Abstract
Background: The aim of this study is to evaluate the association between heart rate turbulence (HRT) parameters and clinical characteristics of coronary artery disease (CAD) patients.
Methods and Results: In 122 patients (mean age 62 ± 9 years) with angiographically documented CAD, 24‐hour Holter monitoring with HRT analysis was performed to evaluate turbulence onset (TO) and turbulence slope (TS). There was a significant correlation between TO and TS (P =−0.31; P < 0.001). According to quartile values, TO ≥−0.37% and TS ≤ 4.25 ms/RR were considered as abnormal in this patient population. Average values of TO were higher and TS lower in patients over 60 years, in patients with a past history of myocardial infarction and in those with EF < 40%. Considering pharmacotheraphy, higher (better) values of TS were observed in patients on statins, nitrates, and beta‐blockers while lower TS values were noted in patients on calcium blockers. Patients with abnormal parameters of HRT compared to group with normal HRT values were characterized by features of more advanced CAD: age over 60 years (75% vs 49%), past history of MI (75% vs 64%), and EF < 40% (25% vs 3%). Multivariate analysis revealed age > 60 years (OR 1.27; P = 0.002) and EF < 40% (OR 1.39; P = 0.001) as independent clinical factors associated with abnormal HRT parameters.
Conclusions: HRT parameters are influenced by clinical characteristics and pharmacotherapy of studied patients with TS more than abnormal TO depending on clinical characteristics of patients. Advanced age, prior myocardial infarction and left ventricular dysfunction are key factors influencing values of HRT parameters.
Keywords: heart rate turbulence, coronary artery disease, Holter monitoring
Sudden cardiac death is one of the leading causes of death among patients with coronary artery disease. 1 Various predictors of cardiac death have been introduced into clinical practice to find the best selection of patients at high risk of sudden death, who may benefit from preventive treatment such as revascularization, pharmacotheraphy or implantable cardioverter‐defibrillators. 2 , 3 In 1999 Schmidt et al. 4 proposed heart rate turbulence (HRT) as a new, promising method to identify patients at increased risk of cardiac death. HRT is a physiological phenomenon consisting of an early acceleration and subsequent deceleration of a sinus rhythm after a VPB. This fluctuation of sinus rhythm is triggered by a transient drop in arterial pressure provoked by a VPB and this reaction is believed to be mediated by baroreceptors. 5 The presence of the evident acceleration and deceleration of sinus rhythm in response to a VPB represents normal HRT observed in healthy subjects and patients without abnormal baroreflex response. In patients at increased risk of cardiac death, the response of sinus rhythm to a VPB is blunted or there is no response at all. 4
HRT analysis is a new method; thus, data concerning the relationship between HRT parameters and clinical covariates are limited. So far HRT and its predictive value has been evaluated in retrospective databases of patients in early postinfarction period from three large studies: MPIP, EMIAT and ATRAMI. 4 , 6 These studies concentrated on the predictive value of HRT parameters and did not focus on analyzing the clinical dependence of HRT parameters. Therefore, the aim of this study is to evaluate clinical covariates of abnormal HRT parameters in patients with multivessel CAD who were studied prior to elective coronary artery bypass grafting (CABG).
METHODS
Study Population
The study population consisted of 146 consecutive patients (117 men and 29 women) aged 38–78 years (mean 62) with angiographically documented multivessel CAD who were qualified to have elective CABG surgery. Exclusion criteria were as follows: nonsinus rhythm (atrial fibrillation and paced rhythm), coexisting valvular heart disease, unstable angina, myocardial infarction (MI) less than 3 months prior to CABG, heart failure symptoms >NYHA (New York Heart Association) III Class. The study protocol was approved by local Human Investigation Committee and all patients signed informed consent.
In all the patients, data on demographics (age, sex), clinical characteristics (post‐MI, ejection fraction, diabetes, hypertension, obesity, smoking, lipid profile, family history of coronary disease) and medication were acquired.
Heart Rate Turbulence
Twenty‐four‐hour Holter ECG monitoring was performed using 3‐channel analogue recorders and analyzed using Oxford Medilog System (Oxford, UK) to evaluate the presence of ventricular arrhythmias and calculate HRT parameters; the latter only in patients with ventricular arrhythmias.
HRT parameters were calculated using an algorithm adapted from the web page popularizing the noncommercial use of HRT. In HRT analysis two numerical descriptors were estimated: Turbulence onset (TO) reflecting the initial phase of sinus rhythm acceleration and turbulence slope (TS) describing deceleration phase. TO was defined as a percentage difference between the mean of first two R‐R intervals after a VPB and the last two sinus R‐R intervals before a VPB. TS was described as a maximum positive slope of a regression line assessed over any of five consecutive R‐R intervals within the first 20 sinus R‐R intervals after a VPB. TO was calculated for all VPBs separately and then averaged while TS was calculated based on an averaged local tachogram. Filtering algorithms were used to eliminate inappropriate R‐R intervals and VPBs with too long coupling intervals or too short compensatory pause.
Filtering algorithms excluded from the HRT calculation R‐R intervals with the following characteristics: <300 ms, >2000 ms, >200 ms difference to the preceding sinus interval, and >20% difference to the reference interval (mean of the five last sinus intervals). Additionally, these algorithms limit the HRT calculations to VPBs with a minimum prematurity of 20% and a postextrasystole interval which is at least 20% longer than the normal interval.
Abnormal Values of HRT Parameters
TO and TS were defined as abnormal values according to quartile division in the studied population: TO values from the upper quartile and TS values from the lower quartile. We chose our own definition of abnormal values since previously proposed cut‐offs were designed using patients exclusively in the early postinfarction period. When using both HRT parameters simultaneously, patients were categorized as having both HRT parameters normal, one HRT parameter abnormal and both HRT parameters abnormal, similarly to other studies. Furthermore, in a group of patients with one HRT parameters abnormal the distinction between patients with abnormal TO and those with abnormal TS was done.
Statistical Analysis
All continuous variables are expressed as a mean ± SD for normally distributed data and as a median for variables with nonnormal (skewed) distribution. Univariate comparisons of data between patients with normal and abnormal HRT values were performed using the t‐test, Mann‐Whitney test and the chi‐square analysis, where appropriate. Multivariate regression analyses were performed to determine the associations between HRT parameters and clinical covariates. TS and TO were analyzed separately as well as in combination. P value < 0.05 was considered statistically significant. Bonferroni's correction was used for comparisons between three studied subgroups (P < 0.017 was considered statistically significant).
RESULTS
Clinical Characteristics of Studied Patients and Heart Rate Turbulence Analysis
The study population consisted of 146 consecutive patients (117 men and 29 women) aged 38– 78 years (mean 62 ± 9). Most of the patients (70%) had a past history of MI (39 patients with Q wave MI; 59 with anterior MI and 64 with inferior MI). Left ventricle ejection fraction assessed by echocardiography varied from 33% to 74%, av. 54% (10 patients with EF < 40%). There were 33 (23%) diabetics and 89 (61%) patients with hypertension. There were 23 (16%) current and 41 (28%) past smokers. Most of the patients were overweight (BMI > 30 kg/ m2 in 22 patients). All patients were in a stable stage according to CCS and NYHA classifications.
Critical coronary artery stenosis (defined as over 75% of vessel diameter stenosis for major arteries and over 50% for left main artery on angiography) were found in: left main artery in 8 (6%) patients, in 2 vessels in 9 (6%) and in >3 vessels in 129 (88%) patients. Patients were treated with beta blockers (84%), calcium channel blockers (14%), ACE inhibitors (41%), statins (79%) and nitrates (94%). During Holter recordings performed few days prior to CABG, no medication was withdrawn.
Heart Rate Turbulence Analysis
In a group of 146 patients initially enrolled into the study, HRT parameters were calculated in 122 (84%) patients. In 15 patients no ventricular beats were found, in additional 9 patients filtering HRT algorithms eliminated VPBs. HRT parameters showed broad spectrum of values: TO ranging from −8.3% to +4.45%, mean ± SD: −1.29 ± 1.63 with normal distribution and TS from 0.42 to 54.7ms/R‐R, mean ± SD = 11.29 ± 10.34 (median 8.24) with markedly skewed distribution. According to their quartile values, TO ≥−0.37% (fourth quartile cut‐off) and TS ≤ 4.25 ms/RR (first quartile cut‐off) were considered abnormal. There was a significant correlation between TO and TS (Fig. 1; r =−0.31; P < 0.001).
Figure 1.
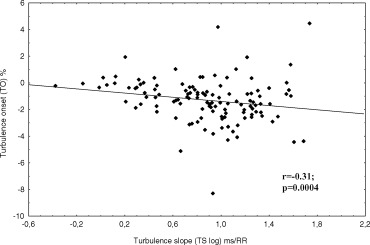
Correlation between turbulence onset (TO) and turbulence slope (TS) values (TS expressed in logarithmic scale due to skewed distribution).
There were 30 (25%) of 122 patients with abnormal TO or TS, while in 16 (13%) patients both TO and TS were found abnormal. Both HRT parameters were normal in remaining 76 patients. When dichotomizing patients according to abnormal values proposed by Schmidt et al. 4 : TO > 0% and TS <2.5 ms/RR, 26 (19%) patients had 1 HRT parameter abnormal, while 5 (4%) patients had both TO and TS abnormal.
Levels of HRT Parameters in Clinical Subgroups
Although, no statistical difference between males and females was found women had somewhat higher TO values (Table 2). Both TO and TS significantly correlated with age: TO displayed positive (r = 0.17; P = 0.05) while TS negative (r =−0.25; P = 0.005) correlation with age (Fig. 2). Post‐MI patients had significantly higher TO values (−0.99 vs −1.60%), while no difference in TS values was observed. Patients with decreased left ventricle ejection fraction (<40%) showed higher TO and lower TS values. Average values of TO were higher and TS lower in patients over 60 years, with MI past history, and in those with EF < 40%. Diabetes predisposed to lower TS values.
Table 2.
Median Values of TO and TS Depending on Clinical Characteristics
| Clinical Covariates | Group | TO (%) | P | TS (ms/RR) | P | ||
|---|---|---|---|---|---|---|---|
| Age (years) | >60 | −1.07 | 0.11 | 7.08 | 0.12 | ||
| <60 | −1.50 | 8.60 | |||||
| Gender | F | −1.01 | 0.50 | 8.56 | 0.89 | ||
| M | −1.30 | 8.15 | |||||
| Prior MI | (+) | −0.99 | 0.007 | 8.13 | 0.54 | ||
| (−) | −1.60 | 8.53 | |||||
| EF < 40% | (+) | −0.36 | 0.04 | 2.32 | 0.04 | ||
| (−) | −1.31 | 8.54 | |||||
| Diabetes | (+) | −1.08 | 0.64 | 5.82 | 0.12 | ||
| (−) | −1.40 | 8.53 | |||||
| Hypertension | (+) | −1.16 | 0.42 | 8.15 | 0.69 | ||
| (−) | −1.27 | 8.24 | |||||
| Smoking | (+) | −1.29 | 0.62 | 7.82 | 0.97 | ||
| (−) | −1.16 | 8.07 | |||||
| BMI > 25 kg/m2 | (+) | −1.36 | 0.10 | 8.15 | 0.59 | ||
| (−) | −0.88 | 8.90 | |||||
| Beta‐blockers | (+) | −1.28 | 0.68 | 8.57 | 0.03 | ||
| (−) | −1.15 | 5.62 | |||||
| Calcium blockers | (+) | −1.07 | 0.99 | 5.23 | 0.30 | ||
| (−) | −1.27 | 8.33 | |||||
| ACE inhibitors | (+) | −1.11 | 0.95 | 7.56 | 0.49 | ||
| (−) | −1.38 | 8.40 | |||||
| Statins | (+) | −1.30 | 0.30 | 8.75 | 0.02 | ||
| (−) | −0.98 | 5.23 | |||||
| Nitrates | (+) | −1.28 | 0.30 | 8.53 | 0.06 | ||
| (−) | −0.72 | 4.50 |
Variables with significant (p < 0.05) differences in HRT parameters between respective subgroups are in bold.
Abbreviations as in text.
Figure 2.
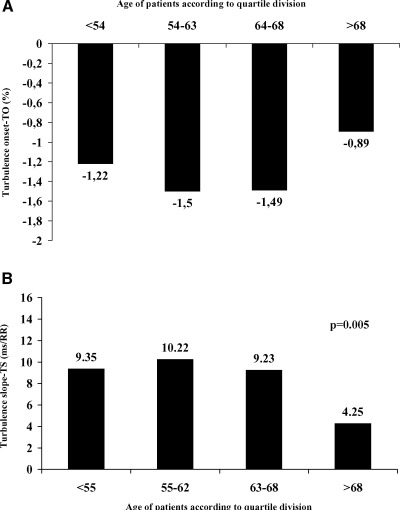
The Association between Age and HRT Parameters: A. Median of turbulence onset (TO) according to age quartile. B. Median of turbulence slope (TS) according to age quartile. P value calculated for trend.
Considering pharmacotheraphy, higher values of TS were observed in patients on statins, nitrates and beta‐blockers while lower TS values were observed in patients on calcium blockers (Table 2).
Univariate and Multivariate Analyses of Clinical Covariates of Abnormal HRT
Patients with abnormal parameters of HRT compared to a group with normal HRT values were older and characterized by feature of more advanced CAD: age over 60 years (75% vs 49%), MI past history (75% vs 64%) and EF < 40% (25% vs 3%). Multivariate analysis revealed age > 60 years (OR 1.27, P = 0,002) and EF < 40% (OR 1.39, P = 0.001) as independent factors associated with abnormal HRT parameters. Considering pharmacotheraphy patients with normal HRT values were more frequently treated with beta‐blockers, statins and nitrates (Table 3). To assess which of the two HRT parameter is more dependent on clinical covariates an additional uni‐ and multivariate analysis in subgroups of patients with one abnormal (TO or TS) HRT parameters was performed. This analysis revealed more advanced CAD features in patients with abnormal TS compared to those with abnormal TO (Table 4).
Table 3.
Clinical Characteristics of Coronary Patients with Abnormal One or Two HRT Parameters in Univariate and Multivariate Analysis
| Univariate Analysis | |||||||
|---|---|---|---|---|---|---|---|
| Multivariate Analysis | |||||||
| Group A | Group B | Group C | |||||
| TO and TS | TO or TS | TO and TS | B vs A | C vs A | |||
| Normal | Abnormal | Abnormal | |||||
| (n = 76) | (n = 30) | (n = 16) | OR | P | OR | P | |
| Age (years) | 60 ± 8 | 64 ± 16a | 66 ± 8a | ||||
| Age > 60 years | 37 (49%) | 21(70%)a | 12 (75%)a | 1.29 | 0.007 | 1.27 | 0.002 |
| Females | 12 (16%) | 5 (17%) | 4 (25%) | ||||
| Diabetes | 18 (24%) | 6 (20%) | 6 (37%) | ||||
| Hypertension | 47 (63%) | 18 (60%) | 11 (69%) | ||||
| MI | 48 (64%) | 23 (76%) | 12 (75%) | ||||
| EF mean (%) | 52 ± 10 | 52 ± 9 | 48 ± 8 | ||||
| EF < 40% | 2 (3%) | 3 (10%) | 4 (25%) | 1.39 | 0.001 | ||
| Beta blockers | 66 (88%) | 25 (83%) | 14 (87%) | ||||
| Calcium blockers | 7 (9%) | 5 (17%) | 3 (18%) | ||||
| Statins | 64 (85%) | 21 (70%)b | 11 (69%) | 0.83 | 0.004 | 0.8 | 0.02 |
| ACE inhibitors | 31 (41%) | 8 (26%) | 11 (69%) | ||||
| Nitrates | 73 (97%) | 27 (90%) | 15 (94%) | 1.17 | 0.08 | ||
a P < 0.017; bP = 0,07 when comparing to Group A. OR: odds ratio; MI: myocardial infarction; EF: ejection fraction.
Abbrevations as in text.
Table 4.
Clinical Characteristics of Coronary Patients with Abnormal Single HRT Parameter in Univariate and Multivariate Analysis
| Univariate Analysis | |||||||
|---|---|---|---|---|---|---|---|
| Multivariate Analysis | |||||||
| Group A | |||||||
| To i Ts | Group D | Group E | D vs A | E vs A | |||
| Normal | To Abnormal | Ts Abnormal | |||||
| (n = 76) | (n = 15) | (n = 15) | OR | P | OR | P | |
| Age (years) | 60 ± 8 | 64 ± 8a | 64 ± 9a | ||||
| Age > 60 years | 37 (49%) | 11 (73%)a | 10 (67%)a | 1.23 | 0.005 | 1.27 | 0.02 |
| Females | 12 (16%) | 3 (20%) | 2 (13%) | ||||
| Diabetes | 18 (24%) | 2 (13%) | 4 (27%) | ||||
| Hypertension | 47 (63%) | 8 (53%) | 10 (67%) | ||||
| MI | 48 (64%) | 13 (87%) | 10 (67%) | ||||
| EF (%) | 52 ± 10 | 52 ± 7 | 51 ± 10 | ||||
| EF < 40% | 2 (3%) | 1 (7%) | 2 (13%) | ||||
| Beta‐blockers | 66 (88%) | 14 (93%) | 11 (73%) | ||||
| Calcium blockers | 7 (9%) | 1 (7%) | 4 (27%) | ||||
| Statins | 64 (85%) | 11 (73%) | 10 (67%) | 0.82 | 0.04 | ||
| ACE inhibitors | 31 (41%) | 4 (26%) | 5 (33%) | ||||
| Nitrates | 73 (97%) | 14 (93%) | 13 (86%) | 0.82 | 0.05 | ||
aP < 0.017 when comparing to Group A. OR: odds ratio; MI: myocardial infarction; EF: ejection fraction.
Abbreviations as in text.
DISCUSSION
HRT, recently described as a new ECG predictor of cardiac death, is considered to reflect baroreflex response. 4 , 5 Baroreceptors localized in aortic arch and carotic sinus constitute one of the basic mechanism of heart rate and blood pressure control. They are constantly stimulated by tonic arterial blood pressure being more responsive to sudden hypotonia than to an increase in blood pressure. 7 Baroreceptors sensitivity (BRS) could be studied using invasive and noninvasive methods. The prognostics value of phenylephrine test (invasive pharmacological stimulation of alpha receptors) is high, although its use in clinical practice remains limited. 8 HRT, as a noninvasive method of BRS evaluation, is likely to be used more commonly than phenylephrine test.
In our study, HRT parameters were evaluated in 122 coronary patients. Abnormal HRT parameters were found in 38% patients, that indicates a high incidence of baroreflex dysfunction in coronary patients. HRT parameters were found significantly worsened with age, especially in subjects above 68 years. Age‐related decrease in BRS sensitivity is considered to be an effect of a reduced arterial compliance. 9 In our study, diabetes, past history of MI, and decreased ejection fraction have also predisposed to worsened HRT parameters. While analyzing pharmacotherapy, HRT parameters showed better values in patients treated with beta‐blockers, statins and nitrates. It was postulated that when comparing to heart rate variability parameters, HRT remains a significant risk stratifier in patients on beta‐blockers. 10 The favorable effect of beta‐blockers on HRT could be explained by its influence on sympathovagal balance. 11 The positive influence of statins on HRT might be mediated by an increase of arterial walls compliance, while the influence of nitrates by its direct endothelial effect and blood pressure decrease. 12 , 13 The effect of drugs on HRT parameters requires further studies with patients being his/her own control with HRT parameters calculated before and on drugs.
HRT is a new method, thus it is uncertain what values of HRT parameters should be considered as abnormal. Abnormal HRT values proposed by the authors of the method (TO ≥ 0% and TS ≤ 2.5 ms/RR), possessing high predictive value of cardiac death risk, however, were based on populations of early postinfarction patients from 1980s and early 1990s. Our studied group consisted of patients with chronic CAD who were treated according to new standards including trombolysis and primary angioplasty procedures. Thus, we considered high risk quartile as abnormal values instead of the above values relevant for early postinfarction period. Abnormal values were observed in 38% of patients. While dichotomizing according to more strict values by Schmidt et al., 4 abnormal values of HRT were found in 23% patients.
TS and TO correlate with each other (Fig. 1). Among two HRT parameters TS is more dependent on clinical characteristics of patients and simultaneously it is believed to better reflect baroreceptors sensitivity. 14 Davies et al. 14 demonstrated TS as the predominant HRT parameter reflecting baroreflex sensitivity. It might be explained by a fact that TS better than TO reflects dynamicity of RR changes.
In conclusion, abnormal values of HRT are observed in about one‐third of coronary patients indicating that abnormalities of baroreceptor function are quite common in this patient population. Age and clinical covariates influencing regulation of the heart by the autonomic nervous system (prior MI, diabetes, left ventricular dysfunction) as well as pharmacotheraphy might influence values of HRT parameters. Therefore, when analyzing prognostic significance of HRT parameters it is necessary to adjust for clinical covariates. Treatment with statins, beta‐blockers and nitrates seem to ameliorate HRT parameters, most likely through modification of baroreflex sensitivity. Our data also indicate that TS more than TO is dependent on clinical characteristics; what remains in agreement is that TS seems to better reflect baroreflex sensitivity than TO.
REFERENCES
- 1. Priori SG, Aliot E, Blomstrom–Lundqvist C, et al Task Force on Sudden Cardiac Death, European Society of Cardiology. Eur Heart J 2001;22: 1374–1450. [DOI] [PubMed] [Google Scholar]
- 2. Moss AJ. Noninvasive ECG testing in patients with chronic coronary artery disease patients In Zareba W, Maison‐ Blanche P, Locati E, (eds.). Noninvasive Electrocardiology in Clinical Practice. Armonk , NY , Futura Publishing Company, 2001, pp 373–392. [Google Scholar]
- 3. Huikuri HV, Castellanos A, Myerburg RJ. Sudden death due to cardiac arrhythmias. N Engl J Med 2001;345: 1473–1482. [DOI] [PubMed] [Google Scholar]
- 4. Schmidt G, Malik M, Barthel P, et al Heart‐rate turbulence after VPBs as a predictor of mortality after acute myocardial infarction. Lancet 1999;353: 1390–1396. [DOI] [PubMed] [Google Scholar]
- 5. Mrowka R, Persson PB, Theres H, et al Blunted arterial baroreflex causes “pathological” heart rate turbulence. Am J Physiol Regulatory Integrative Comp Physiol 2000;279: R1171–R1175. [DOI] [PubMed] [Google Scholar]
- 6. Ghuran A, Reid F, La Rovere MT, et al The ATRAMI Investigators. Heart rate turbulence‐based predictors of fatal and nonfatal cardiac arrest (The Autonomic Tone and Reflexes after Myocardial Infarction substudy). Am J Cardiol 2002;89: 184–190. [DOI] [PubMed] [Google Scholar]
- 7. La Rovere MT, Maestri R, Mortara A. Baroreflex sensitivity In Zareba W, Maison‐Blanche P, Locati EH. (eds.) Noninvasive Electrocardiology in Clinical Practice. Armonk , NY , Futura Publishing Company, 2001, pp 181–205. [Google Scholar]
- 8. La Rovere MT, Bigger JT Jr, Marcus FI, et al Baroreflex sensitivity and heart rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes after Myocardial Infarction) Investigators. Lancet 1998;351: 478–484. [DOI] [PubMed] [Google Scholar]
- 9. Monahan KD, Dinenno FA, Seals DR, et al Age‐associated changes in cardiovagal baroreflex sensitivity are related to central arterial compliance. Am J Physiol Heart Circ Physiol 2001;281: H284–H289. [DOI] [PubMed] [Google Scholar]
- 10. Schmidt G, Malik M. Heart rate turbulence In Zareba W, Maison‐Blanche P, Locati EH. (eds.): Noninvasive Electrocardiology in Clinical Practice. Armonk , NY , Futura Publishing Company, 2001, pp 207–216. [Google Scholar]
- 11. Wikstrand J, Kendall M. The role of beta receptor blockade in preventing sudden death. Eur Heart J 1992;13(suppl D): 111–120. [PubMed] [Google Scholar]
- 12. Liao JK. Beyond lipid lowering: The role of statins in vascular protection. Int J Cardiol 2002, 86: 5–18. [DOI] [PubMed] [Google Scholar]
- 13. Gewaltig MT, Kojda G. Vasoprotection by nitric oxide: Mechanisms and therapeutical potential. Cardiovasc Res 2002, 55: 250–260. [DOI] [PubMed] [Google Scholar]
- 14. Davies LC, Francis DP, Ponikowski P, et al Relation of heart rate and blood pressure turbulence following premature ventricular complexes to baroreflex sensitivity in chronic congestive heart failure. Am J Cardiol 2001;87: 737–742. [DOI] [PubMed] [Google Scholar]


