Abstract
Objective: We aimed to examine the outcomes of our novel multicomponent lower extremity training (MLT) technique on physical function in older adults. Methods: Participants were randomly divided into a training group (TG) or a control group (CG). The TG (4 men, 14 women) received MLT for 24 weeks, once per week. MLT contains strength, balance, and flexibility components. The CG (5 men, 10 women) did not receive any training for 24 weeks. Nine lower extremity range of motions (ROMs; hip flexion, hip abduction, hip adduction, hip extension, internal and external hip rotations, knee flexion, ankle dorsiflexion, and ankle plantar flexion) and two muscle strength assessments (knee extension and flexion) were collected. Physical performance tests were also performed, including the functional reach test, timed up and go test (TUGT), and five times sit-to-stand test (FTSST). Results: After 24 weeks, significant increases were observed in the TG in all ROMs (with the exception of knee flexion), knee extension strength, and performance in the TUGT and FTSST. Conclusions: MLT significantly improved ROM, muscle strength, and physical performance in healthy older adults. We suggest that it is an efficacious intervention in the maintenance and improvement of mobility and functional independence in healthy older adults.
Trial registration: UMIN CTR, UMIN000037463. https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000041955
Keywords: exercise, lower extremity, older adults, range of motion, strength
Introduction
Age-related reductions in lower extremity function are related to multiple health problems, including fractures and physical frailty. As a result, lower extremity function can result in a loss of independence, a decrease in quality of life, and increased mortality rates (Grimmer et al., 2019). Ding and Yang (2016) indicated that decreased knee strength could contribute to unsuccessful recovery rates due to a fall and could lead to an unexpected loss of balance during walking. Decreased lower extremity range of motion (ROM) was also found in older adults who experienced a fall within the past year (Gehlsen & Whaley, 1990). In addition, a reduction in physical performance capacity, including decreased mobility and limited balance, was detected in frail older adults (Zhong et al., 2018). Therefore, it is necessary to implement exercise training to improve lower extremity function in older adults.
Klein et al. (2002) reported on the use of a proprioceptive neuromuscular facilitation (PNF) intervention in assisted-living older adults, which consisted of both strength and flexibility components. In that study, there was an improvement in ROM, isometric strength, and several physical function tasks. Although PNF does not require weight machines, it is expensive to hire qualified personal trainers who offer one-on-one training for the technique (Klein et al., 2002). Furthermore, Pilates has been shown to improve ROM, postural balance, and muscle strength (Oliveira et al., 2015, 2016) but also requires sessions twice a week and/or expensive equipment (e.g., Trapeze, Reformer, and Ladder Barrel) for older adults. To the best of our knowledge, there are few exercise interventions by one instructor, without equipment, with muscle strengthening in concurrence with stretching, at a low frequency (less than 2 times per week), which may result in simultaneously improved ROM, muscle strength, and physical performance ability of older adults.
We excogitated a multicomponent lower extremity training (MLT) model for older adults, whose component exercises were almost all developed by the current authors. Those exercises did not involve movements in PNF or Pilates. MLT was designed to satisfy the following conditions: (a) provide progressive strength, balance, and flexibility exercises; (b) provide a cost-effective exercise program led by one trained exercise instructor; (c) induce improvements in lower extremity function; (d) provide an appropriately intense stimulus while facilitating muscle activation by stretching agonist muscles and/or their surrounding muscles; (e) not require any expensive equipment; and (f) provide training exercises once per week. As such, the purpose of this study was to examine the impact of MLT on physical function in older adults by assessing ROM, muscle strength, and physical performance ability. We hypothesized that our MLT technique would lead to improvements in physical function of older adults.
Method
Trial Design
This study was approved by the ethical committee of the Graduate School of Integrated Arts and Science of Hiroshima University (ID: 26-32). This study was a randomized controlled trial.
Participants
Participants were recruited in Higashi-Hiroshima City, Hiroshima, Japan, with the assistance of public community centers through various methods (e.g., fliers, posters, or seminars related to physical ability of older adults). The eligibility criteria for participation in the study were as follows: (a) age ≥65 years; (b) living independently in the community; (c) the ability to perform activities of daily living without assistance; (d) no cognitive impairment that could impact understanding of the written informed consent; (e) no serious neurological, musculoskeletal, visual, sensory, or cognitive disorders diagnosed by clinicians that could preclude voluntary participation in a weekly group exercise program; and (f) no use of walking aids (e.g., a cane, walker, or crutches). Prior to entering into the study, the purpose and procedures of this study were explained to all participants. All participants provided written informed consent.
Sample Size
To determine the sample size of the study, we considered a calculated sample size (n = 14, in each group) based on effect size = 1.3, power = 0.95, and α-error = .05 (Marques et al., 2016). The sample numbers increased by more than 14 for each group to accommodate for unintended dropouts.
Randomization and Blinding
All participants were randomly separated into either a training group (TG) or a control group (CG) using a computerized program to randomly generate the number 1 (the TG) or 2 (the CG) by an individual independent of the investigators. The staff who performed the trial measurements were blinded to the study group assignment, and the same staff measured each test at baseline and after 24 weeks.
Intervention: MLT
The participants in the TG received 60-min exercise sessions once per week, for 24 weeks, in community centers. Only one set of all exercises was utilized, with a 1-min break between the exercises. The trainer performed a sample of each exercise in front of all participants, along with a verbal explanation of the movement. Then, the trainer corrected any errors in each participant’s movement while the participant was performing the exercise.
The participants performed a standard sequence of MLT (Table 1). MLT progresses from non-weight-bearing exercises to weight-bearing exercises, and the protocol is divided into three steps. In the second and third steps, new exercises were added to increase the intensity, excluding exercises performed in the previous step when the targeted muscle groups overlapped.
Table 1.
Sequence of Exercises in MLT.
| The first step | 1a | 1b | 1c | 1d | 1e | 1f | 1g | 1h | 1i | 1j | 2a | 2b | 2c | 2d | 2e | 2f | 2g | 2h | 2i | 2j | |||||||||||
| (1–8 weeks) | |||||||||||||||||||||||||||||||
| The second stepa | 1a | 1b | 1c | 1e | 1f | 1i | 1j | 3a | 3b | 3c | 2c | 2d | 2e | 3d | 3e | 3f | 2f | 3g | 3h | 2h | 2i | 2j | |||||||||
| (9–16 weeks) | |||||||||||||||||||||||||||||||
| The third stepb | 1a | 1b | 1c | 1e | 1f | 1i | 1j | 3a | 3b | 4a | 3c | 4b | 2c | 2e | 3d | 3e | 4c | 2f | 3g | 3h | 2h | 2i | 2j | ||||||||
| (17–24 weeks) |
Note. MLT = multicomponent lower extremity training.
Eight exercises (3a, 3b, 3c, 3d, 3e, 3f, 3g, and 3h) were added while excluding 1d, 1g, 1h, 2a, 2b, and 2g.
Three exercises (4a, 4b, and 4c) were inserted while excluding two exercises (2d and 3f).
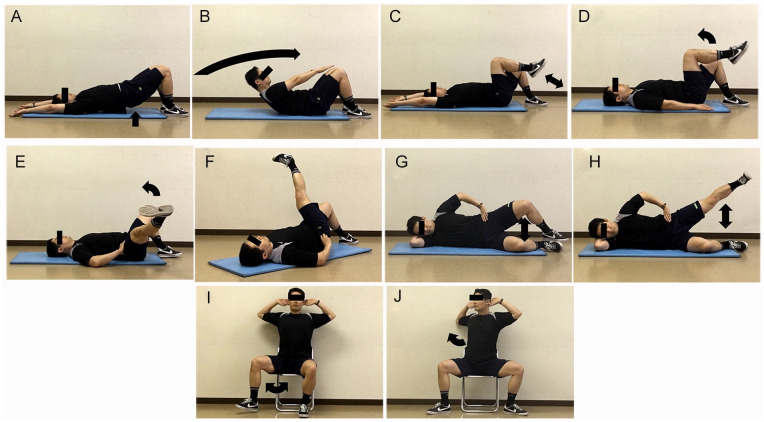
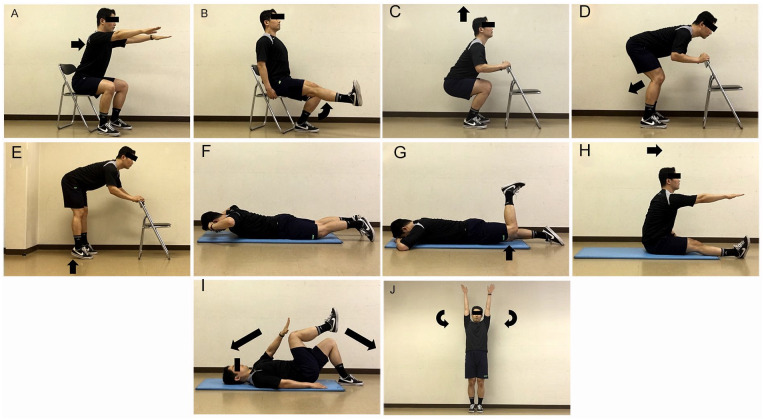
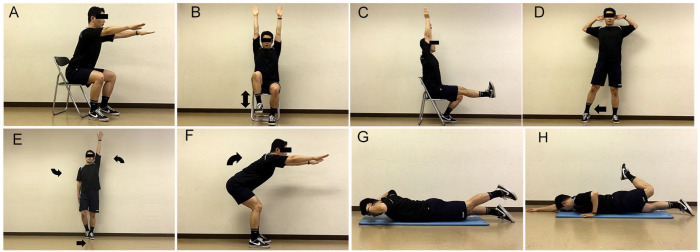
The first exercise step (1–8 weeks) was designed for movement of the lower extremity and included non-weight-bearing exercises which had a lower load on the spine. Figures 1 and 2 show the 20 exercises used in the first exercise step. In the second step (9–16 weeks), several exercises were added that extended the spine to a greater extent than in stage 1, or which could be performed in a full standing position without both hands on the backrest of the chair (Figure 3). In the third step (17–24 weeks), exercises which put additional weight on the foot or required maintenance of balance in a sitting or standing position were added (Figure 4).
Figure 1.
The participants performed 10 repetitions of each exercise. (A) Raise the pelvis. (B) Elevate the upper body with fingertips reaching as close as possible to the knees. (C) Hip and knee flexion/extension movements. (D) Knee flexion/extension movements, from the hip and knee joint angles positioned at 90 degrees. (E) Rotate the hip to the outside of the body’s center line. (F) Rotate the hip to the inside of the body’s center line. (G) Hip abduction/external rotation (Mascal et al., 2003). (H) Lift the top limb off the other bottom limb as high as possible with the knee extended without rotation of the pelvis (Mascal et al., 2003). (I) Rotate the hip to the outside of the body’s center line, with the knee joint angles positioned at 90 degrees. (J) Twist the upper body while the limbs are wide open with the knee joint angles positioned at 90 degrees.
Figure 2.
Ten repetitions of all exercises, except 30 repetitions of (C) and (E) exercises, (F) and (G) exercises (hold the posture for 30 s), and three repetitions of (J) exercise. (A) With the upper body and head straight, bend the upper body forward, with the arms straightened forward. (B) Knee extension movement. (C) Squat. (D) Bend the knees slightly for the extension of hamstring, knee extension. (E) Move the hips back for the extension of hamstring, raise the heels. (F) Keep a slightly raised upper body. (G) Keep the slightly raised hip, with flexion of the knee at 90 degrees. (H) Flex the upper body forward, with the arm straight forward. (I) Extension of the spine by extending the left arm and the right limb. (J) Inhaling deeply, raise the arms, exhaling, lower the arms while spreading out to the side of the body.
Figure 3.
The participants kept postures of A, C, G, and H exercises for 30 s. Ten repetitions of B, D, E, and F exercises. (A) Keep sitting for 30 s with the spine straightened. (B) Raise the knees. (C) Keep the knee extended for 30 s. (D) Travel three side steps to the right and three to the left with the knees extended, while the spine is straight. (E) From a standing position with the limbs slightly apart with the arms are parallel to the floor, inhale deeply, exhaling, raise the left arm while the right arm lower, drawing the right limb in beside the left limb. Bend the knee of the right limb slightly, while raising the right heel, keeping the right foot on the floor. Contract the left quadriceps muscle to straighten the knee. (F) Pull the hips backward while bending the knees slightly to stretch the hamstring muscles. Inhale deeply, exhaling, stand by extending the knees and raise both arms over the head. When standing completely, contract the hip muscles. (G) Raise the limb with the knee extended. (H) Raise the completely bent left knee while reaching the right arm straight ahead.
Figure 4.
The participants kept postures of all exercises for 30 s. (A) Spread the limbs wide open with the arms parallel to the floor, bend the upper body forward with the spine straight. (B) Lower body until the right thigh is parallel to the floor while the right shin is vertical, and the right hand is on the backrest of the chair, raise the left arm over the head. (C) Pull the hips backward while bending the knees slightly to stretch hamstring muscles.
The CG did not perform any training, but resumed their everyday life for 24 weeks.
Outcomes
Anthropometric measurements
Body height was measured in centimeters (cm) by a vertical standard wall tape. Body mass was measured in kilograms (kg) using a calibrated digital scale. Body mass index (BMI) was also calculated as body weight divided by squared body height (kg/m2).
ROM
ROM measurements were performed using the method described by Norkin and White (2011). The same physical therapist, with 6 years’ experience in ROM measurements, performed all bilateral measurements of lower extremity ROMs using a double-arm (30 cm) stainless steel goniometer (Tsutsumi Corp., Kamagaya City, Chiba, Japan).
The participants were taught about each ROM movement. If necessary, rest breaks were given to the participants between ROM measurements, and measurements were reperformed when the participant indicated that he or she was ready to continue. Hip extension and knee flexion ROMs were recorded while the participants were lying in a prone position. Internal and external hip rotation ROMs and ankle dorsiflexion and plantar flexion ROMs were obtained while the participants were seated on a tall chair with their feet off the floor and knees flexed at 90°. Hip flexion, abduction, and adduction ROMs were obtained with the participants positioned in a supine position. All ROM measurements were performed precisely once, and the mean values of the left and right sides of each motion were selected for analysis.
Muscle strength
Measurements of the knee extensor and flexor muscles were performed using a hand-held dynamometer (HHD; μTasF-1, Anima Corp., Tokyo, Japan), with the participants seated in a tall chair with the dynamometer sensor fastened around the leg 10 cm above the ankle joint, and the hip and knee joint angles stabilized at 90 degrees. For measurement of the knee extensor muscle, an anchor belt was affixed to a crossbar position behind the participant. For measurement of the knee flexor muscle, an anchor belt was affixed to a crossbar positioned in front of the participant. Maximal voluntary isometric strength over a 5-s period was measured twice and recorded in Newtons (N). There was a 5-min rest period between the two trials. The mean values of the two trials on the right and left legs were used for analysis.
Physical performance tests
For the functional reach test (FRT) (Duncan et al., 1990), participants were asked to take a standing position, and the right arm was raised straight forward, horizontally from their shoulders. The participant was then asked to reach their arm forward as far as possible without losing their balance. The distance reached was recorded.
We used the timed up and go test (TUGT) as modified by Podsiadlo and Richardson (1991). This records the time taken (in seconds) for the participant to: (a) get up from an armless chair with a seat height of 43 cm, (b) walk 3 m forward at a comfortable pace, (c) turn around, (d) walk back to the chair, and (e) sit down again.
For the five times sit-to-stand test (FTSST) (Lord et al., 2002), the participants were required to stand up and sit down from an armless 43 cm high chair as fast as possible 5 times, with their arms folded across their chest. Timing began when the participant stood up from the initial sitting position and ended when the participant was in a fully upright position at the fifth stand.
Statistical Methods
All statistical analyses were performed in SPSS, version 18.0, for Windows. All variables are expressed as means and standard deviations. An unpaired t-test was used to compare baseline characteristics, apart from gender, between groups. Levene’s test was used to evaluate the homogeneity of variance. Gender was compared between the groups by using chi-square test. A two-way analysis of variance (ANOVA) with repeated measures was performed to evaluate the effect of the intervention on measurements of ROM, muscle strength, and physical performance tests. The groups of “trained” and “controls” were considered as the between-subjects factor, and the time of measurements at the baseline and at 24 weeks as the within-subjects factor. If a significant interaction was found, a post hoc analysis using a Bonferroni adjustment was conducted for the time factor. F-statistic, eta-squared (n2), and p-values were extracted. To avoid Type I errors, a significance level was adjusted to <.025 using the Bonferroni method.
Results
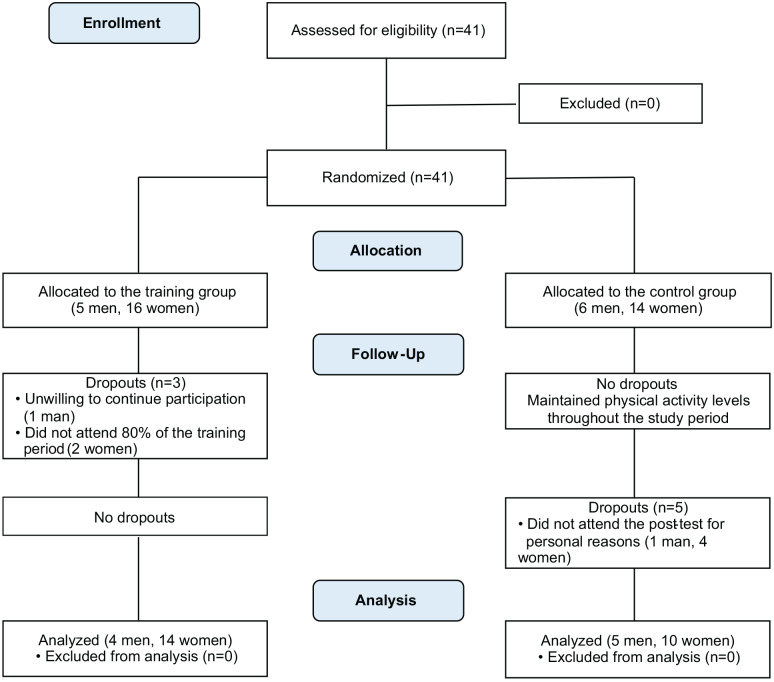
The study flowchart is presented in Figure 5. All 41 eligible older adults were enrolled in the study during December 2014. Three participants enrolled in the TG and five participants enrolled in the CG declined participation. The mean attendance rate for the TG sessions was 95.4%. After the 24-week study period, the data from the remaining 33 participants were analyzed in the study.
Figure 5.
Flow diagram of the participants.
No significant differences were found between the groups in terms of baseline characteristics (Table 2). Table 3 shows ROM, muscle strength, and physical performance test scores at baseline and at 24 weeks. All ROM measures presented significant interaction effects. The TG expressed significant improvements in all ROM measurements, except knee flexion. The greatest increase was in the hip extension ROM, which presented with a 33.3% increase, F(1,17) = 79.510, p < .001, n2 = 0.719. The increase in the ankle plantar flexion ROM had the lowest improvement at 5.3%, F(1,17) = 9.513, p = .004, n2 = 0.235.
Table 2.
Baseline Characteristics of the Participants (M ± SD).
| Variables | Training group | Control group | p-value |
|---|---|---|---|
| Male/female | 4/14 | 5/10 | .475a |
| Age (years) | 71.7 ± 4.6 | 74.3 ± 5.6 | .151 |
| Height (cm) | 153.6 ± 5.8 | 158.4 ± 8.8 | .071 |
| Mass (kg) | 53.1 ± 6.1 | 57.5 ± 6.7 | .053 |
| BMI (kg/m2) | 22.4 ± 1.7 | 23.0 ± 2.3 | .460 |
Note. BMI = body mass index.
Chi-square test.
Table 3.
Range of Motion, Muscle Strength, and Physical Performance Test Scores Before and After 24 Weeks (M ± SD).
| Variables | Training group† | Control group† | Group × Time Interaction‡ | ||||
|---|---|---|---|---|---|---|---|
| Baseline | 24 Weeks | Baseline | 24 Weeks | F(1,31) | p-value | n 2 | |
| Range of motion (degrees) | |||||||
| Hip flexion | 124.3 ± 7.5 | 127.6 ± 6.1b | 124.0 ± 8.5 | 121.6 ± 7.0a | 18.604 | <.001 | 0.375 |
| Hip abduction | 32.6 ± 5.1 | 40.9 ± 7.3b | 32.3 ± 4.5 | 32.5 ± 3.6 | 26.017 | <.001 | 0.456 |
| Hip adduction | 19.1 ± 3.1 | 21.9 ± 3.2b | 18.2 ± 3.1 | 17.2 ± 3.0 | 16.867 | <.001 | 0.352 |
| Hip extension | 17.7 ± 4.2 | 23.6 ± 3.8b | 15.1 ± 3.4 | 16.2 ± 3.4 | 23.900 | <.001 | 0.435 |
| Hip internal rotation | 28.8 ± 5.6 | 36.6 ± 5.2b | 28.9 ± 6.3 | 27.8 ± 4.6 | 24.983 | <.001 | 0.446 |
| Hip external rotation | 26.9 ± 4.3 | 32.9 ± 5.9b | 29.9 ± 5.3 | 25.9 ± 4.4a | 25.384 | <.001 | 0.450 |
| Knee flexion | 127.7 ± 8.6 | 128.7 ± 8.7 | 123.6 ± 8.0 | 121.8 ± 8.0 | 5.842 | .022 | 0.159 |
| Ankle dorsiflexion | 16.2 ± 5.8 | 18.3 ± 5.7a | 14.3 ± 5.6 | 13.6 ± 5.3 | 5.666 | .024 | 0.155 |
| Ankle plantar flexion | 61.8 ± 6.9 | 65.1 ± 6.3b | 56.5 ± 6.3 | 53.6 ± 7.4a | 15.652 | <.001 | 0.336 |
| Muscle strength (N) | |||||||
| Knee extension strength | 178.8 ± 46.0 | 204.1 ± 56.8b | 205.4 ± 80.9 | 198.9 ± 67.3 | 5.715 | .023 | 0.156 |
| Knee flexion strength | 83.0 ± 25.0 | 99.5 ± 36.2 | 90.4 ± 33.5 | 88.4 ± 28.9 | 5.342 | .028 | 0.147 |
| Physical performance tests | |||||||
| Functional reach test (cm) | 32.2 ± 4.5 | 35.4 ± 3.2 | 29.8 ± 2.8 | 30.5 ± 5.0 | 3.125 | .087 | 0.092 |
| Timed up and go test (s) | 6.6 ± 0.9 | 5.7 ± 0.9b | 7.0 ± 1.7 | 7.1 ± 1.8 | 9.039 | .005 | 0.226 |
| Five stands sit-to-stand test (s) | 7.0 ± 1.2 | 6.1 ± 1.2a | 8.7 ± 2.7 | 9.4 ± 3.3 | 7.874 | .009 | 0.203 |
Note. The significance level was set at <.025. ANOVA = analysis of variance.
The post hoc analysis (ap < .025; bp < .01).
The two-way ANOVA with repeated measures.
There was a significant interaction effect in the knee extension strength. The knee extension strength in the TG showed a significant increase of 14.1%, F(1,17) = 7.970, p = .008, n2 = 0.205.
The TUGT and FTSST showed significant interaction effects. Significant improvements in the TG were found in the TUGT (13.6%), F(1,17) = 15.205, p < .001, n2 = 0.329, and in the FTSST (13.1%), F(1,17) = 5.600, p = .024, n2 = 0.153.
Discussion
The purpose of this study was to evaluate the effectiveness of the MLT technique on physical function in older adults. The program used in this study contained strength, balance, and flexibility components and a progressive increase in intensity level through three steps. After 24 weeks, we showed improved ROM, muscle strength, and physical performance in the lower extremities using this specific MLT technique.
The intervention study by Oliveira et al. (2016) indicated that while static stretching exercises improved only hip flexion ROM, Pilates exercises improved hip flexion, ankle plantar flexion, and ankle dorsiflexion ROMs. Whereas Pilates for older adults requires using specific Pilates equipment (Oliveira et al., 2016) and/or participation more than 2 times per week (Bueno de Souza et al., 2018), MLT is performed with no equipment in the improvement of ROM in older adults for 24 weeks, once per week. The improvements in ROM induced by passive PNF flexibility exercises required professional one-on-one attention by qualified trainers (Klein et al., 2002). The results from our study demonstrated that MLT, which was led by only one trainer, could improve lower extremity function—including ROM, muscle strength, and physical function ability—with no professional guidance, and in a group setting. This is a substantial benefit when compared with PNF.
The results of our study provide strong evidence that ROM can be increased by the MLT technique. This is particularly true of hip extension, hip abduction, and internal and external hip rotations when considering that the mean error between repeated ROM measurements is only 5 degrees (Walker et al., 1984). A larger hip extension ROM can have an influence on the performance of the FTSST (Jung & Yamasaki, 2016). Furthermore, a previous study showed that limited abduction and external rotation of the hip was observed in women with difficulties climbing up and down stairs (Mascal et al., 2003). Therefore, both our results and previous studies suggest that the increment of these ROMs may contribute to functional independence in older adults.
Resistance training has been shown to improve knee extension strength in older adults when compared with a group that performed no exercise (Chen et al., 2017). However, resistance training generally requires the use of various resistance machines or equipment to obtain a marked improvement in muscle strength (Chen et al., 2017). Our results indicate that, despite not using any specialized equipment, the MLT technique induced a significant improvement in the knee extension strength in older adults, considering that the differences of repeated measurements of knee extension strength with an HHD ranged from 0.98 to 5.8 N (Katoh & Yamasaki, 2009).
In this study, there were significant improvements in physical performance test scores that have been shown previously to be vital factors in the prediction of physical frailty (Chang et al., 2014). Both ankle plantar flexion ROM and knee extension strength have been shown previously to be determinants of performance in the TUGT (Jung & Yamasaki, 2016), both of which showed notable increases in this study. In addition, hip extension ROM was improved substantially by MLT in this study, which has been noted as a determinant of performance in the FTSST (Jung & Yamasaki, 2016). This may account for the improvements on the TUGT and FTSST found in this study.
Previously, studies by Kanda et al. (2018) and Watanabe et al. (2014) showed significant increases in physical performance ability and muscle strength using low-intensity bodyweight and low-intensity (30% of one repetition maximum) resistance training, respectively. This is consistent with the results of this study. However, we also demonstrated an increase in ROM. Figure 3C shows one of the important exercises in MLT used in this study. This exercise requires maintenance of posture while both raising the limb with knee extended and keeping the back straight while extending both arms overhead. As such, it requires strength, balance, and flexibility. This demonstrates the advantage of the MLT technique in simultaneously improving ROM, muscle strength, and physical performance ability. This exercise has not yet been presented in other exercise intervention studies.
Exercises targeting muscle power and common mobility tasks showed improvements in leg power and leg speed of older adults with mobility limitations (Bean et al., 2016). Practicing yoga, with the support of a chair, improved gait speed of older adults with lower extremity osteoarthritis who are unable to participate in standing exercises (Park et al., 2017). The MLT technique from our study may meet the conditions of exercises mentioned above, which are based on normal functional tasks and performed in a sitting position on a chair, applying to older adults with the aforementioned issues. An intervention study (Hwang et al., 2016) showed that self-practice of home-based exercises reduced injurious falls in older adults who had fall-related emergency department visits. Similarly, the MLT technique includes movements that are easy to understand for older adults without equipment, indicating a possibility of self-practice, which may contribute to a decrease in injurious fall rates. In addition, the MLT technique was conducted by only one instructor, once per week. This is a low-cost exercise and is effective for older adults and may be applied to communities and prison settings in developing countries.
This study had several limitations. We cannot be certain that a causal association exist between physical performance ability and ROM and/or muscle strength in this study, due to the small sample size. Furthermore, we did not measure the entire lower extremity muscle strength. Measurements of muscle strength were determined based on the participant’s voluntary effort in generating maximum muscle strength over a 5-s period. To minimize the burden of measurement on participants, we selected knee strength as a single representation of the totality of lower extremity muscle strength (Bohannon et al., 2012).
Conclusion
Our findings suggest that the MLT technique is a low-cost intervention suitable for older adults for the improvement of lower extremity function, which may be applied to communities and prison settings in developing countries. The MLT technique simultaneously increases ROM, muscle strength, and physical performance ability. Clinically, this technique would improve mobility and functional independence in older adults with mobility limitation or lower extremity osteoarthritis. This technique can be self-practiced, contributing to a decrease in injurious fall rates. Further study will be needed to verify the effects of MLT on different populations, such as frail older adults or residents in elderly care homes.
Acknowledgments
We would like to thank the individuals enrolled in this study who live in Higashi-Hiroshima city. After finishing this study, they continue to regularly participate in the multi-component lower extremity training (MLT). MLT is being referred to as the three-step exercise program in the community. Furthermore, we would like to thank Editage (www.editage.com) for English language editing.
Footnotes
Author Contributions: H.J. contributed to the study design, data acquisition, statistical analysis, interpretation of the results, and manuscript preparation. Y.M., R.T., and M.Y. participated in the study design and reviewed the manuscript. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hungu Jung  https://orcid.org/0000-0001-7500-7029
https://orcid.org/0000-0001-7500-7029
References
- Bean J. F., Beauchamp M. K., Ni M. (2016). Targeted exercise training to optimize leg power, leg speed, and mobility in older adults. Journal of the American Geriatrics Society, 64(12), 2608–2609. 10.1111/jgs.14397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohannon R. W., Magasi S. R., Bubela D. J., Wang Y. C., Gershon R. C. (2012). Grip and knee extension muscle strength reflect a common construct among adults. Muscle & Nerve, 46, 555–558. 10.1002/mus.23350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno de Souza R. O., Marcon L. F., Arruda A. S. F., Pontes Junior F. L., Melo R. C. (2018). Effects of mat Pilates on physical functional performance of older adults: A meta-analysis of randomized controlled trials. American Journal of Physical Medicine & Rehabilitation, 97, 414–425. 10.1097/PHM.0000000000000883 [DOI] [PubMed] [Google Scholar]
- Chang S. F., Yang R. S., Lin T. C., Chiu S. C., Chen M. L., Lee H. C. (2014). The discrimination of using the short physical performance battery to screen frailty for community-dwelling elderly people. Journal of Nursing Scholarship, 46, 207–215. 10.1111/jnu.12068 [DOI] [PubMed] [Google Scholar]
- Chen H. T., Chung Y. C., Chen Y. J., Ho S. Y., Wu H. J. (2017). Effects of different types of exercise on body composition, muscle strength, and IGF-1 in the elderly with sarcopenic obesity. Journal of the American Geriatrics Society, 65, 827–832. 10.1111/jgs.14722 [DOI] [PubMed] [Google Scholar]
- Ding L., Yang F. (2016). Muscle weakness is related to slip-initiated falls among community-dwelling older adults. Journal of Biomechanics, 49, 238–243. [DOI] [PubMed] [Google Scholar]
- Duncan P. W., Weiner D. K., Chandler J., Studenski S. (1990). Functional reach: A new clinical measure of balance. The Journals of Gerontology, 45, M192–M197. [DOI] [PubMed] [Google Scholar]
- Gehlsen G. M., Whaley M. H. (1990). Falls in the elderly: Part II, Balance, strength, and flexibility. Archives of Physical Medicine and Rehabilitation, 71, 739–741. [PubMed] [Google Scholar]
- Grimmer M., Riener R., Walsh C. J., Seyfarth A. (2019). Mobility related physical and functional losses due to aging and disease—A motivation for lower limb exoskeletons. Journal of NeuroEngineering and Rehabilitation, 16, Article 2. 10.1186/s12984-018-0458-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang H. F., Chen S. J., Lee-Hsieh J., Chien D. K., Chen C. Y., Lin M. R. (2016). Effects of home-based tai chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the emergency department—A randomized controlled trial. Journal of the American Geriatrics Society, 64(3), 518–525. 10.1111/jgs.13952 [DOI] [PubMed] [Google Scholar]
- Jung H., Yamasaki M. (2016). Association of lower extremity range of motion and muscle strength with physical performance of community-dwelling older women. Journal of Physiological Anthropology, 35, Article 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanda K., Yoda T., Suzuki H., Okabe Y., Mori Y., Yamasaki K., Kitano H., Kanda A., Hirao T. (2018). Effects of low-intensity bodyweight training with slow movement on motor function in frail elderly patients: A prospective observational study. Environmental Health and Preventive Medicine, 23, Article 4. 10.1186/s12199-018-0693-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katoh M., Yamasaki H. (2009). Test-retest reliability of isometric leg muscle strength measurements made using a hand-held dynamometer restrained by a belt: Comparisons during and between sessions. Journal of Physical Therapy Science, 21, 239–243. [Google Scholar]
- Klein D. A., Stone W. J., Phillips W. T., Gangi J., Hartman S. (2002). PNF training and physical function in assisted-living older adults. Journal of Aging and Physical Activity, 10, 476–488. [Google Scholar]
- Lord S. R., Murray S. M., Chapman K., Munro B., Tiedemann A. (2002). Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 57, M539–M543. [DOI] [PubMed] [Google Scholar]
- Marques N. R., Hallal C. Z., Spinoso D. H., Crozara L. F., Morcelli M. H., Karuka A. H., Navega M. T., Gonçalves M. (2016). Age-related alterations in the activation of trunk and lower limb muscles during walking. Journal of Back and Musculoskeletal Rehabilitation, 29, 295–300. [DOI] [PubMed] [Google Scholar]
- Mascal C. L., Landel R., Powers C. (2003). Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 Case reports. Journal of Orthopaedic & Sports Physical Therapy, 33, 647–660. [DOI] [PubMed] [Google Scholar]
- Norkin C. C., White D. J. (2011). Measurement of joint motion: A guide to goniometry (2nd ed.). Davis. [Google Scholar]
- Oliveira L. C., Oliveira R. G., Pires-Oliveira D. A. (2015). Effects of Pilates on muscle strength, postural balance and quality of life of older adults: A randomized, controlled, clinical trial. Journal of Physical Therapy Science, 27, 871–876. 10.1589/jpts.27.871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira L. C., Oliveira R. G., Pires-Oliveira D. A. (2016). Comparison between static stretching and the Pilates method on the flexibility of older women. Journal of Bodywork and Movement Therapies, 20, 800–806. 10.1016/j.jbmt.2016.01.008 [DOI] [PubMed] [Google Scholar]
- Park J., McCaffrey R., Newman D., Liehr P., Ouslander J. G. (2017). A pilot randomized controlled trial of the effects of chair yoga on pain and physical function among community-dwelling older adults with lower extremity osteoarthritis. Journal of the American Geriatrics Society, 65(3), 592–597. 10.1111/jgs.14717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D., Richardson S. (1991). The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society, 39, 142–148. [DOI] [PubMed] [Google Scholar]
- Walker J. M., Sue D., Miles-Elkousy N. (1984). Active mobility of the extremities in older subjects. Physical Therapy, 64, 919–923. [DOI] [PubMed] [Google Scholar]
- Watanabe Y., Madarame H., Ogasawara R., Nakazato K., Ishii N. (2014). Effect of very low-intensity resistance training with slow movement on muscle size and strength in healthy older adults. Clinical Physiology and Functional Imaging, 34, 463–470. 10.1111/cpf.12117 [DOI] [PubMed] [Google Scholar]
- Zhong R., Rau P. L. P., Yan X. (2018). Application of smart bracelet to monitor frailty-related gait parameters of older Chinese adults: A preliminary study. Geriatrics & Gerontology International, 18, 1366–1371. 10.1111/ggi.13492 [DOI] [PubMed] [Google Scholar]