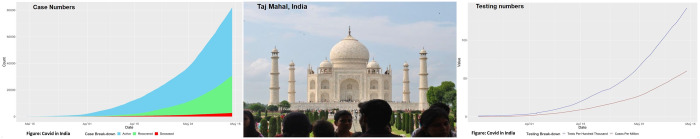
Given its vast population of 1.35 billion people and being the second most populous country in the world, there was a nervous expectation that India would be overwhelmed with COVID-19 patients and the health system would be unable to cope with this surge. Therefore, India was viewed by the world with concerns about containment strategies, and the ability to cope in preventing and managing COVID-19. At the time of writing (12 May 2020), India reported ∼70 827 cases of COVID-19 and ∼2294 deaths.
The World Health Organization (WHO) confirmed on 12 January 2020 that a novel coronavirus was the cause of respiratory illness in Wuhan city, China. Since then, the disease has been declared a pandemic and has spread unabated, particularly in the global north. India reported its first case of COVID-19 on 30 January. No significant spread was observed in February. However, on 4 March, 22 new cases were diagnosed mainly among an Italian tourist group. The transmission escalated from then and spread across the entire Indian subcontinent, with most cases linked to people with a travel history from affected countries. On 12 March, a 76-year-old man who returned from Saudi Arabia became the first fatality. Since then, the spread of the infection has continued at a variable pace in all the Indian states, with no area of the country spared. The largest concentration of cases has been in the metropolitan cities of New Delhi, Mumbai, Ahmedabad, and Chennai.
Government response
The Government of India was quick to recognize the threat of COVID-19 and introduced a series of steps expeditiously to contain the transmission, which has received widespread appreciation. Protective measures such as thermal screening, travel history, securing symptoms of the disease, and airport screening began at the end of January. The Government also started dedicated and aggressive public awareness campaigns through multiple media channels.
The innovative messages and mode of communication were effective in convincing the public to react enthusiastically and in a spirited manner to the Government’s directive, including a countrywide lockdown, which began on 24 March. This unprecedented response to these sudden measures was accepted and well coordinated by implementing disease mitigation efforts by the state governments.
Physical distancing, personal hygiene, and use of face masks were emphasized and are widely practised, with remarkable compliance. After the completion of 3 weeks of the first lockdown, it was further extended by an additional 5 weeks. No country has witnessed such a widespread yet prolonged lockdown. The Government has introduced and implemented a series of innovations including a novel smartphone application called Aarogya Setu for contact tracing and aiding in quarantine and related containment measures.1
Testing
Initially, the testing for coronavirus was limited to those high-risk patients characterized by a variable combination of symptoms, close contacts, and travel history. The testing has been further expanded to several categories in consultation with the state governments. As of 10 May, 1.6 million tests have been conducted, with 64 558 positive individuals, yielding 4% positivity in the country. The debate continues on whether to expand the testing.
Community transmission
With the progression of the outbreak in India, a major controversy concerns community transmission. The Ministry of Health has reiterated that India has not entered stage 3, and the World Health Organization has supported this assertion. Several other experts in the country argue that there is widespread community transmission. This discordance may be due to lack of a clear definition of what constitutes community transmission for countries such as India. While the assertion ‘absence of evidence is not evidence of absence’ holds good here too, there has also been no evident surge in manifest cases overwhelming the health system warranting any such suspicion. The testing strategy has been revised many times, and tests have increased many fold. With indigenous enzyme-linked immunosorbent assay (ELISA) tests added as of 10 May, the Government is on the path towards defining what proportion of positivity for COVID-19 in severe community-acquired respiratory infections (SARIs) will constitute stage 3 transmission.2
Clinical management of COVID-19 in India
While the clinical management of COVID is similar to that of other countries, there are certain differences. For example, the Indian Council of Medical Research (ICMR) task force recommended chemoprophylaxis with hydroxychloroquine (HCQ), 400 mg twice a day, and 400 mg once a week thereafter. This is prescribed for asymptomatic healthcare workers who are treating patients with suspected or confirmed COVID-19 and also for asymptomatic household contacts of confirmed cases.3 Empirical therapy includes neuraminidase inhibitors such as oseltamivir for the treatment of influenza when there is a strong suspicion due to local factors or in the presence of exposure to animal influenza viruses. Patients’ comorbid conditions are to be identified before initiation of treatment.4
There are set protocols in terms of admission and discharges. Several hospitals have been designated as COVID hospitals, and also many hospitals triage these patients at registration to fever clinics or specialized areas within the hospitals. All confirmed patients with symptoms are admitted and managed based on their severity.5
While anecdotal reports suggest that all persons with COVID-19 are treated with HCQ, a combination of HCG 400 mg twice a day for 1 day followed by 200 mg twice a day for 4 days and azithromycin 500 mg once a day for 5 days is recommended as an off-label indication in patients with severe disease requiring intensive care management.4
How are patients with established CVD or risk factors coping?
It is well known that Indians have a high propensity for cardiovascular disease (CVD) and diabetes. There are currently 79 million individuals with diabetes and 200 million individuals with hypertension. Anecdotal evidence suggests there has been a substantial reduction in patients with acute coronary syndrome (ACS) attending emergency departments. Whether this is real or artificial is unknown at the moment. From previous registries, we know that patients largely use public or private transport to reach hospitals when they develop symptoms of ACS. Given the lack of public transportation and severe restriction of vehicles on the roads, it may be particularly difficult to reach hospitals from rural and far-flung areas. Talking to a cross-section of cardiologists, we have the impression that most CVD cases reach the hospital in the end stages. Women and the elderly traditionally avoid hospitals, and an empirical evaluation is needed to assess the impact of COVID on CVD in these populations. Given the economic difficulties as well as the additional efforts in obtaining drugs, we speculate poor compliance with antidiabetic, antihypertensive, and lipid-lowering drugs.
Challenges and opportunities for India in 2020 and beyond
Vaccine development
The world is witnessing a race of sorts in finding a vaccine for COVID-19. Given its experience in producing several vaccines on a large scale, India has a head start in terms of vaccine development. The Government aims to develop a vaccine through a public–private partnership, the National Institute of Virology (NIV).6 This joint initiative will seek fast-track approvals to expedite vaccine development, subsequent animal studies, and clinical evaluation of the candidate vaccine. The Translational Health Science and Technology Institute, an autonomous institution of the Government of India, has announced that six companies are working towards developing a vaccine.7
Pandemic preparedness
The measures that India has taken now have leveraged the capacity of India to fight future pandemics. This pandemic paved the way for an evaluation of the health system to help understand the strengths and weaknesses of the system. A large number of funding agencies have come forward to support the COVID-19 response in India. More than ever before, greater emphasis on strengthening the public health system in India is imperative. India has proved its capability in terms of polio eradication and is emerging as a leader in helping other countries in managing a COVID-19 response. However, the greatest emphasis now is on gearing up the surveillance systems in India to prevent, address, and mitigate the effects related to any pandemic diseases in the future. While the pandemic has widened the gap between the rich and poor in India, health inequities can worsen in the immediate term and can have long-term consequences.
Changes in healthcare
The Medical Council of India amended its rules to facilitate Tele consultations, and telehealth is likely to be here to stay.
The India case study
India’s COVID-19 is unique in several ways. Some sceptics believe that India may not be doing well and, with the lifting of the lockdown, there will be a huge surge in cases. However, the reality indicates that there is no apparent surge in cases, and the healthcare system is not stretched—many blame the low testing rates in India to explain the relatively lower case burden in India. However, the declining test positivity rate in all the south Indian states indicates that there are not many cases as of now. Several hypotheses have attracted interest, including the protection offered by a warmer climate, malaria-prone country, and BCG vaccine.8 While these are yet to be proven, the lower mortality rates in India are most probably explained by the demographic advantage of a higher proportion of young people.
So far, the proactive measures taken by the Government of India have helped in delaying the surge in cases effectively. India had the advantage that it could prepare well based on the errors of other countries and acted in a timely manner in the early phase of the outbreak. It appears that India has flattened the curve, but the looming question is will there be a surge with the lifting of lockdown, and how do we prevent a second wave?
The COVID-19 pandemic reflects the classic Hamletian dilemma for the policymakers when lives and livelihood are competing with each other. While the efforts so far have been good, the country looks for a breakthrough in drug trials and vaccine production.
India is also currently evaluating several pharmaceuticals, biotechnology, and immunology technologies to face COVID-19 challenges. The real impact of the pandemic in India on all segments of the society will only be known when the lockdown is lifted, and a new ‘normalcy’ is established.
Supplementary Material
Acknowledgements
We thank Daisy A. John and Ms N. Madhavi Latha for review and proofreading.
Published simultaneously with the Journal of Hypertension
References
References are available as supplementary material at European Heart Journal online.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.