Abstract
Objective: To study the cases of H1N1 influenza admitted in our hospital. Method: Hospital records of all the admitted patients diagnosed as H1N1 positive by throat swab rt-PCR (real time polymerase chain reaction) were retrospectively studied. Results: Between November 2009 and February 2010 total 62 children were hospitalized with 2009 H1N1 influenza virus infection. Of the admitted children, 19 (30.6%) were admitted in ICU and 4 (6.4%) expired. Consolidation was observed in 25 (40%) cases while 4 (6%) patients had pleural effusion and 1 patient each developed pneumothorax and pulmonary edema. Conclusions: Pandemic 2009 H1N1 influenza caused serious respiratory complications in children not usually seen with seasonal influenza.
Keywords: H1N1 Pandemic 2009, H1N1 influenza, pleural effusion
In March 2009, a new strain of influenza was detected in Mexico which caused severe respiratory illness in humans. The first case of 2009 H1N1 pandemic influenza was reported by CDC on April 21 2009 after which this virus spread to various parts of the world and affected people of all ages [1–4]. It reached India as well and spread to various parts of the country causing mild to severe respiratory illness. Till date, >30 000 persons have been diagnosed with this infection in India, out of which 1443 had died [5]. Usually influenza virus does not cause severe respiratory illness but during this pandemic many developed fatal complications. Thus, we studied children admitted to our hospital who were diagnosed as H1N1 positive.
Methods
Ours is a tertiary health center for children in western Rajasthan. Pandemic 2009 H1N1 influenza virus outbreak started in October 2009 in our region. In November 2009, first cases of H1N1 in children were seen at our centre following which there were frequent similar cases. A total of 1532 patients were clinically screened out, of whom 196 were admitted in hospital and investigated. Of admitted cases, 62 (32%) were found to be H1N1 positive and here we have studied the effect of H1N1 virus on these cases retrospectively. The study period involve cases from November 2009 to February 2010. Cases of 2009 H1N1 influenza were confirmed by testing throat swabs with the use of real time polymerase chain reaction. The study was conducted as a retrospective public health analysis of the identified data, so approval by the institutional review board at each participating institution and informed consent were not required.
Results
A total of 62 pediatric patients with confirmed H1N1 influenza were studied. Of the 62 cases, 47 (76%) were male and 15 (24%) female. The mean age of the cases was 68.9 ± 49.5 months, ranging from 6 to 216 months. Most of the cases (82%) were between 1 and 10 years of age with very few cases outside this range. Of the pre-existing conditions, 9% had recurrent wheeze associated respiratory infections (WARI) or bronchial asthma. Out of 62 cases, 30 (48%) had anemia, but severe anemia was seen in only 7% children. None of the children had heart disease or immunosuppressive conditions. Out of 62, 30 (48%) were malnourished but only 5% were severely malnourished (Table 1).
Table 1.
Epidemiologic features and pre-existing conditions in children hospitalized with 2009 H1N1 influenza
| Variables | Males | Females | Total |
|---|---|---|---|
| Age of the patient (months) | |||
| Mean ± SD | 66.2 ± 50.4 | 77.6 ± 47.3 | 68.9 ± 49.5 |
| Range | 6–180 | 30–216 | 6–216 |
| Sex of the patient, n (%) | 47 (76) | 15 (24) | 62 |
| Pre-existing condition (if any)a, n (%) | |||
| Asthma/recurrent WARI | 4 (9) | Nil | 4 (7) |
| Anemia | 18 (38) | 12 (80) | 30 (48) |
| Hemoglobin 9–11 g% | 11 (61) | 8 (67) | 19 (63) |
| Hemoglobin 6–9 g% | 5 (28) | 4 (33) | 9 (30) |
| Hemoglobin <6 g% | 2 (11) | Nil | 2 (7) |
| Tuberculosis | 2 | Nil | 2 |
| Heart disease | Nil | Nil | Nil |
| Immunosuppression | Nil | Nil | Nil |
| Malnutrition, n (%) | 22 (47) | 8 (53) | 30 (48) |
| Grade I, n (%) | 9 (19) | 3 (20) | 12 (19) |
| Grade II, n (%) | 7 (15) | 3 (20) | 10 (16) |
| Grade III, n (%) | 4 (9) | 1 (6) | 5 (8) |
| Grade IV, n (%) | 2 (4) | 1 (6) | 3 (5) |
aSome children had more than one pre-existing condition.
Most common signs and symptoms on admission included fever (in 98%) and cough (in 94%). Of all children, 32% had complaint of difficulty in respiration. Other symptoms observed were myalgia, headache and vomiting (Table 2). On examination, 66% cases had crepitations and 42% had wheezing. Hypoxemia was observed in 31% cases at admission (Table 2).
Table 2.
Clinical signs and symptoms and respiratory complications in children hospitalized with 2009 H1N1 influenza
| Variables | <1 year | 1–5 years | >5 years | Total |
|---|---|---|---|---|
| (N = 4), n (%) | (N = 30), n (%) | (N = 28), n (%) | (N = 62), n (%) | |
| Fever | 4 (100) | 30 (100) | 27 (96) | 61 (98) |
| Cough | 4 (100) | 29 (96) | 25 (89) | 58 (94) |
| Difficulty in respiration | 4 (100) | 8 (27) | 8 (29) | 20 (32) |
| Myalgia | Cannot tell | 1 (3) | 8 (29) | 9 (16) |
| Headache | Cannot tell | Nil | 9 (32) | 9 (16) |
| Diarrhea | Nil | 1 (3) | Nil | 1 (2) |
| Vomiting | 1 (25) | 3 (10) | 5 (18) | 9 (16) |
| Respiratory Complications | ||||
| Wheezing | 2 (50) | 20 (67) | 4 (14) | 26 (42) |
| Bronchopneumonia | 4 (100) | 20 (67) | 17 (61) | 41 (66) |
| Empyema/pleural effusion | Nil | 2 (7) | 2 (7) | 4 (6) |
| Pneumothorax | Nil | Nil | 1 (4) | 1 (2) |
| Hypoxemiaa | 3 (75) | 7 (23) | 9 (32) | 19 (31) |
aSpO2 <93% on ambient air was considered hypoxemia.
On investigations, mean hemoglobin of admitted patients was 10.3 ± 2.1 gdl−1, ranging from 5.8 to 14.1 gdl−1. Mean leukocyte count was 9702 ± 5579.7 cmm−1. Total leukocyte count was >15 000 cmm−1 in 8 (13%) cases while it was <4000 cmm−1 in 6 (10%) (Table 3). On chest X-ray, consolidation was found in 25 (40%) patients; out of these cases, 12 patients (48%) had bilateral consolidation while 10 (40%) patients had right lung consolidation. Left lung consolidation was seen in three (12%) patients only. Of other complications, four (6%) cases had pleural effusion and one patient each developed pneumothorax and pulmonary edema (Table 3).
Table 3.
Lab results and X-ray findings of children hospitalized for H1N1 influenza
| Variables | |
|---|---|
| Hemoglobin (g%) | |
| Mean ± SD | 10.3 ± 2.1 |
| Range | 5.8–14.1 |
| Leukocyte count (cells/cmm) | |
| Mean ± SD | 9702 ± 5579.7 |
| Range | 2190–26 100 |
| X-ray findings, n (%) | |
| Perihilar infilteration | 4 (6) |
| Consolidation | 25 (40) |
| Right | 10 (40) |
| Left | 3 (12) |
| Bilateral | 12 (48) |
| Pleural Effusion/empyema | 4 (6) |
| Pneumothorax | 1 (2) |
| Pulmonary edema | 1 (2) |
Infants constituted only 6% of the studied cases while majority of patients were 1–5 years of age, closely followed by children from 5 to 10 years. Children >10 years were also less affected making only 11% of the diagnosed cases. However, severity of illness was more in infants as well as children from 1 to 10 years while in children >10 years, it was not as severe as none of the child >10 years required ICU admission. Maximum ICU admissions (38%) were among children in 5–10 year age group and similarly highest mortality (3 out of 21 i.e. 14%) was also among this age group. None of the children <1 year or >10 years of age expired (Fig. 1).
Fig. 1.
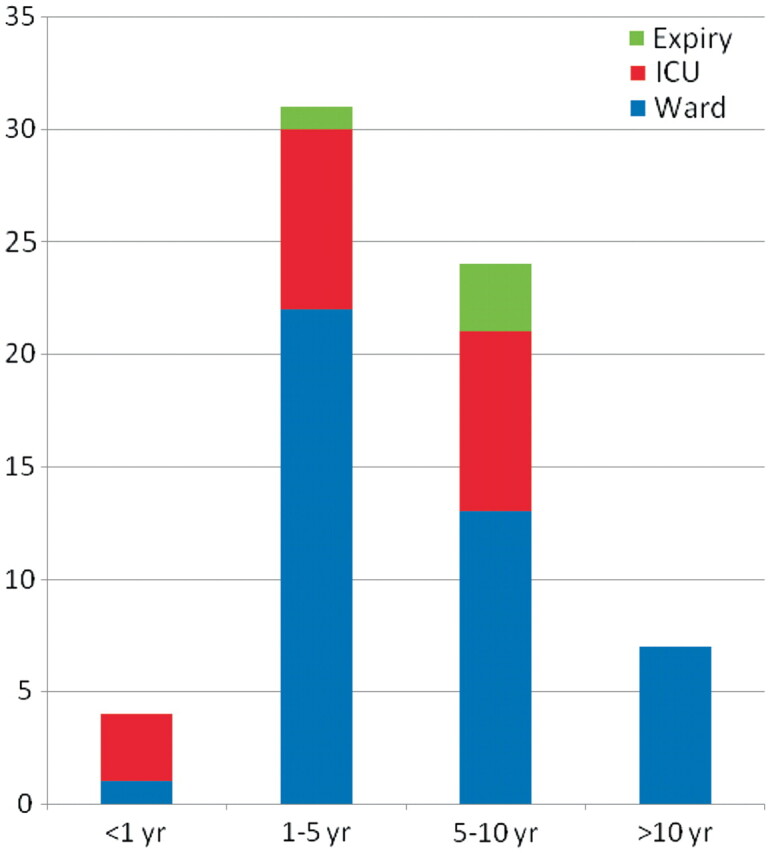
Chart showing severity of illness and fate of the children as per age.
Discussion
Our study indicates that children are prone to develop severe respiratory illness after infection with 2009 H1N1 influenza. Although we do not have the exact data to compare case with seasonal influenza getting admitted at our center, definitely admission rates of children with 2009 H1N1 influenza was higher than those with seasonal influenza every year. As is consistent with our current study, a study in Argentina among 2009 H1N1positive pediatric population, admission rates were high as compared to their previous years admission [3].
Fever is the commonest symptom followed by cough as seen in our as well as other studies all over the world [3, 6, 7]. A few cases may develop symptoms like myalgia, headache, diarrhea and vomiting but these are not so common. The system mainly affected is respiratory system leading to respiratory complications. The most common respiratory complication in our study was bronchopneumonia as seen in 66% cases and lung consolidation was observed in 40% cases. Surprisingly, right lung was observed to be more commonly affected in comparison to left lung. The same finding was reported in a study in Argentina where 55% children had right lung involved, whereas only 16% had involvement of left lung only. Similarly in our study, isolated involvement of right lung was seen in 40% cases, whereas isolated left lung involvement was seen in 12% cases only. This may have something related to right bronchus being wider and straighter in comparison to left main bronchus, and aspiration of secretions rather than hematogenous spread may well be a mechanism of development of consolidation in these cases.
It has been said that children with asthma, immunosupression and neurological disorders are more at risk to infection with 2009 H1N1 influenza [8], but in our study only 9% diagnosed cases had either established bronchial asthma or recurrent attacks of WARI. None of the child had any immunosuppressive state and only 5% diagnosed cases were severely malnourished.
Children at younger age are thought to be more susceptible to infection, but surprisingly infants constituted only 6% of diagnosed cases. The same has been the data from various parts of India where of total diagnosed cases, only 10% were children <5 years of age and maximum cases were between 5 and 40 years of age [5]. We observed that maximum ICU admissions were among 5–10 year age group and as expected mortality was highest among them. The same has been reported from the United States, where maximum pediatric mortality due to 2009 H1N1 infection was among 5–11 years of age and children <2 years contributed <20% pediatric deaths [9]. This also supports that 2009 H1N1 influenza infection is not as severe in younger children as it was expected and further studies are required to look into the issue.
In conclusion, 2009 H1N1 infection can lead to fatal complications in children and may even cause death. General measures should be stressed upon, such as educating people about hygiene and cleanliness, distancing, adequate room ventilation and use of masks for those in close contact with patients with respiratory illness [10]. Besides, vaccine has been developed against 2009 H1N1 influenza and preliminary data have shown good efficacy in children with the use of one dose of 15 µg in children between 9 and 17 years and single dose of 7.5 µg among children between 3 and 8 years of age [11]. World Health Organization is coordinating the distribution of donated pandemic influenza vaccine to eligible countries to help countries protect people from developing severe disease from pandemic influenza H1N1 infection [12]. All these collective efforts will hopefully prevent any further outbreak and at least, such high-mortality rates will not be seen.
References
- 1. Outbreak of 2009 pandemic influenza A (H1N1) at a school - Hawaii, May 2009. MMWR Morb Mortal Wkly Rep 2010;58:1440–4. [PubMed] [Google Scholar]
- 2.Perez-Padilla R, de la Rossa-Zamboni D, de Leon SP, et al. Pneumonia and respiratory failure from Swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361:680–9. doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 3.Libster R, Bugna J, Coviello S, et al. Pediatric hospitalizations associated with 2009 Pandemic Influenza A (H1N1) in Argentina. N Engl J Med. 2010;362:45–55. doi: 10.1056/NEJMoa0907673. [DOI] [PubMed] [Google Scholar]
- 4.Pandemic (H1N1) 2009 –update 95. [(7 April 2010, date last accessed)]. World Health Organisation. http://www.who.int/csr/don/2010_04_09/en/index.html. [Google Scholar]
- 5.Situational update on H1N1, 28 March 2010. [(7 April 2010, date last accessed)]. Ministry of Health and Family Welfare, Government of India. http://india.gov.in/outerwin.php?id=http://mohfw-h1n1.nic.in. [Google Scholar]
- 6.Lessler J, Reich NG. Cummings DAT and the New York City Department of Health and Mental Hygiene Swine Influenza Investigation Team. Outbreak of 2009 Pandemic Influenza A (H1N1) at a New York City School. N Engl J Med. 2009;361:2628–36. doi: 10.1056/NEJMoa0906089. [DOI] [PubMed] [Google Scholar]
- 7.Cauchemez S, Donnelly CA, Reed C, et al. Household transmission of 2009 Pandemic Influenza A (H1N1) Virus in the United States. N Engl J Med. 2009;361:2619–27. doi: 10.1056/NEJMoa0905498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Who is more at risk of severe illness? What about other risks? World Health Organisation. [(7 April 2010, date last accessed)]. http://www.who.int/csr/disease/swineflu/frequently_asked_questions/risk/en/index.html. [Google Scholar]
- 9.Fluview. A weekly influenza surveillance report prepared by the Influenza Division. [(7 April 2010, date last accessed)]; 2009-2010 Influenza season week 13 ending April 3 2010. CDC. http://www.cdc.gov/flu/weekly/pdf/External_F1013.pdf. [Google Scholar]
- 10.Clinical management of human infection with pandemic (H1N1) revised guidance. [(7 April 2010, date last accessed)];World Health Organisation. 2009 http://www.who.int/csr/resources/publications/swineflu/clinical_management/en/index.html. [Google Scholar]
- 11.Arguedas A, Soley C, Linder K. Responses to 2009 H1N1 vaccine in children 3 to 17 years of age. N Engl J Med. 2010;362:4. doi: 10.1056/NEJMc0909988. [DOI] [PubMed] [Google Scholar]
- 12.Pandemic (H1N1) 2009 vaccine deployment update-31 March 2010. World Health Organisation. [(7 April 2010, date last accessed)]; http://wwwwho.int/csr/disease/swineflu/action/h1n1_vaccine_deployment_update20100331.pdf. [Google Scholar]


