ABSTRACT
Introduction
The COVID-19 outbreak posed a threat to the readiness of military forces as well as their ability to fulfill missions. Seeing that military forces have been encountering similar challenges, we found it eminent to share the Israeli Defense Force (IDF) Northern Command’s (NC) preliminary experience.
Materials and Methods
We retrospectively summarized the actions that were taken by our team, focusing on 18 battalions at the Israeli NC. These actions included promoting a series of organizational changes in terms of social distancing and medical regulations as well as working to strengthen medical leadership through designated video meetings with medical commanders across our organization. Meetings included relevant clinical education, updates, and leadership building. These actions and others were aimed to increase our influence on the decision-making processes. While we conducted real-time reverse transcriptase polymerase chain reaction SARS-CoV-2 laboratory tests for soldiers who were suspected to have COVID-19 (those presenting with compatible signs and symptoms after having been exposed to a confirmed COVID-19 patient), we were not able to screen healthy populations, nor did we have serum antibody serologic tests available during the study period. We reviewed the COVID-19 outbreak national data, obtained from Ministry of Health publishings and the IDF databases. Data were included from February 26th, 2020 (day 0, first COVID-19 patient in Israel) to April 19th, 2020 (day 53, about 1 month after most of the COVID-19 regulation were issued in the NC).
Results
The mean age of the battalion soldiers was 21.29 ± 4.06 (range 18–50), 81.34% male. Most restrictions were issued on day 18. On day 53, 98.85% of the personnel in the battalions were kept active and asymptomatic in their units.
Conclusions
Despite the limited availability of laboratory testing for COVID-19 our actions enabled us to lead a strict risk-management policy while maintaining most of the available workforce.
INTRODUCTION
On December 31, 2019, a novel coronavirus, later designated SARS-CoV-2 was diagnosed in a cluster of patients in China.1 This was the source of what was later developed into the COVID-19 pandemic.2 The clinical presentation of COVID-19 was found to range from an asymptomatic infection3 to a devastating pneumonia, multi-organ failure, and death.4,5 In a meta-analysis by Rodriguez-Morales et al.,6 it was found that 20.3% of the patients in china who had been found positive for COVID-19 by real-time reverse transcriptase polymerase chain reaction (rRT-PCR) for SARS-CoV-2 warranted an intensive care unit admission because of their illness. This rate varied considerably between different publications,4,7–9 but reflected on the potential implications that this new disease might impose.
The first COVID-19 patient in Israel was diagnosed on February 26th, 2020 and was followed by a national disease outbreak.10 National measures including public commute restrictions and quarantines were taken to limit the infectivity rates among the general population.10
A broad spread of the disease within the Israeli Defense Forces (IDF) could have potentially limited its ability to carry out missions. In this article, we aimed to present the measures that were taken by the IDF Northern Command (NC) to limit the COVID-19 outbreak among soldiers and minimize its effect on the commands’ ability to fulfill its mission. Since military forces worldwide encountered the same challenges, we find it a global interest to share ideas, directives, and cumulative experience.
METHODS
This study is a retrospective review summarizing the actions taken by our team (the NC surgeon office) to limit the effect of the COVID-19 outbreak on the soldiers’ health, and units’ workforce. These actions were implemented as a set of orders that aimed to promote social distancing and medical regulations. They were directed by medical officers, but delivered by commanders to assure adherence and to promote organizational changes.
We reviewed both national data that were obtained from the Ministry of Health publishing and data from the IDF healthcare databases. The national data of interest was the daily number of patients who were diagnosed positive for COVID-19 by nasopharyngeal swabs that underwent an rRT-PCR studies for SARS-CoV-2.11,12 These tests were available for both citizens and military personnel who answered the clinical and epidemiological criteria13 for a “suspected case” or a “low suspicion” (Fig. 1). PCR screening and serologic tests for SARS-CoV-2 serum antibodies for asymptomatic populations were not available during the study period. We analyzed the rate of sick leave days that were issued attributable to any cause, and specifically because of COVID-19-related symptoms (respiratory symptoms or a fever above 38°C), the rate of soldiers quarantined and the rate of soldiers that have been temporarily released as part of a workforce dilution. We analyzed the period between February 26th (regarded as day 0) and April 19th, 2020 (day 53). In order to evaluate the effect of our actions on the frontline personnel, we analyzed all 18 battalions that have been placed under the NC during the outbreak. These battalions were considered to be representative of the IDFs frontline units.
FIGURE 1.
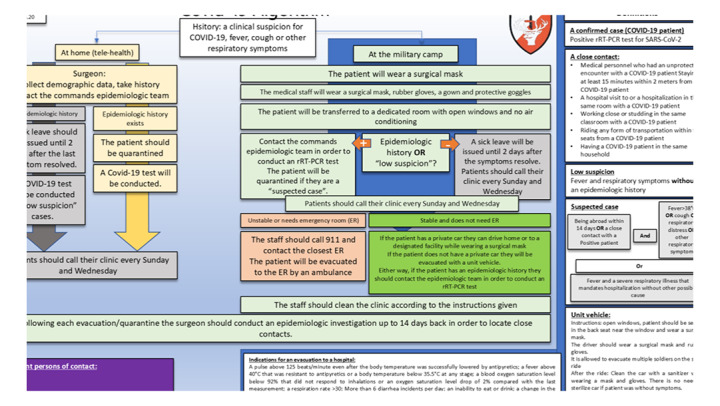
An algorithm for managing patients who were treated by the IDF NC medical teams and had respiratory symptoms or a fever during the COVID-19 outbreak in Israel. During the first 32 days after the first positive COVID-19 patient was diagnosed in Israel, rRT-PCR test were available only for “suspected cases” or “low suspicion” cases.
An SPSS 25.0 software (Chicago, Illinois) was used to collect and analyze data. Descriptive statistics and an accumulative case epidemiological curve were used to present data. In cases where security did not allow the exposure of rough numbers, we presented rates alone. The t-test was used to compare continuous variables such as sick leave days and the daily number of physician encounters. A P-value of 0.05 was considered statistically significant.
RESULTS
In the 18 NC battalions, the mean age was 21.29 ± 4.06 (range 18–50), 81.34% male. On day 11 (March 8th, 2020), we gradually started to impose COVID-19-related restrictions and the vast majority of the orders were issued on day 18 (March 15th, 2020). During the first month following these restrictions were issued, six soldiers were found positive for COVID-19 (rRT-PCR). On day 53, the NC battalions were able to maintain 98.85% of their personnel out of quarantine, and without fever or respiratory symptoms (Fig. 2). When compared to the year before (2019) during the first 3 weeks that followed the new restrictions, there were more documented physician encounters (P = 0.03) and more sick leave days were issued (P < 0.01; Fig. 3).
FIGURE 2.
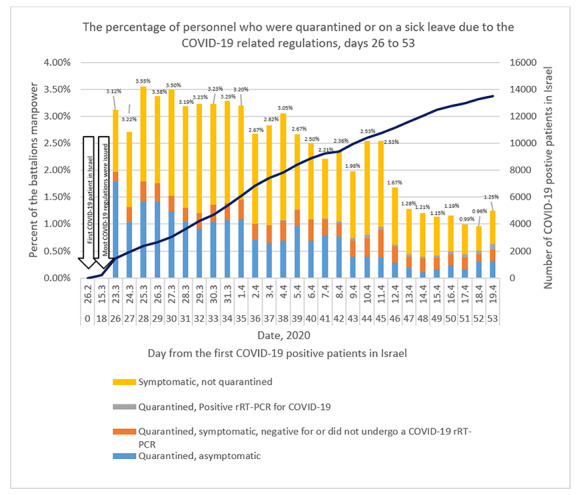
A daily differentiation of COVID-19-related workforce decline, days 26–49 (7 days–1 month after most of the COVID-19-related restrictions were issued). During the presented period, rRT-PCT tests were limited to quarantined symptomatic patients, and no rRT-PCR or serum antibody serologic tests were available for other patients. Because of this limitation on day 26, we started to monitor the prevalence of respiratory symptoms and fever among soldiers on a daily basis as were reported by the medical teams. This enabled to trace illness trends within units and although we did not know how many of these soldiers actually had COVID-19. Day 0 represented the day on which the first COVID-19 patient was found positive for SARS-CoV-2 with rRT-PCR in Israel. We applied a 14 days quarantine on soldiers who have been in a close contact with a COVID-19 positive patient. Symptomatic: a patient with either a respiratory symptom or a fever above 38°C.
FIGURE 3.
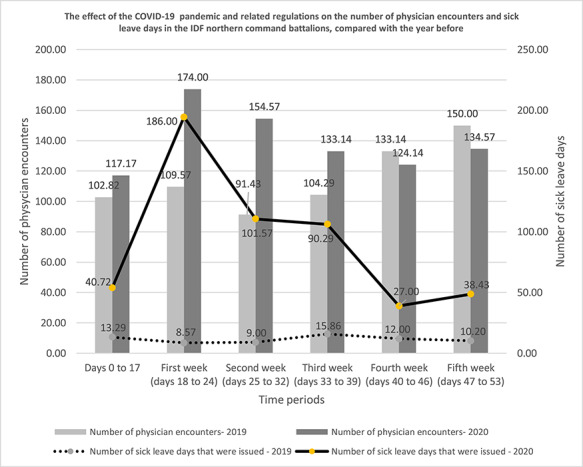
The effect of the COVID-19 pandemic and related regulations on the number of physician encounters and sick leave days in the IDF NC’s battalions (year 2020) compared with the same period during 2019. Day 0 (February 26, 2020) represented the day on which the first COVID-19 patient was found positive for SARS-CoV-2 with rRT-PCR in Israel. The week numbers represent the time that passed from day 18, when most of the COVID-19-related regulations were issued. Among these regulations were a curfew that was applied on the battalions. Furthermore, all soldiers who had fever above 38°C or any respiratory symptoms were released on a sick leave. The difference between days 0–17 and the first 3 weeks was found to be statistically significant (P < 0.05) for both variables.
Social distancing
The IDF is unique in the proximity, and often mixture, between military bases and civilian residencies. We implemented a curfew that started on day 18. This was aimed to minimize exposure between civilians and military personnel and to decrease the amount of people who used public transportation on a national scale. We instructed commanders to allow all military personnel not deemed critical for urgent or immediate missions to stay at home. The commanders were instructed to avoid physical encounters with their deputies and to split their personnel into separate shifts, to prefer video-assisted conferences, to avoid any unnecessary physical contact and to forbid meetings of more than five people at the same room. We did not allow civilians to enter any military facility, unless they were personally approved by a senior officer (colonel or above).
The first instructions that we issued with regard to dining rooms were aimed to promote hygiene and to avoid crowding and were based almost solely on personal discipline. We quickly realized that soldiers were not obedient enough to these orders and progressed to organizational changes. We closed most of the dining facilities, and food was delivered as meal boxes. If dining halls could not be closed because of logistical limitations, we enforced a maximum 100 people limit at any given time with a minimal distance of 2 m between any two people.
Medical restrictions, quarantine instructions, and hygiene
An isolation period of 14 days14 was applied on any person who was in a close contact with a confirmed COVID-19 patient (definitions for “close contact” and “confirmed case” are presented in Fig. 1). We also imposed a 14 days isolation period starting on the arrival for any person who was from abroad, regardless of symptoms.15
The surgeon general headquarters assembled a list of disease codes that have been associated with a worse clinical course of COVID-19. Every person suffering from a disease on that list was released home. In order to enter a military base, soldiers needed to sign a written statement declaring that they had not been from abroad during the last 14 days, had not been in a close contact with a confirmed COVID-19 patient, and did not have any respiratory symptoms or a fever above 38°C.15,16 Entrance restrictions to military facilities that were regarded as imitable and necessary were more strict and included a separate temperature measurment15 and hand disinfection with a 70% alcohol solution.
Medical encounters and organizational changes
Patients were instructed to contact the clinic by phone whenever they needed medical assistance.17 If surgeons decided that a physical examination was mandatory, the patients were instructed to approach the clinic. This allowed the medical teams to wear their protection equipment in advance whenever needed3,5,13,17 and to spare this valuable gear when possible.
In order to protect themselves from droplet transmission, in any medical encounter with patients who had respiratory symptoms or a fever, or answered the criteria for a “close contact” (Fig. 1), the patients were instructed to wear a surgical mask18 and the medical personnel wore a surgical mask and rubber gloves.18,19–21 On day 30, these orders were broadened and medical personal were instructed to wear a surgical mask and gloves in any medical encounter, and to add a gown21 and protective goggles when they examined patients with respiratory symptoms or a fever.19 If procedures that increased the risk for aerosol spreading such as an intubation, inhalation, etc.22 were conducted, the medical providers were instructed to replace their surgical masks with N95 masks that offered an increased protection in these circumstances.18,20,22 We broadened the primary instructions after acknowledging that there may be a high proportion of asymptomatic or mildly symptomatic patients,3,15,23,24 that COVID-19 patients may initially present with nonrespiratory symptoms,4,7,25,26 and that the masks did not protect the staff from droplets that would enter their eyes or fall on their clothes and would later be transferred to their mucus membranes.19,23 Even though these protective measures have been hypothesized to be effective against COVID-19 transmission19–22 and were based on the international guidelines,18,22 we were not able to prove whether they were effective in preventing infection in the NC since we did not screen asymptomatic medical teams for SARS-CoV-2.
Medical personnel who treated patients who turned out to be positive for SARS-CoV-2 were not quarantined if both the patient and the caregivers were protected as instructed. This was in concordance with the Centers for Disease Control and Prevention Guidelines.27 A mechanical cleaning and chemical disinfection of the entire clinic and all surfaces with freshly made chlorine or bleach solutions was mandated following any encounter with a suspected COVID-19 patient. The disinfection steps followed previously published guidelines.28–30
We closed all the waiting rooms in our clinics and patients were instructed to wait outside of the clinics in the open air until they were allowed to enter.17 This enabled clinics to avoid crowding in closed waiting rooms where the probability to have a SARS-CoV-2 positive person was presumed to be higher.17 Nevertheless, we could not document a case in which a viral spread was avoided by this restriction, and its added value was therefore difficult to assess. In each clinic, a specific room was allocated for examining patients who answered the criteria for a “suspected case” (Fig. 1). This room had a fingertip Pulse Oximeter monitor and a thermometer. Its windows were kept open with the air conditioner closed. Medical personnel who had risk factors for a more severe illness and higher mortality rates did not enter this room. Specialist clinics were limited to emergency visits. Physical therapy was limited to postoperative rehabilitation. We stopped all scheduled dental care appointments and treated only first aid cases.
We installed video cameras in battalion clinics and platoons posts to support telemedicine platforms,17 by that minimizing the need to transport soldiers. This was accompanied by an implementation process.31 Each surgeon and all medics were obligated to read and sign the telehealth guidelines and restrictions manual, to participate in an interactive video explanatory session, to participate in a group video session of simulated guided patient encounters, and to practice telehealth in front of 10 simulated patients. We formed protocols for prescribing medications by digital means. Permissive criteria were applied for issuing a sick leave so that soldiers who reported a new cough or a fever could be released (Fig. 1).
We opened a call center that operated 24/7 and included a team that was led by a senior medical officer who was a physician by training.17 This center was appointed to assist and guide medical personnel, patients, and their families in comprehending and executing the new regulations. It provided assistance to patients who were quarantined or under a sick leave. It also offered telemedicine consultation to soldiers using video and audio communication platforms.
SARS-Cov-2 rRT-PCR tests have been centrally regulated by the national health administration. This test was therefor available mostly for symptomatic patients with a positive epidemiologic history. This limitation prevented us from identifying and isolating asymptomatic COVID-19 personnel who might have been infectious to others. It also prevented us from assessing the true COVID-19 spread among the units. As the national availability of this tool grew, we were able to test patients who did not answer both criteria but whose diagnosis would have been valuable to their units (asymptomatic COVID-19 personnel who might be shedding SARS-CoV-2). Serum antibody serologic tests for SARS-CoV-2 were unavailable in Israel during this period.
Patient evacuation
We instructed the medical teams to call an ambulance for any evacuation to a hospital. This was indicated when the patients’ medical status deteriorated (Fig. 1). We allowed an evacuation with a military unit vehicle for patients who answered the “close contact” or “low suspicion” criteria (Fig. 1) and for symptomatic persons who were quarantined. Because of a limited availability of rRT-PCR or serologic antibody tests, none of the later was screened for COVID-19 during this reports’ timeframe. The driver was instructed to wear a surgical mask and rubber gloves.32 The patient was instructed to sit in the back seat nearby the window. All windows were kept open during the ride. After the evacuation if the patient was symptomatic the vehicle was disinfected and ventilated for 24 hours.32 If both the patient and driver were protected, the driver was not quarantined.21,32,33 Out of more than 150 evacuations, none of the drivers developed symptoms that were compatible with COVID-19, although we were not able to screen them for SARS-CoV-2.
Only if respiratory symptoms alone were reported with no fever and no close contact criteria and no history of an international flight during the last 14 days, patients were allowed to use modes of public transportation. This form of transportation was the least favored and was completely banned on day 22 as we acknowledged that this could jeopardize those using public transportation if any of these soldiers had COVID-19.
Medical education
We structured an algorithm (Fig. 1) that was based on the national instructions given by the ministry of health and the surgeon general’s commands guidelines. This algorithm was sent to all physicians and simplified the central command’s directives into a clear one-page graphic manual.
Most information was sent to our caregivers both via the internal IDF network and online via the “WhatsApp” (Facebook) and “Telegram” applications to maximize information accessibility. Guidelines have been edited both to text form, video guides, and PowerPoint presentations. A designated “WhatsApp” group was launched to allow information sharing and anonymized clinical discussions. The group was led by the command surgeon who was an internal medicine specialist. Explanatory digital pamphlets were printed and sent online to soldiers and commanders. Screensavers throughout the command were replaced with educational information regarding social distancing and hygiene recommendations.
Leadership
We held video-based meetings with all frontline healthcare providers twice weekly. In these meetings, the command surgeon led educational activities, provided guidance, and encouraged the medical personal to share their difficulties. We have guided the surgeons to attend all decision crossroads in their units. They were instructed to help their commanders to make decisions that were based on evidence and science, which mandated them to be updated with the most relevant guidelines and to make sure these data became the ground on which decisions were taken in their units. We spoke with surgeons about the soldiers and commanders need for emotional reassurance in this era of stress and uncertainty. The senior medical officers have visited the frontline units, evaluated the adherence to the new regulations and acted to raise the spirit of the medical teams. We made sure that these visits were scaled to prevent infection spread between the units. We bought and sent e-book coupons to military medical personal as an act of appreciation.
DISCUSSION
We planned actions that were derived from the national restrictions, the surgeon general directives, and the military’s needs and abilities. We established our acts in light of a few basic concepts: (1) The IDF was facing a new disease that posed an uncertainty to the entire chain of command, which included both medical officers and unit commanders. This obligated us to learn, guide, and lead. (2) Soldiers obedience to hygiene instructions was important, but organizational measures were presumed to be more effective.34 (3) Common areas such as dining rooms and residencies posed a risk because of both people’s proximity25,35 and the use of shared emnities14,24,36 such as toilets,37 showers, 37 sinks, 37 door handles,37 and plastic and stainless steel serving tools.37,38 (4) The illness was a threat to both our patients and the national defense mission. The national quarantine restrictions could put many soldiers away from the frontlines since each confirmed COVID-19 patient within the battalion might have obliged us to quarantine all soldiers who have been exposed to him/her.39 Because of the crowded nature of these units, one patient could have affected dozens of soldiers. Accordingly, the approach warranted to contend with the COVID-19 pandemic within the defense forces mandated specifications.
The hierarchical nature of the organization enabled us to impose policies in a fast manner and a wide scale. We found it of high importance to utilize our commanders’ authority to enforce organizational changes that were aimed to promote social distancing and hygiene. This mandated all medical officers to step forward and lead decision-making processes throughout the units, where medical directives were translated into practical instructions. We found that commanders have progressed from an indifference to a hyper-reactive state. This might have led to actions that were based on common knowledge and general and social media-mediated information. Our task was to translate knowledge that was based on the most updated medical literature into orders that would be given by commanders to their subordinates.
The military personnel were 18 to 45 years of age. Although men and women alike were enlisted to the military when they were 18 years old and discharged at 20 to 21 years of age, the battalions had a clear male predominance. People who suffered from chronic diseases were often released from the compulsory draft in Israel, so our military personnel were comparably free of comorbidities that would have put them at risk for a severe illness.40,41 The association between the mentioned population features and COVID-19 is presented in Table I.
TABLE I.
A Summary of Published Findings That Were Relevant for the Population Features in the IDF NC Battalions—age 18–45 and a male sex predominance.a The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, This Report Included All Confirmed COVID-19 Cases in China and Might Have Included Data From Other Reports From China That Were Presented in This Table
| Authors | Population features | Relevant information |
|---|---|---|
| Livingston and Bucher 26 | Age 18–45 | This age group accounted for approximately 24% of the entire patient population. The case fatality rate in this age group was 0–0.4%. This was significantly lower than the total CFR of 7.2% in the same report, and 3.8%8 to 7%7 in other reports |
| Guan et al.4 | Age 18–45 | This age group accounted for approximately 51.1% of the entire patient population. In this age group, 12.03% of the patients had a severe fatality rate (compared to 31.18% in the rest of the patient population in the same report and 24.9–29.9% in the entire patient population in a Livingston and Bucher26 report) |
| Wu and McGoogan8 | Age 20–29 | This age group accounted for approximately 8% of the entire patient population |
| Zhang* | Age 20–29 | Out of 44,672 confirmed COVID-1 patients 8.1% were within this age group, and 36.2% were 20–49 years old |
| Zhou et al.9, Livingston and Bucher26, Guan et al.4 | Sex differences | In all three papers, a male predominance was found among COVID-19 patients |
| Yang et al.44 | Sex differences | Male sex was associated with a more severe disease |
| Kon et al.45 | Sex differences | The association between male sex and a more severe disease was weak |
| Zhanga | Sex differences | Out of 44,672 confirmed COVID-1 patients, 51.4% were male |
A significant proportion of COVID-19 patients were either asymptomatic or had only mild symptoms.24,42,43 The cumulative evidence on the infective potential of these patients24,42,43 encouraged us to become very permissive with sick leave regulations to decrease COVID-19 spread potential. Since screening asymptomatic soldiers with an rRT-PCR or an antibody serologic testing was unavailable to us, we could not prevent asymptomatic and presymptomatic COVID-19 patients from spreading the disease. Nevertheless, since a cough and a fever were considered to be the most common symptoms upon presentation,4,7,9,41 soldiers who reported these symptoms4,41 were not allowed to enter military camps and were released until their symptoms resolved. This allowed us to keep potentially symptomatic COVID-19 patients from shedding SARS-CoV-2 to others. Surprisingly, during the first couple of weeks, this approach did not lead to an abuse of the situation by the soldiers, and our available manpower was hardly affected.
This article has limitations. Since this report was written at the midst of the pandemic, we acknowledged that we were unable to comprehensively evaluate the long-term outcomes of our actions. We did not have the possibility to screen asymptomatic populations with rRT-PCR or antibody serologic tests. Therefore, our ability to assess the extent of the SARS-CoV-2 spread among the NC was practically absent. Moreover, under this limitation, we were unable to evaluate whether specific organizational restrictions did prevent asymptomatic COVID-19 carriers from infecting other soldiers. Because of security restrictions, we were unable to present all rough numbers.
CONCLUSIONS
In the short term, the actions taken to limit the COVID-19 effect on the military personnel enabled to lead a risk-management policy without defecting the available workforce scales. At this time point, we were unable to evaluate the long-term effects of these actions, and follow-up studies are required.
ACKNOWLEDGMENTS
We thank Eran Biton MA and Taher sirhan R.N., and all the medical personnel in the IDF for their significant contribution in the fight against COVID-19.
REFERENCES
- 1. WHO : Pneumonia of unknown cause—China. Available athttps://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/; accessed, March 20, 2020.
- 2. World Health Organization : WHO characterizes COVID-19. Available at https://scholar.google.com/scholar?hl=iw&as_sdt=0%2C5&q=World+Health+Organization+.+WHO+characterizes+COVID-19+as+a+pandemic+-+11+March+2020.+2020&btnG; accessed April 24, 2020.
- 3. Nishiura H, Kobayashi T, Miyama T, et al. : Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis 2020; 94, 154–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guan W, Ni Z, Hu Y, et al. : Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382: 1708–20. Available athttp://www.nejm.org/doi/10.1056/NEJMoa2002032; accessed March 20, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guo YR, Cao QD, Hong ZS, et al. : The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—an update on the status. Mil Med Res 2020; 7: 11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E et al. : Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020; 34: 101623 Available athttps://linkinghub.elsevier.com/retrieve/pii/S1477893920300910; accessed March 22, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li L-Q, Huang T, Wang Y-Q, et al. : Novel coronavirus patients’ clinical characteristics, discharge rate and fatality rate of meta-analysis. J Med Virol 2020; 577–83. Available athttp://www.ncbi.nlm.nih.gov/pubmed/32162702; accessed March 22, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu Z, McGoogan JM: Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 1239–42. Available athttp://www.ncbi.nlm.nih.gov/pubmed/32091533; accessed March 22, 2020. [DOI] [PubMed] [Google Scholar]
- 9. Zhou F, Yu T, Du R, et al. : Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395(10229): 1054–62. Available at 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ministry of Health The novel coronavirus. Available athttps://www.health.gov.il/English/Topics/Diseases/corona/Pages/default.aspx; accessed March 28, 2020.
- 11. Wang W, Xu Y, Gao R, et al. : Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020; 323(18): 1843–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chan JF-W, Yip CC-Y, To KK, et al. : Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol 2020; 58(5): pii: e00310–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou T-T, Wei F-X: Primary stratification and identification of suspected corona virus disease 2019 (COVID-19) from clinical perspective by a simple scoring proposal. Mil Med Res 2020; 7(1): –16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li Q, Guan X, Wu P, et al. : Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020; 382(13): 1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bwire GM, Paulo LS: Coronavirus disease-2019: is fever an adequate screening for the returning travelers? Trop Med Health 2020; 48(1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jin YH, Cai L, Cheng ZS, et al. : A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 2020; 7: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. CDC : Guidance for outpatient and ambulatory care settings. Available athttps://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html; accessed, April 25, 2020.
- 18. WHO : Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (COVID-19) outbreak. Available athttps://www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak; accessed, April 24, 2020.
- 19. Klompas M, Morris CA, Sinclair J, et al. : Universal masking in hospitals in the Covid-19 era. N Engl J Med 2020; 382(21): e63. [DOI] [PubMed] [Google Scholar]
- 20. Grinshpun SA, Haruta H, Eninger RM, et al. : Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Environ Hyg 2009; 6(10): 593–603. Available athttp://www.tandfonline.com/doi/abs/10.1080/15459620903120086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Verbeek JH, Rajamaki B, Ijaz S, et al. : Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev 2016; 2016. doi: 10.1002/14651858.CD011621.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lockhart SL, Duggan LV, Wax RS, et al. : Personal protective equipment (PPE) for both anesthesiologists and other airway managers: principles and practice during the COVID-19 pandemic. Can J Anesth 2020. Available athttp://link.springer.com/10.1007/s12630-020-01673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lai CC, Liu YH, Wang CY, et al. : Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. J Microbiol Immunol Infect 2020. doi: 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rothe C, Schunk M, Sothmann P, et al. : Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020; 382: 970–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. He F, Deng Y, Li W: Coronavirus disease 2019 (COVID-19): what we know. J Med Virol 2020. doi: 10.1002/jmv.25766 Available athttps://onlinelibrary.wiley.com/doi/abs/10.1002/jmv.25766; accessed March 4, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Livingston E, Bucher K: Coronavirus disease 2019 (COVID-19) in Italy. JAMA 2020. doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 27. CDC : Interim U.S. Guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease 2019 (COVID-19). Available athttps://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html; accessed April 24, 2020.
- 28. Environmental cleaning and disinfecting principles for health and residential care facilities-version 2 coronavirus disease (COVID-19). Available atwww.health.gov.au/covid19-resources; accessed April 25, 2020.
- 29. CDC : Interim recommendations for US community facilities with suspected/confirmed coronavirus disease 2019. Available athttps://www.cdc.gov/coronavirus/2019-ncov/community/organizations/cleaning-disinfection.html; accessed April 25, 2020.
- 30. World Health Organization Infection prevention and control guidance for long-term care facilities in the context of COVID-19: interim guidance, 21 March 2020. World Health Organization 2020. Available at https://apps.who.int/iris/handle/10665/331508. License: CC BY-NC-SA 3.0 IGO; accessed March 4, 2020.
- 31. Greenhalgh T, Wherton J, Shaw S, Morrison C: Video consultations for Covid-19. BMJ 2020; 368: m998 Available athttp://www.bmj.com/lookup/doi/10.1136/bmj.m998; accessed March 22, 2020. [DOI] [PubMed] [Google Scholar]
- 32. CDC : Interim guidance for emergency medical services (EMS) systems and 911 public safety answering points (PSAPs) for COVID-19 in the United States. Available athttps://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-for-ems.html; accessed April 25, 2020.
- 33. CDC : Using personal protective equipment (PPE). Available athttps://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html; accessed April 25, 2020.
- 34. Cohen JM: Remarkable solutions to impossible problems lessons for malaria from the eradication of smallpox. Malar J 2019; 18: 323 Available athttp://www.ncbi.nlm.nih.gov/pubmed/31547809; accessed March 22, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lu J, Gu J, Li K, et al. : COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg Infect Dis 2020; 26(7). doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Doremalen N, Bushmaker T, Morris DH, et al. : Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382(16): 1564–7. Available athttp://www.ncbi.nlm.nih.gov/pubmed/32182409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ong SWX, Tan YK, Chia PY, et al. : Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020; 323(16). doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Doremalen N, Bushmaker T, Morris DH, et al. : Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382(16). doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. : Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev 2020; 4: CD013574. doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R: Features, evaluation and treatment coronavirus (COVID-19). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. Jan–. 2020. [PubMed] [Google Scholar]
- 41. Wang D, Hu B, Hu C, et al. : Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323(11): 1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chan JFW, Yuan S, Kok KH, et al. : A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020; 395(10223): 514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lai C-C, Liu YH, Wang C-Y, et al. : Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. J Microbiol Immunol Infect 2020. doi: 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yang X, Yu Y, Xu J, et al. : Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cai H: Sex difference and smoking predisposition in patients with COVID-19. Lanct Respir Med 2020; 84(4): e20 Available at 10.1016/S2213-2600. [DOI] [PMC free article] [PubMed] [Google Scholar]


