Induced Inflammatory Histopathological Alterations are Similar in Trpa1+/+ and Trpa1−/− Mice
After one month of CSE remarkable perivascular oedema developed (Figure 6C,E) that significantly decreased by time in both strains, and almost completely resolved at the end of the 4th month (Figure 7A). However, the accumulation of perivascular and peribronchial, as well as interstitial neutrophil granulocytes, macrophages and lymphocytes remained moderately increased throughout the experimental protocol (Figure 7B,C). At the end of the 3rd month of CSE, structural destruction characteristic to emphysema (Figure 6G–J) already developed.
Figure 6.
Representative histological pictures of the lungs of Trpa1+/+ (A,C,E,G,I) and Trpa1−/− (B,D,F,H,J) mice under intact conditions (A,B), and after 1–4 months of CSE (C–J). One month of CSE induced a perivascular and peribronchial oedema formation associated with inflammatory cell infiltration, that gradually subsided over the 4-month long protocol. After the 3rd month of CSE, emphysema formation was observed in both wildtype and gene-deficient mice. (hematoxylin-eosin staining; 200× g magnification; a: alveolus, b: bronchiolus, v: venula, oed: oedema, e: emphysema).
Figure 7.
Semiquantitative evaluation of the histopathological changes of the lung after chronic cigarette smoke exposure. (A) Perivascular/peribronchial oedema developed after 1 month of CSE, which significantly decreased by time in both strains. The accumulation of perivascular and peribronchial, as well as interstitial (B) neutrophil granulocytes, (C) macrophages and lymphocytes did not differ in either groups significantly. Boxplots represent the minimum, first quartile, mean, third quartile and maximum values, n = 5–13/group, Kruskal–Wallis followed by Dunn’s post-test; + p < 0.05, ++ p < 0.005 vs. 1st month of CSE.
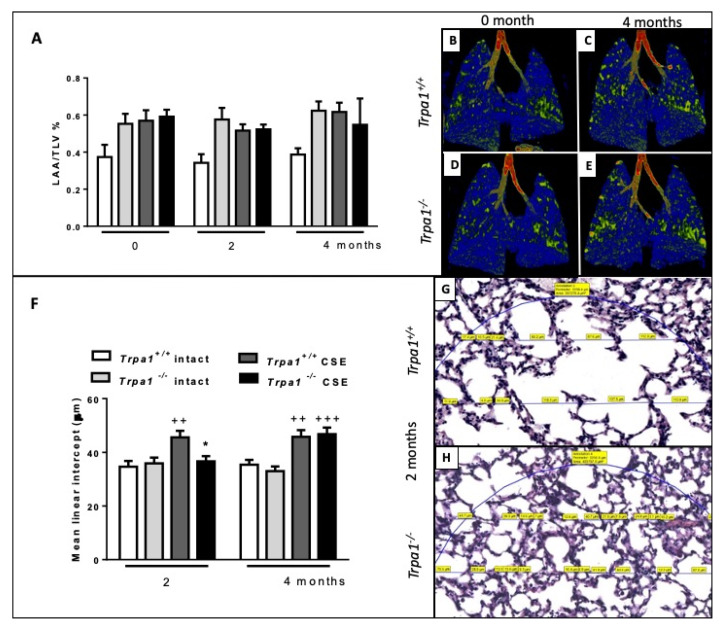
2.7. Cigarette Smoke-Induced Emphysema Develops Earlier in Trpa1+/+ Mice
Emphysema was quantified by in vivo microCT by the ratio of the low attenuation area (LAA) and total lung volume (TLV) before and after 2 and 4 months of CSE. The ratio correlating with the extent of air-filled regions did not show alterations either by CSE treatment or time (Figure 8A). However, the more sensitive mean linear intercept (Lm) measurement revealed that in Trpa1+/+ mice emphysema already started to develop at an earlier timepoint compared to the gene-deleted counterparts, Lm was significantly increased in the wildtypes after 2 months of CSE, however, not in the Trpa1−/−. At the end of the 4th month, Lm was elevated in both strains exposed to CS (Figure 8F).
Figure 8.
Quantitative evaluation of emphysema. (A) LAA/TLV ratio correlating with air-filled regions of the lungs exposed to CSE showed no significant alterations. Representative microCT pictures of lungs (B,D) before and (C,E) after 4 months of CSE in Trpa1+/+ and Trpa1−/− mice, respectively. (F) Microscopic quantitative assessment of Lm showed a significant increase in Trpa1+/+ already after 2 months of CSE, but not in the Trpa1−/−. Values represent means ± SEM, n = 6–7 mice/group; repeated measures two-way ANOVA followed by Tukey’s post-test. Representative microscopic pictures of (G) Trpa1+/+ and (H) Trpa1−/− mouse lung tissues after 2 months of CSE. Values represent means ± SEM, n = 60–100 measurements/group; two-way ANOVA followed by Tukey’s post-test; ++ p < 0.005, +++ p < 0.001 vs. PBS-treated respective group; * p < 0.05 vs. CSE-treated Trpa1+/+. (The blue circle indicates the region of interest in which Lm was measured. The measured chord lengths represented by blue lines were expressed in µm on the scanned slides and labelled in yellow.).
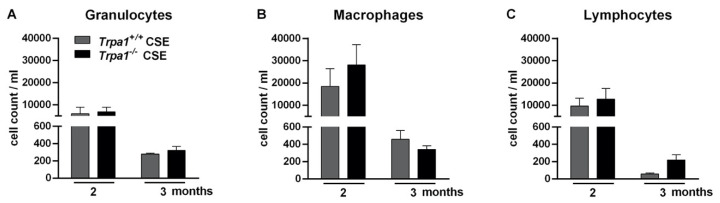
2.8. Chronic Cigarette Smoke-Induced Inflammatory Cell Accumulation in the BALF Shows No Strain Difference
CSE induced massive accumulations of granulocytes, macrophages and lymphocytes measured in the bronchoalveolar lavage fluid (BALF) of both Trpa1+/+ and Trpa1−/− mice. In agreement with our previous findings [63], the number of inflammatory cells reduced by the end of the 3rd month of CSE. There was no biologically relevant difference between the wildtype and gene-deficient mice in either inflammatory cell component (Figure 9).
Figure 9.
Number of inflammatory cells in the bronchoalveolar lavage fluid (BALF) after 2–3 months of CSE in Trpa1+/+ and Trpa1−/− mice. After the peak of inflammatory cell infiltration at a 2-month timepoint, the number of (A) granulocytes, (B) macrophages and (C) lymphocytes remarkably decreased by the end of the 3rd month in both Trpa1+/+ and Trpa1−/− mice. Values represent means ± SEM, n = 6–7 mice/group; two-way ANOVA followed by Tukey’s post-test.
3. Discussion and Conclusion
We provide here the first evidence that the TRPA1 channel has a complex role in basal airway function regulation and inflammatory mechanisms. It protects against LPS-induced acute pneumonitis and hyperresponsiveness, but triggers chronic CSE-evoked emphysema formation and respiratory deterioration (Table 1).
Table 1.
The complex regulatory role of TRPA1 in acute and chronic airway inflammation (ns: non-significant; arrows indicate change compared to control PBS-treated or non-inflamed intact mice, ++ p < 0.005, +++ p < 0.001; asterisks indicate strain difference, * p < 0.05, ** p < 0.005 vs. Trpa1+/+).
| Endotoxin-Induced Acute Inflammation | Trpa1+/+ | Trpa1−/− |
Trpa1+/+ vs. Trpa1−/−
LPS-Treated Inflamed |
| Compared to PBS-Treated Control | |||
| Bronchial hyperreactivity | ns. | ↑(++) | * |
| Myeloperoxidase activity | ns. | ↑(+++) | ** |
| Inflammatory histopathological changes | ↑(++) | ns | ns |
| CSE-induced Chronic Inflammation | Trpa1+/+ | Trpa1−/− |
Trpa1+/+ vs. Trpa1−/−
CSE-Treated Inflamed |
| Compared to Intact Control | |||
| TV, MV, PIF, PEF | ↓(++/+++) | ns | * |
| Oedema | ↑ | ↑ | ns. |
| Inflammatory cell infiltration | ↑ | ↑ | ns. |
| Emphysema | earlier | later | * |
Increasing data have suggested the involvement of the TRPA1 receptor in the pathophysiological mechanisms of several airway diseases, such as asthma, COPD and allergic/irritative cough [7,46,56,57,58,59,60,62,64,65,66,67], but little is known about its activation mechanisms and its potential as a drug target in lung inflammation is still controversial. Our results demonstrating seemingly opposing regulatory functions of TRPA1 in the acute and chronic models can be explained by its multiple localizations that might evoke different responses. Neuronal TRPA1 in the airways is expressed almost exclusively on vagal afferents that are a subpopulation of sensory afferents. It is co-localized with Transient Receptor Potential Vanilloid 1 (TRPV1) on capsaicin-sensitive vagal bronchopulmonary nociceptive C-fibers originating from the jugular ganglion. Most of these peptidergic bronchopulmonary C-fibers modulate the inflammatory process and induce defensive reflexes, shallow breathing, mucus secretion [68,69]. However, TRPA1-mediated effects via the sensory trigeminal afferentation of the upper airways also might contribute to our results in both models [70]. Besides the neuronal expression, TRPA1 is also located on epithelial, inflammatory and bronchial smooth muscle cells [6,47,48,50].
The virtually contradicting role of TRPA1 might also be explained by the very distinct pathophysiological mechanisms of the LPS and CSE models involving different signaling pathways in different cell types. Moreover, endotoxin and cigarette smoke components are able to directly activate TRPA1 among other exogenous irritants reaching the airways, besides a variety of endogenous inflammatory mediators (protons, hydrogen peroxide, prostaglandins etc.) [5,8,10,18,22].
Direct interactions between endotoxins and TRPA1 [71,72] has been described in LPS-induced acute inflammatory pain, CGRP-release and vascular response that developed via the activation of TRPA1 on nociceptive sensory fibers, independently from TLR4 signaling [5]. The TRPA1 agonist cinnamaldehyde exerts complex immunomodulatory effects on LPS-induced systemic inflammatory response syndrome [73]. TRPA1 mediates the LPS-induced inflammatory responses in primary human osteoarthritic fibroblast-like synoviocytes [74]. The role of TRPA1 as an LPS sensor is suggested to be evolutionarily conserved [75], that occurs via mechanical modifications of the plasma lipid membrane. Interestingly, Escherichia coli (E. coli) LPS seems to be more effective on TRPA1 than other types of endotoxins [76]. Although previous studies demonstrate TRPA1 activation by LPS and its implication in acute LPS-induced pain and neurogenic inflammation [5], the relative importance of TLR4 and TRPA1 activation by LPS in our pneumonitis model remains to be elucidated.
The protective role of TRPA1 in the LPS-induced acute inflammatory processes including bronchial hyperreactivity is supported by previous results of our group reporting similar protective actions of capsaicin-sensitive sensory nerves and the TRPV1 receptor in the same model [77,78]. The similar functions of TRPA1 and TRPV1 ion channels are not surprising, since they are often co-expressed and interact with each other on the peptidergic sensory nerves [1,79]. The TRPA1-mediated protective effect might be explained by the release of anti-inflammatory sensory neuropeptides from primary afferents, such as somatostatin, similarly to the mechanism described earlier for TRPV1 activation [34,77].
TRPA1 proved to be protective against inflammatory bronchial hyperresponsiveness potentially via smooth muscle relaxant neuropeptides released from the sensory nerves, despite its presence on bronchial smooth muscle cells [47], which might directly lead to bronchoconstriction. Furthermore, bronchodilator effects of TRPA1 activation via non-epithelial PGE2 production was recently reported in allergic airway inflammation models [80]. Such mechanism might also be involved in our results. A recent study also demonstrated significantly increased airway hyperresponsiveness in Trpv4 and Trpa1/Trpv1 double knockout mice as well. The TRPV4 antagonist HC067047 administered to Trpa1/Trpv1 double knockout animals further increased the Penh value [81] supporting the protective role of these TRP channels in the LPS-induced acute airway inflammation model.
TRPA1-deficiency did not significantly alter inflammatory cell numbers in the histopathological pictures, but significantly increased neutrophil- and macrophage-derived MPO activity, which is supported by TRPA1 expression on these cells [36,82]. The discrepancies between the histopathological semiquantitative scores and the MPO activity might be due to the different sensitivity of the functional and morphological assessments, however, it has also been described that MPO protein expression itself might not correlate strongly with MPO activity due to genetic polymorphism or endogenous inhibitors [83]. Consequently, increased ROS production might contribute to the increased bronchial hyperreactivity in the Trpa1-deleted mice. These results are supported by earlier data that TRPA1 activation by irritants evokes defensive functions in the airways [54].
Despite these protective functions of TRPA1 in the acute LPS-evoked pneumonitis model, TRPA1 activation is required for chronic CSE-evoked emphysema and respiratory deterioration, such as MV, TV, PIF and PEF decrease with a peak after 3 months.
These data are supported by findings, that 4-week CSE increases TRPA1 mRNA level in the nodose and jugular ganglia, positively correlating with the inflammatory cell infiltration in the BALF [84]. Moreover, cigarette smoke extract also increased the expression of TRPA1 in airway epithelial cells in a hypoxia-inducible factor-1α-mediated manner [17,85]. Mostly in vitro data using cigarette smoke extract are available about the role of TRPA1 in cigarette smoke-induced airway inflammation. Isolated bronchi experiments suggested that cigarette smoke extract, as well as its components (acrolein and crotonaldehyde) caused Ca2+-dependent CGRP- and SP-release from the capsaicin-sensitive nerve endings, and TRPA1 was involved in the cigarette smoke extract-induced tracheal plasma extravasation and bronchoconstriction [6]. Cigarette smoke-induced CGRP release in the trachea were predominantly mediated by TRPA1 rather than nicotinic receptors [9]. Cigarette smoke and acrolein released keratinocyte chemoattractant (CXCL1/KC, mouse analogue of IL-8), which was attenuated by TRPA1 antagonists and TRPA1-deficiency [47]. Furthermore, cigarette smoke extract-induced and TRPA1-mediated IL-8 release was shown to develop via NADPH-oxidase activation and the MAPKs/NFκB signaling pathway-related Ca2+ influx [17]. TRPA1 is involved in cigarette smoke extract-evoked alveolar and bronchial epithelial damage [49]. Nicotine directly activates the TRPA1 receptor [8,10], which might mediate bronchoconstriction [47]. Similarly, ROS and several lipid peroxidation products also stimulate TRPA1, which is likely to contribute to oxidative stress-evoked airway pathologies induced by CSE [7,17,55], such as emphysema, for which we provided the first data here.
The extent of perivascular/peribronchial oedema was the most severe after 1 month and gradually decreasing afterwards, and the inflammatory cell infiltration reached its maximum after 2 months of CSE in both groups, which is in agreement with our earlier findings in the same model [63]. TRPA1 deficiency did not result in significant changes of the cellular components of these chronic inflammatory processes, as shown by both the histopathological results and BALF analysis.
Since the activation of TRPA1 exerts protective effects in LPS-induced acute pneumonitis and subsequent bronchial hyperreactivity, our findings clearly support the concept that short-term activation of TRPA1 results in defensive effects presumably via sensory nerves and consequently released protective neuropeptides. However, permanent stimulation of the receptor under chronic inflammatory conditions of the airways results in complex regulatory functions due to the diverse localization of TRPA1 also on non-neural cells and its broad range of both exogenous and endogenous activators.
The genetic deletion of the receptor does not directly predict prophylactic or therapeutic potential of TRPA1 agonists or antagonists. However, the activation of TRPA1 by commonly inhaled substances, e.g., cinnamaldehyde or carvacrol [7] (components of cinnamon or thyme essential oils) could be beneficial against acute inflammatory changes of the lung, additionally considering their antimicrobial potentials against pathogens predominant in airway infections [86].
Therefore, further research is needed to determine TRPA1 potential as a pharmacological target in the lung.
4. Methods
4.1. Animals
Experiments were performed on male and female Trpa1−/− mice and their Trpa1+/+ counterparts (8–10 weeks, 20–25 g). The original heterozygote Trpa1+/− breeding pairs were a generous gift of Pierangelo Geppetti (Firenze, Italy) [87]. The endotoxin-induced pneumonitis model was carried out on female animals, while in the cigarette smoke-induced bronchitis model mice of both sexes were used. Background strain of the gene-deleted animals was C57Bl/6, and the germline transmission of the mutated allele and excision of the selection cassette were verified by PCR analysis. Animals were bred and kept in the Laboratory Animal House of the Department of Pharmacology and Pharmacotherapy, University of Pécs, Pécs, Hungary at 24–25 °C, provided with standard chow and water ad libitum and maintained under a 12-h light–dark cycle.
4.2. Ethics
All experimental procedures were carried out according to the 40/2013 (II.14.) Government Regulation on Animal Protection, Consideration Decree of Scientific Procedures of Animal Experiments (243/1988) and Directive 2010/63/EU of the European Parliament. Studies were approved and a license was given by the Ethics Committee on Animal Research of University of Pécs, Pécs, Hungary according to the Ethical Codex of Animal Experiments (licence No.: BA02/2000-35/2016, BA02/2000-26/2018). We addressed the ARRIVE guidelines for designing, performing and reporting the experiments wherever possible.
4.3. Endotoxin-Induced Acute Pneumonitis
Acute interstitial lung inflammation was evoked by intranasal (i.n.) administration of 60 μL, 167 µg/mL E. coli (serotype: O83) endotoxin (lipopolysaccharide, LPS) under light ether anaesthesia [77]. LPS was isolated and purified in the Department of Microbiology, University of Pécs, Pécs, Hungary [88]. Control animals received the same volume of sterile PBS.
Endotoxin is a component of the cell wall of Gram-negative bacteria, composed of a phosphoglycolipid (lipid A) covalently bound to a hydrophilic heteropolysaccharide part [89]. LPS—connected to the specific LPS binding protein (LBP)—is able to bind to Toll-like receptor 4 (TLR4)-CD14 glycoprotein complex expressed on macrophages and monocytes [90]. Via the p38-MAPK signaling pathway it induces the activation and accumulation of immune cells [91,92]. As a result, inflammatory cytokines and proinflammatory mediators (e.g., bradykinin, leukotrienes and prostaglandins) are released from the activated immune cells directly activating the sensory nerve endings [93]. Beside the activation of immune cells, LPS also elicits bronchial contraction in the lung causing enhanced airway resistance [94].
4.4. Cigarette Smoke-Induced Chronic Airway Inflammation
Chronic bronchitis was elicited by whole body cigarette smoke exposure for 4 months. Mice were exposed to cigarette smoke (3R4F Kentucky Research Cigarette; University of Kentucky, Lexington, KY, USA) twice daily, 10 times per week in a whole body smoke exposure chamber (Teague Enterprises, Woodland, CA, USA) for 30 min followed by a ventilation period of 30 min as described previously [63].
4.5. Investigation of Airway Function and Bronchial Responsiveness
Parameters of the airway function were measured in conscious, spontaneously breathing mice with the help of unrestrained whole-body plethysmography (Buxco Europe Ltd., Winchester, UK).
In the endotoxin-induced acute pneumonitis model, breathing frequency (f) and carbachol-induced airway reactivity were measured before and 24 h after intranasal PBS/LPS administration [95]. Bronchoconstriction was induced by increasing concentrations (5.5, 11 and 22 mM) of the muscarinic receptor agonist carbachol (50 µL/mouse), and the Penh (enhanced pause) value was determined. Penh is a complex calculated parameter ((expiratory time/relaxation time) − 1)/(max. expiratory flow/max. inspiratory flow), well correlating with bronchoconstriction and airway resistance measured in ventilated animals using invasive techniques [34].
Considering that cigarette smoke-induced chronic bronchitis model is a disease model with high translational relevance, we performed an extended analysis of the respiratory functions determining f, TV, MV, Ti, Te, RT, PIF, PEF and Penh before and at the end of every month of the 4-month-investigational period as described previously [63].
4.6. Cell Composition Analysis of the Bronchoalveolar Lavage Fluid (BALF)
In the cigarette smoke exposure model, mice were anaesthetised with ketamine and xylazine (100 mg/kg and 5 mg/kg, s.c., respectively) and the lungs were washed with 5 mL PBS. BALF was collected in centrifuge tubes (1000 rpm, 5 min) and the supernatants were removed. Cells were resuspended in staining buffer (0.1% NaN3 and 0.1% BSA dissolved in 500 µL PBS), and 1 µL CD45 fluorescein-5-isothiocyanate (FITC) solution was given to the samples. After incubation of 30 min, 1 µL propidium-iodide was given to the samples and after centrifugation (1000 rpm, 5 min) the supernatant was removed again. Cells were resuspended in fixation buffer (3% formaldehyde dissolved in 700 µL PBS) and the cell profile of the samples was analysed with a CyFlow Space flow cytometer (Sysmex Partec, Münster, Germany) [96].
We previously showed that in the CSE model perivascular/peribronchial oedema developed in the 1st month, while in the 2nd and 3rd months inflammatory cell infiltration dominated the histopathological picture, which decreased by the 4th month accompanied by tissue destruction [63]. Based on these data, we investigated the amount of inflammatory cells in the BALF after the 2nd and 3rd months.
4.7. Histological Examination of the Lungs
In both models, lungs were removed following cervical dislocation in deep anaesthesia. The left lung was fixed in 4% formaldehyde and embedded in paraffin for histopathological processing. Sections were made with 5–7 µm microtome and stained with hematoxylin-eosin (HE). One section of the lungs of the endotoxin-treated mice was stained with periodic acid-Schiff (PAS) reagent in order to visualize mucus producing goblet cells. Semiquantitative evaluation of the histological alterations was performed by an expert pathologist blinded from the experimental design.
In the acute pneumonitis model, semiquantitative histopathological scoring of the lungs was performed based on the following parameters: perivascular oedema (0–3), accumulation of the perivascular and peribonchial neutrophil granulocytes (0–3), infiltration of activated macrophages and mononuclear cells into the alveolar space (0–2), as well as hyperplasia of the bronchiolar goblet cells (0–2) [97]. The composite inflammatory score (ranging between 0 and 10) was generated by addition of the individual histopathological parameters.
In the chronic COPD model, semiquantitative histopathological scoring of the lungs was established by our work group and performed on the basis of perivascular oedema, the accumulation of neutrophil granulocytes into the perivascular/peribronchial and interstitial space, as well as the perivascular/peribronchial and interstitial infiltration of macrophages and lymphocytes with scores ranging from 0–3 (0: intact, 0.5: focal mild, 1: diffuse mild, 1.5: focal moderate, 2: diffuse moderate, 2.5: focal severe, 3: diffuse severe).
Quantitative histopathological evaluation of emphysema was performed by the measurement of the mean linear intercept as described previously [98]. Briefly, air space enlargement was assessed by the measurement of the alveolar space or alveolar and ductal air space along parallel lines on approximately 400,000 µm2 representative areas on each slide by The Case Viewer software (3DHISTECH, Budapest, Hungary).
4.8. Morphological Evaluation of the Lungs with In Vivo MicroCT Investigation
In the cigarette smoke exposure model, structural alterations, such as the LAA/TLV% characteristic to emphysema was also measured by in vivo microCT in a self-controlled manner, before, as well as 2 and 4 months after CSE exposure as described previously [63]. Briefly, mice were anaesthetized with pentobarbital (70 mg/kg) i.p. and their lungs were imaged by breath-gated tomography on a Skyscan 1176 high resolution microtomograph (Skyscan, Kontich, Belgium). Reconstruction and morphometric analysis were performed with the software provided by the manufacturer.
4.9. Determination of Myeloperoxidase (MPO) Activity from Lung Homogenates with Spectrophotometry
During the evolvement of endotoxin-induced acute pneumonitis, MPO enzyme is produced by the accumulated neutrophil granulocytes, monocytes and macrophages [99]. The MPO activity of the lung homogenates were measured by spectrophotometry using H2O2-3,3′,5,5′-tetramethyl-benzidine (TMB/H2O2) and compared to a standard MPO preparation as described earlier [98].
4.10. Statistical Analysis
Statistical analysis was performed by the GraphPad Prism v6 software (GraphPad Software, San Diego, CA, USA). Comparison of basal respiratory functions of intact wildtype and TRPA-deficient mice was performed by a Student’s t-test for unpaired comparison. Parameters of the respiratory function in both the LPS and CSE study, as well as LAA/TLV%, mean linear intercept, and BALF inflammatory cell counts were evaluated by two-way ANOVA followed by Tukey’s post hoc test. MPO activity was analysed by one-way ANOVA followed by Bonferroni’s post-test. Histopathological semiquantitative scores were evaluated by Kruskal–Wallis analysis followed by Dunn’s post-test. In all cases p < 0.05 was accepted as significant.
Acknowledgments
The in vivo imaging experiments were performed in the Small Animal Imaging Core Facility of the Szentágothai Research Centre, University of Pécs, Hungary.
Author Contributions
Conceptualization, Z.H. (Zsuzsanna Helyes), Z.H. (Zsófia Hajna), K.C., E.P.; funding acquisition, Z.H. (Zsuzsanna Helyes), E.P., investigation, Z.H. (Zsófia Hajna), K.C., Á.K., I.S.; formal analysis: Z.H. (Zsófia Hajna), K.C., L.K., T.K., methodology, Z.H. (Zsófia Hajna), K.C., Á.K., T.K., B.K., A.P., Z.H. (Zsuzsanna Helyes).; project administration, Z.H. (Zsófia Hajna), K.C., I.S.; resources, B.K., Z.H. (Zsuzsanna Helyes), E.P.; supervision, Z.H. (Zsuzsanna Helyes); visualization, Z.H. (Zsófia Hajna), K.C., A.P., T.K., L.K., writing—original draft, Z.H. (Zsófia Hajna), K.C., Z.H. (Zsuzsanna Helyes); writing—review and editing, Z.H. (Zsófia Hajna), K.C., Á.K., L.K., T.K., A.P., I.S., B.K., E.P., Z.H. (Zsuzsanna Helyes). All authors have read and approved the final manuscript.
Funding
Z.H. (Zsuzsanna Helyes) was supported by the Higher Education Institutional Excellence Program of the Ministry of Human Capacities in Hungary, 20765-3/2018/FEKUTSRTAT; PEPSYS: Complexity of Peptidergic Signalization and its Role in Systemic Diseases, GINOP-2.3.2-15-2016-00050; Human Resource Development Operational Program, EFOP-3.6.2-16-2017-00006 LIVE LONGER and EFOP-3.6.1-16-2016-00004; and Economic Development and Innovation Operational Program, GINOP-2.3.2-15-2016-00048 STAY ALIVE. K.C. was supported by the ÚNKP-19-3-III-PTE-211 New National Excellence Program of the Ministry of Human Capacities. Á.K. was supported by János Bolyai Research Scholarships of the Hungarian Academy of Sciences and ÚNKP-19-4 New National Excellence Program of the Ministry For Innovation And Technology.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Nassenstein C., Kwong K., Taylor-Clark T., Kollarik M., MacGlashan D.M., Braun A., Undem B.J. Expression and function of the ion channel TRPA1 in vagal afferent nerves innervating mouse lungs. J. Physiol. 2008;586:1595–1604. doi: 10.1113/jphysiol.2007.148379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zygmunt P.M., Högestätt E.D. TRPA1. In: Nilius B., Flockerzi V., editors. Mammalian Transient Receptor Potential (TRP) Cation Channels. Springer; Berlin/Heidelberg, Germany: 2014. Mammalian. [Google Scholar]
- 3.Gaudet R. A primer on ankyrin repeat function in TRP channels and beyond. Mol. Biosyst. 2008;4:372–379. doi: 10.1039/b801481g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cordero-Morales J.F., Gracheva E.O., Julius D. Cytoplasmic ankyrin repeats of transient receptor potential A1 (TRPA1) dictate sensitivity to thermal and chemical stimuli. Proc. Natl. Acad. Sci. USA. 2011;108:E1184–E1191. doi: 10.1073/pnas.1114124108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meseguer V., Alpizar Y.A., Luis E., Tajada S., Denlinger B., Fajardo O., Manenschijn J.-A., Fernández-Pena C., Talavera A., Kichko T., et al. TRPA1 channels mediate acute neurogenic inflammation and pain produced by bacterial endotoxins. Nat. Commun. 2014;5 doi: 10.1038/ncomms4125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andrè E., Campi B., Materazzi S., Trevisani M., Amadesi S., Massi D., Creminon C., Vaksman N., Nassini R., Civelli M., et al. Cigarette smoke—Induced neurogenic inflammation is mediated by α,β-unsaturated aldehydes and the TRPA1 receptor in rodents. J. Clin. Investig. 2008;118:2574–2582. doi: 10.1172/JCI34886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bessac B.F., Jordt S.-E. Breathtaking TRP Channels: TRPA1 and TRPV1 in Airway Chemosensation and Reflex Control. Physiology. 2008;23:360–370. doi: 10.1152/physiol.00026.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung S., Baumlin N., Dennis J.S., Moore R., Salathe S.F., Whitney P.L., Sabater J., Abraham W.M., Kim M.D., Salathe M. Electronic cigarette vapor with nicotine causes airway mucociliary dysfunction preferentially via TRPA1 receptors. Am. J. Respir. Crit. Care Med. 2019;200:1134–1145. doi: 10.1164/rccm.201811-2087OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kichko T.I., Kobal G., Reeh P.W. Cigarette smoke has sensory effects through nicotinic and TRPA1 but not TRPV1 receptors on the isolated mouse trachea and larynx. Am. J. Physiol. Lung Cell. Mol. Physiol. 2015;309:L812–L820. doi: 10.1152/ajplung.00164.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Talavera K., Gees M., Karashima Y., Meseguer V.M., Vanoirbeek J.A.J., Damann N., Everaerts W., Benoit M., Janssens A., Vennekens R., et al. Nicotine activates the chemosensory cation channel TRPA1. Nat. Neurosci. 2009;12:1293–1299. doi: 10.1038/nn.2379. [DOI] [PubMed] [Google Scholar]
- 11.Shapiro D., Deering-Rice C.E., Romero E.G., Hughen R.W., Light A.R., Veranth J.M., Reilly C.A. Activation of Transient Receptor Potential Ankyrin-1 (TRPA1) in Lung Cells by Wood Smoke Particulate Material. Chem. Res. Toxicol. 2013;26:750–758. doi: 10.1021/tx400024h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deering-Rice C.E., Memon T., Lu Z., Romero E.G., Cox J., Taylor-Clark T., Veranth J.M., Reilly C.A. Differential Activation of TRPA1 by Diesel Exhaust Particles: Relationships between Chemical Composition, Potency, and Lung Toxicity. Chem. Res. Toxicol. 2019;32:1040–1050. doi: 10.1021/acs.chemrestox.8b00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Memon T.A., Nguyen N.D., Burrell K.L., Scott A.F., Almestica-Roberts M., Rapp E., Deering-Rice C.E., Reilly C.A. Wood Smoke Particles Stimulate MUC5AC Overproduction by Human Bronchial Epithelial Cells through TRPA1 and EGFR Signaling. Toxicol. Sci. 2020;174:278–290. doi: 10.1093/toxsci/kfaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trevisani M., Siemens J., Materazzi S., Bautista D.M., Nassini R., Campi B., Imamachi N., André E., Patacchini R., Cottrell G.S., et al. 4-Hydroxynonenal, an endogenous aldehyde, causes pain and neurogenic inflammation through activation of the irritant receptor TRPA1. Proc. Natl. Acad. Sci. USA. 2007;104:13519–13524. doi: 10.1073/pnas.0705923104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor-Clark T.E., McAlexander M.A., Nassenstein C., Sheardown S.A., Wilson S., Thornton J., Carr M.J., Undem B.J. Relative contributions of TRPA1 and TRPV1 channels in the activation of vagal bronchopulmonary C-fibres by the endogenous autacoid 4-oxononenal. J. Physiol. 2008;14:3447–3459. doi: 10.1113/jphysiol.2008.153585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graepel R., Fernandes E.S., Aubdool A.A., Andersson D.A., Bevan S., Brain S.D. 4-Oxo-2-nonenal (4-ONE): Evidence of Transient Receptor Potential Ankyrin 1-Dependent and -Independent Nociceptive and Vasoactive Responses In Vivo. J. Pharmacol. Exp. Ther. 2011;337:117–124. doi: 10.1124/jpet.110.172403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin A.-H., Liu M.-H., Ko H.-K., Perng D.-W., Lee T.-S., Kou Y.R. Lung Epithelial TRPA1 Transduces the Extracellular ROS into Transcriptional Regulation of Lung Inflammation Induced by Cigarette Smoke: The Role of Influxed Ca2+ Mediat. Inlfammation. 2015;2015 doi: 10.1155/2015/148367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taylor-Clark T.E., Undem B.J., MacGlashan D.W., Ghatta S., Carr M.J., McAlexander M.A. Prostaglandin-Induced Activation of Nociceptive Neurons via Direct Interaction with Transient Receptor Potential A1 (TRPA1) Mol. Pharmacol. 2008;73:274–281. doi: 10.1124/mol.107.040832. [DOI] [PubMed] [Google Scholar]
- 19.Al-Shamlan F., El-Hashim A.Z. Bradykinin sensitizes the cough reflex via a B2 receptor dependent activation of TRPV1 and TRPA1 channels through metabolites of cyclooxygenase and 12-lipoxygenase. Respir. Res. 2019;20 doi: 10.1186/s12931-019-1060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pozsgai G., Hajna Z., Bagoly T., Boros M., Kemény Á., Materazzi S., Nassini R., Helyes Z., Szolcsányi J., Pintér E. The role of transient receptor potential ankyrin 1 (TRPA1) receptor activation in hydrogen-sulphide-induced CGRP-release and vasodilation. Eur. J. Pharmacol. 2012;689:56–64. doi: 10.1016/j.ejphar.2012.05.053. [DOI] [PubMed] [Google Scholar]
- 21.Hajna Z., Sághy É., Payrits M., Aubdool A.A., Szőke É., Pozsgai G., Bátai I.Z., Nagy L., Filotás D., Helyes Z., et al. Capsaicin-Sensitive Sensory Nerves Mediate the Cellular and Microvascular Effects of H2S via TRPA1 Receptor Activation and Neuropeptide Release. J. Mol. Med. 2016;60:157–170. doi: 10.1007/s12031-016-0802-z. [DOI] [PubMed] [Google Scholar]
- 22.Bandell M., Story G.M., Hwang S.W., Viswanath V., Eid S.R., Petrus M.J., Earley T.J., Patapoutian A. Noxious Cold Ion Channel TRPA1 Is Activated by Pungent Compounds and Bradykinin. Neuron. 2004;41:849–857. doi: 10.1016/S0896-6273(04)00150-3. [DOI] [PubMed] [Google Scholar]
- 23.Hinman A., Chuang H., Bautista D.M., Julius D. TRP channel activation by reversible covalent modification. Proc. Natl. Acad. Sci. USA. 2006;103:19564–19568. doi: 10.1073/pnas.0609598103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Macpherson L.J., Dubin A.E., Evans M.J., Marr F., Schultz P.G., Cravatt B.F., Patapoutian A. Noxious compounds activate TRPA1 ion channels through covalent modification of cysteines. Nature. 2007;445:541–545. doi: 10.1038/nature05544. [DOI] [PubMed] [Google Scholar]
- 25.Nilius B., Prenen J., Owsianik G. Irritating channels: The case of TRPA1. J. Physiol. 2011;589:1543–1549. doi: 10.1113/jphysiol.2010.200717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen J., Hackos D.H. TRPA1 as a drug target—Promise and challenges. Naunyn. Schmiedebergs. Arch. Pharmacol. 2015;388:451–463. doi: 10.1007/s00210-015-1088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grace M., Birrell M.A., Dubuis E., Maher S.A., Belvisi M.G. Transient receptor potential channels mediate the tussive response to prostaglandin E2 and bradykinin. Thorax. 2012;67:891–900. doi: 10.1136/thoraxjnl-2011-201443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang S., Dai Y., Fukuoka T., Yamanaka H., Kobayashi K., Obata K., Cui X., Tominaga M., Noguchi K. Phospholipase C and protein kinase A mediate bradykinin sensitization of TRPA1: A molecular mechanism of inflammatory pain. Brain. 2008;131:1241–1251. doi: 10.1093/brain/awn060. [DOI] [PubMed] [Google Scholar]
- 29.Meents J.E., Fischer M.J.M., McNaughton P.A. Sensitization of TRPA1 by Protein Kinase A. PLoS ONE. 2017;12:e0170097. doi: 10.1371/journal.pone.0170097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun H., Meeker S., Undem B.J. Role of TRP channels in Gq-coupled Protease-activated Receptor 1-mediated activation of Mouse Nodose Pulmonary C-fibers. Am. J. Physiol. Lung Cell. Mol. Physiol. 2020;318:L192–L199. doi: 10.1152/ajplung.00301.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kádková A., Synytsya V., Krusek J., Zímová L., Vlachová V. Molecular Basis of TRPA1 Regulation in Nociceptive Neurons. A Review. Physiol. Res. 2017;66:425–439. doi: 10.33549/physiolres.933553. [DOI] [PubMed] [Google Scholar]
- 32.Geppetti P., Nassini R., Materazzi S., Benemei S. The concept of neurogenic inflammation. BJU Int. 2008;101:2–6. doi: 10.1111/j.1464-410X.2008.07493.x. [DOI] [PubMed] [Google Scholar]
- 33.Szolcsányi J. Capsaicin-sensitive sensory nerve terminals with local and systemic efferent functions: Facts and scopes of an unorthodox neuroregulatory mechanism. Prog. Brain Res. 1996;113:343–359. doi: 10.1016/s0079-6123(08)61097-3. [DOI] [PubMed] [Google Scholar]
- 34.Helyes Z., Pintér E., Sándor K., Elekes K., Bánvölgyi Á., Keszthelyi D., Szőke É., Tóth D.M., Sándor Z., Kereskai L., et al. Impaired defense mechanism against inflammation, hyperalgesia, and airway hyperreactivity in somatostatin 4 receptor gene-deleted mice. Proc. Natl. Acad. Sci. USA. 2009;106:13088–13093. doi: 10.1073/pnas.0900681106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernandes E.S., Fernandes M.A., Keeble J.E. The functions of TRPA1 and TRPV1: Moving away from sensory nerves. Br. J. Pharmacol. 2012;166:510–521. doi: 10.1111/j.1476-5381.2012.01851.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kun J., Perkecz A., Knie L., Sétáló G., Jr., Tornóczki T., Pintér E., Bán Á. TRPA1 receptor is upregulated in human oral lichen planus. Oral. Dis. 2017;23:189–198. doi: 10.1111/odi.12593. [DOI] [PubMed] [Google Scholar]
- 37.Bertin S., Aoki-Nonaka Y., Lee J., de Jong P.R., Kim P., Han T., Yu T., To K., Takahashi N., Boland B.S., et al. The TRPA1 ion channel is expressed in CD4+ T cells and restrains T cell-mediated colitis through inhibition of TRPV1. Gut. 2017;66:1584–1596. doi: 10.1136/gutjnl-2015-310710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sahoo S.S., Majhi R.K., Tiwari A., Acharya T., Kumar P.S., Saha S., Kumar A., Goswami C., Chattopadhyay S. Transient receptor potential ankyrin1 channel is endogenously expressed in T cells and is involved in immune functions. Biosci. Rep. 2019;39:1–16. doi: 10.1042/BSR20191437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Atoyan R., Shnader D., Botchkareva N. Non-Neuronal Expression of Transient Receptor Potential Type A1 (TRPA1) in Human Skin. J. Invest. Dermatol. 2009;129:2312–2315. doi: 10.1038/jid.2009.58. [DOI] [PubMed] [Google Scholar]
- 40.Kemény Á., Kodji X., Horváth S., Komlódi R., Szőke É., Sándor Z., Perkecz A., Gyömörei C., Sétáló G., Kelemen B., et al. TRPA1 acts in a protective manner in imiquimod-induced psoriasiform dermatitis in mice. J. Investig. Dermatol. 2018;138:1774–1784. doi: 10.1016/j.jid.2018.02.040. [DOI] [PubMed] [Google Scholar]
- 41.Streng T., Axelsson H.E., Hedlund P., Andersson D.A., Jordt S.-E., Bevan S., Andersson K.-E., Högestätt E.D., Zygmunt P.M. Distribution and Function of the Hydrogen Sulfide—Sensitive TRPA1 Ion Channel in Rat Urinary Bladder. Eur. Urol. 2008;53:391–400. doi: 10.1016/j.eururo.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 42.Earley S., Gonzales A.L., Crnich R. Endithelium-Dependent Cerebral Artery Dilation Mediated by TRPA1 and Ca2+-Activated K+ Channels. Circ. Res. 2009;104:987–994. doi: 10.1161/CIRCRESAHA.108.189530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nummenmaa E., Hämäläinen M., Moilanen L.J., Paukkeri E.-L., Nieminen R.M., Moilanen T., Vuolteenaho K., Moilanen E. Transient receptor potential ankyrin 1 (TRPA1) is functionally expressed in primary human osteoarthritic chondrocytes. Arthritis Res. Ther. 2016;18:185. doi: 10.1186/s13075-016-1080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jaquemar D., Schenker T., Trueb B. An Ankyrin-like Protein with Transmembrane Domains Is Specifically Lost after Oncogenic Transformation of Human Fibroblasts. J. Biol. Chem. 1999;274:7325–7333. doi: 10.1074/jbc.274.11.7325. [DOI] [PubMed] [Google Scholar]
- 45.Stokes A., Wakano C., Koblan-Huberson M., Adra C.N., Fleig A., Turner H. TRPA1 is a substrate for de-ubiquitination by the tumor suppressor CYLD. Cell. Signal. 2006;18:1584–1594. doi: 10.1016/j.cellsig.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 46.Mukhopadhyay I., Kulkarni A., Khairatkar-Joshi N. Blocking TRPA1 in Respiratory Disorders: Does It Hold a Promise? Pharmaceuticals. 2016;9:70. doi: 10.3390/ph9040070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nassini R., Pedretti P., Moretto N., Fusi C., Carnini C., Facchinetti F., Viscomi A.R., Pisano A.R., Stokesberry S., Brunmark C., et al. Transient Receptor Potential Ankyrin 1 Channel Localized to Non-Neuronal Airway Cells Promotes Non-Neurogenic Inflammation. PLoS ONE. 2012;7:e42454. doi: 10.1371/journal.pone.0042454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kannler M., Lüling R., Yildirim A.Ö., Gudermann T., Steinritz D., Dietrich A. TRPA1 channels: Expression in non-neuronal murine lung tissues and dispensability for hyperoxia-induced alveolar epithelial hyperplasia. Pflügers Arch. Eur. J. Physiol. 2018;470:1231–1241. doi: 10.1007/s00424-018-2148-6. [DOI] [PubMed] [Google Scholar]
- 49.Wang M., Zhang Y., Xu M., Zhang H., Chen Y., Fan K., Adcock I.M., Li F. Free Radical Biology and Medicine Roles of TRPA1 and TRPV1 in cigarette smoke -induced airway epithelial cell injury model. Free Radic. Biol. Med. 2019;134:229–238. doi: 10.1016/j.freeradbiomed.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 50.Yap M.J.G., Ueda T., Takeda N., Fukumitsu K., Fukuda S., Uemura T., Tajiri T., Ohkubo H., Maeno K., Ito Y., et al. Cytokine An inflammatory stimulus sensitizes TRPA1 channel to increase cytokine release in human lung fibroblasts. Cytokine. 2020;129:155027. doi: 10.1016/j.cyto.2020.155027. [DOI] [PubMed] [Google Scholar]
- 51.Nilius B., Appendino G., Owsianik G. The transient receptor potential channel TRPA1: From gene to pathophysiology. Pflügers Arch. Eur. J. Physiol. 2012;464:425–458. doi: 10.1007/s00424-012-1158-z. [DOI] [PubMed] [Google Scholar]
- 52.López-Requena A., Boonen B., van Greven L., Hellings P.W., Alpizar Y.A., Talavera K. Roles of Neuronal TRP Channels in Neuroimmune Interactions. In: Emir T.L.R., editor. Neurobiology of TRP Channels. CRC Press/Taylor & Francis; Boca Raton, FL, USA: 2017. [PubMed] [Google Scholar]
- 53.Talavera K., Startek J.B., Alvarez-Collazo J., Boonen B., Alpizar Y.A., Sanchez A., Naert R., Nilius B. Mammalian Transient Receptor Potential TRPA1 Channels: From Structure to Disease. Physiol. Rev. 2020;100:725–803. doi: 10.1152/physrev.00005.2019. [DOI] [PubMed] [Google Scholar]
- 54.Chen J., McGaraughty S., Kym P. TRPA1 in drug discovery. In: Szallasi A., Bíró T., editors. TRP Channels in Drug Discovery. Humana Press, Springer; Totowa, NJ, USA: 2012. pp. 43–59. [Google Scholar]
- 55.Viana F. TRPA1 channels: Molecular sentinels of cellular stress and tissue damage. J. Physiol. 2016;594:4151–4169. doi: 10.1113/JP270935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grace M.S., Baxter M., Dubuis E., Birrell M.A., Belvisi M.G. Transient receptor potential (TRP) channels in the airway: Role in airway disease. Br. J. Pharmacol. 2014;171:2593–2607. doi: 10.1111/bph.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Banner H.K., Igney F., Poll C. TRP channels: Emerging targets for respiratory disease. Pharmacol. Ther. 2011;130:371–384. doi: 10.1016/j.pharmthera.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 58.Yang H., Li S. Transient Receptor Potential Ankyrin 1 (TRPA1) Channel and Neurogenic Inflammation in Pathogenesis of Asthma. Med. Sci. Monit. 2016;22:2917–2923. doi: 10.12659/MSM.896557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bonvini S.J., Belvisi M.G. Cough and airway disease: The role of ion channels. Pulm. Pharmacol. Ther. 2017;47:21–28. doi: 10.1016/j.pupt.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 60.Wallace H. Airway Pathogenesis Is Linked to TRP Channels. In: Emir T.L.R., editor. Neurobiology of TRP Channels. CRC Press/Taylor & Francis; Boca Raton, FL, USA: 2017. [PubMed] [Google Scholar]
- 61.Prandini P., De Logu F., Fusi C., Provezza L., Nassini R., Montagner G., Materazzi S., Munari S., Gilioli E., Bezzerri V., et al. Transient Receptor Potential Ankyrin 1 Channels Modulate Inflammatory Response in Respiratory Cells from Patients with Cystic Fibrosis. Am. J. Respir. Cell Mol. Biol. 2016;55:645–656. doi: 10.1165/rcmb.2016-0089OC. [DOI] [PubMed] [Google Scholar]
- 62.Dietrich A. Modulators of Transient Receptor Potential (TRP) Channels as Therapeutic Options in Lung Disease. Pharmaceuticals. 2019;12:23. doi: 10.3390/ph12010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kemény Á., Csekő K., Szitter I., Varga Z.V., Bencsik P., Kiss K., Halmosi R., Deres L., Erős K., Perkecz A., et al. Integrative characterization of chronic cigarette smoke-induced cardiopulmonary comorbidities in a mouse model. Environ. Pollut. 2017;229:746–759. doi: 10.1016/j.envpol.2017.04.098. [DOI] [PubMed] [Google Scholar]
- 64.Caceres A.I., Brackmann M., Elia M.D., Bessac B.F., del Camino D., D’Amours M., Witek J.S., Fanger C.M., Chong J.A., Hayward N.J., et al. A sensory neuronal ion channel essential for airway inflammation and hyperreactivity in asthma. Proc. Natl. Acad. Sci. USA. 2009;106:9099–9104. doi: 10.1073/pnas.0900591106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Raemdonck K., de Alba J., Birrell M.A., Grace M., Maher S.A., Irvin C.G., Fozard J.R., O’Byrne P.M., Belvisi M.G. A role for sensory nerves in the late asthmatic response. Thorax. 2012;67:19–25. doi: 10.1136/thoraxjnl-2011-200365. [DOI] [PubMed] [Google Scholar]
- 66.Geppetti P., Patacchini R., Nassini R., Materazzi S. Cough: The Emerging Role of the TRPA1 Channel. Lung. 2010;188:S63–S68. doi: 10.1007/s00408-009-9201-3. [DOI] [PubMed] [Google Scholar]
- 67.Nassini R., Materazzi S., De Siena G., De Cesaris F., Geppetti P. Transient receptor potential channels as novel drug targets in respiratory diseases. Curr. Opin. Investig. Drugs. 2010;11:535–542. [PubMed] [Google Scholar]
- 68.Mazzone S.B., Undem B.J. Vagal afferent innervation of the airways in health and disease. Physiol. Rev. 2016;96:975–1024. doi: 10.1152/physrev.00039.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Undem B.J., Kollarik M. The role of vagal afferent nerves in chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 2005;2:355–360. doi: 10.1513/pats.200504-033SR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Canning B.J. Afferent nerves regulating the cough reflex: Mechanisms and Mediators of Cough in Disease. Otolaryngol. Clin. N. Am. 2010;43:15–25. doi: 10.1016/j.otc.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boonen B., Alpizar Y.A., Meseguer V.M., Talavera K. TRP Channels as Sensors of Bacterial Endotoxins. Toxins (Basel) 2018;10:326. doi: 10.3390/toxins10080326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mazgaeen L., Gurung P. Recent Advances in Lipopolysaccharide Recognition Systems. Int. J. Mol. Sci. 2020;21:379. doi: 10.3390/ijms21020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mendes S.J.F., Sousa F.I.A.B., Pereira D.M.S., Ferro T.A.F., Pereira I.C.P., Silva B.L.R., Pinheiro A.J.M.C.R., Mouchrek A.Q.S., Monteiro-Neto V., Costa S.K.P., et al. Cinnamaldehyde modulates LPS-induced systemic inflammatory response syndrome through TRPA1-dependent and independent mechanisms. Int. Immunopharmacol. 2016;34:60–70. doi: 10.1016/j.intimp.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 74.Yin S., Wang P., Xing R., Zhao L., Li X., Zhang L., Xiao Y. Transient Receptor Potential Ankyrin 1 (TRPA1) Mediates Lipopolysaccharide (LPS)-Induced Inflammatory Responses in Primary Human Osteoarthritic Fibroblast-Like Synoviocytes. Inflammation. 2018;41:700–709. doi: 10.1007/s10753-017-0724-0. [DOI] [PubMed] [Google Scholar]
- 75.Soldano A., Alpizar Y.A., Boonen B., Franco L., López-Requena A., Liu G., Mora N., Yaksi E., Voets T., Vennekens R., et al. Gustatory-mediated avoidance of bacterial lipopolysaccharides via TRPA1 activation in Drosophila. Elife. 2016;5:e13133. doi: 10.7554/eLife.13133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Startek J.B., Talavera K., Voets T., Alpizar Y.A. Differential interactions of bacterial lipopolysaccharides with lipid membranes: Implications for TRPA1-mediated chemosensation. Sci. Rep. 2018;8 doi: 10.1038/s41598-018-30534-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Elekes K., Helyes Z., Németh J., Sándor K., Pozsgai G., Kereskai L., Börzsei R., Pintér E., Szabó Á., Szolcsányi J. Role of capsaicin-sensitive afferents and sensory neuropeptides in endotoxin-induced airway inflammation and consequent bronchial hyperreactivity in the mouse. Regul. Pept. 2007;141:44–54. doi: 10.1016/j.regpep.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 78.Helyes Z., Elekes K., Németh J., Pozsgai G., Sándor K., Kereskai L., Börzsei R., Pintér E., Szabó Á., Szolcsányi J. Role of transient receptor potential vanilloid 1 receptors in endotoxin-induced airway inflammation in the mouse. Am. J. Physiol. Lung Cell. Mol. Physiol. 2007;292:1173–1181. doi: 10.1152/ajplung.00406.2006. [DOI] [PubMed] [Google Scholar]
- 79.Lee L.-Y., Hsu C.-C., Lin Y.-J., Lin R.-L., Khosravi M. Interaction between TRPA1 and TRPV1: Synergy on pulmonary sensory nerves. Pulm. Pharmacol. Ther. 2015;35:87–93. doi: 10.1016/j.pupt.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Marsh B.J., Fryer A.D., Jacoby D.B., Drake M.G. TRPA1 causes rapid bronchodilation via non-epithelial PGE2. Am. J. Physiol. Cell. Mol. Physiol. 2020;318:L943–L952. doi: 10.1152/ajplung.00277.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alpizar Y.A., Boonen B., Sanchez A., Jung C., López-Requena A., Naert R., Steelant B., Luyts K., Plata C., De Vooght V., et al. TRPV4 activation triggers protective responses to bacterial lipopolysaccharides in airway epithelial cells. Nat. Commun. 2017;8:1059. doi: 10.1038/s41467-017-01201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chao L.K., Hua K.-F., Hsu H.-Y., Cheng S.-S., Lin I.-F., Chen C.-J., Chen S.-T., Chang S.-T. Cinnamaldehyde inhibits pro-inflammatory cytokines secretion from monocytes/macrophages through suppression of intracellular signaling. Food Chem. Toxicol. 2008;46:220–231. doi: 10.1016/j.fct.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 83.Pulli B., Ali M., Forghani R., Schob S., Hsieh K.L.C., Wojtkiewicz G., Linnoila J.J., Chen J.W. Measuring Myeloperoxidase Activity in Biological Samples. PLoS ONE. 2013;8:e67976. doi: 10.1371/journal.pone.0067976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dupont L.L., Alpizar Y.A., Brusselle G.G., Bracke K.R., K T., Joos G.F., Maes T. Expression of transient receptor potential (TRP) channels in a murine model of cigarette smoke exposure; Proceedings of the C34 Insights into COPD Pathogenesis from Pre-Clinical Studies; San Diego, CA, USA. 16–21 May 2014. [Google Scholar]
- 85.Nie Y., Huang C., Zhong S., Wortley M.A., Luo Y., Luo W., Xie Y., Lai K., Zhong N. Cigarette smoke extract (CSE) induces transient receptor potential ankyrin 1 (TRPA1) expression via activation of HIF1αin A549 cells. Free Radic. Biol. Med. 2016;99:498–507. doi: 10.1016/j.freeradbiomed.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 86.Ács K., Bencsik T., Böszörményi A., Kocsis B., Horváth G. Essential Oils and Their Vapors as Potential Antibacterial Agents Against Respiratory Tract Pathogens. Nat. Pord. Commun. 2016;11:1709–1712. doi: 10.1177/1934578X1601101121. [DOI] [PubMed] [Google Scholar]
- 87.Bautista D.M., Jordt S.-E., Nikai T., Tsuruda P.R., Read A.J., Poblete J., Yamoah E.N., Basbaum A.I., Julius D. TRPA1 Mediates the Inflammatory Actions of Environmental Irritants and Proalgesic Agents. Cells. 2006;124:1269–1282. doi: 10.1016/j.cell.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 88.Westphal O., Jahn K. Bacterial lipopolysaccharides: Extraction with phenolwater and further applications of the procedure. In: Whistler R.L., editor. Methods in Carbohydrate Chemistry. Academic Press; New York, NY, USA: 1965. pp. 83–91. [Google Scholar]
- 89.Rietschel E.T., Kirikae T., Schade F.U., Mamai U., Günter S., Loppnow H., Ulmer A.J., Zähringer U., Seydel U., Di Padova F., et al. Bacterial endotoxin: Molecular rekationships of sturcutre to activity and function. FASEB J. 1994;8:217–225. doi: 10.1096/fasebj.8.2.8119492. [DOI] [PubMed] [Google Scholar]
- 90.Poltorak A., He X., Smirnova I., Liu M.-Y., Van Huffel C., Du X., Birdwell D., Alejos E., Silva M., Galanos C., et al. Defective LPS Signaling in C3H/HeJ and C57BL/10ScCr Mice: Mutations in Tlr4 Gene. Science. 1998;282:2085–2088. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 91.Haddad E.-B., Birrell M., McCluskie K., Ling A., Webber S.E., Foster M.L., Belvisi M.G. Role of p38 MAP kinase in LPS-induced airway inflammation in the rat. Br. J. Pharmacol. 2001;132:1715–1724. doi: 10.1038/sj.bjp.0704022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Togbe D., Schnyder-Candrian S., Schnyder B., Doz E., Noulin N., Janot L., Secher T., Gasse P., Lima C., Coelho F.R., et al. Toll-like receptor and tumour necrosis factor dependent endotoxin-induced acute lung injury. Int. J. Exp. Path. 2007;88:387–391. doi: 10.1111/j.1365-2613.2007.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Helyes Z., Hajna Z. Endotoxin-induced airway inflammation and asthma models. In: Szallasi A., Bíró T., editors. TRP Channels in Drug Discovery. Humana Press; Totowa, NJ, USA: 2012. pp. 301–342. [Google Scholar]
- 94.Lefort J., Motreff L., Vargaftig B.B. Airway Administration of Escherichia coli Endotoxin to Mice Induces Glucocorticosteroid-Resistant Bronchoconstriction and Vasopermeation. Am. J. Respir. Cell Mol. Biol. 2001;24:345–351. doi: 10.1165/ajrcmb.24.3.4289. [DOI] [PubMed] [Google Scholar]
- 95.Hajna Z., Borbély É., Kemény Á., Botz B., Kereskai L., Szolcsányi J., Pintér E., Paige C.J., Berger A., Helyes Z. Hemokinin-1 is an important mediator of endotoxin-induced acute airway inflammation in the mouse. Peptides. 2015;64:1–7. doi: 10.1016/j.peptides.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 96.Ma W., Cui W., Lin Q. Improved immnunophenotyping of lymphocytes in bronchoalveolar lavage fluid (BALF) by flow cytometry. Clin. Chim. Acta. 2001;313:133–138. doi: 10.1016/S0009-8981(01)00664-7. [DOI] [PubMed] [Google Scholar]
- 97.Zeldin D.C., Wohlford-Lenane C., Chulada P., Bradbury J.A., Scarborough P.E., Roggli V., Langenbach R., Schwartz D.A. Airway Inflammation and Responsiveness in Prostaglandin H Synthase – Deficient Mice Exposed to Bacterial Lipopolysaccharide. Am. J. Respir. Cell Mol. Biol. 2001;25:457–465. doi: 10.1165/ajrcmb.25.4.4505. [DOI] [PubMed] [Google Scholar]
- 98.Helyes Z., Kemény Á., Csekő K., Szőke É., Elekes K., Mester M., Sándor K., Perkecz A., Kereskai L., Márk L., et al. Marijuana smoke induces severe pulmonary hyperresponsiveness, inflammation, and emphysema in a predictive mouse model not via CB1 receptor activation. Am. J. Physiol. Lung Cell. Mol. Physiol. 2017;313:L267–L277. doi: 10.1152/ajplung.00354.2016. [DOI] [PubMed] [Google Scholar]
- 99.Rodrigues M.R., Rodriguez D., Russo M., Campa A. Macrophage Activation Includes High Intracellular Myeloperoxidase Activity. Biochem. Biophys. Res. Commun. 2002;292:869–873. doi: 10.1006/bbrc.2002.6724. [DOI] [PubMed] [Google Scholar]