Abstract
Chronic treatment involving opioids exacerbates both the risk and severity of ischemic stroke. We have provided experimental evidence showing the anti-inflammatory and neuroprotective effects of the μ opioid receptor antagonist β-funaltrexamine for neurodegenerative diseases in rat neuron/glia cultures and a rat model of cerebral Ischemia/Reperfusion (I/R) injury. Independent of in vitro Lipopolysaccharide (LPS)/interferon (IFN-γ)-stimulated neuron/glia cultures and in vivo cerebral I/R injury in Sprague–Dawley rats, β-funaltrexamine downregulated neuroinflammation and ameliorated neuronal degeneration. Alterations in microglia polarization favoring the classical activation state occurred in LPS/IFN-γ-stimulated neuron/glia cultures and cerebral I/R-injured cortical brains. β-funaltrexamine shifted the polarization of microglia towards the anti-inflammatory phenotype, as evidenced by decreased nitric oxide, tumor necrosis factor-α, interleukin-1β, and prostaglandin E2, along with increased CD163 and arginase 1. Mechanistic studies showed that the suppression of microglia pro-inflammatory polarization by β-funaltrexamine was accompanied by the reduction of NF-κB, AP-1, cyclic AMP response element-binding protein, along with signal transducers and activators of transcription transcriptional activities and associated upstream activators. The effects of β-funaltrexamine are closely linked with its action on neuroinflammation by switching microglia polarization from pro-inflammatory towards anti-inflammatory phenotypes. These findings provide new insights into the anti-inflammatory and neuroprotective mechanisms of β-funaltrexamine in combating neurodegenerative diseases, such as stroke.
Keywords: microglia polarization, neuroinflammation, opioid, stroke
1. Introduction
Opioids are potent analgesics and commonly prescribed for the treatment of severe pain and for use in anesthesia. Dynorphins, enkephalins, and β-endorphins are members of the endogenous opioid peptide family which mediate their effects through three subtypes of G-protein coupled membrane receptors, named, μ, δ, and κ. The endogenous opioidergic system is widely distributed throughout the Central Nervous System (CNS) as well as the peripheral tissues. Beyond its effect on the nociceptive/analgesic systems, the opioidergic system also displays effects on physiological and behavioral functions, including respiration, ion channel activity, and immune responses [1,2]. Additionally, alteration in the opioidergic system has been reported in the disease initiation and progression of several acute and chronic diseases, including neurodegenerative diseases [3,4,5,6,7,8,9]. These phenomena highlight the potential pathogenic roles that the opioidergic system may have and candidate targets for intervention with an aim to prevent and/or treat diseases.
As with naturally occurring opioid peptides, the exogenous opioid peptide mimetic exerts the pharmacological effects through binding to specific opioid receptors. Upon binding with either the μ, δ, or κ opioid receptor, they display shared or distinct biological consequences. For example, the neuroprotective effects of the δ and κ opioid receptor agonists and μ opioid receptor antagonist have been described [7,9,10,11]. Despite morphine long being known to have immunosuppressive properties in vivo, a chronic morphine infusion causes neuroinflammation [12,13]. In vitro, both microglia and macrophages respond to morphine by releasing pro-inflammatory cytokines [14,15,16,17,18]. Because the well-known effects of morphine are mediated specifically by the μ opioid receptor subtype, the activation of the μ opioid receptor is closely linked with neuroinflammation. Accordingly, the μ opioid receptor agonists such as d- Ala2-MePhe4-Glyol5-Enkephalin (DAMGO) and fentanyl display pro-inflammatory potential in microglia and astrocytes, while the μ opioid receptor antagonists suppress immune cell activation and pro-inflammatory cytokine expression challenged with morphine, Lipopolysaccharide (LPS), ethanol, or fentanyl [15,17,19,20]. Parallel suppression in inflammatory responses is observed in the presence of δ and κ opioid receptor agonists against LPS or ethanol treatments [20,21,22,23]. Since neuroinflammation plays a substantial role in the pathogenesis of neurodegenerative diseases, the distinct biological functions towards neuroprotection amongst the three subtypes of opioid receptors seem to be closely linked with their effects on neuroinflammation.
The anti-inflammatory and neuroprotective effects of (−)-naloxone, a nonselective opioid receptor antagonist, have been described [11,24,25,26]. However, the anti-inflammatory effects of its inactive stereoisomer (+)-naloxone occur through an opioid receptor in an independent manner [3,18]. β-funaltrexamine is a selective μ opioid receptor antagonist. Increasing evidence suggests it has anti-inflammatory effects in LPS-stimulated human astrocytes and mice. However, it is ineffective in reversing μ opioid receptor agonist-induced pro-inflammatory responses [19,27,28,29,30]. These findings indicate that β-funaltrexamine and naloxone may have the potential to be developed as alternative anti-inflammatory agents.
Previously, we had reported on the neuroprotective effects of opioidergic agents, BW373U86 (δ agonist), dynorphin A 1-13 (κ agonist), and naloxone (nonselective antagonist) but not H-Tyr-d-Ala-Phe-Phe-NH2 (TAPP) (μ agonist) in rat model of cerebral Ischemia/Reperfusion (I/R) injury [11,24]. To extend the scope of β-funaltrexamine’s biological implications, its anti-inflammatory and neuroprotective identities were further explored in rat primary neuron/glia cultures, with the effects then extrapolated to in vivo evaluation in a rat model of cerebral I/R injury.
2. Results
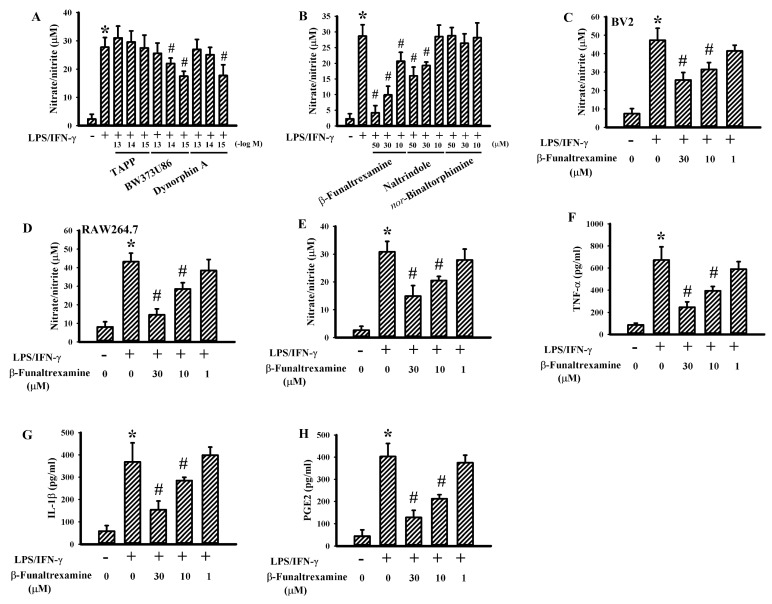
2.1. β-Funaltrexamine Alleviated Neurotoxic Cytokine Production
To explore the anti-inflammatory potential of opioidergic compounds, neonatal rat neuron/glia cultures consisting of neurons, astrocytes, and microglia were prepared. LPS/interferon-gamma (IFN-γ) stimulation caused the release of elevated levels of Nitric Oxide (NO). Ultralow concentrations of the δ opioid receptor agonist BW373U86 and κ opioid receptor agonist Dynorphin A but not the μ opioid receptor agonist TAPP decreased LPS/IFN-γ-induced NO production (Figure 1A). A parallel reduction in NO release was observed in the presence of the μ opioid receptor antagonist β-funaltrexamine and δ opioid receptor antagonist naltrindole, while the κ opioid receptor antagonist nor-binaltorphimine experienced the least effects (Figure 1B). As with the neuron/glia cultures, the effects of β-funaltrexamine were duplicated in the murine BV2 microglial cell line (Figure 1C) and the RAW264.7 macrophage cell line (Figure 1D). Concurrently, β-funaltrexamine alleviated the production of NO (Figure 1E), Tumor Necrosis Factor-α (TNF-α) (Figure 1F), Interleukin-1β (IL-1β) (Figure 1G), and Prostaglandin E2 (PGE2) (Figure 1H) in LPS/IFN-γ-stimulated neuron/glia cultures as well. These findings indicate that there is an inhibitory effect of β-funaltrexamine on neurotoxic cytokine production.
Figure 1.
β-funaltrexamine alleviated neurotoxic cytokine production in neuron/glia cultures. Neuron/glia cultures were pretreated with vehicle, various concentrations of H-Tyr-d-Ala-Phe-Phe-NH2 (TAPP), BW373U86, dynorphin A (A), β-funaltrexamine, naltrindole, or nor-binaltorphimine (B) for 30 min before being incubated with Lipopolysaccharide (LPS) (100 ng/mL)/Interferon-gamma (IFN-γ) (10 U/mL) for an additional 24 h. BV2 cells (C) and RAW264.7 cells (D) were pretreated with vehicle or various concentrations of β-funaltrexamine for 30 min before being incubated with LPS (100 ng/mL)/IFN-γ (10 U/mL) for an additional 24 h. Supernatants were collected and subjected to Griess reagent for the measurement of NO. Neuron/glia cultures were pretreated with vehicle or various concentrations of β-funaltrexamine for 30 min before being incubated with LPS (100 ng/mL)/IFN-γ (10 U/mL) for an additional 24 h. Supernatants were collected and subjected to Griess reagent or ELISA for the measurement of NO (E), Tumor Necrosis Factor-α (TNF-α) (F), Interleukin-1β (IL-1β) (G), and Prostaglandin E2 (PGE2) (H). * p < 0.05 vs. untreated control and # p < 0.05 vs. LPS/IFN-γ control, n = 4.
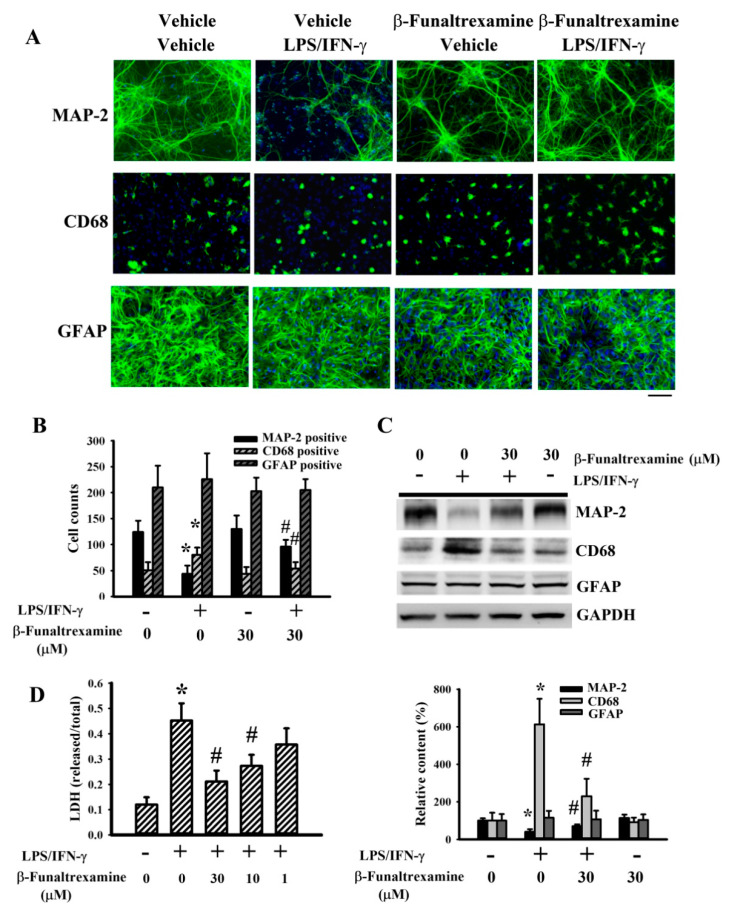
2.2. β-Funaltrexamine Alleviated Neuronal Cell Death
The production of neurotoxic cytokines simultaneously causes neuronal cell death in LPS/IFN-γ-treated neuron/glia cultures [31]. The morphological integrities of visible neurons, microglia, and astrocytes in neuron/glia cultures were examined by the immunoreactivity of Microtubule-Associated Protein 2 (MAP-2), CD68, and Glial Fibrillary Acidic Protein (GFAP) (Figure 2A), respectively. LPS/IFN-γ treatment caused neuronal cell degeneration and the disruption of neuronal cell integrity, while a reduction of visible neuronal cell numbers was alleviated by β-funaltrexamine (Figure 2A). Upon LPS/IFN-γ exposure, ramified microglia changed into reactive microglia of phagocytic morphology. The alternations in microglia morphology were alleviated by β-funaltrexamine (Figure 2A). However, the morphological integrity of astrocytes was not remarkably altered by LPS/IFN-γ or β-funaltrexamine (Figure 2A). Quantitative measurement of cell numbers in MAP-2-, CD68-, and GFAP-immunopositivity (Figure 2B) as well as protein contents in MAP-2, GFAP, and CD68 displayed the same results (Figure 2C) as those in immunofluorescence detection (Figure 2A). Cell damage was further examined by measuring Lactate Dehydrogenase (LDH) efflux. LPS/IFN-γ treatment caused an increase of LDH efflux, while β-funaltrexamine decreased the LDH efflux (Figure 2D). These findings indicate that LPS/IFN-γ induced selective neuronal cell death within neuron/glia cultures and that β-funaltrexamine showed neuroprotective effects.
Figure 2.
β-funaltrexamine alleviated neuronal cell death. Neuron/glia cultures were pretreated with vehicle or β-funaltrexamine (30 μM) for 30 min before being incubated with LPS (100 ng/mL)/IFN-γ (10 U/mL) for an additional 48 h. Cells were subjected to immunofluorescence staining with antibodies recognizing Microtubule-Associated Protein 2 (MAP-2), CD68, and Glial Fibrillary Acidic Protein (GFAP). The cell nuclei were counterstained with Hoechst 33342. Representative micrographs are shown. Bar = 60 μm (A). Quantitative numbers of immunopositivity are shown (B). Total cellular proteins were extracted and subjected to Western blot analysis with indicated antibodies. One representative blot of four independent culture batches is shown (C). Cell damage was measured by LDH efflux assay (D). * p < 0.05 vs. untreated control and # p < 0.05 vs. LPS/IFN-γ control, n = 4.
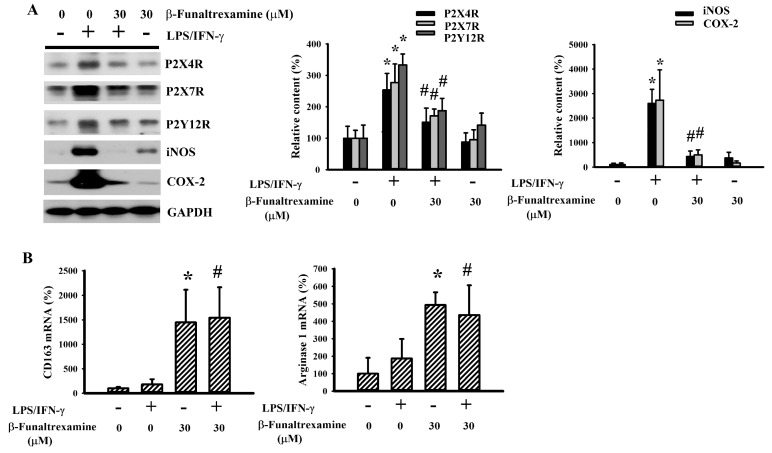
2.3. β-Funaltrexamine Alleviated Microglia Activation
The pro-inflammatory phenotype of microglia is closely linked with an increased expression of P2X purinoceptor 4 (P2X4R), P2X7R, P2Y12R, Inducible Nitric Oxide Synthase (iNOS), Cyclooxygenase 2 (COX-2), and CD68. Oppositely, the alternative or anti-inflammatory phenotype of microglia is associated with a high expression of CD163 and arginase 1 [16,17,22,31,32,33]. In neuron/glia cultures, LPS/IFN-γ elevated the protein levels of P2X4R, P2X7R, P2Y12R, iNOS, COX-2 (Figure 3A), and CD68 (Figure 2C) while had little effect on the mRNA levels of CD163 and arginase 1 (Figure 3B). The levels of reactive microglia-associated proteins were alleviated by β-funaltrexamine (Figure 2C and Figure 3A). However, β-funaltrexamine elevated mRNA expression in anti-inflammatory phenotype microglia-associated CD163 and arginase 1 (Figure 3B). These findings imply that microglia are targets to the actions of β-funaltrexamine and that the alleviation of pro-inflammatory and promotion of anti-inflammatory phenotypes of microglia may be attributed to the anti-inflammatory effects of β-funaltrexamine.
Figure 3.
β-funaltrexamine alleviated microglial activation. Neuron/glia cultures were pretreated with vehicle or β-funaltrexamine (30 μM) for 30 min before being incubated with LPS (100 ng/mL)/IFN-γ (10 U/mL) for an additional 24 h. (A) Total cellular proteins were extracted and subjected to Western blot analysis with indicated antibodies. One representative blot of four independent culture batches is shown. (B) Total cellular RNAs were extracted and subjected to quantitative RT-PCR for the measurement of CD163 and arginase 1 mRNA expression. * p < 0.05 vs. untreated control and # p < 0.05 vs. LPS/IFN-γ control, n = 4.
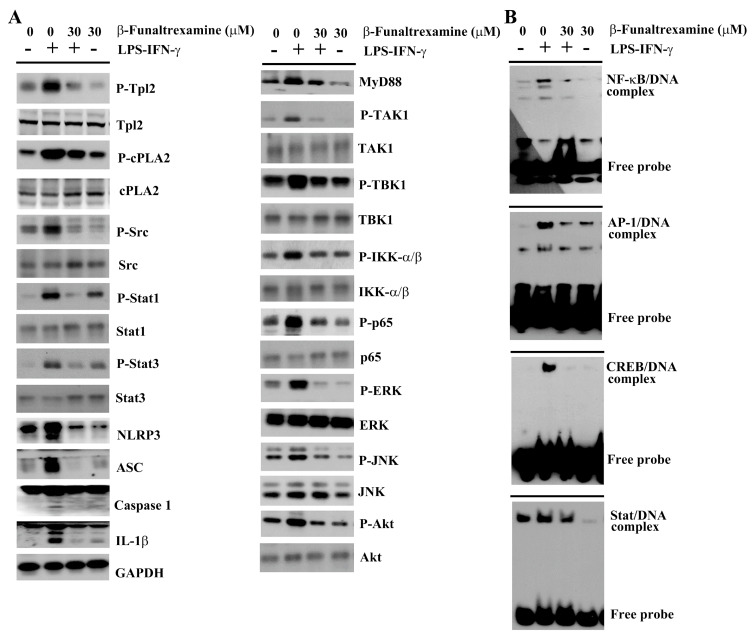
2.4. β-Funaltrexamine Alleviated Inflammatory Intracellular Signaling
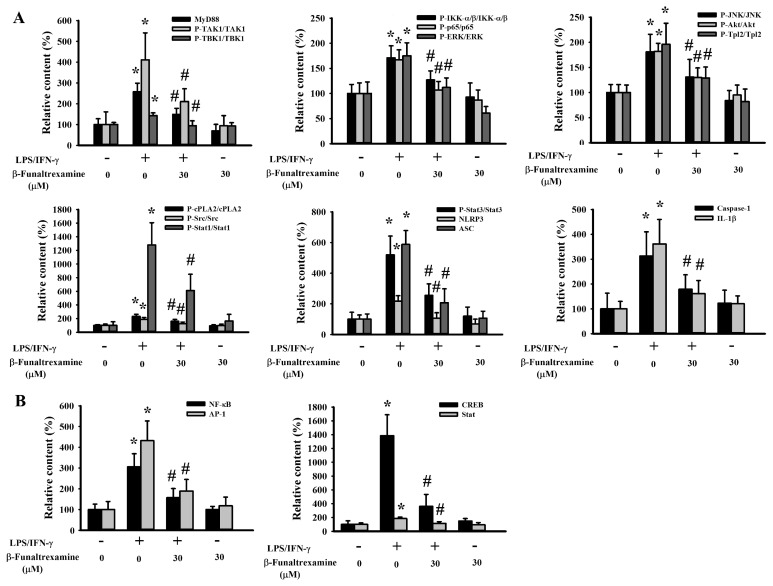
The Toll-Like Receptor (TLR) axis commonly converges various endogenous and exogenous stimuli, including the LPS and IFN-γ, to intracellular signaling molecules and latent transcriptional factors critical to the acquisition of pro-inflammatory phenotypes of microglia and the transcriptional activation of pro-inflammatory cytokines [31,34]. Treatment of neuron/glia cultures with LPS/IFN-γ increased protein expression in MyD88, NLR Family Pyrin Domain Containing 3 (NLRP3), Apoptosis-Associated Speck-Like Protein Containing a CARD (ASC), protein phosphorylation in Transforming Growth Factor β-Activated Kinase-1 (TAK1), TANK-binding Kinase 1 (TBK1), IκB Kinase α/β (IKK-α/β), p65, Extracellular Signal-regulated Kinase (ERK), c-Jun N-terminal Kinase (JNK), Akt, Tumor Progression Locus 2 (Tpl2), cytosolic Phospholipase A2 (cPLA2), Src, Signal Transducers and Activators of Transcription 1 (Stat1), and Stat3 (Figure 4A and Figure 5A) as well as DNA binding activity in NF-κB, AP-1, cAMP-Response Element Binding Protein (CREB), and Stat (Figure 4B and Figure 5B). Besides, a cleavage of caspase-1 and IL-1β protein was found (Figure 4A and Figure 5A). In the presence of β-funaltrexamine, there was a decline in protein expression, protein phosphorylation, protein cleavage, and DNA binding activity (Figure 4 and Figure 5). These findings imply that the anti-inflammatory and neuroprotective effects of β-funaltrexamine may be attributed to its inhibition on the axis of TLRs, NF-κB, AP-1, CREB, and Stat signaling.
Figure 4.
β-funaltrexamine alleviated intracellular signaling molecule activation. Neuron/glia cultures were pretreated with vehicle or β-funaltrexamine (30 μM) for 30 min before being incubated with LPS (100 ng/mL)/IFN-γ (10 U/mL) for an additional 4 h. (A) Total cellular proteins were extracted and subjected to Western blot analysis with indicated antibodies. (B) Nuclear proteins were extracted and subjected to Electrophoretic Mobility Shift Assay (EMSA) for the measurement of NF-κB, AP-1, cAMP-Response Element Binding Protein (CREB), and Stat DNA binding activities. One representative blot of four independent culture batches is shown.
Figure 5.
Quantitative data of β-funaltrexamine-alleviated intracellular signaling molecules: Neuron/glia cultures were pretreated with vehicle or β-funaltrexamine (30 μM) for 30 min before being incubated with LPS (100 ng/mL)/IFN-γ (10 U/mL) for an additional 4 h. (A) Total cellular proteins were extracted and subjected to Western blot analysis with indicated antibodies. (B) Nuclear proteins were extracted and subjected to EMSA for the measurement of NF-κB, AP-1, CREB, and Stat DNA binding activities. Quantitative data are shown. * p < 0.05 vs. untreated control and # p < 0.05 vs. LPS/IFN-γ control, n = 4.
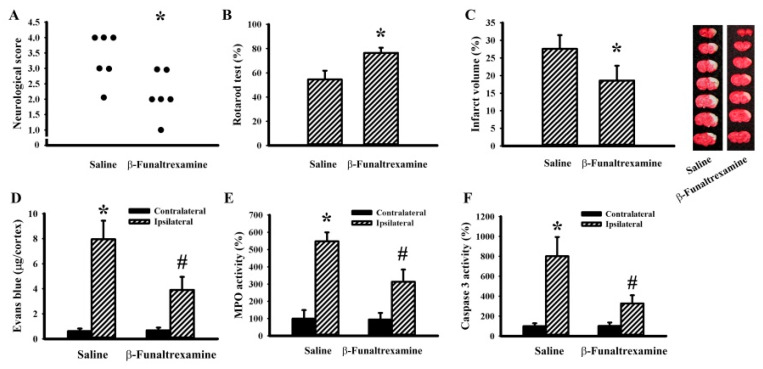
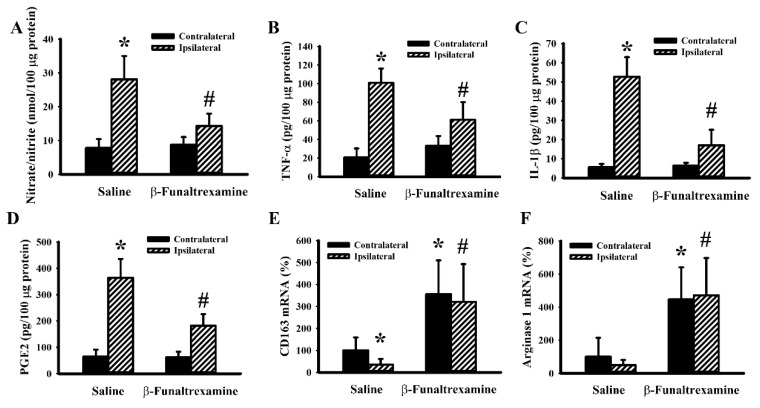
2.5. β-Funaltrexamine Alleviated Cerebral I/R Injury
To further explore the in vivo effects of β-funaltrexamine on neuroinflammation and neurodegeneration, a rat model showing cerebral I/R brain injury was established. Transient focal cerebral I/R caused neurological deficits (Figure 6A), impaired sensorimotor performance (Figure 6B), brain infarction (Figure 6C), Blood–brain Barrier (BBB) disruption (Figure 6D), neutrophil infiltration (Figure 6E), and cell apoptosis (Figure 6F). Intracerebroventricular β-funaltrexamine infusion improved postischemic changes (Figure 6). It was noted that a parallel reduction in reactive microglia released NO (Figure 7A), TNF-α (Figure 7B), IL-1β (Figure 7C), and PGE2 (Figure 7D) as well. The mRNA levels of anti-inflammatory microglia-associated CD163 (Figure 7E) and arginase 1 (Figure 7F) were elevated by β-funaltrexamine. Therefore, β-funaltrexamine displays protective potential against ischemic brain injury concurrently with the amelioration of microglia activation and neuroinflammation.
Figure 6.
β-funaltrexamine protected against cerebral I/R injury. Rats receiving normal saline vehicle or β-funaltrexamine (82.5 nmol/30 μL) intracerebroventricular infusion were subjected to both Common Carotid Arteries (CCAs) and the right middle cerebral artery (MCA) occlusion for 90 min followed by 24-h reperfusion. (A) Neurological deficits were evaluated by neurological score. (B) The motor performance was assessed by a Rotarod test. (C) Representative photographs show the histological examination of a brain infarction by Triphenyltetrazolium Chloride (TTC) staining. The average percentage of infarction volume in the ipsilateral hemisphere is depicted. (D) The contents of Evans blue in contralateral and ipsilateral cortical tissues were measured by an Evans blue extravasation assay. Proteins were extracted from the contralateral and ipsilateral cortical tissues and subjected to an enzymatic assay of Myeloperoxidase (MPO) activity (E) and caspase 3 activity (F). * p < 0.05 vs. saline or the contralateral tissues of the vehicle groups and # p < 0.05 vs. the ipsilateral tissues of the vehicle groups, n = 6.
Figure 7.
β-funaltrexamine alleviated cerebral I/R-induced neurotoxic cytokine production. Rats receiving normal saline vehicle or β-funaltrexamine (82.5 nmol/30 μL) intracerebroventricular infusion were subjected to both CCAs and the right MCA occlusion for 90 min followed by 24-h reperfusion. Total homogenates (ipsilateral and contralateral cortical tissues) were subjected to Griess reagent or ELISA for the measurement of NO (A), TNF-α (B), IL-1β (C), and PGE2 (D) content. Total cellular RNAs were isolated from the ipsilateral and contralateral cortical tissues and subjected to quantitative RT-PCR for the measurement of CD163 (E) and arginase 1 (F) mRNA content. * p < 0.05 vs. the contralateral tissues of the vehicle groups and # p < 0.05 vs. the ipsilateral tissues of the vehicle groups, n = 6.
3. Discussion
Our groups have demonstrated that opioids modulate postischemic progression in a rat model experiencing stroke [11,24]. The studies presented here further extend earlier findings that the μ opioid receptor antagonist β-funaltrexamine possesses both anti-inflammatory and neuroprotective effects in vitro and in vivo. Using rat neuron/glia cultures, β-funaltrexamine protected against LPS/IFN-γ-induced microglia activation, neurotoxic cytokine expression, and neuronal cell death. β-funaltrexamine-mediated the downregulation of pro-inflammatory phenotype of microglia, the upregulation of anti-inflammatory phenotype of microglia, the reduction of neurotoxic cytokine expression, and the inhibition of neuronal cell death, which could be attributed to its interference in the TLR axis and NF-κB, AP-1, CREB, and Stat controlled transcriptional programs. Parallel anti-inflammatory and neuroprotective effects were demonstrated in a rat model experiencing cerebral I/R injury through an intracerebroventricular injection of β-funaltrexamine. These findings provide new insight into the anti-inflammatory and neuroprotective mechanisms of β-funaltrexamine in combating neurodegenerative diseases, such as stroke.
The interaction between the opioidergic and immune systems has been a long-term concern for healthcare professionals. Morphine induces potent analgesia and is commonly prescribed to patients with moderate-to-severe pain. However, the chronic use of morphine leads to tolerance and hyperalgesia due to its pro-inflammatory potential. There have been many studies performed over the years showing the pro-inflammatory mechanisms of morphine and the μ opioid receptor agonists in humans, rodents, and cells, including the microglia [13,14,15,16,17,18]. Contrary to the actions of the μ opioid receptor agonists, the agonists of δ and κ opioid receptors suppress inflammatory responses [20,21,22,23]. The opioid-immune crosstalk is further complicated by the findings that the nonselective opioid receptor antagonist (−)-naloxone and its inactive stereoisomer (+)-naloxone share both anti-inflammatory and neuroprotective effects under certain situations [3,11,13,18,24,25,26]. Currently, the opioid receptor-dependent and -independent anti-inflammatory mechanisms in the relevant studies have been described as being associated with the involvement of TLRs, P2XRs, Histone Deacetylase 6 (HDAC6), Protein Kinase C, Mitogen-Activated Protein Kinase (MAPKs), NF-κB, LPS binding, superoxide anion, and macrophages/microglia polarization.
Clinically, cancer patients undergoing intensive morphine treatment have an increased risk of stroke incidence [34]. Accordingly, a growing body of evidence has revealed the neuroprotective effects of the nonselective opioid receptor antagonist naloxone, δ opioid receptor agonists, and κ opioid receptor agonists in rodent models experiencing neurodegeneration [3,7,9,10,11,24,25,26,35,36,37]. Being a CNS-penetrating compound, the selective μ opioid receptor antagonist β-funaltrexamine is capable of inhibiting LPS-induced neuroinflammation in mice after receiving an intraperitoneal injection [29,30]. Its anti-inflammatory actions are further demonstrated in human astroglial cells under distinct stimuli, including LPS, HIV-1 Tat, and IL-1β. The inhibition of iNOS and chemokine expression is mediated through μ opioid receptor independent mechanisms and involves p38 and NF-κB pro-inflammatory cascade [19,27,28,29,30]. Through intracerebroventricular infusion, we had described the neuroprotective potential of β-funaltrexamine against cerebral I/R injury in rats [24]. Herein, extended studies surrounding anti-neuroinflammation and neuroprotection were demonstrated in rat neuron/glia cultures and a rat model with cerebral I/R injury, while highlighting microglia phenotypes as being targets of β-funaltrexamine’s actions. Despite the distinct insults in vitro or in vivo, we found that the presence of β-funaltrexamine downregulated the pro-inflammatory phenotype of microglia, reduced neurotoxic cytokine expression, and upregulated the anti-inflammatory phenotype of microglia. Our findings imply that β-funaltrexamine may act as an anti-inflammatory agent against various inflammatory insults.
As with macrophages, microglia adopt a series of molecular and biochemical events to switch genetic programs, morphological cytoskeletons, cell membrane surface presentation, and functional outcomes. The rising of pro-inflammatory and the subsiding of anti-inflammatory phenotypes of microglia have been implicated in various neurodegenerative diseases as well as a reversal in the balance of ameliorate disease progression [38,39,40,41]. Typically, neurotoxic cytokines such as TNF-α, IL-1β, IL-18, IL-6, IFN-γ, NO, PGE2, and free radicals come from classical activation polarized microglia. Microglia, in the alternative activation polarization, release Transforming Growth Factor (TGF-β), IL-4, and IL-10, with the consequences of suppressing inflammation and restoring homeostasis. The presence of P2X4R, P2X7R, and P2Y12R promote microglia polarization towards the classical activation state, while CD163 and arginase 1 promote polarizing microglia towards the alternative activation state [32,38,39,40,41,42]. Alterations in microglia polarization favoring the classical activation state occurred in LPS/IFN-γ-stimulated neuron/glia cultures and cerebral I/R-injured cortical brains. β-funaltrexamine shifted the polarization of microglia towards the anti-inflammatory phenotype from the pro-inflammatory, as evidenced by a decrease in NO, TNF-α, IL-1β, and PGE2 as well as increased CD163 and arginase 1. In a cell model of neuron/glia cultures, the effects of β-funaltrexamine were further supported by decreasing the expression of polarization transcription factors and regulators, including P2X4R, P2X7R, and P2Y12R. Although the microglia polarization-associated regulators and the detailed microglia phenotypes were not completely investigated, current findings highlight that the reversal of microglia pro-inflammatory polarization and a switch towards the alternative activation state may be an action mechanism of β-funaltrexamine done to ameliorate neuroinflammation.
Upon cerebral I/R injury or LPS/IFN-γ stimulation, the transmembrane TLR4 represents an active player to engage with various exogenous and endogenous immunocompetent ligands. It can then turn on and spread signaling networks and eventually impact on the nuclear influx activity, DNA binding activity, and transcriptional activity of transcription factors, including NF-κB, AP-1, CREB, and Stat [34,42]. Likewise, the engagement of IFN-γ with receptors activates Stat1 to drive Interferon Regulatory Factor 1 (IRF1) expression, by which transcription factors Stat1 and IRF1 work in concert to boost another wave of transcriptional program. Additionally, the activation of the Stat family latent transcriptional factors is promoted by upstream stimulatory tyrosine kinases such as the Janus Kinase (Jak) and Src family kinases [31,34]. A vast array of linking adaptors and signaling molecules, including MyD88, TAK1, TBK1, Tpl2, cPLA2, ERK, JNK, IKK-α/β, p65, Src, as well as Akt, will have their expression or phosphorylation elevated in LPS/IFN-γ-stimulated neuron/glia cultures. The activation of inflammasome (NLRP3, ASC, and caspase-1) and IL-1β production can boost another wave of pro-inflammatory signaling. Our previous studies indicate that pharmacological inhibitors corresponding to several steps of LPS/IFN-γ intracellular actions caused a reduction in both the production of neurotoxic mediators and neuronal cell death in cultured neuron/glia cultures [31]. β-funaltrexamine alleviated LPS/IFN-γ-activated downstream adaptors, signaling molecules, and transcription factors. Other than microglia, β-funaltrexamine downregulated HIV-1 Tat-, LPS-, and IL-1β-induced NF-κB activation and chemokine expression in human astroglial cells [19,27,28,29,30]. These phenomena highlight the role of β-funaltrexamine in suppressing intracellular pro-inflammatory signaling.
The endogenous opioidergic system is widely distributed throughout the CNS and periphery, while also linking with many physiological activities. The shared and distinct post-receptor consequences from the μ, δ, and κ receptors not only highlight but also complicate their roles in disease initiation and progression. Currently, their crosstalk with the immune system is of clinical attraction. The development of κ opioid receptor mimetic and μ opioid receptor antagonists based on β-funaltrexamine and the μ opioid receptor complex are continuing to find neuroactive candidates [43,44]. Through this study, we have provided experimental evidence showing the anti-inflammatory and neuroprotective effects of β-funaltrexamine for neurodegenerative diseases in rat neuron/glia cultures as well as a rat model with cerebral I/R injury. The effects of β-funaltrexamine are closely linked with its actions on microglia by switching microglia polarization from pro-inflammatory towards anti-inflammatory phenotypes. However, its effects on CNS cell types other than microglia have yet to be explored. Chronic treatment with morphine increases the risk of stroke incidence, and rodent studies have indicated its effects on the blood–brain barrier breakdown involving the μ oipoid receptor [25,45]. Although there still remain limitations to our experiments, the CNS permeable β-funaltrexamine is a proposed anti-inflammatory and neuroprotective candidate for the treatment of neuroinflammation-accompanied neurodegenerative diseases such as stroke. Before it can be translated into clinical practice, however, a deeper investigative insight into its peripheral administration and CNS actions is still required.
4. Materials and Methods
4.1. Cell Cultures
The Animal Experimental Committee of Taichung Veterans General Hospital reviewed and approved the protocols for preparation of primary neuron/glia and microglia cultures from the cerebral cortices of postnatal day 1 Sprague–Dawley rats (La-101986, 29 October 2012). Briefly, the dissected cortices were dissociated by physical trituration and enzymatic digestion, with the dissociated cells then plated onto poly-d-lysine-coated dishes in accordance with previously reported methods [31]. Neuron/glia was prepared by maintaining the cells in a minimum essential medium, supplemented with 10% Fetal Bovine Serum (FBS) and 10% horse serum for 10–12 days. The specific cell types were identified by immunofluorescence staining with antibodies recognizing neurons (MAP-2, Transduction Laboratories, Franklin Lakes, NJ, USA), astrocytes (GFAP, Santa Cruz Biotechnology, Dallas, TX, USA), and microglia (CD68, Santa Cruz Biotechnology). Neuron/glia consisted of 30–40% neurons, 40–50% astrocytes, and 10–15% microglia. The murine microglia BV2 cell line and macrophage RAW264.7 cell line were maintained in Dulbecco’s Modified Eagle Medium (DMEM) containing 10% FBS [33].
4.2. Cytotoxicity Assessment
The cytotoxicity was assessed based upon the efflux of LDH to the culture media using the PierceTM LDH Cytotoxicity Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA). The levels of cytotoxicity were expressed as the ratio of released LDH and total LDH.
4.3. Immunofluorescence Staining
Prior to antibody reaction, neuron/glia (24-well plates) were fixed with 4% paraformaldehyde, permeabilized with 0.1% Triton X-100, and blocked with 5% nonfat milk. Then, the cells were incubated with antibodies against MAP-2, GFAP, or CD68 and followed by Fluorescein Isothiocyanate (FITC)-conjugated secondary antibody. The cell nuclei were counterstained with Hoechst 33342. The immunofluorescence signals were visualized using a fluorescence microscope. For the measurement of MAP-2-, CD68-, and GFAP-positive cell numbers, the total numbers of immunopositive cells were counted from randomly selected four fields in a well of 24-well plates. Four replicates were done for each experiment.
4.4. Enzyme-Linked Immunosorbent Assay (ELISA)
The cell cultured supernatants (100 μL) and brain cortical protein extracts (100 μg) were subjected to the measurement of TNF-α, IL-1β, and PGE2 using commercial ELISA kits (R&D Systems, Minneapolis, MN, USA). For HNO2−/HNO3− (nitrite/nitrate) determination, the samples were subjected to the measurement using a Griess Reagent Kit (Thermo Fisher Scientific).
4.5. Western Blot Analysis
Proteins were extracted from cells and the dissected cortical tissues using the commercial Tissue Protein Extraction Reagents (T-PER, Pierce Biotechnology, Rockford, IL, USA). Proteins went through SDS-PAGE separation and electrical transfer, with the membranes sequentially incubated with primary antibodies, horseradish peroxidase-labeled IgG, and enhanced chemiluminescence Western blotting reagents. The visualized signals were quantitated using a computer image analysis system (IS1000; Alpha Innotech Corporation, San Leandro, CA, USA). Proteins recognized by the primary antibodies were MyD88 (sc-136970), TAK1 (sc-7967), phospho-TAK1(sc-130219), TBK1 (sc-52957), phospho-TBK1 (sc-130219), IKK-α/β (sc-7607), phospho-IKK-α/β (sc-293135), p65 (sc-8008), phospho-p65 (sc-166748), ERK (sc-514302), phospho-ERK (sc-7383), JNK (sc-7345), phospho-JNK (sc-6254), Akt (sc-8312), phospho-Akt (sc-7985-R), Src (sc-5266), phospho-Src (sc-166860), Stat1 (sc-8394), phospho-Stat1 (sc-136229), Stat3 (sc-8019), phospho-Stat3 (sc-8059), P2X4R (sc-15190), P2X7R (sc-514962), P2Y12R (sc-27152), CD68 (sc-20060), iNOS (sc-651), COX-2 (sc-19999), GFAP (sc-33673), cPLA2 (sc-454), Glyceraldehyde 3-Phosphate Dehydrogenase (GAPDH) (sc-32233), ASC (sc-271054), caspase-1 (sc-392736) (Santa Cruz Biotechnology), phospho-cPLA2 (#2831, Cell Signaling, Danvers, MA, USA), MAP-2 (sc-74421) (Transduction Laboratories), Tpl2 (sc-720), phospho-Tpl2 (sc-1717) (R&D Systems), NLRP3 (sc-134306), and IL-1β (sc-52012)(Thermo Fisher Scientific).
4.6. RNA Isolation and Quantitative Real-Time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR)
The total RNAs were extracted from the cells and cortical tissues and subjected to the cDNA synthesis and real-time PCR (ABI StepOneTM, Applied Biosystems, Foster City, CA, USA) according to our previously reported methods [42]. The levels of mRNA expression were calculated using the ΔΔCt method and normalized with β-actin. Oligonucleotide sequences used in PCR were 5’-CCAGTCCCAAACACTGTCCT and 5’-ATGCCAGTGAGCTTCCCGTTCAGC for CD163; 5’-GGAATCTGCATGGGCAACCTGTGT and 5’AGGGTCTACGTCTCGCAAGCCA for arginase 1; and 5′-AAGTCCCTCACCCTCCCAAAAG and 5′-AAGCAATGCTGTCACCTTCCC for β-actin.
4.7. Preparation of Nuclear Extracts and Electrophoretic Mobility Shift Assay (EMSA)
Nuclear proteins were extracted from the cells and dissected cortical tissues using a commercially available nuclear extraction kit and an EMSA kit (Panomics, Fremont, CA, USA). As with our previous studies [31], nuclear extracts (5 μg) were reacted with AP-1 oligonucleotide (5′-CGCTTGATGAGTCAGCCGGAA), NF-κB oligonucleotide (5′-AGTTGAGGGGACTTTCCCAGGC), Stat oligonucleotide (5′-ATCGTTCATTTCCCGTAAATCCCTA), or CREB oligonucleotide (5′-AGAGATTGCCTGACGTCAGAGAGCTAG). The DNA/protein complexes in the membranes were visualized by enhanced chemiluminescence Western blotting reagents and quantitated using a computer image analysis system (IS1000; Alpha Innotech Corporation).
4.8. Cerebral I/R
The Animal Experimental Committee of Taichung Veterans General Hospital reviewed and approved the protocols involving animal studies, while strictly adhering to the institute’s guidelines (La-101986, 29 October 2012). Transient focal cerebral I/R was produced on adult male Sprague–Dawley rats (300 ± 20 g, n = 36 in total) by occluding the two Common Carotid Arteries (CCA) and the right Middle Cerebral Artery (MCA) for 90 min, followed by reperfusion for 24 h [11]. Under anesthesia with isoflurane (2–4%), the rat’s head was mounted in a stereotaxic apparatus and the skull was then partially removed to show the MCA. Pharmacological agents were infused through a cannula inserted perpendicularly into the right lateral ventricle anteroposteriorly at −0.9 mm, mediolaterally at 1.5 mm from the Bregma, and dorsoventrally at −3.5 mm from the dural surface. An intracerebroventricular infusion was initiated 1 h prior to the occlusions and continued for a total of 4 h. The animals were sacrificed 24 h after behavioral evaluation.
4.9. Quantification of Ischemic Infarction
Under anesthesia with isoflurane (2–4%), the rats (n = 6 per group) were decapitated. The brains were cut into a serial coronal section at a 2-mm interval from the frontal pole. The slices were then immersed in 2% Triphenyltetrazolium Chloride (TTC) solution at 37 °C for 30 min, followed by fixation in a 10% phosphate-buffered formalin for 45 min [11]. Brain infarction was highlighted by a white color, and the volume was measured with a computer image analysis system (IS1000; Alpha Innotech Corporation).
4.10. Evans Blue Extravasation Assay
Under anesthesia with isoflurane (2–4%), rats (n = 6 per group) were injected with Evans blue (4%, 1 mL/kg) via the tail vein 3 h prior to being sacrificed. Following perfusing with heparinized saline solution, the rats were decapitated and the ipsilateral and contralateral cortices were isolated. The tissues were homogenized with Phosphate-Buffered Saline (PBS) and precipitated with Trichloroacetic Acid (TCA) (100%). The contents of Evans blue in the supernatants were measured in a photometer (absorbance at 620 nm) and calculated according to a standard curve.
4.11. Neurological Evaluation
Technicians who had been blind to the treatment evaluated the sensorimotor performances using a modified six-point neurological deficit severity scale (n = 6 per group) [42]. Neurological evaluation was performed prior to animal sacrifice, as follows: 0: no neurological deficit; 1: difficulty in fully extending the left forepaw; 2: unable to extend the left forepaw; 3: mild circling to the left; 4: severe circling to the left; and 5: falling to the left.
4.12. Rotarod Test
Motor coordination was evaluated through use of a Rotarod test [46]. Rats (n = 6 per group) were placed on the Rotarod cylinder with speed increasing from 4 rpm to 40 rpm within 5 min time, with the time that the animals remained on the Rotarod cylinder being measured. The mean duration time on the device was recorded with three Rotarod measurements. A percentage of mean duration on the Rotarod cylinder before sacrifice as well as each basal control (before occlusion) were calculated.
4.13. Myeloperoxidase (MPO) Activity Assay
Under anesthesia with isoflurane (2–4%), rats (n = 6 per group) were decapitated and the ipsilateral and contralateral cortices were isolated. Proteins were extracted and subjected to MPO activity measurement using a Myeloperoxidase (MPO) Activity Assay Kit (Abcam, ab105136), according to the manufacturer’s instructions.
4.14. Caspase 3 Activity Assay
Under anesthesia with isoflurane (2–4%), rats (n = 6 per group) were decapitated and the ipsilateral and contralateral cortices were isolated. Proteins were extracted and subjected to enzymatic measurement of caspase 3 activity using a commercial fluorometric protease assay kit (BioVision, Mountain View, CA, USA).
4.15. Statistical Analysis
All statistical results are presented as mean ± standard deviation. A one-way analysis of variance (ANOVA) was performed to evaluate experimental values between groups, with a consequent Dunnett’s test or Tukey post–hoc test performed for the purpose of comparison. It was considered statistically significant when the p value was less than 0.05.
Abbreviations
| ASC | Apoptosis-Associated Speck-Like Protein Containing a CARD |
| BBB | Blood–Brain Barrier |
| CCA | Common Carotid Arteries |
| CNS | Central Nervous System |
| COX-2 | Cyclooxygenase 2 |
| cPLA2 | cytosolic Phospholipase A2 |
| DMEM | Dulbecco’s Modified Eagle Medium |
| ELISA | Enzyme-Linked Immunosorbent Assay |
| EMSA | Electrophoretic Mobility Shift Assay |
| ERK | Extracellular Signal-regulated Kinase |
| FBS | Fetal Bovine Serum |
| FITC | Fluorescein Isothiocyanate |
| GADPH | Glyceraldehyde 3-Phosphate Dehydrogenase |
| GFAP | Glial Fibrillary Acidic Protein |
| IFN-γ | Interferon-γ |
| IL-1β | Interleukin-1β |
| IKK-α/β | IκB Kinase α/β |
| iNOS | Inducible Nitric Oxide Synthase |
| I/R | Ischemia/Reperfusion |
| IRF1 | Interferon Regulatory Factor 1 |
| JNK | c-Jun N-terminal Kinase |
| LDH | Lactate Dehydrogenase |
| LPS | Lipopolysaccharide |
| MAP-2 | Microtubule-associated Protein 2 |
| MCA | Middle Cerebral Artery |
| MPO | Myeloperoxidase |
| NLRP3 | NLR Family Pyrin Domain Containing 3 |
| NO | Nitric Oxide |
| P2X4R | P2X purinoceptor 4 |
| PGE2 | Prostaglandin E2 |
| RT-PCR | Reverse Transcriptase Polymerase Chain Reaction |
| Stat1 | Signal Transducers and Activators of Transcription 1 |
| TAK1 | Transforming Growth Factor β-Activated Kinase-1 |
| TBK1 | TANK-binding Kinase 1 |
| TCA | Trichloroacetic Acid |
| TLR | Toll-Like Receptor |
| TNF-α | Tumor Necrosis Factor-α |
| Tpl2 | Tumor Progression Locus 2 |
Author Contributions
C.-C.W., C.-Y.C., and C.-J.C. conceived and designed the experiments; K.-C.S., C.-J.H., Y.-Y.W., S.-Y.L., W.-Y.C., Y.-H.K., S.-L.L., and W.-Y.W. performed the experiments; C.-J.H., Y.-Y.W., and S.-Y.L. analyzed the data; C.-C.W. and C.-Y.C. wrote the paper; C.-J.C. edited the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by grants from Taichung Veterans General Hospital (TCVGH-1066301B), Taichung Veterans General Hospital and Hung Kuang University (TCVGH-HK1028003), the Central Region Hospital Alliance (Ministry of Health and Welfare), and Feng Yuan Hospital, Taiwan.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Stein C. Opioid receptors. Annu. Rev. Med. 2016;67:433–451. doi: 10.1146/annurev-med-062613-093100. [DOI] [PubMed] [Google Scholar]
- 2.Valentino R.J., Volkow N.D. Untangling the complexity of opioid receptor function. Neuropsychopharmacology. 2018;43:2514–2520. doi: 10.1038/s41386-018-0225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anttila J.E., Albert K., Wires E.S., Mätlik K., Loram L.C., Watkins L.R., Rice K.C., Wang Y., Harvey B.K., Airavaara M. Post-stroke intranasal (+)-naloxone delivery reduces microglial activation and improves behavioral recovery from ischemic injury. eNeuro. 2018;5:ENEURO.0395-17.2018. doi: 10.1523/ENEURO.0395-17.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bissonnette S., Vaillancourt M., Hébert S.S., Drolet G., Samadi P. Striatal pre-enkephalin overexpression improves Huntington’s disease symptoms in the R6/2 mouse model of Huntington’s disease. PLoS ONE. 2013;8:e75099. doi: 10.1371/journal.pone.0075099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bissonnette S., Muratot S., Vernoux N., Bezeau F., Calon F., Hébert S.S., Samadi P. The effect of striatal pre-enkephalin overexpression in the basal ganglia of the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson’s disease. Eur. J. Neurosci. 2014;40:2406–2416. doi: 10.1111/ejn.12596. [DOI] [PubMed] [Google Scholar]
- 6.Boutin H., Dauphin F., MacKenzie E.T., Jauzac P. Differential time-course decreases in nonselective, mu-, delta-, and kappa-opioid receptors after focal cerebral ischemia in mice. Stroke. 1999;30:1271–1277. doi: 10.1161/01.STR.30.6.1271. [DOI] [PubMed] [Google Scholar]
- 7.Lv M.R., Li B., Wang M.G., Meng F.G., Yu J.J., Guo F., Li Y. Activation of the PI3K-Akt pathway promotes neuroprotection of the d-opioid receptor agonist against cerebral ischemia-reperfusion injury in rat models. Biomed. Pharm. 2017;93:230–237. doi: 10.1016/j.biopha.2017.05.121. [DOI] [PubMed] [Google Scholar]
- 8.Sekine Y., Siegel C.S., Sekine-Konno T., Cafferty W.B.J., Strittmatter S.M. The nociceptin receptor inhibits axonal regeneration and recovery from spinal cord injury. Sci. Signal. 2018;11:eaao4180. doi: 10.1126/scisignal.aao4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheng S., Huang J., Ren Y., Zhi F., Tian X., Wen G., Ding G., Xia T.C., Hua F., Xia Y. Neuroprotection against hypoxic/ischemic injury: D-opioid receptors and BDNF-TrkB pathway. Cell Physiol. Biochem. 2018;47:302–315. doi: 10.1159/000489808. [DOI] [PubMed] [Google Scholar]
- 10.Fang S., Xu H., Lu J., Zhu Y., Jiang H. Neuroprotection by the kappa-opioid receptor agonist, BRL52537, is mediated via up-regulating phosphorylated signal transducer and activator of transcription-3 in cerebral ischemia/reperfusion injury in rats. Neurochem. Res. 2013;38:2305–2312. doi: 10.1007/s11064-013-1139-4. [DOI] [PubMed] [Google Scholar]
- 11.Kao T.K., Ou Y.C., Liao S.L., Chen W.Y., Wang C.C., Chen S.Y., Chiang A.N., Chen C.J. Opioids modulate post-ischemic progression in a rat model of stroke. Neurochem. Int. 2008;52:1256–1265. doi: 10.1016/j.neuint.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Brown J.N., Ortiz G.M., Angel T.E., Jacobs J.M., Gritsenko M., Chan E.Y., Purdy D.E., Murnane R.D., Larsen K., Palermo R.E., et al. Morphine produces immunosuppressive effects in nonhuman primates at the proteomic and cellular levels. Mol. Cell Proteom. 2012;11:605–618. doi: 10.1074/mcp.M111.016121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsai R.Y., Chou K.Y., Shen C.H., Chien C.C., Tsai W.Y., Huang Y.N., Tao P.L., Lin Y.S., Wong C.S. Resveratrol regulates n-methyl-d-aspartate receptor expression and suppresses neuroinflammation in morphine-tolerant rats. Anesth. Analg. 2012;115:944e52. doi: 10.1213/ANE.0b013e31825da0fb. [DOI] [PubMed] [Google Scholar]
- 14.Aceves M., Terminel M.N., Okoreeh A., Aceves A.R., Gong Y.M., Polanco A., Sohrabji F., Hook M.A. Morphine increases macrophages at the lesion site following spinal cord injury: Protective effects of minocycline. Brain Behav. Immun. 2019;79:125–138. doi: 10.1016/j.bbi.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 15.Gessi S., Borea P.A., Bencivenni S., Fazzi D., Varani K., Merighi S. The activation of m-opioid receptor potentiates LPS-induced NF-kB promoting an inflammatory phenotype in microglia. FEBS Lett. 2016;590:2813–2826. doi: 10.1002/1873-3468.12313. [DOI] [PubMed] [Google Scholar]
- 16.Liang Y., Chu H., Jiang Y., Yuan L. Morphine enhances IL-1b release through toll-like receptor 4-mediated endocytic pathway in microglia. Purinergic Signal. 2016;12:637–645. doi: 10.1007/s11302-016-9525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Merighi S., Gessi S., Varani K., Fazzi D., Stefanelli A., Borea P.A. Morphine mediates a proinflammatory phenotype via μ-opioid receptor-PKCε-Akt-ERK1/2 signaling pathway in activated microglial cells. Biochem. Pharm. 2013;86:487–496. doi: 10.1016/j.bcp.2013.05.027. [DOI] [PubMed] [Google Scholar]
- 18.Tsai R.Y., Cheng Y.C., Wong C.S. (+)-Naloxone inhibits morphine-induced chemotaxis via prevention of heat shock protein 90 cleavage in microglia. J. Med. Assoc. 2015;114:446–455. doi: 10.1016/j.jfma.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Davis R.L., Buck D.J., Saffarian N., Stevens C.W. The opioid antagonist, beta-funaltrexamine, inhibits chemokine expression in human astroglial cells. J. Neuroimmunol. 2007;186:141–149. doi: 10.1016/j.jneuroim.2007.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shrivastava P., Cabrera M.A., Chastain L.G., Boyadjieva N.I., Jabbar S., Franklin T., Sarkar D.K. Mu-opioid receptor and delta-opioid receptor differentially regulate microglial inflammatory response to control proopiomelanocortin neuronal apoptosis in the hypothalamus: Effects of neonatal alcohol. J. Neuroinflammation. 2017;14:83. doi: 10.1186/s12974-017-0844-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feng X., Wu C.Y., Burton F.H., Loh H.H., Wei L.N. b-arrestin protects neurons by mediating endogenous opioid arrest of inflammatory microglia. Cell Death Differ. 2014;21:397–406. doi: 10.1038/cdd.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu L., Xu Y., Dai H., Tan S., Mao X., Chen Z. Dynorphin activation of kappa opioid receptor promotes microglial polarization toward M2 phenotype via TLR4/NF-κB pathway. Cell Biosci. 2020;10:42. doi: 10.1186/s13578-020-00387-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu H.Y., Mao X.F., Tang X.Q., Ali U., Apryani E., Liu H., Li X.Y., Wang Y.X. Spinal interleukin-10 produces antinociception in neuropathy through microglial b-endorphin expression, separated from antineuroinflammation. Brain Behav. Immun. 2018;73:504–519. doi: 10.1016/j.bbi.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 24.Liao S.L., Chen W.Y., Raung S.L., Chen C.J. Neuroprotection of naloxone against ischemic injury in rats: Role of mu receptor antagonism. Neurosci. Lett. 2003;345:169–172. doi: 10.1016/S0304-3940(03)00540-8. [DOI] [PubMed] [Google Scholar]
- 25.Peyravian N., Dikici E., Deo S., Toborek M., Daunert S. Opioid antagonists as potential therapeutics for ischemic stroke. Prog. Neurobiol. 2019;182:101679. doi: 10.1016/j.pneurobio.2019.101679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X., Sun Z.J., Wu J.L., Quan W.Q., Xiao W.D., Chew H., Jiang C.M., Li D. Naloxone attenuates ischemic brain injury in rats through suppressing the NIK/IKKa/NF-kB and neuronal apoptotic pathways. Acta Pharm. Sin. 2019;40:170–179. doi: 10.1038/s41401-018-0053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davis R.L., Buck D.J., Saffarian N., Mohan S., DeSilva U., Fernando S.C., Stevens C.W. Beta-funaltrexamine inhibits inducible nitric-oxide synthase expression in human astroglial cells. J. Neuroimmune Pharm. 2008;3:150–153. doi: 10.1007/s11481-008-9102-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davis R.L., Das S., Buck D.J., Stevens C.W. β-funaltrexamine inhibits chemokine (CXCL10) expression in normal human astrocytes. Neurochem. Int. 2013;62:478–485. doi: 10.1016/j.neuint.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davis R.L., Das S., Thomas Curtis J., Stevens C.W. The opioid antagonist, β-funaltrexamine, inhibits NF-κB signaling and chemokine expression in human astrocytes and in mice. Eur. J. Pharm. 2015;762:193–201. doi: 10.1016/j.ejphar.2015.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davis R.L., Stevens C.W., Thomas Curtis J. The opioid antagonist, b-funaltrexamine, inhibits lipopolysaccharide-induced neuroinflammation and reduces sickness behavior in mice. Physiol. Behav. 2017;173:52–60. doi: 10.1016/j.physbeh.2017.01.037. [DOI] [PubMed] [Google Scholar]
- 31.Chen W.Y., Chang C.Y., Li J.R., Wang J.D., Wu C.C., Kuan Y.H., Liao S.L., Wang W.Y., Chen C.J. Anti-inflammatory and neuroprotective effects of fungal immunomodulatory protein involving microglial inhibition. Int. J. Mol. Sci. 2018;19:E3678. doi: 10.3390/ijms19113678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al Mamun A., Chauhan A., Yu H., Xu Y., Sharmeen R., Liu F. Interferon regulatory factor 4/5 signaling impacts on microglial activation after ischemic stroke in mice. Eur. J. Neurosci. 2018;47:140–149. doi: 10.1111/ejn.13778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rossetti I., Zambusi L., Finardi A., Bodini A., Provini L., Furlan R., Morara S. Calcitonin gene-related peptide decreases IL-1beta, IL-6 as well as Ym1, Arg1, CD163 expression in a brain tissue context-dependent manner while ameliorating experimental autoimmune encephalomyelitis. J. Neuroimmunol. 2018;323:94–104. doi: 10.1016/j.jneuroim.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 34.Chen C.J., Raung S.L., Liao S.L., Chen S.Y. Inhibition of inducible nitric oxide synthase expression by baicalein in endotoxin/cytokine-stimulated microglia. Biochem. Pharm. 2004;67:957–965. doi: 10.1016/j.bcp.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 35.Hsu Y.Y., Jong Y.J., Lin Y.T., Tseng Y.T., Hsu S.H., Lo Y.C. Nanomolar naloxone attenuates neurotoxicity induced by oxidative stress and survival motor neuron protein deficiency. Neurotox. Res. 2014;25:262–270. doi: 10.1007/s12640-013-9414-3. [DOI] [PubMed] [Google Scholar]
- 36.Tian X., Guo J., Zhu M., Li M., Wu G., Xia Y. d-Opioid receptor activation rescues the functional TrkB receptor and protects the brain from ischemia-reperfusion injury in the rat. PLoS ONE. 2013;8:e69252. doi: 10.1371/journal.pone.0069252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang Z., Chen T.Y., Kirsch J.R., Toung T.J., Traystman R.J., Koehler R.C., Hurn P.D., Bhardwaj A. Kappa-opioid receptor selectivity for ischemic neuroprotection with BRL 52537 in rats. Anesth. Analg. 2003;97:1776–1783. doi: 10.1213/01.ANE.0000087800.56290.2E. [DOI] [PubMed] [Google Scholar]
- 38.Bok E., Chung Y.C., Kim K.S., Baik H.H., Shin W.H., Jin B.K. Modulation of M1/M2 polarization by capsaicin contributes to the survival of dopaminergic neurons in the lipopolysaccharide-lesioned substantia nigra in vivo. Exp. Mol. Med. 2018;50:76. doi: 10.1038/s12276-018-0111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chang C.Y., Kuan Y.H., Li J.R., Chen W.Y., Ou Y.C., Pan H.C., Liao S.L., Raung S.L., Chang C.J., Chen C.J. Docosahexaenoic acid reduces cellular inflammatory response following permanent focal cerebral ischemia in rats. J. Nutr. Biochem. 2013;24:2127–2137. doi: 10.1016/j.jnutbio.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 40.Ślusarczyk J., Trojan E., Głombik K., Piotrowska A., Budziszewska B., Kubera M., Popiołek-Barczyk K., Lasoń W., Mika J., Basta-Kaim A. Targeting the NLRP3 Inflammasome-related pathways via tianeptine treatment-suppressed microglia polarization to the M1 phenotype in lipopolysaccharide-stimulated cultures. Int. J. Mol. Sci. 2018;19:1965. doi: 10.3390/ijms19071965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Velagapudi R., Jamshaid F., Lepiarz I., Katola F.O., Hemming K., Olajide O.A. The tiliroside derivative, 3-O-[(E)-(2-oxo-4-(p-tolyl) but-3-en-1-yl] kaempferol produced inhibition of neuroinflammation and activation of AMPK and Nrf2/HO-1 pathways in BV-2 microglia. Int Immunopharmacol. 2019;77:105951. doi: 10.1016/j.intimp.2019.105951. [DOI] [PubMed] [Google Scholar]
- 42.Kao T.K., Chang C.Y., Ou Y.C., Chen W.Y., Kuan Y.H., Pan H.C., Liao S.L., Li G.Z., Chen C.J. Tetramethylpyrazine reduces cellular inflammatory response following permanent focal cerebral ischemia in rats. Exp. Neurol. 2013;247:188–201. doi: 10.1016/j.expneurol.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 43.Kaserer T., Lantero A., Schmidhammer H., Spetea M., Schuster D. m Opioid receptor: Novel antagonists and structural modeling. Sci. Rep. 2016;6:21548. doi: 10.1038/srep21548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tangherlini G., Kalinin D.V., Schepmann D., Che T., Mykicki N., Ständer S., Loser K., Wünsch B. Development of novel quinoxaline-based κ-opioid receptor agonists for the treatment of neuroinflammation. J. Med. Chem. 2019;62:893–907. doi: 10.1021/acs.jmedchem.8b01609. [DOI] [PubMed] [Google Scholar]
- 45.Lee C.W., Muo C.H., Liang J.A., Sung F.C., Kao C.H. Association of intensive morphine treatment and increased stroke incidence in prostate cancer patients: A population-based nested case-control study. Jpn. J. Clin. Oncol. 2013;43:776–781. doi: 10.1093/jjco/hyt080. [DOI] [PubMed] [Google Scholar]
- 46.Kao T.K., Ou Y.C., Kuo J.S., Chen W.Y., Liao S.L., Wu C.W., Chen C.J., Ling N.N., Zhang Y.H., Peng W.H. Neuroprotection by tetramethylpyrazine against ischemic brain injury in rats. Neurochem. Int. 2006;48:166–176. doi: 10.1016/j.neuint.2005.10.008. [DOI] [PubMed] [Google Scholar]