Abstract
Background:
Fluoroscopy use during ERCP exposes patients and providers to deleterious effects of radiation. Formal training in fluoroscopy/radiation protection is not widely emphasized during therapeutic endoscopy training, and radiation use during GI endoscopy has not previously been characterized in the United States (US). In this study we evaluated radiation training, fluoroscopy use patterns and radiation protection practices among US therapeutic endoscopists.
Methods:
An anonymous electronic survey was distributed to US therapeutic endoscopists and responses were analyzed using descriptive statistics. State-specific requirements for fluoroscopy utilization were determined from state radiologic health branches.
Results:
159 endoscopists (response rate 67.8%) predominantly those working in university hospitals (69.2%) with >5 years of experience performing ERCP (74.9%), completed the questionnaire. Although the majority of endoscopists (61.6%) reported that they personally controlled fluoroscopy during ERCP, most (56.6 %) had not received training on operating their fluoroscopy system. Only a minority (18-31%) of all respondents reported consistently utilizing modifiable fluoroscopy system parameters that minimize patient radiation exposure (pulsed fluoroscopy, frame rate modification or collimation). Endoscopists appear to undertake adequate personal radiation protective measures although use of a dosimeter was not consistent in half of respondents. The majority of states (56.8%) do not have any stated requirement for certification of non-radiologist physicians who intend to operate fluoroscopy.
Conclusions:
Most US gastroenterologists performing ERCP have not received formal training in operating their fluoroscopy system or in minimizing radiation exposure to themselves and to their patients. Such formal training should be included in all therapeutic endoscopy training programs and fluoroscopy system-specific training should be offered at all hospitals.
Keywords: Radiation, ERCP, Fluoroscopy, Endoscopist
INTRODUCTION
Fluoroscopy is an integral part of Endoscopic Retrograde Cholangiopancreatography (ERCP) and endoluminal stent placement within the GI tract. Fluoroscopy utilization places patients, endoscopists and endoscopy room staff at risk for deleterious radiation-induced deterministic and stochastic effects.1 Although exposure to high dose-rate ionizing radiation is well known to be associated with genomic instability,2,3 more recent evidence indicates that exposure to even low dose-rate ionizing radiation, typically utilized for diagnostic medical tests and therapeutic procedures, is also associated with a linear increase in cancer mortality.4
Medical radiation accounts for approximately half of the radiation exposure in the US population,5 with an estimated 2% of cancers diagnosed annually in the U.S. attributed to radiation from computed tomography (CT) scans alone.6,7 In response, the radiology community has implemented programs and guidelines to enhance provider training and minimize patient radiation exposure.8–12 The range of reported ERCP-associated radiation doses is broad, with older studies indicating that therapeutic ERCP is associated with an effective radiation dose of 12.4 mSv, higher than the 10 mSv associated with a CT scan of the abdomen.13 These radiation doses would be estimated to confer a lifetime risk of cancer of approximately 1 in 1700.13 However radiation doses associated with ERCP are highly variable, with some radiation conscious centers reporting substantially lower doses, particularly with the advent of newer fluorosocpy machines and increasing awareness and attention to radiation protection. Numerous factors may account for the noted variation in ERCP associated radiation exposure, including endoscopist or radiology technician control of fluoroscopy, operator familiarity with fluoroscopy machine/equipment and settings that minimize patient radiation exposure, and the culture of site-specific emphasis on the ‘as low as reasonably achievable’ (ALARA) principle for radiation use.
As therapeutic endoscopists increasingly control fluoroscopy during endoscopic procedures,14 it is important for them to be aware of risks associated with radiation exposure and to have the training necessary to minimize radiation use during their procedures. The European Society of Digestive Endoscopy has established guidelines/recommendations pertaining to radiation use during digestive endoscopy/ERCP.15 Efforts of the US gastroenterology community in minimizing patient radiation exposure during endoscopic procedures have thus far been tepid, primarily comprising a broad recommendation to keep radiation doses as low as reasonably achievable and to record the radiation dose for all ERCPs.16,17 Additionally, there has not been a broad regulatory push in the US for quality indicators for endoscopy-associated fluoroscopy use, or for education of endoscopists in minimizing patient radiation exposure during ERCP.
Several factors may underlie the relative inattention among many therapeutic endoscopists in minimizing procedural radiation use. Therapeutic endoscopists may perceive their personal risk as being lower, as they are exposed to less radiation than cardiologists, vascular surgeons and interventional radiologists.18–20 Additionally, in contrast to interventional cardiology fellowships where radiation safety/physics are integral parts of the training curriculum and board certification,21 therapeutic endoscopy fellowships are unaccredited and without a board certification process. Consequently, there is no formal curriculum, and radiation protection is not typically emphasized during therapeutic endoscopy fellowship training. This may contribute to a lower level of attention by therapeutic endoscopy attendings/trainers in minimizing procedural radiation use, a cycle which may be perpetuated over subsequent generations of therapeutic endoscopy trainees.
Nationwide data regarding radiation protection practices and training for endoscopists performing ERCP have not previously been reported in the US. The aim of this survey study including endoscopists at all levels of experience, from therapeutic endoscopy fellows to seasoned endoscopists, was to assess endoscopist training in use of their fluoroscopy systems, familiarity with fluoroscopy interventions which minimize patient radiation exposure, and the personal radiation protective measures endoscopists routinely undertake. Additionally we sought to characterize state-based fluoroscopy certification requirements.
METHODS
Survey Instrument
We designed an online survey to assess radiation protection and fluoroscopy utilization practices among US therapeutic endoscopists. The survey comprised a self-administered electronic questionnaire with 19 questions, designed to be completed in less than 3 minutes. The survey included a number of questions pertinent to fluoroscopy utilization including practice setting, ERCP volume, radiation protection measures, and training in/utilization of modifiable fluoroscopy system settings which minimize radiation exposure. A pilot version of the survey was scrutinized by three therapeutic endoscopists to confirm the clarity and appropriateness of each question. Minor revisions were implemented in the survey prior to its utilization for this study, based on the received feedback.
Survey Distribution
A direct link to the online survey instrument (SurveyMonkey, Palo Alto, CA, USA) was distributed via email to therapeutic endoscopists in adult GI programs in the United States (n = 214) including 49 program directors of therapeutic endoscopy fellowship programs in the US. Program directors were asked to extend the invitation to participate in the study to their therapeutic endoscopy fellows. Nonresponders to the initial survey were sent a reminder e-mail three months after the initial survey distribution e-mail. E-mail addresses for distribution were obtained from the membership directory of the American Society for Gastrointestinal Endoscopy (ASGE).
There were no incentive programs utilized to increase the response rate. Responses were collected over a 6-month period. All answers remained anonymous to minimize the potential for response bias. Informed consent was implied by respondents’ willingness to complete the survey.
Evaluation of Fluoroscopy Operator Regulations by State
Contact information for each state’s radiologic health and safety branch was obtained from the American Society of Radiologic Technologists. We subsequently contacted radiation agencies in all 50 states and the District of Columbia, to determine individual state requirements for operation of fluoroscopy equipment by non-radiologist physicians.
We accessed the websites of the radiation health and safety branch in each state, to determine fluoroscopy certification requirements. We additionally placed a telephone call to the representatives of the radiation health and safety branch in each state to confirm online information where available, and to clarify requirements for states in which this information was not available online.
Statistical Analysis
Descriptive statistics were used for analysis of demographic data. Chi-squared testing was applied to categorical data. Fisher’s exact test was used for sparsely distributed data. Statistical significance was defined as a P value less than 0.05. All analyses were conducted using SurveyMonkey and Microsoft Excel (Microsoft Corporation, Redmond, WA).
RESULTS
Respondents:
The questionnaire was completed by 145 attending endoscopists of the 214 to whom it was distributed (response rate 67.8%). Additionally, 14 therapeutic endoscopy fellows responded, for a total of 159 respondents with fellows comprising 8.8% of the total respondents (Table 1A). All respondents answered all survey questions. The majority of respondents reported working in university hospitals (69.2%). High and low volume endoscopists were both well represented in this survey (≤ 50 ERCPs/year: 8.8%, 51-200 ERCPs/year: 42.8%, 201-500 ERCPs/year: 44.7%, >500 ERCPs/year: 3.8%). The majority were well experienced and reported performing ERCP for >10 years (<5 years: 16.4%, 5-10 years: 19.5%, >10 years: 55.4%).
TABLE 1A.
Overall Characteristics: Endoscopists & Healthcare Facilities
| Survey Question | Responses (%) | |
|---|---|---|
| Please indicate your experience in ERCP? | Attending: | 91.2% |
| Advanced Fellow: | 8.8% | |
| What is your personal annual volume of ERCPs? | ≤50: | 8.8% |
| 51-200: | 42.8% | |
| 201-500: | 44.7% | |
| >500: | 3.8% | |
| What is the annual volume of ERCPs at your center? | ≤250: | 13.8% |
| 251-500: | 27.7% | |
| 501-750: | 22.0% | |
| 751-1000: | 16.4% | |
| >1000: | 20.1% | |
| Does your state require a fluoroscopy license for endoscopists to perform fluoroscopy? | Yes: | 34.6% |
| No: | 47.8% | |
| Don’t Know: | 17.6% | |
Geographic Representation of Respondents
States with >3% of Respondents: California: 25.2%, Massachusetts: 8.8%, Texas: 8.2%, Pennsylvania: 6.9%, Illinois: 6.3%, New York: 4.4%, Arizona: 3.8%, Ohio: 3.8%, Florida: 3.8%, Connecticut: 3.1%
States with <3% of Respondents: Alabama, Arkansas, Colorado, Georgia, Indiana, Louisiana, Maryland, Michigan, Minnesota, Mississippi, Missouri, New Hampshire, North Carolina, Oklahoma, Oregon, South Carolina, Tennessee, Virginia, Washington, Wisconsin
States with no Respondents: Alaska, Delaware, Hawaii, Idaho, Iowa, Kansas, Kentucky, Maine, Montana, Nebraska, Nevada, New Jersey, New Mexico, North Dakota, Rhode Island, South Dakota, Utah, Vermont, West Virginia, Wyoming
Fluoroscopy system:
The majority of respondents (56.6%) had not received formal training in operating their healthcare facility’s fluoroscopy system (Figure 1 depicts overall training responses). Endoscopists working at university hospitals were more likely to receive such training than those working at non-university hospitals (49.1% vs. 30.6%, p=0.03). Of attending respondents who had not received instruction, most (77.8%) felt formal education on operating their fluoroscopy system and in minimizing radiation exposure would have been beneficial (Table 1B, overall responses depicted in Figure 1A, B). Among therapeutic endoscopy fellows, 78.6% reported that they had not received formal training focused on operating their healthcare facility’s fluoroscopy system and 91.7% of these fellow respondents who had not received fluoroscopy training felt that formal education focused on operating their fluoroscopy system and minimizing radiation exposure would have been beneficial (Table 1B).
Fig. 1:
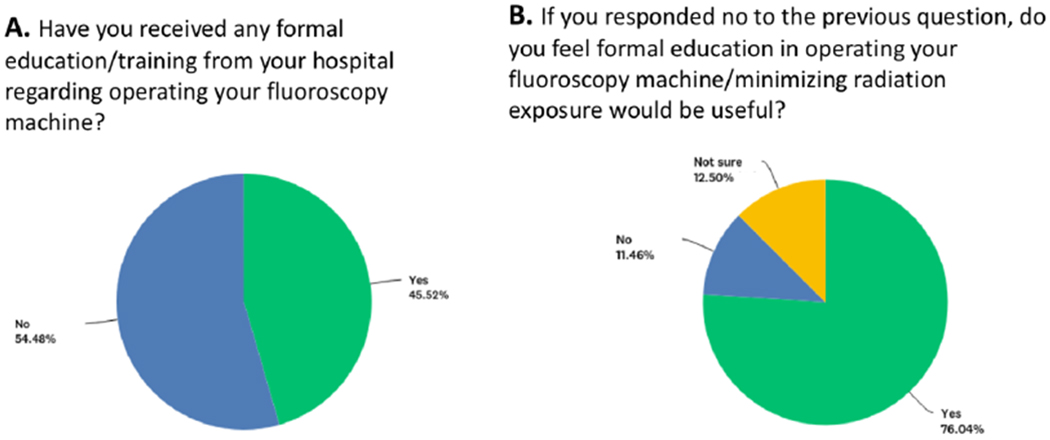
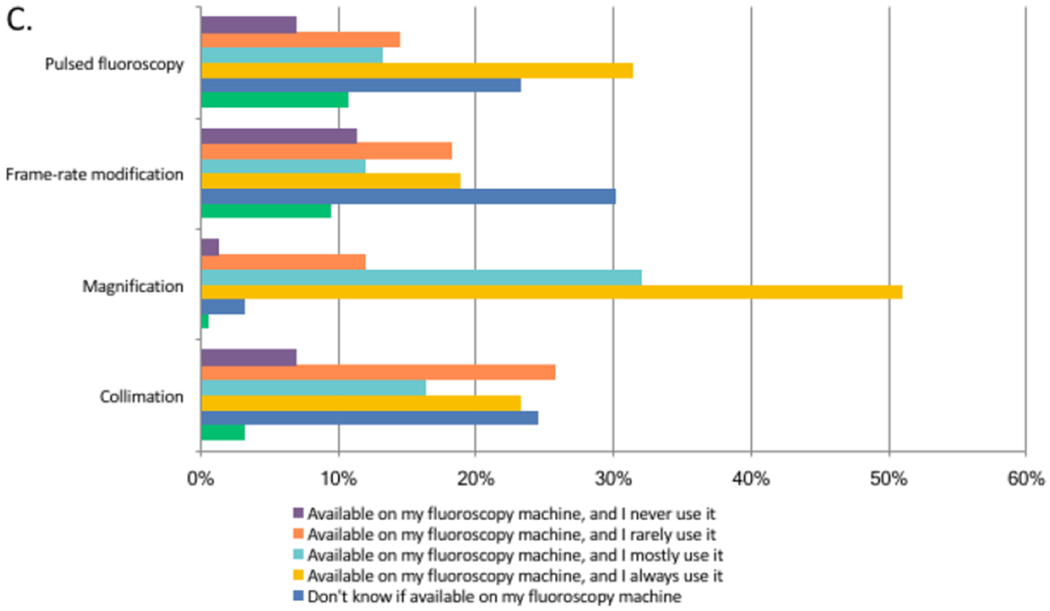
a, b Pie chart reflecting overall (fellow + attending) responses to the indicated survey questions regarding fluoroscopy training. c Bar graph depicting overall endoscopist respondent familiarity with and utilization of modifiable parameters to minimize patient and provider radiation exposure
TABLE 1B.
Overall Training & Fluoroscopy System Operation among University & Non-University Endoscopists
| Survey Question | Overall Responses | University (69.2%, n=110) | Non-University (30.8%, n=49) | |
|---|---|---|---|---|
| Have you received any formal education/training from your hospital regarding operating your fluoroscopy machine? | Attending: Advanced Fellow: |
No: 54.5% Yes: 45.5% No: 78.6% Yes: 21.4% |
No: 50.9% Yes: 49.1% |
No: 69.4% Yes: 30.6% |
| If you responded no to the previous question, do you feel formal education in operating your fluoroscopy machine/minimizing radiation exposure would be useful? | Attending: Advanced Fellow: |
Yes: 76.0% No: 11.5% Not Sure: 12.5% Yes: 91.7% No: 0% Not sure: 8.3% |
Yes: 82.2% No: 9.6% Not Sure: 8.2% |
Yes: 68.6% No: 11.4% Not Sure: 20.0% |
| Who operates the fluoroscopy machine during your ERCPs? | Endoscopist: 61.6% Radiology Technician: 37.7% Radiologist: 0.6% |
Endoscopist: 65.5% Radiology Technician: 33.6% Radiologist: 0.9% |
Endoscopist: 53.1% Radiology Technician: 46.9% Radiologist: 0% |
|
| What kind of fluoroscopy machine/s do you use for performing ERCPs? (check multiple if necessary) | Fixed dedicated: 61.0% Portable C arm: 51.6% Fixed C arm: 12.6% |
Fixed dedicated: 67.3% Portable C arm: 43.6% Fixed C arm: 14.6% |
Fixed dedicated: 46.9% Portable C arm: 69.4% Fixed C arm: 8.2% |
|
| What kind of technology does your fluoroscopy machine/s have? | Image intensifier: 48.4% Flat panel: 5.0% Both on different machines:15.7% I don’t know: 30.8% |
Image intensifier: 51.8% Flat panel: 5.5% Both on different machines: 13.6% I don’t know: 29.1% |
Image intensifier: 40.8% Flat panel: 4.1% Both on different machines: 20.4% I don’t know: 34.7% |
|
Modifiable Fluoroscopy Settings:
Overall responses from all attendings and fellows surveyed are depicted in Figure 1C. Between 19.3% and 24.8% of all attending respondents did not know whether their fluoroscopy system allowed modification of parameters which impact radiation dose, such as pulsed fluoroscopy, frame rate modification and collimation. Among attending endoscopists who received training on their institution’s fluoroscopy system, 6-21.2% were nevertheless unaware as to whether these modifiable settings were available. Between 20 and 33% of all attending respondents reported consistently utilizing these modifiable fluoroscopy settings, with a higher proportion (26-41%) of attending endoscopists trained on their fluoroscopy system reporting consistent use of these settings.
The magnification setting was the most commonly modulated feature during ERCP. Of attending endoscopists, 98.6% were aware that adjustment of magnification settings was possible on their fluoroscopy system, with 84.8% reporting that they always or mostly utilized this feature during ERCP (overall responses depicted in Figure 1C). Responses of therapeutic endoscopy fellows largely mirrored those of attending endoscopists with regard to modifiable fluoroscopy system settings; however, the majority of fellow respondents were unaware if their fluoroscopy system allowed frame rate modification (85.7%) or collimation (64.3%) suggesting that these modalities may be underutilized.
Personal Protection Measures:
Almost all respondents reported always wearing a lead apron (98.1%) and thyroid shield (96.2%) while performing ERCP (overall responses depicted in Figure 2A, Table 2A). A two-piece wrap apron was favored by the majority of attending respondents (60%) with 26.2% using a one-piece wrap lead apron and 13.8% using a one-piece frontal cover-type apron. Most attending respondents (66.2%) were not aware of the thickness of the lead apron they used (Table 2B) Fewer attending respondents reported always (21.4%) or mostly (11%) using lead glasses during ERCP (Figure 2A) and the likelihood of using lead glasses did not increase with higher annual ERCP volume. All therapeutic endoscopy fellows reported consistently wearing lead aprons and thyroid shields, although only 14.3% used lead glasses. The majority of fellows (85.7%) were unaware of the thickness of their lead apron.
Fig. 2:
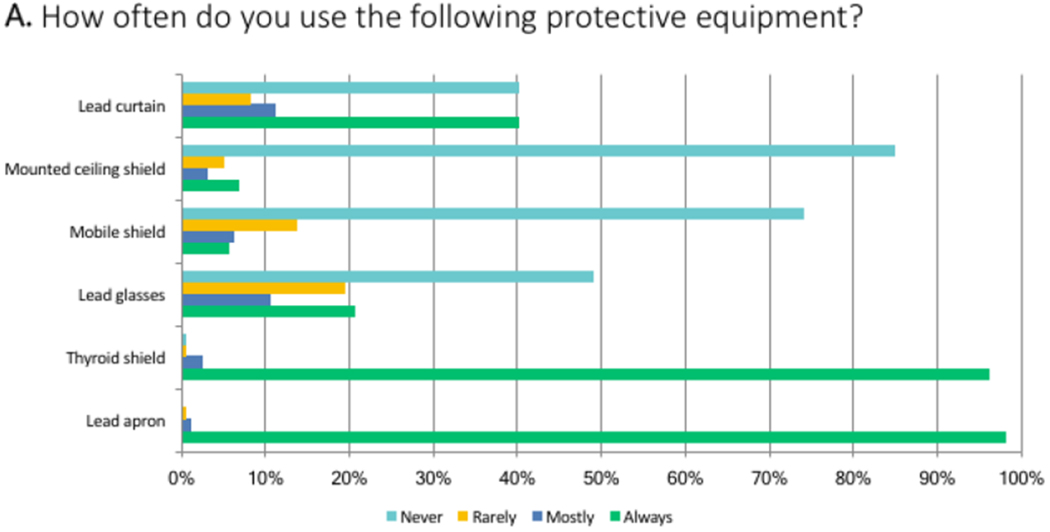
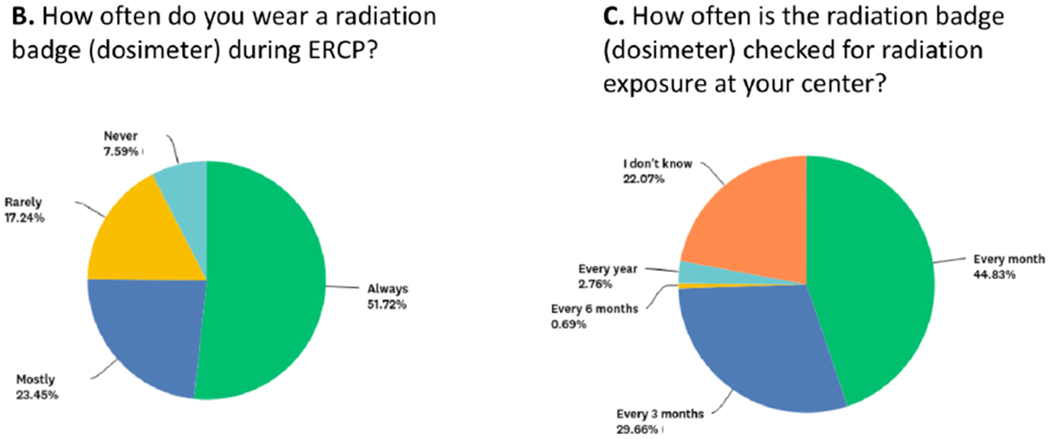
a Bar graph depicting overall endoscopist respondent utilization of the indicated radiation protection equipment. b, c Pie charts reflecting overall (fellow + attending) responses to the indicated survey questions regarding personal radiation dose monitoring practices
TABLE 2A.
Overall Personal Protective Measures
| Survey Question | Responses (%) | |
|---|---|---|
| What type of lead apron do you use to perform ERCP? | Two piece wrap apron | 60.4% |
| One piece wrap apron: | 26.4% | |
| One piece frontal cover | 13.2% | |
| What is the thickness of your lead apron? | 0.25 mm | 3.8% |
| 0.5 mm | 20.1% | |
| 0.75 mm | 4.4% | |
| 1 mm | 3.8% | |
| Don’t know | 67.9% | |
| Does your endoscopy center have a dedicated hanger for lead apron storage? | Yes: | 95.0% |
| No: | 5.0% | |
| How often do you wear a radiation badge (dosimeter) during ERCP? | Always: | 50.3% |
| Mostly: | 23.9% | |
| Rarely: | 16.4% | |
| Never: | 9.4% | |
| How often is the radiation badge (dosimeter) checked for radiation exposure at your center? | Every month: | 42.8% |
| Every 3 months: | 28.9% | |
| Every 6 months: | 0.6% | |
| Every year: | 3.1% | |
| Don’t know: | 24.5% | |
TABLE 2B.
Overall Radiation Protection & Training among Fellow and Attending Respondents
| Survey Question | Fellow Respondents (8.8%, n=14) | Attending Respondents (91.2%, n=145) |
|---|---|---|
| What type of lead apron do you use to perform ERCP? | One piece frontal cover: 7.1% One piece wrap apron: 28.6% Two piece wrap apron: 64.3% |
One piece frontal cover: 13.8% One piece wrap apron: 26.2% Two piece wrap apron: 60.0% |
| What is the thickness of your lead apron? | 0.25 mm: 0% 0.5 mm: 7.1% 0.75 mm: 0% 1 mm: 7.1% Don’t know: 85.7% |
0.25 mm: 4.1% 0.5 mm: 21.4% 0.75 mm: 4.8% 1 mm: 3.5% Don’t know: 66.2% |
| How often do you wear a radiation badge (dosimeter) during ERCP? | Always: 35.7% Mostly: 28.6% Rarely: 7.1% Never: 28.6% |
Always: 51.7% Mostly: 23.5% Rarely: 17.2% Never: 7.6% |
| How often Is the radiation badge (dosimeter) checked for radiation exposure at your center? | Every month: 21.4% Every 3 months: 21.4% Every 6 months: 0% Every year: 7.1% Don’t know: 50.0% |
Every month: 44.8% Every 3 months: 29.7% Every 6 months: 0.7% Every year: 2.8% Don’t know: 22.1% |
| What kind of technology does your fluoroscopy machine/s have? | Image intensifier: 28.6% Flat panel: 0% Both on different machines: 7.1% I don’t know: 64.3% |
Image intensifier: 50.3% Flat panel: 5.5% Both on different machines: 16.6% I don’t know: 27.6% |
Additional protection from scatter radiation:
Consistent use of a shielding lead curtain was reported by 40.7% of attending respondents, with mobile shields and mounted ceiling shields used by only a minority (4.8% for each). Fellow responses mirrored attending responses with respect to use of additional protection against scatter radiation.
Monitoring of Occupational Radiation Exposure:
Approximately half of attending respondents (51.7%) reported that they did not consistently wear a dosimeter and 22.1% did not know how often their dosimeter was checked for radiation exposure (Table 2B, overall responses depicted in Figure 2B/2C). Non-university endoscopists were more likely to wear a dosimeter during ERCP compared to their university colleagues (66.7% vs. 27.3%, p= 0.03). Among therapeutic endoscopy fellows, 35.7% reported consistent use of a dosimeter, but half (50%) did not know how often their dosimeter was checked (Table 2B).
State requirements for Fluoroscopy certification:
Most responding attending endoscopists (49.6%) reported that their state did not require a fluoroscopy license for endoscopists to operate fluoroscopy equipment. 13.8% of attending respondents were not aware of their state’s fluoroscopy licensing requirements; fluoroscopy equipment was operated by a radiation technician at the healthcare facilities of all of these respondents (Table 1A). Therapeutic endoscopy fellows were more frequently unaware of their state fluoroscopy licensing requirements (57.1%).
State Specific Fluoroscopy Certification:
Requirements for fluoroscopy use vary widely and are state-specific. Some states have formal certification processes and/or training recommendations for non-radiologist physicians who intend to operate fluoroscopy equipment. Other states entrust healthcare institutions with the fluoroscopy accreditation process for their physicians. Our queries to state radiologic health and safety agencies indicated that only one state (California) has a curriculum and mandatory examination requirement. Passing this examination is necessary to obtain a permit allowing non-radiologist physicians to operate fluoroscopy equipment. Several states (21 states, 41.2%) do not have a formal examination, but do have recommendations regarding radiation instruction/training, including independent reading, online educational modules and continuing medical education. Twenty-nine states (56.8%) do not appear to have any explicit training or certification requirements for physicians and surgeons who intend to operate fluoroscopy (Table 3).
TABLE 3.
State-based Requirements for Non-Radiologist Physicians Operating Fluoroscopy
| Fluoroscopy Certification Requirements | States |
|---|---|
| Examination-based Licensure Criteria (n=1) | California |
| Non-Examination Based Recommendations (n=21) (Radiation instruction, continuing medical education) | Alaska, Arizona, Colorado, Connecticut, Florida, Illinois, Kentucky, Maine, Massachusetts, Mississippi, Nebraska, New York, New Jersey, Ohio, Oregon, Pennsylvania, South Carolina, Tennessee, Texas, Vermont, West Virginia |
| No regulations (n=29) | Alabama, Arkansas, Delaware, District of Columbia, Georgia, Hawaii, Idaho, Indiana, Iowa, Kansas, Louisiana, Maryland, Michigan, Minnesota, Missouri, Montana, Nevada, New Hampshire, New Mexico, North Carolina, North Dakota, Oklahoma, Rhode Island, South Dakota, Utah, Virginia, Washington, Wisconsin, Wyoming |
DISCUSSION
Medical radiation exposure in the US has increased significantly over the past three decades as a consequence of increased utilization of radiologic studies and radiation based therapies.6,22 Radiation exposure can result in significant detrimental health consequences including cancer,7 and it is believed that up to 2% of cancers in the US may be attributable to CT scans alone.6,7 Controlled in vitro and in vivo experiments have demonstrated that exposure to high dose ionizing radiation is associated with genomic instability and an increased risk of developing some types of cancer.2,3 These risks are associated with both high-dose-rate radiation exposure and the low-dose-rate exposure which results from fluoroscopy during procedures such as ERCP.23 Medical radiation exposure has therefore become an issue of increasing public health concern. The radiology community has responded vigorously to the concern of excessive population radiation exposure by establishing appropriateness criteria for ordering CT scans, creating decision support software, educating its membership with awareness campaigns, developing educational websites, and implementing dose registries which allow individual institutional radiation utilization to be compared with national averages.8,10–12
Within the realm of interventional endoscopy, ERCP is the most commonly performed procedure requiring fluoroscopy. Therapeutic ERCP has been associated with even greater radiation exposure than abdominal CT scans,13 and the proportion of therapeutic ERCPs has increased significantly over the last decade, making ERCP-associated radiation exposure an issue of escalating relevance.1,24 Radiation protection practices and training for U.S. endoscopists performing ERCP have not been previously characterized.
Radiation training tailored to endoscopic needs is a necessary and key prerequisite to making patient and endoscopist radiation protection a central tenant of therapeutic endoscopy practice. The Joint Commission of the Accreditation of Healthcare Organizations (JCAHO) has previously recommended that all physicians and technicians who prescribe diagnostic radiation or use diagnostic radiation equipment receive dosing education and are trained on the specific model of equipment being used.25 However, this survey highlights the current lack of radiation/fluoroscopy system training among therapeutic endoscopists, both at the fellowship level and also subsequently at the healthcare facility of employment, with the majority indicating an absence of formal training in operation of their institution’s fluoroscopy system. This lack of training is more evident in non-university practice settings where only 30% of respondents indicated receiving training in operating their institution’s fluoroscopy system. Despite the widespread sentiment among endoscopists that training in use of their fluoroscopy system would be beneficial, it appears that few are receiving it. Such training need not be protracted, difficult or burdensome. We previously demonstrated that even a brief 20 minute educational program on minimizing radiation by optimizing fluoroscopy system settings (image frame rate, magnification and collimation), resulted in a marked decrease in ERCP associated radiation exposure.26
In particular, endoscopists can minimize radiation exposure by implementing best practices listed in Table 4. Appropriate shielding of staff with radiation protection aprons and mobile shields is essential and distance of staff from the patient should be maximized where possible. The main source of staff radiation exposure is scatter radiation originating from the patient. Therefore minimizing patient radiation exposure is of paramount importance. Fluoroscopy machine best practices should be implemented including using pulse fluoroscopy at the lowest possible frame rate setting and tapping the fluoroscopy pedal intermittently and only when necessary. Using a lower frame rate has been shown to have no impact on image quality in gastrointestinal and cardiovascular interventions.27,28 Additionally image collimation and lower magnification should be utilized, all of which will result in significantly lower patient radiation exposure.29 The FT should be included in the procedure report as per the recommendations of the ASGE.16 As lowering frame rate, collimation and use of lower magnification will decrease overall radiation exposure for any given FT, institutions should ideally also record the DAP (product of radiation dose and areas to which it is applied]. Therapeutic endoscopy fellows comprised 8.8% of all respondents to this survey. Although the number of fellow respondents was small, these data nevertheless provide a window into the state of radiation protection and training for fellows. A larger proportion of fellows than attendings (78.6% vs 54.5%) appear to have received no formal training in use of their institution’s fluoroscopy equipment, and consequently the majority were even unaware if their fluoroscopy systems offered settings that modulate and decrease radiation dose. These findings highlight an opportunity for therapeutic endoscopy fellowship programs to improve their curriculum by including training in radiation protection and in the operation of fluoroscopy equipment.
TABLE 4.
Tips for Optimizing Fluoroscopy Safety
| Confirm that everyone in the room is wearing lead |
| Ensure that the fluoroscopy image intensifier is as close to the patient as possible |
| Set magnification to lowest possible setting |
| Make sure that the image is collimated to the minimum field necessary for visualization during the procedure |
| Utilize pulse fluoroscopy settings and ensure image frame rate to lowest possible setting (typically 4/ sec) |
| Tap fluoroscopy pedal intermittently rather than holding the pedal down continuously |
| Make sure that each person in the room is standing as far from the fluoroscopy machine as possible for his/her role. |
Approximately 40% of endoscopists indicated that radiology technicians operated fluoroscopy equipment at their institutions. A recent study demonstrated significantly lower radiation exposure during ERCP when endoscopists rather than radiology technicians operate fluoroscopy,30 underscoring the importance and desirability of endoscopist-directed fluoroscopy. Nevertheless, even when radiology technicians operate fluoroscopy, the attending endoscopist is ultimately responsible for all aspects of patient care and safety including radiation exposure, an element which has not previously been sufficiently emphasized. Recent studies have indicated that a visual cue (flashing light) which is activated during fluoroscopy utilization results in less radiation exposure during ERCP.31 Additional studies focused on practices which minimize radiation exposure during ERCP would be of great interest and benefit to patients and providers.
Endoscopists appear to practice adequate personal radiation protection, with 98% of respondents consistently wearing a lead apron and thyroid shield when performing ERCPs. Additionally, apron storage was appropriate with the vast majority indicating that hangers were utilized for lead apron storage to minimize the risk of apron cracking. Approximately 60% of respondents reported that they use the recommended two-piece wrap apron,32 which provides optimal radiation protection and ergonomics, by allowing distribution of the weight of the apron across both the upper and lower body. Just over one quarter of respondents reported wearing a one-piece wrap apron, which is ergonomically less sound, as it can result in upper body and neck muscle strain. 13.2% of respondents reported wearing a one-piece frontal cover only lead apron which is suboptimal as it provides only frontal radiation protection, leaving endoscopists vulnerable to scatter radiation laterally/posteriorly as well as to increased ergonomic strain. Overall, our data indicate that 40% of respondents are using lead aprons that provide either suboptimal radiation protection or put them at some risk for long term ergonomic injury. Lead shielding and curtains can significantly reduce scatter radiation to endoscopists and staff;33,34 however, only 40% of respondents utilize these additional protective measures.
Lead glasses offer protection against radiation-induced cataract formation and also offer splash protection. Our data indicate that almost 80% of respondents do not always wear lead glasses when performing ERCP. Some studies indicate that lead glasses are most necessary for protection against radiation-induced cataract formation for individuals who accrue an annual fluoroscopy time of >59.4 hours.35 Assuming a mean fluoroscopy time of 5 minutes per procedure, roughly 700 annual ERCPs would be needed to exceed this threshold. Based on self-reported procedure volumes in our study, many therapeutic endoscopists would not be expected to reach this threshold. However, further research in this area would be informative.
It is noteworthy that over a quarter of endoscopists rarely or never wore a radiation dosimeter. Dosimeter use amongst interventional specialties varies, and likely reflects both differences in radiation education as well as perceived risk and concern regarding amount of occupational radiation exposure by the members of each specialty. Interventional cardiologists and radiologists are exposed to much higher levels of radiation compared to endoscopists, and not surprisingly, higher proportions of these interventionalists utilize dosimeters.36, 37 The widely utilized passive dosimetry adequately monitors overall radiation exposure, but the infrequent three-monthly or yearly feedback provided may be less effective in motivating consistent use of the dosimeter. Dosimeters which provide immediate postprocedural radiation dose readings are commercially available; these may potentially promote both increased dosimeter utilization as well as minimization of patient and provider radiation exposure.38
Governmental regulation of fluoroscopy use and certification varies considerably across the United States. Our telephone survey of state radiologic regulatory agencies indicated that only 41.2% of US states have certification/training requirements for non-radiologist physicians operating fluoroscopy. Additionally, California is the only state with an educational curriculum on radiation/fluoroscopy, and non-radiologist physicians are required to pass a formal written examination prior to certification for operation of fluoroscopy equipment. Such a formal curriculum and certification process may be a desirable requirement, as it offers the best opportunity for endoscopists to acquire knowledge of the risks associated with radiation use, as well as methods to minimize radiation exposure. Our data additionally suggest low prevailing thresholds in healthcare facilities for credentialing endoscopists in fluoroscopy use. Endoscopist familiarity with the fluoroscopy systems they use or oversee is suboptimal, highlighting a potential target for minimizing radiation exposure through education. Implementation of fluoroscopy system-specific training by healthcare facilities will result in lower patient and provider radiation exposure and a safer practice environment.
Limitations of this study include the self-reported nature of responses and the typical sources of bias present in any survey study, which are often not amenable to quantification. These include sampling/coverage error, non-responder bias, and limitations associated with question/response wording and post-survey analysis. The survey was kept deliberately brief (~3 minutes) to enhance the response rate from this respondent population of busy therapeutic endoscopists. Due to limitations in survey length, we could not query all points of potential interest or availability of equipment at each institution and therefore prioritized questions included in the survey. California state was disproportionately represented among the respondents (25% of respondents) and not all states were represented. High volume, experienced endoscopists were also disproportionately represented, with over 45% of respondents performing over 200 ERCPs per year and more than half of respondents reporting over 10 years of experience in performing therapeutic endoscopy. Lower volume and less experienced endoscopists may reasonably be expected to have less familiarity with fluoroscopy equipment and minimizing procedural radiation use than the majority of endoscopist respondents to this survey.26,39 Therefore, the data we present here may reflect the ‘best-case’ scenario with respect to radiation protection, fluoroscopy equipment training and use patterns of endoscopists. State-specific fluoroscopy certification information was obtained by reviewing online information on each state’s radiologic health branch website, and also by direct telephone contact of the radiation health agency in each state. It is possible that radiologic health branch personnel responding to our queries in each state may lack comprehensive knowledge regarding certification requirements and endoscopists should clarify current guidelines for their own states.
Over recent decades, management of the fluoroscopy component of ERCP is increasingly becoming the responsibility of endoscopists. Although best suited for this task, endoscopists lack the rigorous education in radiation safety and protection which radiologists receive. Our findings suggest that nationwide fluoroscopy training and credentialing practices for endoscopists are highly variable and could be significantly improved. Gastroenterology societies may consider developing quality guidelines for fluoroscopy use during endoscopic procedures. Additionally, consideration could be given to creation of a therapeutic endoscopy fellowship curriculum and board certification process which incorporates formal radiation training. These measures may be expected to result in effective educational programs, and minimize radiation exposure during GI endoscopy by improving adherence to the ALARA principle.
Fig. 3:
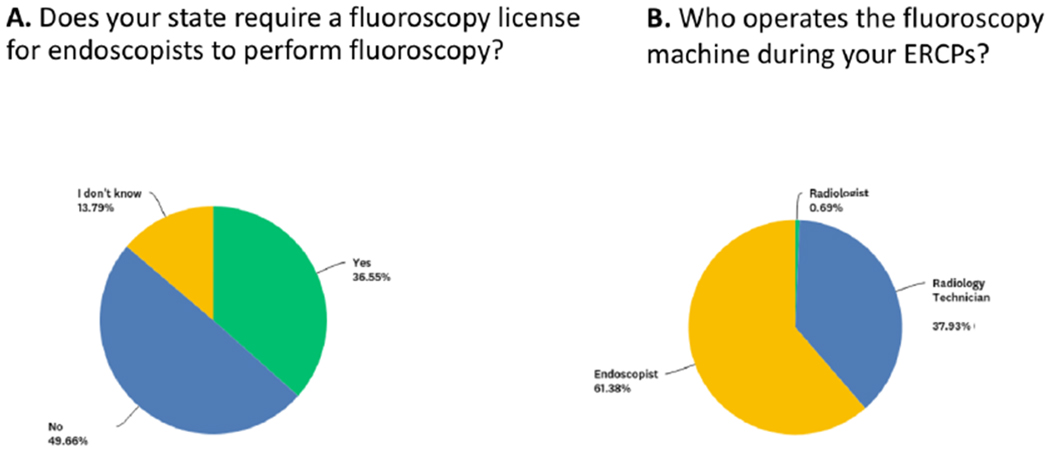
Pie charts reflecting overall (fellow + attending) responses to the indicated survey questions regarding a fluoroscopy certification and b fluoroscopy operation practices
Acknowledgement of Financial Support:
This work was supported by a NIH T32 Training Grant (DK007056) supporting MTB.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest:
None of the authors have conflicts of interest to declare.
Disclosures
Saurabh Sethi: No corporate/commercial relationships to declare
Monique T. Barakat: No corporate/commercial relationships to declare
Shai Friedland: Consultant, Boston Scientific
Subhas Banerjee: Consultant and Research Support, Boston Scientific
References
- 1.Ho IK, Cash BD, Cohen H, et al. Radiation exposure in gastroenterology: improving patient and staff protection. Am J Gastroenterol 2014;109:1180–94. [DOI] [PubMed] [Google Scholar]
- 2.Bouffler S, Silver A, Cox R. Mechanistic and genetic studies of radiation tumorigenesis in the mouse--implications for low dose risk estimation. J Radiol Prot 2002;22:A11–6. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe D, Bowden GT. Ionizing radiation as an initiator: effects of proliferation and promotion time on tumor incidence in mice. Cancer Res 1987;47:6692–6. [PubMed] [Google Scholar]
- 4.Richardson DB, Cardis E, Daniels RD, et al. Risk of cancer from occupational exposure to ionising radiation: retrospective cohort study of workers in France, the United Kingdom, and the United States (INWORKS). BMJ 2015;351:h5359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schauer DA, Linton OW. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology 2009;253:293–6. [DOI] [PubMed] [Google Scholar]
- 6.Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med 2009;169:2071–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84. [DOI] [PubMed] [Google Scholar]
- 8.Bhargavan-Chatfield M, Morin RL. The ACR Computed Tomography Dose Index Registry: the 5 million examination update. J Am Coll Radiol 2013;10:980–3. [DOI] [PubMed] [Google Scholar]
- 9.Bruner A, Sutker W, Maxwell G. Minimizing patient exposure to ionizing radiation from computed tomography scans. Proc (Bayl Univ Med Cent) 2009;22:119–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chintapalli KN, Montgomery RS, Hatab M, et al. Radiation dose management: part 1, minimizing radiation dose in CT-guided procedures. AJR Am J Roentgenol 2012;198:W347–51. [DOI] [PubMed] [Google Scholar]
- 11.Little BP, Duong PA, Knighton J, et al. A Comprehensive CT Dose Reduction Program Using the ACR Dose Index Registry. J Am Coll Radiol 2015;12:1257–65. [DOI] [PubMed] [Google Scholar]
- 12.Nolan DJ. Minimizing radiation in diagnostic radiology. Br J Hosp Med 1991;45:337. [PubMed] [Google Scholar]
- 13.Larkin CJ, Workman A, Wright RE, et al. Radiation doses to patients during ERCP. Gastrointest Endosc 2001;53:161–4. [DOI] [PubMed] [Google Scholar]
- 14.Saurabh Sethi SF, Banerjee Subhas. US survey assessing current ERCP-related radiation protection practices. Gastrointest Endosc 2015;81:AB352. [Google Scholar]
- 15.Dumonceau JM, Garcia-Fernandez FJ, Verdun FR, et al. Radiation protection in digestive endoscopy: European Society of Digestive Endoscopy (ESGE) guideline. Endoscopy 2012;44:408–21. [DOI] [PubMed] [Google Scholar]
- 16.Adler DG, Lieb JG 2nd, Cohen J, et al. Quality indicators for ERCP. Gastrointest Endosc 2015;81:54–66. [DOI] [PubMed] [Google Scholar]
- 17.Adler DG, Lieb JG 2nd, Cohen J, et al. Quality indicators for ERCP. Am J Gastroenterol 2015;110:91–101. [DOI] [PubMed] [Google Scholar]
- 18.Weltermann BM, Rock T, Brix G, et al. Multiple procedures and cumulative individual radiation exposure in interventional cardiology: A long-term retrospective study. Eur Radiol 2015;25:2567–74. [DOI] [PubMed] [Google Scholar]
- 19.Morishima Y, Chida K, Katahira Y, et al. Need for radiation safety education for interventional cardiology staff, especially nurses. Acta Cardiol 2016;71:151–5. [DOI] [PubMed] [Google Scholar]
- 20.Valuckiene Z, Jurenas M, Cibulskaite I. Ionizing radiation exposure in interventional cardiology: current radiation protection practice of invasive cardiology operators in Lithuania. J Radiol Prot 2016;36:695–708. [DOI] [PubMed] [Google Scholar]
- 21.Jacobs AK, Babb JD, Hirshfeld JW Jr., et al. Task force 3: training in diagnostic and interventional cardiac catheterization endorsed by the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2008;51:355–61. [DOI] [PubMed] [Google Scholar]
- 22.Mettler FA Jr., Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources--1950-2007. Radiology 2009;253:520–31. [DOI] [PubMed] [Google Scholar]
- 23.Cardis E, Gilbert ES, Carpenter L, et al. Effects of low doses and low dose rates of external ionizing radiation: cancer mortality among nuclear industry workers in three countries. Radiat Res 1995;142:117–32. [PubMed] [Google Scholar]
- 24.Huang RJ, Thosani NC, Barakat MT, et al. Evolution in the Utilization of Biliary Interventions in the United States: Results of a Nationwide Longitudinal Study from 1998 to 2013. Gastrointest Endosc 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radiation Risks of Diagnostic Imaging. The Joint Commission Sentinel Event Alert 2011. [PubMed] [Google Scholar]
- 26.Barakat MT, Thosani NC, Huang RJ, et al. Effects of a Brief Educational Program on Optimization of Fluoroscopy to Minimize Radiation Exposure During Endoscopic Retrograde Cholangiopancreatography. Clin Gastroenterol Hepatol 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schultz C, Dixon S. SU-F-I-77: Radiation Dose in Cardiac Catheterization Procedures: Impact of a Systematic Reduction in Pulsed Fluoroscopy Frame Rate. Med Phys 2016;43:3404. [Google Scholar]
- 28.Boland GW, Murphy B, Arellano R, et al. Dose reduction in gastrointestinal and genitourinary fluoroscopy: use of grid-controlled pulsed fluoroscopy. AJR Am J Roentgenol 2000;175:1453–7. [DOI] [PubMed] [Google Scholar]
- 29.Thosani N, Chen AM, Friedland S, Banerjee S. Prospective Evaluation of Predictors of Increased Patient Radiation During ERCP: the Stanford ERCP Radiation Safety (Sers) Study. Gastrointestinal Endoscopy 2014;79(5):AB340–AB341. [Google Scholar]
- 30.Norton I, Bell CJ, Cho S, Kim B, Erdman K . Proceduralist-driven Fluoroscopy Significantly Reduces Irradiation During ERCP. Gastrointest Endosc 2018. [Google Scholar]
- 31.Zeng HZ, Liu Q, Chen HL, et al. A pilot single-center prospective randomized trial to assess the short-term effect of a flashing warning light on reducing fluoroscopy time and radiation exposure during ERCP. Gastrointest Endosc 2018;88:261–266. [DOI] [PubMed] [Google Scholar]
- 32.Alexandre D, Prieto M, Beaumont F, et al. Wearing lead aprons in surgical operating rooms: ergonomic injuries evidenced by infrared thermography. J Surg Res 2017;209:227–233. [DOI] [PubMed] [Google Scholar]
- 33.Kurihara T, Itoi T, Sofuni A, et al. Novel protective lead shield and pulse fluoroscopy can reduce radiation exposure during the ERCP procedure. Hepatogastroenterology 2012;59:709–12. [DOI] [PubMed] [Google Scholar]
- 34.Muniraj T, Aslanian HR, Laine L, et al. A double-blind, randomized, sham-controlled trial of the effect of a radiation-attenuating drape on radiation exposure to endoscopy staff during ERCP. Am J Gastroenterol 2015;110:690–6. [DOI] [PubMed] [Google Scholar]
- 35.Garg MS, Patel P, Blackwood M, et al. Ocular Radiation Threshold Projection Based off of Fluoroscopy Time During ERCP. Am J Gastroenterol 2017;112:716–721. [DOI] [PubMed] [Google Scholar]
- 36.Bordoli SJ, Carsten CG 3rd, Cull DL, et al. Radiation safety education in vascular surgery training. J Vasc Surg 2014;59:860–4. [DOI] [PubMed] [Google Scholar]
- 37.Morin RL, Mahesh M. Radiation Exposure and Patient Dose in Cardiology. J Am Coll Radiol 2017. [DOI] [PubMed] [Google Scholar]
- 38.Pradhan AS, Lee JI, Kim JL. On the scenario of passive dosimeters in personnel monitoring: Relevance to diagnostic radiology and fluoroscopy-based interventional cardiology. J Med Phys 2016;41:81–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liao C, Thosani N, Kothari S, et al. Radiation exposure to patients during ERCP is significantly higher with low-volume endoscopists. Gastrointest Endosc 2015;81:391–8 e1. [DOI] [PubMed] [Google Scholar]


