To the Editor:
Catastrophic events disrupt the neurosurgeon's ability to provide clinical care. Events such as natural disaster, mass casualty, war, and even pandemic, constitute humanitarian emergencies that threaten every aspect of care delivery. Neurosurgeons may face shortages of critical resources, including access to surgical supplies, staff, operating rooms, and intensive care beds. Accordingly, neurosurgeons are forced into the difficult position of deciding how to deploy essential resources when supply is insufficient to cover the demand. This is known as neurosurgical triage.
Triage is a key principle in the medical management of disasters. Yet, despite the obvious life-saving implications, there is no universal agreement on how neurosurgical patients should be triaged. Further, existing triage algorithms focus on initial field assessments of patients, well before neurosurgeons are consulted. Here we consider neurosurgical triage drawing upon insights from military and emergency medicine to create principles specific to our patient population facing disaster scenarios. Appreciating the implications of triage during resource scarcity will become an essential skill for neurosurgeons.
BACKGROUND
The topic of surgical triage has been examined in the context of mass casualty and battlefield medicine extensively.1 Deriving from trier, French for “separating out,” the literal definition of triage is the act of sorting items according to quality. In the setting of disaster, triage refers to the prioritization of services and supplies based upon the need for treatment and likelihood of a good prognosis.2,3
Neurosurgeons are uncommonly involved in primary or secondary triage – that is, battlefield and prehospital triage. In these settings, front line paramedics apply a triage sieve to sort the walking wounded from more severely injured patients. In this United States, the Move Assess Sort Send Adult triage method is widely adopted.4 This method assesses patients based on their ability to walk, the presence of spontaneous respirations, the respiratory rate, the presence of peripheral vascular perfusion, and mental status. Similar systems, such as the Sort Assess Lifesaving intervention and Treatment/Transport, introduced by the Centers for Disease Control in 2008, are also utilized. Central to all triage systems is the principle of classification and prioritization of individuals in need of medical care.5
Neurosurgeons can be expected to be involved in the third stage of triage: determining the order of care and level of services provided within the hospital setting. For a comprehensive review of prehospital triage systems, readers are referred to Bazyar et al1,5 Here we define the guiding principles of neurosurgical triage.
Neurosurgical Triage Considerations
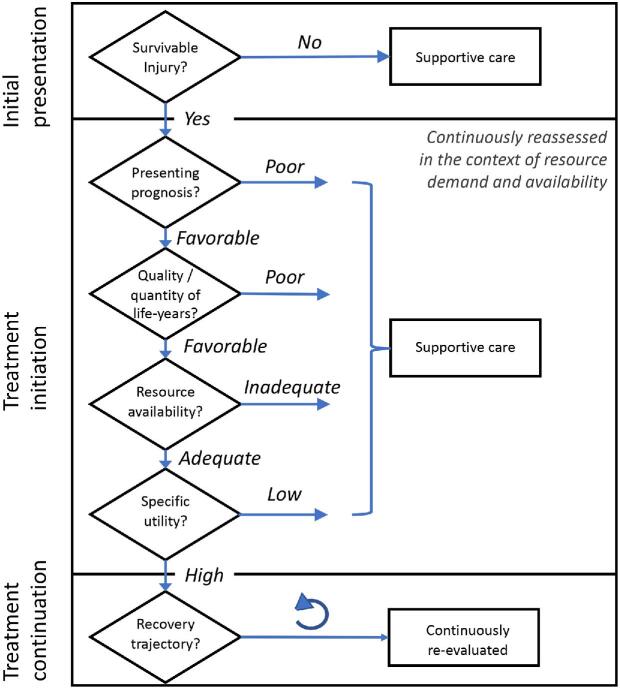
The types of triage decisions required of neurosurgeons evolve over the patient's clinical course. There are at least 3 time points when triage decisions must be made – the initial presentation, the initiation of treatment, and the continuation of treatment.
Initial Presentation
Neurosurgeons face their first triage decision during the initial patient presentation for neurosurgical care. This occurs in the form of a consultation from the emergency room (ER) or intensive care unit (ICU). The initial assessment answers the immediate question of whether the neurological injury is survivable. Examples of conditions which have a low probability of survival include penetrating missile injuries (ie, gunshot wound) to the head6 and atlanto-occipital dislocation.7 Exceptions to this generalization exist. However, in a time of disaster, injuries associated with a low probability of survival are assigned a lower treatment priority, thus permitting the allocation of resources to individuals with higher probability of survival.
Treatment Initiation
To provide guidance on triage decisions after an injury is deemed survivable, the surgeon must consider four essential factors: prognosis, quality of life, available resources, and specific utility.
Prognosis
The literature on prognosis of neurological disease is vast and well-known to the practicing neurosurgeon. Estimates of prognosis may be tabulated for conditions that are routinely encountered (Table). Among the general predictors of poor prognosis are increased age, abnormal pupillary responses, low Glasgow Outcome Score, intracranial hemorrhage, subarachnoid hemorrhage (SAH),8 and penetrating cranial injury.6,9
TABLE.
Conditions Requiring Urgent Neurosurgical Intervention
| Median survival | ||
|---|---|---|
| Condition | (%) | Reference |
| Normal pressure hydrocephalus | >95 | Andren et al (2020)28 |
| Chronic subdural hematoma | 86 | Manickam et al (2016)29 |
| Acute subdural hematoma | 73a | Fountain et al (2017)30 |
| SAH* | 72 | Alotaibi et al (2017)8 |
| Intracerebral hemorrhage | 59 | Flaherty et al (2006)31 |
| Glioblastoma | 40 | deSouza et al (2016)32 |
| Gunshot wound | 30b | Joseph et al (2014)33 |
outcome at 1 mo.
outcome at 5 yr.
Poor grade SAH patients undergoing decompressive craniectomy.
Example conditions are rank ordered by median survival at 1 yr, unless otherwise stated. All conditions are considered under ideal treatment conditions with ample medical resources.
Under normal circumstances, the highest quality of evidence is provided by data from carefully controlled studies. The objective of these studies is to remove confounds, such as comorbid infections, scarce resources, and nonideal treatment environments. Class I data represent best-case scenarios. Best-case scenarios may not translate to expected outcomes in disaster situations where realities on-the-ground lower expectations. The surgeon must evaluate prognostic factors and advise referring providers and family members prior to initiation of treatment.
Quality-adjusted life-years
Quality-adjusted life year (QALY) is a measure of disease treatment that incorporates both quality and quantity of life gained. This measure was developed by health economists to assess the value of medical interventions to set priorities in the allocation of scarce public resources.10-13 QALYs are generated by prolonged survival, improved quality of life, or both. Cost per QALY is widely used by industrialized countries to ascertain health maximization given finite resources. In the United States, economists observe that a specific surgical treatment is considered cost-effective when 1 QALY is gained per US$50 000 spent.14 This “willingness-to-pay” threshold varies across countries.
Under normal conditions, QALYs are scaled over a given currency, as this permits normalization of life-years for comparisons of different interventions. During disaster, a more appropriate numerator commodity for normalization might be the availability of medical supplies. During the coronavirus (COVID-19) pandemic, ICU beds were in short supply. Estimates of intensive care demand predicted that between 3 and 4 million ICU beds would be needed assuming a 40% prevalence of COVID-19.15,16 Prior to COVID-19, the Society of Critical Care Medicine estimated that there were between 64 000 and 68 000 adult ICU beds in the United States,17,18 and the pre-COVID occupancy rates were 66.6%.19 Thus, an ICU bed during pandemic may constitute a more tangible commodity to normalize QALYs than currency. The relevant treatment threshold shifts from the “willingness-to-pay” a finite amount of money to the “willingness-to-allocate” a finite scarce resource.
To illustrate this point with an example, consider 2 identical 55-yr old patients in a triage bay at an urban hospital during the COVID-19 pandemic. One patient presents with a large SAH, and 1 with early signs of acute respiratory distress syndrome. Both patients may be assumed to require an ICU bed for 1 to 3 wk. The COVID patient may be assumed to have a mortality between 0.25% and 15%, equating to a 85% to 99% survival.20,21 Here, it can be argued that the COVID patient has a higher likelihood of gaining QALYs with the allocation of an ICU bed than the SAH patient. The surgeon must consider how to best maximize quantity and quality of life in the presence of overwhelming health system crisis when standards of care are necessarily altered.
Available resources
During hurricanes Katrina and Sandy, physicians were forced to ration the use of ventilators in the ICU.22 At Memorial Medical Center in Uptown New Orleans in 2005,23 and later at Bellevue Hospital in New York city in 2012, Drs Anna Pou and Laura Evans were left in the position of making point-of-care decisions about which patients would live or die. These sobering experiences underscore the fact that the rate limiting step in survival is the availability of critical resources. In a hurricane, electricity to run medical equipment may be the rate limiting resource. During contagion, it may be the availability of personal protective equipment to prevent further infection.
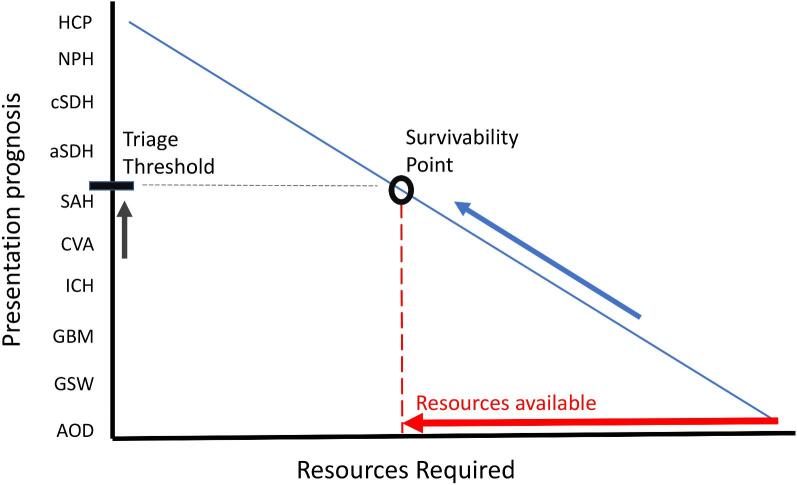
The prognosis for common neurosurgical conditions is a function of the resources required to render effective treatment (Figure 1). Low acuity conditions, such as chronic subdural hematomas and normal pressure hydrocephalus, have an excellent overall prognosis and require few resources to restore the patient to preoperative health. On the opposite end of the spectrum, cranial gunshot wounds have poor overall prognosis even with unlimited resources. The relationship between prognosis and the available resources is illustrated in Figure 1. At any point along the line, the survivability of a condition may be estimated based on the ability to offer adequate treatment. This ability depends on the resources that are available. As the resources are reduced (red arrow), the survivability point shifts leftward and the corresponding triage threshold increases. This conceptual framework illustrates a key concept: triage thresholds dynamically change as a function of available resources. While aggressive treatment for at least 72 h is advocated following devastating injury,24 that luxury does not apply as resources are exhausted.
FIGURE 1.
Survivability function. Predicted survivability is a function of the presenting prognosis and medical resources available. Available resources are exhausted during a humanitarian crisis (red arrow). This results in a leftward shift of the survivability point (black circle). The triage threshold corresponding to the point of survivability provides an estimate of the conditions along the continuum of presenting prognosis that may be effectively treated with scarce resources. Common neurosurgical conditions are presented in ascending order of presentation prognosis (y-axis). Relative availability of medical resources required to treat neurosurgical conditions is plotted on the x-axis. Abbreviations: Acute hydrocephalus (HCP); normal pressure hydrocephalus (NPH); chronic subdural hematoma (cSDH); acute subdural hematoma (aSDH); subarachnoid hemorrhage (SAH); cerebrovascular accident (CVA); intracerebral hemorrhage (ICH); glioblastoma (GBM); gunshot wound to the head (GSW); atlanto-occipital dislocation (AOD).
The surgeon must demonstrate excellent situational awareness of the available resources. Toward this aim, the surgeon must maintain open channels of communication with acute care providers (eg, ER and ICU), operative staff, nursing management, and hospital leadership.
Specific utility
To understand utility, we must first draw upon the experience of the military physician. Military physicians have a different role than their civilian counterparts. Military physicians assume the fiduciary duty to provide a standard of care to warfighters, while also contending with the goal of returning them to the battlefield as quickly as possible. This is necessary to maintain the strength of the fighting force.25
Disasters are not battlefields, but some parallels may be drawn. During disasters, the civilian physician faces an enemy in the form of pandemic or other pressing humanitarian crisis. Injured civilians are not warfighters, but some civilian duties are essential to combat an ongoing threat. Police and fire fighters are examples of civil servants whose duties lessen the deleterious effects of disaster on society. Similarly, health-care providers maximize the health of the injured and facilitate their return to a society in crisis.
Health-care providers and civil servants are force multipliers. Force multipliers are factors that amplify the capacity of others to accomplish a mission. Civil servants amplify the capacity of society to not only battle a disaster, but also to function in an orderly manner. Accordingly, civil servants have high specific utility. The term utility, borrowed from health economics, is a tangible measure of the usefulness of an individual or object in a specific context. It is similar to instrumental value, a term borrowed from medical ethics, which has been proposed as a method of assigning treatment priority to those who can save lives, or who have saved lives in the past.26 In the context of an ongoing threat, the neurosurgeon may be placed in a position of having to weight context-specific utility of the injured to prioritize treatment to those who maximally mitigate the threat.
Simultaneously, the surgeon must avoid force dividers. These are factors which incapacitate the medical infrastructure, or personnel, and thereby critically limit the execution of care. Surgeons must avoid exposure that would result in injury. In the case of COVID-19, this means maintaining personal protective equipment protocols.
Continuation of Treatment
One of the most difficult decisions pertains to the continuation of treatment. The allocation of scarce resources has a cost function measured in quality and quantity of life. These metrics must be integrated not only for the beneficiary of the resource, but also for those who were denied the resource, such as a mechanical ventilator. During disasters, the time scale for meaningful recovery is compressed. If a patient with a serious neurological injury does not demonstrate a trajectory toward ultimate recovery within a finite interval, the surgeon must consider the opportunity cost to other patients. Specific criteria for the termination of care have proven elusive.27 However, 1 criterion that may be considered is the expected duration of use of the resource per patient. If the duration of illness X is expected to require 1 wk of mechanical ventilation, whereas the duration of illness Y is expected to require 3 wk, then 3 X patients can be effectively treated for every Y patient for the same unit resource. In a time of crisis, these factors must be considered during every treatment decision.
Triage Algorithm
Based on the above, a neurosurgical disaster triage algorithm is proposed (Figure 2). The default triage decision is always to offer treatment based on existing standard of care. Treatment initiation decisions are prioritized against the presenting prognosis, quality and quantity of life-years estimated, availability of critical resources, and specific utility. The relative weights of these considerations must be updated continuously across the duration of disaster and duration of illness as resource demand and supply fluctuates. Treatment continuation decisions are likewise continuously re-evaluated based on the patient's recovery trajectory.
FIGURE 2.
Neurosurgical disaster triage algorithm. Triage decisions occur at 3 time points: initial presentation, treatment initiation, and treatment continuation. Key considerations for each time point are illustrated in the process diagram (diamonds). Considerations must be continuously assessed in the context of the availability of critical medical resources. Considerations are not intended to be exclusionary of other important factors, such as family wishes.
DISCUSSION
Disaster places extraordinary demands on health-care providers. Neurosurgeons can be trusted to rise to the occasion. Executing one's duty as a surgeon may require critical triage decisions. Triage considerations include evaluating the patient's presenting prognosis, the expected quality and quantity of life afforded by treatment, the availability of scarce resources, and the specific utility of those treated. These are difficult topics that must be discussed in the context of society's needs.
Triage strikes at the heart of the ethics of medical rationing.16 The most daunting determination is who will be treated and who will not. Above, we introduced specific utility as a measure of the tangible usefulness of an individual or object in a specific disaster context. Importantly, specific utility is a utilitarian assignment that maximizes total benefits to society. An example of a patient with a high specific utility is an injured paramedic who is returned to the front lines during a disaster to rescue other sick personnel. Allocating scarce resources based on specific utility is a form of force multiplication.
There are other methods of adjudicating neurosurgical triage. They include treating all patients equally (eg, a treatment lottery), first-come/first-served, prioritizing the sickest, prioritizing the youngest (to maximize life-years saved), prioritizing the most vulnerable (eg, pregnant women and children), reciprocity (eg, favoring those who have demonstrated social value), and others.26 Finally, it must be acknowledged that each disaster is unique, and is uniquely experienced by each hospital. The nature of this discussion is to introduce these topics for further consideration. Interested readers are referred to Emanuel et al16 for a contemporary discussion of the ethics of resource allocation.
CONCLUSION
Neurosurgical triage assigns treatment priority to the sick. During disaster, neurosurgeons may face difficult decisions as critical resources become scarce. Decisions evolve over the time course of patient illness and the disaster. Triage algorithms offer guideposts to organize decision-making at times of critical need. Neurosurgeons must rise to the occasion and be prepared to make difficult decisions to maximize the health and sustainability of society. Formal guidelines must be developed within organized neurosurgeon so that individual surgeons are not left to shoulder the burden at the point of care.
Disclosures
The author has no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
REFERENCES
- 1. Bazyar J, Farrokhi M, Khankeh H. Triage systems in mass casualty incidents and disasters: a review study with a worldwide approach. Open Access Maced J Med Sci. 2019;7(3):482-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Koenig K, Schultz c eds. Koenig and Schultz's Disaster Medicine: Comprehensive Principles and Practices. New York: Cambridge University Press; 2010. [Google Scholar]
- 3. Ciottone G, Biddinger P, Darling R, Fares S, Keim M, Molloy M. Ciottone's Disaster Medicine. New York: Elsevier Health Science; 2015. [Google Scholar]
- 4. Bhalla M, Frey J, Rider C, Nord M, Hegerhorst M. Simple triage algorithm and rapid treatment and sort, assess, lifesaving, interventions, treatment, and transportation mass casualty triage methods for sensitivity, specificity, and predictive values. Am J Emerg Med. 2015;33(11):1687-1691. [DOI] [PubMed] [Google Scholar]
- 5. Bazyar J, Farrokhi M, Salari A, Khankey H. The prinicples of triage in emergencies and disasters: a systematic review. Prehosp Disaster Med. 2020;6:1-9. [DOI] [PubMed] [Google Scholar]
- 6. Gressot L, Chamoun R, Patel A et al.. Predictors of outcome in civilians with gunshot wound to the head upon presentation. J Neurosurg. 2014;121(3):645-652. [DOI] [PubMed] [Google Scholar]
- 7. Shkrum M, Green R, Nowak E. Upper cervical trauma in motor vehicle collisions. J Forensic Sci. 1989;34(2):381-390. [PubMed] [Google Scholar]
- 8. Alotaibi N, Elkarim G, Samuel N et al.. Effects of decompressive craniectomy on functional outcomes and death in poor-grade aneurysmal subarachnoid hemorrhage: a systemic review and meta-analysis. J Neurosurg. 2017;127(6):1315-1325. [DOI] [PubMed] [Google Scholar]
- 9. Fahalla H, Ashry A, El-Fiki A. Managing military penetrating brain injuries in the war zone: lessons learned. Neurosurg Focus. 2018;45(6):E6. [DOI] [PubMed] [Google Scholar]
- 10. Weinstein M, Torrance G, McGuire A. QALYs: the basics. Value Heal. 2009;12(1):s5-s9. [DOI] [PubMed] [Google Scholar]
- 11. Weinstein M, Stason W. Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med. 1977;296(13):716-721. [DOI] [PubMed] [Google Scholar]
- 12. Pliskin J, Shepard D, Weinstein M. Utility functions for life years and health status. Oper Res. 1980;28(1):206-224. [Google Scholar]
- 13. Lancsar E, Gu Y, Dorte G et al.. The relative value of different QALY types. J Heal Econ. 2020;70):102303 (doi:10.1016/j.jhealeco.2020.102303). [DOI] [PubMed] [Google Scholar]
- 14. Ryu H, Yang M, Muram S, Jacobs B, Casha S, Riva-Cambrin J. Systematic review of health economic studies in cranil neurosurgery. Neurosurg Focus. 2018;44(5):E2. [DOI] [PubMed] [Google Scholar]
- 15. Tsai T, Jacobson B, Jha A. American hospital capacity and projected need for COVID-19 patient care. Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20200317.457910/full/. Published2020. Accessed March 23, 2020. [Google Scholar]
- 16. Emanuel E, Persad G, Upshur R et al.. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. published online: 2020(doi:10.1056/NEJMsb2005114). [DOI] [PubMed] [Google Scholar]
- 17. Halpern N, Tan K. United states resource availability for COVID-19. Society of Critical Care Medicine. https://sccm.org/Blog/March-2020/United-States-Resource-Availability-for-COVID-19?_zs=jxpjd1&_zl=w9pb6. Accessed March 24, 2020. [Google Scholar]
- 18. Sanger-Katz M, Kliff S, Parlapiano A. These places could run out of hospital beds as coronavirus spreads. The New York Times. https://www.nytimes.com/interactive/2020/03/17/upshot/hospital-bed-shortages-coronavirus.html. Accessed March 24, 2020. [Google Scholar]
- 19. CMMS Centers for medicare and medicaid services, Cost Reports. January 21, 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Cost-Reports. Accessed March 24, 2020.
- 20. Wilson N, Kvalsvig A, Barnard L, Baker M. Case-fatality risk estimates for COVID-10 calculated by using a lag time for fatality. Emerg Infect Dis. published online: 2020(doi:10.3201/eid2606.200320). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. published online: 2020(doi:10.1016/S1473-3099(20)30195-X). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fink S. The hardest questions doctors may face: who will be saved? Who won’t? New York Times. https://www.nytimes.com/2020/03/21/us/coronavirus-medical-rationing.html. Accessed March 30, 2020. [Google Scholar]
- 23. Fink S. The deadly choices at memorial. The New York Times Magazine. https://www.nytimes.com/2009/08/30/magazine/30doctors.html. Accessed March 30, 2020. [Google Scholar]
- 24. Pratt A, Chang J, Sederstrom N. A fate worse than death: prognostication of devastating brain injury. Crit Care Med. 2019;47(4):591-598. [DOI] [PubMed] [Google Scholar]
- 25. Adams M. Triage priorities and military physicians. In: Allhoff F, ed. Physicians at War, Vol. 41 Dordrecht: Springer; 2008:215-236. [Google Scholar]
- 26. Persad G, Wertheimer A, Emanuel E. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423-431. [DOI] [PubMed] [Google Scholar]
- 27. Wilkinson D, Savulescu J. Knowing when to stop: futility in the intensive care unit. Curr Opin Anaesthesiol. 2011;24(2):160-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Andren K, Wikkelso C, Sundstrom N et al.. Survival in treated idiopathic normal pressure hydrocephalus. J Neurol. 2020;267(3):640-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Manickam A, Marshman L, Johnston R. Long-term survival after chronic subdural haematoma. J Clin Neurosci. 2016;34:100-104. [DOI] [PubMed] [Google Scholar]
- 30. Fountain D, Kolias A, Lecky F et al.. Survival trends after surgery for acute subdural hematoma in adults over a 20-year period. Ann Surg. 2017;265(3):590-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Flaherty M, Haverbusch M, Sekar P et al.. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66(8):1182-1186. [DOI] [PubMed] [Google Scholar]
- 32. DeSouza R, Shaweis H, Han C et al.. Has the survival of patients with glioblastoma changed over the years? Br J Cancer. 2016;114(12):146-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Joseph B, Aziz H, Pandit V et al.. Improving survival rates after civilian gunshot wounds to the brain. J Am Coll Surg. 2014;218(1):58-65. [DOI] [PubMed] [Google Scholar]